Abstract
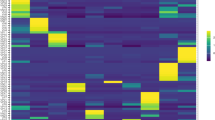
Bacterial pneumonia is a major cause of morbidity and mortality in elderly. We hypothesize that dysbiosis between regular residents of the upper respiratory tract (URT) microbiome, that is balance between commensals and potential pathogens, is involved in pathogen overgrowth and consequently disease. We compared oropharyngeal microbiota of elderly pneumonia patients (n=100) with healthy elderly (n=91) by 16S-rRNA-based sequencing and verified our findings in young adult pneumonia patients (n=27) and young healthy adults (n=187). Microbiota profiles differed significantly between elderly pneumonia patients and healthy elderly (PERMANOVA, P<0.0005). Highly similar differences were observed between microbiota profiles of young adult pneumonia patients and their healthy controls. Clustering resulted in 11 (sub)clusters including 95% (386/405) of samples. We observed three microbiota profiles strongly associated with pneumonia (P<0.05) and either dominated by lactobacilli (n=11), Rothia (n=51) or Streptococcus (pseudo)pneumoniae (n=42). In contrast, three other microbiota clusters (in total n=183) were correlated with health (P<0.05) and were all characterized by more diverse profiles containing higher abundances of especially Prevotella melaninogenica, Veillonella and Leptotrichia. For the remaining clusters (n=99), the association with health or disease was less clear. A decision tree model based on the relative abundance of five bacterial community members in URT microbiota showed high specificity of 95% and sensitivity of 84% (89% and 73%, respectively, after cross-validation) for differentiating pneumonia patients from healthy individuals. These results suggest that pneumonia in elderly and young adults is associated with dysbiosis of the URT microbiome with bacterial overgrowth of single species and absence of distinct anaerobic bacteria. Whether the observed microbiome changes are a cause or a consequence of the development of pneumonia or merely coincide with disease status remains a question for future research.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Accession codes
References
Beighton D, Gilbert SC, Clark D, Mantzourani M, Al-Haboubi M, Ali F et al. (2008). Isolation and identification of bifidobacteriaceae from human saliva. Appl Environ Microbiol 74: 6457–6460.
Biesbroek G, Sanders EAM, Roeselers G, Wang X, Caspers MPM, Trzciñski K et al. (2012). Deep sequencing analyses of low density microbial communities: working at the boundary of accurate microbiota detection. PLoS One 7: e32942.
Bogaert D, Keijser B, Huse S, Rossen J, Veenhoven R, van Gils E et al. (2011). Variability and diversity of nasopharyngeal microbiota in children: a metagenomic analysis. PLoS One 6: e17035.
Bousbia S, Papazian L, Saux P, Forel JM, Auffray J-P, Martin C et al. (2012). Repertoire of intensive care unit pneumonia microbiota. PLoS One 7: e32486.
Breiman L . (1984) Classification and regression trees. Chapman & Hall/CRC: New York, NY.
Buffie CG, Pamer EG . (2013). Microbiota-mediated colonization resistance against intestinal pathogens. Nat Rev Immunol 13: 790–801.
Caporaso JG, Kuczynski J, Stombaugh J, Bittinger K, Bushman FD, Costello EK et al. (2010). QIIME allows analysis of high-throughput community sequencing data. Nat Methods 7: 335–336.
Carvalho MDGS, Tondella ML, McCaustland K, Weidlich L, McGee L, Mayer LW et al. (2007). Evaluation and improvement of real-time PCR assays targeting lytA, ply, and psaA genes for detection of pneumococcal DNA. J Clin Microbiol 45: 2460–2466.
Chaban B, Albert A, Links MG, Gardy J, Tang P, Hill JE . (2013). Characterization of the upper respiratory tract microbiomes of patients with pandemic H1N1 influenza. PLoS One 8: e69559.
Charlson ES, Chen J, Custers-Allen R, Bittinger K, Li H, Sinha R et al. (2010). Disordered microbial communities in the upper respiratory tract of cigarette smokers. PLoS One 5: e15216.
Cho I, Blaser MJ . (2012). The human microbiome: at the interface of health and disease. Nat Rev Genet 13: 260–270.
Dethlefsen L, McFall-Ngai M, Relman DA . (2007). An ecological and evolutionary perspective on human-microbe mutualism and disease. Nature 449: 811–818.
Dickson RP, Erb-Downward JR, Huffnagle GB . (2014). Towards an ecology of the lung: new conceptual models of pulmonary microbiology and pneumonia pathogenesis. Lancet Resp Med 2: 238–246.
Duncan SH, Louis P, Thomson JM, Flint HJ . (2009). The role of pH in determining the species composition of the human colonic microbiota. Environ Microbiol 11: 2112–2122.
Eribe ERK, Olsen I . (2008). Leptotrichia species in human infections. Anaerobe 14: 131–137.
Faust K, Sathirapongsasuti JF, Izard J, Segata N, Gevers D, Raes J et al. (2012). Microbial co-occurrence relationships in the human microbiome. PLoS Comput Biol 8: e1002606.
File TM . (2003). Community-acquired pneumonia. Lancet 362: 1991–2001.
Fine MJ, Auble TE, Yealy DM, Hanusa BH, Weissfeld LA, Singer DE et al. (1997). A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med 336: 243–250.
Hansel TT, Johnston SL, Openshaw PJ . (2013). Microbes and mucosal immune responses in asthma. Lancet 381: 861–873.
Hilty M, Burke C, Pedro H, Cardenas P, Bush A, Bossley C et al. (2010). Disordered microbial communities in asthmatic airways. PLoS One 5: e8578.
Huijskens EGW, van Erkel AJM, Palmen FMH, Buiting AGM, Kluytmans JAJW, Rossen JWA . (2012). Viral and bacterial aetiology of community-acquired pneumonia in adults. Influenza Other Respir Viruses 7: 567–573.
Iwai S, Fei M, Huang D, Fong S, Subramanian A, Grieco K et al. (2012). Oral and airway microbiota in HIV-infected pneumonia patients. J Clin Microbiol 50: 2995–3002.
Jackson ML, Neuzil KM, Thompson WW, Shay DK, Yu O, Hanson CA et al. (2004). The burden of community-acquired pneumonia in seniors: results of a population-based study. Clin Infect Dis 39: 1642–1650.
Jansen AGSC, Rodenburg GD, van der Ende A, van Alphen L, Veenhoven RH, Spanjaard L et al. (2009). Invasive pneumococcal disease among adults: associations among serotypes, disease characteristics, and outcome. Clin Infect Dis 49: e23–e29.
Kaplan V, Clermont G, Griffin MF, Kasal J, Watson RS, Linde-Zwirble WT et al. (2003). Pneumonia. Arch Intern Med 163: 317–323.
Krone CL, Biesbroek G, Trzciński K, Sanders EAM, Bogaert D . (2014). Respiratory microbiota dynamics following Streptococcus pneumoniae acquisition in young and elderly mice. Infect Immun 82: 1725–1731.
Krone CL, van de Groep K, Trzciñski K, Sanders EA, Bogaert D . (2014). Immunosenescence and pneumococcal disease: an imbalance in host–pathogen interactions. Lancet Resp Med 2: 141–153.
Kumar PS, Griffen AL, Moeschberger ML, Leys EJ . (2005). Identification of candidate periodontal pathogens and beneficial species by quantitative 16S clonal analysis. J Clin Microbiol 43: 3944–3955.
Lardner A . (2001). The effects of extracellular pH on immune function. J Leukoc Biol 69: 522–530.
Laufer AS, Metlay JP, Gent JF, Fennie KP, Kong Y, Pettigrew MM . (2011). Microbial communities of the upper respiratory tract and otitis media in children. mBio 2: e00245–10.
Letunic I, Bork P . (2011). Interactive Tree Of Life v2: online annotation and display of phylogenetic trees made easy. Nucleic Acids Res 39: W475–W478.
Leung RKK, Zhou JW, Guan W, Li SK, Yang ZF, Tsui SKW . (2013). Modulation of potential respiratory pathogens by pH1N1 viral infection. Clin Microbiol Infect 19: 930–935.
Maechler M, Rousseeuw P, Struyf A, Hubert M, Hornik K . (2014). Cluster: cluster analysis basics and extensions.
Magurran AE . (2004) Measuring Biological Diversity. Blackwell Science: Oxford.
Mathers CD, Boerma T, Fat DM . (2008). The Global Burden of Disease: 2004 Update. World Health Organization: Geneva, Switzerland, 1–60.
Millett ERC, Quint JK, Smeeth L, Daniel RM, Thomas SL . (2013). Incidence of community-acquired lower respiratory tract infections and pneumonia among older adults in the United Kingdom: a population-based study. PLoS One 8: e75131.
Molyneaux PL, Mallia P, Cox MJ, Footitt J, Willis-Owen SAG, Homola D et al. (2013). Outgrowth of the bacterial airway microbiome after rhinovirus exacerbation of chronic obstructive pulmonary disease. Am J Respir Crit Care Med 188: 1224–1231.
Morris A, Beck JM, Schloss PD, Campbell TB, Crothers K, Curtis JL et al. (2013). Comparison of the respiratory microbiome in healthy nonsmokers and smokers. Am J Respir Crit Care Med 187: 1067–1075.
Ramanan P, Barreto JN, Osmon DR, Tosh PK . (2014). Rothia bacteremia - A 10 year experience at Mayo Clinic, Rochester, Minnesota. J Clin Microbiol 52: 3184–3189.
Sakwinska O, Bastic Schmid V, Berger B, Bruttin A, Keitel K, Lepage M et al. (2014). Nasopharyngeal microbiota in healthy children and pneumonia patients. J Clin Microbiol 52: 1590–1594.
Segata N, Haake SK, Mannon P, Lemon KP, Waldron L, Gevers D et al. (2012). Composition of the adult digestive tract bacterial microbiome based on seven mouth surfaces, tonsils, throat and stool samples. Genome Biol 13: R42.
Shipitsyna E, Roos A, Datcu R, Hallén A, Fredlund H, Jensen JS et al. (2013). Composition of the vaginal microbiota in women of reproductive age—sensitive and specific molecular diagnosis of bacterial vaginosis is possible? PLoS One 8: e60670.
Solís G, de los Reyes-Gavilan CG, Fernández N, Margolles A, Gueimonde M . (2010). Establishment and development of lactic acid bacteria and bifidobacteria microbiota in breast-milk and the infant gut. Anaerobe 16: 307–310.
Tichopad A, Roberts C, Gembula I, Hajek P, Skoczynska A, Hryniewicz W et al. (2013). Clinical and economic burden of community-acquired pneumonia among adults in the Czech Republic, Hungary, Poland and Slovakia Borrow. PLoS One 8: e71375.
Tusher VG, Tibshirani R, Chu G . (2001). Significance analysis of microarrays applied to the ionizing radiation response. Proc Natl Acad Sci USA 98: 5116–5121.
van de Pol AC, van Loon AM, Wolfs TFW, Jansen NJG, Nijhuis M, Breteler EK et al. (2007). Increased detection of respiratory syncytial virus, influenza viruses, parainfluenza viruses, and adenoviruses with real-time PCR in samples from patients with respiratory symptoms. J Clin Microbiol 45: 2260–2262.
van de Pol AC, Wolfs TFW, Jansen NJG, Kimpen JLL, van Loon AM, Rossen JWA . (2009). Human bocavirus and KI/WU polyomaviruses in pediatric intensive care patients. Emerging Infect Dis 15: 454–457.
van Gils EJM, Veenhoven RH, Hak E, Rodenburg GD, Bogaert D, IJzerman EPF et al. (2009). Effect of reduced-dose schedules with 7-valent pneumococcal conjugate vaccine on nasopharyngeal pneumococcal carriage in children. JAMA 302: 159–167.
Wang X, Eijkemans MJC, Wallinga J, Biesbroek G, Trzciñski K, Sanders EAM et al. (2012). Multivariate approach for studying interactions between environmental variables and microbial communities. PLoS One 7: e50267.
Wu GD, Chen J, Hoffmann C, Bittinger K, Chen Y-Y, Keilbaugh SA et al. (2011). Linking long-term dietary patterns with gut microbial enterotypes. Science 334: 105–108.
Wyllie AL, MLJN Chu, Schellens MHB, van Engelsdorp Gastelaars J, Jansen MD, van der Ende A et al. (2014). Streptococcus pneumoniae in saliva of Dutch primary school children. PLoS One 9: e102045.
Zaura E, Keijser BJ, Huse SM, Crielaard W . (2009). Defining the healthy ‘core microbiome’ of oral microbial communities. BMC Microbiol 9: 259.
Zhou Y, Lin P, Li Q, Han L, Zheng H, Wei Y et al. (2010). Analysis of the microbiota of sputum samples from patients with lower respiratory tract infections. Acta Biochim Biophys Sin 42: 754–761.
Acknowledgements
This research has received funding from the Wilhelmina Children’s Hospital Fund, ZonMW (grant 91209010) and NWO-VENI (grant 91610121). We thank Mei Ling Chu for her technical assistance and Dr Marinus JC Eijkemans for his input on the statistical analysis. This work is dedicated to the memory of Dr Reinier H Veenhoven who contributed to the planning of the design and execution of the clinical studies in healthy controls and Dr Marcel F Peeters, who was investigator in the adult pneumonia study.
Author contributions
RHV, MJB, EAMS, JWAR and DB designed the study. EGWH, GB and MRvdB wrote the study protocols. EGWH, GB, MRvdB and RHV were responsible for the recruitment of patients and collection of the samples. KT, EGWH and ALW were responsible for the conventional culturing/qPCR on the samples. ALW was responsible for sample preparation for pyrosequencing. WAAdSP, DB and XW were responsible for the post-processing of sequences and data analysis. All authors were involved in data interpretation and drafting of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
EAMS declares to have received unrestricted research support from Pfizer, grant support for vaccine studies from Pfizer and GlaxoSmithKline and fees paid to the institution for advisory boards or participation in independent data monitoring committees for Pfizer and GSK. RHV reported receiving grant support from GlaxoSmithKline and Wyeth/Pfizer for vaccine studies and consulting fees from GlaxoSmithKline. KT received grant support and consulting fees from Pfizer. DB received consulting fees from Pfizer. These grants and fees were not received for the research described in this paper. The remaining authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on The ISME Journal website
Supplementary information
Rights and permissions
About this article
Cite this article
de Steenhuijsen Piters, W., Huijskens, E., Wyllie, A. et al. Dysbiosis of upper respiratory tract microbiota in elderly pneumonia patients. ISME J 10, 97–108 (2016). https://doi.org/10.1038/ismej.2015.99
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/ismej.2015.99
This article is cited by
-
A multicentre study reveals dysbiosis in the microbial co-infection and antimicrobial resistance gene profile in the nasopharynx of COVID-19 patients
Scientific Reports (2023)
-
A Review on the Nasal Microbiome and Various Disease Conditions for Newer Approaches to Treatments
Indian Journal of Otolaryngology and Head & Neck Surgery (2023)
-
Periodontal disease as a model to study chronic inflammation in aging
GeroScience (2023)
-
Microbiota composition in the lower respiratory tract is associated with severity in patients with acute respiratory distress by influenza
Virology Journal (2023)
-
Endotracheal tube microbiome in hospitalized patients defined largely by hospital environment
Respiratory Research (2022)