Abstract
Purpose
Dry eye syndrome (DES) causes significant morbidity. Trials of blood-derived products in treatment of the condition show promising results. However, their production is expensive and time-consuming. We investigate fingerprick autologous blood (FAB) as an alternative low-cost, readily accessible treatment for DES.
Patients and methods
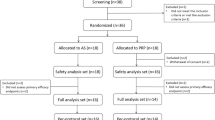
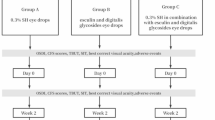
Prospective, non-comparative, interventional case series. In total, 29 eyes of 16 DES patients (2 males and 14 females) from two NHS sites in the United Kingdom. Patients instructed to clean a finger, prick with a blood lancet, and apply a drop of blood to the lower fornix of the affected eye(s), 4 times daily for 8 weeks then stop and review 4 weeks later. Follow-up visits occurred ~3 days, 2, 4, 8 weeks into therapy, and 4 weeks post-cessation. At each visit, visual acuity, corneal staining, Schirmer’s test, tear break-up time (TBUT), and ocular comfort index (OCI) were measured, and photographs taken. Results were analysed using Student’s paired t-test.
Results
At 8 weeks, there was improvement in mean Oxford corneal staining grade (3.31 to 2.07 (P<0.0001)), TBUT (5.00 to 7.80 s (P<0.05)), visual acuity (0.08 to 0.01 LogMAR equivalent (P<0.05)), and OCI score (56.03 to 39.72 (P<0.0001)). There was no statistically significant change in Schirmer’s test results. Four weeks post-cessation versus immediately after completion of FAB therapy, mean staining grade worsened from 2.07 to 2.86 (P<0.0001). OCI score worsened from 39.72 to 44.67 (P<0.05).
Conclusions
In our limited case series FAB appears to be a safe and effective treatment for DES.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
The Epidemiology of Dry Eye Disease: Report of the Epidemiology Subcommittee of the International Dry Eye WorkShop. Ocular Surf 2007; 5: 93–107.
Rauz S, Saw VP . Serum eye drops, amniotic membrane and limbal epithelial stem cells—tools in the treatment of ocular surface disease. Cell Tissue Bank 2010; 11: 13–27.
Yamada C, King KE, Ness PM . Autologous serum eyedrops: literature review and implications for transfusion medicine specialists. Transfusion 2008; 48: 1245–1255.
Fox RI, Chan R, Michelson JB, Belmont JB, Michelson PE . Beneficial effect of artificial tears made with autologous serum in patients with keratoconjunctivitis sicca. Arthritis Rheum 1984; 27: 459–461.
Noble BA . Comparison of autologous serum eye drops with conventional therapy in a randomised controlled crossover trial for ocular surface disease. Br J Ophthalmol 2004; 88: 647–652.
Schrader S, Wedel T, Moll R, Geerling G . Combination of serum eye drops with hydrogel bandage contact lenses in the treatment of persistent epithelial defects. Graefes Arch Clin Exp Ophthalmol 2006; 244: 1345–1349.
Young AL, Cheng ACO, Ng HK, Cheng LL, Leung GYS, Lam DSC . The use of autologous serum tears in persistent corneal epithelial defects. Eye 2004; 18: 609–614.
Chiang CC, Chen WL, Lin JM, Tsai YY . Allogeneic serum eye drops for the treatment of persistent corneal epithelial defect. Eye (Lond) 2009; 23: 290–293.
Matsumoto Y . Autologous serum application in the treatment of neurotrophic keratopathy*1. Ophthalmology 2004; 111: 1115–1120.
del Castillo JMB, de la Casa JM, Sardiña RC, Fernandez RM, Feijoo JG, Gomez AC et al. Treatment of recurrent corneal erosions using autologous serum. Cornea 2002; 21: 781–783.
Fernando AI, Burton BJL, Smith GT, Corbett MC . Autologous serum drop-dependent re-epithelialisation following penetrating keratoplasty in chronic graft vs host disease. Eye (Lond) 2005; 19: 823–825.
Ogawa Y, Okamoto S, Mori T, Yamada M, Mashima Y, Watanabe R et al. Autologous serum eye drops for the treatment of severe dry eye in patients with chronic graft-versus-host disease. Bone Marrow Transplant 2003; 31: 579–583.
Goto E, Shimmura S, Shimazaki J, Tsubota K . Treatment of superior limbic keratoconjunctivitis by application of autologous serum. Cornea 2001; 20: 807–810.
Partal A, Scott E . Low-cost protocol for the production of autologous serum eye drops by blood collection and processing centres for the treatment of ocular surface diseases. Transfus Med 2011; 21: 271–277.
Cho YK, Huang W, Kim GY, Lim BS . Comparison of autologous serum eye drops with different diluents. Curr Eye Res 2013; 38: 9–17.
López-García JS, García-Lozano I, Rivas L, Ramírez N, Raposo R, Méndez MT . Autologous serum eye drops diluted with sodium hyaluronate: clinical and experimental comparative study. Acta Ophthalmol 2014; 92: e22–e29.
Fischer KR, Opitz A, Böeck M, Geerling G . Stability of serum eye drops after storage of 6 months. Cornea 2012; 31: 1313–1318.
Rocha EM, Pelegrino FSA, de Paiva CS, Vigorito AC, de Souza CA . GVHD dry eyes treated with autologous serum tears. Bone Marrow Transplant 2000; 25: 1101–1103.
Tananuvat N, Daniell M, Sullivan LJ, Yi Q, McKelvie P, McCarty DJ et al. Controlled study of the use of autologous serum in dry eye patients. Cornea 2001; 20: 802–806.
Poon AC . Autologous serum eyedrops for dry eyes and epithelial defects: clinical and in vitro toxicity studies. Br J Ophthalmol 2001; 85: 1188–1197.
Welder JD, Bakhtiari P, Djalilian AR . Limbitis secondary to autologous serum eye drops in a patient with atopic keratoconjunctivitis. Case Rep Ophthalmol Med 2011; 2011: 1–3.
McDonnell PJ, Schanzlin DJ, Rao NA . Immunoglobulin deposition in the cornea after application of autologous serum. Arch Ophthalmol 1988; 106: 1423–1425.
Johnson ME, Murphy PJ . Measurement of ocular surface irritation on a linear interval scale with the ocular comfort index. Invest Ophthalmol Vis Sci 2007; 48: 4451–4458.
Bron AJ, Evans VE, Smith JA . Grading of corneal and conjunctival staining in the context of other dry eye tests. Cornea 2003; 22: 640–650.
Chang J-H, Garg NK, Lunde E, Han K-Y, Jain S, Azar DT . Corneal neovascularization: an anti-VEGF therapy review. Surv Ophthalmol 2012; 57: 415–429.
Joyce NC . Cell cycle status in human corneal endothelium. Exp Eye Res 2005; 81: 629–638.
Hartwig D, Herminghaus P, Wedel T, Liu L, Schlenke P, Dibbelt L et al. Topical treatment of ocular surface defects: comparison of the epitheliotrophic capacity of fresh frozen plasma and serum on corneal epithelial cells in an in vitro cell culture model. Transfus Med 2005; 15: 107–113.
Blair P, Flaumenhaft R . Platelet α-granules: Basic biology and clinical correlates. Blood Rev 2009; 23: 177–189.
Yang ZW, Yang SH, Chen L, Qu J, Zhu J, Tang Z . Comparison of blood counts in venous, fingertip and arterial blood and their measurement variation. Clin Lab Haematol 2001; 23: 155–159.
Podgórski T, Bartkowiak U, Pawlak M . Comparison of hematological parameters of venous and capillary blood in athletes. Trends Sport Sci 2014; 21.
Kim MJ, Jin JH, Kwon YS, Jun YH, Kim SK . Comparison of blood counts in capillary and venous blood in children. Korean J Hematol 2009; 44: 237.
Leppänen E . Experimental basis of standardized specimen collection: The effect of the site of venipuncture on the blood picture, the white blood cell differential count, and the serum albumin concentration. Eur J Haematol 2009; 41: 445–448.
Daae LNW, Hallerud M, Halvorsen S . A comparison between haematological parameters in ‘capillary’ and venous blood samples from hospitalized children aged 3 months to 14 years. Scand J Clin Lab Invest 1991; 51: 651–654.
Bond MM, Richards-Kortum RR . Drop-to-drop variation in the cellular components of fingerprick blood. Am J Clin Pathol 2015; 144: 885–894.
Phasukkijwatana N, Lertrit P, Liammongkolkul S, Prabhasawat P . Stability of epitheliotrophic factors in autologous serum eye drops from chronic Stevens-Johnson syndrome dry eye compared to non-autoimmune dry eye. Curr Eye Res 2011; 36: 775–781.
Bradley JC, Bradley RH, McCartney DL, Mannis MJ . Serum growth factor analysis in dry eye syndrome. Clin Exp Ophthalmol 2008; 36: 717–720.
Antunes RF, Brandão C, Maia M, Arosa FA . Red blood cells release factors with growth and survival bioactivities for normal and leukemic T cells. Immunol Cell Biol 2011; 89: 111–121.
Zapuskalov I, Krivosheina O, Elegesheva O . [Use of autologous blood mononuclear cells in the complex treatment of corneal ulcers]. Vestn Oftalmol 2008; 124: 32–35.
Kahraman S, Rezai SM, Dogu H, Sayan MA, Akar Z . Painful traumatic neuroma after a finger stick. Anesth Analg 2005; 100: 1414–1415.
Acknowledgements
Infrastructural support from the NIHR Moorfields Biomedical Research Centre.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on Eye website
Rights and permissions
About this article
Cite this article
Than, J., Balal, S., Wawrzynski, J. et al. Fingerprick autologous blood: a novel treatment for dry eye syndrome. Eye 31, 1655–1663 (2017). https://doi.org/10.1038/eye.2017.118
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/eye.2017.118
This article is cited by
-
THBS1 inhibition alleviates inflammatory response by inhibiting TGF-β and NLRP3 inflammasome in experimental murine dry eye
Medical Molecular Morphology (2025)
-
Autologe Serumaugentropfen bei therapieresistenten Epitheldefekten der Kornea
Die Ophthalmologie (2023)
-
Treatment of Non-Infectious Corneal Injury: Review of Diagnostic Agents, Therapeutic Medications, and Future Targets
Drugs (2022)
-
Reducing the burden of ocular surface disease with serum eye drops
Eye (2021)
-
Effects of electroacupuncture on conjunctival cell apoptosis and the expressions of apoptosis-related proteins Caspase-3, Fas and Bcl-2 in rabbits with dry eye syndrome
Journal of Acupuncture and Tuina Science (2020)