Key Points
-
Suggests that the evidence with regard to an association between oral health and dementia is weak because of the lack of well-designed cohort and case-control studies and variation in how dementia and oral health are defined and measured.
-
Highlights that dementia and cognitive decline are risk factors for poor oral health.
-
Suggests that patients with suboptimal oral health appear to have an associated increased risk of cognitive impairment, but more evidence from different settings is required.
Abstract
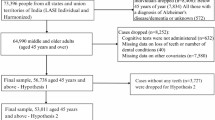
This is the fourth and final paper of a series of reviews undertaken to explore the relationships between oral health and general medical conditions, in order to support teams within Public Health England, health practitioners and policy makers. This review aimed to explore the most contemporary evidence on whether poor oral health and dementia occurs in the same individuals or populations, to outline the nature of the relationship between these two health outcomes and to discuss the implication of any findings for health services and future research. The review was undertaken by a working group comprising consultant clinicians from medicine and dentistry, trainees, public health and academic staff. Whilst other rapid reviews in the current series limited their search to systematic reviews, this review focused on primary research involving cohort and case-control studies because of the lack of high level evidence in this new and important field. The results suggest that poor oral hygiene is associated with dementia, and more so amongst people in advanced stages of the disease. Suboptimal oral health (gingivitis, dental caries, tooth loss, edentulousness) appears to be associated with increased risk of developing cognitive impairment and dementia. The findings are discussed in relation to patient care and future research.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Department of Health. Prime Minister's challenge on dementia 2020. 2015. Available at https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/414344/pm-dementia2020.pdf (accessed October 2017).
World Health Organization. International Classification of Diseases – 10. Geneva: WHO, 2016.
Alzheimer's Society. Alzheimer's Society. What is Alzheimers Disease? 2015. Available at https://www.alzheimers.org.uk/site/scripts/download_info.php?downloadID=1093 (accessed October 2017).
Prince M, Knapp M, Guerchet M et al. Dementia UK: Update 2014. 2015. Available at https://www.alz.co.uk/research/WorldAlzheimerReport2014.pdf (accessed November 2017).
Hughes T F, Ganguli M . Modifiable midlife risk factors for late-life cognitive impairment and dementia. Curr Psychiatry Rev 2009; 5: 73–92.
Marcenes W, Kassebaum N, Bernabé E et al. Global burden of oral conditions in 1990–2010 A systematic analysis. J Dent Res 2013; 92: 592–597.
Steele J, O'Sullivan I . Adult Dental Health Survey 2009. 2011. Available at https://digital.nhs.uk/catalogue/PUB01086 (accessed November 2017)
Sheiham A, Watt R . The common risk factor approach: a rational basis for promoting oral health. Community Dent Oral Epidemiol 2000; 28: 399–406.
de Souza Rolim T, Fabri G M, Nitrini R et al. Oral infections and orofacial pain in Alzheimer's disease: a case-control study. J Alzheimers Dis 2014; 38: 823–829.
Paganini-Hill A, White S C, Atchison K A . Dentition, dental health habits, and dementia: the Leisure World Cohort Study. J Am Geriatr Soc 2012; 60: 1556–1563.
Noble J M, Scarmeas N, Celenti R S et al. Serum IgG antibody levels to periodontal microbiota are associated with incident Alzheimer disease. PLoS One 2014; 9: e114959.
Sparks Stein P, Steffen M J, Smith C et al. Serum antibodies to periodontal pathogens are a risk factor for Alzheimer's disease. Alzheimers Dement 2012; 8: 196–203.
Khangura S, Konnyu K, Cushman R, Grimshaw J, Moher D . Evidence summaries: the evolution of a rapid review approach. Syst Rev 2012; 1: 10.
Wells G, Shea B, O'Connell D et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2000. Available at http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed October 2017).
Chu C H, Ng A, Chau A M, Lo E C . Oral health status of elderly chinese with dementia in Hong Kong. Oral Health Prev Dent 2015; 13: 51–57.
Gil-Montoya J A, Sanchez-Lara I, Carnero-Pardo C et al. Is periodontitis a risk factor for cognitive impairment and dementia? A case-control study. J Periodontol 2015; 86: 244–253.
Hatipoglu M G, Kabay S C, Güven G . The clinical evaluation of the oral status in Alzheimer-type dementia patients. Gerodontology 2011; 28: 302–306.
Adam H, Preston A J . The oral health of individuals with dementia in nursing homes. Gerodontology 2006; 23: 99–105.
Ellefsen B, Holm-Paedersen P, Morse D E, Schroll M, Andersen B B, Waldemar G . Assessing caries increments in elderly patients with and without dementia: a one-year follow-up study. J Am Dent Assoc 2009; 140: 1392–1400.
Chen X, Clark J J J, Naorungroj S . Oral health in older adults with dementia living in different environments: a propensity analysis. Spec Care Dentist 2013; 33: 239–247.
Chen X, Shuman S K, Hodges J S, Gatewood L C, Xu J . Patterns of tooth loss in older adults with and without dementia: a retrospective study based on a Minnesota cohort. J Am Geriatr Soc 2010; 58: 2300–2307.
Stewart R, Weyant R J, Garcia M E et al. Adverse oral health and cognitive decline: the health, aging and body composition study. J Am Geriatr Soc 2013; 61: 177–184.
Batty G D, Li Q, Huxley R et al. Oral disease in relation to future risk of dementia and cognitive decline: prospective cohort study based on the Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified-Release Controlled Evaluation (ADVANCE) trial. Eur Psychiatry 2013; 28: 49–52.
Yamamoto T, Kondo K, Hirai H, Nakade M, Aida J, Hirata Y . Association between self-reported dental health status and onset of dementia: a 4-year prospective cohort study of older Japanese adults from the Aichi Gerontological Evaluation Study (AGES) Project. Psychosom Med 2012; 74: 241–248.
Okamoto N, Morikawa M, Tomioka K, Yanagi M, Amano N, Kurumatani N . Association between tooth loss and the development of mild memory impairment in the elderly: the Fujiwara-kyo Study. J Alzheimers Dis 2015; 44: 777–786.
Kaye E K, Valencia A, Baba N, Spiro A, 3rd, Dietrich T, Garcia R I . Tooth loss and periodontal disease predict poor cognitive function in older men. J Am Geriatr Soc 2010; 58: 713–718.
Arrive E, Letenneur L, Matharan F et al. Oral health condition of French elderly and risk of dementia: a longitudinal cohort study. Community Dent Oral Epidemiol 2012; 40: 230–238.
Stewart R, Stenman U, Hakeberg M, Hagglin C, Gustafson D, Skoog I . Associations between oral health and risk of dementia in a 37-year follow-up study: the prospective population study of women in Gothenburg. J Am Geriatr Soc 2015; 63: 100–105.
Tsakos G, Watt R G, Rouxel PL, de Oliveira C, Demakakos P . Tooth loss associated with physical and cognitive decline in older adults. J Am Geriatr Soc 2015; 63: 91–99.
Cerutti-Kopplin D, Feine J, Padilha D et al. Tooth Loss Increases the Risk of Diminished Cognitive Function A Systematic Review and Meta-analysis. JDR Clin Transl Res 2016; 1: 10–19.
Wu B, Fillenbaum G G, Plassman B L, Guo L . Association Between Oral Health and Cognitive Status: A Systematic Review. J Am Geriatr Soc 2016; 64: 739–751.
Public Health England. Delivering better oral health: an evidence-based toolkit for prevention (third edition). London: PHE, 2014. Available at https://www.gov.uk/government/publications/delivering-better-oral-health-an-evidence-based-toolkit-for-prevention (accessed November 2017).
American Academy of Periodontology Task Force. American Academy of Periodontology Task Force Report on the Update to the 1999 Classification of Periodontal Diseases and Conditions. J Periodontol 2015; 86: 835–838.
Acknowledgements
We would like to acknowledge the support of Carly Tutti of Public Health England during a workshop in preparation for this paper. We further acknowledge the overall support of Public Health England, the Faculty of Dental Surgery of The Royal College of Surgeons of England and The British Dental Association.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Supplementary information
Supplementary Table 1
Cohort and case-control studies: Is dementia (including cognitive decline) a risk factor for poor oral health? (PDF 174 kb)
Supplementary Table 2
Cohort and case-control studies: Is poor oral health a risk factor for developing dementia (including cognitive decline)? (PDF 216 kb)
Supplementary Table 3
Systematic review on tooth loss and periodontal disease and cognitive impairment (PDF 92 kb)
Rights and permissions
About this article
Cite this article
Daly, B., Thompsell, A., Sharpling, J. et al. Evidence summary: the relationship between oral health and dementia. Br Dent J 223, 846–853 (2017). https://doi.org/10.1038/sj.bdj.2017.992
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/sj.bdj.2017.992
This article is cited by
-
Evaluating the role of the smartjournal digital intervention in improving oral hygiene among nursing home residents: a cluster randomised trial
BMC Oral Health (2025)
-
The impact of social and commercial determinants on the unequal increase of oral disorder disease burdens across global, regional, and national contexts
BMC Oral Health (2025)
-
Healthcare utilization among Japanese older adults during later stage of prolonged pandemic
Scientific Reports (2025)
-
Longitudinal association between posterior occlusal contact and dementia development in a large retrospective cohort study using a Japanese claims database
Scientific Reports (2024)
-
Healthy ageing and oral health: priority, policy and public health
BDJ Open (2024)