Abstract
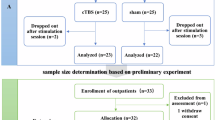
Cognitive-behavioral therapy (CBT) is effective for pediatric obsessive-compulsive disorder (OCD), but non-response is common. Brain glutamate (Glu) signaling may contribute to OCD pathophysiology and moderate CBT outcomes. We assessed whether Glu measured with magnetic resonance spectroscopy (MRS) was associated with OCD and/or CBT response. Youths aged 7–17 years with DSM-IV OCD and typically developing controls underwent 3 T proton echo-planar spectroscopic imaging (PEPSI) MRS scans of pregenual anterior cingulate cortex (pACC) and ventral posterior cingulate cortex (vPCC)—regions possibly affected by OCD—at baseline. Controls returned for re-scan after 8 weeks. OCD youth—in a randomized rater-blinded trial—were re-scanned after 12–14 weeks of CBT or after 8 weeks of minimal-contact waitlist; waitlist participants underwent a third scan after crossover to 12–14 weeks of CBT. Forty-nine children with OCD (mean age 12.2±2.9 years) and 29 controls (13.2±2.2 years) provided at least one MRS scan. At baseline, Glu did not differ significantly between OCD and controls in pACC or vPCC. Within controls, Glu was stable from scan-to-scan. Within OCD subjects, a treatment-by-scan interaction (p=0.034) was observed, driven by pACC Glu dropping 19.5% from scan-to-scan for patients randomized to CBT, with minor increases (3.8%) for waitlist participants. The combined OCD participants (CBT-only plus waitlist-CBT) also showed a 16.2% (p=0.004) post-CBT decrease in pACC Glu. In the combined OCD group, within vPCC, lower pre-CBT Glu predicted greater post-CBT improvement in symptoms (CY-BOCS; r=0.81, p=0.00025). Glu may be involved in the pathophysiology of OCD and may moderate response to CBT.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Arnold PD, Macmaster FP, Richter MA, Hanna GL, Sicard T, Burroughs E et al (2009). Glutamate receptor gene (GRIN2B) associated with reduced anterior cingulate glutamatergic concentration in pediatric obsessive-compulsive disorder. Psychiatry Res 172: 136–139.
Benazon NR, Moore GJ, Rosenberg DR (2003). Neurochemical analyses in pediatric obsessive-compulsive disorder in patients treated with cognitive-behavioral therapy. J Am Acad Child Adolesc Psychiatry 42: 1279–1285.
Bhattacharyya S, Khanna S, Chakrabarty K, Mahadevan A, Christopher R, Shankar SK (2009). Anti-brain autoantibodies and altered excitatory neurotransmitters in obsessive-compulsive disorder. Neuropsychopharmacology 34: 2489–2496.
Brennan BP, Jensen JE, Perriello C, Pope HG Jr, Jenike MA, Hudson JI et al (2016). Lower posterior cingulate cortex glutathione levels in obsessive-compulsive disorder. Biol Psychiatry Cogn Neurosci Neuroimaging 1: 116–124.
Brennan BP, Rauch SL, Jensen E, Pope HG Jr (2013). A critical review of magnetic resonance spectroscopy studies of obsessive-compulsive disorder. Biol Psychiatry 73: 24–31.
Brennan BP, Tkachenko O, Schwab ZJ, Juelich RJ, Ryan EM, Athey AJ et al (2015). An examination of rostral anterior cingulate cortex function and neurochemistry in obsessive-compulsive disorder. Neuropsychopharmacology 40: 1866–1876.
Carlsson ML (2000). On the role of cortical glutamate in obsessive-compulsive disorder and attention-deficit hyperactivity disorder, two phenomenologically antithetical conditions. Acta Psychiatr Scand 102: 401–413.
Chakrabarty K, Bhattacharyya S, Christopher R, Khanna S (2005). Glutamatergic dysfunction in OCD. Neuropsychopharmacology 30: 1735–1740.
Cheng Y, Xu J, Nie B, Luo C, Yang T, Li H et al (2013). Abnormal resting-state activities and functional connectivities of the anterior and the posterior cortexes in medication-naive patients with obsessive-compulsive disorder. PLoS ONE 8: e67478.
Ciesielski KT, Rauch SL, Ahlfors SP, Vangel ME, Wilhelm S, Rosen BR et al (2012). Role of medial cortical networks for anticipatory processing in obsessive-compulsive disorder. Hum Brain Mapp 33: 2125–2134.
Desikan RS, Segonne F, Fischl B, Quinn BT, Dickerson BC, Blacker D et al (2006). An automated labeling system for subdividing the human cerebral cortex on MRI scans into gyral based regions of interest. Neuroimage 31: 968–980.
Feusner JD, Kerwin L, Saxena S, Bystritsky A (2009). Differential efficacy of memantine for obsessive-compulsive disorder vs. generalized anxiety disorder: an open-label trial. Psychopharmacol Bull 42: 81–93.
Fullana MA, Cardoner N, Alonso P, Subirà M, López-Solà C, Pujol J et al (2014). Brain regions related to fear extinction in obsessive-compulsive disorder and its relation to exposure therapy outcome: a morphometric study. Psychol Med 44: 845–856.
Geller DA (2006). Obsessive-compulsive and spectrum disorders in children and adolescents. Psychiatr Clin N Am 29: 353–370.
Goodman WK, McDougle CJ, Barr LC, Aronson SC, Price LH (1993). Biological approaches to treatment-resistant obsessive compulsive disorder. J Clin Psychiatry 54: 16–26.
Hyder F, Fulbright RK, Shulman RG, Rothman DL (2013). Glutamatergic function in the resting awake human brain is supported by uniformly high oxidative energy. J Cereb Blood Flow Metab 33: 339–347.
Hyder F, Patel AB, Gjedde A, Rothman DL, Behar KL, Shulman RG (2006). Neuronal-glial glucose oxidation and glutamatergic-GSABAergic function. J Cereb Blood Flow Metab 26: 865–877.
Lázaro L, Bargallo N, Andrés S, Falcón C, Morer A, Junque C et al (2012). Proton magnetic resonance spectroscopy in pediatric obsessive-compulsive disorder: longitudinal study before and after treatment. Psychiatry Res 201: 17–24.
MacMaster FP, O'Neill J, Rosenberg DR (2008). Brain imaging in pediatric obsessive- compulsive disorder. J Am Acad Child Adolesc Psychiatry 47: 1262–1272.
McGuire J, Piacentini J, Lewin A, Brennan E, Murphy T, Storch E A meta-analysis of cognitive behavior therapy and medication for child obsessive compulsive disorder: treatment efficacy, response and remission. Depress Anxiety 32: 580–593 (2015).
Milad MR, Rauch SL (2012). Obsessive-compulsive disorder: beyond segregated cortico- striatal pathways. Trends Cogn Sci 16: 43–51.
Morgiève M, N'Diaye K, Haynes WI, Granger B, Clair AH, Pelissolo A et al (2014). Dynamics of psychotherapy-related cerebral haemodynamic changes in obsessive compulsive disorder using a personalized exposure task in functional magnetic resonance imaging. Psychol Med 44: 1461–1473.
Nakao T, Nakagawa A, Yoshiura T, Nakatani E, Nabeyama M, Yoshizato C et al (2005). Brain activation of patients with obsessive-compulsive disorder during neuropsychological and symptom provocation tasks before and after symptom improvement: a functional magnetic resonance imaging study. Biol Psychiatry 57: 901–910.
O'Neill J, Gorbis E, Feusner JD, Yip JC, Chang S, Maidment KM et al (2013). Effects of intensive cognitive-behavioral therapy on cingulate neurochemistry in obsessive-compulsive disorder. J Psychiatr Res 47: 494–504.
O'Neill J, Lai TM, Sheen C, Salgari GC, Ly R, Armstrong C et al (2016). Cingulate and thalamic metabolites in obsessive-compulsive disorder. Psychiatry Res 254: 34–40.
O'Neill J, Levitt JG, Alger JR (2013). Magnetic resonance spectroscopy studies of attention deficit hyperactivity disorder. In: Blüml S, Panigrahy A (eds). MR Spectroscopy of Pediatric Brain Disorders. Springer: New York, USA, pp 229–276.
O'Neill J, Piacentini JC, Chang S, Levitt JG, Rozenman M, Bergman L et al (2012). MRSI correlates of cognitive-behavioral therapy in pediatric obsessive-compulsive disorder. Prog Neuropsychopharmacol Biol Psychiatry 36: 161–168.
Ortiz AE, Ortiz AG, Falcon C, Morer A, Plana MT, Bargalló N et al (2015). 1H-MRS of the anterior cingulate cortex in childhood and adolescent obsessive-compulsive disorder: a case-control study. Eur Neuropsychopharmacol 25: 60–68.
Piacentini JLA, Roblek T (2007) Overcoming Childhood OCD: A Therapist’s Guide. Oxford University Press: New York, USA.
Piacentini J, Bergman RL, Chang S, Langley A, Peris T, Wood JJ et al (2011). Controlled comparison of family cognitive behavioral therapy and psychoeducation/relaxation training for child obsessive-compulsive disorder. J Am Acad Child Adolesc Psychiatry 50: 1149–1161.
Pittenger CBM, Wegner R, Teitelbaum C, Krystal JH, Coric V (2006). Glutamate dysfunction in obsessive-compulsive disorder and the potential clinical utility of glutamate-modulating agents. Primary Psychiatry 13: 65–77.
Pittenger C, Bloch MH, Williams K (2011). Glutamate abnormalities in obsessive compulsive disorder: neurobiology, pathophysiology, and treatment. Pharmacol Ther 132: 314–332.
Posse S, Otazo R, Caprihan A, Bustillo J, Chen H, Henry PG et al (2007). Proton echo- planar spectroscopic imaging of J-coupled resonances in human brain at 3 and 4 Tesla. Magn Reson Med 58: 236–244.
Rosenberg DR, Keshavan MS (1998). AE Bennett Research Award. Toward a neurodevelopmental model of obsessive–compulsive disorder. Biol Psychiatry 43: 623–640.
Rosenberg DR, MacMaster FP, Keshavan MS, Fitzgerald KD, Stewart CM, Moore GJ (2000). Decrease in caudate glutamatergic concentrations in pediatric obsessive-compulsive disorder patients taking paroxetine. J Am Acad Child Adolesc Psychiatry 39: 1096–1103.
Rosenberg DR, Mirza Y, Russell A, Tang J, Smith JM, Banerjee SP et al (2004). Reduced anterior cingulate glutamatergic concentrations in childhood OCD and major depression versus healthy controls. J Am Acad Child Adolesc Psychiatry 43: 1146–1153.
Rothman DL, De Feyter HM, de Graaf RA, Mason GF, Behar KL (2011). 13C MRS studies of neuroenergetics and neurotransmitter cycling in humans. NMR Biomed 24: 943–957.
Saxena S, Gorbis E, O'Neill J, Baker SK, Mandelkern MA, Maidment KM et al (2009a). Rapid effects of brief intensive cognitive-behavioral therapy on brain glucose metabolism in obsessive-compulsive disorder. Mol Psychiatry 14: 197–205.
Saxena S, O'Neill J, Rauch SL (2009b). The role of cingulate cortex dysfunction in obsessive-compulsive disorder. In: Vogt B (ed). Cingulate Neurobiology and Disease. Oxford University Press: New York, USA, pp 587–618.
Seese RR, O'Neill J, Hudkins M, Siddarth P, Levitt J, Tseng B et al (2011). Proton magnetic resonance spectroscopy and thought disorder in childhood schizophrenia. Schizophr Res 133: 82–90.
Simpson HB, Shungu DC, Bender J Jr, Mao X, Xu X, Slifstein M et al (2012). Investigation of cortical glutamate-glutamine and gamma-aminobutyric acid in obsessive-compulsive disorder by proton magnetic resonance spectroscopy. Neuropsychopharmacology 37: 2684–2692.
Starck G, Ljungberg M, Nilsson M, Jonsson L, Lundberg S, Ivarsson T et al (2008). A 1H magnetic resonance spectroscopy study in adults with obsessive compulsive disorder: relationship between metabolite concentrations and symptom severity. J Neural Transm (Vienna) 115: 1051–1062.
Tang W, Li B, Huang X, Jiang X, Li F, Wang L et al (2013). Morphometric brain characterization of refractory obsessive-compulsive disorder: diffeomorphic anatomic registration using exponentiated Lie algebra. Prog Neuropsychopharmacol Biol Psychiatry 46: 126–131.
Torp NC, Dahl K, Skarphedinsson G, Compton S, Thomsen PH, Weidle B et al (2015). Predictors associated with improved cognitive-behavioral therapy outcome in pediatric obsessive-compulsive disorder. J Am Acad Child Adolesc Psychiatry 54: 200–207.
Vogt B (2009) Regions and subregions of the cingulate gyrus. In: Vogt B (ed). Cingulate Neurobiology and Disease. Oxford University Press: New York, USA. pp 3–30.
Whiteside SP, Abramowitz JS, Port JD (2012). Decreased caudate N-acetyl-l-aspartic acid in pediatric obsessive-compulsive disorder and the effects of behavior therapy. Psychiatry Res 202: 53–59.
Wu K, Hanna GL, Rosenberg DR, Arnold PD (2012). The role of glutamate signaling in the pathogenesis and treatment of obsessive–compulsive disorder. Pharm Biochem Behav 100: 726–735.
Yücel M, Wood SJ, Wellard RM, Harrison BJ, Fornito A, Pujol J et al (2008). Anterior cingulate glutamate-glutamine levels predict symptom severity in women with obsessive-compulsive disorder. Aust NZ J Psychiatry 42: 467–477.
Zhang J (2013). Human brain glutamate, glutamine, γ-aminobutyric acid, proton magnetic resonance, spectral quantification with the fast Padé transform. Doctoral dissertation, University of California, Los Angeles, CA, USA.
Zurowski B, Freyer T, Wahl K, Büchert M, Kuel AK, Hohagen F et al (2007). Neurochemical abnormalities in patients with obsessive-compulsive disorder diminish in the course of behavior therapy. Soc Neurosci Abstr 450: 10.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supplementary Information accompanies the paper on the Neuropsychopharmacology website
Supplementary information
Rights and permissions
About this article
Cite this article
O'Neill, J., Piacentini, J., Chang, S. et al. Glutamate in Pediatric Obsessive-Compulsive Disorder and Response to Cognitive-Behavioral Therapy: Randomized Clinical Trial. Neuropsychopharmacol 42, 2414–2422 (2017). https://doi.org/10.1038/npp.2017.77
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/npp.2017.77
This article is cited by
-
Neurophysiological Signatures of Mindfulness-Based Stress Reduction in Adults with Autism: Putative Mechanism of Anxiety Alleviation
Mindfulness (2023)
-
Role of Sonic Hedgehog Signaling Activation in the Prevention of Neurological Abnormalities Associated with Obsessive–Compulsive Disorder
Neurotoxicity Research (2022)
-
Neurochemical properties measured by 1H magnetic resonance spectroscopy may predict cognitive behaviour therapy outcome in paediatric OCD: a pilot study
Journal of Neural Transmission (2021)
-
Is glutamate associated with fear extinction and cognitive behavior therapy outcome in OCD? A pilot study
European Archives of Psychiatry and Clinical Neuroscience (2020)
-
Current Pharmacological Treatments for Childhood Onset OCD
Current Treatment Options in Psychiatry (2019)