Abstract
Objective:
To assess the prevalence of overweight, obesity and underweight among Vietnamese adults living in urban areas of Ho Chi Minh City (HCMC), Vietnam.
Design:
This cross-sectional survey was conducted in the local health stations of 30 randomly selected wards, which represent all 13 urban districts of HCMC, over a period of 2 months from March to April 2004.
Subjects:
A total of 1488 participants aged 20–60 years completed the interview, physical examination and venous blood collection.
Measurements:
Anthropometric measurements of body weight, height, waist and hip circumference were taken to construct indicators of adiposity including body mass index (BMI), waist circumference, and waist-to-height and waist-to-hip ratios. Both systolic and diastolic blood pressure and biochemical indicators of cardiovascular disease and type II diabetes risk (lipid profile and fasting blood glucose) were also measured.
Results:
The age and sex standardized prevalence of overweight and obesity using Asian specific BMI cutoffs of 23.0 and 27.5 kg/m2 was 26.2 and 6.4%, respectively. The prevalence of overweight and obesity was slightly higher in females (33.6%) than males (31.6%), and progressively increased with age. The age and sex-standardized prevalence of underweight (BMI <18.5 kg/m2) among Vietnamese adults living in HCMC was 20.4%. The prevalence was slightly higher in males (22.0%) than in females (18.9%), and there was a much higher prevalence in all underweight categories in younger women than in men but this was reversed for older men.
Conclusion:
The adult population in HCMC Vietnam is in an early ‘nutrition transition’ with approximately equal prevalence of low and high BMI. The prevalence of overweight and obesity of Vietnamese urban adults was lower than that reported for other east and southeast Asian countries.
Similar content being viewed by others
Introduction
There is a vast amount of evidence worldwide that shows obesity is a chronic disease, which can predispose to potentially fatal chronic conditions such as type II diabetes, cardiovascular diseases and stroke (Bjorntorp, 2001). Obesity is nowadays considered one of the most important global health problems alongside AIDS, cancer and cardiovascular diseases. In Western countries, the prevalence of overweight and obesity are very high and are continuing to increase.
In Asian countries, the emerging problem of increasing overweight and obesity was highlighted more than a decade ago (Tee, 2002). A recent report indicates that the prevalence of overweight (defined as BMI ⩾25 kg/m2) was higher than 23% in many cities in Asia such as Beijing, Hong Kong, Kuala Lumpur, Manila and Bangkok (Sakamoto et al., 1997). This increase in the prevalence of overweight is probably associated with industrialization and urbanization, which results in changed eating habits and lifestyles in these populations (Popkin and Gordon-Larsen, 2004).
In Vietnam, over the past 10 years, the economic situation has improved dramatically following the introduction of the social and economic policy reforms called ‘Doi moi’ and the lifting of the embargo on Vietnam by the US government. It is considered that the resulting changes in the economy have in part contributed to changing morbidity patterns with decreases in infectious diseases and malnutrition and increases in chronic diseases like type II diabetes, hyperlipidemia, hypertension and overweight especially in large cities like HCMC.
Ho Chi Minh City (HCMC), with a population of approximately seven million people, is the largest and also the most economically dynamic urban area in Vietnam. This urban population is the group most likely in Vietnam to be undergoing a nutrition transition. It has a rapidly changing nutritional situation where both under and overnutrition co-exist in the same population and shows evidence of the emergence of obesity and other chronic diseases in adults. Preliminary evidence of an emerging problem with overnutrition can be found in type II diabetes surveillance data collected from adults in HCMC in 2000 where the prevalence of overweight (BMI ⩾25 kg/m2) of Vietnamese adults (>15 years) living in HCMC was 12.9% (both genders) (Hung et al., 2002). Another study reported the prevalence of overweight of women (15–49 years) was 9.7% (Hung and Loan, 2002). Furthermore, a survey in 1999 of 300 middle-aged Vietnamese 40–60 years living in HCMC reported the prevalence of overweight (BMI ⩾25 kg/m2) in urban, suburban and rural areas of the city as 18, 13 and 6%, respectively (Hanh et al., 2001). However, all these previous estimates of overweight in adults in HCMC were derived from studies that had been designed to assess other specific health issues (such as type II diabetes, maternal and child healthcare or middle age health) rather than specifically designed to assess overweight and obesity in adults. Thus, this survey was designed with the specific purpose of assessing the prevalence and risk factors for overweight and obesity in Vietnamese adults living in HCMC. This study will also provide important baseline information on obesity in adults for future assessments.
Methods
Study design
A cross-sectional study of a representative sample of adults aged 20–60 years living in urban areas of HCMC over a period of 2 months from March to April 2004.
Setting and population
HCMC with its population of over five million people is the largest and economically most advanced city in Vietnam. The city is divided into four administrative levels; districts, wards, quarters and hamlets. In total, it has 22 districts with 303 wards, and on average, there are 15 wards per district. The districts have been classified into urban, suburban and rural districts. There are 13 urban districts with 182 wards, four suburban districts with 56 wards and four rural districts with 65 wards. This cross-sectional study was restricted to adults aged 20–60 years living in the 13 urban districts of HCMC.
Sampling
The study used a multistage cluster sampling strategy. Firstly, 30 wards (clusters) were randomly selected from 182 wards in 13 urban districts of HCMC using the proportionate to the population size method based on the data from the 1999 Vietnam national census (HCMC Statistics Department, 2000). Secondly, simple random sampling was used to select one-quarter in each of the selected wards from stage one with an assumption of approximately equal population in each quarter. Next, simple random sampling was used to select one hamlet from each of the selected quarters from stage two with an assumption of approximately equal population in each hamlet. Then, a list of all households in each hamlet was prepared by the local health workers. Fifty households were randomly selected from this list. Each hamlet usually contained approximately 50 houses. If there were less than 50 houses, then more households were identified from a neighboring hamlet in that quarter. The lists of all adults aged 20–60 years in each selected household were prepared by community health workers. Finally, one adult was selected from each household using simple random sampling. Exclusion criteria for potential participants included pregnant women, critically ill subjects, mentally disordered subjects and persons who had deformities that prevented accurate measurement of height and percent of body fat.
All selected participants were visited by community health workers in their homes to provide the information about the study, to invite them to participate in the study and to obtain witnessed verbal consent. The survey clinics were held at local health stations for one morning in each of the 30 selected clusters (ward) during the study period.
A sample size of 1462 adults was required to estimate the prevalence of overweight and obesity with precision of 2.5%.
The study protocol was approved by the Human Research Ethics Committee of University of Newcastle, Australia and the Research and Ethical Review Board of HCMC Health Services, Vietnam. The Nutrition Center in HCMC Vietnam was involved in supporting the study by providing staff for data collection.
Measurements
Socio-demographic characteristics
An interviewer administered questionnaire about socio-demographic status was used, which included an assessment of the subjects’ age, ethnicity, education, occupation and household assets. Education level was classified into five groups: no school, primary school, junior high school, senior high school and college or university. Occupation was classified into five groups: teacher/professional, government officers, small business/skilled workers, labourers/street or home traders, retired/home makers/students.
Clinical assessment
Systolic and diastolic blood pressures were measured in all participants using the left arm by trained nurses using appropriate sized cuffs for Matsuyoshi mercurial sphygmomanometers (MY 605 P-Japan). Blood pressure was measured using the auscultatory method with the subject in the sitting position after allowing participants to appropriately rest. The systolic blood pressure was determined by the onset of the ‘tapping’ Korotkoff sounds (K1). The fifth Korotkoff sound (K5), or the disappearance of Korotkoff sound, was used to define diastolic blood pressure.
Anthropometry and adiposity
Anthropometric measurements were obtained from all participants using standardized anthropometric measurement techniques adapted from the ‘Anthropometric standardization reference manual’ (Lohman et al., 1991). Height was measured using a Microtoise tape suspended from a wall and was recorded to the nearest 0.1 cm. Weight was measured by Tanita electronic scale (Tanita body fat monitor, BF 571, Tanita Corporation, Japan) and was recorded to the nearest 100 g. Waist and hip circumference were measured by non-stretch tape and recorded to the nearest 0.1 cm. Waist circumference was measured at navel level and hip circumference was measured at the largest level of the buttock. Skinfold thicknesses were measured in a randomly selected subsample of participants (600/1488 persons) using the Harpenden skinfold caliper (H.E. Morse Co. British Indicators, Ltd, Burgess Hill, West Sussex, UK). Four sites were chosen: triceps, subscapular, abdominal and thigh skinfold thickness.
Biochemical indicators
All participants were asked to fast overnight before the survey day. A venous blood sample of 4 ml was collected from a vein on the participants’ forearm by trained and experienced laboratory technicians from the Nutrition Centre HCMC. Serum biochemical indicators including fasting blood glucose, lipid profile (triglyceride, total cholesterol, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol) were measured using a photometer technique (Fully Automated Bio Chemistry Analyzer, Hitachi, Japan) by Medic Medical Center Laboratory, HCMC.
Definition of overweight and obesity
Analyses of this cross-sectional survey data reported elsewhere have identified optimal BMI and waist circumference cutoff values for defining overweight and obesity in this adult Vietnamese population (Cuong, 2004). The optimal BMI cut offs for overweight were ⩾23 kg/m2 for both genders and for obesity were ⩾26.1 kg/m2 for men and ⩾27.3 kg/m2 for women. WHO has suggested for Asian populations additional BMI cut offs for overweight and obesity as ‘action trigger points for public health action’. In this modified definition, the cutoff values for underweight and normal weight are similar to those recommended for Western populations, but the differences are with the cutoff values for defining overweight (⩾23 kg/m2) and obesity (⩾27.5 kg/m2). Both the traditional BMI cutoff values recommended by WHO for Western populations (overweight: BMI 25–29.9kg/m2; obesity: BMI ⩾30 kg/m2) and the Asian-specific BMI cutoff values described above were used in the analyses. The traditional BMI cutoff values derived from Western populations were used to allow comparisons with other studies. However, the analysis based on Asian-specific BMI cutoff values gives a better estimation of the prevalence of high BMI associated with increased cardiovascular and diabetes risks in populations in Vietnam (Cuong, 2004), and thus allows a meaningful comparison of health risks across populations.
In this Vietnamese adult population, the optimal waist circumference cut offs for overweight were ⩾79 cm for men and ⩾77 cm for women, and for obesity were ⩾86 cm for both genders (Cuong, 2004). These waist circumference cutoff values for defining abdominal obesity, together with the traditional cutoff values used in Western populations (overweight: 94–101.9 cm (male), 80–87.9 cm (female); obesity: ⩾102 cm (male) and ⩾88 cm (female), were both used in the analyses.
Statistical analysis
Household assets were used to construct a household wealth index as an indicator of economic status. Ownership of a list of household assets was gathered by interview and included household vehicles, entertainment appliances and household appliances. A wealth index was constructed using methods recommended by the World Bank Poverty Network and UNICEF, and described by Filmer and Pritchett, (2001).
Prevalence of overweight and obesity as well as underweight have been calculated for each age and gender group, and for the total population. Confidence intervals (CI) for prevalence estimates were calculated to take account of the first stage of the cluster sampling design using the ‘svy’ commands in STATA version 8.2 (2003; Stata Corporation, College Station, TX, USA) (Stata, 2003). The total prevalence was adjusted for age and sex by a direct standardization method with the Vietnamese National Census April 1999 (HCMC Statistics Department, 2000) as the standard population. Ninety-five percent CI for age and sex-adjusted prevalence have been calculated using the following formula: 95% CI=adjusted prevalence±1.96* standard error (s.e.). The s.e. were obtained from ‘svy’ commands in STATA and were adjusted for cluster sampling design used in the survey (Stata, 2003).
Results
Socio-demographic and clinical characteristics of the sample
One thousand five hundred people were contacted, and among them, 21% declined but were replaced by 317 participants of similar background from the same cluster. One thousand four hundred and eighty-eight participants completed the survey in which 48% were male, and the mean age was 38 years ±11 years. The socio-demographic and clinical characteristics for men and women separately and for the total population studied are presented in Tables 1 and 2. The distributions for age were different for men and women. There were more men in the age group 20–29 years and fewer men in the age group 50–60 years compared with women, thus indicating the need for age-adjustment if the calculated prevalence estimates are to represent the population in HCMC. Migration into HCMC for work and study are possible explanations for the gender differences in specific age groups. There were different patterns of occupation for men and women but no gender differences for level of education, household wealth and ethnicity.
Men were found to have higher mean blood pressure, a much higher prevalence of current smoking compared with women. In contrast the prevalence of high fasting blood glucose and the lipid profiles were similar for men and women.
Prevalence of overweight and obesity
Using the traditional BMI cutoff values recommended by WHO for Western populations (overweight: BMI 25–29.9kg/m2; obesity: BMI ⩾30 kg/m2) (World Health Organisation, 1998), the age-standardized prevalence of overweight and obesity among Vietnamese adults in HCMC was 15.4 and 1.8%, respectively. Using the traditional waist circumference cutoff values for defining abdominal obesity (overweight: 94–101.9 cm (male), 80–87.9 cm (female); obesity: ⩾102 cm (male) and ⩾88 cm (female)) (World Health Organisation, 1998), the age-standardized prevalence of abdominal overweight and obesity among Vietnamese adults living in urban area was 8.1 and 3.3%, respectively.
However, using the Asian-specific BMI cutoff values (overweight: BMI 23–27.4 kg/m2; obesity: BMI⩾27.5 kg/m2) (Barba et al., 2004) the age-standardized prevalence of overweight and obesity among Vietnamese adults in HCMC was much higher at 26.2 and 6.4%, respectively (Table 3). Similarly, using the Vietnamese-specific cutoffs for defining abdominal overweight (waist circumference ⩾79–85.9 cm in males and ⩾77–85.9 cm in females), and abdominal obesity (waist circumference ⩾86 cm in both sexes), the age standardized prevalence of abdominal overweight and obesity among Vietnamese adults living in urban areas was 18.7 and 10.0%, respectively (Table 3).
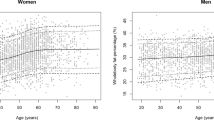
Prevalence of under-weight
The age-standardized prevalence of underweight among Vietnamese adults living in HCMC was 20.4%. Overall, the age-standardized prevalence of underweight (BMI <18.5 kg/m2) was higher in males than in females although this difference was not significant (Table 4). However there was a markedly different age-specific pattern of underweight for each sex. There was a much higher prevalence in all underweight categories in younger women than in men, but this was reversed for older men. These gender differences were statistically significant as seen from the CI for the age group 50–60 years, but not for the younger age groups (Table 4).
Household wealth status
The prevalence of overweight (both defined by BMI and waist circumference) grouped by household wealth status is presented in Table 5. The prevalence of overweight defined by BMI or waist circumference differed by sex across the household wealth categories. In men, the prevalence of overweight progressively increased as household wealth status increased and the difference between the men from the highest vs lowest household wealth categories was statistically significant as seen from the CI (Table 5). In women, there were no differences in the prevalence of overweight across the household wealth categories.
Discussion
The results from this survey show that both overnutrition and undernutrition are present in this Vietnamese urban adult population. Overweight and obesity (defined as BMI 23–27.4 kg/m2 and BMI⩾27.5 kg/m2) were found in 26.2 and 6.4%, respectively, of the population, whereas underweight (defined as BMI <18.5 kg/m2) was found in 20.4% of the population. This finding of a high prevalence of both underweight and overweight provides evidence of a ‘nutrition transition’ (Popkin et al., 2001) occurring in this urban population in Vietnam, and further supports the relevance of this concept.
Compared with other countries in the region, the problem of overweight in urban areas of Vietnam is less severe. The prevalence of overweight (defined as BMI 25–29.9 kg/m2) of Vietnamese adults living in HCMC Vietnam of 15.4% was lower than Malaysian adults nationwide (20.7%) (Tee, 2002), Malaysian urban adults (29.0%) (Tee, 1999), Singapore adults nationwide (24.4%) (Ministry of Health Singapore, 1999), Japanese men (24.5%), Japanese women (17.8%) (Yoshiike and Kaneda, 22–24 April 2002), Hong Kong Chinese adults (28.9%) (Ko et al., 2001), Thai adults (28.3%) (Aekplakorn et al., 2004) and Chinese adults (18.6%) (Wang et al., 2001).
Similarly, the prevalence of obesity (defined as BMI ⩾30 kg/m2) of Vietnamese adults living in HCMC Vietnam (1.8%) was also lower than adults in Malaysia nationwide (5.8%) (Tee, 2002), Malaysia urban adults (12.0%) (Tee, 1999), Singapore adults nationwide (6.0%) (Ministry of Health Singapore, 1999), Japanese men (2.3%), Japanese women (3.4%) (Yoshiike and Kaneda, 22–24 April 2002), Hong Kong Chinese adults (3.6%) (Ko et al., 2001), Thai adults (6.8%) (Aekplakorn et al., 2004) and Chinese adults (2.5%) (Wang et al., 2001).
These differences in prevalence of overweight and obesity between Vietnam and other countries in the region indicate the early stage of the nutrition transition in Vietnam. However, the trend in overweight is more important than the absolute prevalence. In HCMC Vietnam, the prevalence of overweight (BMI 25–29.9 kg/m2) in Vietnamese adults living in urban areas has increased from 13.8% (in adults ⩾15 years) in 2001 Hung et al., 2002) to 15.4% in adults 20–60 years in our survey in 2004. Although the age ranges of the populations assessed in this comparison were not exactly identical, the analysis does give an indication that the prevalence of overweight in adults in HCMC has tended to increase over the past few years. A similar rapid trend of increasing prevalence of overweight in adults can also be seen in other countries in the region. For example, in China the prevalence of overweight in urban areas has increased from 9.7% in 1982 to 14.9% in 1992, and to 18.6% in 2001 (Ke-You and Da-Wei, 2001). Other examples of this trend pattern can be seen in Malaysia, Thailand and Philippines (Tee, 1999; World Health Organisation, 2000; Aekplakorn et al., 2004). However, the prevalence of overweight and obesity seems to have stabilized in some countries for example Japan, Hong Kong, and Singapore at around 20% of the adult population. Differences in the speed of economic change, the rate of dietary change, the underlying traditional diets, the nutritional experiences of the adults as young children and environmental changes leading to reduced-physical activity might all explain some of the differences in the rate of change of the prevalence of overweight in adults among these countries in Asia.
We found that the adjusted prevalence of overweight (defined by both cutoff values: BMI 25–29.9 kg/m2 or BMI 23–27.4 kg/m2) was similar for men and women. However, women did have a higher prevalence of obesity compared to men (see Table 3). These findings are consistent with others studies from Thailand (Aekplakorn et al., 2004) and China (Wang et al., 2001) and with the majority of studies worldwide, which have reported slightly higher prevalence of obesity in women (James et al., 2001). The reason for this difference is probably biological and related to differences in the ability of men and women to deposit fat vs lean tissues when in energy imbalance, or might be related to gender differences in behavior change in response to alterations in the environment. In addition, social and environmental factors may also contribute to this difference in the prevalence of obesity between men and women. Women are more often in a domestic environment with constant access to food that is more conducive to recurrent eating (James et al., 2001). Finally, differences in physical activity and occupation or even smoking might in part explain the gender differences.
The prevalence of overweight (defined as BMI 23–27.4 kg/m2) and obesity (BMI ⩾27.5 kg/m2) in Vietnamese adults more than doubled between the age groups 20–29 and 50–60 years (Table 3). This pattern is similar to that reported from other countries where usually the prevalence of overweight and obesity progressively increases with age, although the extent of this increase varies in different countries (James et al., 2001). However, in our study population there were gender differences in this age pattern of the prevalence of overweight and obesity. In men, the prevalence of overweight and obesity gradually increased and reached a peak at 40–49 years and then dropped at age 50–60 years (Table 3). On the other hand, the prevalence of overweight and obesity in women progressively increased from age 20–29 to 50–60 years. Overweight and obesity are strongly related to economic status and occupation in men and by age 40–49 years many men will have reached the highest position in their career and have their highest income (Cuong, 2004). For Vietnamese women, biological factors like pregnancy and menopause might be more important and economic status and occupation less important.
Remarkably, we found that the increasing prevalence of overweight associated with higher economic status, as measured by the household wealth index, was only observed in men. Overweight (BMI⩾23 mg/m2) in men increased from 22.6% in the lowest household wealth category to 44.9% in the highest household wealth category. This pattern is the reverse of the pattern usually seen in Western countries where the prevalence of overweight and obesity decreases with increasing economic status especially in women rather than men (Sobal and Stunkard, 1989; James et al., 2001). However, in developing countries, the relationship between socio-economic status and obesity is strong and consistency in the reverse direction and is equally between men and women (Sobal and Stunkard, 1989). Weight perception and weight control behaviour are possible explanations for the difference (Cuong, 2004). Results from this study (data not presented here) (Cuong, 2004) indicate men in HCMC are less concerned about their weight and are less concerned to lose weight if there are overweight compared with women. Men in Vietnamese society may perceive fatness as a sign of success and wealth.
There is limited survey data about underweight in adults in East Asia and Southeast, Asia making it difficult to compare the prevalence of adult underweight in Vietnam with other countries in Asia. Most of the reports about underweight are for children. Our findings indicate that underweight in Vietnamese adults in urban areas is as important a public health problem as overweight, because the prevalence of both conditions was similar. From the limited data available in other countries, it appears that the prevalence of underweight in Vietnamese urban adults is higher than for Chinese urban adults (9% in China in 1992 (Wang et al., 2001) versus 20.4% in Vietnam) but quite similar to Thailand in 1996 (25.1 and 16.1% in men and women, respectively) (Kosulwat, 2002). Within HCMC, the prevalence of underweight has decreased slightly from 24.9% in 2001 (Hung and Loan, 2002) to 20.4% in 2004. This trend was evident in all age groups (data not shown), indicating that differences in the age structure of the samples for the two surveys did not account for the trend to decreasing prevalence of underweight between 2001 and 2004.
Although countries in East Asia and Southeast Asia are all undergoing a ‘nutrition transition’, they are at different stages in this process. The further the nutrition transition has progressed, the higher the prevalence of overweight and the lower the prevalence of underweight. Urban areas in Vietnam at present are at a stage behind other East Asian and Southeast Asian countries in this ‘nutrition transition’. This can be seen from the slightly higher prevalence of underweight than overweight in Vietnamese urban adults. Vietnam needs to formulate appropriate public health policies to deal with both those nutrition issues.
In conclusion, urban areas in Vietnam currently confront an early nutrition transition with the double burden of underweight and overweight in the adult population. The problem of overweight and obesity was slightly more prevalent in females than in males, in older age groups and in men of high economic status. Appropriate public health policies are needed to deal with both problems and continued surveillance is required to estimate the trends in nutritional status of Vietnamese urban adults and to provide information to evaluate future interventions.
References
Aekplakorn W, Chaiyapong Y, Neal B, Chariyalertsak S, Kunanusont C, Phoolcharoen W et al. (2004). Prevalence and determinants of overweight and obesity in Thai adults: results of the Second National Health Examination Survey. J Med Assoc Thai 87, 685–693.
Barba C, Cavalli-Sforza T, Cutter J, Darnton-Hill I (2004). Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. The Lancet 363, 157.
Bjorntorp P (ed) (2001). International Textbook of Obesity. John Wiley & Sons Ltd: Chichester,pp 337–410.
Cuong TQ (2004). Assessment of the prevalence of obesity and related risk factors in Vietnamese adults living in urban areas of Ho Chi Minh City, Vietnam. Faculty of Health, University of Newcastle: Newcastle.
Filmer D, Pritchett LH (2001). Estimating wealth effects without expenditure data – or tears: an application to educational enrollments in states of India. Demography 38, 115–132.
Hanh TTM, Komatsu T, Hung NTK (2001). Nutrition status of middle-aged Vietnamese in HCMC. J Am College Nutr 20, 616–622.
Hochiminh City Statistics Department (2000). Ho Chi Minh City Population-Results from the National Census 1st April 1999. Statistics Department: Hochiminh.
Hung NTK, Loan TTH (2002). The overweight and obesity status in Ho Chi Minh City demographic strata 1996–2001. The Technical, Public Health and Preventive Medicine Symposium in Ho Chi Minh City 28–36.
Hung NTK, Loan TTH, Son LNTD (2002). An epidemiological survey on diabetes in population over 15 years old in HCM city-2001. Vietnam National Scientific Symposium on Nutrition.
James PT, Leach R, Kalamara E, Shayeghi M (2001). The worldwide obesity epidemic. Obes Res 9, 228S–233S.
Ke-You G, Da-Wei F (2001). The magnitude and trends of under- and over-nutrition in Asian countries. Biomed Environ Sci 14, 53–60.
Ko GT, Wu MM, Tang J, Wai HP, Chan CH, Chen R (2001). Body mass index profile in Hong Kong Chinese adults. Ann Acad Med, Singapore 30, 393–396.
Kosulwat V (2002). The nutrition and health transition in Thailand. Public Health Nutr 5, 183–189.
Lohman TG, Roche AF, Martorell R (1991). Anthropometric Standardization Reference Manual. A Division of Human Kinetics Publishers, Inc: Champaign.
Ministry of Health Singapore (1999). National Health Survey 1998, Singapore. Singapore, Ministry of Health, Epidemiology and Disease Control.
Popkin BM, Horton SH, Kim S (2001). The Nutrition Transition and Prevention of Diet-Related Diseases in Asia and Pacific. Food Nutri Bullet 22, 1–58.
Popkin BM, Gordon-Larsen P (2004). The nutrition transition: worldwide obesity dynamics and their determinants. Int J Obes Relat Metab Disord 28, S2–S9.
Sakamoto M, Ishii S, Kashiwazaki H, Chiu P, Chen C, Chang N et al. (1997). A collaborative study of nutritional knowledge, attitude and food practices among urban adults in the Asian region. 2nd International Workshop on Nutritional Problems and Strategies in the Asian region, Kuala Lumpur.
Sobal J, Stunkard AJ (1989). Socioeconomic Status and Obesity: A Review of the Literature. Psychol Bull 105, 260–275.
Stata (2003). Statistics/Data analysis software. Stata Corporation: College Station, TX, USA.
Tee ES (1999). Nutrition of Malaysia: where are we heading? Malays J Nutr 5, 87–109.
Tee E-S (2002). Obesity in Asia: prevalence and issues in assessment methodologies. Asia Pac J Clin Nutr 11, S694–S701.
Wang W, Wang K, Li T (2001). A study on the epidemiological characteristics of obesity in Chinese Adults]. Zhonghua Liu Xing Bing Xue Za Zhi 22, 129–132.
World Health Organisation (1998). Prevention and Management of the Global Epidemic of Obesity. In: Report of the WHO Consultation on Obesity. WHO: Geneva.
World Health Organisation, International Association for the Study of Obesity, International Obesity Task Force (2000). The Asia-Pacific Perspective: Redefining Obesity and its Treatment. Publisher: Health Communications: Sydney.
Yoshiike N, Kaneda F (22–24 April 2002). What are reasonable and effective population approaches to combat an increasing trend of overweight in Japan?. ILSI Symposium and Workshop on Forging Effective Strategies for Prevention and Management of Overweight and Obesity in Asia ILSI: Singapore.
Acknowledgements
We are grateful to Health Consequences for Population Change Program of The Wellcome Trust, United Kingdom for financial support for this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cuong, T., Dibley, M., Bowe, S. et al. Obesity in adults: an emerging problem in urban areas of Ho Chi Minh City, Vietnam. Eur J Clin Nutr 61, 673–681 (2007). https://doi.org/10.1038/sj.ejcn.1602563
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/sj.ejcn.1602563
Keywords
This article is cited by
-
Nutrition transition in Vietnam: changing food supply, food prices, household expenditure, diet and nutrition outcomes
Food Security (2020)
-
Disordered eating behaviors in university students in Hanoi, Vietnam
Journal of Eating Disorders (2015)
-
Household food insecurity, diet, and weight status in a disadvantaged district of Ho Chi Minh City, Vietnam: a cross-sectional study
BMC Public Health (2015)
-
Etiology of Obesity Over the Life Span: Ecological and Genetic Highlights from Asian Countries
Current Obesity Reports (2014)
-
Prevalence and Risk Factors of Type 2 Diabetes in Older Vietnam-Born Australians
Journal of Community Health (2014)