Abstract
Purpose
To investigate peripheral lamina cribrosa depth (PLCD) and its vertical-horizontal difference in eyes with primary open-angle glaucoma (POAG).
Methods
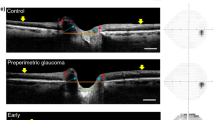
Patients with POAG (n=90 eyes) and age-matched healthy individuals (n=90 eyes) underwent swept-source optical coherence tomography (SS-OCT) scans centered at the optic discs. The PLCD was defined as the vertical distance between the most peripheral visible end of anterior lamina cribrosa (LC) surface and the reference plane connecting the Bruch’s membrane openings. The PLCD in each quadrant region and the vertical-horizontal PLCD difference were compared between the POAG and healthy eyes. The clinical factors associated with increased PLCD were evaluated.
Results
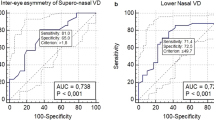
The PLCD was significantly larger in the POAG eyes than the control eyes at the horizontal (P=0.034) and vertical (P=0.001) meridians. The vertical PLCD was significantly larger than the horizontal PLCD, both in the POAG eyes (P<0.001) and in the control eyes (P=0.003). However, the vertical-horizontal PLCD difference was significantly larger in the POAG eyes (47±60 μm) than in the control eyes (18±54 μm, P=0.001). Multivariate regression showed a significant association of male gender (P=0.005), increased baseline IOP (P=0.043), and decreased MD of VF (P=0.025) with increased PLCD.
Conclusions
The peripheral LC was displaced more posteriorly in the POAG eyes compared with the age-matched healthy eyes. In the POAG eyes, the peripheral LC was displaced more posteriorly at the vertical meridian than at the horizontal meridian. The peripheral LC in the vertical meridian might have increased IOP-related strain (deformation) compared with horizontal meridian in glaucomatous eyes.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Emery JM, Landis D, Paton D, Boniuk M, Craig JM . The lamina cribrosa in normal and glaucomatous human eyes. Trans Am Acad Ophthalmol Otolaryngol 1974; 78 (2): OP290–OP297.
Quigley HA, Addicks EM . Regional differences in the structure of the lamina cribrosa and their relation to glaucomatous optic nerve damage. Arch Ophthalmol 1981; 99 (1): 137–143.
Quigley HA, Addicks EM, Green WR, Maumenee AE . Optic nerve damage in human glaucoma. II. The site of injury and susceptibility to damage. Arch Ophthalmol 1981; 99 (4): 635–649.
Radius RL . Regional specificity in anatomy at the lamina cribrosa. Arch Ophthalmol 1981; 99 (3): 478–480.
Radius RL, Gonzales M . Anatomy of the lamina cribrosa in human eyes. Arch Ophthalmol 1981; 99 (12): 2159–2162.
Quigley HA, Hohman RM, Addicks EM, Massof RW, Green WR . Morphologic changes in the lamina cribrosa correlated with neural loss in open-angle glaucoma. Am J Ophthalmol 1983; 95 (5): 673–691.
Bellezza AJ, Rintalan CJ, Thompson HW, Downs JC, Hart RT, Burgoyne CF . Deformation of the lamina cribrosa and anterior scleral canal wall in early experimental glaucoma. Invest Ophthalmol Vis Sci 2003; 44 (2): 623–637.
Burgoyne CF, Downs JC, Bellezza AJ, Suh JK, Hart RT . The optic nerve head as a biomechanical structure: a new paradigm for understanding the role of IOP-related stress and strain in the pathophysiology of glaucomatous optic nerve head damage. Prog Retin Eye Res 2005; 24 (1): 39–73.
Crawford Downs J, Roberts MD, Sigal IA . Glaucomatous cupping of the lamina cribrosa: a review of the evidence for active progressive remodeling as a mechanism. Exp Eye Res 2011; 93 (2): 133–140.
Sigal IA, Yang H, Roberts MD, Grimm JL, Burgoyne CF, Demirel S et al. IOP-induced lamina cribrosa deformation and scleral canal expansion: independent or related? Invest Ophthalmol Vis Sci 2011; 52 (12): 9023–9032.
Yang H, Thompson H, Roberts MD, Sigal IA, Downs JC, Burgoyne CF . Deformation of the early glaucomatous monkey optic nerve head connective tissue after acute IOP elevation in 3-D histomorphometric reconstructions. Invest Ophthalmol Vis Sci 2011; 52 (1): 345–363.
Yang H, Williams G, Downs JC, Sigal IA, Roberts MD, Thompson H et al. Posterior (outward) migration of the lamina cribrosa and early cupping in monkey experimental glaucoma. Invest Ophthalmol Vis Sci 2011; 52 (10): 7109–7121.
Lee KM, Kim TW, Weinreb RN, Lee EJ, Girard MJ, Mari JM . Anterior lamina cribrosa insertion in primary open-angle glaucoma patients and healthy subjects. PLoS One 2014; 9 (12): e114935.
Dandona L, Quigley HA, Brown AE, Enger C . Quantitative regional structure of the normal human lamina cribrosa. A racial comparison. Arch Ophthalmol 1990; 108 (3): 393–398.
Jonas JB, Mardin CY, Schlotzer-Schrehardt U, Naumann GO . Morphometry of the human lamina cribrosa surface. Invest Ophthalmol Vis Sci 1991; 32 (2): 401–405.
Sigal IA, Ethier CR . Biomechanics of the optic nerve head. Exp Eye Res 2009; 88 (4): 799–807.
Kim TW, Kagemann L, Girard MJ, Strouthidis NG, Sung KR, Leung CK et al. Imaging of the lamina cribrosa in glaucoma: perspectives of pathogenesis and clinical applications. Curr Eye Res 2013; 38 (9): 903–909.
Park SC . In vivo evaluation of lamina cribrosa deformation in glaucoma. J Glaucoma 2013; 22 (Suppl 5): S29–S31.
Park SC, Kiumehr S, Teng CC, Tello C, Liebmann JM, Ritch R . Horizontal central ridge of the lamina cribrosa and regional differences in laminar insertion in healthy subjects. Invest Ophthalmol Vis Sci 2012; 53 (3): 1610–1616.
Furlanetto RL, Park SC, Damle UJ, Sieminski SF, Kung Y, Siegal N et al. Posterior displacement of the lamina cribrosa in glaucoma: in vivo interindividual and intereye comparisons. Invest Ophthalmol Vis Sci 2013; 54 (7): 4836–4842.
Seo JH, Kim TW, Weinreb RN . Lamina cribrosa depth in healthy eyes. Invest Ophthalmol Vis Sci 2014; 55 (3): 1241–1251.
Wei WB, Xu L, Jonas JB, Shao L, Du KF, Wang S et al. Subfoveal choroidal thickness: the Beijing Eye Study. Ophthalmology 2013; 120 (1): 175–180.
Lee SW, Yu SY, Seo KH, Kim ES, Kwak HW . Diurnal variation in choroidal thickness in relation to sex, axial length, and baseline choroidal thickness in healthy Korean subjects. Retina 2014; 34 (2): 385–393.
Ren R, Yang H, Gardiner SK, Fortune B, Hardin C, Demirel S et al. Anterior lamina cribrosa surface depth, age, and visual field sensitivity in the Portland Progression Project. Invest Ophthalmol Vis Sci 2014; 55 (3): 1531–1539.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Meeting Presentation: Poster presentation at AAO annual meeting 2014, Chicago. (PO382)
Author contributions
Design and conduct of the study: YWK, JWJ and KHP, collection of the data: YWK, DWK, JWJ, KHP and DMK, management of the data: YWK, DWK, JWJ and KHP, analysis of the data: YWK, DWK, JWJ and KHP, interpretation of the data: YWK, DWK, JWJ, KHP and DMK, preparation of the manuscript: YWK, DWK, JWJ and KHP, review of the manuscript: YWK, JWJ and KHP, approval of the manuscript: YWK and KHP.
Supplementary Information accompanies this paper on Eye website
Supplementary information
Rights and permissions
About this article
Cite this article
Kim, Y., Kim, D., Jeoung, J. et al. Peripheral lamina cribrosa depth in primary open-angle glaucoma: a swept-source optical coherence tomography study of lamina cribrosa. Eye 29, 1368–1374 (2015). https://doi.org/10.1038/eye.2015.162
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/eye.2015.162
This article is cited by
-
The role of intracranial pressure in glaucoma and therapeutic implications
Eye (2020)
-
Age-Dependent Variation of Lamina Cribrosa Displacement During the Standardized Valsalva Maneuver
Scientific Reports (2019)
-
Optic disc cupping characteristics of normal pressure hydrocephalus patients with normal-tension glaucoma
Scientific Reports (2019)
-
Combination of Enhanced Depth Imaging Optical Coherence Tomography and Fundus Images for Glaucoma Screening
Journal of Medical Systems (2019)
-
Comparison of glaucoma-diagnostic ability between wide-field swept-source OCT retinal nerve fiber layer maps and spectral-domain OCT
Eye (2018)