Abstract
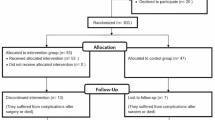
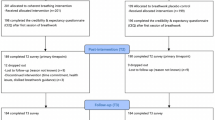
Physicians face intense work-related stress, which can harm their health, increase the risk of medical errors, lower healthcare quality, and increase costs within the healthcare system. In this 4-week intervention study, individual-level and population-level effects of two short and easy-to-perform breathing exercises designed to reduce stress are evaluated among 76 physicians in residency in Germany in a series of N-of-1 trials. Levels of stress and levels of stress expected for the following day were assessed electronically every day via the StudyU App (protocol adherence: 91.9%). Average intervention effects were estimated using Bayesian linear regression models. They were overall small on the population level, but they showed large heterogeneity between individuals, with strong effects for selected individuals, with stress reduction of up to 3 points on a 1 to 10 stress scale. Thirty-one participants benefited from the anti-stress exercises. Three (mindfulness breathing) and seven participants (box breathing) had a ≥70% probability for a daily stress reduction of ≥0.5 points and thereby fulfilled our responder criteria. Of the 17 participants who completed the follow-up survey about 4.5 months after completion of the individual N-of-1 trials, 58% reported that they felt they had benefited from the intervention and 42% planned to use it in the future. The results highlight the value of personalized perspectives: while the studied interventions showed only small positive benefits for the “average person”, they may well help actual individual persons, here 10 of 76 or even 31 of 76 participants.
Similar content being viewed by others
Data availability
The study setup, all information on the protocol of the conducted N-of-1 trials as well as all data collected as part of the N-of-1 trials are publicly available through the StudyU data repository at https://designer.studyu.health (mindfulness breathing: “ASIP-Studie: Anti-Stress Übung”, box breathing: “ASIP-Studie: Box-Atmung”). All data used to produce the results shown in this manuscript (including the data from the baseline and follow-up questionnaires collected through REDCap) are published at https://github.com/HIAlab/ASIP. Statistical code used to produce all statistical analyses and figures is available at https://github.com/HIAlab/ASIP.
References
Stucky, E. R. et al. Intern to attending: assessing stress among physicians. Acad. Med. 84, 251–257 (2009).
Wallace, J. E., Lemaire, J. B. & Ghali, W. A. Physician wellness: a missing quality indicator. Lancet 374, 1714–1721 (2009).
Thompson, W. T. et al. Challenge of culture, conscience, and contract to general practitioners’ care of their own health: qualitative study. BMJ 323, 728–731 (2001).
Fahrenkopf, A. M. et al. Rates of medication errors among depressed and burnt out residents: prospective cohort study. BMJ 336, 488–491 (2008).
Shanafelt, T. D. et al. Burnout and self-reported patient care in an internal medicine residency program. Ann. Intern. Med. 136, 358–367 (2002).
Goehring, C. et al. Psychosocial and professional characteristics of burnout in Swiss primary care practitioners: a cross-sectional survey. Swiss Med. Wkly. 135, 101–108 (2005).
Dyrbye, L. N. et al. Association of clinical specialty with symptoms of burnout and career choice regret among US resident physicians. JAMA 320, 1114–1130 (2018).
Klein, J. et al. Burnout and perceived quality of care among German clinicians in surgery. Int. J. Qual. Health Care 22, 525–530 (2010).
Ramirez, A. et al. Burnout and psychiatric disorder among cancer clinicians. Br. J. Cancer 71, 1263–1269 (1995).
Dyrbye, L. N. et al. Burnout and suicidal ideation among US medical students. Ann. Intern. Med. 149, 334–341 (2008).
Hsu, K. & Marshall, V. Prevalence of depression and distress in a large sample of. Am. J. Psychiatry 144, 1561–1566 (1987).
Raspe, M. et al. Arbeitsbedingungen und Gesundheitszustand junger Ärzte und professionell Pflegender in deutschen Krankenhäusern. Bundesgesundheitsblatt Gesundheitsforsch. Gesundheitsschutz 63, 113–121 (2020).
Frank, E. & Dingle, A. D. Self-reported depression and suicide attempts among US women physicians. Am. J. Psychiatry 156, 1887–1894 (1999).
Graham, J. et al. How hospital consultants cope with stress at work: implications for their mental health. Stress Health. 17, 85–89 (2001).
Van der Heijden, F. et al. Suicidal thoughts among medical residents with burnout. Arch. Suicide Res. 12, 344–346 (2008).
Panagopoulou, E., Montgomery, A. & Benos, A. Burnout in internal medicine physicians: differences between residents and specialists. Eur. J. Intern. Med. 17, 195–200 (2006).
Cannon, W. B. Bodily changes in pain, hunger, fear, and rage (D. Appleton and Company, 1915).
Chrousos, G. P. Stress and disorders of the stress system. Nat. Rev. Endocrinol. 5, 374–381 (2009).
Cohen, S., Janicki-Deverts, D. & Miller, G. E. Psychological stress and disease. JAMA 298, 1685–1687 (2007).
Chrousos, G. P. and P.W. Gold, The concepts of stress and stress system disorders: overview of physical and behavioral homeostasis. JAMA 267, 1244–1252 (1992).
McEwen, B. S. Protective and damaging effects of stress mediators. N. Engl. J. Med. 338, 171–179 (1998).
Cohen, S., Kessler, R. C. & Gordon, L. U. Strategies for measuring stress in studies of psychiatric and physical disorders. in Measuring Stress: a Guide for Health and Social Scientists, Vol 28, 3–26 (Oxford Academic, 1995).
Dhabhar, F. S. Effects of stress on immune function: the good, the bad, and the beautiful. Immunol. Res. 58, 193–210 (2014).
Padro, C. J. & Sanders, V. M. Neuroendocrine regulation of inflammation. Semin. Immunol. 26, 357–368 (2014).
Sweitzer, M. M. et al. Delay discounting and smoking: association with the Fagerström test for nicotine dependence but not cigarettes smoked per day. Nicotine Tob. Res. 10, 1571–1575 (2008).
Pomerleau, O. F. & Pomerleau, C. S. Research on stress and smoking: progress and problems. Br. J. Addict. 86, 599–603 (1991).
Sinha, R. Chronic stress, drug use, and vulnerability to addiction. Ann. N. Y. Acad. Sci. 1141, 105–130 (2008).
Fields, S. A. et al. The relationship between stress and delay discounting: a meta-analytic review. Behav. Pharmacol. 25, 434–444 (2014).
Miller, G. E., Cohen, S. & Ritchey, A. K. Chronic psychological stress and the regulation of pro-inflammatory cytokines: a glucocorticoid-resistance model. Health Psychol. 21, 531 (2002).
Kivimäki, M. et al. Work stress in the etiology of coronary heart disease—a meta-analysis. Scand. J. Work Environ. Health 32, 431–442 (2006).
Turner, A. I. et al. Psychological stress reactivity and future health and disease outcomes: a systematic review of prospective evidence. Psychoneuroendocrinology 114, 104599 (2020).
Firth-Cozens, J. & Greenhalgh, J. Doctors’ perceptions of the links between stress and lowered clinical care. Soc. Sci. Med. 44, 1017–1022 (1997).
Yates, S. W. Physician stress and burnout. Am. J. Med. 133, 160–164 (2020).
Pottier, P. et al. Effect of stress on clinical reasoning during simulated ambulatory consultations. Med. Teach. 35, 472–480 (2013).
Tawfik, D. S. et al. Physician burnout, well-being, and work unit safety grades in relationship to reported medical errors. Mayo Clin. Proc. 93, 1571–1580 (2018).
Owoc, J. et al. Burnout, well being, and self reported medical errors among physicians. Pol. Arch. Intern. Med. 131, 626–632 (2021).
Brown, S. D., Goske, M. J. & Johnson, C. M. Beyond substance abuse: stress, burnout, and depression as causes of physician impairment and disruptive behavior. J. Am. Coll. Radiol. 6, 479–485 (2009).
Van den Hombergh, P. et al. High workload and job stress are associated with lower practice performance in general practice: an observational study in 239 general practices in the Netherlands. BMC Health Serv. Res. 9, 1–8 (2009).
West, C. P. et al. Association of resident fatigue and distress with perceived medical errors. JAMA 302, 1294–1300 (2009).
Shanafelt, T. D. et al. Burnout and medical errors among American surgeons. Ann. Surg. 251, 995–1000 (2010).
Halbesleben, J. R. & Rathert, C. Linking physician burnout and patient outcomes: exploring the dyadic relationship between physicians and patients. Health Care Manag. Rev. 33, 29–39 (2008).
Regehr, C. et al. Interventions to reduce the consequences of stress in physicians: a review and meta-analysis. J. Nerv. Ment. Dis. 202, 353–359 (2014).
Shanafelt, T., Goh, J. & Sinsky, C. The business case for investing in physician well-being. JAMA Intern. Med. 177, 1826–1832 (2017).
Han, S. et al. Estimating the attributable cost of physician burnout in the United States. Ann. Intern. Med. 170, 784–790 (2019).
Willard-Grace, R. et al. Burnout and health care workforce turnover. Ann. Fam. Med. 17, 36–41 (2019).
Rutledge, T. et al. A real-time assessment of work stress in physicians and nurses. Health Psychol. 28, 194 (2009).
Linzer, M. et al. Predicting and preventing physician burnout: results from the United States and the Netherlands. Am. J. Med. 111, 170–175 (2001).
Taylor, H., Strauss, C. & Cavanagh, K. Can a little bit of mindfulness do you good? A systematic review and meta-analyses of unguided mindfulness-based self-help interventions. Clin. Psychol. Rev. 89, 102078 (2021).
Zaccaro, A. et al. How breath-control can change your life: a systematic review on psycho-physiological correlates of slow breathing. Front. Human Neurosci. 12, 353 (2018).
Röttger, S. et al. The effectiveness of combat tactical breathing as compared with prolonged exhalation. Appl. Psychophysiol. Biofeedback 46, 19–28 (2021).
Bouchard, S. et al. Using biofeedback while immersed in a stressful videogame increases the effectiveness of stress management skills in soldiers. PloS ONE 7, e36169 (2012).
Dillard, C. C. et al. Slow breathing reduces biomarkers of stress in response to a virtual reality active shooter training drill. Healthcare 11, 2351 (2023).
Balban, M. Y. et al. Brief structured respiration practices enhance mood and reduce physiological arousal. Cell Rep. Med. 4, 100895 (2023).
Fincham, G. W. et al. Effect of breathwork on stress and mental health: a meta-analysis of randomised-controlled trials. Sci. Rep. 13, 432 (2023).
Boettcher, J. et al. Internet-based mindfulness treatment for anxiety disorders: a randomized controlled trial. Behav. Ther. 45, 241–253 (2014).
Carrington, P. et al. The use of meditation–relaxation techniques for the management of stress in a working population. J. Occup. Environ. Med. 22, 221–231 (1980).
Kühberger, A. et al. The significance fallacy in inferential statistics. BMC Res. Notes 8, 84 (2015).
McShane, B. B. et al. Abandon statistical significance. Am. Stat. 73, 235–245 (2019).
Wasserstein, R. L., Schirm, A. L. & Lazar, N. A. Moving to a world beyond “p< 0.05”, 1–19 (Taylor & Francis, 2019).
Witmer, J. (ed.) Journal of Statistics Education, Vol 27, 136–137 (2019).
Rosenberg, A. & Hamiel, D. Reducing test anxiety and related symptoms using a biofeedback respiratory practice device: a randomized control trial. Appl. Psychophysiol. Biofeedback 46, 69–82 (2021).
James, T. A., James, D. & Larkey, L. K. Heart-focused breathing and perceptions of burden in Alzheimer’s caregivers: An online randomized controlled pilot study. Geriatr. Nurs. 42, 397–404 (2021).
Goodwin, A. M. et al. Protocol for randomized personalized trial for stress management compared to standard of care. Front. Psychol. 14, 1233884 (2023).
Zainal, N. H. & Newman, M. G. Mindfulness enhances cognitive functioning: a meta-analysis of 111 randomized controlled trials. Health Psychol. 18, 369–395 (2024).
Holman, D., Johnson, S. & O’Connor, E. Stress management interventions: improving subjective psychological well-being in the workplace. In Handbook of well-being, 1–13 (DEF, 2018).
Nikles, J. & Mitchell, G. The essential guide to N-of-1 trials in health, Vol. 10 (Springer, 2015).
Hawksworth, O. et al. A methodological review of randomised n-of-1 trials. Trials 25, 263 (2024).
Zhou, L. et al. Analyzing population-level trials as N-of-1 trials: an application to gait. Contemp. Clin. Trials Commun. 38, 101282 (2024).
Vetter, V. M., Kurth, T. and Konigorski, S. Evaluation of easy-to-implement anti-stress interventions in a series of N-of-1 trials: study protocol of the anti-stress intervention among physicians study. Front. Psychiatry 15, 1420097 (2024).
Daza, E. J. Causal analysis of self-tracked time series data using a counterfactual framework for N-of-1 Trials. Methods Inf. Med 57, e10–e21 (2018).
Piccininni, M. et al. Causal inference for N-of-1 trials. Preprint at arXiv https://doi.org/10.48550/arXiv.2406.10360.
Collins, F. S. & Varmus, H. A new initiative on precision medicine. N. Engl. J. Med. 372, 793–795 (2015).
Schork, N. J. Personalized medicine: time for one-person trials. Nature 520, 609–611 (2015).
Ginsburg, G. S. & Phillips, K. A. Precision medicine: from science to value. Health Aff. 37, 694–701 (2018).
Kim-McManus, O. et al. A framework for N-of-1 trials of individualized gene-targeted therapies for genetic diseases. Nat. Commun. 15, 9802 (2024).
Guyatt, G. et al. Determining optimal therapy—randomized trials in individual patients. N. Engl. J. Med. 314, 889–892 (1986).
Gabler, N. B. et al. N-of-1 trials in the medical literature: a systematic review. Med. Care 49, 761–768 (2011).
Kravitz, R. L. et al. Effect of Mobile device–supported single-patient multi-crossover trials on treatment of chronic musculoskeletal pain: a randomized clinical trial. JAMA Intern. Med. 178, 1368–1377 (2018).
Nurmi, J. et al. Biofeedback and digitalized motivational interviewing to increase daily physical activity: series of factorial N-of-1 randomized controlled trials piloting the precious app. JMIR Form. Res. 7, e34232 (2023).
Sniehotta, F. F. et al. Testing self-regulation interventions to increase walking using factorial randomized N-of-1 trials. Health Psychol. 31, 733 (2012).
Justo, C. F. Reducción de los niveles de estrés y ansiedad en médicos de Atención Primaria mediante la aplicación de un programa de entrenamiento en conciencia plena (mindfulness). Aten. Primaria 42, 564–570 (2010).
McCue, J. D. & Sachs, C. L. A stress management workshop improves residents’ coping skills. Arch. Intern. Med. 151, 2273–2277 (1991).
Saadat, H. et al. Wellness program for anesthesiology residents: a randomized, controlled trial. Acta Anaesthesiol. Scand. 56, 1130–1138 (2012).
Sood, A. et al. Stress management and resilience training among Department of Medicine faculty: a pilot randomized clinical trial. J. Gen. Intern. Med. 26, 858–861 (2011).
Schumer, M. C., Lindsay, E. K. & Creswell, J. D. Brief mindfulness training for negative affectivity: a systematic review and meta-analysis. J. Consult Clin. Psychol. 86, 569–583 (2018).
Creswell, J. D. Mindfulness interventions. Annu. Rev. Psychol. 68, 491–516 (2017).
Kristensen, T. S. et al., The Copenhagen Psychosocial Questionnaire-a tool for the assessment and improvement of the psychosocial work environment. Scand. J. Work Environ. Health 31, 438–449 (2005).
Nübling, M. et al. Methoden zur Erfassung psychischer Belastungen—Erprobung eines Messinstrumentes (COPSOQ). in Schriftenreihe der Bundesanstalt für Arbeitsschutz und Arbeitsmedizin (Wirtschaftsverlag NW, 2005).
Siegrist, J. et al. A short generic measure of work stress in the era of globalization: effort–reward imbalance. Int. Arch. Occup. Environ. Health 82, 1005–1013 (2009).
Klein, E. M. et al. The German version of the Perceived Stress Scale – psychometric characteristics in a representative German community sample. BMC Psychiatry 16, 159 (2016).
Braunheim, L. et al. The effects of effort-reward imbalance on the job, overcommitment, and income on life satisfaction in Germany from a longitudinal perspective. Soc. Sci. Med. 341, 116523 (2024).
Janke, S. & Glöckner-Rist, A. Deutsche version der satisfaction with life scale (SWLS). in (eds Danner, D. & Glöckner-Rist, A.) Zusammenstellung sozialwissenschaftlicher Items und Skalen. (Mannheim: GESIS, 2014).
Kase, S. M. et al. A pilot study exploring interventions for physician distress in pediatric subspecialists. Pediatr. Res. 88, 398–403 (2020).
Konigorski, S. et al. StudyU: a platform for designing and conducting innovative digital N-of-1 trials. J. Med. Internet Res. 24, e35884 (2022).
Vohra, S. et al. CONSORT extension for reporting N-of-1 trials (CENT) 2015 statement. BMJ 350, h1738 (2015).
Harris, P. A. et al. The REDCap consortium: building an international community of software platform partners. J. Biomed. Inform. 95, 103208 (2019).
Rödel, A. et al. Fragebogen zur Messung beruflicher Gratifikationskrisen. Z. Differ. Diagn. Psychol. 25, 227–238 (2004).
Cohen, S., Kamarck, T. & Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 24, 385–396 (1983).
Beschoner, P. et al. The prevalence of effort-reward imbalance and its associations with working conditions, psychosocial resources and burden among health care workers during the COVID-19 pandemic: results of the egePan-Voice study. PloS ONE 18, e0287509 (2023).
Koch, P. et al. The effect of effort-reward imbalance on the health of childcare workers in Hamburg: a longitudinal study. J. Occup. Med. Toxicol. 12, 1–9 (2017).
Brooke, J. SUS-A quick and dirty usability scale. Usability Eval. Ind. 189, 4–7 (1996).
Bangor, A., Kortum, P. & Miller, J. Determining what individual SUS scores mean: adding an adjective rating scale. J. Usability Stud. 4, 114–123 (2009).
Yang, J., Steingrimsson, J. A. & Schmid, C. H. Sample size calculations for n-of-1 trials. Preprint at arXiv, https://doi.org/10.48550/arXiv.2110.08970 (2021).
Lesage, F.-X., Berjot, S. & Deschamps, F. Clinical stress assessment using a visual analogue scale. Occup. Med. 62, 600–605 (2012).
Naughton, F. & Johnston, D. A starter kit for undertaking n-of-1 trials. Eur. Health Psychol. 16, 196–205 (2014).
Lu, C. P. et al. The effect of mindfulness-based interventions on reducing stress in future health professionals: a systematic review and meta-analysis of randomized controlled trials. Appl. Psychol. Health Well-Being 16, 765–792 (2023).
R Development Core Team (2010) R: A Language and Environment for Statistical Computing. R Foundation for Statistical computing, Vienna, Austria. http://www.R-project.org.
Acknowledgements
The authors would like to thank Ellen Zitzmann for her valuable input and help in developing the mindfulness-based breathing exercise and recording the intervention audio files.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
V.M.V.: conceptualization, methodology, formal analysis, investigation, data curation, writing—original draft, writing—review and editing, visualization, project administration. T.K.: conceptualization, resources, supervision, writing—review and editing. S.K.: conceptualization, methodology, resources, supervision, writing—review and editing.
Corresponding authors
Ethics declarations
Competing interests
V.M.V.: none. T.K.: reports outside of the submitted, to have received research grants from the German Federal Joint Committee (G-BA). He also received personal compensation from Eli Lilly & Company, Novartis, the BMJ, and Frontiers. S.K.: none.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Vetter, V.M., Kurth, T. & Konigorski, S. Evaluation of two easy-to-implement digital breathing interventions in the context of daily stress levels in a series of N-of-1 trials: results from the Anti-Stress Intervention Among Physicians (ASIP) study. npj Digit. Med. (2026). https://doi.org/10.1038/s41746-025-02317-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41746-025-02317-3