Abstract
Purpose
The purpose of the study was to audit the use of non-contact ultra-widefield retinal imaging in infants with suspected abusive head trauma (AHT) using the Optos P200MA Scanning Laser Ophthalmoscope.
Patients and methods
A retrospective, observational case series. Ten eyes of five consecutive infants (aged 1–15 months) with suspected (or in 1 case, known) AHT referred for an ophthalmological opinion were included. Each infant underwent non-contact ultra-widefield retinal imaging using the Optos P200MA scanning laser ophthalmoscope. Optos fundus fluorescein angiography (FFA) was performed in one infant with oral sedation. The other four infants did not require sedation. The main outcome measure was the acquisition of a single, definitive ultra-widefield retinal image in each eye. Safety was audited by determining adverse changes in heart rate and oxygen saturations that required cessation of imaging.
Results
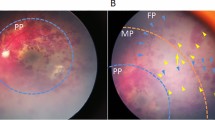
The Optos P200MA ultra-widefield scanning laser ophthalmoscope acquired good quality retinal images in all infants. Documentation of acute, widespread retinal haemorrhages contributed to a diagnosis of AHT in three infants. Chronic pre-macular haemorrhage and macular schisis were documented by FFA in a fourth infant. The absence of retinal haemorrhages was documented in a fifth infant contributing to the exclusion of a diagnosis of AHT. There were no adverse safety signals in any infant in this series.
Conclusion
The Optos P200MA ultra-widefield scanning laser ophthalmoscope appears safe to use in infants with suspected AHT, providing high-quality retinal images in a single frame without ocular contact. Optos P200MA may be used as alternative to RetCam to document retinal haemorrhages in stable infants with suspected AHT.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Maguire SA, Watts PO, Shaw AD, Holden S, Taylor RH, Watkins WJ et al. Retinal haemorrhages and related findings in abusive and non-abusive head trauma: a systematic review. Eye 2013; 27 (1): 28–36.
Carty H, Ratcliffe J . The shaken infant syndrome. BMJ 1995; 310 (6976): 344–345.
Tandon A, McIntyre S, Yu A, Stephens D, Leiby B, Croker S et al. Retinal haemorrhage description tool. Br J Ophthalmol 2011; 95 (12): 1719–1722.
Nakagawa TA, Skrinska R . Improved documentation of retinal hemorrhages using a wide-field digital ophthalmic camera in patients who experienced abusive head trauma. Arch Pediatr Adolesc Med 2001; 155 (10): 1149–1152.
Blair MP, Shapiro MJ, Hartnett ME . Fluorescein angiography to estimate normal peripheral retinal nonperfusion in children. J AAPOS 2012; 16 (3): 234–237.
Saleh M, Schoenlaub S, Desprez P, Bourcier T, Gaucher D, Astruc D et al. Use of digital camera imaging of eye fundus for telemedicine in children suspected of abusive head injury. Br J Ophthalmol 2009; 93 (4): 424–428.
Mulvihill AO, Jones P, Tandon A, Fleck BW, Minns RA . An inter-observer and intra-observer study of a classification of RetCam images of retinal haemorrhages in children. Br J Ophthalmol 2011; 95 (1): 99–104.
Fung TH, Muqit MM, Mordant DJ, Smith LM, Patel CK . Noncontact high-resolution ultra-wide-field oral fluorescein angiography in premature infants with retinopathy of prematurity. JAMA Ophthalmol 2014; 132 (1): 108–110.
Patel CK, Fung TH, Muqit MM, Mordant DJ, Brett J, Smith L et al. Non-contact ultra-widefield imaging of retinopathy of prematurity using the Optos dual wavelength scanning laser ophthalmoscope. Eye 2013; 27 (5): 589–596.
Patel CK, Fung TH, Muqit MM, Mordant DJ, Geh V . Non-contact ultra-widefield retinal imaging and fundus fluorescein angiography of an infant with incontinentia pigmenti without sedation in an ophthalmic office setting. J AAPOS 2013; 17 (3): 309–311.
Fung TH, Yusuf IH, Smith LM, Brett J, Weston L, Patel CK . Outpatient ultra wide-field intravenous fundus fluorescein angiography in infants using the Optos P200MA scanning laser ophthalmoscope. Br J Ophthalmol 2014; 98 (3): 302–304.
Kemper AR, Wallace DK, Quinn GE . Systematic review of digital imaging screening strategies for retinopathy of prematurity. Pediatrics 2008; 122 (4): 825–830.
Castellanos MA, Schwartz S, Leal R, Chan RV, Quiroz-Mercado H . Pain assessment in premature infants treated with intravitreal antiangiogenic therapy for retinopathy of prematurity under topical anesthesia. Graefes Arch Clin Exp Ophthalmol 2013; 251 (2): 491–494.
Adams GG, Clark BJ, Fang S, Hill M . Retinal haemorrhages in an infant following RetCam screening for retinopathy of prematurity. Eye 2004; 18 (6): 652–653.
Acknowledgements
CK Patel had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Author contributions
Design and conduct of the study: IHY, THMF, JSE, CKP. Collection, management, analysis, and interpretation of data: IHY, JKB, THMF, JSE, CKP. Preparation, review, or approval of the manuscript: IHY, JKB, THMF, JSE, CKP.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on Eye website
Supplementary information
Rights and permissions
About this article
Cite this article
Yusuf, I., Barnes, J., Fung, T. et al. Non-contact ultra-widefield retinal imaging of infants with suspected abusive head trauma. Eye 31, 353–363 (2017). https://doi.org/10.1038/eye.2017.2
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/eye.2017.2
This article is cited by
-
The role of retinal imaging in the management of abusive head trauma cases
International Journal of Legal Medicine (2022)