Abstract
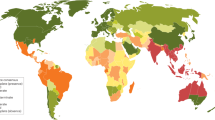
Burkholderia pseudomallei is a Gram-negative environmental bacterium and the aetiological agent of melioidosis, a life-threatening infection that is estimated to account for ∼89,000 deaths per year worldwide. Diabetes mellitus is a major risk factor for melioidosis, and the global diabetes pandemic could increase the number of fatalities caused by melioidosis. Melioidosis is endemic across tropical areas, especially in southeast Asia and northern Australia. Disease manifestations can range from acute septicaemia to chronic infection, as the facultative intracellular lifestyle and virulence factors of B. pseudomallei promote survival and persistence of the pathogen within a broad range of cells, and the bacteria can manipulate the host's immune responses and signalling pathways to escape surveillance. The majority of patients present with sepsis, but specific clinical presentations and their severity vary depending on the route of bacterial entry (skin penetration, inhalation or ingestion), host immune function and bacterial strain and load. Diagnosis is based on clinical and epidemiological features as well as bacterial culture. Treatment requires long-term intravenous and oral antibiotic courses. Delays in treatment due to difficulties in clinical recognition and laboratory diagnosis often lead to poor outcomes and mortality can exceed 40% in some regions. Research into B. pseudomallei is increasing, owing to the biothreat potential of this pathogen and increasing awareness of the disease and its burden; however, better diagnostic tests are needed to improve early confirmation of diagnosis, which would enable better therapeutic efficacy and survival.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 1 digital issues and online access to articles
$119.00 per year
only $119.00 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Whitmore, A. An Account of a Glanders-like Disease occurring in Rangoon. J. Hyg. 13, 1–34.1 (1913).
Kaestli, M. et al. Out of the ground: aerial and exotic habitats of the melioidosis bacterium Burkholderia pseudomallei in grasses in Australia. Environ. Microbiol. 14, 2058–2070 (2012).
Limmathurotsakul, D. et al. Predicted global distribution of Burkholderia pseudomallei and burden of melioidosis. Nat. Microbiol. 1, 15008 (2016). This is a key publication on the global burden of melioidosis that uses human, animal and environmental data to estimate the number of human melioidosis cases per year at 165,000 worldwide, of which 89,000 are fatal.
Wiersinga, W. J., Currie, B. J. & Peacock, S. J. Melioidosis. N. Engl. J. Med. 367, 1035–1044 (2012). This article reviews the clinical manifestations, epidemiology, pathogenesis, diagnosis and treatment of melioidosis, with an emphasis on clinical management.
Limmathurotsakul, D. et al. Activities of daily living associated with acquisition of melioidosis in northeast Thailand: a matched case-control study. PLoS Negl. Trop. Dis. 7, e2072 (2013).
Cheng, A. C. & Currie, B. J. Melioidosis: epidemiology, pathophysiology, and management. Clin. Microbiol. Rev. 18, 383–416 (2005).
Currie, B. J., Ward, L. & Cheng, A. C. The epidemiology and clinical spectrum of melioidosis: 540 cases from the 20 year Darwin prospective study. PLoS Negl. Trop. Dis. 4, e900 (2010). This is the Darwin prospective study of melioidosis that has provided numerous new insights into the epidemiology and clinical spectrum of melioidosis. This article concludes that melioidosis should be regarded as an opportunistic infection that is unlikely to kill a healthy person in a resource-rich environment, provided the infection is diagnosed early.
Yee, K. C., Lee, M. K., Chua, C. T. & Puthucheary, S. D. Melioidosis, the great mimicker: a report of 10 cases from Malaysia. J. Trop. Med. Hyg. 91, 249–254 (1988).
Maharjan, B. et al. Recurrent melioidosis in patients in northeast Thailand is frequently due to reinfection rather than relapse. J. Clin. Microbiol. 43, 6032–6034 (2005).
Chetchotisakd, P. et al. Trimethoprim-sulfamethoxazole versus trimethoprim-sulfamethoxazole plus doxycycline as oral eradicative treatment for melioidosis (MERTH): a multicentre, double-blind, non-inferiority, randomised controlled trial. Lancet 383, 807–814 (2014).
Suputtamongkol, Y. et al. Amoxycillin-clavulanic acid treatment of melioidosis. Trans. R. Soc. Trop. Med. Hyg. 85, 672–675 (1991).
Currie, B. J. Melioidosis: evolving concepts in epidemiology, pathogenesis, and treatment. Semin. Respir. Crit. Care Med. 36, 111–125 (2015).
Willcocks, S. J., Denman, C. C., Atkins, H. S. & Wren, B. W. Intracellular replication of the well-armed pathogen Burkholderia pseudomallei. Curr. Opin. Microbiol. 29, 94–103 (2016).
Centers for Disease Control and Prevention. Possession, use, and transfer of select agents and toxins; biennial review. Final rule. Fed. Regist. 77, 61083–61115 (2012).
Silva, E. B. & Dow, S. W. Development of Burkholderia mallei and pseudomallei vaccines. Front. Cell. Infect. Microbiol. 3, 10 (2013).
Titball, R. W., Burtnick, M. N., Bancroft, G. J. & Brett, P. Burkholderia pseudomallei and Burkholderia mallei vaccines: are we close to clinical trials? Vaccine 35, 5981–5989 (2017). This is an up-to-date summary of vaccine research and front-line contenders with potential for success.
Limmathurotsakul, D. et al. Systematic review and consensus guidelines for environmental sampling of Burkholderia pseudomallei.. PLoS Negl. Trop. Dis. 7, e2105 (2013).
Pumpuang, A. et al. Survival of Burkholderia pseudomallei in distilled water for 16 years. Trans. R. Soc. Trop. Med. Hyg. 105, 598–600 (2011).
Hantrakun, V. et al. Soil nutrient depletion is associated with the presence of Burkholderia pseudomallei. Appl. Environ. Microbiol. 82, 7086–7092 (2016).
Yip, T. W. et al. Endemic melioidosis in residents of desert region after atypically intense rainfall in central australia, 2011. Emerg. Infect. Dis. 21, 1038–1040 (2015).
Currie, B. J. et al. A cluster of melioidosis cases from an endemic region is clonal and is linked to the water supply using molecular typing of Burkholderia pseudomallei isolates. Am. J. Trop. Med. Hyg. 65, 177–179 (2001).
Inglis, T. J. et al. Acute melioidosis outbreak in Western Australia. Epidemiol. Infect. 123, 437–443 (1999).
Limmathurotsakul, D. et al. Melioidosis caused by Burkholderia pseudomallei in drinking water, Thailand, 2012. Emerg. Infect. Dis. 20, 265–268 (2014).
Merritt, A. J. et al. Cutaneous melioidosis cluster caused by contaminated wound irrigation fluid. Emerg. Infect. Dis. 22, 1420–1427 (2016).
Gal, D. et al. Contamination of hand wash detergent linked to occupationally acquired melioidosis. Am. J. Trop. Med. Hyg. 71, 360–362 (2004).
Kinoshita, R. E. Epidemiology of melioidosis in an oceanarium: a clinical, environmental & molecular study. Thesis, Univ. of Hong Kong (2003).
Chen, P. S. et al. Airborne transmission of melioidosis to humans from environmental aerosols contaminated with B. pseudomallei. PLoS Negl. Trop. Dis. 9, e0003834 (2015).
Currie, B. J. et al. Use of whole-genome sequencing to link Burkholderia pseudomallei from air sampling to mediastinal melioidosis, Australia. Emerg. Infect. Dis. 21, 2052–2054 (2015).
Thatrimontrichai, A. & Maneenil, G. Neonatal melioidosis: systematic review of the literature. Pediatr. Infect. Dis. J. 31, 1195–1197 (2012).
Rolim, D. B. et al. Melioidosis, northeastern Brazil. Emerg. Infect. Dis. 11, 1458–1460 (2005).
Salam, A. P. et al. Melioidosis acquired by traveler to Nigeria. Emerg. Infect. Dis. 17, 1296–1298 (2011).
Birnie, E., Wiersinga, W. J., Limmathurotsakul, D. & Grobusch, M. P. Melioidosis in Africa: should we be looking more closely? Future Microbiol. 10, 273–281 (2015).
Wiersinga, W. J. et al. Clinical, environmental, and serologic surveillance studies of melioidosis in Gabon, 2012–2013. Emerg. Infect. Dis. 21, 40–47 (2015).
McLeod, C. et al. Clinical presentation and medical management of melioidosis in children: a 24-year prospective study in the Northern Territory of Australia and review of the literature. Clin. Infect. Dis. 60, 21–26 (2015).
Limmathurotsakul, D. et al. Increasing incidence of human melioidosis in Northeast Thailand. Am. J. Trop. Med. Hyg. 82, 1113–1117 (2010).
Currie, B. J. et al. Melioidosis epidemiology and risk factors from a prospective whole-population study in northern Australia. Trop. Med. Int. Health 9, 1167–1174 (2004).
Fong, S. M., Wong, K. J., Fukushima, M. & Yeo, T. W. Thalassemia major is a major risk factor for pediatric melioidosis in Kota Kinabalu, Sabah, Malaysia. Clin. Infect. Dis. 60, 1802–1807 (2015).
Turner, P. et al. A retrospective analysis of melioidosis in Cambodian children, 2009–2013. BMC Infect. Dis. 16, 688 (2016).
Lim, M. K., Tan, E. H., Soh, C. S. & Chang, T. L. Burkholderia pseudomallei infection in the Singapore Armed Forces from 1987 to 1994 — an epidemiological review. Ann. Acad. Med. Singapore 26, 13–17 (1997).
Ooi, W. F. et al. The condition-dependent transcriptional landscape of Burkholderia pseudomallei. PLoS Genet. 9, e1003795 (2013).
Wiersinga, W. J., van der Poll, T., White, N. J., Day, N. P. & Peacock, S. J. Melioidosis: insights into the pathogenicity of Burkholderia pseudomallei. Nat. Rev. Microbiol. 4, 272–282 (2006).
Allwood, E. M., Devenish, R. J., Prescott, M., Adler, B. & Boyce, J. D. Strategies for intracellular survival of Burkholderia pseudomallei. Front. Microbiol. 2, 170 (2011).
Stone, J. K., DeShazer, D., Brett, P. J. & Burtnick, M. N. Melioidosis: molecular aspects of pathogenesis. Expert Rev. Anti Infect. Ther. 12, 1487–1499 (2014).
Lazar Adler, N. R. et al. The molecular and cellular basis of pathogenesis in melioidosis: how does Burkholderia pseudomallei cause disease? FEMS Microbiol. Rev. 33, 1079–1099 (2009).
Sun, G. W. & Gan, Y. H. Unraveling type III secretion systems in the highly versatile Burkholderia pseudomallei. Trends Microbiol. 18, 561–568 (2010).
Stevens, M. P. et al. An Inv/Mxi-Spa-like type III protein secretion system in Burkholderia pseudomallei modulates intracellular behaviour of the pathogen. Mol. Microbiol. 46, 649–659 (2002).
Burtnick, M. N., Brett, P. J. & DeShazer, D. Proteomic analysis of the Burkholderia pseudomallei type II secretome reveals hydrolytic enzymes, novel proteins, and the deubiquitinase TssM. Infect. Immun. 82, 3214–3226 (2014).
Campos, C. G., Byrd, M. S. & Cotter, P. A. Functional characterization of Burkholderia pseudomallei trimeric autotransporters. Infect. Immun. 81, 2788–2799 (2013).
Ahmed, K. et al. Attachment of Burkholderia pseudomallei to pharyngeal epithelial cells: a highly pathogenic bacteria with low attachment ability. Am. J. Trop. Med. Hyg. 60, 90–93 (1999).
Essex-Lopresti, A. E. et al. A type IV pilin, PilA, contributes to adherence of Burkholderia pseudomallei and virulence in vivo. Infect. Immun. 73, 1260–1264 (2005).
Phewkliang, A., Wongratanacheewin, S. & Chareonsudjai, S. Role of Burkholderia pseudomallei in the invasion, replication and induction of apoptosis in human epithelial cell lines. Southeast Asian J. Trop. Med. Public Health 41, 1164–1176 (2010).
David, J., Bell, R. E. & Clark, G. C. Mechanisms of disease: host-pathogen interactions between Burkholderia species and lung epithelial cells. Front. Cell. Infect. Microbiol. 5, 80 (2015).
Chuaygud, T., Tungpradabkul, S., Sirisinha, S., Chua, K. L. & Utaisincharoen, P. A role of Burkholderia pseudomallei flagella as a virulent factor. Trans. R. Soc. Trop. Med. Hyg. 102 (Suppl. 1), S140–S144 (2008).
Balder, R. et al. Identification of Burkholderia mallei and Burkholderia pseudomallei adhesins for human respiratory epithelial cells. BMC Microbiol. 10, 250 (2010).
Stevens, M. P. et al. A Burkholderia pseudomallei type III secreted protein, BopE, facilitates bacterial invasion of epithelial cells and exhibits guanine nucleotide exchange factor activity. J. Bacteriol. 185, 4992–4996 (2003).
Kager, L. M., Wiersinga, W. J., Roelofs, J. J., van ‘t Veer, C. & van der Poll, T. Deficiency of protease-activated receptor-1 limits bacterial dissemination during severe Gram-negative sepsis (melioidosis). Microbes Infect. 16, 171–174 (2014).
Pruksachartvuthi, S., Aswapokee, N. & Thankerngpol, K. Survival of Pseudomonas pseudomallei in human phagocytes. J. Med. Microbiol. 31, 109–114 (1990).
Jones, A. L., Beveridge, T. J. & Woods, D. E. Intracellular survival of Burkholderia pseudomallei. Infect. Immun. 64, 782–790 (1996).
Harley, V. S., Dance, D. A., Tovey, G., McCrossan, M. V. & Drasar, B. S. An ultrastructural study of the phagocytosis of Burkholderia pseudomallei. Microbios 94, 35–45 (1998).
Kespichayawattana, W., Rattanachetkul, S., Wanun, T., Utaisincharoen, P. & Sirisinha, S. Burkholderia pseudomallei induces cell fusion and actin-associated membrane protrusion: a possible mechanism for cell-to-cell spreading. Infect. Immun. 68, 5377–5384 (2000).
Ray, K., Marteyn, B., Sansonetti, P. J. & Tang, C. M. Life on the inside: the intracellular lifestyle of cytosolic bacteria. Nat. Rev. Microbiol. 7, 333–340 (2009).
Stevens, M. P. et al. Attenuated virulence and protective efficacy of a Burkholderia pseudomallei bsa type III secretion mutant in murine models of melioidosis. Microbiology 150, 2669–2676 (2004).
Sun, G. W., Lu, J., Pervaiz, S., Cao, W. P. & Gan, Y. H. Caspase-1 dependent macrophage death induced by Burkholderia pseudomallei. Cell. Microbiol. 7, 1447–1458 (2005).
Suparak, S. et al. Multinucleated giant cell formation and apoptosis in infected host cells is mediated by Burkholderia pseudomallei type III secretion protein BipB. J. Bacteriol. 187, 6556–6560 (2005).
Ireland, P. M., Marshall, L., Norville, I. & Sarkar-Tyson, M. The serine protease inhibitor Ecotin is required for full virulence of Burkholderia pseudomallei. Microb. Pathog. 67–68, 55–58 (2014).
Nathan, S. A. & Puthucheary, S. D. An electronmicroscopic study of the interaction of Burkholderia pseudomallei and human macrophages. Malays. J. Pathol. 27, 3–7 (2005).
Miyagi, K., Kawakami, K. & Saito, A. Role of reactive nitrogen and oxygen intermediates in gamma interferon-stimulated murine macrophage bactericidal activity against Burkholderia pseudomallei. Infect. Immun. 65, 4108–4113 (1997).
Ekchariyawat, P. et al. Burkholderia pseudomallei-induced expression of suppressor of cytokine signaling 3 and cytokine-inducible src homology 2-containing protein in mouse macrophages: a possible mechanism for suppression of the response to gamma interferon stimulation. Infect. Immun. 73, 7332–7339 (2005).
Wiersinga, W. J. et al. Immunosuppression associated with interleukin-1R-associated-kinase-M upregulation predicts mortality in Gram-negative sepsis (melioidosis). Crit. Care Med. 37, 569–576 (2009).
Vanaporn, M. et al. Superoxide dismutase C is required for intracellular survival and virulence of Burkholderia pseudomallei. Microbiology 157, 2392–2400 (2011).
Loprasert, S., Whangsuk, W., Sallabhan, R. & Mongkolsuk, S. Regulation of the katG-dpsA operon and the importance of KatG in survival of Burkholderia pseudomallei exposed to oxidative stress. FEBS Lett. 542, 17–21 (2003).
Loprasert, S., Sallabhan, R., Whangsuk, W. & Mongkolsuk, S. Compensatory increase in ahpC gene expression and its role in protecting Burkholderia pseudomallei against reactive nitrogen intermediates. Arch. Microbiol. 180, 498–502 (2003).
Loprasert, S., Whangsuk, W., Sallabhan, R. & Mongkolsuk, S. DpsA protects the human pathogen Burkholderia pseudomallei against organic hydroperoxide. Arch. Microbiol. 182, 96–101 (2004).
Myers, N. D. et al. The role of NOD2 in murine and human melioidosis. J. Immunol. 192, 300–307 (2014).
Rinchai, D. et al. Macroautophagy is essential for killing of intracellular Burkholderia pseudomallei in human neutrophils. Autophagy 11, 748–755 (2015).
Pudla, M., Kananurak, A., Limposuwan, K., Sirisinha, S. & Utaisincharoen, P. Nucleotide-binding oligomerization domain-containing protein 2 regulates suppressor of cytokine signaling 3 expression in Burkholderia pseudomallei-infected mouse macrophage cell line RAW 264.7. Innate Immun. 17, 532–540 (2011).
Gong, L. et al. The Burkholderia pseudomallei type III secretion system and BopA are required for evasion of LC3-associated phagocytosis. PLoS ONE 6, e17852 (2011).
Cullinane, M. et al. Stimulation of autophagy suppresses the intracellular survival of Burkholderia pseudomallei in mammalian cell lines. Autophagy 4, 744–753 (2008).
Chanchamroen, S., Kewcharoenwong, C., Susaengrat, W., Ato, M. & Lertmemongkolchai, G. Human polymorphonuclear neutrophil responses to Burkholderia pseudomallei in healthy and diabetic subjects. Infect. Immun. 77, 456–463 (2009).
Breitbach, K. et al. Actin-based motility of Burkholderia pseudomallei involves the Arp 2/3 complex, but not N-WASP and Ena/VASP proteins. Cell. Microbiol. 5, 385–393 (2003).
Stevens, M. P. et al. Identification of a bacterial factor required for actin-based motility of Burkholderia pseudomallei. Mol. Microbiol. 56, 40–53 (2005).
St John, J. A. et al. Burkholderia pseudomallei penetrates the brain via destruction of the olfactory and trigeminal nerves: implications for the pathogenesis of neurological melioidosis. mBio 5, e00025 (2014).
Sarovich, D. S. et al. Variable virulence factors in Burkholderia pseudomallei (melioidosis) associated with human disease. PLoS ONE 9, e91682 (2014).
Harley, V. S., Dance, D. A., Drasar, B. S. & Tovey, G. Effects of Burkholderia pseudomallei and other Burkholderia species on eukaryotic cells in tissue culture. Microbios 96, 71–93 (1998).
French, C. T. et al. Dissection of the Burkholderia intracellular life cycle using a photothermal nanoblade. Proc. Natl Acad. Sci. USA 108, 12095–12100 (2011).
Williams, N. L., Morris, J. L., Rush, C. M. & Ketheesan, N. Migration of dendritic cells facilitates systemic dissemination of Burkholderia pseudomallei. Infect. Immun. 82, 4233–4240 (2014).
Newland, R. C. Chronic melioidosis: a case in Sydney. Pathology 1, 149–152 (1969).
Chodimella, U., Hoppes, W. L., Whalen, S., Ognibene, A. J. & Rutecki, G. W. Septicemia and suppuration in a Vietnam veteran. Hosp. Pract. 32, 219–221 (1997).
Gee, J. E. et al. Phylogeography of Burkholderia pseudomallei Isolates, Western Hemisphere. Emerg. Infect. Dis. 23, 1133–1138 (2017).
Gan, Y. H. Interaction between Burkholderia pseudomallei and the host immune response: sleeping with the enemy? J. Infect. Dis. 192, 1845–1850 (2005).
Vasu, C., Vadivelu, J. & Puthucheary, S. D. The humoral immune response in melioidosis patients during therapy. Infection 31, 24–30 (2003).
Vadivelu, J. et al. Survival and intra-nuclear trafficking of Burkholderia pseudomallei : strategies of evasion from immune surveillance? PLoS Negl Trop. Dis. 11, e0005241 (2017).
Welkos, S. L. et al. Characterization of Burkholderia pseudomallei strains using a murine intraperitoneal infection model and in vitro macrophage assays. PLoS ONE 10, e0124667 (2015).
Lewis, E. R. & Torres, A. G. The art of persistence-the secrets to Burkholderia chronic infections. Pathog. Dis. 74, ftw070 (2016).
Otsuka, Y. Prokaryotic toxin-antitoxin systems: novel regulations of the toxins. Curr. Genet. 62, 379–382 (2016).
Hamad, M. A. et al. Adaptation and antibiotic tolerance of anaerobic Burkholderia pseudomallei. Antimicrob. Agents Chemother. 55, 3313–3323 (2011).
Hayden, H. S. et al. Evolution of Burkholderia pseudomallei in recurrent melioidosis. PLoS ONE 7, e36507 (2012).
Price, E. P. et al. Within-host evolution of Burkholderia pseudomallei over a twelve-year chronic carriage infection. mBio 4, e00388-13 (2013).
Nuntayanuwat, S., Dharakul, T., Chaowagul, W. & Songsivilai, S. Polymorphism in the promoter region of tumor necrosis factor-alpha gene is associated with severe meliodosis. Hum. Immunol. 60, 979–983 (1999).
West, T. E. et al. Toll-like receptor 4 region genetic variants are associated with susceptibility to melioidosis. Genes Immun. 13, 38–46 (2012).
Chantratita, N. et al. Screen of whole blood responses to flagellin identifies TLR5 variation associated with outcome in melioidosis. Genes Immun. 15, 63–71 (2014).
West, T. E. et al. NLRC4 and TLR5 each contribute to host defense in respiratory melioidosis. PLoS Negl. Trop. Dis. 8, e3178 (2014).
Grube, M. et al. TLR5 stop codon polymorphism is associated with invasive aspergillosis after allogeneic stem cell transplantation. Med. Mycol. 51, 818–825 (2013).
Egan, A. M. & Gordon, D. L. Burkholderia pseudomallei activates complement and is ingested but not killed by polymorphonuclear leukocytes. Infect. Immun. 64, 4952–4959 (1996).
Ceballos-Olvera, I., Sahoo, M., Miller, M. A., Del Barrio, L. & Re, F. Inflammasome-dependent pyroptosis and IL-18 protect against Burkholderia pseudomallei lung infection while IL-1beta is deleterious. PLoS Pathog. 7, e1002452 (2011).
Easton, A., Haque, A., Chu, K., Lukaszewski, R. & Bancroft, G. J. A critical role for neutrophils in resistance to experimental infection with Burkholderia pseudomallei. J. Infect. Dis. 195, 99–107 (2007).
Wiersinga, W. J., Wieland, C. W., Roelofs, J. J. & van der Poll, T. MyD88 dependent signaling contributes to protective host defense against Burkholderia pseudomallei. PLoS ONE 3, e3494 (2008).
Wiersinga, W. J. et al. Toll-like receptor 2 impairs host defense in gram-negative sepsis caused by Burkholderia pseudomallei (Melioidosis). PLoS Med. 4, e248 (2007). This is the first in-depth investigation of the expression and function of TLRs in human and murine melioidosis.
Hii, C. S. et al. Interleukin-8 induction by Burkholderia pseudomallei can occur without Toll-like receptor signaling but requires a functional type III secretion system. J. Infect. Dis. 197, 1537–1547 (2008).
Wiersinga, W. J. et al. CD14 impairs host defense against gram-negative sepsis caused by Burkholderia pseudomallei in mice. J. Infect. Dis. 198, 1388–1397 (2008).
Novem, V. et al. Structural and biological diversity of lipopolysaccharides from Burkholderia pseudomallei and Burkholderia thailandensis. Clin. Vaccine Immunol. 16, 1420–1428 (2009).
Korneev, K. V. et al. Structural Relationship of the Lipid A Acyl Groups to Activation of Murine Toll-Like Receptor 4 by Lipopolysaccharides from Pathogenic Strains of Burkholderia mallei. Acinetobacter baumannii, and Pseudomonas aeruginosa. Front. Immunol. 6, 595 (2015).
Weehuizen, T. A. et al. Differential Toll-like receptor-signalling of Burkholderia pseudomallei lipopolysaccharide in murine and human models. PLoS ONE 10, e0145397 (2015).
Teh, B. E. et al. Type three secretion system-mediated escape of Burkholderia pseudomallei into the host cytosol is critical for the activation of NFκB. BMC Microbiol. 14, 115 (2014).
Bast, A. et al. Caspase-1-dependent and -independent cell death pathways in Burkholderia pseudomallei infection of macrophages. PLoS Pathog. 10, e1003986 (2014).
Wiersinga, W. J. et al. Endogenous interleukin-18 improves the early antimicrobial host response in severe melioidosis. Infect. Immun. 75, 3739–3746 (2007).
Wiersinga, W. J. et al. High-throughput mRNA profiling characterizes the expression of inflammatory molecules in sepsis caused by Burkholderia pseudomallei. Infect. Immun. 75, 3074–3079 (2007).
Lauw, F. N. et al. Elevated plasma concentrations of interferon (IFN)-gamma and the IFN-gamma-inducing cytokines interleukin (IL)-18, IL-12, and IL-15 in severe melioidosis. J. Infect. Dis. 180, 1878–1885 (1999).
Barnes, J. L. et al. Adaptive immunity in melioidosis: a possible role for T cells in determining outcome of infection with Burkholderia pseudomallei. Clin. Immunol. 113, 22–28 (2004).
Ulett, G. C., Ketheesan, N. & Hirst, R. G. Macrophage-lymphocyte interactions mediate anti-Burkholderia pseudomallei activity. FEMS Immunol. Med. Microbiol. 21, 283–286 (1998).
Jenjaroen, K. et al. T-Cell responses are associated with survival in acute melioidosis patients. PLoS Negl. Trop. Dis. 9, e0004152 (2015).
Aschenbroich, S. A., Lafontaine, E. R. & Hogan, R. J. Melioidosis and glanders modulation of the innate immune system: barriers to current and future vaccine approaches. Expert Rev. Vaccines 15, 1163–1181 (2016).
Wong, K. T., Puthucheary, S. D. & Vadivelu, J. The histopathology of human melioidosis. Histopathology 26, 51–55 (1995).
Taramasso, L., Tatarelli, P. & Di Biagio, A. Bloodstream infections in HIV-infected patients. Virulence 7, 320–328 (2016).
Chierakul, W. et al. Short report: disease severity and outcome of melioidosis in HIV coinfected individuals. Am. J. Trop. Med. Hyg. 73, 1165–1166 (2005).
Gordon, M. A. et al. Primary macrophages from HIV-infected adults show dysregulated cytokine responses to Salmonella, but normal internalization and killing. AIDS 21, 2399–2408 (2007).
Haque, A. et al. Role of T cells in innate and adaptive immunity against murine Burkholderia pseudomallei infection. J. Infect. Dis. 193, 370–379 (2006).
Simpson, A. J. et al. Prognostic value of cytokine concentrations (tumor necrosis factor-alpha, interleukin-6, and interleukin-10) and clinical parameters in severe melioidosis. J. Infect. Dis. 181, 621–625 (2000).
Lauw, F. N. et al. The CXC chemokines gamma interferon (IFN-gamma)-inducible protein 10 and monokine induced by IFN-gamma are released during severe melioidosis. Infect. Immun. 68, 3888–3893 (2000).
Barnes, J. L., Williams, N. L. & Ketheesan, N. Susceptibility to Burkholderia pseudomallei is associated with host immune responses involving tumor necrosis factor receptor-1 (TNFR1) and TNF receptor-2 (TNFR2). FEMS Immunol. Med. Microbiol. 52, 379–388 (2008).
Ekchariyawat, P. et al. Expression of suppressor of cytokine signaling 3 (SOCS3) and cytokine-inducible Src homology 2-containing protein (CIS) induced in Burkholderia pseudomallei—infected mouse macrophages requires bacterial internalization. Microb. Pathog. 42, 104–110 (2007).
Massey, S. et al. Comparative Burkholderia pseudomallei natural history virulence studies using an aerosol murine model of infection. Sci. Rep. 4, 4305 (2014).
Wiersinga, W. J. et al. Expression and function of macrophage migration inhibitory factor (MIF) in melioidosis. PLoS Negl. Trop. Dis. 4, e605 (2010).
Charoensup, J. et al. High HMGB1 level is associated with poor outcome of septicemic melioidosis. Int. J. Infect. Dis. 28, 111–116 (2014).
Doker, T. J. et al. Fatal Burkholderia pseudomallei infection initially reported as a Bacillus species, Ohio, 2013. Am. J. Trop. Med. Hyg. 91, 743–746 (2014).
Currie, B. J., Fisher, D. A., Anstey, N. M. & Jacups, S. P. Melioidosis: acute and chronic disease, relapse and re-activation. Trans. R. Soc. Trop. Med. Hyg. 94, 301–304 (2000).
Chierakul, W. et al. Melioidosis in 6 tsunami survivors in southern Thailand. Clin. Infect. Dis. 41, 982–990 (2005).
Hoffmaster, A. R. et al. Melioidosis diagnostic workshop, 2013. Emerg. Infect. Dis.https://doi.org/10.3201/eid2102.141045 (2015). This is a CDC workshop paper involving the efforts of a large working group to update the diagnosis for melioidosis.
Centers for Disease Control and Prevention. Federal Select Agent Programhttps://www.selectagents.gov/ (2017).
Wuthiekanun, V., Suputtamongkol, Y., Simpson, A. J., Kanaphun, P. & White, N. J. Value of throat swab in diagnosis of melioidosis. J. Clin. Microbiol. 39, 3801–3802 (2001).
Cheng, A. C. et al. Role of selective and nonselective media for isolation of Burkholderia pseudomallei from throat swabs of patients with melioidosis. J. Clin. Microbiol. 44, 2316 (2006).
Limmathurotsakul, D. et al. Role and significance of quantitative urine cultures in diagnosis of melioidosis. J. Clin. Microbiol. 43, 2274–2276 (2005).
Dance, D. A. B., Limmathurotsakul, D. & Currie, B. J. Burkholderia pseudomallei: challenges for the clinical microbiology laboratory — a response from the front line. J. Clin. Microbiol. 55, 980–982 (2017).
Podin, Y. et al. Burkholderia pseudomallei isolates from Sarawak, Malaysian Borneo, are predominantly susceptible to aminoglycosides and macrolides. Antimicrob. Agents Chemother. 58, 162–166 (2014).
Limmathurotsakul, D. et al. Defining the true sensitivity of culture for the diagnosis of melioidosis using Bayesian latent class models. PLoS ONE 5, e12485 (2010).
Duval, B. D. et al. Evaluation of a latex agglutination assay for the identification of Burkholderia pseudomallei and Burkholderia mallei. Am. J. Trop. Med. Hyg. 90, 1043–1046 (2014).
Suttisunhakul, V. et al. Matrix-assisted laser desorption/ionization time-of-flight mass spectrometry for the identification of Burkholderia pseudomallei from Asia and Australia and differentiation between Burkholderia species. PLoS ONE 12, e0175294 (2017).
Gee, J. E. et al. Use of 16S rRNA gene sequencing for rapid identification and differentiation of Burkholderia pseudomallei and B. mallei. J. Clin. Microbiol. 41, 4647–4654 (2003).
Koh, S. F. et al. Development of a multiplex PCR assay for rapid identification of Burkholderia pseudomallei, Burkholderia thailandensis, Burkholderia mallei and Burkholderia cepacia complex. J. Microbiol. Methods 90, 305–308 (2012).
Sheridan, E. A. et al. Evaluation of the Wayson stain for the rapid diagnosis of melioidosis. J. Clin. Microbiol. 45, 1669–1670 (2007).
Tandhavanant, S. et al. Monoclonal antibody-based immunofluorescence microscopy for the rapid identification of Burkholderia pseudomallei in clinical specimens. Am. J. Trop. Med. Hyg. 89, 165–168 (2013).
Houghton, R. L. et al. Development of a prototype lateral flow immunoassay (LFI) for the rapid diagnosis of melioidosis. PLoS Negl. Trop. Dis. 8, e2727 (2014).
Robertson, G. et al. Rapid diagnostics for melioidosis: a comparative study of a novel lateral flow antigen detection assay. J. Med. Microbiol. 64, 845–848 (2015).
Kaestli, M. et al. Comparison of TaqMan PCR assays for detection of the melioidosis agent Burkholderia pseudomallei in clinical specimens. J. Clin. Microbiol. 50, 2059–2062 (2012).
Richardson, L. J. et al. Towards a rapid molecular diagnostic for melioidosis: comparison of DNA extraction methods from clinical specimens. J. Microbiol. Methods 88, 179–181 (2012).
Chaowagul, W. et al. Melioidosis: a major cause of community-acquired septicemia in northeastern Thailand. J. Infect. Dis. 159, 890–899 (1989).
Cheng, A. C. et al. Prospective evaluation of a rapid immunochromogenic cassette test for the diagnosis of melioidosis in northeast Thailand. Trans. R. Soc. Trop. Med. Hyg. 100, 64–67 (2006).
Cheng, A. C., O’Brien, M., Freeman, K., Lum, G. & Currie, B. J. Indirect hemagglutination assay in patients with melioidosis in northern Australia. Am. J. Trop. Med. Hyg. 74, 330–334 (2006).
Pumpuang, A. et al. Comparison of O-polysaccharide and hemolysin co-regulated protein as target antigens for serodiagnosis of melioidosis. PLoS Negl. Trop. Dis. 11, e0005499 (2017).
Suttisunhakul, V. et al. Development of rapid enzyme-linked immunosorbent assays for detection of antibodies to Burkholderia pseudomallei. J. Clin. Microbiol. 54, 1259–1268 (2016).
Suttisunhakul, V. et al. Evaluation of polysaccharide-based latex agglutination assays for the rapid detection of antibodies to Burkholderia pseudomallei. Am. J. Trop. Med. Hyg. 93, 542–546 (2015).
Kohler, C. et al. Rapid and sensitive multiplex detection of Burkholderia pseudomallei-specific antibodies in melioidosis patients based on a protein microarray approach. PLoS Negl. Trop. Dis. 10, e0004847 (2016).
Boyd, R., McGuiness, S., Draper, A. D., Neilson, M. & Krause, V. Melioidosis awareness campaign.... Don't get melioidosis. Northern Territory Dis. Control Bull. 23, 1–6 (2016).
Howard, K. & Inglis, T. J. The effect of free chlorine on Burkholderia pseudomallei in potable water. Water Res. 37, 4425–4432 (2003).
McRobb, E. et al. Melioidosis from contaminated bore water and successful UV sterilization. Am. J. Trop. Med. Hyg. 89, 367–368 (2013).
Suntornsut, P. et al. Barriers and recommended interventions to prevent melioidosis in Northeast Thailand: a focus group study using the behaviour change wheel. PLoS Negl. Trop. Dis. 10, e0004823 (2016).
US National Library of Medicine. ClinicalTrials.gov, https://clinicaltrials.gov/ct2/show/NCT02089152 (2016).
Lipsitz, R. et al. Workshop on treatment of and postexposure prophylaxis for Burkholderia pseudomallei and B. mallei Infection, 2010. Emerg. Infect. Dis. 18, e2 (2012). This is a CDC workshop paper involving the efforts of a large working group to update the treatment for melioidosis.
Crowe, A., McMahon, N., Currie, B. J. & Baird, R. W. Current antimicrobial susceptibility of first-episode melioidosis Burkholderia pseudomallei isolates from the Northern Territory. Australia. Int. J. Antimicrob. Agents 44, 160–162 (2014).
Dance, D. A. et al. Trimethoprim/sulfamethoxazole resistance in Burkholderia pseudomallei. Int. J. Antimicrob. Agents 44, 368–369 (2014).
Saiprom, N. et al. Trimethoprim/sulfamethoxazole resistance in clinical isolates of Burkholderia pseudomallei from Thailand. Int. J. Antimicrob. Agents 45, 557–559 (2015).
Chaowagul, W., Simpson, A. J., Suputtamongkol, Y. & White, N. J. Empirical cephalosporin treatment of melioidosis. Clin. Infect. Dis. 28, 1328 (1999).
Dance, D. Treatment and prophylaxis of melioidosis. Int. J. Antimicrob. Agents 43, 310–318 (2014).
Harris, P., Engler, C. & Norton, R. Comparative in vitro susceptibility of Burkholderia pseudomallei to doripenem, ertapenem, tigecycline and moxifloxacin. Int. J. Antimicrob. Agents 37, 547–549 (2011).
Ashdown, L. R. Nosocomial infection due to Pseudomonas pseudomallei: two cases and an epidemiologic study. Rev. Infect. Dis. 1, 891–894 (1979).
Markovitz, A. Inoculation by bronchoscopy. West. J. Med. 131, 550 (1979).
Kelen, G. D., Hansen, K. N., Green, G. B., Tang, N. & Ganguli, C. Determinants of emergency department procedure- and condition-specific universal (barrier) precaution requirements for optimal provider protection. Ann. Emerg. Med. 25, 743–750 (1995).
Pittet, D., Allegranzi, B., Boyce, J. & World Health Organization World Alliance for Patient Safety First Global Patient Safety Challenge Core Group of Experts. The World Health Organization guidelines on hand hygiene in health care and their consensus recommendations. Infect. Control Hosp. Epidemiol. 30, 611–622 (2009).
White, N. J. et al. Halving of mortality of severe melioidosis by ceftazidime. Lancet 2, 697–701 (1989).
Simpson, A. J. et al. Comparison of imipenem and ceftazidime as therapy for severe melioidosis. Clin. Infect. Dis. 29, 381–387 (1999).
Chierakul, W. et al. Two randomized controlled trials of ceftazidime alone versus ceftazidime in combination with trimethoprim-sulfamethoxazole for the treatment of severe melioidosis. Clin. Infect. Dis. 41, 1105–1113 (2005).
Chierakul, W. et al. Addition of trimethoprim-sulfamethoxazole to ceftazidime during parenteral treatment of melioidosis is not associated with a long-term outcome benefit. Clin. Infect. Dis. 45, 521–523 (2007).
Smith, M. D., Wuthiekanun, V., Walsh, A. L. & White, N. J. Susceptibility of Pseudomonas pseudomallei to some newer beta-lactam antibiotics and antibiotic combinations using time-kill studies. J. Antimicrob. Chemother. 33, 145–149 (1994).
Smith, M. D., Wuthiekanun, V., Walsh, A. L. & White, N. J. In vitro activity of carbapenem antibiotics against beta-lactam susceptible and resistant strains of Burkholderia pseudomallei. J. Antimicrob. Chemother. 37, 611–615 (1996).
Cheng, A. C. et al. Outcomes of patients with melioidosis treated with meropenem. Antimicrob. Agents Chemother. 48, 1763–1765 (2004).
Cheng, A. C. et al. Dosing regimens of cotrimoxazole (trimethoprim-sulfamethoxazole) for melioidosis. Antimicrob. Agents Chemother. 53, 4193–4199 (2009).
Cheng, A. C. et al. Consensus guidelines for dosing of amoxicillin-clavulanate in melioidosis. Am. J. Trop. Med. Hyg. 78, 208–209 (2008).
Pitman, M. C. et al. Intravenous therapy duration and outcomes in melioidosis: a new treatment paradigm. PLoS Negl. Trop. Dis. 9, e0003586 (2015).
Chaowagul, W. et al. Relapse in melioidosis: incidence and risk factors. J. Infect. Dis. 168, 1181–1185 (1993).
Limmathurotsakul, D. et al. Risk factors for recurrent melioidosis in northeast Thailand. Clin. Infect. Dis. 43, 979–986 (2006).
Limmathurotsakul, D. et al. A simple scoring system to differentiate between relapse and re-infection in patients with recurrent melioidosis. PLoS Negl. Trop. Dis. 2, e327 (2008).
Lumbiganon, P., Chotechuangnirun, N., Kosalaraksa, P. & Teeratakulpisarn, J. Localized melioidosis in children in Thailand: treatment and long-term outcome. J. Trop. Pediatr. 57, 185–191 (2011).
Pagnarith, Y. et al. Emergence of pediatric melioidosis in Siem Reap, Cambodia. Am. J. Trop. Med. Hyg. 82, 1106–1112 (2010).
Morse, L. P. et al. Osteomyelitis and septic arthritis from infection with Burkholderia pseudomallei: a 20-year prospective melioidosis study from northern Australia. J. Orthop. 10, 86–91 (2013).
Shetty, R. P. et al. Management of melioidosis osteomyelitis and septic arthritis. Bone Joint J. 97-B, 277–282 (2015).
Cheng, A. C., West, T. E., Limmathurotsakul, D. & Peacock, S. J. Strategies to reduce mortality from bacterial sepsis in adults in developing countries. PLoS Med. 5, e175 (2008).
Stephens, D. P., Thomas, J. H., Ward, L. M. & Currie, B. J. Melioidosis causing critical illness: a review of 24 years of experience from the Royal Darwin Hospital ICU. Crit. Care Med. 44, 1500–1505 (2016).
Rhodes, A. et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Med. 43, 304–377 (2017).
Cheng, A. C., Stephens, D. P., Anstey, N. M. & Currie, B. J. Adjunctive granulocyte colony-stimulating factor for treatment of septic shock due to melioidosis. Clin. Infect. Dis. 38, 32–37 (2004).
Cheng, A. C. et al. A randomized controlled trial of granulocyte colony-stimulating factor for the treatment of severe sepsis due to melioidosis in Thailand. Clin. Infect. Dis. 45, 308–314 (2007).
Weehuizen, T. A. et al. Therapeutic administration of a monoclonal anti-Il-1beta antibody protects against experimental melioidosis. Shock 46, 566–574 (2016).
Koh, G. C. et al. Glyburide is anti-inflammatory and associated with reduced mortality in melioidosis. Clin. Infect. Dis. 52, 717–725 (2011).
Sarovich, D. S. et al. Recurrent melioidosis in the Darwin Prospective Melioidosis Study: improving therapies mean that relapse cases are now rare. J. Clin. Microbiol. 52, 650–653 (2014).
Teparrakkul, P. et al. Rheumatological manifestations in patients with melioidosis. Southeast Asian J. Trop. Med. Publ. Health 39, 649–655 (2008).
Molyneux, D. H., Savioli, L. & Engels, D. Neglected tropical diseases: progress towards addressing the chronic pandemic. Lancet 389, 312–325 (2017).
Teerawattanasook, N. et al. Capacity and utilisation of blood culture in two referral hospitals in Indonesia and Thailand. Am. J. Trop. Med. Hyg. 97, 1257–1261 (2017).
Skvarc, M., Stubljar, D., Rogina, P. & Kaasch, A. J. Non-culture-based methods to diagnose bloodstream infection: Does it work? Eur. J. Microbiol. Immunol. 3, 97–104 (2013).
Paek, S. C., Meemon, N. & Wan, T. T. Thailand's universal coverage scheme and its impact on health-seeking behavior. Springerplus 5, 1952 (2016).
van Dijk, D. P., Dinant, G. & Jacobs, J. A. Inappropriate drug donations: what has happened since the 1999 WHO guidelines? Educ. Health 24, 462 (2011).
Schweizer, H. P., Tuanyok, A. & Bertherat, E. Eighth World Melioidosis Congress, 2016: presenting an emerging infectious disease in the context of “One Health”. Wkly Epidemiol. Rec. 91, 543–547 (2016).
Gibbs, P. Origins of One Health and One Medicine. Vet. Rec. 174, 152 (2014).
Peacock, S. J. et al. Melioidosis vaccines: a systematic review and appraisal of the potential to exploit biodefense vaccines for public health purposes. PLoS Negl. Trop. Dis. 6, e1488 (2012).
Limmathurotsakul, D. et al. Consensus on the development of vaccines against naturally acquired melioidosis. Emerg. Infect. Dis.https://doi.org/10.3201/eid2106.141480 (2015).
Sarkar-Tyson, M. & Titball, R. W. Progress toward development of vaccines against melioidosis: A review. Clin. Ther. 32, 1437–1445 (2010).
Patel, N. et al. Development of vaccines against Burkholderia pseudomallei. Front. Microbiol. 2, 198 (2011).
Torres, A. G. et al. Protection of non-human primates against glanders with a gold nanoparticle glycoconjugate vaccine. Vaccine 33, 686–692 (2015).
Muruato, L. A. & Torres, A. G. Melioidosis: where do we stand in the development of an effective vaccine? Future Microbiol. 11, 477–480 (2016).
Lankelma, J. M. et al. The gut microbiota as a modulator of innate immunity during melioidosis. PLoS Negl. Trop. Dis. 11, e0005548 (2017).
van Crevel, R., van de Vijver, S. & Moore, D. A. J. The global diabetes epidemic: what does it mean for infectious diseases in tropical countries? Lancet Diabetes Endocrinol. 5, 457–468 (2017).
Cheng, A. C., Jacups, S. P., Gal, D., Mayo, M. & Currie, B. J. Extreme weather events and environmental contamination are associated with case-clusters of melioidosis in the Northern Territory of Australia. Int. J. Epidemiol. 35, 323–329 (2006).
Liu, C. L., Huang, J. J., Lin, H. C., Huang, S. T. & Liu, D. P. Investigation and analysis of melioidosis outbreak after Typhoon Nanmadol in Southern Taiwan, 2011. Int. J..Infect. Dis. 16, e351 (2012).
Wang, J. et al. Multiple mechanisms involved in diabetes protection by lipopolysaccharide in non-obese diabetic mice. Toxicol. Appl. Pharmacol. 285, 149–158 (2015).
Maniam, P., Nurul Aiezzah, Z., Mohamed, R., Embi, N. & Hasidah, M. S. Regulatory role of GSK3beta in the activation of NF-kappaB and modulation of cytokine levels in Burkholderia pseudomallei-infected PBMC isolated from streptozotocin-induced diabetic animals. Trop. Biomed. 32, 36–48 (2015).
Buddhisa, S., Rinchai, D., Ato, M., Bancroft, G. J. & Lertmemongkolchai, G. Programmed death ligand 1 on Burkholderia pseudomallei-infected human polymorphonuclear neutrophils impairs T cell functions. J. Immunol. 194, 4413–4421 (2015).
Koh, G. C., Peacock, S. J., van der Poll, T. & Wiersinga, W. J. The impact of diabetes on the pathogenesis of sepsis. Eur. J. Clin. Microbiol. Infect. Dis. 31, 379–388 (2012).
Liu, X. et al. Sulphonylurea usage in melioidosis is associated with severe disease and suppressed immune response. PLoS Negl. Trop. Dis. 8, e2795 (2014).
Kewcharoenwong, C. et al. Glibenclamide impairs responses of neutrophils against Burkholderia pseudomallei by reduction of intracellular glutathione. Sci. Rep. 6, 34794 (2016).
Galyov, E. E., Brett, P. J. & DeShazer, D. Molecular insights into Burkholderia pseudomallei and Burkholderia mallei pathogenesis. Annu. Rev. Microbiol. 64, 495–517 (2010). This is a review article that presents a comprehensive history of the mechanisms of pathogenesis associated with both B. pseudomallei and B. mallei (up to 2010).
Holden, M. T. et al. Genomic plasticity of the causative agent of melioidosis, Burkholderia pseudomallei. Proc. Natl Acad. Sci. USA 101, 14240–14245 (2004).
Price, E. P. et al. Within-host evolution of Burkholderia pseudomallei in four cases of acute melioidosis. PLoS Pathog. 6, e1000725 (2010).
Tumapa, S. et al. Burkholderia pseudomallei genome plasticity associated with genomic island variation. BMC Genom. 9, 190 (2008).
Chewapreecha, C. et al. Global and regional dissemination and evolution of Burkholderia pseudomallei. Nat. Microbiol. 2, 16263 (2017). This is a study in which whole-genome sequencing of 469 B. pseudomallei isolates from 30 countries maps the regional dissemination and evolution of B. pseudomallei across the globe.
Rhodes, K. A. & Schweizer, H. P. Antibiotic resistance in Burkholderia species. Drug Resist. Updat. 28, 82–90 (2016).
Bugrysheva, J. V. et al. Antibiotic resistance markers in Burkholderia pseudomallei strain Bp1651 identified by genome sequence analysis. Antimicrob. Agents Chemother. 61, e00010-17 (2017).
Chantratita, N. et al. Antimicrobial resistance to ceftazidime involving loss of penicillin-binding protein 3 in Burkholderia pseudomallei. Proc. Natl Acad. Sci. USA 108, 17165–17170 (2011).
Randall, L. B., Dobos, K., Papp-Wallace, K. M., Bonomo, R. A. & Schweizer, H. P. Membrane-bound PenA beta-lactamase of Burkholderia pseudomallei. Antimicrob. Agents Chemother. 60, 1509–1514 (2015).
Price, E. P. et al. Whole-genome sequences of Burkholderia pseudomallei isolates exhibiting decreased meropenem susceptibility. Genome Announc. 5, e00053-17 (2017).
Podnecky, N. L., Wuthiekanun, V., Peacock, S. J. & Schweizer, H. P. The BpeEF-OprC efflux pump is responsible for widespread trimethoprim resistance in clinical and environmental Burkholderia pseudomallei isolates. Antimicrob. Agents Chemother. 57, 4381–4386 (2013).
Sirijant, N., Sermswan, R. W. & Wongratanacheewin, S. Burkholderia pseudomallei resistance to antibiotics in biofilm-induced conditions is related to efflux pumps. J. Med. Microbiol. 65, 1296–1306 (2016).
Kager, L. M., van der Poll, T. & Wiersinga, W. J. The coagulation system in melioidosis: from pathogenesis to new treatment strategies. Expert Rev. Anti-Infective Ther. 12, 993–1002 (2014).
LaRosa, S. P. et al. Decreased protein C, protein S, and antithrombin levels are predictive of poor outcome in Gram-negative sepsis caused by Burkholderia pseudomallei. Int. J. Infect. Dis. 10, 25–31 (2006).
Wiersinga, W. J. et al. Activation of coagulation with concurrent impairment of anticoagulant mechanisms correlates with a poor outcome in severe melioidosis. J. Thromb. Haemost. 6, 32–39 (2008).
Kager, L. M. et al. Overexpression of activated protein C is detrimental during severe experimental gram-negative sepsis (melioidosis). Crit. Care Med. 41, e266–274 (2013).
Kager, L. M. et al. Plasminogen activator inhibitor type I contributes to protective immunity during experimental Gram-negative sepsis (melioidosis). J. Thromb. Haemost. 9, 2020–2028 (2011).
Kager, L. M. et al. Endogenous alpha2-antiplasmin is protective during severe gram-negative sepsis (melioidosis). Am. J. Respir. Crit. Care Med. 188, 967–975 (2013).
Currie, B. J. Melioidosis: The 2014 Revised RDH Guideline. Northern Territory Dis. Control Bull. 21, 4–8 (2014).
Rachlin, A. et al. Investigation of recurrent melioidosis in Lao People's Democratic Republic by multilocus sequence typing. Am. J. Trop. Med. Hyg. 94, 1208–1211 (2016).
Tauran, P. M. et al. Emergence of melioidosis in Indonesia. Am. J. Trop. Med. Hyg. 93, 1160–1163 (2015).
Rothe, C. et al. Clinical Cases in Tropical Medicine (Saunders Ltd., 2014).
Lafontaine, E. R., Balder, R., Michel, F. & Hogan, R. J. Characterization of an autotransporter adhesin protein shared by Burkholderia mallei and Burkholderia pseudomallei. BMC Microbiol. 14, 92 (2014).
DeShazer, D., Brett, P. J., Carlyon, R. & Woods, D. E. Mutagenesis of Burkholderia pseudomallei with Tn5-OT182: isolation of motility mutants and molecular characterization of the flagellin structural gene. J. Bacteriol. 179, 2116–2125 (1997).
Chua, K. L., Chan, Y. Y. & Gan, Y. H. Flagella are virulence determinants of Burkholderia pseudomallei. Infect. Immun. 71, 1622–1629 (2003).
Muangsombut, V. et al. Inactivation of Burkholderia pseudomallei bsaQ results in decreased invasion efficiency and delayed escape of bacteria from endocytic vesicles. Arch. Microbiol. 190, 623–631 (2008).
Burtnick, M. N. et al. Burkholderia pseudomallei type III secretion system mutants exhibit delayed vacuolar escape phenotypes in RAW 264.7 murine macrophages. Infect. Immun. 76, 2991–3000 (2008).
Pilatz, S. et al. Identification of Burkholderia pseudomallei genes required for the intracellular life cycle and in vivo virulence. Infect. Immun. 74, 3576–3586 (2006).
Warawa, J. & Woods, D. E. Type III secretion system cluster 3 is required for maximal virulence of Burkholderia pseudomallei in a hamster infection model. FEMS Microbiol. Lett. 242, 101–108 (2005).
Vanaporn, M., Vattanaviboon, P., Thongboonkerd, V. & Korbsrisate, S. The rpoE operon regulates heat stress response in Burkholderia pseudomallei. FEMS Microbiol. Lett. 284, 191–196 (2008).
Utaisincharoen, P., Arjcharoen, S., Limposuwan, K., Tungpradabkul, S. & Sirisinha, S. Burkholderia pseudomallei RpoS regulates multinucleated giant cell formation and inducible nitric oxide synthase expression in mouse macrophage cell line (RAW 264.7). Microb. Pathog. 40, 184–189 (2006).
Leiman, P. G. et al. Type VI secretion apparatus and phage tail-associated protein complexes share a common evolutionary origin. Proc. Natl Acad. Sci. USA 106, 4154–4159 (2009).
Basler, M., Pilhofer, M., Henderson, G. P., Jensen, G. J. & Mekalanos, J. J. Type VI secretion requires a dynamic contractile phage tail-like structure. Nature 483, 182–186 (2012).
Burtnick, M. N. et al. The cluster 1 type VI secretion system is a major virulence determinant in Burkholderia pseudomallei. Infect. Immun. 79, 1512–1525 (2011).
Chieng, S., Mohamed, R. & Nathan, S. Transcriptome analysis of Burkholderia pseudomallei T6SS identifies Hcp1 as a potential serodiagnostic marker. Microb. Pathog. 79, 47–56 (2015).
Toesca, I. J., French, C. T. & Miller, J. F. The Type VI secretion system spike protein VgrG5 mediates membrane fusion during intercellular spread by pseudomallei group Burkholderia species. Infect. Immun. 82, 1436–1444 (2014). This is an important basic science research paper from the past decade of B. pseudomallei research.
Tan, K. S. et al. Suppression of host innate immune response by Burkholderia pseudomallei through the virulence factor TssM. J. Immunol. 184, 5160–5171 (2010).
Reckseidler-Zenteno, S. L. et al. Characterization of the type III capsular polysaccharide produced by Burkholderia pseudomallei. J. Med. Microbiol. 59, 1403–1414 (2010).
Woodman, M. E., Worth, R. G. & Wooten, R. M. Capsule influences the deposition of critical complement C3 levels required for the killing of Burkholderia pseudomallei via NADPH-oxidase induction by human neutrophils. PLoS ONE 7, e52276 (2012).
Mongkolrob, R., Taweechaisupapong, S. & Tungpradabkul, S. Correlation between biofilm production, antibiotic susceptibility and exopolysaccharide composition in Burkholderia pseudomallei bpsI, ppk, and rpoS mutant strains. Microbiol. Immunol. 59, 653–663 (2015).
Norris, M. H., Schweizer, H. P. & Tuanyok, A. Structural diversity of Burkholderia pseudomallei lipopolysaccharides affects innate immune signaling. PLOS Negl Trop. Dis. 11, e0005571 (2017).
Ulrich, R. L. et al. Role of quorum sensing in the pathogenicity of Burkholderia pseudomallei. J. Med. Microbiol. 53, 1053–1064 (2004).
Chan, Y. Y. & Chua, K. L. The Burkholderia pseudomallei BpeAB-OprB efflux pump: expression and impact on quorum sensing and virulence. J. Bacteriol. 187, 4707–4719 (2005).
Cruz, A. et al. A Burkholderia pseudomallei toxin inhibits helicase activity of translation factor eIF4A. Science 334, 821–824 (2011).
Walsh, M. J., Dodd, J. E. & Hautbergue, G. M. Ribosome-inactivating proteins: potent poisons and molecular tools. Virulence 4, 774–784 (2013).
Chantratita, N. et al. Biological relevance of colony morphology and phenotypic switching by Burkholderia pseudomallei. J. Bacteriol. 189, 807–817 (2007).
Acknowledgements
W.J.W. received a Vidi grant (91716475) from the Netherlands Organisation for Scientific Research (NWO) and Marie Curie Skledowska Innovative Training Network (MC-ITN) European Sepsis Academy, funded by the European Union's Horizon 2020 programme. H.S.V. received a Marie Curie Skledowska fellowship under the European Sepsis Academy, funded by the European Union's Horizon 2020 programme. A.G.T. is supported by the NIH and the National Institute of Allergy and Infectious Diseases (NIAID) R01 grant AI12660101. B.J.C. is supported by Australian National Health and Medical Research Council grants, including the HOT NORTH initiative. S.J.P. is an NIH Research Senior Investigator. D.A.B.D. is supported by The Wellcome Trust of Great Britain (grant number 106698/Z/14/Z). D.L. is supported by The Wellcome Trust Public Health and Tropical Medicine Intermediate Fellowship (grant number 101103/Z/13/Z). The authors thank G. Wongsuvan, P. Amornchai, P. Wannapinij and V. Wuthiekanun for their assistance with the images in Fig. 5.
Author information
Authors and Affiliations
Contributions
Introduction (H.S.V. and W.J.W.); Epidemiology (D.L. and D.A.B.D.); Mechanisms/pathophysiology (H.S.V., W.J.W., A.G.T. and S.J.P.); Diagnosis, screening and prevention (D.A.B.D., D.L. and B.J.C.); Management (B.J.C.); Quality of life (B.J.C.); Outlook (A.G.T., H.S.V., D.A.B.D., D.L. and W.J.W.); Overview of Primer (all authors).
Corresponding authors
Ethics declarations
Competing interests
D.A.B.D. acted as a consultant to Soligenix, Inc. All other authors declare no competing interests.
Rights and permissions
About this article
Cite this article
Wiersinga, W., Virk, H., Torres, A. et al. Melioidosis. Nat Rev Dis Primers 4, 17107 (2018). https://doi.org/10.1038/nrdp.2017.107
Published:
Version of record:
DOI: https://doi.org/10.1038/nrdp.2017.107
This article is cited by
-
Concurrent resistance and virulence traits in extremely drug-resistant Burkholderia pseudomallei from bovine milk samples: potential for zoonotic transmission
Veterinary Research Communications (2026)
-
Diagnostic accuracy of non-culture methods for the diagnosis of melioidosis: a systematic review and meta-analysis
BMC Infectious Diseases (2025)
-
A rare case of cutaneous melioidosis manifesting as infective panniculitis: a case report
BMC Infectious Diseases (2025)
-
Neonatal patients with melioidosis: a systematic review
BMC Infectious Diseases (2025)
-
Phage-mediated control of melioidosis in Southern China: molecular insights and therapeutic potential of N4-like viruses from Hainan
BMC Microbiology (2025)