Abstract
Mucinous carcinoma is considered a distinct pathological entity. However, mucinous tumours can be divided into a least two groups: mucinous A (or paucicellular) and mucinous B (or hypercellular). Mucinous B cancers display histological features that significantly overlap with those of neuroendocrine carcinomas. We investigate using genome-wide oligonucleotide microarrays whether mucinous A, mucinous B and neuroendocrine carcinomas are entities distinct from histological grade- and molecular subtype-matched invasive ductal carcinomas of no special type. Mucinous A and B and five neuroendocrine carcinomas were of luminal A subtype, whereas one neuroendocrine tumour was of luminal B phenotype. When analysed in conjunction with grade- and molecular subtype-matched invasive ductal carcinomas, hierarchical clustering analysis showed that the majority of mucinous and neuroendocrine cancers formed a separate cluster. Significance analysis of microarrays identified 3155 genes differentially expressed between mucinous/ neuroendocrine carcinomas and grade- and molecular subtype-matched invasive ductal carcinomas (false discovery rate <0.85%), and revealed that genes associated with connective tissue/extracellular matrix were downregulated in mucinous/neuroendocrine cancers compared to invasive ductal carcinomas. When subjected to hierarchical clustering analysis separately, mucinous A cancers formed a discrete subgroup, whereas no separation was observed between mucinous B and neuroendocrine cancers. In fact, significance of microarray analysis showed no transcriptomic differences between mucinous B and neuroendocrine cancers, whereas mucinous A cancers displayed 89 up- and 26 downregulated genes when compared with mucinous B (false discovery rate <1.15%) and 368 up- and 48 downregulated genes when compared to neuroendocrine carcinomas (false discovery rate <1.0%). Our results provide circumstantial evidence to suggest that mucinous and neuroendocrine carcinomas are transcriptionally distinct from histological grade- and molecular subtype-matched invasive ductal carcinomas, and that luminal A breast cancers are a heterogeneous group of tumours. These findings support the contention that mucinous B and neuroendocrine carcinomas are part of a spectrum of lesions, whereas mucinous A is a discrete entity.
Similar content being viewed by others
Main
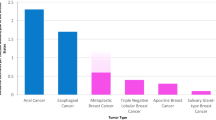
Pure mucinous carcinoma of the breast is a rare histological type, which accounts for approximately 2% of all invasive breast cancers and is characterised by clusters of tumour cells floating in large amounts of extracellular mucus.1 Neuroendocrine carcinoma represents 2–5% of invasive breast cancers and displays morphological features similar to those of neuroendocrine neoplasms of other organs, including the gut.1
Both mucinous and neuroendocrine carcinomas are recognised as distinct histological entities in the latest edition of the World Health Organisation (WHO) classification of breast neoplasms.1, 2 Capella et al,3 however, reported that pure mucinous carcinoma of the breast is not a single homogeneous entity, but comprises two main subtypes based on structural and cytological features: mucinous A (or paucicellular), which represents the ‘classical’ variant with large quantities of extracellular mucin, and mucinous B (or hypercellular) tumours, which contain less mucin and often show neuroendocrine differentiation and argyrophilia.3 Neuroendocrine carcinoma has also been suggested to not constitute a single clinicopathological entity, and several histological subtypes have been described including the cellular mucinous type,4, 5, 6, 7, 8, 9 which could also be classified as part of the spectrum of mucinous lesions (ie mucinous B). In addition, some have suggested that neuroendocrine differentiation may represent a pathway of neoplastic development in a range of breast cancers,10 although its biological and clinical behaviour remains a matter of contention.11, 12, 13, 14
The advent of expression profiling analysis has led to the development of a working model for a breast cancer molecular taxonomy comprising five molecular subtypes (ie luminal A, luminal B, basal-like, HER2+ and normal breast-like).15 This classification has shown to be of prognostic significance: the luminal A group of tumours have good outcome, whereas the luminal B, HER2+ and basal-like groups have a significantly worse prognosis.16, 17 Each molecular subtype, however, may constitute a heterogeneous group of cancers with distinct transcriptomic and genomic characteristics, clinical behaviour and drug response. This has been comprehensively shown for basal-like breast cancers,18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28 which are heterogeneous at the clinical, histological and molecular levels; however, only few studies addressed the diversity of other molecular subtypes.
Recent studies have shown that both mucinous and neuroendocrine tumours consistently pertain to the luminal molecular subtype;19, 29 however, the similarities and differences between these entities at the molecular level has thus far not been explored. The aims of this study were twofold: (i) to determine whether mucinous and neuroendocrine carcinomas are molecular entities distinct from histological grade- and molecular subtype-matched invasive ductal carcinomas of no special type; and (ii) to define whether the histological entities mucinous and neuroendocrine carcinomas are distinct at the transcriptomic level given the overlapping morphological features between mucinous A and mucinous B and between mucinous B and neuroendocrine breast cancers.
Materials and methods
Samples
Mucinous and neuroendocrine carcinomas
Consecutive samples of tumours classified as pure mucinous and neuroendocrine carcinomas were selected from the frozen tissue bank of The Netherlands Cancer Institute/Antoni van Leeuwenhoek hospital (NKI/AVL). Before and after cutting tissue sections for RNA extraction, a representative section was stained with haematoxylin and eosin and semi-quantitatively assessed for the percentage of tumour areas over the total sample area. Only samples containing ≥60% tumour cells were selected for downstream analysis. The transcriptomic profiles of the cases reported in this study were published in part in an earlier study.19 Gene expression data are publicly available at ArrayExpress (E-NCMF-3).
Control group (invasive ductal carcinomas of no special type)
We retrieved gene expression data from 102 invasive breast carcinomas that were part of an unrelated research project in our institute and were published in part by Kreike et al.18, 30 This gene-expression dataset differs only in tumour type analysis (ie predominantly invasive ductal carcinomas), but is similar with regards to experimental work-up. Of these 102 invasive breast carcinomas, 91 were invasive ductal carcinomas of no special type (henceforward ‘invasive ductal carcinomas’) and used as controls. Gene expression data are publicly available at ArrayExpress (E-NCMF-24). Detailed information on RNA extraction, amplification, labelling, hybridisation, scanning, microarray platform and analysis has been described earlier.18, 19
Histopathological Review and Immunohistochemistry
All samples of mucinous and neuroendocrine carcinomas were independently reviewed by two pathologists (FCG and JSR-F). Tumours were classified as of mucinous histological type according to the criteria outlined by Ellis et al1 and subclassified into mucinous A and mucinous B according to the criteria outlined by Capella et al.3 In brief, mucinous A tumours were paucicellular and 60–90% of the tumour areas were composed of extracellular mucin in which scattered neoplastic cells arranged in trabeculae, ribbons, festoons and rings were found. These neoplastic cells either lacked or only rarely showed intracellular mucin. Mucinous B tumours had a higher cellularity, a lower mucin content (30–75% of tumour area), and were preferentially characterised by neoplastic cells, often containing intracytoplasmic mucin, arranged in large, densely packed clumps and sheet-like structures.3 Neuroendocrine carcinomas were defined according to the WHO criteria. In brief, tumours displayed morphological features reminiscent of those of neuroendocrine carcinomas of gastrointestinal tract and lungs, including tumour cells arranged in solid nests and/ or trabeculae separated by delicate fibrovascular stroma. Rosettes, peripheral palisading and solid papillary formations were also considered features of neuroendocrine cancers. To establish an objective diagnosis, neuroendocrine carcinomas were diagnosed only when usual morphological features and expression of at least one neuroendocrine marker (eg chromogranin, synaptophysin or CD56) in at least 50% of cells were found.1 A perfect agreement between the two pathologists was reached in all but in one case (3683). The discrepancy was resolved by simultaneous analysis of representative histological sections of this tumour on a multi-headed microscope. The pathological characteristics of all cases are presented in Table 1.
Immunohistochemical analysis of mucinous and neuroendocrine carcinomas was performed as described earlier19 with antibodies raised against chromogranin (DAK-A3, 1:8000, Dako), synaptophysin (polyclonal, 1:400, Dako) and CD56 (123C3,31 1:800). For chromogranin and synaptophysin only cytoplasmic staining was considered as specific, for CD56 both membrane and cytoplasmic expression.
Out of the 91 invasive ductal carcinomas, none displayed overt features of mucinous or neuroendocrine differentiation in >10% of the tumour areas. Owing to the lack of material available from the invasive ductal carcinomas, immunohistochemical analysis of the neuroendocrine markers chromogranin, synaptophysin and CD56 was not performed on these control tumours.
Data Analysis
A subset of the 34 580 probes was selected, based on the following criteria: unambiguous mapping information for the probe, expression data available for at least 75% of all experiments and the expression level significantly different from the reference expression in at least 10% of experiments with a P-value of <0.01. These criteria reduced the total number of transcripts to 8398 significantly regulated transcripts.
To define whether a tumour pertained to basal-like, luminal A, luminal B, HER2 or normal breast-like molecular subgroup, we determined the Spearman's rank correlation of each case with the ‘Intrinsic/UNC’ class centroids by Hu et al.17 Almost all ‘intrinsic genes’ were identified (293 out of 306 unique genes).
After defining the molecular subtypes of the invasive ductal carcinomas, a subset of 24 of these tumours were selected to match with the mucinous A, mucinous B and neuroendocrine carcinomas based on histological grade and molecular subtype.
For unsupervised clustering analysis, we performed average-linkage hierarchical clustering of a centred correlation similarity matrix of the mucinous, neuroendocrine carcinomas and invasive ductal carcinomas (23 pertaining to the luminal A and 1 to the luminal B subtype) with 8398 filtered genes using the program Cluster,32 and results were visualised with TreeView. Genes and arrays were median centred.
To determine the significantly differentially expressed genes between mucinous A, mucinous B, neuroendocrine and grade- and molecular subtype-matched invasive ductal carcinomas, we used significance analysis of microarrays software33 performing 1000 permutations, as described earlier.20
Exact Hypergeometric Probability Analysis for Gene List Enrichment
Analysis for enrichment of differentially expressed genes identified by significance analysis of microarrays was performed using hypergeometric probability analysis, whereby the number of genes in common between two groups was identified and a representation factor (the number of overlapping genes divided by the expected number of overlapping genes drawn from two independent groups) was calculated. A representation factor >1 indicates more overlap than expected of two independent groups, whereas a representation factor <1 indicates less overlap than expected. The probability of finding an overlap of that number of genes was then calculated using the hypergeometric probability formula: C(D, x) * C(N–D, n–x)/C(N,n). (http://elegans.uky.edu/MA/progs/representation.stats.html).
Ingenuity Pathway Analysis
To determine pathways and networks that were significantly regulated in the gene expression data of mucinous, neuroendocrine tumours and grade- and molecular subtype-matched invasive ductal carcinomas, we performed pathway analysis using the Ingenuity Pathway Analysis program (http://www.ingenuity.com). The differentially expressed genes as identified by significance analysis of microarrays were mapped to networks available in the Ingenuity database and were ranked by score. The score indicates the likelihood of the genes in a network being found together because of random chance. Using a 99% confidence level, scores of ≥3 are significant.
Results
Mucinous and Neuroendocrine Carcinomas are Molecularly Distinct from Grade- and Molecular Subtype-Matched Invasive Ductal Carcinomas of no Special Type
Out of 24 cases, six were classified as neuroendocrine carcinomas and 18 as mucinous carcinomas according to the WHO criteria.1 Mucinous cancers were subclassified into A and B subgroups according to the criteria of Capella et al:3 10 were bona fide mucinous A and 8 were mucinous B; no case was classified as mixed (Figure 1; Table 1). All neuroendocrine carcinomas displayed features consistent with the diagnosis of solid neuroendocrine carcinoma of the breast1 and expressed at least one marker of neuroendocrine differentiation in >50% of cells as evaluated by immunohistochemistry (Figure 2; Table 1), whereas only 3 of the 10 mucinous A (30%) and 2 of the 8 mucinous B tumours (25%) expressed neuroendocrine markers in >10% of cells (Table 1). To define the basal-like, luminal A, luminal B, HER2 and normal breast-like molecular subtype class, we determined the correlation between the expression profile of each tumour with the ‘Intrinsic/UNC’ class centroids described by Hu et al.17 Mucinous cancers were homogeneous and consistently displayed a luminal A expression profile; neuroendocrine carcinomas were assigned to the luminal A (n=5) or B (n=1) molecular subtypes (Table 1).
We next assessed whether mucinous and neuroendocrine carcinomas would constitute distinct special types and discrete entities from invasive ductal carcinomas not only at the histological but also at the molecular level. For comparison, we selected from a control group of 102 invasive breast carcinomas a series of 24 invasive ductal carcinomas that were histological grade- and molecular subtype-matched with the cohort of mucinous and neuroendocrine cancers. This series consisted of 23 luminal A and one luminal B tumours, of which 14, eight and two were of grades 1, 2 or 3, respectively (Supplementary Table 1). Unsupervised hierarchical clustering using 8398 significantly regulated transcripts revealed that, with the exception of three mucinous A tumours, mucinous and neuroendocrine carcinomas formed a separate group. In fact, the mucinous/neuroendocrine cluster was significantly enriched for these tumours (Fisher's exact test P<10−9; Figure 3). We further observed that in the mucinous/neuroendocrine cluster the mucinous B cancers were intermingled with neuroendocrine carcinomas, whereas mucinous A tumours clustered significantly more tightly together (Fisher's exact test P<10−6). These results provide evidence to suggest that mucinous and neuroendocrine tumours are distinct transcriptomic entities from grade- and molecular-subtype-matched invasive ductal carcinomas.
Unsupervised hierarchical clustering of mucinous, neuroendocrine and grade- and molecular subtype-matched invasive ductal carcinomas. Average-linkage clustering of 10 mucinous A, 8 mucinous B, 6 neuroendocrine cancers and 24 invasive ductal carcinomas of no special type (IDC-NST) using 8398 significantly regulated transcripts.
Given the separation observed between mucinous/neuroendocrine and histological grade- and molecular subtype-matched invasive ductal carcinomas in the hierarchical clustering, we sought to define their transcriptional differences. Supervised analysis using significance of microarray analysis revealed 3155 transcripts differentially expressed between mucinous/neuroendocrine tumours vs grade- and molecular subtype-matched invasive ductal carcinomas (1582 and 1573 transcripts were preferentially expressed in mucinous/neuroendocrine cancers and grade- and molecular subtype-matched invasive ductal carcinomas, respectively; false discovery rate<0.85%; Supplementary Table 2). Of note, extracellular matrix genes (eg, collagens, matrix metalloproteinases, insulin-like growth factor-binding proteins, laminins), ERBB2 and high molecular weight cytokeratins KRT5 and KRT14 were downregulated, whereas ESR1 and the oestrogen receptor-α (ER)-regulated genes BCL2, ERBB4 and TFF3, the luminal KRT18 but also CDKN1A (p21) were upregulated in mucinous/neuroendocrine tumours compared with grade- and molecular subtype-matched invasive ductal carcinomas. These differences were further explored by Ingenuity Pathway Analysis of the 3155 differentially regulated transcripts identified by significance of microarray analysis, which revealed that extracellular matrix genes of the ‘Connective Tissue Disorders, Dermatological Diseases and Conditions, Genetic Disorder’ (score 36) and ‘Cell Death, Protein Degradation, Cellular Function and Maintenance’ (score 29) networks were predominantly downregulated in mucinous/neuroendocrine carcinomas compared to grade- and molecular subtype-matched invasive ductal carcinomas (Supplementary Table 3; Supplementary Figure 1).
To define the molecular pathways differentially regulated between mucinous, neuroendocrine cancers and grade- and molecular subtype-matched invasive ductal carcinomas, we analysed mucinous A, mucinous B and neuroendocrine tumours separately. Significance of microarray analysis revealed 651 transcripts differentially expressed between mucinous A (n=10) and grade- and molecular subtype-matched invasive ductal carcinomas (n=10) (361 up- and 290 downregulated in mucinous A cancers; false discovery rate <0.85%), 597 transcripts between mucinous B (n=8) and grade- and molecular subtype-matched invasive ductal carcinomas (n=8) (179 up- and 418 downregulated in mucinous B carcinomas; false discovery rate <0.85%) and 337 transcripts between neuroendocrine (n=6) and grade- and molecular subtype-matched invasive ductal carcinomas (n=6) (11 and 326 transcripts preferentially expressed in neuroendocrine and in grade- and molecular subtype-matched invasive ductal carcinomas, respectively; false discovery rate <0.85%) (Supplementary Table 4).
Ingenuity Pathway Analysis of the 651 differentially expressed transcripts identified by significance of microarray analysis revealed four ‘Connective Tissue’-related networks (scores 39, 37, 34 and 28, respectively) among the 10 most significant networks, in which extracellular matrix genes (eg, collagens, laminins, matrix metalloproteinases) were predominantly downregulated in mucinous A tumours compared with grade- and molecular subtype-matched invasive ductal carcinomas of luminal A phenotype (Figure 4a; Supplementary Figure 2a; Supplementary Table 5). Of note, genes of the FGF family (eg, FGF10, FGF13, FGF14) were found to be upregulated in mucinous A cancers compared with grade-matched invasive ductal carcinomas of luminal A subtype (Figure 4a; Supplementary Table 4), and the differentially expressed transcripts between mucinous A and grade- and molecular subtype-matched invasive ductal carcinomas were significantly enriched for genes of the ‘FGF Signalling’ canonical pathway (P=0.0108; Supplementary Table 5). Furthermore, the ‘Endoplasmic Reticulum Stress Response’ canonical pathway was upregulated in mucinous A compared with grade- and molecular subtype-matched invasive ductal carcinomas (P=0.0281; Supplementary Figure 2b).
Ingenuity Pathway Analysis. Extracellular matrix genes of the ‘Connective Tissue Development and Function, Skeletal and Muscular System Development and Function, Tissue Development’ network (score 37) are downregulated in mucinous A vs histological grade- and molecular subtype-matched invasive ductal carcinomas (a), of the ‘Cell Morphology, Connective Tissue Development and Function, Tissue Development’ network (score 44) are downregulated in mucinous B vs histological grade- and molecular subtype-matched invasive ductal carcinomas (b), of the ‘Cancer, Reproductive System Disease, Ophthalmic Disease’ (score 43) are downregulated in neuroendocrine vs grade- and molecular subtype-matched invasive ductal carcinomas (c). Green: downregulation, red: upregulation. IDCs-NST: invasive ductal carcinomas of no special type.
Ingenuity Pathway Analysis revealed that, like in mucinous A carcinomas, downregulation of extracellular matrix genes (eg, collagens, fibulins and matrix metalloproteinases) pertaining to networks involved in ‘Cell Morphology, Connective Tissue Development and Function, Tissue Development’, ‘Post-Translational Modification, Cancer, Reproductive System Disease’ and ‘Cellular Movement, Skeletal and Muscular Disorders, Tissue Development’ (scores 44, 43 and 37, respectively) was observed in mucinous B compared with grade-matched invasive ductal carcinomas of luminal A phenotype (Figure 4b; Supplementary Figure 3a; Supplementary Tables 4 and 5). Furthermore, the high molecular weight cytokeratins KRT5 and KRT14 were downregulated, whereas ESR1, BCL2, ERBB4 and FOXA1 were found to be upregulated in mucinous B vs grade- and molecular subtype-matched invasive ductal carcinomas (Supplementary Table 4). Ingenuity Pathway Analysis of genes differentially expressed between mucinous B vs grade-matched invasive ductal carcinomas of luminal A phenotype revealed an enrichment for genes of the ‘p53 Signalling’ (P=0.0042) and of the ‘Wnt/β-catenin Signalling’ canonical pathways (P=0.0299), the latter being downregulated in mucinous B tumours compared with invasive ductal carcinomas of the same histological grade and molecular subtype (Supplementary Table 5; Supplementary Figure 3b).
Similar to mucinous A and B tumours, the functional mapping of the 337 significantly differentially regulated transcripts between neuroendocrine and grade- and molecular subtype-matched invasive ductal carcinomas to the Ingenuity database identified networks of genes having a role in ‘Cancer, Reproductive System Disease, Ophthalmic Disease’ (score 43) and ‘Cell-To-Cell Signalling and Interaction, Connective Tissue Development and Function, Post-Translational Modification’ (score 42), including matrix metalloproteinases, collagens, fibulins and ITGB1, to be downregulated in neuroendocrine carcinomas, as was the ‘IGF-1 Signalling’ canonical pathway (P=0.0071; Figure 4c; Supplementary Figure 4; Supplementary Table 5).
As mucinous B and neuroendocrine carcinomas have significantly overlapping morphological features and were intermingled in the hierarchical clustering analysis, we defined the transcriptomic differences of these two subtypes and histological grade- and molecular subtype-matched invasive ductal carcinomas. Significance of microarray analysis revealed 2315 transcripts differentially expressed (1020 up- and 1295 downregulated transcripts in mucinous B/neuroendocrine cancers at a false discovery rate <0.90%) between mucinous B/neuroendocrine cancers (n=14) and grade- and molecular subtype-matched invasive ductal carcinomas (n=14). (Supplementary Table 4). Of note, transcriptional regulators (eg, MED23, GMEB1, TCF25, EEF1A2), ESR1 and the ER-regulated genes FOXA1, XBP1, ERBB4 and BCL2 and ‘Lipid Metabolism, Molecular Transport, Small Molecule Biochemistry’ gene network (score 31) were upregulated in mucinous B/neuroendocrine carcinomas vs grade- and molecular subtype-matched invasive ductal carcinomas (Supplementary Figure 5a; Supplementary Table 5). In addition, extracellular matrix genes (eg, collagens, laminins, PLAU, VCAN, SERPINH1) as seen in the ‘Ophthalmic Disease, Cardiovascular Disease, Genetic Disorder’ network (score 36) were downregulated in mucinous B/neuroendocrine carcinomas compared with grade- and molecular subtype-matched invasive ductal carcinomas (Supplementary Figure 5b).
Taken together, our results provide evidence to suggest that mucinous A, mucinous B and neuroendocrine carcinomas are transcriptionally distinct from histological grade- and molecular subtype-matched invasive ductal carcinomas of no special type. Furthermore, discrete molecular pathways/networks were found to be activated in mucinous and neuroendocrine cancers compared with grade- and molecular subtype-matched invasive ductal carcinomas. Most strikingly, mucinous and neuroendocrine tumours displayed downregulation of extracellular matrix and connective tissue-associated genes compared with grade- and molecular subtype-matched invasive ductal carcinomas.
Mucinous A Cancers are Distinct Entities, Whereas Mucinous B and Neuroendocrine Carcinomas Share Similar Transcriptomic Profiles
Given that (i) mucinous A, mucinous B and neuroendocrine carcinomas formed a separate cluster when subjected to hierarchical clustering analysis with grade- and molecular subtype-matched invasive ductal carcinomas and that (ii) there is a significant overlap between the morphological features of mucinous B and neuroendocrine carcinomas, we sought to determine whether these histological entities would constitute distinct entities at the transcriptomic level.
Unsupervised hierarchical clustering analysis of mucinous A, mucinous B and neuroendocrine carcinomas revealed that all mucinous A tumours formed a discrete cluster, whereas mucinous B and neuroendocrine carcinomas were intermingled in a separate cluster (Figure 5). These results provide evidence to suggest that mucinous A is a molecular entity distinct from mucinous B and neuroendocrine carcinomas, whereas mucinous B and neuroendocrine carcinomas have a highly similar transcriptome.
To further define the differences between mucinous A, mucinous B and neuroendocrine carcinomas, we performed significance of microarray analysis using the 8398 significantly regulated transcripts. This analysis revealed 115 transcripts differentially expressed between mucinous A and mucinous B carcinomas (89 up- and 26 transcripts downregulated in mucinous A cancers; false discovery rate <1.15%; Supplementary Table 6). Compared with mucinous B carcinomas, mucinous A cancers were found to upregulate cell-junction genes (eg, WTIP, GJA1), cytokeratins (eg, KRT7, KRT23) and VIM, ITGB5 and VEGFC, but downregulate genes having a role in lipid synthesis/transport (eg, AGPAT5, APOL6), as well as ERBB4 and FOXA1 (Supplementary Table 6). The upregulation of molecular transporters (eg, SLC12A6), cell-junction genes as well as MET and ITGB5 was also seen in the top network ‘Carbohydrate Metabolism, Lipid Metabolism, Molecular Transport (score 39; Supplementary Table 7; Supplementary Figure 6a).
The 416 differentially expressed transcripts identified between mucinous A and neuroendocrine tumours using significance of microarray analysis (false discovery rate <1.00%; Supplementary Table 6) showed great overlap with the 115 genes discriminating mucinous A and mucinous B cancers (73 genes overlap; representation factor: 12.8; P<10−68). For instance, downregulation of ERBB4 or FOXA1, and upregulation of VIM, FOS or IL4R were found in both comparisons. These findings show that the similarities in the transcriptomic differences between mucinous A and mucinous B and between mucinous A and neuroendocrine carcinomas cannot be attributed by chance, providing another line of indirect evidence to suggest that mucinous B and neuroendocrine carcinomas are closely related at the molecular level.
Ingenuity Pathway Analysis of 416 differentially expressed transcripts identified between mucinous A and neuroendocrine tumours revealed ‘Cell-to-Cell Signalling and Interaction, Tissue Development, Cell Morphology’ (score 46) and ‘Cell Morphology, Cellular Assembly and Organization, Cellular Movement’ (score 41) networks of integrins (eg, ITGA5, ITGB2, ITGB5), calcium-binding proteins (eg, S100A8, S100A11) and actin cytoskeleton/actin-binding genes (eg, DIAPH2, ANXA1, ACTN1, AFAP, RDX, TMSB4X, VCL), which were upregulated in mucinous A compared with neuroendocrine cancers (Supplementary Figure 6b and 6c; Supplementary Tables 6 and 7). These differentially expressed transcripts were also found to be enriched for ‘Macropinocytosis’ canonical pathway genes (P=0.002), a clathrin-independent form of endocytosis, and ‘IGF-1 Signalling’ genes (P=0.00189) (Supplementary Figure 7; Supplementary Table 7), which were predominantly upregulated in mucinous A compared with neuroendocrine cancers. Of note, the genes identified of this ‘IGF-1 Signalling’ pathway were different from the ones of the same pathway differentially expressed between neuroendocrine cancers and invasive ductal carcinomas (Supplementary Figure 4).
Remarkably, significance of microarray analysis of mucinous B and neuroendocrine carcinomas showed no transcriptomic differences between these two breast cancer types as no differentially expressed genes could be assigned (false discovery rate <1–<52%; Supplementary Table 6). These results were further confirmed by maxT test,34 which failed to show any differentially expressed transcripts (data not shown).
Given the striking similarity between mucinous B and neuroendocrine tumours at the molecular level, we sought to define the transcriptomic differences between these two histological types and mucinous A tumours. Ingenuity Pathway Analysis of the 663 differentially expressed genes identified by significance of microarray analysis (581 up- and 82 transcripts downregulated in mucinous A cancers, respectively; false discovery rate <1.05%; Supplementary Table 6) revealed that ‘Cell Morphology, Skeletal and Muscular System Development and Function, Cancer’ (score 56) and ‘Ophthalmic Disease, Cancer, Cell Signalling’ (score 48) networks of extracellular matrix genes (eg, collagens, fibulins) are upregulated in mucinous A compared to mucinous B and neuroendocrine tumours, as are TGFB1 and KRT7 (Supplementary Table 7; Supplementary Figure 8). Furthermore, the ‘Integrin Signalling’ canonical pathway (P=0.00018) was found to be upregulated in mucinous A vs mucinous B and neuroendocrine carcinomas (Supplementary Figure 9).
Taken together, our results provide evidence to suggest that the histological entity of mucinous carcinoma comprises two distinct molecular entities, mucinous A and mucinous B cancers, and that mucinous B and neuroendocrine carcinomas are strikingly similar at the transcriptomic level.
Discussion
Here, we show that by microarray-based gene expression analysis the histological special types mucinous and neuroendocrine carcinomas of the breast are entities distinct from histological grade- and molecular subtype-matched invasive ductal carcinomas of no special type, and that different molecular pathways are activated in these tumours. Furthermore, our study shows that the histological variants of mucinous carcinoma, mucinous A and mucinous B, harbour significantly different gene expression profiles, whereas mucinous B and neuroendocrine carcinomas are strikingly similar at the transcriptomic level.
Invasive ductal carcinomas were not tested for the immunohistochemical expression of neuroendocrine markers. It should be noted, however, that although 2–18% of consecutive breast cancers may express at least focally neuroendocrine markers,1, 12 in this study neuroendocrine carcinomas formed a separate group by genome-wide transcriptional analysis and harboured 337 genes at a false discovery rate <0.85% differentially expressed when compared with grade- and molecular subtype-matched invasive ductal carcinomas. One could hypothesise that if the control group comprised only invasive ductal carcinomas devoid of any expression of neuroendocrine markers, even more pronounced differences would have been identified.
The expression of genes having a role in the extracellular matrix and connective tissue was significantly decreased in mucinous A, mucinous B and neuroendocrine cancers compared to grade- and molecular subtype-matched invasive ductal carcinomas. This is not surprising, given that the stroma of pure mucinous carcinomas is predominantly composed of pools of mucin with scattered stromal cells (ie fibroblasts, endothelial and inflammatory cells), and the stroma of neuroendocrine carcinomas is scant, given that these tumours are predominantly composed of solid masses or nests and islands of cells with few intervening stromal cells, as opposed to luminal types of invasive ductal carcinomas.1, 35 Another potential mechanism for downregulation of extracellular matrix genes in mucinous B cancers stems from the significant downregulation of the Wnt/β-catenin canonical signalling pathway. This pathway not only regulates cell fate decisions, proliferation, morphology and migration,36 but also extracellular matrix components and cell adhesion.37 Our results suggest that owing to the distinctive histological characteristics of not only cancer cells but also stroma, mucinous and neuroendocrine cancers may have distinct interactions with the microenvironment or receive distinct microenvironmental cues compared with those of invasive ductal carcinomas.
Compared to grade-matched luminal cancers, mucinous A and B, and neuroendocrine carcinomas displayed higher levels of ESR1 expression, and more overt characteristics of luminal differentiation were observed in mucinous B and neuroendocrine carcinomas. In fact, these tumours not only displayed significantly higher levels of ESR1 expression, the downstream target of ER-α activation BCL2, the ER-pathway partners FOXA1, XBP1 and ERBB4,38, 39 but also significant upregulation of a network of ER-regulated lipid metabolism genes and the luminal cytokeratin KRT18 compared to grade- and molecular subtype-matched invasive ductal carcinomas. Mucinous A, on the other hand, when compared with mucinous B and neuroendocrine carcinomas displayed decreased expression of AKT1, FOXA1 and ERBB4. Furthermore, mucinous A and B, and neuroendocrine cancers showed significantly lower levels of ‘basal’ cytokeratins KRT5 and KRT14 compared with grade- and molecular subtype-matched invasive ductal carcinomas, which is supported by earlier work showing that CK5 and CK14 were rarely expressed in carcinomas with neuroendocrine differentiation.40 Our results provide evidence to suggest that there is a spectrum of luminal differentiation even within luminal A cancers, and that mucinous B and neuroendocrine tumours may have a more overt luminal phenotype and are more homogenous at the transcriptomic level than grade- and molecular subtype-matched invasive ductal carcinomas.
In mucinous A tumours, we observed upregulation of ESR1 but also of members of FGF family (eg, FGF10, FGF14, FGF18) compared to grade-matched invasive ductal carcinomas of luminal A phenotype, and an enrichment for genes of the ‘FGF-Signalling’ canonical pathway. Single nucleotide polymorphisms of FGFR2 have been shown repeatedly to be associated with increased risk of breast cancer, especially in ER-positive disease.41, 42, 43 Given that mucinous A cancers may have a consistent activation of the FGF signalling pathway, our results warrant further testing of FGF/ FGFR inhibitors in preclinical models of mucinous cancers. Ingenuity Pathway Analysis further showed upregulation of the canonical endoplasmic reticulum stress pathway. The accumulation of misfolded/unfolded proteins in the endoplasmic reticulum induced by stimuli such as hypoxia or low pH has been shown to induce a stress response (ie ‘unfolded protein response’) and the activation of specific signalling pathways, such as the mitogen-activated protein kinases (MAPKs).44, 45, 46 Epithelial mucins secreted by breast cancer cells of mucinous tumours have been reported to be acidic,47, 48 and we observed an upregulation of heat shock protein genes and MAP3K5 in mucinous A cancers compared to grade-matched invasive ductal carcinomas of luminal A subtype. The transcriptional activation of protein degradation and folding genes has been described to serve as a mechanism in cancer cells in hypoxic environments to re-establish homeostasis and normal endoplasmic reticulum function and to escape apoptosis induction.49 These endoplasmic reticulum stress response genes are currently under investigation as potential drug targets.49 Our results provide a rationale for testing agents targeting endoplasmic reticulum stress response genes in preclinical models of mucinous A breast cancers.
We not only show here that mucinous and neuroendocrine carcinomas of the breast are molecularly distinct from histological grade- and molecular subtype-matched invasive ductal carcinomas, but we also provide several lines of evidence to propose that mucinous A and mucinous B cancers as described by Capella et al may be discrete at the transcriptomic level,3 whereas mucinous B and neuroendocrine carcinomas may represent a single ‘molecular entity’ or a spectrum of closely related molecular entities. First, hierarchical clustering analysis revealed that mucinous A tumours form a distinct cluster from mucinous B and neuroendocrine cancers. Second, using significance of microarray analysis, mucinous A and mucinous B tumours showed differential expression of ER-regulated genes (ie ERBB4, FOXA1) and genes of the oestrogen-regulated lipid synthesis/transport, which indicates a reduced ER-α pathway activation in mucinous A vs mucinous B cancers. Third, we observed a significant overlap in genes differentially expressed between mucinous A vs mucinous B tumours and mucinous A vs neuroendocrine tumours. And finally, significance of microarray analysis revealed no transcriptomic differences between mucinous B and neuroendocrine carcinomas.
In the seminal study by Capella et al,3 a subgroup of mucinous cancers (17%) displayed mixed features of mucinous A and B cancers. Although we have not encountered any of these tumours in this study, one could speculate that some of these tumours would harbour transcriptomic features of mucinous B/neuroendocrine cancers, whereas others would be more similar to mucinous A tumours. Alternatively, the allocation of these tumours to transcriptomic mucinous A or mucinous B/neuroendocrine would potentially depend on the percentage of each component in mucinous A/B tumours. Finally, mucinous A/B cancers may constitute yet another molecular subgroup. Further transcriptomic analyses of mixed mucinous cancers are warranted.
The overlapping histological features of mucinous A and mucinous B as well as mucinous B and neuroendocrine carcinomas are corroborated and expanded by our transcriptomic findings. Although we defined differences in gene expression between mucinous A, mucinous B and neuroendocrine cancers, these tumours were more similar to each other than to invasive ductal carcinomas of the same histological grade and molecular subtype, which provides support to the contention that mucinous and neuroendocrine carcinomas may constitute a spectrum of differentiation. The transcriptional homogeneity of the mucinous and neuroendocrine cancers compared to invasive ductal carcinomas together with the finding that mucinous cancers have fewer genomic alterations than invasive ductal carcinomas50 suggest that the study of special types of breast cancer may be an effective way of reducing the complexity of breast cancer and expedite the identification of biological drivers and potential therapeutic targets for subgroups of breast cancer patients.2 Our transcriptome analysis of mucinous A, mucinous B and neuroendocrine carcinomas showed that not only basal-like breast cancers are a heterogeneous group of tumours, but also that the molecular subtype group of luminal A breast cancers encompasses a diverse and heterogeneous group of tumours in terms of gene expression, prognosis,51 biology and morphology.
References
Ellis P, Schnitt SJ, Sastre-Garau X, et al. Invasive breast carcinoma. In: Tavassoli FA, Devilee P (eds). WHO Classification of Tumours. Pathology and Genetics of Tumours of the Breast and Female Genital Organs. IARC Press: Lyon, 2003, pp 9–47.
Reis-Filho JS, Lakhani SR . Breast cancer special types: why bother? J Pathol 2008;216:394–398.
Capella C, Eusebi V, Mann B, et al. Endocrine differentiation in mucoid carcinoma of the breast. Histopathology 1980;4:613–630.
Papotti M, Macrì L, Finzi G, et al. Neuroendocrine differentiation in carcinomas of the breast: a study of 51 cases. Semin Diagn Pathol 1989;6:174–188.
Maluf HM, Zukerberg LR, Dickersin GR, et al. Spindle-cell argyrophilic mucin-producing carcinoma of the breast. Histological, ultrastructural, and immunohistochemical studies of two cases. Am J Surg Pathol 1991;15:677–686.
Papotti M, Gherardi G, Eusebi V, et al. Primary oat cell (neuroendocrine) carcinoma of the breast. Report of four cases. Virchows Arch A Pathol Anat Histopathol 1992;420:103–108.
Sapino A, Righi L, Cassoni P, et al. Expression of the neuroendocrine phenotype in carcinomas of the breast. Semin Diagn Pathol 2000;17:127–137.
Zekioglu O, Erhan Y, i° M, et al. Neuroendocrine differentiated carcinomas of the breast: a distinct entity. Breast 2003;12:251–257.
Nassar H, Qureshi H, Volkanadsay N, et al. Clinicopathologic analysis of solid papillary carcinoma of the breast and associated invasive carcinomas. Am J Surg Pathol 2006;30:501–507.
Maluf HM, Koerner FC . Carcinomas of the breast with endocrine differentiation: a review. Virchows Arch 1994;425:449–457.
Sapino A, Papotti M, Righi L, et al. Clinical significance of neuroendocrine carcinoma of the breast. Ann Oncol 2001;12:S115–S117.
Miremadi A, Pinder SE, Lee AH, et al. Neuroendocrine differentiation and prognosis in breast adenocarcinoma. Histopathology 2002;40:215–222.
Makretsov N, Gilks CB, Coldman AJ, et al. Tissue microarray analysis of neuroendocrine differentiation and its prognostic significance in breast cancer. Hum Pathol 2003;34:1001–1008.
Louwman MW, Vriezen M, van Beek MW, et al. Uncommon breast tumors in perspective: incidence, treatment and survival in the Netherlands. Int J Cancer 2007;121:127–135.
Perou CM, Sorlie T, Eisen MB, et al. Molecular portraits of human breast tumours. Nature 2000;406:747–752.
Sorlie T, Tibshirani R, Parker J, et al. Repeated observation of breast tumor subtypes in independent gene expression data sets. Proc Natl Acad Sci USA 2003;100:8418–8423.
Hu Z, Fan C, Oh D, et al. The molecular portraits of breast tumors are conserved across microarray platforms. BMC Genomics 2006;7:96.
Kreike B, van Kouwenhove M, Horlings H, et al. Gene expression profiling and histopathological characterization of triple negative/basal-like breast carcinomas. Breast Cancer Res 2007;9:R65.
Weigelt B, Horlings HM, Kreike B, et al. Refinement of breast cancer classification by molecular characterization of histological special types. J Pathol 2008;216:141–150.
Weigelt B, Kreike B, Reis-Filho JS . Metaplastic breast carcinomas are basal-like breast cancers: a genomic profiling analysis. Breast Cancer Res Treat 2008, e-pub ahead of print; doi:10.1007/s10549-008-0197-9.
Lien HC, Hsiao YH, Lin YS, et al. Molecular signatures of metaplastic carcinoma of the breast by large-scale transcriptional profiling: identification of genes potentially related to epithelial-mesenchymal transition. Oncogene 2007;26:7859–7871.
Bertucci F, Finetti P, Cervera N, et al. Gene expression profiling shows medullary breast cancer is a subgroup of basal breast cancers. Cancer Res 2006;66:4636–4644.
Jacquemier J, Padovani L, Rabayrol L, et al. Typical medullary breast carcinomas have a basal/myoepithelial phenotype. J Pathol 2005;207:260–268.
Vincent-Salomon A, Gruel N, Lucchesi C, et al. Identification of typical medullary breast carcinoma as a genomic sub-group of basal-like carcinomas, a heterogeneous new molecular entity. Breast Cancer Res 2007;9:R24.
Azoulay S, Lae M, Freneaux P, et al. KIT is highly expressed in adenoid cystic carcinoma of the breast, a basal-like carcinoma associated with a favourable outcome. Mod Pathol 2005;18:1623–1631.
Reis-Filho JS, Milanezi F, Steele D, et al. Metaplastic breast carcinomas are basal-like tumours. Histopathology 2006;49:10–21.
Rakha EA, Reis-Filho JS, Ellis IO . Basal-like breast cancer: a critical review. J Clin Oncol 2008;26:2568–2581.
Turner NC, Reis-Filho JS, Russell AM, et al. BRCA1 dysfunction in sporadic basal-like breast cancer. Oncogene 2007;26:2126–2132.
López-Bonet E, Alonso-Ruano M, Barraza G, et al. Solid neuroendocrine breast carcinomas: incidence, clinico-pathological features and immunohistochemical profiling. Oncol Rep 2008;20:1369–1374.
Kreike B, Halfwerk H, Armstrong N, et al. Local recurrence after breast conserving therapy in relation to gene expression patterns in a large series of patients. Clin Cancer Res 2009;15:4181–4190.
Moolenaar CE, Muller EJ, Schol DJ, et al. Expression of neural cell adhesion molecule-related sialoglycoprotein in small cell lung cancer and neuroblastoma cell lines H69 and CHP-212. Cancer Res 1990;50:1102–1106.
Eisen M, Spellman P, Brown P, et al. Cluster analysis and display of genome-wide expression patterns. Proc Natl Acad Sci USA 1998;95:14863–14868.
Tusher VG, Tibshirani R, Chu G . Significance analysis of microarrays applied to the ionizing radiation response. Proc Natl Acad Sci USA 2001;98:5116–5121.
Korkola JE, DeVries S, Fridlyand J, et al. Differentiation of lobular versus ductal breast carcinomas by expression microarray analysis. Cancer Res 2003;63:7167–7175.
Tomasek JJ, Gabbiani G, Hinz B, et al. Myofibroblasts and mechano-regulation of connective tissue remodelling. Nat Rev Mol Cell Biol 2002;3:349–363.
Brennan KR, Brown AM . Wnt proteins in mammary development and cancer. J Mammary Gland Biol Neoplasia 2004;9:119–131.
Schambony A, Kunz M, Gradl D . Cross-regulation of Wnt signaling and cell adhesion. Differentiation 2004;72:307–318.
Thorat MA, Marchio C, Morimiya A, et al. Forkhead box A1 expression in breast cancer is associated with luminal subtype and good prognosis. J Clin Pathol 2008;61:327–332.
Wilson BJ, Giguere V . Meta-analysis of human cancer microarrays reveals GATA3 is integral to the estrogen receptor alpha pathway. Mol Cancer 2008;7:49.
Papotti M, Sapino A, Righi L, et al. 34betaE12 cytokeratin immunodetection in the differential diagnosis of neuroendocrine carcinomas of the breast. Appl Immunohistochem Mol Morphol 2001;9:229–233.
Easton DF, Pooley KA, Dunning AM, et al. Genome-wide association study identifies novel breast cancer susceptibility loci. Nature 2007;447:1087–1093.
Hunter DJ, Kraft P, Jacobs KB, et al. A genome-wide association study identifies alleles in FGFR2 associated with risk of sporadic postmenopausal breast cancer. Nat Genet 2007;39:870–874.
Garcia-Closas M, Hall P, Nevanlinna H, et al. Heterogeneity of breast cancer associations with five susceptibility loci by clinical and pathological characteristics. PLoS Genet 2008;4:e1000054.
Schröder M, Kaufman RJ . The mammalian unfolded protein response. Annu Rev Biochem 2005;74:739–789.
Xu C, Bailly-Maitre B, Reed JC . Endoplasmic reticulum stress: cell life and death decisions. J Clin Invest 2005;115:2656–2664.
Moenner M, Pluquet O, Bouchecareilh M, et al. Integrated endoplasmic reticulum stress responses in cancer. Cancer Res 2007;67:10631–10634.
Hanna WM, Corkill M . Mucins in breast carcinoma. Hum Pathol 1988;19:11–14.
Sáez C, Japón MA, Poveda MA, et al. Mucinous (colloid) adenocarcinomas secrete distinct O-acylated forms of sialomucins: a histochemical study of gastric, colorectal and breast adenocarcinomas. Histopathology 2001;39:554–560.
Kim I, Xu W, Reed JC . Cell death and endoplasmic reticulum stress: disease relevance and therapeutic opportunities. Nat Rev Drug Discov 2008;7:1013–1030.
Fujii H, Anbazhagan R, Bornman DM, et al. Mucinous cancers have fewer genomic alterations than more common classes of breast cancer. Breast Cancer Res Treat 2002;76:255–260.
Di Saverio S, Gutierrez J, Avisar E . A retrospective review with long term follow up of 11 400 cases of pure mucinous breast carcinoma. Breast Cancer Res Treat 2008;111:541–547.
Acknowledgements
The authors would like to thank Kay Savage for technical assistance with the immunohistochemical stainings. FCG and JSR-F are supported by Breakthrough Breast Cancer Centre. We also acknowledge NHS funding to the NIHR Biomedical Research Centre.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Disclosure/conflict of interest
The authors declare no conflict of interest.
Supplementary Information accompanies the paper on Modern Pathology website (http://www.nature.com/modpathol)
Supplementary information
Rights and permissions
About this article
Cite this article
Weigelt, B., Geyer, F., Horlings, H. et al. Mucinous and neuroendocrine breast carcinomas are transcriptionally distinct from invasive ductal carcinomas of no special type. Mod Pathol 22, 1401–1414 (2009). https://doi.org/10.1038/modpathol.2009.112
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/modpathol.2009.112
Keywords
This article is cited by
-
Breast cancer with neuroendocrine differentiation: an update based on the latest WHO classification
Modern Pathology (2021)
-
Papillary neoplasms of the breast—reviewing the spectrum
Modern Pathology (2021)
-
Exploring Collagen Parameters in Pure Special Types of Invasive Breast Cancer
Scientific Reports (2019)
-
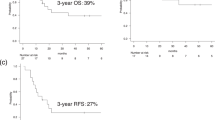
Primary neuroendocrine breast carcinomas are associated with poor local control despite favourable biological profile: a retrospective clinical study
BMC Cancer (2017)
-
Neuroendocrine Tumors of the Breast
Endocrine Pathology (2017)