Abstract
Public health campaigns that raise awareness about mental health problems are designed to decrease stigma, increase help-seeking and improve mental health literacy. However, there is some theoretical concern that, alongside benefits, such campaigns might negatively impact how some individuals interpret, label and respond to mental health problems. In this Review, we summarize the extant evidence for the positive and negative psychological impacts of mental health awareness efforts. We integrate theoretical literature with studies using experimental designs in which mental health awareness content is manipulated in a controlled environment that might provide preliminary insights into potential causal relationships. We find that awareness materials can change cognitions and beliefs relating to one’s own mental health and to mental health more generally (such as self-diagnosis and beliefs about recovery). These effects can vary depending on individual characteristics (such as existing symptoms, stability of self-concept and suggestibility), the message being presented, identification with the messenger, and whether there is personalized information about one’s own symptoms. We discuss the implications of this work for adolescent populations and directions for future research.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$59.00 per year
only $4.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Hahn, J. S., Chua, K.-C., Jones, R. & Henderson, C. The Every Mind Matters campaign: changes in mental health literacy and its associations with campaign awareness. Eur. J. Public Health 33, 1008–1013 (2023).
Henderson, C., Potts, L. & Robinson, E. J. Mental illness stigma after a decade of Time to Change England: inequalities as targets for further improvement. Eur. J. Public Health 30, 497–503 (2020).
Hoover, S. & Bostic, J. Schools as a vital component of the child and adolescent mental health system. Psychiat. Serv. 72, 37–48 (2021).
Lever, N. et al. Using the whole school, whole community, whole child model to support mental health in schools. J. Sch. Health 94, 200–203 (2024).
March, A., Stapley, E., Hayes, D., Town, R. & Deighton, J. Barriers and facilitators to sustaining school-based mental health and wellbeing interventions: a systematic review. Int. J. Environ. Res. Public Health 19, 3587 (2022).
Draganidis, A., Fernando, A. N., West, M. L. & Sharp, G. Social media delivered mental health campaigns and public service announcements: a systematic literature review of public engagement and help-seeking behaviours. Soc. Sci. Med. 359, 117231 (2024).
Foulkes, L. & Andrews, J. L. Are mental health awareness efforts contributing to the rise in reported mental health problems? A call to test the prevalence inflation hypothesis. N. Ideas Psychol. 69, 101010 (2023).
Booth, R. G., Allen, B. N., Bray Jenkyn, K. M., Li, L. & Shariff, S. Z. Youth mental health services utilization rates after a large-scale social media campaign: population-based interrupted time-series analysis. JMIR Ment. Health 5, e27 (2018).
Durlak, J. A., Mahoney, J. L. & Boyle, A. E. What we know, and what we need to find out about universal, school-based social and emotional learning programs for children and adolescents: a review of meta-analyses and directions for future research. Psychol. Bull. 148, 765–782 (2022).
Werner-Seidler, A. et al. School-based depression and anxiety prevention programs: an updated systematic review and meta-analysis. Clin. Psychol. Rev. 89, 102079 (2021).
Ecclestone, K. Resisting images of the ‘diminished self’: the implications of emotional well-being and emotional engagement in education policy. J. Educ. Policy 22, 455–470 (2007).
Wright, K. Student wellbeing and the therapeutic turn in education. Aust. Educ. Dev. Psychol. 31, 141–152 (2014).
Cuijpers, P. Universal prevention of depression at schools: dead end or challenging crossroad? Evidence-based Ment. Health 25, 96–98 (2022).
Foulkes, L. & Stringaris, A. Do no harm: can school mental health interventions cause iatrogenic harm? BJPsych Bull. 47, 267–269 (2023).
Guzman-Holst, C., Streckfuss Davis, R., Andrews, J. L. & Foulkes, L. Scoping review: potential harm from school-based group mental health interventions. Child Adolesc. Ment. Health 30, 208–222 (2025).
Kearney, C. A. The perniciousness and promise of school-based mental health service delivery for youth. Res. Child. Adolesc. Psychopathol. 53, 609–624 (2025).
Beeker, T. et al. Psychiatrization of society: a conceptual framework and call for transdisciplinary research. Front. Psychiatry 12, 645556 (2021).
Underhill, R. & Foulkes, L. Self-diagnosis of mental disorders: a qualitative study of attitudes on Reddit. Qual. Health Res. 35, 779–792 (2025).
Lane, R. “He doesn’t really have bipolar …”. The rise of strategic essentialism and diagnostic possessiveness in bipolar disorder. SSM Ment. Health 5, 100299 (2024).
Dakin, B. C., McGrath, M. J., Rhee, J. J. & Haslam, N. Broadened concepts of harm appear less serious. Soc. Psychol. Personal. Sci. 14, 72–83 (2023).
Haslam, N. Concept creep: psychology’s expanding concepts of harm and pathology. Psychol. Inq. 27, 1–17 (2016).
Tam, M. T., Wu, J. M., Zhang, C. C., Pawliuk, C. & Robillard, J. M. A systematic review of the impacts of media mental health awareness campaigns on young people. Health Prom. Pract. 25, 907–920 (2024).
Walsh, D. A. B. & Foster, J. L. H. A call to action. A critical review of mental health related anti-stigma campaigns. Front. Public Health 8, 569539 (2021).
Evans-Lacko, S., Corker, E., Williams, P., Henderson, C. & Thornicroft, G. Effect of the time to change anti-stigma campaign on trends in mental-illness-related public stigma among the English population in 2003–13: an analysis of survey data. Lancet Psychiatry 1, 121–128 (2014).
Ronaldson, A. & Henderson, C. Investigating changes in mental illness stigma and discrimination after the Time To Change programme in England. BJPsych Open 10, e199 (2024).
Reavley, N. J. & Jorm, A. F. Public recognition of mental disorders and beliefs about treatment: changes in Australia over 16 years. Br. J. Psychiatry 200, 419–425 (2012).
Jorm, A. F., Christensen, H. & Griffiths, K. M. The impact of Beyond Blue: the national depression initiative on the Australian public’s recognition of depression and beliefs about treatments. Aust. NZ J. Psychiatry 39, 248–254 (2005).
Donovan, R. J., Drane, C. F., Santini, Z. I. & Jalleh, G. Impact on help-seeking behaviours of a campaign perceived to decrease stigma and increase openness around mental health. Health Prom. J. Aust. 35, 1378–1385 (2024).
Aftab, A. & Druss, B. G. Addressing the mental health crisis in youth — sick individuals or sick societies? JAMA Psychiatry 80, 863 (2023).
Ahuvia, I. L. & Link, B. G. The mental illness self-labeling model: a conceptual model for studying the effects of mental-illness self-labeling on clinical outcomes. Clin. Psychol Sci. 13, 1031–1050 (2025).
Bantjes, J., Hunt, X. & Stein, D. J. Anxious, depressed, and suicidal: crisis narratives in university student mental health and the need for a balanced approach to student wellness. Int. J. Environ. Res. Public Health 20, 4859 (2023).
Coppock, V. Psychiatrised childhoods. Glob. Stud. Child. 10, 3–11 (2020).
Corzine, A. & Roy, A. Inside the black mirror: current perspectives on the role of social media in mental illness self-diagnosis. Discov. Psychol. 4, 40 (2024).
Malla, A. & Gold, I. Public discourse on mental health: a critical view. J. Psychiatry Neurosci. 49, E126–E131 (2024).
Monteith, S. et al. Implications of online self-diagnosis in psychiatry. Pharmacopsychiatry 57, 45–52 (2024).
Samuel, L., Kuijpers, K. & Bleakley, A. TherapyTok for depression and anxiety: a quantitative content analysis of high engagement Tiktok videos. J. Adolesc. Health 74, 1184–1190 (2024).
Tsou, J. Y. Hacking on the looping effects of psychiatric classifications: what is an interactive and indifferent kind? Int. Stud. Phil. Sci. 21, 329–344 (2007).
Coppock, V. Liberating the mind or governing the soul? Psychotherapeutic education, children’s rights and the disciplinary state. Educ. Inq. 2, 385–399 (2011).
Foulkes, L. & Stapley, E. Want to improve school mental health interventions? Ask young people what they actually think. J. Phil. Educ. 56, 41–50 (2022).
Frawley, A., Wakeham, C., McLaughlin, K. & Ecclestone, K. Constructing a crisis: mental health, higher education and policy entrepreneurs. Sociol. Res. Online 29, 351–369 (2024).
Sullivan, G. M. & Feinn, R. Using effect size — or why the P value is not enough. J. Graduate Med. Educ. 4, 279–282 (2012).
Grant, S. et al. Effectiveness of school-based depression prevention interventions: an overview of systematic reviews with meta-analyses on depression outcomes. J. Consult. Clin. Psychol. 93, 194–212 (2025).
Hayes, D. et al. Universal, school-based, interventions to improve emotional outcomes in children and young people: a systematic review and meta-analysis. Front. Child Adolesc. Psychiatry 4, 1526840 (2025).
Deighton, J. et al. Effectiveness of School Mental Health Awareness Interventions: Universal Approaches in English Secondary Schools (UK Department for Education, 2025).
Harvey, L. J., White, F. A., Hunt, C. & Abbott, M. Investigating the efficacy of a dialectical behaviour therapy-based universal intervention on adolescent social and emotional well-being outcomes. Behav. Res. Ther. 169, 104408 (2023).
Kuyken, W. et al. Effectiveness and cost-effectiveness of universal school-based mindfulness training compared with normal school provision in reducing risk of mental health problems and promoting well-being in adolescence: the MYRIAD cluster randomised controlled trial. Evidence-based Ment. Health 25, 99–109 (2022).
Andrews, J. L. et al. Evaluating the effectiveness of a universal eHealth school-based prevention programme for depression and anxiety, and the moderating role of friendship network characteristics. Psychol. Med. 53, 5042–5051 (2023).
Foulkes, L., Andrews, J. L., Reardon, T. & Stringaris, A. Research recommendations for assessing potential harm from universal school-based mental health interventions. Nat. Ment. Health 2, 270–277 (2024).
Bridgland, V. M. E., Jones, P. J. & Bellet, B. W. A meta-analysis of the efficacy of trigger warnings, content warnings, and content notes. Clin. Psychol. Sci. 12, 751–771 (2024).
Miller, E. J., Crane, C., Medlicott, E., Robson, J. & Taylor, L. Non-positive experiences encountered by pupils during participation in a mindfulness-informed school-based intervention. Sch. Ment. Health 15, 851–872 (2023).
Garmy, P., Berg, A. & Clausson, E. K. A qualitative study exploring adolescents’ experiences with a school-based mental health program. BMC Public Health 15, 1074 (2015).
Lindholm, S. K. & Zetterqvist Nelson, K. “Apparently I’ve got low self-esteem”: schoolgirls’ perspectives on a school-based public health intervention. Child. Soc. 29, 473–483 (2015).
Stapley, E. et al. A qualitative study of English school children’s experiences of two brief, universal, classroom-based mental health and wellbeing interventions: mindfulness and relaxation. Contemp. School Psychol. https://doi.org/10.1007/s40688-025-00567-2 (2025).
Ahuvia, I. L. Refining the prevalence inflation hypothesis: disentangling overinterpretation from self-fulfilling prophecies. N. Ideas Psychol. 75, 101106 (2024).
Ndour, A. & Foulkes, L. The romanticisation of mental health problems in adolescents and its implications: a narrative review. Eur. Child. Adolesc. Psychiatry 34, 2297–2326 (2025).
Acheson, R. & Papadima, M. The search for identity: working therapeutically with adolescents in crisis. J. Child. Psychother. 49, 95–119 (2023).
Chan, D. & Sireling, L. ‘I want to be bipolar’…a new phenomenon. Psychiatrist 34, 103–105 (2010).
Fellowes, S. Self-diagnosis in psychiatry and the distribution of social resources. R. Inst. Phil. Suppl. 94, 55–76 (2023).
Haslam, N. & Tse, J. S. Public awareness of mental illness: mental health literacy or concept creep? Australasian Psychiatry 33, 18–20 (2025).
Rutter, L. A. et al. “I haven’t been diagnosed, but I should be” — insight into self-diagnoses of common mental health disorders: cross-sectional study. JMIR Form. Res. 7, e39206 (2023).
Brinkmann, S. Languages of suffering. Theory Psychol. 24, 630–648 (2014).
David, A. S. & Deeley, Q. Dangers of self-diagnosis in neuropsychiatry. Psychol. Med. 54, 1057–1060 (2024).
Hofmann, B., Reid, L., Carter, S., Rogers, W. et al. Overdiagnosis, one concept, three perspectives, and a model. Eur. J. Epidemiol. 36, 655–656 (2021).
Hasan, F., Foster, M. M. & Cho, H. Normalizing anxiety on social media increases self-diagnosis of anxiety: the mediating effect of identification (but not stigma). J. Health Commun. 28, 563–572 (2023).
Jones, P. J. & McNally, R. J. Does broadening one’s concept of trauma undermine resilience? Psychol. Trauma 14, S131–S139 (2022).
Hardman, C. A. et al. “Food addiction is real”. The effects of exposure to this message on self-diagnosed food addiction and eating behaviour. Appetite 91, 179–184 (2015).
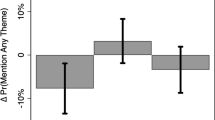
Sandra, D. A. et al. Inform and do no harm: nocebo education reduces false self-diagnosis caused by mental health awareness. Psychol. Med. 55, e330 (2025).
Merckelbach, H., Jelicic, M. & Pieters, M. Misinformation increases symptom reporting: a test–retest study. JRSM Short Rep. 2, 1–6 (2011).
Van Helvoort, D., Otgaar, H. & Merckelbach, H. Worsening of self-reported symptoms through suggestive feedback. Clin. Psychol. Sci. 8, 359–365 (2020).
Jelicic, M., Frederix, M. & Merckelbach, H. Brief report: writing about chronic fatigue increases somatic complaints. Psychol. Top. 22, 405–412 (2013).
Whitted, W. M. et al. Seeing is believing: the effect of subtle communication in social media on viewers’ beliefs about depression and anxiety symptom trajectories. J. Clin. Psychol. 80, 1050–1064 (2024).
Kemp, J. J., Lickel, J. J. & Deacon, B. J. Effects of a chemical imbalance causal explanation on individuals’ perceptions of their depressive symptoms. Behav. Res. Ther. 56, 47–52 (2014).
Ruddock, H. K. et al. Believing in food addiction: helpful or counterproductive for eating behavior? Obesity 24, 1238–1243 (2016).
Siegel, J. T., Flores-Medel, E., Martinez, D. A. & Berger, D. E. Can mental health anti-stigma messages have untoward effects on some people with depression?: an exploratory study. J. Health Commun. 24, 821–828 (2019).
Dolan, P., Hallsworth, M., Halpern, D., King, D. & Vlaev, I. MINDSPACE: Influencing Behaviour for Public Policy (Institute for Government, 2010).
Dolan, P. et al. Influencing behaviour: the mindspace way. J. Econ. Psychol. 33, 264–277 (2012).
Kassin, S. M. Deposition testimony and the surrogate witness: evidence for a ‘messenger effect’ in persuasion. Personal. Soc. Psychol. Bull. 9, 281–288 (1983).
Rooney, T., Sharpe, L., Todd, J., Richmond, B. & Colagiuri, B. The relationship between expectancy, anxiety, and the nocebo effect: a systematic review and meta-analysis with recommendations for future research. Health Psychol. Rev. 17, 550–577 (2023).
Stein, M. V., Heller, M., Chapman, S., Rubin, G. J. & Terhune, D. B. Trait responsiveness to verbal suggestions predicts nocebo responding: a meta-analysis. Br. J. Health Psychol. 30, e12774 (2025).
Marcotulli, D., Foulkes, L. & Stringaris, A. Editorial perspective: how spreading mental health information can be (un-) helpful — a dynamic systems approach. Child Psychol. Psychiatry https://doi.org/10.1111/jcpp.70055 (2025).
Ormel, J., Hollon, S. D., Kessler, R. C., Cuijpers, P. & Monroe, S. M. More treatment but no less depression: the treatment-prevalence paradox. Clin. Psychol. Rev. 91, 102111 (2022).
Saunders, R. et al. Effectiveness of psychological interventions for young adults versus working age adults: a retrospective cohort study in a national psychological treatment programme in England. Lancet Psychiatry 12, 650–659 (2025).
Sawyer, S. M., Azzopardi, P. S., Wickremarathne, D. & Patton, G. C. The age of adolescence. Lancet Child Adolesc. Health 2, 223–228 (2018).
Erikson, E. H. Identity, Youth and Crisis (W. W. Norton, 1968).
Sebastian, C., Burnett, S. & Blakemore, S.-J. Development of the self-concept during adolescence. Trends Cogn. Sci. 12, 441–446 (2008).
Munawar, K., Kuhn, S. K. & Haque, S. Understanding the reminiscence bump: a systematic review. PLoS ONE 13, e0208595 (2018).
McAdams, D. P. Narrative identity: what is it? what does it do? how do you measure it? Imag. Cogn. Personal. 37, 359–372 (2018).
Granic, I., Morita, H. & Scholten, H. Beyond screen time: identity development in the digital age. Psychol. Inq. 31, 195–223 (2020).
Foster, A. & Ellis, N. TikTok-inspired self-diagnosis and its implications for educational psychology practice. Educ. Psychol. Pract. 40, 491–508 (2024).
O’Connor, C., Kadianaki, I., Maunder, K. & McNicholas, F. How does psychiatric diagnosis affect young people’s self-concept and social identity? A systematic review and synthesis of the qualitative literature. Soc. Sci. Med. 212, 94–119 (2018).
Farnood, A., Johnston, B. & Mair, F. S. A mixed methods systematic review of the effects of patient online self-diagnosing in the ‘smart-phone society’ on the healthcare professional–patient relationship and medical authority. BMC Med. Inf. Decis. Mak. 20, 253 (2020).
Harness, J. & Getzen, H. TikTok’s sick-role subculture and what to do about it. J. Am. Acad. Child Adolesc. Psychiatry 61, 351–353 (2021).
McGrath, J. J. et al. Age of onset and cumulative risk of mental disorders: a cross-national analysis of population surveys from 29 countries. Lancet Psychiatry 10, 668–681 (2023).
Casey, B. J. et al. The storm and stress of adolescence: insights from human imaging and mouse genetics. Dev. Psychobiol. 52, 225–235 (2010).
Silvers, J. A. Adolescence as a pivotal period for emotion regulation development. Curr. Opin. Psychol. 44, 258–263 (2022).
Steare, T., Gutiérrez Muñoz, C., Sullivan, A. & Lewis, G. The association between academic pressure and adolescent mental health problems: a systematic review. J. Affect. Disord. 339, 302–317 (2023).
Foulkes, L., Leung, J. T., Fuhrmann, D., Knoll, L. J. & Blakemore, S.-J. Age differences in the prosocial influence effect. Dev. Sci. 21, e12666 (2018).
Knoll, L. J., Magis-Weinberg, L., Speekenbrink, M. & Blakemore, S.-J. Social influence on risk perception during adolescence. Psychol. Sci. 26, 583–592 (2015).
Alho, J. et al. Transmission of mental disorders in adolescent peer networks. JAMA Psychiatry 81, 882 (2024).
Rooney, T., Sharpe, L., Todd, J., Tang, B. & Colagiuri, B. The nocebo effect across health outcomes: a systematic review and meta-analysis. Health Psychol. 43, 41–57 (2023).
Ehlers, A., Margraf, J., Roth, W. T., Taylor, C. B. & Birbaumer, N. Anxiety induced by false heart rate feedback in patients with panic disorder. Behav. Res. Ther. 26, 1–11 (1988).
Pauli, P. et al. Anxiety induced by cardiac perceptions in patients with panic attacks: a field study. Behav. Res. Ther. 29, 137–145 (1991).
Story, T. J. & Craske, M. G. Responses to false physiological feedback in individuals with panic attacks and elevated anxiety sensitivity. Behav. Res. Ther. 46, 1001–1008 (2008).
Wild, J., Clark, D. M., Ehlers, A. & McManus, F. Perception of arousal in social anxiety: effects of false feedback during a social interaction. J. Behav. Ther. Exp. Psychiatry 39, 102–116 (2008).
Lazarov, A., Dar, R., Liberman, N. & Oded, Y. Obsessive–compulsive tendencies and undermined confidence are related to reliance on proxies for internal states in a false feedback paradigm. J. Behav. Ther. Exp. Psychiatry 43, 556–564 (2012).
Makkar, S. R. & Grisham, J. R. Effects of false feedback on affect, cognition, behavior, and postevent processing: the mediating role of self-focused attention. Behav. Ther. 44, 111–124 (2013).
Hacking, I. in Causal Cognition (eds Sperber, D. et al.) 351–383 (Oxford Univ. Press, 1996).
Link, B. G., Cullen, F. T., Struening, E., Shrout, P. E. & Dohrenwend, B. P. A modified labeling theory approach to mental disorders: an empirical assessment. Am. Sociol. Rev. 54, 400 (1989).
Scheff, T. J. The labelling theory of mental illness. Am. Sociol. Rev. 39, 444 (1974).
Ecclestone, K. & Hayes, D. The Dangerous Rise of Therapeutic Education (Routledge, 2009).
Corneille, O. & Lush, P. Sixty years after Orne’s American Psychologist article: a conceptual framework for subjective experiences elicited by demand characteristics. Personal. Soc. Psychol. Rev. 27, 83–101 (2023).
Iarygina, O., Hornbæk, K. & Mottelson, A. Demand characteristics in human–computer experiments. Int. J. Human–Computer Stud. 193, 103379 (2025).
Nichols, A. L. & Maner, J. K. The good-subject effect: investigating participant demand characteristics. J. Gen. Psychol. 135, 151–166 (2008).
Orne, M. T. On the social psychology of the psychological experiment: with particular reference to demand characteristics and their implications. Am. Psychol. 17, 776–783 (1962).
Ju, R., Jia, M. & Cheng, J. Promoting mental health on social media: a content analysis of organizational tweets. Health Commun. 38, 1540–1549 (2023).
Saha, K. et al. A computational study of mental health awareness campaigns on social media. Transl. Behav. Med. 9, 1197–1207 (2019).
Milton, A., Ajmani, L., DeVito, M. A. & Chancellor, S. “I see me here”: mental health content, community, and algorithmic curation on TikTok. In Proc. 2023 CHI Conf. Human Factors in Computing Systems (eds Schmidt, A. et al.) 480 (ACM, 2023).
Montero-Marin, J. et al. School-based mindfulness training in early adolescence: what works, for whom and how in the MYRIAD trial? Evidence-based Ment. Health 25, 117–124 (2022).
Stallard, P. et al. Classroom based cognitive behavioural therapy in reducing symptoms of depression in high risk adolescents: pragmatic cluster randomised controlled trial. BMJ 345, e6058 (2012).
Bonell, C., Jamal, F., Melendez-Torres, G. J. & Cummins, S. ‘Dark logic’: theorising the harmful consequences of public health interventions. J. Epidemiol. Community Health 69, 95–98 (2015).
Guttman, N. & Salmon, C. T. Guilt, fear, stigma and knowledge gaps: ethical issues in public health communication interventions. Bioethics 18, 531–552 (2004).
Stratil, J. M., Baltussen, R., Scheel, I., Nacken, A. & Rehfuess, E. A. Development of the WHO-INTEGRATE evidence-to-decision framework: an overview of systematic reviews of decision criteria for health decision-making. Cost. Eff. Resour. Alloc. 18, 8 (2020).
Kirsch, I. Response expectancy as a determinant of experience and behavior. Am. Psychol. 40, 1189–1202 (1985).
Kirsch, I. Response expectancy and the placebo effect. Int. Rev. Neurobiol. 138, 81–93 (2018).
Kirsch, I. Response expectancy theory and application: a decennial review. Appl. Prevent. Psychol. 6, 69–79 (1997).
Crichton, F., Chapman, S., Cundy, T. & Petrie, K. J. The link between health complaints and wind turbines: support for the nocebo expectations hypothesis. Front. Public Health 2, 220 (2014).
Crichton, F. & Petrie, K. J. Accentuate the positive: counteracting psychogenic responses to media health messages in the age of the internet. J. Psychosom. Res. 79, 185–189 (2015).
Crichton, F. & Petrie, K. J. Health complaints and wind turbines: the efficacy of explaining the nocebo response to reduce symptom reporting. Environ. Res. 140, 449–455 (2015).
Frey, J., Black, K. J. & Malaty, I. A. TikTok Tourette’s: are we witnessing a rise in functional tic-like behavior driven by adolescent social media Use? PRBM 15, 3575–3585 (2022).
Zea Vera, A. et al. The phenomenology of tics and tic-like behavior in TikTok. Pediatric Neurol. 130, 14–20 (2022).
Fremer, C. et al. Mass social media-induced illness presenting with Tourette-like behavior. Front. Psychiatry 13, 963769 (2022).
Müller-Vahl, K. R., Pisarenko, A., Jakubovski, E. & Fremer, C. Stop that! It’s not Tourette’s but a new type of mass sociogenic illness. Brain 145, 476–480 (2022).
Niesten, I. J. M., Merckelbach, H., Dandachi-FitzGerald, B. & Jelicic, M. The iatrogenic power of labeling medically unexplained symptoms: a critical review and meta-analysis of ‘diagnosis threat’ in mild head injury. Psychol. Conscious. 10, 454–474 (2023).
Renwick, L. et al. Mental health literacy in children and adolescents in low- and middle-income countries: a mixed studies systematic review and narrative synthesis. Eur. Child Adolesc. Psychiatry 33, 961–985 (2024).
Van Den Broek, M. et al. Interventions to increase help-seeking for mental health care in low- and middle-income countries: a systematic review. PLoS Glob. Public Health 3, e0002302 (2023).
Clay, J., Eaton, J., Gronholm, P. C., Semrau, M. & Votruba, N. Core components of mental health stigma reduction interventions in low- and middle-income countries: a systematic review. Epidemiol. Psychiat. Sci. 29, e164 (2020).
Nwokoroku, S. C., Neil, B., Dlamini, C. & Osuchukwu, V. C. A systematic review of the role of culture in the mental health service utilisation among ethnic minority groups in the United Kingdom. Glob. Ment. Health 9, 84–93 (2022).
Eylem, O. et al. Stigma for common mental disorders in racial minorities and majorities a systematic review and meta-analysis. BMC Public. Health 20, 879 (2020).
Kapadia, D. Stigma, mental illness & ethnicity: time to centre racism and structural stigma. Sociol. Health Illness 45, 855–871 (2023).
Author information
Authors and Affiliations
Contributions
L.F., I.W., C.G.H. and D.S. researched data for the article. L.F., C.G.H., J.L.A., M.I. and D.S. contributed substantially to discussion of the content. All authors wrote the article and reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Psychology thanks Mark D. Weist and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Foulkes, L., Winterburn, I., Sandra, D. et al. The psychological consequences of mental health awareness efforts. Nat Rev Psychol (2026). https://doi.org/10.1038/s44159-026-00532-7
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s44159-026-00532-7