Abstract
Gastric cancer (GC) is among the most common malignancy in the world with poor prognosis and limited treatment options. It has been established that gastric carcinogenesis is caused by a complex interaction between host and environmental factors. Copy number variation (CNV) refers to a form of genomic structural variation that results in abnormal gene copy numbers, including gene amplification, gain, loss and deletion. DNA CNV is an important influential factor for the expression of both protein-coding and non-coding genes, affecting the activity of various signaling pathways. CNV arises as a result of preferential selection that favors cancer development, and thus, targeting the amplified 'driver genes' in GC may provide novel opportunities for personalized therapy. The detection of CNVs in chromosomal or mitochondrial DNA from tissue or blood samples may assist the diagnosis, prognosis and targeted therapy of GC. In this review, we discuss the recent CNV discoveries that shed light on the molecular pathogenesis of GC, with a specific emphasis on CNVs that display diagnostic, prognostic or therapeutic significances in GC.
Similar content being viewed by others
Introduction
Gastric cancer (GC) is the fifth most common malignancy and the third leading cause of cancer death worldwide.1, 2 With a 5-year survival rate merely ranging from 25 to 35% in advanced GC,3, 4, 5 more than 1.1 million patients die from GC every year.6 Although the decrease of incidence and mortality rates in GC has been reported because of a lower prevalence of Helicobacter pylori (Hp), lower salt intake and a higher consumption of fresh fruits and vegetables,7 GC still remains a main clinical challenge as many cases are diagnosed in advanced stages with limited treatment options and poor prognosis.8 Although therapeutic methods are improving in surgical combined with radiotherapy and chemotherapy, the benefits for advanced GC are still not optimistic. The improvements in early diagnosis and the treatment of the GC may continue to be the most effective strategy for improving patient survival. Thus, seeking for more sensitive detecting approaches and effective drugs, particularly those targeting cancer progression mechanisms, is urgently needed.
A recent phase III randomized study (ToGA) revealed that the addition of trastuzumab to chemotherapy improved survival in patients with advanced GC with HER2 gene amplification.9 It not only laid the foundation of gene detection in the diagnosis and treatment of GC, but also indicates the potential effect of targeted therapy against gene copy number variations (CNVs) in GCs.10, 11
CNV refers to a form of genomic structural variation that results in abnormal or, for certain genes, a normal variation in the number of copies of one or more sections of the DNA.12 DNA CNVs include gene amplification, gain, loss and deletion. In addition to gene mutation, CNV has a significant role in tumorigenesis in many cancers, such as GC,13 ovarian cancer,14 hepatocellular carcinoma,15 testicular germ cell tumors,16 colorectal carcinoma,17 bladder cancer18 and so on. The accumulation of CNVs during gastric oncogenesis may be a result of preferential selection by which transforming cells gain evolutionary advantage. The copies of apoptosis effector genes are often lost during cancer development, in comparison with the frequent amplification of proliferation-related genes.19 A recent study on 183 primary GC samples suggested that some established or potential anticancer drug target genes exhibited high levels of CNVs, including HER2, TUBB3 and TOP2A.20 Given the indicative value of CNVs in deregulated signaling pathways, CNV may provide useful information for the molecular subtyping of GC and optimization of therapeutic strategies.21 Increasing evidence showed that CNV genes are promising biomarkers and therapeutic targets in GC, which can be detected by various methods including flourescence in situ hybridization, array comparative genomic hybridization and single nucleotide polymorphism arrays.
Although a number of review articles have focused on the roles of specific genes that are relevant to molecular pathogenesis or targeted therapy of GC,22, 23 a systematic review with respect to gene CNVs in GC has not been provided.24 In this review, we discuss the recent CNV researches that shed light on the molecular pathogenesis of GC, with a specific emphasis on CNVs and associated genes that display biomarker potentials in GC.
GC involves CNVs and other genetic aberrations
GC is a very complex and heterogeneous disease, which is a multistep process involving deregulation of many oncogenic pathways. Adenocarcinoma is the major histological type of GC, in possession of 90–95% of all gastric malignancies. According to Lauren classification, adenocarcinomas are divided into two distinct pathological entities, intestinal and diffuse types, while the latter has a more aggressive behavior and worse prognosis than the former.25 Gastric carcinogenesis is considered as a result of a complex interaction between inheritance and environmental factors. In addition to hereditary predispositions, GC is also associated with Hp infection,26, 27, 28 obesity, nutritional supplement29 and certain dietary structures, such as high salt diet, food content with nitrates and smoked meats.30 Exposure to those risk factors for a long time will eventually result in cancer through a multistep process.31 Of note, the infection of Hp is associated with certain features of CNVs in GC. As an example, the loss of 16p occurs in 10% of the Hp-negative samples compared with 0% in the Helicobacter-positive samples, whereas the gain or amplification in 16p gain can be found in up to 14.71% of Hp-positive samples but only in 3.33% of the Hp-negative samples.32
The initiation and progression of GC involve deregulation of different signaling pathways by genetic and epigenetic alterations.33, 34, 35 Genetic alterations, such as gene mutations, CNVs and chromosomal translocations, could also influence the expression of tumor-suppressor genes, oncogenes and other genes, ultimately contributing to gastric carcinogenesis.36 In recent years, many micro-RNA (miRNAs) have been supposed as oncogenes or tumor suppressors by altering the expression of target genes participated in multiple steps of primary and metastasis GC, which are related to gene deletions, mutations, promoter hypermethylation or histone acetylation as well as other mechanisms.37, 38
CNVs affect both protein-coding and non-coding genes
Previous researches have revealed numerous chromosomal DNA gains and losses in GC patients, with the former far more prevalent than the latter. Recent high-throughput studies identified gains of 3p22, 4q25, 8q24, 11p13 and 20q13, as well as losses of 1p36 and 9p21 where many cancer-related genes (CTNNB1, MYC, CDKN2A, TOP2A and so on) are located.39, 40 DNA CNVs are significant influential factors for gene expression, which may affect the activities of different oncogenic or tumor-suppressing pathways. This may explain the clinical relevance of many CNVs in GC. It has been reported that GC patients with lymph node metastasis have remarkably higher numbers of gains, losses and total CNVs than those cases without metastasis. In addition, another research indicated that frequent gains observed on chromosomes 1q, 5p, 7, 8, 13 and 20 and losses observed on chromosomes 1p, 3p, 4, 5q, 9p, 17p, 18q, 19p, 21 and 22.41 Although an increased number of CNV regions have been identified in GC,42 it still requires further investigation which of the affected genes may have functional roles in GC.13, 43
Most previous studies have focused on protein-coding genes in CNV regions, but it is increasingly likely that the expression levels of long non-coding RNAs and miRNAs are also influenced by CNVs. A recent study by Fang, Xu and colleagues44 revealed that one-third of aberrantly expressed long non-coding RNAs are associated with CNVs in the GC genome. Because long non-coding RNAs may have causative roles in oncogenesis,45 it deserves further investigation whether CNV-associated long non-coding RNAs may have oncogenic roles and present diagnostic or prognostic significance in GC. Moreover, recent studies have demonstrated that miRNA deregulation caused by CNVs may contribute to gastric oncogenesis.45 As discussed above, CNVs are clustered in different chromosomal regions and may affect the expression of different types of genes, therefore contributing to gastric oncogenesis. In the following paragraphs, we will discuss significant CNVs in GC according to their locations in the genome (from different chromosomes to mitochondrial DNA (mtDNA)).
Chromosome 3
PIK3CA gene, which is located on chromosome 3q26.3, is frequently amplified in GC.46 Importantly, the overexpression of PIK3CA resulted from gene amplification increased PI3-kinase activity and phosphorylated Akt level, contributing to aberrant cell proliferation and apoptosis which are directly associated with tumorigenesis (schematic representation in Figure 1).47 Furthermore, PIK3CA amplification notably influenced the overall prognosis in GC regardless of early or late stage tumors, suggesting that this genetic event has an important role in the multistep process of gastric carcinogenesis.48, 49 Taken together, PIK3CA may function as a GC driver with independent prognostic significance.
An overview of CNV-affected genes in association with signaling pathways, pathological features and therapeutic targets in GC. The genes on CNV regions have been highlighted either in red (indicating gain or amplification) or green (loss or deletion). Their relationships with different signaling pathway have been shown with arrows. In addition, the relevance to disease features ('R'), targeted therapy ('T') and oncogenic functions ('F') have also been labeled for each gene. The signaling pathways related to the receptor tyrosine kinase genes (MET, EGFR, FGFR2 and HER2) have been labeled in the graph.
In addition, Yoshida et al.50 detected that ribosomal protein S6 kinase2 (S6K2) amplification was associated with poor prognosis, and S6K2 may function as an upstream driver gene leading to deregulation of mammalian target of rapamycin (mTOR) in GC. Beyond that, Shinmura et al.51 suggested that TNK2 (locate on 3q29) amplification may be an independent indicator of poor prognosis in GC patients, contributing to an increase in the malignant potential.
Chromosome 5
The adenomatous polyposis coli (APC), a tumor-suppressor gene, located on 5q21-q22, has a critical role in several cellular processes including microtubule polymerization, signal transduction and cell adhesion.52 Its protein product negatively regulates WNT signaling and its inactivation leads to β-catenin accumulation and transcriptional activation of genes (MYC, cyclin D1) related to cell proliferation.53, 54 As reported, the chromosome locus of APC is frequently deleted in GCs,55, 56, 57, 58, 59 and its decreased copy number significantly associated with lymph node invasion and metastasis in GC patients.55 Moreover, APC deletion was principally found in advanced GCs, suggesting that it might be involved in the progression but not initiation of GCs. Furthermore, in a study concerning 131 sporadic gastric adenocarcinoma samples with matched normal tissues, Fang et al.60 demonstrated APC copy number deletions were found in a relatively high percentage (25.9%) and were associated with lymph node invasion or metastasis of GC.
The IRX1 tumor-suppressor gene is located on 5p15.33, a cancer susceptibility locus which is frequently deleted in GC.61 IRX1 expression suppresses cell proliferation, invasion, migration and oncogenesis both in vitro and in vivo. Guo et al.62 also confirmed the deletion of IRX1 gene and the crucial functions of IRX1 as a tumor suppressor in GC. In addition to gene copy number deletion, the expression level of IRX1 in GC also correlates with promoter methylation.61
Chromosome 7
MET locates on chromosome 7q21 that codes the hepatocyte growth factor receptor. The hepatocyte growth factor/MET pathway dysfunction has been observed in GC and many other human cancers.63 In GC, the activation of MET signaling is mainly caused by MET amplification,64 causing increased tumor cell growth, invasion and angiogenesis.63, 65, 66
The amplification of MET gene has been found in 0–23% of GCs, and is associated with advanced disease stages or worse clinical outcome.67, 68, 69, 70 In addition, a recent report showed MET gene amplification significantly associated with mRNA overexpression and poor GC patient survival.71 MET gene copy number amplification was also significantly associated with the depth of tumor invasion, metastasis and poor prognosis, suggesting it may be more valuable as a prognostic marker than protein overexpression.72 The clinical impact of MET amplification is highly consistent with the role of MET as a functional driver gene in GC. Recent studies have suggested that MET CNVs may serve as a selectable marker for MET inhibitor therapy. MET amplification labels a subgroup of GC patients who are susceptible to MET-TKIs.66, 73 In addition, the investigation of volitinib as a therapeutic option for GC patients points out a strong rationale for selecting patients harboring amplified MET.74 In future clinical studies, the effectiveness of MET amplification as a marker for treatment response should be further explored.69
Epidermal growth factor receptor (EGFR) resides on chromosome 7p12 and encodes a receptor tyrosine kinase ErbB and the other members are HER2, HER3 and HER4 (signaling related to receptor tyrosine kinases are shown in Figure 1).75 Inhibition of EGFR contributes to cell division, migration and apoptosis in GC.76, 77 EGFR copy number gains associate with an increased risk of invasion and metastasis in solid tumors including GC, suggesting its potential significance as a prognostic marker.78, 79, 80, 81 As reported, there is a strong relationship between EGFR gene copy number, protein expression and chromosome 7 polisomy.82 Oh et al.83 further observed that EGFR CNVs existed in a series of GC cases and discovered that it was associated with unfavorable prognosis. Another study based on 855 cases reported that gained EGFR gene copy can be found in 22.7% of GC patients, and it associates with poor disease outcome.84 These data collectively demonstrate that EGFR CNV may be a valuable biomarker for GC.
Chromosome 8
The c-MYC gene is located in this chromosome at the 8q24.1 band, encoding a transcriptional factor that regulates genes related to proliferation, differentiation and apoptosis. The deregulation of c-MYC has been considered as one of the main events in the pathogenesis of many cancers, including GC.85, 86 Many studies reported that a significant increase in MYC copy number can be detected in the carcinogenic process of GC and in gastric cell lines.87, 88, 89, 90, 91, 92 The amplification of MYC has also been suggested with independent prognostic value on overall survival.93 In addition, MYC CNVs has a tight connection with the clinicopathological features of GC. Wang et al.94 reported that gained copy number in MYC or TNFRSF11B (located at 8q24) genes strongly associated with the depth of lymph node metastasis, invasion and TNM stages. In another study, MYC amplification significantly correlated with MYC mRNA levels and MYC immunoreactivity, suggesting that MYC CNV indeed contributes to its overexpression in GC.95 In mucinous gastric carcinoma, c-MYC amplification was correlated with greater invasion depth and advanced tumor stage, while these differences were not found in non-mucinous gastric carcinomas, suggesting that c-MYC amplification in mucinous gastric carcinoma may be a genetic alteration contributing to the frequent presentation of advanced stage of MGC.96
The POU5F1B gene (POU domain class 5 transcription factor 1B, the OCT4 pseudogene), which is located on human chromosome 8q24 near MYC,97 is frequently amplified in GC. Hayashi et al.98 detected that POU5F1B copy number is amplified and overexpressed in GC, and it also promotes tumorigenicity and tumor growth. Therefore, POU5F1B amplification seems to be a GC-associated event that has oncogenic roles.
Chromosome 17
HER2 is located on human chromosome 17q21 and is a member of the EGFR family. Once bounded to its ligand, Her-2 is phosphorylated and it functions as a tyrosine kinase that promotes cell proliferation.99 The reported HER2 amplification in patients with GC ranged from 6 to 23%, and amplified HER2 gene was mostly associated with poor outcome.100, 101 HER2 gene amplification was significantly correlated with the depth of invasion, lymphatic metastasis and the TNM stage.102, 103 A recent report demonstrated H. pylori CagA may induce overexpression of the Her2 protein by increasing HER2 DNA copy number,104 thus adding to the connection between environmental factors and genomic aberrations. As high incidence of intratumoral HER2 heterogeneity has been reported, it is important to detect HER2 gene status with larger tissue samples.42, 105 Many methods for detecting HER2 CNVs, including flourescence in situ hybridization, in situ hybridization, chromogenic in situ hybridization and silver in situ hybridization, have been demonstrated as effective approaches.42, 101, 106 Moreover, the HER2:chr17 (chromosome 17) ratio may be an additional index to eliminate incorrect HER2 status determination in GC.107
The utilization of molecularly targeted therapeutics against HER2 has emerged as a significant strategy for advanced GCs. Trastuzumab, a monoclonal antibody targeting HER2, induces cellular cytotoxicity and inhibits HER2-mediated signaling pathways.108 This HER2 antibody has been tested by a randomized clinical trial (ToGA), which reported prolonged survival time of patients with advanced GC after combined with chemotherapy.9, 109 The European Medicines Agency has also approved trastuzumab in association with chemotherapy for the treatment of metastatic gastric adenocarcinoma with minor modifications of the ToGA trial criteria.110
TP53 gene mapped on 17p13.1 encodes a master regulator of genomic stability.111, 112 In response to DNA damage, the p53 protein triggers multiple cellular responses, including cell cycle arrest, DNA repair and apoptosis, cellular differentiation, metabolism, angiogenesis and the immune response.113, 114, 115 In the carcinogenic progression of GC, loss of the TP53 locus is one of the most common mechanisms involved in this gene dysfunction and is frequently found in GC.87, 88, 90, 116 A significant correlation has been found between loss of TP53 and gastric precancerous lesions, suggesting that TP53 CNV may be an early event in gastric carcinogenesis.117
Chromosome 20
The centrosome-associated kinase aurora A (AURKA) gene is located on chromosome locus of 20q13, encoding the Aurka protein that is ubiquitously expressed and regulates cell cycle events emerging from late S-phase through the M phase.118 In addition, AURKA overexpression results in the activation of several carcinogenic pathways including PI3K/AKT, β-catenin, NF-kB and JAK2-STAT3.119 Accumulating data revealed that AURKA was frequently amplified and overexpressed in GC,36, 120, 121, 122 and AURKA amplification associated with significantly worse survival.123 A recent study showed copy number gains of AUKRA were detected in a relative high percentage of GC samples (30.5%). A positive connection has been found between AURKA amplification and tumor progression,124 suggesting that AURKA may have prognostic significance.
The amplification and gain of C20orf11 gene at 20q13.33 almost discriminated moderately differentiated GC from poorly differentiated type,125 and C20orf11 CNV is correlated with TNM stages and histological subtypes of GC. It is helpful in highlighting this interesting gene as a potential marker for the differentiation status of GC.
CNVs on other chromosomes
The octamer transcription factor 1 (OCT1) gene locates on human chromosome 1, encoding Oct1 protein that belongs to the POU homeodomain family of transcription factors.126 Interestingly, OCT1 shares similar downstream target genes as the OCT4 pluripotent factor, and OCT1 has been reported as a determinant of somatic and cancer stem cells.127 High expression of OCT1 could activate synbindin, which promotes ERK phosphorylation on the Golgi apparatus.128, 129 An recent study revealed that OCT1 overexpression by amplification triggers synbindin-mediated ERK signaling and increases the aggressiveness of GC cells. The amplification, mRNA and protein overexpression of OCT1 were consistently correlated with poor survival of GC patients.130 These findings suggest that OCT1 may function as an oncogenic driver in GC, and it may be a promising diagnostic and prognostic marker for this deadly disease.
Kang et al.131 successfully identified the AMY2A gene as a 1p21.1 homozygous deletion target in GC. It is considered that the AMY2A gene may function as a tumor suppressor. Gastrokine 1 (GKN1), located on chromosome 2p13.3, has been found as a potent tumor suppressor that regulates gastric epithelial cell growth.132 Loss of GKN1 gene copy number has been frequently observed in GC,133 suggesting that GKN1 inactivation may be involved in GC development.
FGFR2 gene locates on 10q26, and amplifications of FGFR2 (reported in 4–10% of GC) associates with poor prognosis in diffuse type GC.134, 135 FGFR2 encodes a receptor tyrosine kinase regulating cell growth and development.136 FGFR2 amplification was detected in 4.1% GC using formalin-fixed paraffin-embedded samples, which associated with poorer outcome. In addition, the development of FGFR2 inhibitors for the treatment of GC in consideration of FGFR2 amplification has been proposed.137
The variously sized 11q13.3 amplicon containing cyclin D1 (CCND1) and oral cancer overexpressed 1 (ORAOV1) are among the most frequent amplification events in GC.138, 139 The oncogenic role of CCND1 in GC is supported by its function on gearing the cell cycle from G1 phase to S phase.140 Stahl et al.141 found that CCND1 amplification often represents an early event during tumor development. Another study also suggest that the CCND1 gene may have a critical role in the development or progression of GC.142 Kang et al.142 reported that the ORAOV1 gene at the 11q13.3 region is associated with lymphatic metastasis, suggesting that ORAOV1 may have prognostic significance in GC.
Interestingly, it has been reported that miR-23a in amplified 19p13.13 loci targets metallothionein 2 A (MT2A) and promotes growth in GC cells.143 By integrating CNV and miRNA profiles in the same samples, the authors identified eight miRNAs (miR-1274a, miR-196b, miR-4298, miR-181c, miR-181d, miR-23a, miR-27a and miR-24-2) that were located in the amplified regions and were upregulated in GC. The amplification of miRNAs were confirmed by real-time PCR and in situ hybridization assays. Knockdown of miR-23a expression neutralized the effect of CNV and inhibited GC cell proliferation, suggesting potential therapeutic value of CNV-associated miRNAs in GC.
Mitochondrial DNA (mtDNA)
Human mtDNA is a 16.6 kb double-stranded circular DNA molecule, with a range of few hundreds to several thousands copies of mtDNA present in each cell, encoding 13 polypeptides of respiratory enzyme complexes, transfer RNAs and 2 ribosomal RNAs required for protein synthesis in mitochondria.144 Several somatic mutations in the mtDNA have been observed in GCs, including a very large deletion of 4977 bp and mutations in the D-loop region.145 Mitochondrial dysfunction by mtDNA somatic mutations and CNVs might have an important role in the malignant progression of GC owing to its important roles in energy production, cell metabolism and apoptosis.146 MtDNA copy number losses and point mutations are the two most common type of mtDNA alterations in GCs.147 Significant efforts have been made to develop therapeutic strategies by targeting mitochondria in cancers.148, 149
Interestingly, Fernandes et al.150 discovered that mtDNA quantification approaches by blood sampling would allow an early detection of GC, suggesting the diagnostic potential of mtDNA CNV. In addition, Wen et al.151 demonstrated that the mtDNA copy number deletion may be particularly notable in ill-defined GCs of clinicopathological stages III and IV.
Methods for discovering cancer-driver genes with CNVs
One major challenge in genome-wide CNV research is to identify cancer-driver genes that cause functional abnormalities. In recent studies, efforts have been made to pinpoint cancer-driver genes by combining cancer genomic data including gene CNVs, mutations and expression levels. The dominant effects of cancer-driver genes (DEOD) algorithm has been developed based on a partial covariance selection approach, which builds a gene network based on the above-mentioned data types.152 In comparison, the DawnRank algorithm was designated to identify personalized driver genes in cancer.153 Along with the expansion in cancer genomic datasets and continuous improvement of data-mining methods, the identification of cancer-driver genes may bring enormous therapeutic opportunities in the future.
Conclusions
GC is a complex, multistep process that involves aberrant CNV events in different genomic regions. Frequently occurring CNVs in GC result from preferential selections that favor the oncogenic process, thus the CNV-associated genes should be further characterized for their roles in gastric oncogenesis. Given the rich information that CNVs may provide in regard to disease signaling patterns and clinicopathological features, future studies in this field would provide enomous mechanistic insights and facilitate the development of novel biomarkers for this deadly disease. Challenges in accurate detection of CNV in the presence of intratumoral heterogeneity should be further tackled to obtain highly confident CNV information for guiding GC diagnosis, prognosis and targeted therapy.
References
Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 2015; 136: E359–E386.
Chen W, Zheng R, Zhang S, Zhao P, Zeng H, Zou X . Report of cancer incidence and mortality in China, 2010. Ann Transl Med 2014; 2: 61.
Waddell T, Chau I, Cunningham D, Gonzalez D, Frances A, Okines C et al. Epirubicin, oxaliplatin, and capecitabine with or without panitumumab for patients with previously untreated advanced oesophagogastric cancer (REAL3): a randomised, open-label phase 3 trial. Lancet Oncol 2013; 14: 9.
Lordick F, Kang YK, Chung HC, Salman P, Oh SC, Bodoky G et al. Capecitabine and cisplatin with or without cetuximab for patients with previously untreated advanced gastric cancer (EXPAND): a randomised, open-label phase 3 trial. Lancet Oncol 2013; 14: 10.
Smalley SR, Benedetti JK, Haller DG, Hundahl SA, Estes NC, Ajani JA et al. Updated Analysis of SWOG-Directed Intergroup Study 0116:A Phase III Trial of Adjuvant Radiochemotherapy Versus Observation After Curative Gastric Cancer Resection. J Clin Oncol 2012; 30: 7.
Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM . Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 2010; 127: 2893–2917.
Siegel RL, Miller KD, Jemal A . Cancer statistics, 2015. CA Cancer J Clin 2015; 65: 5–29.
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A . Global cancer statistics, 2012. CA Cancer J Clin 2015; 65: 87–108.
Bang YJ, Van Cutsem E, Feyereislova A, Chung HC, Shen L, Sawaki A et al. Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): A phase 3, open-label, randomised controlled trial. Lancet 2010; 376: 11.
Xie L, Su X, Zhang L, Yin X, Tang L, Zhang X et al. FGFR2 gene amplification in gastric cancer predicts sensitivity to the selective FGFR inhibitor AZD4547. Clin Cancer Res 2013; 19: 2572–2583.
Okamoto W, Okamoto I, Arao T, Kuwata K, Hatashita E, Yamaguchi H et al. Antitumor action of the MET tyrosine kinase inhibitor crizotinib (PF-02341066) in gastric cancer positive for MET amplification. Mol Cancer Ther 2012; 11: 1557–1564.
Nakamura Y . DNA variations in human and medical genetics: 25 years of my experience. J Hum Genet 2009; 54: 1–8.
Leary RJ, Lin JC, Cummins J, Boca S, Wood LD, Parsons DW et al. Integrated analysis of homozygous deletions, focal amplifications, and sequence alterations in breast and colorectal cancers. Proc Natl Acad Sci USA 2008; 105: 16224–16229.
Despierre E, Moisse M, Yesilyurt B, Sehouli J, Braicu I, Mahner S et al. Somatic copy number alterations predict response to platinum therapy in epithelial ovarian cancer. Gynecol Oncol 2014; 135: 415–422.
Xu H, Zhu X, Xu Z, Hu Y, Bo S, Xing T et al. Non-invasive analysis of genomic copy number variation in patients with hepatocellular carcinoma by next generation DNA sequencing. J Cancer 2015; 6: 247–253.
Silveira SM, da Cunha IW, Marchi FA, Busso AF, Lopes A, Rogatto SR . Genomic screening of testicular germ cell tumors from monozygotic twins. Orphanet J Rare Dis 2014; 9: 9.
Horpaopan S, Spier I, Zink AM, Altmuller J, Holzapfel S, Laner A et al. Genome-wide CNV analysis in 221 unrelated patients and targeted high-throughput sequencing reveal novel causative candidate genes for colorectal adenomatous polyposis. Int J Cancer 2015; 136: E578–E589.
Bonberg N, Pesch B, Behrens T, Johnen G, Taeger D, Gawrych K et al. Chromosomal alterations in exfoliated urothelial cells from bladder cancer cases and healthy men:a prospective screening study. BMC Cancer 2014; 14: 11.
Mauro JA, Butler SN, Ramsamooj M, Blanck G . Copy number loss or silencing of apoptosis-effector genes in cancer. Gene 2015; 554: 50–57.
Labots M, Buffart TE, Haan JC, van Grieken NC, Tijssen M, van de Velde CJ et al. High-level copy number gains of established and potential drug target genes in gastric cancer as a lead for treatment development and selection. Cell Oncol 2014; 37: 41–52.
Niels TF, Anja B, Jan TJ . The HER2 CISH pharmDx™ Kit in the assessment of breast cancer patients for anti-HER2 treatment. Expert Rev Mol Diagn 2013; 13: 10.
Shi J, Qu Y-P, Hou P . Pathogenetic mechanisms in gastric cancer. World J Gastroenterol 2014. 20.
Figueiredo C, Garcia-Gonzalez MA, Machado JC . Molecular pathogenesis of gastric cancer. Helicobacter 2013; 18: 28–33.
Park CH, Rha SY, Jeung HC, Kang SH, Ki DH, Lee WS et al. Identification of novel gastric cancer-associated CNVs by integrated analysis of microarray. J Surg Oncol 2010; 102: 454–461.
Piazuelo MB, Correa P . Gastric cancer: Overview. Colomb Med 2013; 44: 10.
Zhang L, Sung JJ, Yu J, Ng SC, Wong SH, Cho CH et al. Xenophagy in Helicobacter pylori- and Epstein-Barr virus-induced gastric cancer. J Pathol 2014; 233: 103–112.
Hatakeyama M . Helicobacter pylori CagA and gastric cancer: a paradigm for hit-and-run carcinogenesis. Cell Host Microbe 2014; 15: 306–316.
Ferreira RM, Machado JC, Figueiredo C . Clinical relevance of Helicobacter pylori vacA and cagA genotypes in gastric carcinoma. Best Pract Res Clin Gastroenterol 2014; 28: 1003–1015.
Sun K, Chen S, Xu J, Li G, He Y . The prognostic significance of the prognostic nutritional index in cancer: a systematic review and meta-analysis. J Cancer Res Clin Oncol 2014; 140: 1537–1549.
Ang TL, Fock KM . Clinical epidemiology of gastric cancer. Singapore Med J 2014; 55: 621–628.
Bornschein J, Kandulski A, Selgrad M, Malfertheiner P . From gastric inflammation to gastric cancer. Dig Dis 2010; 28: 609–614.
Fan B, Dachrut S, Coral H, Yuen ST, Chu KM, Law S et al. Integration of DNA copy number alterations and transcriptional expression analysis in human gastric cancer. PloS One 2012; 7: e29824.
Takeshima H, Niwa T, Takahashi T, Wakabayashi M, Yamashita S, Ando T et al. Frequent involvement of chromatin remodeler alterations in gastric field cancerization. Cancer Lett 2015; 357: 328–338.
Yoda Y, Takeshima H, Niwa T, Kim JG, Ando T, Kushima R et al. Integrated analysis of cancer-related pathways affected by genetic and epigenetic alterations in gastric cancer. Gastric Cancer 2015; 18: 65–76.
Katoh M . Therapeutics targeting angiogenesis: genetics and epigenetics, extracellular miRNAs and signaling networks (Review). Int J Mol Med 2013; 32: 763–767.
Hudler P . Genetic aspects of gastric cancer instability. ScientificWorldJournal 2012; 2012: 10.
Xia J, Guo X, Yan J, Deng K . The role of miR-148a in gastric cancer. J Cancer Res Clin Oncol 2014; 140: 1451–1456.
Shi ZQ, Wei QX, She JJ . MicroRNAs in gastric cancer metastasis. Crit Rev Eukaryot Gene Expr 2014; 24: 14.
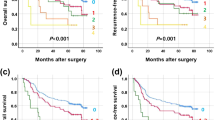
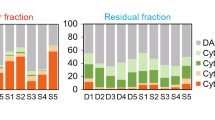
Deng N, Goh LK, Wang H, Das K, Tao J, Tan IB et al. A comprehensive survey of genomic alterations in gastric cancer reveals systematic patterns of molecular exclusivity and co-occurrence among distinct therapeutic targets. Gut 2012; 61: 673–684.
Zhang D, Wang Z, Luo Y, Xu Y, Liu Y, Yang W et al. Analysis of DNA copy number aberrations by multiple ligation-dependent probe amplification on 50 intestinal type gastric cancers. J Surg Oncol 2011; 103: 124–132.
Wang K, Yuen ST, Xu J, Lee SP, Yan HH, Shi ST et al. Whole-genome sequencing and comprehensive molecular profiling identify new driver mutations in gastric cancer. Nat Genet 2014; 46: 573–582.
Kiyose S, Igarashi H, Nagura K, Kamo T, Kawane K, Mori H et al. Chromogenic in situ hybridization (CISH) to detect HER2 gene amplification in breast and gastric cancer: comparison with immunohistochemistry (IHC) and fluorescence in situ hybridization (FISH). Pathol Int 2012; 62: 728–734.
Krepischi ACV, Pearson PL, Rosenberg C . Germline copy number variations and cancer predisposition. Future Oncol 2012; 8: 10.
Hu Y, Wang J, Qian J, Kong X, Tang J, Wang Y et al. Long noncoding RNA GAPLINC regulates CD44-dependent cell invasiveness and associates with poor prognosis of gastric cancer. Cancer Res 2014; 74: 6890–6902.
Hu L, Wu Y, Tan D, Meng H, Wang K, Bai Y et al. Up-regulation of long noncoding RNA MALAT1 contributes to proliferation and metastasis in esophageal squamous cell carcinoma. J Exp Clin Cancer Res 2015; 34: 7.
Samuels Y, Wang Z, Bardelli A, Silliman N, Ptak J, Szabo S et al. High frequency of mutations of the PIK3CA gene in human cancers. Science 2004. 304.
Shi J, Yao D, Liu W, Wang N, Lv H, Zhang G et al. Highly frequent PIK3CA amplification is associated with poor prognosis in gastric cancer. BMC Cancer 2012; 12: 50.
Yang Q, Shao Y, Shi J, Qu Y, Wu K, Dang S et al. Concomitant PIK3CA amplification and RASSF1A or PAX6 hypermethylation predict worse survival in gastric cancer. Clin Biochem e-pub ahead of print 25 October 2013. doi: 10.1016/j.clinbiochem.2013.10.014.
Takahashi N, Yamada Y, Taniguchi H, Fukahori M, Sasaki Y, Shoji H et al. Clinicopathological features and prognostic roles of KRAS, BRAF, PIK3CA and NRAS mutations in advanced gastric cancer. BMC Res Notes 2014; 7: 271.
Yoshida S, Matsumoto K, Arao T, Taniguchi H, Goto I, Hanafusa T et al. Gene amplification of ribosomal protein S6 kinase-1 and -2 in gastric cancer. Anticancer Res 2013; 33: 469–475.
Shinmura K, Kiyose S, Nagura K, Igarashi H, Inoue Y, Nakamura S et al. TNK2 gene amplification is a novel predictor of a poor prognosis in patients with gastric cancer. J Surg Oncol 2014; 109: 189–197.
Li Z, Li W, Song L, Zhu W . Cilia adenomatous polyposis coli and associated diseases. Oncogene 2012; 31: 1475–1483.
Gray SE, Kay EW, Mary L, Mabruk M . Analysis of APC allelic imbalance/loss of heterozygosity and APC protein expression in cutaneous squamous cell carcinomas. Cancer Genomics Proteomics 2011. 8.
Bria E, De Manzoni G, Beghelli S, Tomezzoli A, Barbi S, Di Gregorio C et al. A clinical-biological risk stratification model for resected gastric cancer: prognostic impact of Her2, Fhit, and APC expression status. Ann Oncol 2013; 24: 693–701.
Tsai PC, Huang SW, Tsai HL, Ma CJ, Hou MF, Yang LP et al. The association between DNA copy number aberrations at chromosome 5q22 and gastric cancer. PLoS One 2014. 9.
Buffart TE, Carvalho B, van Grieken NC, van Wieringen WN, Tijssen M, Kranenbarg EM et al. Losses of chromosome 5q and 14q are associated with favorable clinical outcome of patients with gastric cancer. Oncologist 2012; 17: 653–662.
Qian Z, Zhu G, Tang L, Wang M, Zhang L, Fu J et al. Whole genome gene copy number profiling of gastric cancer identifies PAK1 and KRAS gene amplification as therapy targets. Genes Chromosomes Cancer 2014; 53: 883–894.
Chang VY, Federman N, Martinez-Agosto J, Tatishchev SF, Nelson SF . Whole exome sequencing of pediatric gastric adenocarcinoma reveals an atypical presentation of Li-Fraumeni syndrome. Pediatr Blood Cancer 2013; 60: 570–574.
Lee J, van Hummelen P, Go C, Palescandolo E, Jang J, Park HY et al. High-throughput mutation profiling identifies frequent somatic mutations in advanced gastric adenocarcinoma. PLoS One 2012; 7: e38892.
Fang Z, Xiong Y, Li J, Liu L, Zhang W, Zhang C et al. APC gene deletions in gastric adenocarcinomas in a Chinese population: a correlation with tumour progression. Clin Transl Oncol 2012; 14: 60–65.
Jin G, Xu L, Shu Y, Tian T, Liang J, Xu Y et al. Common genetic variants on 5p15.33 contribute to risk of lung adenocarcinoma in a Chinese population. Carcinogenesis 2009; 30: 987–990.
Guo X, Liu W, Pan Y, Ni P, Ji J, Guo L et al. Homeobox gene IRX1 is a tumor suppressor gene in gastric carcinoma. Oncogene 2010; 29: 3908–3920.
Jung KH, Park BH, Hong SS . Progress in cancer therapy targeting c-Met signaling pathway. Arch Pharm Res 2012; 35: 595–604.
An X, Wang F, Shao Q, Wang F-H, Wang Z-Q, Chen C et al. METamplification is not rare and predicts unfavorable clinical outcomes in patients with recurrent/metastatic gastric cancer after chemotherapy. Cancer 2014; 120: 675–682.
Gherardi E, Birchmeier W, Birchmeier C, Vande Woude G, Targeting MET . in cancer: rationale and progress. Nat Rev Cancer 2012; 12: 89–103.
Liu X, Newton RC, Scherle PA . Developing c-MET pathway inhibitors for cancer therapy: progress and challenges. Trends Mol Med 2010; 16: 37–45.
Janjigian YY, Tang LH, Coit DG, Kelsen DP, Francone TD, Weiser MR et al. MET expression and amplification in patients with localized gastric cancer. Cancer Epidemiol Biomarkers Prev 2011; 20: 1021–1027.
Lennerz JK, Kwak EL, Ackerman A, Michael M, Fox SB, Bergethon K et al. MET amplification identifies a small and aggressive subgroup of esophagogastric adenocarcinoma with evidence of responsiveness to crizotinib. J Clin Oncol 2011; 29: 4803–4810.
Lee J, Seo JW, Jun HJ, Ki CS, Park SH, Park YS et al. Impact of MET amplification on gastric cancer: possible roles as a novel prognostic marker and a potential therapeutic target. Oncol Rep 2011; 25: 1517–1524.
Graziano F, Galluccio N, Lorenzini P, Ruzzo A, Canestrari E, D'Emidio S et al. Genetic activation of the MET pathway and prognosis of patients with high-risk, radically resected gastric cancer. J Clin Oncol 2011; 29: 4789–4795.
Ha SY, Lee J, Kang SY, Do IG, Ahn S, Park JO et al. MET overexpression assessed by new interpretation method predicts gene amplification and poor survival in advanced gastric carcinomas. Mod Pathol 2013; 26: 1632–1641.
Teng L, Lu J . cMET as a potential therapeutic target in gastric cancer (Review). Int J Mol Med 2013; 32: 1247–1254.
Kawakami H, Okamoto I, Arao T, Okamoto W, Matsumoto K, Taniguchi H et al. MET amplification as a potential therapeutic target in gastric cancer. Oncotarget 2013; 4: 9.
Gavine PR, Ren Y, Han L, Lv J, Fan S, Zhang W et al. Volitinib, a potent and highly selective c-Met inhibitor, effectively blocks c-Met signaling and growth in c-MET amplified gastric cancer patient-derived tumor xenograft models. Mol Oncol 2015; 9: 323–333.
Patel R, Leung HY . Targeting the EGFR-family for therapy: Biological challenges and clinical perspective. Curr Pharm Des 2012; 18: 2672–2679.
Hong L, Han Y, Brain L . The role of epidermal growth factor receptor in prognosis and treatment of gastric cancer. Exp Rev Gastroenterol Hepatol 2014; 8: 111–117.
Yarden Y, Pines G . The ERBB network: at last, cancer therapy meets systems biology. Nat Rev Cancer 2012; 12: 553–563.
Seshacharyulu P, Ponnusamy MP, Haridas D, Jain M, Ganti AK, Batra SK . Targeting the EGFR signaling pathway in cancer therapy. Exp Opin Ther Targets 2012. 16.
Fuse N, Kuboki Y, Kuwata T, Nishina T, Kadowaki S, Shinozaki E et al. Prognostic impact of HER2, EGFR, and c-MET status on overall survival of advanced gastric cancer patients. Gastric Cancer e-pub ahead of print 15 February 2015.
Hong L, Han Y, Yang J, Zhang H, Jin Y, Brain L et al. Prognostic value of epidermal growth factor receptor in patients with gastric cancer: a meta-analysis. Gene 2013; 529: 69–72.
Wang YK, Gao CF, Yun T, Chen Z, Zhang XW, Lv XX et al. Assessment of ERBB2 and EGFR gene amplification and protein expression in gastric carcinoma by immunohistochemistry and fluorescence in situ hybridization. Mol Cytogenet 2011; 4: 14.
Rossi E, Villanacci V, Danesino C, Donato F, Nascimbeni R, Bassotti G . Epidermal growth factor receptor overexpression/amplification in adenocarcinomas arising in the gastrointestinal tract. Rev Esp Enferm Dig 2011; 103: 632–639.
Oh HS, Eom DW, Kang GH, Ahn YC, Lee SJ, Kim JH et al. Prognostic implications of EGFR and HER-2 alteration assessed by immunohistochemistry and silver in situ hybridization in gastric cancer patients following curative resection. Gastric Cancer 2014; 17: 402–411.
Higaki E, Kuwata T, Nagatsuma AK, Nishida Y, Kinoshita T, Aizawa M et al. Gene copy number gain of EGFR is a poor prognostic biomarker in gastric cancer: evaluation of 855 patients with bright-field dual in situ hybridization (DISH) method. Gastric Cancer e-pub ahead of print 9 December 2014.
Herold S, Herkert B, Eilers M . Facilitating replication under stress: an oncogenic function of MYC? Nat Rev Cancer 2009; 9: 441–444.
Zhang L, Hou Y, Ashktorab H, Gao L, Xu Y, Wu K et al. The impact of C-MYC gene expression on gastric cancer cell. Mol Cell Biochem 2010; 344: 125–135.
Silva TC, Leal MF, Calcagno DQ, de Souza CR, Khayat AS, dos Santos NP et al. hTERT, MYC and TP53 deregulation in gastric preneoplastic lesions. BMC Gastroenterol 2012; 12: 85.
Leal MF, Calcagno DQ, Borges da Costa Jde F, Silva TC, Khayat AS, Chen ES et al. MYC, TP53, and chromosome 17 copy-number alterations in multiple gastric cancer cell lines and in their parental primary tumors. J Biomed Biotechnol 2011; 2011: 631268.
Ribeiro HF, Alcântara DFA, Matos LA, Sousa JMC, Leal MF, Smith MAC et al. Cytogenetic characterization and evaluation of c-MYC gene amplification in PG100, a new Brazilian gastric cancer cell line. Braz J Med Biol Res 2010; 43: 717–721.
Sonoda A, Mukaisho K, Nakayama T, Diem VT, Hattori T, Andoh A et al. Genetic lineages of undifferentiated-type gastric carcinomas analysed by unsupervised clustering of genomic DNA microarray data. BMC Med Genomics 2013; 6: 25.
da Costa Jde F, Leal MF, Silva TC, Andrade Junior EF, Rezende AP, Muniz JA et al. Experimental gastric carcinogenesis in Cebus apella nonhuman primates. PLoS One 2011; 6: e21988.
Calcagno DQ, Leal MF, Demachki S, Araujo MT, Freitas FW, Oliveira e Souza D et al. MYC in gastric carcinoma and intestinal metaplasia of young adults. Cancer Genet Cytogenet 2010; 202: 63–66.
Kim HK, Choi IJ, Kim CG, Kim HS, Oshima A, Yamada Y et al. Three-gene predictor of clinical outcome for gastric cancer patients treated with chemotherapy. Pharmacogenomics J 2012; 12: 119–127.
Wang X, Liu Y, Shao D, Qian Z, Dong Z, Sun Y et al. Recurrent amplification of MYC and TNFRSF11B in 8q24 is associated with poor survival in patients with gastric cancer. Gastric Cancer e-pub ahead of print 25 January 2015.
de Souza CR, Leal MF, Calcagno DQ, Costa Sozinho EK, Borges Bdo N, Montenegro RC et al. MYC deregulation in gastric cancer and its clinicopathological implications. PLoS One 2013; 8: e64420.
Choi JS, Seo J, Jung EJ, Kim EJ, Lee GK, Kim WH . c-MYC amplification in mucinous gastric carcinoma: a possible genetic alteration leading to deeply invasive tumors. Anticancer Res 2012; 32: 8.
Zhao S, Yuan Q, Hao H, Guo Y, Liu S, Zhang Y et al. Expression of OCT4 pseudogenes in human tumours: lessons from glioma and breast carcinoma. J Pathol 2011; 223: 672–682.
Hayashi H, Arao T, Togashi Y, Kato H, Fujita Y, De Velasco MA et al. The OCT4 pseudogene POU5F1B is amplified and promotes an aggressive phenotype in gastric cancer. Oncogene 2015; 34: 199–208.
Matsuoka T, Yashiro M . Recent advances in the HER2 targeted therapy of gastric cancer. World J Clin Cases 2015; 3: 42–51.
Sheng WQ, Huang D, Ying JM, Lu N, Wu HM, Liu YH et al. HER2 status in gastric cancers: a retrospective analysis from four Chinese representative clinical centers and assessment of its prognostic significance. Ann Oncol 2013; 24: 2360–2364.
Garcia-Garcia E, Gomez-Martin C, Angulo B, Conde E, Suarez-Gauthier A, Adrados M et al. Hybridization for human epidermal growth factor receptor 2 testing in gastric carcinoma: a comparison of fluorescence in-situ hybridization with a novel fully automated dual-colour silver in-situ hybridization method. Histopathology 2011; 59: 8–17.
Zhu GJ, Xu CW, Fang MY, Zhang YP, Li Y . Detection of Her-2/neu expression in gastric cancer: Quantitative PCR versus immunohistochemistry. Exp Ther Med 2014; 8: 1501–1507.
He C, Bian XY, Ni XZ, Shen DP, Shen YY, Liu H et al. Correlation of human epidermal growth factor receptor 2 expression with clinicopathological characteristics and prognosis in gastric cancer. World J Gastroenterol 2013; 19: 2171–2178.
Shim JH, Yoon JH, Choi SS, Ashktorab H, Smoot DT, Song KY et al. The effect of Helicobacter pylori CagA on the HER-2 copy number and expression in gastric cancer. Gene 2014; 546: 288–296.
Lee HE, Park KU, Yoo SB, Nam SK, Park do J, Kim HH et al. Clinical significance of intratumoral HER2 heterogeneity in gastric cancer. Eur J Cancer 2013; 49: 1448–1457.
Fox SB, Kumarasinghe MP, Armes JE, Bilous M, Cummings MC, Farshid G et al. Gastric HER2 testing study (GaTHER): an evaluation of gastric/gastroesophageal junction cancer testing accuracy in Australia. Am J Surg Pathol 2012; 36: 6.
Stenzinger A, von Winterfeld M, Aulmann S, Warth A, Weichert W, Denkert C et al. Quantitative analysis of diagnostic guidelines for HER2-status assessment. J Mol Diagn 2012; 14: 199–205.
Okines AF, Cunningham D . Trastuzumab in gastric cancer. Eur J Cancer 2010; 46: 1949–1959.
Park YS, Hwang HS, Park HJ, Ryu MH, Chang HM, Yook JH et al. Comprehensive analysis of HER2 expression and gene amplification in gastric cancers using immunohistochemistry and in situ hybridization: which scoring system should we use? Hum Pathol 2012; 43: 413–422.
Chen K, Yang D, Li X, Sun B, Song F, Cao W et al. Mutational landscape of gastric adenocarcinoma in Chinese: Implications for prognosis and therapy. Proc Natl Acad Sci USA 2015; 112: 1107–1112.
Ozaki T, Nakagawara A . p53: the attractive tumor suppressor in the cancer research field. J Biomed Biotechnol 2011; 2011: 603925.
Xu J, Wang J, Hu Y, Qian J, Xu B, Chen H et al. Unequal prognostic potentials of p53 gain-of-function mutations in human cancers associate with drug-metabolizing activity. Cell Death Dis 2014; 5: e1108.
Bellini MF, Cadamuro AC, Succi M, Proenca MA, Silva AE . Alterations of the TP53 gene in gastric and esophageal carcinogenesis. J Biomed Biotechnol 2012; 2012: 891961.
Suzuki K, Matsubara H . Recent advances in p53 research and cancer treatment. J Biomed Biotechnol 2011; 2011: 978312.
Wang J, Qian J, Hu Y, Kong X, Chen H, Shi Q et al. ArhGAP30 promotes p53 acetylation and function in colorectal cancer. Nat Commun 2014; 5: 4735.
Fassan M, Simbolo M, Bria E, Mafficini A, Pilotto S, Capelli P et al. High-throughput mutation profiling identifies novel molecular dysregulation in high-grade intraepithelial neoplasia and early gastric cancers. Gastric Cancer 2014; 17: 442–449.
Karaman A, Eşrefkabalar M, Nasir Binic D, Öztürk C, Pirim I . Genetic alterations in gastric precancerous lesions. Genetic Couns 2010; 21: 439–450.
Dar AA, Goff LW, Majid S, Berlin J, El-Rifai W . Aurora kinase inhibitors—rising stars in cancer therapeutics? Mol Cancer Ther 2010; 9: 268–278.
Katsha A, Arras J, Soutto M, Belkhiri A, El-Rifai W . AURKA regulates JAK2-STAT3 activity in human gastric and esophageal cancers. Mol Oncol 2014; 8: 1419–1428.
Katsha A, Soutto M, Sehdev V, Peng D, Washington MK, Piazuelo MB et al. Aurora kinase A promotes inflammation and tumorigenesis in mice and human gastric neoplasia. Gastroenterology 2013; 145: e1311–e1318.
Dar AA, Zaika A, Piazuelo MB, Correa P, Koyama T, Belkhiri A et al. Frequent overexpression of Aurora Kinase A in upper gastrointestinal adenocarcinomas correlates with potent antiapoptotic functions. Cancer 2008; 112: 1688–1698.
ÖZdemİR M, ÖZnur M, ÇİFtÇİ E, Durak Aras B, Aslan H, Saygili H et al. Detection of kinase amplifications in gastric adenocarcinomas. Turk J Med Sci 2014; 44: 461–470.
Yen CC, Yeh CN, Cheng CT, Jung SM, Huang SC, Chang TW et al. Integrating bioinformatics and clinicopathological research of gastrointestinal stromal tumors: identification of aurora kinase A as a poor risk marker. Ann Surg Oncol 2012; 19: 3491–3499.
Fang Z, Xiong Y, Li J, Liu L, Li M, Zhang C et al. Copy-number increase of AURKA in gastric cancers in a Chinese population: a correlation with tumor progression. Med Oncol 2011; 28: 1017–1022.
Cheng L, Wang P, Yang S, Yang Y, Zhang Q, Zhang W et al. Identification of genes with a correlation between copy number and expression in gastric cancer. BMC Med Genomics 2012; 5: 14.
Lee MC, Toh LL, Yaw LP, Luo Y . Drosophila octamer elements and Pdm-1 dictate the coordinated transcription of core histone genes. J Biol Chem 2010; 285: 9041–9053.
Maddox J, Shakya A, South S, Shelton D, Andersen JN, Chidester S et al. Transcription factor Oct1 is a somatic and cancer stem cell determinant. PLoS Genet 2012; 8: e1003048.
Parmar NR, Solanki JV, Patel AB, Shah TM, Patel AK, Parnerkar S et al. Metagenome of Mehsani buffalo rumen microbiota: an assessment of variation in feed-dependent phylogenetic and functional classification. J Mol Microbiol Biotechnol 2014; 24: 249–261.
Hwang-Verslues WW, Chang PH, Jeng YM, Kuo WH, Chiang PH, Chang YC et al. Loss of corepressor PER2 under hypoxia up-regulates OCT1-mediated EMT gene expression and enhances tumor malignancy. Proc Natl Acad Sci USA 2013; 110: 12331–12336.
Qian J, Kong X, Deng N, Tan P, Chen H, Wang J et al. OCT1 is a determinant of synbindin-related ERK signalling with independent prognostic significance in gastric cancer. Gut 2014; 64: 12.
Kang JU, Koo SH, Kwon KC, Park JW . AMY2 A: A possible tumor-suppressor gene of 1p21.1 loss in gastric carcinoma. Int J Oncol 2010; 36: 1429–1435.
Kim O, Yoon JH, Choi WS, Ashktorab H, Smoot DT, Nam SW et al. Gastrokine 1 inhibits gastrin-induced cell proliferation. Gastric Cancer e-pub ahead of print 10 March 2015.
Yoon JH, Song JH, Zhang C, Jin M, Kang YH, Nam SW et al. Inactivation of the Gastrokine 1 gene in gastric adenomas and carcinomas. J Pathol 2011; 223: 618–625.
Das K, Gunasegaran B, Tan IB, Deng N, Lim KH, Tan P . Mutually exclusive FGFR2, HER2, and KRAS gene amplifications in gastric cancer revealed by multicolour FISH. Cancer Lett 2014; 353: 167–175.
Chang J, Wang S, Zhang Z, Liu X, Wu Z, Geng R et al. Multiple receptor tyrosine kinase activation attenuates therapeutic efficacy of the fibroblast growth factor receptor 2 inhibitor AZD4547 in FGFR2 amplified gastric cancer. Oncotarget 2015; 6: 2009–2022.
Matsumoto K, Arao T, Hamaguchi T, Shimada Y, Kato K, Oda I et al. FGFR2 gene amplification and clinicopathological features in gastric cancer. Br J Cancer 2012; 106: 727–732.
Oshima T, Masuda M . Molecular targeted agents for gastric and gastroesophageal junction cancer. Surg Today 2012; 42: 313–327.
Liu YY, Chen HY, Zhang ML, Tian D, Li S, Lee JY . Loss of fragile histidine triad and amplification of 1p36.22 and 11p15.5 in primary gastric adenocarcinomas. World J Gastroenterol 2012; 18: 4522–4532.
Beroukhim R, Mermel CH, Porter D, Wei G, Raychaudhuri S, Donovan J et al. The landscape of somatic copy-number alteration across human cancers. Nature 2010; 463: 899–905.
Kuo WH, Huang CY, Fu CK, Liao CH, Hsieh YH, Hsu CM et al. The significant association of CCND1 genotypes with gastric cancer in Taiwan. Anticancer Res 2014; 34: 4963–4968.
Stahl P, Seeschaaf C, Lebok P, Kutup A, Bockhorn M, Izbicki JR et al. Heterogeneity of amplification of HER2, EGFR, CCND1 and MYC in gastric cancer. BMC Gastroenterol 2015; 15: 7.
Kang JU, Koo SH . ORAOV1 is a probable target within the 11q13.3 amplicon in lymph node metastases from gastric adenocarcinoma. Int J Mol Med 2012; 29: 81–87.
An J, Pan Y, Yan Z, Li W, Cui J, Yuan J et al. MiR-23a in amplified 19p13.13 loci targets metallothionein 2A and promotes growth in gastric cancer cells. J Cell Biochem 2013; 114: 2160–2169.
Hung WY, Wu CW, Yin PH, Chang CJ, Li AF, Chi CW et al. Somatic mutations in mitochondrial genome and their potential roles in the progression of human gastric cancer. Biochim Biophys Acta 2010; 1800: 264–270.
Liao LM, Baccarelli A, Shu XO, Gao YT, Ji BT, Yang G et al. Mitochondrial DNA copy number and risk of gastric cancer: a report from the Shanghai Women's Health Study. Cancer Epidemiol Biomarkers Prev 2011; 20: 1944–1949.
Bi R, Li WL, Chen MQ, Zhu Z, Yao YG . Rapid identification of mtDNA somatic mutations in gastric cancer tissues based on the mtDNA phylogeny. Mutat Res 2011; 709-710: 15–20.
Lee HC, Huang KH, Yeh TS, Chi CW . Somatic alterations in mitochondrial DNA and mitochondrial dysfunction in gastric cancer progression. World J Gastroenterol 2014; 20: 3950–3959.
Weinberg SE, Chandel NS . Targeting mitochondria metabolism for cancer therapy. Nat Chem Biol 2015; 11: 9–15.
Fulda S, Galluzzi L, Kroemer G . Targeting mitochondria for cancer therapy. Nat Rev Drug Discov 2010; 9: 447–464.
Fernandes J, Michel V, Camorlinga-Ponce M, Gomez A, Maldonado C, De Reuse H et al. Circulating mitochondrial DNA level, a noninvasive biomarker for the early detection of gastric cancer. Cancer Epidemiol Biomarkers Prev 2014; 23: 2430–2438.
Wen SL, Zhang F, Feng S . Decreased copy number of mitochondrial DNA: A potential diagnostic criterion for gastric cancer. Oncol Lett 2013; 6: 1098–1102.
Amgalan B, Lee H . DEOD: uncovering dominant effects of cancer-driver genes based on a partial covariance selection method. Bioinformatics e-pub ahead of print 26 March 2015.
Hou JP, Ma J . DawnRank: discovering personalized driver genes in cancer. Genome Med 2014; 6: 56.
Acknowledgements
This project was supported by grants from National Natural Science Foundation of China (30971330, 31371420, 81320108024, 81000861, 81322036 and 81272383); Foundation for Innovative Research Groups of the National Natural Science Foundation of China (Grant No. 81421001), the Program for Innovative Research Team of Shanghai Municipal Education Commission; Shanghai 'Oriental Scholars' project (2013XJ); Shanghai Science and Technology Commission 'Pujiang Project' (13PJ1405900) and Shanghai Natural Science Foundation (12ZR1417900). The sponsors of this study had no role in the analysis and interpretation of the literatures, the decision to submit the manuscript for publication or the writing of the manuscript.
Author Contributions
JX conceived this work. LL, JYF and JX wrote the paper. JX generated the schematic representation.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Liang, L., Fang, JY. & Xu, J. Gastric cancer and gene copy number variation: emerging cancer drivers for targeted therapy. Oncogene 35, 1475–1482 (2016). https://doi.org/10.1038/onc.2015.209
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/onc.2015.209
This article is cited by
-
m1A regulator-mediated methylation modification patterns correlated with autophagy to predict the prognosis of hepatocellular carcinoma
BMC Cancer (2024)
-
TMEM65 promotes gastric tumorigenesis by targeting YWHAZ to activate PI3K-Akt-mTOR pathway and is a therapeutic target
Oncogene (2024)
-
Chromosomal copy number amplification-driven Linc01711 contributes to gastric cancer progression through histone modification-mediated reprogramming of cholesterol metabolism
Gastric Cancer (2024)
-
Regulatory role of Chitinase 3-like 1 gene in papillary thyroid carcinoma proved by integration analyses of single-cell sequencing with cohort and experimental validations
Cancer Cell International (2023)
-
Multi-region sequencing depicts intratumor heterogeneity and clonal evolution in cervical cancer
Medical Oncology (2023)