Abstract
Introduction:
We report a case of acute tetraplegia, without any trauma or symptoms prior to onset, who presented with ossification of the posterior longitudinal ligament (OPLL) in the cervical spine with concomitant spinal cord infarction.
Case Presentation:
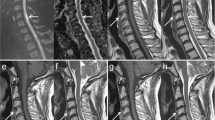
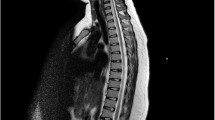
A 64-year-old man with a number of risk factors for vascular disease was admitted to our hospital with progressive motor weakness in the bilateral upper and lower extremities. He had initially felt numbness in his left upper extremity and had no previous neurological symptoms or trauma. The night after the initial symptoms, he developed spastic tetraplegia requiring respiratory support. Computed tomography images of the cervical spine demonstrated the segmental type of OPLL. Spinal cord compression and signal intensity changes were identified at the level of C3/4 on magnetic resonance imaging (MRI). He underwent emergency surgery consisting of posterior decompression with laminoplasty of C3-6. Despite the surgery, the patient’s tetraplegia did not improve and he continued to require respirator support. There was still no improvement in his neurological status at 10 days postoperatively, and MRI demonstrated evidence of marked spinal cord infarction.
Discussion:
Mechanical compression of spinal arteries by OPLL and pre-existing vascular compromise had a role in the pathogenesis of spinal cord infarction. Chronic spinal compression may be characterized by 3 important factors, namely an uncommonly devastating clinical course, vascular risk factors and persistent findings on MRI, and these might lead to early diagnosis of spinal cord infarction.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Chikuda H, Seichi A, Takeshita K, Matsunaga S, Watanabe M, Nakagawa Y et al. Acute cervical spinal cord injury complicated by preexisting ossification of the posterior longitudinal ligament: a multicenter study. Spine 2011; 36: 1453–1458.
Katoh S, Ikata T, Hirai N, Okada Y, Nakauchi K . Influence of minor trauma to the neck on the neurological outcome in patients with ossification of the posterior longitudinal ligament (OPLL) of the cervical spine. Paraplegia 1995; 33: 330–333.
Matsunaga S, Sakou T, Hayashi K, Ishidou Y, Hirotsu M, Komiya S . Trauma-induced myelopathy in patients with ossification of the posterior longitudinal ligament. J Neurosurg 2002; 97: 172–175.
Trojan DA, Pouchot J, Pokrupa R, Ford RM, Adamsbaum C, Hill RO et al. Diagnosis and treatment of ossification of the posterior longitudinal ligament of the spine: report of eight cases and literature review. Am J Med 1992; 92: 296–306.
Matsunaga S, Sakou T . Ossification of the posterior longitudinal ligament of the cervical spine: etiology and natural history. Spine 2012; 37: E309–E314.
Matsunaga S, Sakou T, Taketomi E, Komiya S . Clinical course of patients with ossification of the posterior longitudinal ligament: a minimum 10-year cohort study. J Neurosurg 2004; 100: 245–248.
Terayama K, Kurokawa T, Seki H . National survey of ossification of the posterior longitudinal ligament. In: Investigation Committee 1975 Report on the Ossification of the Spinal Ligaments of the Japanese Ministry of Public Health and Welfare. Tokyo, Japan, 1976, pp 8–33.
Ueyama T, Tamaki N, Kondoh T, Miyamoto H, Akiyama H, Nagashima T . Non-traumatic acute paraplegia associated with cervical disc herniation: a case report. Surg Neurol 1999; 52: 204–206, discussion 206–207.
Suzuki T, Abe E, Murai H, Kobayashi T . Nontraumatic acute complete paraplegia resulting from cervical disc herniation: a case report. Spine 2003; 28: E125–E128.
Sadanand V, Kelly M, Varughese G, Fourney DR . Sudden quadriplegia after acute cervical disc herniation. Can J Neurol Sci 2005; 32: 356–358.
Liu C, Huang Y, Cai HX, Fan SW . Nontraumatic acute paraplegia associated with cervical disk herniation. J Spinal Cord Med 2010; 33: 420–424.
Cho JL, Park YS, Kim YH . Tetraparesis associated with ossification of the posterior longitudinal ligament of the cervical spine. Int Orthop 1999; 23: 247–248.
Cruzeiro MM, Vale TC, Pires LA, Franco GM, Pennisi MF . Tetraparesis secondary to cervical ossification of the posterior longitudinal ligament: case report. Arq Neuropsiquiatr 2007; 65: 532–535.
Rabinstein AA . Vascular myelopathies. Continuum 2015; 21: 67–83.
Rubin MN, Rabinstein AA . Vascular diseases of the spinal cord. Neurol Clin 2013; 31: 153–181.
Novy J, Carruzzo A, Maeder P, Bogousslavsky J . Spinal cord ischemia: clinical and imaging patterns, pathogenesis, and outcomes in 27 patients. Arch Neurol 2006; 63: 1113–1120.
Cheshire WP, Santos CC, Massey EW, Howard JF Jr . Spinal cord infarction: etiology and outcome. Neurology 1996; 47: 321–330.
Rigney L, Cappelen-Smith C, Sebire D, Beran RG, Cordato D . Nontraumatic spinal cord ischaemic syndrome. J Clin Neurosci 2015; 22: 1544–1549.
Loher TJ, Bassetti CL, Lovblad KO, Stepper FP, Sturzenegger M, Kiefer C et al. Diffusion-weighted MRI in acute spinal cord ischaemia. Neuroradiology 2003; 45: 557–561.
Howard RS, Thorpe J, Barker R, Revesz T, Hirsch N, Miller D et al. Respiratory insufficiency due to high anterior cervical cord infarction. J Neurol Neurosurg Psychiatry 1998; 64: 358–361.
Mizuno J, Nakagawa H, Hashizume Y . Pathology of the spinal cord damaged by ossification of the posterior longitudinal ligament associated with spinal cord injury. Spinal Cord 1999; 37: 224–227.
Millichap JJ, Sy BT, Leacock RO . Spinal cord infarction with multiple etiologic factors. J Gen Intern Med 2007; 22: 151–154.
Westwick HJ, Goldstein CL, Shamji MF . Acute spontaneous cervical disc herniation causing rapidly progressive myelopathy in a patient with comorbid ossified posterior longitudinal ligament: case report and literature review. Surg Neurol Int 2014; 5: S368–S372.
Hsieh JH, Wu CT, Lee ST . Cervical intradural disc herniation after spinal manipulation therapy in a patient with ossification of posterior longitudinal ligament: a case report and review of the literature. Spine 2010; 35: E149–E151.
Cheong HS, Hong BY, Ko YA, Lim SH, Kim JS . Spinal cord injury incurred by neck massage. Ann Rehabil Med 2012; 36: 708–712.
Iwamura Y, Onari K, Kondo S, Inasaka R, Horii H . Cervical intradural disc herniation. Spine 2001; 26: 698–702.
Yoshizawa H . Presidential address: pathomechanism of myelopathy and radiculopathy from the viewpoint of blood flow and cerebrospinal fluid flow including a short historical review. Spine 2002; 27: 1255–1263.
Thurnher MM, Bammer R, Diffusion-weighted MR . imaging (DWI) in spinal cord ischemia. Neuroradiology 2006; 48: 795–801.
Reynolds JM, Belvadi YS, Kane AG, Poulopoulos M . Thoracic disc herniation leads to anterior spinal artery syndrome demonstrated by diffusion-weighted magnetic resonance imaging (DWI): a case report and literature review. Spine J 2014; 14: e17–e22.
Bhardwaj A, Long DM, Ducker TB, Toung TJ . Neurologic deficits after cervical laminectomy in the prone position. J Neurosurg Anesthesiol 2001; 13: 314–319.
Cybulski GR, D’Angelo CM . Neurological deterioration after laminectomy for spondylotic cervical myeloradiculopathy: the putative role of spinal cord ischaemia. J Neurol Neurosurg Psychiatry 1988; 51: 717–718.
Ben-David B, Haller G, Taylor P . Anterior spinal fusion complicated by paraplegia. A case report of a false-negative somatosensory-evoked potential. Spine 1987; 12: 536–539.
Kalb S, Fakhran S, Dean B, Ross J, Porter RW, Kakarla UK et al. Cervical spinal cord infarction after cervical spine decompressive surgery. World Neurosurg 2014; 81: 810–817.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Tanida, A., Kamimura, A., Tanishima, S. et al. Spinal cord infarction at the level of ossification of the posterior longitudinal ligament. Spinal Cord Ser Cases 2, 16032 (2016). https://doi.org/10.1038/scsandc.2016.32
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/scsandc.2016.32