Abstract
Study design:
A prospective observational study reporting the correlation between matrix metalloprotein serum levels and remission after traumatic spinal cord injury (SCI).
Objectives:
To investigate serum cytokine levels as predictive markers.
Setting:
Germany, Rhineland-Palatinate (Rheinland-Pfalz).
Methods:
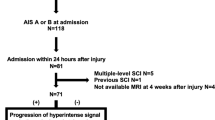
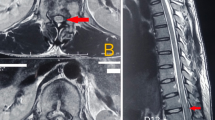
Between 2010 and 2015, data sets from 115 patients (33 female, 82 male) after traumatic SCI were recorded at the BG Trauma Centre Ludwigshafen. We examined the serum levels of Matix metallopraoteinases (MMPs) MMP-2, MMP-8, MMP-9, MMP-10 and MMP-12 over a 12-week period, that is, at admission and 4, 9, 12 h, 1 and 3 days and 1, 2, 4, 8 and 12 weeks after trauma. Following the same match-pair procedure as in our previous studies, we selected 10 patients with SCI and neurological remission (Group 1) and 10 patients with an initial American Spinal Injury Association (ASIA) A grade and no neurological remission (Group 0). Ten patients with an isolated vertebral fracture without neurological deficits served as a control group (Group C). Our analysis was performed using a Luminex Performance Human High Sensitivity Cytokine Panel. Multivariate logistic regression models were used to examine the predictive value of MMPs with respect to neurological remission vs no neurological remission.
Results:
MMP-8 and MMP-9 provided significantly different values. The favoured predictive model allows to differentiate between neurological remission and no neurological remission in 97% of cases.
Conclusions:
The results indicate that further studies with an enlarged collective are warranted in order to investigate current monitoring, prognostic and tracking techniques as well as scoring systems.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Boakye M, Leigh BC, Skelly AC . Quality of life in persons with spinal cord injury: comparisons with other populations. J Neurosurg Spine 2012; 17: 29–37.
Rowland JW, Hawryluk GW, Kwon B, Fehlings MG . Current status of acute spinal cord injury pathophysiology and emerging therapies: promise on the horizon. Neurosurg Focus 2008; 25: E2.
Devivo MJ . Epidemiology of traumatic spinal cord injury: trends and future implications. Spinal Cord 2012; 50: 365–372.
Ito Y, Sugimoto Y, Tomioka M, Kai N, Tanaka M . Does high dose methylprednisolone sodium succinate really improve neurological status in patient with acute cervical cord injury?: a prospective study about neurological recovery and early complications. Spine (Phila Pa 1976) 2009; 34: 2121–2124.
Kwon BK, Okon EB, Plunet W, Baptiste D, Fouad K, Hillyer J et al. A systematic review of directly applied biologic therapies for acute spinal cord injury. J Neurotrauma 2011; 28: 1589–1610.
Evaniew N, Belley-Cote EP, Fallah N, Noonan VK, Rivers CS, Dvorak MF . Methylprednisolone for the treatment of patients with acute spinal cord injuries: a systematic review and meta-analysis. J Neurotrauma 2015; 33: 468–481.
Walters BC, Hadley MN, Hurlbert RJ, Aarabi B, Dhall SS, Gelb DE et al. Guidelines for the management of acute cervical spine and spinal cord injuries: 2013 update. Neurosurgery 2013; 60: 82–91.
Esposito E, Genovese T, Caminiti R, Bramanti P, Meli R, Cuzzocrea S . Melatonin regulates matrix metalloproteinases after traumatic experimental spinal cord injury. J Pineal Res 2008; 45: 149–156.
Rohani MG, McMahan RS, Razumova MV, Hertz AL, Cieslewicz M, Pun SH et al. MMP-10 regulates collagenolytic activity of alternatively activated resident macrophages. J Invest Dermatol 2015; 135: 2377–2384.
Kwon BK, Casha S, Hurlbert RJ, Yong VW . Inflammatory and structural biomarkers in acute traumatic spinal cord injury. Clin Chem Lab Med 2011; 49: 425–433.
Yokobori S, Zhang Z, Moghieb A, Mondello S, Gajavelli S, Dietrich WD et al. Acute diagnostic biomarkers for spinal cord injury: review of the literature and preliminary research report. World Neurosurg 2015; 83: 867–878.
Zhang H, Chang M, Hansen CN, Basso DM, Noble-Haeusslein LJ . Role of matrix metalloproteinases and therapeutic benefits of their inhibition in spinal cord injury. Neurotherapeutics 2011; 8: 206–220.
Kwon BK, Streijger F, Hill CE, Anderson AJ, Bacon M, Beattie MS et al. Large animal and primate models of spinal cord injury for the testing of novel therapies. Exp Neurol 2015; 269: 154–168.
Kwon BK, Stammers AM, Belanger LM, Bernardo A, Chan D, Bishop CM et al. Cerebrospinal fluid inflammatory cytokines and biomarkers of injury severity in acute human spinal cord injury. J Neurotrauma 2010; 27: 669–682.
Moghaddam A, Breier L, Haubruck P, Bender D, Biglari B, Wentzensen A et al. Non-unions treated with bone morphogenic protein 7: introducing the quantitative measurement of human serum cytokine levels as promising tool in evaluation of adjunct non-union therapy. J Inflamm (Lond) 2016; 13: 3.
Moghaddam A, Child C, Bruckner T, Gerner HJ, Daniel V, Biglari B . Posttraumatic inflammation as a key to neuroregeneration after traumatic spinal cord injury. Int J Mol Sci 2015; 16: 7900–7916.
Moghaddam A, Zimmermann G, Hammer K, Bruckner T, Grutzner PA, von Recum J . Cigarette smoking influences the clinical and occupational outcome of patients with tibial shaft fractures. Injury 2011; 42: 1435–1442.
Moghaddam A, Muller U, Roth HJ, Wentzensen A, Grutzner PA, Zimmermann G . TRACP 5b and CTX as osteological markers of delayed fracture healing. Injury 2011; 42: 758–764.
Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med 2011; 34: 535–546.
Marino RJ, Ditunno JF Jr, Donovan WH, Maynard F Jr . Neurologic recovery after traumatic spinal cord injury: data from the Model Spinal Cord Injury Systems. Arch Phys Med Rehabil 1999; 80: 1391–1396.
R Development Core Team (2015). R: A Language and Environment for Statistical Computing. Vienna, Austria, R Foundation for Statistical Computing.
Robin X, Turck N, Hainard A, Tiberti N, Lisacek F, Sanchez JC et al. pROC: an open-source package for R and S+ to analyze and compare ROC curves. BMC Bioinformatics 2011; 12: 77.
Akaike H . Information Theory and an Extension of the Maximum Likelihood Principle. Selected Papers of Hirotugu Akaike. (eds. Parzen E, Tanabe K, Kitagawa G) New York, NY, Springer New York, 199–213 1998.
Biglari B, Buchler A, Swing T, Biehl E, Roth HJ, Bruckner T et al. Increase in soluble CD95L during subacute phases after human spinal cord injury: a potential therapeutic target. Spinal Cord 2013; 51: 183–187.
Biglari B, Buchler A, Swing T, Child C, Biehl E, Reitzel T et al. Serum sCD95L concentration in patients with spinal cord injury. J Int Med Res 2015; 43: 250–256.
Osterthun R, Post MW, van Asbeck FW . Characteristics, length of stay and functional outcome of patients with spinal cord injury in Dutch and Flemish rehabilitation centres. Spinal Cord 2009; 47: 339–344.
Milicevic S, Bukumiric Z, Nikolic AK, Babovic R, Jankovic S . Demographic characteristics and functional outcomes in patients with traumatic and nontraumatic spinal cord injuries. Vojnosanit Pregl 2012; 69: 1061–1066.
Wyndaele M, Wyndaele JJ . Incidence, prevalence and epidemiology of spinal cord injury: what learns a worldwide literature survey? Spinal Cord 2006; 44: 523–529.
Jackson AB, Dijkers M, Devivo MJ, Poczatek RB . A demographic profile of new traumatic spinal cord injuries: change and stability over 30 years. Arch Phys Med Rehabil 2004; 85: 1740–1748.
Cummins JS, Koval KJ, Cantu RV, Spratt KF . Do seat belts and air bags reduce mortality and injury severity after car accidents? Am J Orthop (Belle Mead, NJ) 2011; 40: E26–E29.
Smith JL, Ackerman LL . Management of cervical spine injuries in young children: lessons learned. J Neurosurg Pediatr 2009; 4: 64–73.
Weninger P, Hertz H . Factors influencing the injury pattern and injury severity after high speed motor vehicle accident—a retrospective study. Resuscitation 2007; 75: 35–41.
Richter M, Thermann H, Wippermann B, Otte D, Schratt HE, Tscherne H . Foot fractures in restrained front seat car occupants: a long-term study over twenty-three years. J Orthop Trauma 2001; 15: 287–293.
Kaminska MS, Brodowski J, Karakiewicz B . Fall risk factors in community-dwelling elderly depending on their physical function, cognitive status and symptoms of depression. Int J Environ Res Public Health 2015; 12: 3406–3416.
Chen Y, Tang Y, Allen V, DeVivo MJ . Aging and spinal cord injury: external causes of injury and implications for prevention. Top Spinal Cord Inj Rehabil 2015; 21: 218–226.
Merrill JE, Ignarro LJ, Sherman MP, Melinek J, Lane TE . Microglial cell cytotoxicity of oligodendrocytes is mediated through nitric oxide. J Immunol 1993; 151: 2132–2141.
Kim GM, Xu J, Song SK, Yan P, Ku G, Xu XM et al. Tumor necrosis factor receptor deletion reduces nuclear factor-kappaB activation, cellular inhibitor of apoptosis protein 2 expression, and functional recovery after traumatic spinal cord injury. J Neurosci 2001; 21: 6617–6625.
Hansen CN, Fisher LC, Deibert RJ, Jakeman LB, Zhang H, Noble-Haeusslein L et al. Elevated MMP-9 in the lumbar cord early after thoracic spinal cord injury impedes motor relearning in mice. J Neurosci 2013; 33: 13101–13111.
Jang JW, Lee JK, Kim SH . Activation of matrix metalloproteinases-9 after photothrombotic spinal cord injury model in rats. J Korean Neurosurg Soc 2011; 50: 288–292.
Liu H, Shubayev VI . Matrix metalloproteinase-9 controls proliferation of NG2+ progenitor cells immediately after spinal cord injury. Exp Neurol 2011; 231: 236–246.
Piao MS, Lee JK, Jang JW, Hur H, Lee SS, Xiao L et al. Melatonin improves functional outcome via inhibition of matrix metalloproteinases-9 after photothrombotic spinal cord injury in rats. Acta Neurochir (Wien) 2014; 156: 2173–2182.
Wells JE, Rice TK, Nuttall RK, Edwards DR, Zekki H, Rivest S et al. An adverse role for matrix metalloproteinase 12 after spinal cord injury in mice. J Neurosci 2003; 23: 10107–10115.
Zhang H, Trivedi A, Lee JU, Lohela M, Lee SM, Fandel TM et al. Matrix metalloproteinase-9 and stromal cell-derived factor-1 act synergistically to support migration of blood-borne monocytes into the injured spinal cord. J Neurosci 2011; 31: 15894–15903.
Zhou Y, Cui Z, Xia X, Liu C, Zhu X, Cao J et al. Matrix metalloproteinase-1 (MMP-1) expression in rat spinal cord injury model. Cell Mol Neurobiol 2014; 34: 1151–1163.
Hsu JY, McKeon R, Goussev S, Werb Z, Lee JU, Trivedi A et al. Matrix metalloproteinase-2 facilitates wound healing events that promote functional recovery after spinal cord injury. J Neurosci 2006; 26: 9841–9850.
Lee JY, Choi HY, Na WH, Ju BG, Yune TY . 17beta-estradiol inhibits MMP-9 and SUR1/TrpM4 expression and activation and thereby attenuates BSCB disruption/hemorrhage after spinal cord injury in male rats. Endocrinology 2015; 156: 1838–1850.
Li XQ, Cao XZ, Wang J, Fang B, Tan WF, Ma H . Sevoflurane preconditioning ameliorates neuronal deficits by inhibiting microglial MMP-9 expression after spinal cord ischemia/reperfusion in rats. Mol Brain 2014; 7: 69.
Yang J, Wang G, Gao C, Shao G, Kang N . Effects of hyperbaric oxygen on MMP-2 and MMP-9 expression and spinal cord edema after spinal cord injury. Life Sci 2013; 93: 1033–1038.
Yu F, Kamada H, Niizuma K, Endo H, Chan PH . Induction of mmp-9 expression and endothelial injury by oxidative stress after spinal cord injury. J Neurotrauma 2008; 25: 184–195.
Zhang P, Ma X . Effect of rutin on spinal cord injury through inhibition of the expression of MIP-2 and activation of MMP-9, and downregulation of Akt phosphorylation. Mol Med Rep 2015; 12: 7554–7560.
Hsu JY, Bourguignon LY, Adams CM, Peyrollier K, Zhang H, Fandel T et al. Matrix metalloproteinase-9 facilitates glial scar formation in the injured spinal cord. J Neurosci 2008; 28: 13467–13477.
Austin JW, Afshar M, Fehlings MG . The relationship between localized subarachnoid inflammation and parenchymal pathophysiology after spinal cord injury. J Neurotrauma 2012; 29: 1838–1849.
Benedict AL, Mountney A, Hurtado A, Bryan KE, Schnaar RL, Dinkova-Kostova AT et al. Neuroprotective effects of sulforaphane after contusive spinal cord injury. J Neurotrauma 2012; 29: 2576–2586.
Acknowledgements
We thank Martina Kutsche-Bauer for performing the Luminex assays. Statistical consulting was provided by the Institute for Medical Biometrics and Information Technology at the University of Heidelberg, Germany.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Moghaddam, A., Heller, R., Daniel, V. et al. Exploratory study to suggest the possibility of MMP-8 and MMP-9 serum levels as early markers for remission after traumatic spinal cord injury. Spinal Cord 55, 8–15 (2017). https://doi.org/10.1038/sc.2016.104
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/sc.2016.104
This article is cited by
-
Time trajectories and within-subject correlations of matrix metalloproteinases 3, 8, 9, 10, 12, and 13 serum levels and their ability to predict mortality in polytraumatized patients: a pilot study
European Journal of Medical Research (2024)
-
Acute spinal cord injury serum biomarkers in human and rat: a scoping systematic review
Spinal Cord Series and Cases (2024)
-
Omega-3 fatty acids in the treatment of spinal cord injury: untapped potential for therapeutic intervention?
Molecular Biology Reports (2022)
-
Evaluation of the clinical effectiveness of bioactive glass (S53P4) in the treatment of non-unions of the tibia and femur: study protocol of a randomized controlled non-inferiority trial
Trials (2018)
-
Matrix Metalloproteinase-8 Inhibition Prevents Disruption of Blood–Spinal Cord Barrier and Attenuates Inflammation in Rat Model of Spinal Cord Injury
Molecular Neurobiology (2018)