Abstract
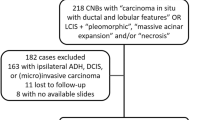
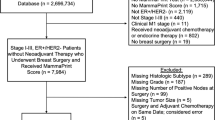
Standardized recommendations for the management of lobular neoplasia in core biopsy specimens are not established. The aim of our study was to define morphologic features of lobular neoplasia in core biopsies that predict the finding of ductal carcinoma in situ or invasive carcinoma in the subsequent excisional specimen. We reviewed 333 cases of atypical lobular hyperplasia or lobular carcinoma in situ without ductal carcinoma in situ or invasive carcinoma diagnosed in core biopsies from 1996 to 2006. Subsequent excision was performed in 41% (136/333) of cases, including atypical lobular hyperplasia (n=48), lobular carcinoma in situ (n=39), and lobular neoplasia associated with atypical ductal hyperplasia (n=49). Upgrades were identified in 2% (1/48) of atypical lobular hyperplasia, 23% (9/39) of lobular carcinoma in situ, and 27% (13/49) of lobular neoplasia associated with atypical ductal hyperplasia cases. When further analyzed, the upgraded cases of lobular carcinoma in situ were associated with radiologic–pathologic discordance in 6/9 cases and with nonclassic pathology (two lobular carcinoma in situ with necrosis and one pleomorphic lobular carcinoma in situ) in the remaining three cases. The frequency of upgrade was 11% (3/26) in classic lobular carcinoma in situ, and 46% (6/13) in nonclassic types (pleomorphic or with necrosis). After excluding cases with discordant imaging/pathology, there was a 5% upgrade in our excisional specimens. After excluding cases where the upgrade was associated with nonclassic morphology, the upgrade in our study was 1%. Our results suggest that atypical lobular hyperplasia and classic lobular carcinoma in situ with concordant radiology and pathology can be appropriately managed with clinical follow-up without surgery.
Similar content being viewed by others
Main
Lobular neoplasia refers to noninvasive proliferative lobular lesions and encompasses both atypical lobular hyperplasia and lobular carcinoma in situ. An alternative classification system proposed by Tavassoli1 classifies lobular neoplasia into three grades and uses the term lobular intraepithelial neoplasia. The management of lobular neoplasia is a subject of much controversy. Lobular neoplasia is a marker of increased risk for developing invasive breast cancer; this risk is multicentric and bilateral. In addition, studies of genomic alterations support a precursor role for some lobular neoplasia lesions with the capacity to directly progress to invasive carcinoma.2 How frequently lobular neoplasia progresses to invasive carcinoma is not known. The specific morphologic or molecular features of lobular neoplasia lesions that predict aggressive behavior are not established. Morphologically, lobular neoplasia is classically characterized by small, bland discohesive cells. Since their original description, variants of lobular carcinoma in situ have been recognized, aided by differential E-cadherin immunostaining.3, 4, 5
These variants include pleomorphic lobular carcinoma in situ characterized by discohesive pleomorphic cells with abundant cytoplasm.6 Rosen described ‘florid’ lobular carcinoma in situ characterized by ‘tumor cells that fill and expand the duct lumen’ that ‘may develop central necrosis and calcifications’.7 Sapino et al8 and Fadare et al9 also have defined in situ lesions with morphologic features of lobular neoplasia but with necrosis as lobular carcinoma in situ. Not only do both pleomorphic lobular carcinoma in situ and lobular carcinoma in situ with necrosis show different morphology, they can also exhibit a more aggressive biologic marker profile compared to classic lobular carcinoma in situ.6, 8, 9, 10, 11, 12 Microinvasive lobular carcinoma has been associated with pleomorphic lobular carcinoma in situ or lobular carcinoma in situ with necrosis,6, 8, 9, 13 although in routine practice, microinvasive carcinomas have also been observed in association with classic lobular carcinoma in situ. Lobular carcinoma in situ with nonclassic features has also been found to be more frequently associated with adjacent invasive carcinoma, especially invasive lobular carcinoma.14 High-grade ductal carcinoma in situ is known to show more aggressive behavior with frequent recurrence and progression to invasive carcinoma.15, 16, 17 Surprisingly, this basic tenet is not as accepted in lobular lesions as it is in ductal lesions.
Standardized recommendations for the management of lobular carcinoma in situ or atypical lobular hyperplasia diagnosed on core biopsy are not established. However, many patients currently undergo excision of the core biopsy site when lobular neoplasia is found. Previous studies have shown an upgrade to ductal carcinoma in situ or invasive carcinoma in 2% to over 40% of cases on subsequent excision of lobular neoplasia on core biopsy.18, 19, 20 Possible explanations for the wide range reported in upgrades include variables in technical aspects of imaging, the degree of pathologic–radiologic correlation, and variability in pathologically defining these lesions.
The aim of our study was to review the pathologic and radiologic features of patients with atypical lobular hyperplasia or lobular carcinoma in situ diagnosed by core biopsy at our institution from 1996 to 2006 and to define features that predict an upgrade to ductal carcinoma in situ or invasive carcinoma in subsequent excisions.
Materials and methods
Patients
Following the IRB approval, we retrieved 362 consecutive core biopsies performed at our institution from 1996 to 2006 with a diagnosis of lobular neoplasia, lobular intraepithelial neoplasia, atypical lobular hyperplasia, lobular carcinoma in situ, or carcinoma in situ with mixed features (mixed carcinoma in situ). Cases of lobular neoplasia associated with invasive carcinoma and/or ductal carcinoma in situ were excluded. Lobular neoplasia cases with atypical ductal hyperplasia were analyzed separately. Follow-up surgical excision was defined as a surgical procedure (eg needle-localization and excision or mastectomy) that was performed within 3 months after the diagnostic core biopsy. Available clinical data were compiled from our patient database and included examination of variables, such as a history of breast carcinoma, synchronous breast carcinoma, and subsequent development of carcinoma.
Imaging
Images were reviewed by dedicated breast radiologists. Abnormalities were grouped into the following categories: microcalcifications, microcalcifications with masses, masses alone, and architectural distortions. The Breast Imaging Reporting and Data System (BI-RADS) was used to stratify lesions according to different levels of suspicion for carcinoma (American College of Radiology, Reston, VA, USA, 4th edn, 2003). All lesions placed in BI-RADS category 4 (suspicious for malignancy) underwent image-guided needle core biopsy. Core biopsy was performed using stereotactic, sonographic, or magnetic resonance imaging (MRI) guidance. Information regarding number of cores and gauge used for core biopsy was recorded when available. Stereotactic biopsy was performed using a directional, vacuum-assisted biopsy device with 9- to 12-gauge needles. A specimen radiograph confirmed the presence of calcifications in each sample, and a clip was used to mark the biopsy site. Sonographically guided biopsy was performed using a spring-activated device with a 14-gauge needle or a vacuum-assisted device with 9- to 12-gauge needles. MRI-guided biopsy was performed using 1.5 T MR system (Siemens) using 9-gauge needles. Radiologic findings were routinely reviewed to evaluate concordance with histopathologic diagnoses.
Pathology
The core biopsy microscopic slides reviewed included all cases with subsequent excisions and additional cases without subsequent excision. On review, lobular neoplasia cases were reclassified as either atypical lobular hyperplasia or lobular carcinoma in situ. Lobular carcinoma in situ was further categorized into classic type, pleomorphic type, or lobular carcinoma in situ with necrosis. Several cases in our study had an original diagnosis of ‘mixed carcinoma in situ.’ In these cases and others where the diagnosis of lobular neoplasia was equivocal (cases with nonclassic morphology), an E-cadherin immunohistochemical stain was performed for definitive classification. On review, none of the cases in this study were categorized as mixed carcinoma in situ as none fit our definition of it. We used the following definitions based on previously described criteria of various authors:
Classic lobular carcinoma in situ. An uniform population of small discohesive cells with bland nuclei with mild to absent pleomorphism. The threshold for the distinction of lobular carcinoma in situ vs atypical lobular hyperplasia is involvement of at least 75% of the units of a lobule7 (Figure 1).
Atypical lobular hyperplasia and lobular carcinoma in situ, classic type, and variants. (a) Atypical lobular hyperplasia with neoplastic cells replacing normal glandular epithelium in acinar units effacing the lumens. The acini remain small, nondistended, and the borders of acinar units remain indistinct (H&E × 200). (b) Lobular carcinoma in situ, classic type, consists of a uniform population of discohesive cells with bland nuclei and intracytoplasmic mucin vacuoles (H&E × 200). (c) Lobular carcinoma in situ with necrosis, with ductules markedly distended by cells with classic morphologic features of lobular neoplasia and displaying central luminal necrosis (H&E × 200). (d) Lobular carcinoma in situ, pleomorphic type, with large discohesive cells with eccentrically placed large nuclei (>3 × the size of lymphocyte), moderate pleomorphism, and distinct small nucleoli (H&E × 400).
Atypical lobular hyperplasia. Same neoplastic cells as described for lobular carcinoma in situ replacing the normal glandular epithelium in acinar units and effacing the lumens. The acini are small, nondistended, and the borders of acinar units remain indistinct.7
Lobular carcinoma in situ with necrosis. Small, bland discohesive cells with marked distention of ductules/acini, and necrosis.7
Pleomorphic lobular carcinoma in situ. Pleomorphic population of medium to large cells, with nuclei at least three times the size of a lymphocyte, eccentrically placed, and with distinct nucleoli. Cells have moderate to abundant cytoplasm and at least focal areas of loss of cohesion. Necrosis and microcalcifications may be present.6
Mixed carcinoma in situ. Proliferation of neoplastic ductal and lobular cells within the same ductule/acini, with heterogeneous expression of E-cadherin.11
In cases with upgrades (ie cases containing invasive carcinoma and/or ductal carcinoma in situ in subsequent excisional specimens), the excisional specimens were also reviewed and the findings were categorized as malignant (ductal carcinoma in situ or invasive carcinoma) or benign (lobular carcinoma in situ, atypical lobular hyperplasia, atypical ductal hyperplasia, or any other benign histologic finding). An E-cadherin immunostain was performed in excisional specimens with an equivocal diagnosis on review.
Results
Patients
From 1996 to 2006, 362 cases of lobular neoplasia on core biopsy were identified in our database. Of those, 29 cases were omitted because (1) lobular neoplasia could not be identified in the core biopsy, (2) malignancy including ductal carcinoma in situ or invasive carcinoma was identified in the core biopsy, or (3) on account of subsequent mastectomy performed for synchronous ipsilateral carcinoma in another part of the breast.
The total number of cases was 333. Nine patients had two different biopsies so that the total number of patients was 324. Patients ranged in age from 29 to 87 years (median of 54 years). No difference in age was observed in patients with atypical lobular hyperplasia, lobular carcinoma in situ, or lobular neoplasia associated with atypical ductal hyperplasia.
Pure lobular neoplasia (atypical lobular hyperplasia and lobular carcinoma in situ cases without associated atypical ductal hyperplasia) was present in 277 cases, whereas atypical ductal hyperplasia was an associated finding in 56 cases. Overall, 41% (136/333) of cases had a subsequent lumpectomy or mastectomy (Table 1): atypical lobular hyperplasia+atypical ductal hyperplasia (n=33), lobular carcinoma in situ+atypical ductal hyperplasia (n=16), atypical lobular hyperplasia (n=48), lobular carcinoma in situ (n=39). Cases without subsequent excision consisted of atypical lobular hyperplasia (n=173), lobular carcinoma in situ (n=17), atypical lobular hyperplasia+atypical ductal hyperplasia (n=3), and lobular carcinoma in situ+atypical ductal hyperplasia (n=4). The majority of lobular neoplasia+atypical ductal hyperplasia cases were followed by surgical excision (49/56, 87.5%), whereas only 31% (87/277) of pure lobular neoplasia cases had an excision. 70% (39/56) of lobular carcinoma in situ cases and 22% (48/221) of atypical lobular hyperplasia cases had an excision. There was a significant trend to excise lobular carcinoma in situ rather than atypical lobular hyperplasia (χ2-test, P<0.001), reflecting a selection bias. There was also a significant trend to proceed to surgery if patients had a personal history of breast carcinoma (χ2-test, P=0.001).
Imaging
The predominant method of biopsy was stereotactic (n=287), followed by ultrasound guided (n=40) and MRI guided (n=4). Biopsies were performed for calcifications in 85% (282/333) and mass lesions in 15% (51/333) (Table 2). A total of 38% (107/282) of cases presenting with calcifications and 57% (29/51) of cases presenting with mass lesions were excised.
Biopsies were performed with 9- to 14-gauge needles (Table 3). The number of passes performed ranged from 4 to 24 with an average of seven cores per biopsy site in lobular neoplasia cases, 4–24 with an average of nine cores in lobular neoplasia+atypical ductal hyperplasia cases, and 4–18 with an average of nine cores in cases without subsequent excision. The amount of tissue removed by core biopsy was similar in cases with and in cases without subsequent excision.
Pathology
The archival cases included in the study were previously diagnosed by various pathologists, some of them using different nomenclatures and classifications (atypical lobular hyperplasia, lobular carcinoma in situ, lobular neoplasia, lobular intraepithelial neoplasia 1–3, mixed carcinoma in situ). We reviewed cases and reclassified them into lobular carcinoma in situ and atypical lobular hyperplasia for uniformity (Table 4). Lobular neoplasia cases with subsequent excision were classified on review as lobular carcinoma in situ (n=39) or atypical lobular hyperplasia (n=48). Lobular carcinoma in situ cases were classified as classic type (n=26), associated with necrosis (n=6), or pleomorphic type (n=7). Two cases of pleomorphic lobular carcinoma in situ also exhibited necrosis. Lobular neoplasia cases without subsequent excision consisted of atypical lobular hyperplasia (n=173) and lobular carcinoma in situ (n=17). All of the nonexcised lobular carcinoma in situ cases were classic type, except one that was associated with necrosis.
E-cadherin immunostaining was performed in cases with an original diagnosis of mixed carcinoma in situ for identification of the lobular carcinoma in situ component. In the lobular carcinoma in situ group, in two cases, the excisional specimens also had an original diagnosis of mixed carcinoma in situ. Histologic review and E-cadherin immunostaining confirmed a diagnosis of pure lobular carcinoma in situ in these two excisional specimens. In another case, the original diagnosis in the excisional specimen was ductal carcinoma in situ and lobular carcinoma in situ. Upon review and with the aid of E-cadherin immunostaining, a diagnosis of pure lobular carcinoma in situ was confirmed. In the atypical lobular hyperplasia group, one case originally diagnosed as lobular intraepithelial neoplasia 2 with atypical ductal hyperplasia was reclassified as pure atypical lobular hyperplasia as no atypical ductal hyperplasia was identified on review. An E-cadherin immunostain on the single mixed carcinoma in situ case confirmed the presence of lobular neoplastic cells only and was reclassified as atypical lobular hyperplasia.
Upgrades
When lobular neoplasia was associated with atypical ductal hyperplasia, 27% (13/49) of cases were upgraded on excision. Upgrades in this group were found in 30% (10/33) of atypical lobular hyperplasia+atypical ductal hyperplasia cases and in 19% (3/16) of lobular carcinoma in situ+atypical ductal hyperplasia cases. Table 5 shows the frequency of upgrades in pure lobular neoplasia (without atypical ductal hyperplasia). Upgrades were seen in 11% of lobular neoplasia cases overall (23% of lobular carcinoma in situ, 2% of atypical lobular hyperplasia). Lobular carcinoma in situ cases with an upgrade had discordant imaging and pathology in 6/9 cases: in three cases, a mass/architectural distortion/MRI enhancement could not be explained by a diagnosis of only lobular carcinoma in situ in core biopsy and in the remaining three cases, calcifications were not adequately sampled. The three upgraded lobular carcinoma in situ cases with concordant imaging and pathology included lobular carcinoma in situ with necrosis (n=2) and pleomorphic lobular carcinoma in situ (n=1) (Table 6).
In the atypical lobular hyperplasia group, four cases had an original diagnosis of mixed carcinoma in situ or ductal carcinoma in situ in the excisional specimen. Two of the mixed carcinoma in situ upgrades were reclassified as lobular carcinoma in situ based on histologic review and E-cadherin immunostains. One upgrade to ductal carcinoma in situ was reclassified as atypical ductal hyperplasia (a less than 0.2 cm focus of cytologic atypia not satisfying the criteria for ductal carcinoma in situ). In the last case, a biopsy was performed for a mass. The core biopsy diagnosis was atypical lobular hyperplasia with a fibroadenoma. The excision showed a 0.4 cm focus of cribriform-type ductal carcinoma in situ with low nuclear grade (unfortunately, the original slide with the ductal carcinoma in situ was not available for review and deeper levels did not show any ductal carcinoma in situ).
Overall, when pure lobular neoplasia was diagnosed on core biopsy with concordant radiology/pathology, 7% (3/39) of lobular carcinoma in situ, and 2% (1/48) of atypical lobular hyperplasia had an upgrade corresponding to an overall upgrade of 5% (4/87). Two of these four cases were lobular carcinoma in situ with necrosis and one was pleomorphic lobular carcinoma in situ. The fourth case was biopsied for a mass, with a diagnosis of atypical lobular hyperplasia associated with a fibroadenoma on core biopsy, and an apparent incidental finding of a 0.4 cm low nuclear grade ductal carcinoma in situ lesion on excision.
Compared to classic lobular carcinoma in situ with an 11% upgrade, upgrades were more common in lobular carcinoma in situ with necrosis (3/6, 50%) and pleomorphic lobular carcinoma in situ (3/7, 43%) (Table 5). The differences in frequency of upgrade between classic and nonclassic lobular carcinoma in situ were significant (χ2-test, P=0.016). All cases of classic lobular carcinoma in situ that were upgraded had radiologic–pathologic discordance (3/26, 11%).
Previous, Synchronous, or Subsequent Carcinoma
Cases associated with atypical ductal hyperplasia were excluded in this analysis. Synchronous carcinoma was defined as carcinoma (invasive carcinoma or ductal carcinoma in situ) diagnosed within 3 months before or after the diagnostic core biopsy with lobular neoplasia. All cases of synchronous ipsilateral carcinoma were in another quadrant of the breast and diagnosed previous to the core biopsy showing lobular neoplasia. Overall, 30% of patients had a history of either previous or synchronous ipsilateral or contralateral carcinoma. Of all patients, 20% had a history of contralateral carcinoma (previous or synchronous). In patients with lobular neoplasia with subsequent excisions, 38% (33/87) had a history of previous or synchronous carcinoma, vs 26% (50/190) of those without excisions (Table 7).
Only cases with a minimum of 6 months follow-up were included. The mean follow-up time was 32 months for lobular neoplasia cases with subsequent excision (n=51) and 49 months for lobular neoplasia cases without subsequent excision (n=148).
In the group that had a lobular neoplasia diagnosis on core biopsy followed by a subsequent excision, 20% (2/10) of patients with an upgrade to ductal carcinoma in situ on excision developed recurrent ductal carcinoma in situ/invasive carcinoma. Both patients were originally treated with lumpectomy and tamoxifen (without radiation). One patient developed recurrent ductal carcinoma in situ in 3 years, whereas the second patient, who had an upgrade to micropapillary ductal carcinoma in situ, developed small grade 1 invasive ductal carcinoma 4 years later. A total of 41 patients without an upgrade had follow-up information and none developed subsequent carcinoma.
Of 190 cases of lobular neoplasia in core biopsy without subsequent excision, 42 had no follow-up at this institution. Follow-up of the remaining 148 cases showed three (2%) subsequent ipsilateral carcinomas and one (0.7%) subsequent contralateral invasive carcinoma. One patient presented with new calcifications in an area adjacent to the core biopsy site 2 years after her lobular neoplasia diagnosis. Biopsy of this new lesion revealed tubular carcinoma. The second patient had a history of contralateral invasive carcinoma and developed invasive carcinoma 7 months after her core biopsy that showed lobular neoplasia. The invasive carcinoma manifested as a mass in the same breast at a different site from her lobular neoplasia. The third patient presented at follow-up with a palpable mass 6 months after her original core biopsy. She underwent an ultrasound guided core biopsy for a mass that demonstrated irregular hypoechogenicity and was again diagnosed with lobular carcinoma in situ. She subsequently had an excision that showed ductal carcinoma in situ in addition to lobular carcinoma in situ (Table 6, case 1). The last patient developed contralateral invasive ductal carcinoma 5 years after her lobular neoplasia diagnosis.
Discussion
The management of lobular neoplasia is an evolving topic. The classification of lobular neoplasia is equally problematic, complicated with increasing recognition of variants of lobular carcinoma in situ. In the past, without confirmatory E-cadherin staining, in situ lesions associated with necrosis were likely to be diagnosed as ductal carcinoma in situ. Although the prevalence of E-cadherin staining has confirmed the existence of lobular carcinoma in situ associated necrosis, some authors still classify E-cadherin negative in situ lesions with necrosis or with high-grade nuclei as ‘mixed’ in situ lesions with the rationale that they should be treated similarly to ductal carcinoma in situ.
Just as the histopathologic spectrum of lobular carcinoma in situ has broadened, the belief that lobular neoplasia has no detectable radiologic abnormalities has been challenged. Although lobular neoplasia is often an incidental finding on core biopsy, microcalcifications can be associated with classic lobular carcinoma in situ.21 Furthermore, lobular carcinoma in situ with necrosis can be associated with microcalcifications and can present mammographically like comedo-type ductal carcinoma in situ.1, 8
In contrast to many previous studies on lobular neoplasia, our study does not support routine excision for classic lobular carcinoma in situ or atypical lobular hyperplasia, but does support routine excision for nonclassic lobular carcinoma in situ, including pleomorphic lobular carcinoma in situ and lobular carcinoma in situ with necrosis. Concordance of radiology and pathology findings must be considered when making a decision to recommend excision. Numerous studies have examined the need for excision following a diagnosis of lobular neoplasia on core biopsy (Table 8). A common drawback of these studies, as well as our own, is the relatively small number of cases that can be identified within a single institution. The number of cases included in previously published studies (combining atypical lobular hyperplasia and lobular carcinoma in situ) varies from less than 10 up to 92 cases of lobular neoplasia followed by immediate excision.22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38 In comparison, our study includes a relatively high number of cases (87 cases of lobular neoplasia followed by immediate excision). Another limitation in our study and others is that it is retrospective and may suffer from selection bias regarding the patients that underwent excision. In our institution, during the time period studied, a greater percentage of lobular carcinoma in situ than atypical lobular hyperplasia cases was excised. Also, patients with a personal history of breast carcinoma were more likely to undergo subsequent excision.
Although most studies have found a significant associated risk of invasive carcinoma/ductal carcinoma in situ on excision after a diagnosis of lobular neoplasia in core biopsy, there is a high degree of variability. One of the reasons for the low rate of upgrade on excision of lobular neoplasia in core biopsy in our study compared with other studies may be the larger volume of tissue sampled by core biopsy at our institution vs other institutions, ie more complete sampling. Renshaw et al36 considered this to be one of the factors in the low incidence of upgrades found in their study. Another reason for the low upgrade incidence in our study may be careful radiologic–pathologic correlation. If cases with discordant imaging and pathology are included in our upgrade category, our upgrade percentage would be comparable to that published in other studies. The significance of radiologic–pathologic discordance has been demonstrated in recent studies by Menon33 and Nagi et al35 Similarly, discordance was the major cause for an upgrade in our study. Findings were considered discordant when (1) the radiologic finding was a mass and lobular neoplasia was the pathologic diagnosis on core biopsy or (2) the radiology showed suspicious calcifications that were not represented in the core biopsy specimen. After excluding discordant cases, our study showed a 5% incidence of invasive carcinoma/ductal carcinoma in situ in the excision. Concordant upgraded cases had nonclassic lobular carcinoma in situ morphology (lobular carcinoma in situ with necrosis or pleomorphic lobular carcinoma in situ) and in one remaining upgraded case of atypical lobular hyperplasia in core biopsy, the reason for the upgrade could not be identified.
In the group of patients with lobular neoplasia in core biopsy that were not followed by a subsequent excision (n=148), 2% of patients developed ipsilateral and 0.7% contralateral carcinoma (mean follow-up time=49 months). Although in our study a low percentage of patients developed subsequent carcinoma, all patients with biopsy proven lobular neoplasia have a well-recognized long-term risk of subsequent carcinoma in either breast and should be followed carefully.
In summary, our results do not support routine excisional biopsy as the standard of care for lobular neoplasia diagnosed on core biopsy. Surgical intervention is warranted in cases of radiologic–pathologic discordance and in cases of pleomorphic lobular carcinoma in situ or lobular carcinoma in situ with necrosis. Radiologic–pathologic correlation is crucial in determining the need for excision and requires effective communication between the pathologist, radiologist, and surgeon. Although at our hospital, management of atypical lobular hyperplasia and classic lobular carcinoma in situ can be accomplished by follow-up without surgery, other institutions need to evaluate their own data to establish similar guidelines. With an increased understanding of lobular neoplasia, a more definitive classification system of noninvasive lobular lesions is warranted and would be useful in establishing standardized guidelines in the management of these lesions.
References
Tavassoli FA . Pathology of the Breast, 2nd edn. McGraw-Hill Professional: New York, 1999, pp 373–400.
Mastracci TL, Boulos FI, Andrulis IL, et al. Genomics and premalignant breast lesions: clues to the development and progression of lobular breast cancer. Breast Cancer Res 2007;9:215.
Acs G, Lawton TJ, Rebbeck TR, et al. Differential expression of E-cadherin in lobular and ductal neoplasms of the breast and its biologic and diagnostic implications. Am J Clin Pathol 2001;115:85–98.
De Leeuw WJ, Berx G, Vos CB, et al. Simultaneous loss of E-cadherin and catenins in invasive lobular breast cancer and lobular carcinoma in situ. J Pathol 1997;183:404–411.
Vos CB, Cleton-Jansen AM, Berx G, et al. E-cadherin inactivation in lobular carcinoma in situ of the breast: an early event in tumorigenesis. Br J Cancer 1997;76:1131–1133.
Sneige N, Wang J, Baker BA, et al. Clinical, histopathologic, and biologic features of pleomorphic lobular (ductal-lobular) carcinoma in situ of the breast: a report of 24 cases. Mod Pathol 2002;15:1044–1050.
Rosen PP . Rosen's Breast Pathology, 2nd edn. Lippincott Williams & Wilkins: Philadelphia, 2001, pp 209–222.
Sapino A, Frigerio A, Peterse JL, et al. Mammographically detected in situ lobular carcinomas of the breast. Virchows Arch 2000;436:421–430.
Fadare O, Dadmanesh F, Alvarado-Cabrero I, et al. Lobular intraepithelial neoplasia [lobular carcinoma in situ] with comedo-type necrosis: a clinicopathologic study of 18 cases. Am J Surg Pathol 2006;30:1445–1453.
Lakhani SR . In-situ lobular neoplasia: time for an awakening. Lancet 2003;361:96.
Jacobs TW, Pliss N, Kouria G, et al. Carcinomas in situ of the breast with indeterminate features: role of E-cadherin staining in categorization. Am J Surg Pathol 2001;25:229–236.
Reis-Filho JS, Simpson PT, Jones C, et al. Pleomorphic lobular carcinoma of the breast: role of comprehensive molecular pathology in characterization of an entity. J Pathol 2005;207:1–13.
Nemoto T, Castillo N, Tsukada Y, et al., Bauer RL Lobular carcinoma in situ with microinvasion. J Surg Oncol 1998;67:41–46.
Bratthauer GL, Tavassoli FA . Lobular intraepithelial neoplasia: previously unexplored aspects assessed in 775 cases and their clinical implications. Virchows Arch 2002;440:134–138.
Lagios MD, Margolin FR, Westdahl PR, et al. Mammographically detected duct carcinoma in situ. Frequency of local recurrence following tylectomy and prognostic effect of nuclear grade on local recurrence. Cancer 1989;63:618–624.
Bijker N, Peterse JL, Duchateau L, et al. Risk factors for recurrence and metastasis after breast-conserving therapy for ductal carcinoma-in-situ: analysis of European Organization for Research and Treatment of Cancer Trial 10853. J Clin Oncol 2001;19:2263–2271.
Sanders ME, Schuyler PA, Dupont WD, et al. The natural history of low-grade ductal carcinoma in situ of the breast in women treated by biopsy only revealed over 30 years of long-term follow-up. Cancer 2005;103:2481–2484.
Cohen MA . Cancer upgrades at excisional biopsy after diagnosis of atypical lobular hyperplasia or lobular carcinoma in situ at core-needle biopsy: some reasons why. Radiology 2004;231:617–621.
Levine P, Simsir A, Cangiarella J . Management issues in breast lesions diagnosed by fine-needle aspiration and percutaneous core breast biopsy. Am J Clin Pathol 2006;125 (Suppl):S124–S134.
Bowman K, Munoz A, Mahvi DM, et al. Lobular neoplasia diagnosed at core biopsy does not mandate surgical excision. J Surg Res 2007;142:275–280.
Georgian-Smith D, Lawton TJ . Calcifications of lobular carcinoma in situ of the breast: radiologic–pathologic correlation. AJR Am J Roentgenol 2001;176:1255–1259.
Arpino G, Allred DC, Mohsin SK, et al. Lobular neoplasia on core-needle biopsy—clinical significance. Cancer 2004;101:242–250.
Berg WA, Mrose HE, Ioffe OB . Atypical lobular hyperplasia or lobular carcinoma in situ at core-needle breast biopsy. Radiology 2001;218:503–509.
Cangiarella J, Guth A, Axelrod D, et al. Is surgical excision necessary for the management of atypical lobular hyperplasia and lobular carcinoma in situ diagnosed on core needle biopsy?: a report of 38 cases and review of the literature. Arch Pathol Lab Med 2008;132:979–983.
Crisi GM, Mandavilli S, Cronin E, et al. Invasive mammary carcinoma after immediate and short-term follow-up for lobular neoplasia on core biopsy. Am J Surg Pathol 2003;27:325–333.
Elsheikh TM, Silverman JF . Follow-up surgical excision is indicated when breast core needle biopsies show atypical lobular hyperplasia or lobular carcinoma in situ: a correlative study of 33 patients with review of the literature. Am J Surg Pathol 2005;29:534–543.
Esserman LE, Lamea L, Tanev S, et al. Should the extent of lobular neoplasia on core biopsy influence the decision for excision? Breast J 2007;13:55–61.
Foster MC, Helvie MA, Gregory NE, et al. Lobular carcinoma in situ or atypical lobular hyperplasia at core-needle biopsy: is excisional biopsy necessary? Radiology 2004;231:813–819.
Karabakhtsian RG, Johnson R, Sumkin J, et al. The clinical significance of lobular neoplasia on breast core biopsy. Am J Surg Pathol 2007;31:717–723.
Liberman L, Sama M, Susnik B, et al. Lobular carcinoma in situ at percutaneous breast biopsy: surgical biopsy findings. AJR Am J Roentgenol 1999;173:291–299.
Mahoney MC, Robinson-Smith TM, Shaughnessy EA . Lobular neoplasia at 11-gauge vacuum-assisted stereotactic biopsy: correlation with surgical excisional biopsy and mammographic follow-up. AJR Am J Roentgenol 2006;187:949–954.
Margenthaler JA, Duke D, Monsees BS, et al. Correlation between core biopsy and excisional biopsy in breast high-risk lesions. Am J Surg 2006;192:534–537.
Menon S, Porter GJ, Evans AJ, et al. The significance of lobular neoplasia on needle core biopsy of the breast. Virchows Arch 2008;452:473–479.
Middleton LP, Grant S, Stephens T, et al. Lobular carcinoma in situ diagnosed by core needle biopsy: when should it be excised? Mod Pathol 2003;16:120–129.
Nagi CS, O'Donnell JE, Tismenetsky M, et al. Lobular neoplasia on core needle biopsy does not require excision. Cancer 2008;112:2152–2158.
Renshaw AA, Derhagopian RP, Martinez P, et al. Lobular neoplasia in breast core needle biopsy specimens is associated with a low risk of ductal carcinoma in situ or invasive carcinoma on subsequent excision. Am J Clin Pathol 2006;126:310–313.
Shin SJ, Rosen PP . Excisional biopsy should be performed if lobular carcinoma in situ is seen on needle core biopsy. Arch Pathol Lab Med 2002;126:697–701.
Yeh IT, Dimitrov D, Otto P, et al. Pathologic review of atypical hyperplasia identified by image-guided breast needle core biopsy. Correlation with excision specimen. Arch Pathol Lab Med 2003;127:49–54.
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclosure/conflict of interest
The authors have no conflict of interest to disclose.
Rights and permissions
About this article
Cite this article
Hwang, H., Barke, L., Mendelson, E. et al. Atypical lobular hyperplasia and classic lobular carcinoma in situ in core biopsy specimens: routine excision is not necessary. Mod Pathol 21, 1208–1216 (2008). https://doi.org/10.1038/modpathol.2008.134
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/modpathol.2008.134
Keywords
This article is cited by
-
Outcomes of classic lobular neoplasia diagnosed on breast core needle biopsy: a retrospective multi-center study
Virchows Archiv (2020)
-
Problematic issues in breast core needle biopsies
Modern Pathology (2019)
-
Role of one-pass breast lesion excision system in complete excision of high-risk breast lesions with atypia expressed as clusters of microcalcifications
European Radiology (2019)
-
Observation versus excision of lobular neoplasia on core needle biopsy of the breast
Breast Cancer Research and Treatment (2018)
-
Upgrade rates of high-risk breast lesions diagnosed on core needle biopsy: a single-institution experience and literature review
Modern Pathology (2016)