Abstract
Background/Objective
Children’s diets in school-age are inherently unhealthy, with few meeting dietary recommendations. Yet, little is known about similarities and differences on dietary patterns across countries and their association with obesity. We aimed to derive dietary patterns in childhood and explore their association with adiposity-related outcomes in childhood and adolescence.
Subjcts/Methods
This study included data from six European countries (Spain, France, UK, Greece, Lithuania and Norway) during childhood (n = 1597) and adolescence (n = 803). Using a food frequency questionnaire, we derived data-driven dietary patterns through exploratory factor analyses and calculated the Mediterranean KIDMED index. We assessed body mass index z-score (zBMI), fat mass proportion and waist-to-height ratio at both visits. Associations were estimated using generalized linear regressions, adjusted for key-confounders.
Results
“Meat”, “Dairy”, “Western”, “Healthy” and “Sweets and fats” dietary patterns were derived. Norwegian children showed better diet quality, with higher consumption of fruits and vegetables, and highest “Healthy pattern” adherence, and Lithuanian children, the worst, with higher sweets consumption, and highest “Western pattern” adherence. Children with lower intake of healthy foods (vegetables, fruits, fish) tended to have higher adiposity, e.g., children with average or low “Healthy pattern” adherence (vs. high) had higher fat mass proportion in childhood (average: β (95% CI) 1.44 (0.48; 2.39), low: 1.10 (0.09; 2.12)). Low adherence to a “Healthy pattern” (vs. high) was associated with increased adolescent zBMI, and child and adolescent waist-to-height ratio. Low “Dairy pattern” adherence (vs. high), was associated with lower zBMI and fat mass in childhood, but not in adolescence. No significant associations were seen with the KIDMED index.
Conclusions
Many European children have poor diets and a low adherence to a healthy diet pattern may be of concern for adiposity-related outcomes. Assessment of children’s dietary patterns can help tailor dietary advice and provide support for families aiming to prevent future excess weight gain.
Similar content being viewed by others
Introduction
The WHO European Childhood Obesity Surveillance Initiative estimates that 29% of school-aged children are currently living with overweight/obesity in Europe [1]. This complex phenotype early in life has shown to have long-lasting effects [2]. Systematic reviews highlighted that a child or adolescent with obesity has approximately five times greater risk of having obesity in adulthood [3] as well as a greater risk of premature morbidity and mortality [4]. Diet-related diseases are large worldwide, with an estimated proportion of premature deaths related to diet being the highest in Europe [5].
Dietary intake has been changing in the past decades, at least in part, due to rapid shifts in globalization and urbanization [6]. Traditional eating habits, such as the Mediterranean diet [7], have been shifting towards highly processed diets. This results in poorer dietary quality [8] and increases the occurrence of obesity later in life [9,10,11]. Thus, the investigation of child diet is of special interest due to their influence on diet-related diseases during childhood (e.g., obesity) [4] and the tracking of dietary habits across the lifespan [12, 13]. Importantly, this is the age-group that exhibits the highest degree of deterioration in diet quality [14].
Methods to derive dietary patterns rely either on pre-existing or a priori dietary indices and scores that use prior scientific knowledge on diet-disease relationships (e.g., the Mediterranean diet profile), or on a posteriori methods, which are entirely based on available dietary data within a certain study population, to identify population-specific dietary patterns [15]. Both a priori and a posteriori methods to derive dietary patterns have their limitations, with the first approach being limited to current knowledge and understanding of the diet-disease relationship and the latter relying on available diet data, without any a priori hypothesis, thus not necessarily representing optimal patterns [16]. To the best of our knowledge, no study has described data-driven and a priori dietary patterns in children across different European countries or explored the association between these patterns and adiposity-related outcomes prospectively. To address this gap, we derived both data-driven and a priori dietary patterns at primary school-age and examined their association with adiposity-related outcomes both cross-sectionally in childhood and prospectively in adolescence across population-based cohorts from each part of Europe.
Materials/subjects and methods
Study population
This study is based on the Human Early-Life Exposome (HELIX) project [17], a longitudinal population-based project of six European birth cohorts: Born in Bradford (BiB; Bradford, UK) [18], Étude des Déterminants pré et postnatals précoces du développement et de la santé de l’Enfant (EDEN; Nancy and Poitiers, France) [19], INfancia y Medio Ambiente (INMA; Sabadell, Spain) [20], Kaunas (KANC; Kaunas, Lithuania) [21], Norwegian Mother, Father and Child Cohort Study (MoBa; Oslo, Norway) [22], and RHEA Mother Child Cohort study (RHEA; Heraklion, Greece) [23].
For the exposure (dietary data) and adiposity-related outcomes in childhood, we used data from the HELIX subcohort follow-up visit when children were 6–11 years old, which occurred between December 2013 and February 2016 (n = 1 637). We excluded 40 participants (INMA 28 (5.6%), BiB 4 (1.7%), KANC 4 (1.9%), MoBa 3 (1.0%) and RHEA 1 (0.5%)) due to missing dietary information, leaving a total of 1597 for analysis. Further details of the selection of the subcohort population and baseline characteristics are described elsewhere [17]. Individuals were re-evaluated in adolescence, when they were between 12–18 years [24]. In total, 877 adolescents were re-evaluated (BiB 126 (14.4%), EDEN 80 (9.1%), KANC 120 (13.7%), MoBa 56 (6.4%), RHEA 119 (13.5%) and INMA 376 (42.9%)), and, for the analyses on adiposity-related outcomes in adolescence, 803 adolescents with available data were included.
Ethics approval and consent to participate
All participants (mothers and children) provided written informed consent/assent before participation. Study procedures across all cohorts were conducted based on the Declaration of Helsinki guidelines. Approval for the HELIX cohort follow-up was obtained at each site by local ethics committees: BiB: HRA and Health and Care
Research Wales (HCRW NHS - 20/YH/0315); EDEN: Ethics committee CPP (Comité de Protection des Personnes) SUD-EST II (2020-A03533-36); INMA: Ethical Committee of Parc Salut Mar (Comité de Ética de la Investigación con medicamentos del Parc de Salut MAR - 2019/8788/I); MoBa: Regional Committee for Medical and Health Research Ethics (REK sør-øst B - 167349); RHEA: Ethical committee of the University Hospital in Heraklion, Greece (208/05.12.2019); KANC: the Lithuanian Bioethics Committee (2021-02-11 Nr. BE-2-8).
Dietary intake
Information on the child’s habitual diet (previous year) was collected through a semiquantitative food frequency questionnaire (FFQ) filled in by the parent at the 6–11 years follow-up visit [17]. The FFQ was developed by the HELIX research group, was translated and applied to all cohorts. Responses were given in nine options (“never” to “4 or more/day”), and responses were transformed in times/week of intake. Forty-four food items were assessed and grouped in 15 food groups, which were the sum of the weekly intake of the specific food items (continuous variables - Supplementary Table 1) and were used as input variables in the exploratory factor analysis. Three food groups did not meet the adequacy criteria for exploratory factor analysis (see Statistical analysis section), and were, therefore, not included as input variables in the current analysis.
Adiposity-related outcomes in childhood and adolescence
Height (cm) and weight (kg) were measured once, without shoes and with light clothing by trained personnel with regularly calibrated instruments following standardized procedures at childhood and adolescence. Height was measured with a Stadiometer (Seca213, d = 1 mm) and weight with a digital weight scale (Seca Bellisima 841, d = 100 g). Body mass index (BMI) (kg/m2) was calculated as the body mass/height2. The World Health Organization (WHO) reference curves were used to calculate standardized z-scores for BMI adjusted for sex and exact age (zBMI) [25] and weight status was defined as: Underweight/Healthy weight: zBMI < +1 standard deviations (SD) and Overweight/Obesity: zBMI ≥ +1 SD.
Besides zBMI, we considered waist circumference and waist-to-height ratio in our sample, since these reflect better body fat distribution, and have been widely used in childhood and adolescence [26, 27]. Waist circumference (cm) was measured twice, to ensure reliability, by trained personnel with the participant in a standing position using standardized procedures with a metric tape (Seca 201, d = 1 mm) in both visits. Measurements were taken in direct contact with the skin at the top of the iliac crests, during minimal respiration, with tape snug but not compressing the skin. Waist-to-height ratio was then defined as waist circumference/height. The cut-off value of 0.5 for waist-to-height ratio has been considered for detecting obesity in childhood and adolescence [26].
Lastly, measurements of bioimpedance were taken in childhood and adolescence without shoes and socks, and with light clothing, using Bodystat 1500 (Bodystat Ltd, Douglas, Isle of Man). In the EDEN cohort, Bodystat MDD 1500 was used at 50 kHz (corresponding to its default frequency). Electrodes were placed on cleaned skin; one measurement was taken after 5 minutes resting in supine position. Fat free mass (FFM) was estimated based on a multiracial equation recently developed for children based on impedance values obtained by a single frequency tetra-polar Bodystat device [28]. From this equation, body mass in kg and as a percentage of total weight were calculated. In the adolescence follow-up, FFM was estimated using the Schaefer et al. equation [29], which considers participant’s age and was validated in childhood and adolescence. From this equation, body fat mass percentage of total weight was estimated.
Covariates
We included the following covariates that are known to affect child food intake and/or adiposity-related outcomes [30] (Supplementary Fig. 1): cohort (KANC/BiB/INMA/MoBa/RHEA/EDEN), child/adolescent age (in years), sex (female/male), maternal pre-pregnancy BMI (in kg/m2), maternal smoking during pregnancy (yes/no), maternal education (defined as the highest level of education reporter by the mother, categorized according to the International Standard Classification of Education as: low, middle or high) [31], family affluence score (as a measure of the family’s economic capital, calculated based on questions regarding vehicle and computer ownership, bedrooms at home, and travels for holiday in the last 12 months, categorized as: low, middle and high) [32, 33] and child sedentary behavior, defined as “any behaviors characterized by an energy expenditure <1.5 metabolic equivalent tasks while in a sitting or reclining posture” and included the average time spent daily (in minutes) watching television, playing computer or video games and other sedentary activities (e.g., reading).
Statistical data analysis
In order to identify distinct data-driven dietary patterns, we employed exploratory factor analyses with orthogonal varimax rotation (most widely used method in dietary pattern analyses [34, 35]). Dietary patterns were derived using children’s combined frequencies of weekly intake of food items aggregated into food groups.
Sample adequacy for factor analysis was assessed using the Bartlett’s sphericity and Kaiser-Meyer-Olkin (KMO) tests, which assesses whether the variables belong together psychometrically and thus the correlation matrix is appropriate for factor analysis [36]. Although the first confirmed appropriate sample adequacy (p < 0.05), the latter revealed three food groups that were not suitable for factor analysis (bread, breakfast cereal, and cereals food groups), thus being excluded (KMO values for these food groups were < 0.5 [36]).
The number of factors to be retained were checked based on: (i) evaluation of eigenvalues using the Kaiser criterion (eigenvalues > 1), (ii) investigation of the inflection point of the scree plot of eigenvalues and parallel analysis, and (iii) factor solution interpretability. After rotation, loading cut-offs were applied to select the food groups in each pattern ( ≥ 0.25 and ≤ −0.25) [35, 37, 38].
Each participant was given, manually, dietary scores on all factors (patterns), which were derived by multiplying the most relevant factor loadings ( ≥ 0.25 and ≤ −0.25) by the corresponding standardized weekly intake of each food group and by adding all these items in each pattern. Greater scores indicate a higher consumption of foods/drinks in these patterns, and lower scores indicate a lower consumption [39]. Adherence to each data-driven dietary pattern was categorized in high, average and low based on the tertiles of factor scores.
The KIDMED quality index questionnaire [40] was used to assess adherence to the Mediterranean diet among children. It consists of 16 questions, with four questions denoting a negative connotation with respect to the adherence to Mediterranean diet assigned a value of −1 (consumption of fast food, baked goods/pastries and sweets/candies, and skipping breakfast) and the remaining 11 questions with a positive aspect were assigned a value of +1 (consumption of olive oil, fish, fruits, vegetables, cereals/grains, nuts, pulses, pasta/rice, dairy products, and yogurts/cheese). The score sum was classified in three levels: >4 points, high; 1–4 points, average; and <1 point, low adherence [41].
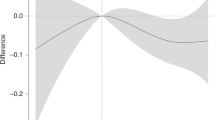
In this study, we were interested in evaluating cross-sectional and longitudinal associations separately, rather than evaluating changes in adiposity-related outcomes in linear mixed models. Analysis of outcome-change scores to estimate causal effects in observational data should be avoided, since these may lead to incorrect or misleading estimates [42]. Therefore, associations between data-driven and a priori dietary patterns in childhood and adiposity-related outcomes (zBMI, fat mass proportion and waist-to-height ratio) in childhood and adolescence, were evaluated using linear regression models specific to each outcome period, and adjusted for key covariates. For the KIDMED index, the “high” adherence was set as the reference category. For the data-driven dietary patterns, tertiles of adherence were used, and the healthiest tertile within each pattern was used as the reference category (e.g., for the “Western pattern”, low adherence was considered as the healthiest tertile and for the “Healthy pattern”, high adherence). We used inverse probability weighting in the estimation of adiposity-related outcomes in adolescence, aiming to deal with the loss of follow-up and reduce selection bias [43]. Weighting was performed using the WeightIt package [44], with the method “energy”, and including the cohort, maternal BMI and education, family affluence score, child sex and sedentary behavior. Statistical significance was set at 5%, and all tests were two-tailed. All analyses were conducted in R version 2022.02.0 Build 443 (R Core Team, Vienna, Austria).
Results
The study population included a greater proportion of Spanish children than the other cohorts (29.4%), with a median age of 8.3 and 14.9 years at the two visits. Children were mainly from families with a high educational level and low social deprivation (Table 1), with mothers from MoBa (Norway) being more likely to have a high educational level (77.6% with high education), and those from BiB (UK) more likely to have a low educational level (42.8% with low education) (Supplementary Table 2). MoBa children reported the highest weekly consumption of fruits (14.1 portions/week) and vegetables (8.5 portions/week). KANC children (Lithuania) reported the highest weekly consumption of sweets (9.5 portions a week) (Supplementary Table 3).
Five dietary patterns were identified (Fig. 1, Supplementary Fig. 2), with a total explained cumulative variance of 45%. Only one food group (sweets, composed by the weekly intake of chocolate, sweets and sugar and other sweeteners (Supplementary Table 1), had high factor loadings and were retained in two patterns (“Western” and “Sweets and Fats”). Dietary patterns were named according to their characteristics: “Meat pattern”, with meat and processed meat products, “Dairy pattern”, with yogurt and dairy products, “Western pattern”, with sweets, beverages, potatoes and bakery products, “Healthy pattern”, with vegetables, fruits and fish, and “Sweets and fats pattern”, with sweets, oil and fats (butter and margarine) (Fig. 1). Characteristics of children with a high adherence to each data-driven pattern are described by cohort in Supplementary Table 4. Almost 58% of children in MoBa (Norway) reported high “Healthy pattern” adherence. On the other hand, children from RHEA (Greece), INMA (Spain) and KANC (Lithuania) had the lowest percentages of high adherence to the “Healthy pattern” (Fig. 2). Children from INMA (Spain), RHEA (Greece) and the BiB (UK) with high adherence to the “Healthy pattern”, were more likely to have a highly educated mother and a wealthier family (Supplementary Table 4).
Dietary patterns are based on factor loadings with absolute values ≥ 0.25. Blue color represents high positive values (>0.25), white color represents average values (midpoint = 0.25) and red color represents low values (<0.25). Cumulative variance explained by each dietary pattern (%) was: “Meat pattern” – 14%, Dairy pattern – 25%, “Western pattern” – 40%, “Healthy pattern” – 40% and “Sweets and fats pattern” – 45%.
Only 18.2% of children had high adherence on the KIDMED index (Table 1), ranging from 31.7% in Norway to 5.4% in Lithuania (Table 2, Fig. 2). No major differences in KIDMED adherence were seen by child age. In the majority of cohorts, with exception of KANC and BiB, children with a low KIDMED adherence had higher median time spent in sedentary behaviors during the day, compared to children with an average/high adherence to this pattern (Table 2).
We found that children with a low “Dairy pattern” adherence, compared to high adherence, had a lower zBMI and fat mass proportion (β (95% CI) −0.18 (−0.34; −0.02) and −1.27 (−2.27; −0.27), respectively). Children with an average or low “Healthy pattern” adherence had a higher fat mass proportion (β (95% CI) 1.44 (0.48; 2.39) and 1.10 (0.09; 2.12), respectively), compared to those with high adherence. Low and average adherence to the “Healthy pattern”, compared to the high adherence, were also associated with higher waist-to-height ratio, besides higher zBMI (average adherence) (Table 3). No statistically significant associations were found for the KIDMED index. Supplementary Table 5 shows cross-sectional associations in childhood restricting to the sample with available data in the adolescence follow-up. Several significant associations described in cross-sectional analyses (Table 3) were maintained: Low adherence to the “Dairy pattern” was associated with lower zBMI and fat mass proportion, low and average adherence to the “Healthy pattern”, compared to high adherence, was associated with higher fat mass proportion and waist-to-height ratio.
Table 4 shows prospective associations between the data-driven and a priori dietary patterns in school-age with adiposity-related outcomes in adolescence. No statistically significant associations were seen between the KIDMED index during childhood and adiposity-outcomes in adolescence. For the data-driven dietary patterns, we found that children with low adherence to the “Healthy pattern”, compared to those with high adherence seen in childhood, showed in adolescence higher zBMI, fat mass proportion and waist-to-height ratio. Also, high adherence to the "Western pattern", compared to low adherence, showed lower waist-to-height ratio in adolescence. The significant associations with the "Dairy pattern", seen in cross-sectional analyses, were not maintained in prospective analyses.
Discussion
We derived dietary patterns among primary school-aged children from six European countries and evaluated associations with adiposity-related outcomes in childhood and adolescence. Children from Norway had healthier diets than those from the other countries, with the highest adherence to Mediterranean diet and the largest proportion of children following a healthy data-driven pattern, characterized by a high intake of fruits, vegetables and fish. On the other hand, children from Lithuania had low adherence to the Mediterranean diet, and a high adherence to the “Western pattern”, characterized by the intake of sweets, beverages, potatoes and bakery products. We did not detect significant associations between the Mediterranean diet adherence and adiposity-related outcomes both in childhood and adolescence. Certain data-driven patterns were significantly associated with adiposity-related outcomes, such as the “Dairy”, the “Healthy” and the “Western” patterns, with low adherence to the “Healthy pattern” being associated with higher fat mass percentage and waist-to-height ratio both in childhood and adolescence.
Systematic reviews demonstrate that certain data-driven dietary patterns, mainly those composed by potentially obesogenic foods (such as processed foods, sugar-sweetened beverages, candies and snacks), are associated with a higher obesity risk, mainly in cross-sectional studies [30, 45]. These diets, commonly referred to as “Western”, “Processed”, or “Junk food” dietary patterns, may be composed by different food groups, but share common features, such as high fat, sugar and/or salt composition and the presence of processed foods. On the other hand, dietary patterns in which children consume healthier foods (i.e., with lower sugar and fat content), such as fruits, vegetables, fish, legumes, etc.) showed to have weaker association on excess weight, and are usually named as “Healthy” or “Traditional” [30, 46]. Our findings suggest the existence of a “Western pattern”, as described by the literature as containing food groups related to higher adiposity (sweets, beverages, potatoes and bakery products), and also a “Healthy pattern”, composed by fruits (canned, dried, as juice or as pieces/whole fruits), vegetables (cooked and raw) and fish (canned, oily, while fish and seafood) among European children.
Regarding the existence of five distinct data-driven dietary patterns among six European countries, the pattern characterized by a higher consumption of fruits, vegetables and fish was inversely associated with adiposity-related outcomes in childhood. Studies on the associations between healthy or traditional dietary patterns, and lower adiposity-related measures in childhood have been demonstrated by some [38, 47], but not all studies. For instance, a fruit dietary pattern in US adolescents [48] and varied-Norwegian (characterized by a traditional Norwegian diet, including fish, fruits and vegetables) and dieting patterns (characterized by artificially sweetened beverages, low fat cheese and fat- and sugar-reduced yoghurt) in Norwegian school-aged children [49], were shown to be associated with a higher risk of overweight/obesity. However previous studies are mainly cross-sectional [30, 38, 45, 47, 49], thus limiting the ability to derive clear conclusions. Many factors, besides dietary intake, may play a role in adiposity in childhood, such as genes, physical activity habits, screen time and the food environment, which need to be taken into account when examining the potentially obesogenic effect of diet [45]. Also, healthy dietary patterns in studies may include different healthy food groups. For instance, the fruits and vegetables food groups may include a wide variety of foods containing essential nutrients and phytochemicals, and a healthy dietary pattern may include all forms of fruits and vegetables (fresh, frozen, canned and dried), as also included in our current food groups (Supplementary Table 1), however, should exclude those with added salt and/or sugar [50].
Consumption of dairy, especially milk, is generally popular in children and has been commonly considered part of a balanced diet [51]. A higher adherence to a dairy dietary pattern in 8-17-year-olds in Greece has been associated with healthier anthropometric measures, better sleeping time and physical fitness, reduced screen time, and greater adherence to the KIDMED index [52]. However, we did not see this protective effect of the “Dairy pattern”; instead, we found that a low adherence was associated with a lower fat mass proportion and zBMI in childhood. This inconsistency may be explained in the difference in proportion of participants considered as high dairy consumers, which was 81.4% (of a total of 177,091 individuals) in the Greek study and between 12.2 and 55.6% of high “Dairy pattern” consumers in the current study (Supplementary Table 4, Fig. 2). Also, foods included in the current dairy and yogurt food groups were low- and whole-fat foods. Dairy recommendations have been inconsistent, with dietary guidelines recommending the consumption of reduced-fat dairy products, and studies showing that the consumption of whole-fat dairy products is not associated with weight gain or adiposity-related measures, besides being beneficial in childhood, with, for example, effects on satiety [51].
A high “Western pattern” adherence, characterized by a high consumption of sweets, beverages, potatoes and bakery products, vs. low adherence, showed no significant cross-sectional or prospective associations with zBMI, which may be explained by a higher chance of under-reporting by parents. This pattern has been previously associated with higher risk of childhood overweight [30] and worse cardiometabolic health [53] in some studies, while others have reported null or even inverse associations [46,47,48,49,54]. This discrepancy in study findings can be explained by several factors, such as parental modification of the diets of overweight children, genetics and physical activity levels. Moreover, there is the possibility of underreporting of food consumption among children with overweight or obesity as a result of social desirability bias [54], with food items and drinks considered unhealthy being underreported more often than food items perceived as healthy [48, 49]. Another probable reason for this discrepancy include differences in the composition of the Western dietary pattern, such as different factor loadings for each food group, and differences in social and cultural factors across countries [46].
We analyzed one a priori dietary pattern, which measures the adherence to the Mediterranean diet, which is rich in plant-based foods, moderate-to-high in the intake of fish and seafood, moderate in eggs, poultry and dairy intake and low in meat. A previous study in Europe showed that higher adherence to the Mediterranean-like dietary patterns is not necessarily a feature of children living in Mediterranean countries [55], with children from Southern Europe having actually lower adherence to this pattern compared to children from the North. Our study corroborates these findings, as we observed greater adherence to this pattern among children from Norway and one of the lowest adherence in the Greek cohort. Systematic reviews in the past years summarized results examining associations between the Mediterranean diet and weight outcomes in both childhood and adolescence, with highly inconsistent results [56,57,58]. Pereira-da-Silva and colleagues described that European preschoolers did not have a high adherence to the KIDMED index, and that lower adherence was associated with higher prevalence of excess weight. Additionally, those with better adherence had families with higher maternal education and family socioeconomic status [57]. On the other hand, a systematic review based on 58 studies worldwide reported that half of analyzed studies (mainly cross-sectional) showed an inverse association between Mediterranean diet adherence and BMI in children and adolescents (2–20-year-olds), but not with other adiposity indicators such as waist circumference [58]. In our study, we did not detect a significant association between Mediterranean diet adherence and adiposity both cross-sectionally in childhood and prospectively in adolescence.
Diet quality is influenced by consumer’s purchasing power, which is in turn influenced by food environments, which provide options from which people make decisions about what to eat, including for example physical access to foods, food promotion, labelling and prices. Food environments are in turn influenced by food systems, which present many opportunities to improve diets, including agricultural production, food retail, storage, transport and trade, among others [59]. All of these factors may play an important role in the variability of dietary patterns adherence among cohorts/countries in the current study. We observed that mean intakes of dairy, bakery products, beverages, vegetables and sweets varied the most between participating countries (Supplementary Table 3). Regarding dietary pattern adherence, we observed in France (EDEN) and the UK (BiB), a higher adherence to the "Dairy pattern", which may be explained by the fact that, together with Germany, these are the main European milk-producing countries [60]. Besides food production and access, economic disparities may also explain differences in food intake among cohorts; Lithuania (KANC) and the UK (BiB) included more deprived populations (Supplementary Table 2) that showed greater adherence to unhealthy dietary patterns, such as the “Western” and “Sweets and fats” patterns in KANC, and BiB (Supplementary Table 4). As highlighted by the WHO European Childhood Obesity Surveillance Initiative [61], the proportion of 6-9-year-old children with low daily consumption of fruits and vegetables and high weekly intake of sugar-sweetened beverages is significantly greater among children with lower parental education and lower family perceived wealth compared with those with higher parental education and family perceived wealth. Lastly, country-specific public health policies implemented in Europe, such as school nutrition, food labelling and reformulations, fiscal and pricing policies, and communication with the public/nutrition literacy may have great impacts in promoting healthy nutrition and preventing diet-related noncommunicable diseases including obesity [62].
Strengths of our study include the investigation of dietary patterns instead of isolated food items/nutrients. When the outcome of study interest is associated with many dietary factors, which is the case of obesity or fat mass proportion, the dietary pattern approach may be useful, since it includes the overall diet [16], and achieves a resemblance of real life, with foods and nutrients being eaten in combination [63]. Also, the main purpose of this study in examining food groups in dietary patterns, instead of food items, is that foods are consumed in combination and dietary pattern analysis utilize the collinearity and reduce the complexity of underlying patterns [63]. This study uses a multicountry design, including Mediterranean and non-Mediterranean countries to investigate this dietary pattern. The use of harmonized data collection protocols in all included countries, besides the availability of repeated adiposity outcomes, besides BMI, are strengths of this study.
This study is not without limitations. Child dietary intake was assessed using a parent-reported questionnaire, so includes only food intake under parental control, excluding school meals. Besides, the report of dietary intake may be biased due to misreporting of diet, and underreporting of certain obesogenic foods. However, FFQs have been widely and commonly used to assess individual usual dietary intake in nutritional epidemiological studies, besides being described to be a reliable tool to measure dietary intake [64]. Third, the FFQ used to assess child dietary intake was not validated. We used an internationally agreed FFQ with portion size examples appropriate to each cohort [17]. Fourth, only one FFQ was analyzed; the use of multiple short-term instruments potentially complemented by a FFQ, has been recommended aiming to increase granularity of dietary intake [65]. Fifth, we used weekly frequencies of food intake and did not have data on child actual total energy intake in calories, so we were not able to adjust for this in our multivariable models. Sixth, a high percentage of families were from a higher socioeconomic status and educational level, which may impact generalizability and comparability. It is also worth mentioning the relatively small sample size of this study, specifically related to the high-country variance. In this sense, analyses were pooled together and multivariable models were adjusted for cohort. Larger sample sizes may have allowed a more detailed exploration of the study findings, by stratifying, for example, by cohort. Finally, residual confounding may be present, especially when taking into account differences by social classes and other lifestyle behaviors.
We described six major dietary patterns observed in six European countries among primary school-aged children and showed that certain dietary patterns may be related to both current and future adiposity-related outcomes, with specific concerns for low adherence to a healthy diet pattern. The estimation of data-driven dietary patterns among children has important implications for child nutrition and health. Dietary quality has shown to worsen with time, from childhood to adolescence, which emphasizes the need of public health strategies to improve dietary quality starting in early ages aiming to translate into improved dietary quality in adolescence and adulthood [14].
In conclusion, obtaining high quality data to strengthen the evidence for an association between child diet and adiposity related outcomes is challenging. Diet is notoriously difficult to measure and largely dependent on self-reports and parental factors. Still, this study shows that many European children have poor diets, and that poor adherence to a healthy diet pattern was associated with adiposity, particularly higher fat mass proportion and higher waist-to-height ratio.
Data availability
The data warehouse has been established in a format that allows future use beyond the project lifespan (2013–2017) as an accessible resource for collaborative research involving researchers external to the project. Access to HELIX data is based on approval by the HELIX Project Executive Committee and by the individual cohorts, who will evaluate potential overlap with ongoing work, adequacy of data protection plans, logistic and financial consequences and adequacy of authorship and acknowledgement plans. Further details on the content of the data warehouse (data catalogue) and procedures for external access are described on the project website (http://www.projecthelix.eu/index.php/es/data-inventory). The authors encourage interested researchers to contact them to set up collaborations.
References
World Health Organization (WHO). Regional Office for Europe. WHO European Childhood Obesity Surveillance Initiative (COSI): report on the fifth round of data collection, 2018–2020. 2022. https://www.who.int/europe/publications/i/item/WHO-EURO-2022-6594-46360-67071.
Geserick M, Vogel M, Gausche R, Lipek T, Spielau U, Keller E, et al. Acceleration of BMI in early childhood and risk of sustained obesity. N. Engl J Med. 2018;379:1303–12.
Simmonds M, Llewellyn A, Owen CG, Woolacott N. Predicting adult obesity from childhood obesity: a systematic review and meta‐analysis. Obes Rev. 2016;17:95–107.
Sharma V, Coleman S, Nixon J, Sharples L, Hamilton‐Shield J, Rutter H, et al. A systematic review and meta‐analysis estimating the population prevalence of comorbidities in children and adolescents aged 5 to 18 years. Obes Rev. 2019;20:1341–9.
2021 Global Nutrition Report: The state of global nutrition. Bristol, UK: Development Initiatives; 2022. https://globalnutritionreport.org/reports/2021-global-nutrition-report/.
Moreno L, Sarría A, Popkin B. The nutrition transition in Spain: a European Mediterranean country. Eur J Clin Nutr. 2002;56:992–1003.
Dinu M, Pagliai G, Casini A, Sofi F. Mediterranean diet and multiple health outcomes: an umbrella review of meta-analyses of observational studies and randomised trials. Eur J Clin Nutr. 2018;72:30–43.
Martínez Steele E, Popkin BM, Swinburn B, Monteiro CA. The share of ultra-processed foods and the overall nutritional quality of diets in the US: evidence from a nationally representative cross-sectional study. Popul Health Metr. 2017;15:1–11.
Leffa PS, Hoffman DJ, Rauber F, Sangalli CN, Valmórbida JL, Vitolo MR. Longitudinal associations between ultra-processed foods and blood lipids in childhood. Br J Nutr. 2020;124:341–8.
De Amicis R, Mambrini SP, Pellizzari M, Foppiani A, Bertoli S, Battezzati A, et al. Ultra-processed foods and obesity and adiposity parameters among children and adolescents: a systematic review. Eur J Nutr. 2022;61:2297–311.
Monteiro CA, Moubarac JC, Levy RB, Canella DS, Da Costa Louzada ML, Cannon G. Household availability of ultra-processed foods and obesity in nineteen European countries. Public Health Nutr. 2018;21:18–26.
Craigie AM, Lake AA, Kelly SA, Adamson AJ, Mathers JC. Tracking of obesity-related behaviours from childhood to adulthood: a systematic review. Maturitas. 2011;70:266–84.
Hovdenak IM, Stea TH, Twisk J, te Velde SJ, Klepp KI, Bere E. Tracking of fruit, vegetables and unhealthy snacks consumption from childhood to adulthood (15 year period): does exposure to a free school fruit programme modify the observed tracking? Int J Behav Nutr Phys Act. 2019;16:22.
Miller V, Webb P, Cudhea F, Shi P, Zhang J, Reedy J, et al. Global dietary quality in 185 countries from 1990 to 2018 shows wide differences by nation, age, education, and urbanicity. Nat Food. 2022;3:694–702.
De Almeida Alves M, Molina MDCB, Da Fonseca MDJM, Lotufo PA, Benseñor IM, Marchioni DML. Different statistical methods identify similar population-specific dietary patterns: an analysis of Longitudinal Study of Adult Health (ELSA-Brasil). Br J Nutr. 2022;128:2249–57.
Martínez-González MÁ, Martín-Calvo N. The major European dietary patterns and metabolic syndrome. Rev Endocr Metab Disord. 2013;14:265–71.
Maitre L, de Bont J, Casas M, Robinson O, Aasvang GM, Agier L, et al. Human early life exposome (HELIX) study: a European population-based exposome cohort. BMJ Open. 2018;8:e021311.
Wright J, Small N, Raynor P, Tuffnell D, Bhopal R, Cameron N, et al. Cohort Profile: the Born in Bradford multi-ethnic family cohort study. Int J Epidemiol. 2013;42:978–91.
Heude B, Forhan A, Slama R, Douhaud L, Bedel S, Saurel-Cubizolles MJ, et al. Cohort Profile: the EDEN mother-child cohort on the prenatal and early postnatal determinants of child health and development. Int J Epidemiol. 2016;45:353–63.
Guxens M, Ballester F, Espada M, Fernández MF, Grimalt JO, Ibarluzea J, et al. Cohort Profile: the INMA—INfancia y Medio Ambiente—(environment and childhood) project. Int J Epidemiol. 2012;41:930–40.
Grazuleviciene R, Nieuwenhuijsen MJ, Vencloviene J, Kostopoulou-Karadanelli M, Krasner SW, Danileviciute A, et al. Individual exposures to drinking water trihalomethanes, low birth weight and small for gestational age risk: a prospective Kaunas cohort study. Environ Health. 2011;10:32.
Magnus P, Birke C, Vejrup K, Haugan A, Alsaker E, Daltveit AK, et al. Cohort profile update: the Norwegian mother and child cohort study (MoBa). Int J Epidemiol. 2016;45:382–8.
Chatzi L, Leventakou V, Vafeiadi M, Koutra K, Roumeliotaki T, Chalkiadaki G, et al. Cohort profile: the mother-child cohort in crete, Greece (Rhea Study). Int J Epidemiol. 2017;46:1392–1393k.
Vrijheid M, Basagaña X, Gonzalez JR, Jaddoe VWV, Jensen G, Keun HC, et al. Advancing tools for human early lifecourse exposome research and translation (ATHLETE). Environ Epidemiol. 2021;5:E166.
de Onis M. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85:660–7.
Braunerová RT, Kunešová M, Heinen M, Rutter H, Hassapidou M, Duleva V, et al. Waist circumference and waist-to-height ratio in 7-year-oldchildren—WHO Childhood Obesity Surveillance Initiative. Obes Rev. 2021;6:e13208.
Brambilla P, Bedogni G, Heo M, Pietrobelli A. Waist circumference-to-height ratio predicts adiposity better than body mass index in children and adolescents. Int J Obes. 2013;37:943–6.
Clasey JL, Bradley KD, Bradley JW, Long DE, Griffith JR. A new BIA equation estimating the body composition of young children. Obesity. 2011;19:1813–7.
Schaefer F, Georgi M, Zieger A, Schärer K. Usefulness of bioelectric impedance and skinfold measurements in predicting fat-free mass derived from total body potassium in children. Pediatr Res. 1994;35:617–24.
Liberali R, Kupek E, Assis MAAde. Dietary patterns and childhood obesity risk: a systematic review. Child Obes. 2020;16:70–85.
Eurostat. International Standard Classification of Education (ISCED). 2016. https://ec.europa.eu/eurostat/statistics-explained/index.php?title=International_Standard_Classification_of_Education_(ISCED).
Liu Y, Wang M, Villberg J, Torsheim T, Tynjälä J, Lv Y, et al. Reliability and validity of family affluence scale (FAS II) among adolescents in Beijing, China. Child Indic Res. 2012;5:235–51.
Boyce W, Torsheim T, Currie C, Zambon A. The family affluence scale as a measure of national wealth: validation of an adolescent self-report measure. Soc Indic Res. 2006;78:473–87.
Sandvik P, Kuronen S, Reijs Richards H, Eli K, Ek A, Somaraki M, et al. Associations of preschoolers’ dietary patterns with eating behaviors and parental feeding practices at a 12-month follow-up of obesity treatment. Appetite. 2022;168:105724.
Chen Y, Kang M, Kim H, Xu W, Lee JE. Associations of dietary patterns with obesity and weight change for adults aged 18-65 years: evidence from the China Health and Nutrition Survey (CHNS). PLoS ONE. 2023;18:e0279625.
Dziuban CD, Shirkey EC. When is a correlation matrix appropriate for fator analysis? Some Decision Rules. Psychol Bull. 1974;81:358–61.
Castro MAde, Baltar VT, Selem SSdeC, Marchioni DML, Fisberg RM. Empirically derived dietary patterns: interpretability and construct validity according to different factor rotation methods. Cad de Saúde Pública. 2015;31:298–310.
Dalrymple KV, Flynn AC, Seed PT, Briley AL, O'Keeffe M, Godfrey KM. et al. Associations between dietary patterns, eating behaviours, and body composition and adiposity in 3-year-old children of mothers with obesity. Pediatr Obes. 2020;15:e12608.
Englund-Ögge L, Brantsæter AL, Juodakis J, Haugen M, Meltzer HM, Jacobsson B, et al. Associations between maternal dietary patterns and infant birth weight, small and large for gestational age in the Norwegian Mother and Child Cohort Study. Eur J Clin Nutr. 2019;73:1270–82.
Serra-Majem L, Ribas L, Ngo J, Ortega RM, García A, Pérez-Rodrigo C, et al. Food, youth and the Mediterranean diet in Spain. Development of KIDMED, Mediterranean diet quality index in children and adolescents. Public Health Nutr. 2004;7:931–5.
Stratakis N, Siskos AP, Papadopoulou E, Nguyen AN, Zhao Y, Margetaki K. et al. Urinary metabolic biomarkers of diet quality in European children are associated with metabolic health. Elife. 2022;11:e71332.
Tennant PWG, Arnold KF, Ellison GTH, Gilthorpe MS. Analyses of ‘change scores’ do not estimate causal effects in observational data. Int J Epidemiol. 2022;51:1604–15.
Hernán MA, Robins JM (eds). Causal Inference: What If. 1st ed. CRC Press, Boca Raton, 2020.
Greifer N. WeightIt: Weighting for Covariate Balance in Observational Studies. 2024. R package version 1.3.1, https://github.com/ngreifer/WeightIt, https://ngreifer.github.io/WeightIt/.
Verduci E, Bronsky J, Embleton N, Gerasimidis K, Indrio F, Köglmeier J, et al. Role of dietary factors, food habits, and lifestyle in childhood obesity development: a position paper from the European society for paediatric gastroenterology, hepatology and nutrition committee on nutrition. J Pediatr Gastroenterol Nutr. 2021;72:769–83.
Kelishadi R, Heshmat R, Mansourian M, Motlagh ME, Ziaodini H, Taheri M, et al. Association of dietary patterns with continuous metabolic syndrome in children and adolescents; a nationwide propensity score-matched analysis: the CASPIAN-V study. Diabetol Metab Syndr. 2018;10:52.
Nasreddine L, Shatila H, Itani L, Hwalla N, Jomaa L, Naja F. A traditional dietary pattern is associated with lower odds of overweight and obesity among preschool children in Lebanon: a cross-sectional study. Eur J Nutr. 2019;58:91–102.
Cutler GJ, Flood A, Hannan PJ, Slavin JL, Neumark-Sztainer D. Association between major patterns of dietary intake and weight status in adolescents. Br J Nutr. 2012;108:349–56.
Oellingrath IM, Svendsen MV, Brantsæter AL. Eating patterns and overweight in 9- to 10-year-old children in Telemark County, Norway: a cross-sectional study. Eur J Clin Nutr. 2010;64:1272–9.
Lichtenstein AH, Appel LJ, Vadiveloo M, Hu FB, Kris-Etherton PM, Rebholz CM. Dietary guidance to improve cardiovascular health: a scientific statement from the American Heart Association. Circulation. 2021;144:e472–e487.
O’Sullivan TA, Schmidt KA, Kratz M. Whole-fat or reduced-fat dairy product intake, adiposity, and cardiometabolic health in children: a systematic review. Adv Nutr. 2020;11:928–50.
Tambalis KD, Panagiotakos D, Psarra G, Sidossis LS. Recommended dairy intake is associated with healthy dietary habits, better physical fitness, less obesity and a healthier lifestyle profile in school age children. Br J Nutr. 2022;128:2046–53.
Pinto A, Santos AC, Lopes C, Oliveira A. Dietary patterns at 7-year-old and their association with cardiometabolic health at 10-year-old. Clin Nutr. 2020;39:1195–1202.
de Almeida Alves M, Retondario A, Bricarello LP, Fernandes R, de Moura Souza A, Zeni LAZR, et al. Association between dietary patterns and overweight/obesity: a Brazilian national school-based research (ERICA 2013–2014). J Public Health. 2020;28:163–71.
Tognon G, Moreno LA, Mouratidou T, Veidebaum T, Molnár D, Russo P, et al. Adherence to a Mediterranean-like dietary pattern in children from eight European countries. The IDEFICS study. Int J Obes. 2014;38:S108–14.
Grosso G, Galvano F. Mediterranean diet adherence in children and adolescents in southern European countries. NFS J. 2016;3:13–9.
Pereira-da-Silva L, Rêgo C, Pietrobelli A. The diet of preschool children in the Mediterranean Countries of the European Union: a systematic review. Int J Environ Res Public Health. 2016;13:572.
Iaccarino Idelson P, Scalfi L, Valerio G. Adherence to the Mediterranean Diet in children and adolescents: a systematic review. Nutr Metab Cardiovasc Dis. 2017;27:283–99.
Global Panel on Agriculture and Food Systems for Nutrition. Food systems and diets: facing the challenges of the 21st century. London; 2016. https://glopan.org/sites/default/files/ForesightReport.pdf.
Atlantic Area Healthy Food Eco-System (AHFES). Dairy: European market, consumer trends, and innovation. 2021. Accessed 20 Feb 2024. https://www.ahfesproject.com/app/uploads/2022/04/AHFES-A6.2_Dairy-report.pdf.
Fismen A, Buoncristiano M, Williams J, Helleve A, Abdrakhmanova S, Bakacs M, et al. Socioeconomic differences in food habits among 6‐ to 9‐year‐old children from 23 countries—WHO European childhood obesity surveillance initiative (COSI 2015/2017). Obes Rev. 2021;22:e13211.
Breda J, Castro LSN, Whiting S, Williams J, Jewell J, Engesveen K, et al. Towards better nutrition in Europe: evaluating progress and defining future directions. Food Policy. 2020;96:101887.
Schulz CA, Oluwagbemigun K, Nöthlings U. Advances in dietary pattern analysis in nutritional epidemiology. Eur J Nutr. 2021;60:4115–30.
Cui Q. A meta-analysis of the reproducibility of food frequency questionnaires in nutritional epidemiological studies. Int J Behav Nutr Phys Act. 2021;18:12.
Carroll RJ, Midthune D, Subar AF, Shumakovich M, Freedman LS, Thompson FE, et al. Taking advantage of the strengths of 2 different dietary assessment instruments to improve intake estimates for nutritional epidemiology. Am J Epidemiol. 2012;175:340–7.
Acknowledgements
We acknowledge the input of the entire HELIX consortium. We are grateful to all the participating families in the six cohorts (BiB, EDEN, INMA, MoBa, KANC, and RHEA cohorts), that took part in this study. We are equally grateful to all the fieldworkers for their dedication and efficiency in this study.
Funding
This project was funded by the European Union’s Horizon 2020 research and innovation programme under grant agreement No 874583 (ATHLETE project). The HELIX cohort data collection also received funding from the European Community’s Seventh Framework Programme (FP7/2007–2013) under grant agreement no. 308333. The Infancia y Medio Ambiente (INMA) study was supported by the Instituto de Salud Carlos III, Centro de Investigacion Biomedica en Red de Epidemiologia y Salud Publica (CIBERESP), and the Generalitat de Catalunya-Catalan National Science Foundation (CIRIT). The Kaunas cohort (KANC) was funded by the grant of the Lithuanian Agency for Science Innovation and Technology (6- 04- 2014_31 V- 66). For a full list of funding that supported the EDEN cohort, refer to: Heude B et al. Cohort Profile: The EDEN mother–child cohort on the prenatal and early postnatal determinants of child health and development. Int J Epidemiol. 2016 Apr;45(2):353–63. The Norwegian Mother, Father and Child Cohort Study (MoBa) is supported by the Norwegian Ministry of Health and Care Services and the Ministry of Education and Research. The Rhea project was financially supported by European projects, and the Greek Ministry of Health (Program of Prevention of Obesity and Neurodevelopmental Disorders in Preschool Children, in Heraklion district, Crete, Greece: 2011–2014; ‘Rhea Plus’: Primary Prevention Program of Environmental Risk Factors for Reproductive Health, and Child Health: 2012–2015). Born in Bradford receives funding from by a joint grant from the UK Medical Research Council (MRC) and UK Economic and Social Science Research Council (ESRC) [MR/N024391/1]; the British Heart Foundation [CS/16/4/32482]; a Wellcome Infrastructure Grant [WT101597MA]; The National Institute for Health Research under its Applied Research Collaboration for Yorkshire and Humber [NIHR200166] which also supports MB. The views expressed are those of the author(s), and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care. SW acknowledges receiving the funding by the Agency for Management of University and Research Grants with a Beatriu de Pinós post-doctoral fellowship (Ref: 2021 BP 00058). NS has received funding from the European Union’s Horizon Europe research and innovation programme under the Marie Skłodowska-Curie Actions (MSCA) Postdoctoral Fellowships (grant no. 101059245). ISGlobal acknowledges support from the grant CEX2023-0001290-S funded by MCIN/AEI/ 10.13039/501100011033, and support from the Generalitat de Catalunya through the CERCA Program.
Author information
Authors and Affiliations
Contributions
Concept and design: SW, MV. Acquisition, analysis, or interpretation of data: SW, MV. Drafting of the manuscript: SW, MV. Critical revision of the manuscript for important intellectual content: all authors. Statistical analysis: SW, LF. Obtained funding: SW, JW, MB, BH, RS, MV, RG, AB, MV. Supervision: MV.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Warkentin, S., Stratakis, N., Fabbri, L. et al. Dietary patterns among European children and their association with adiposity-related outcomes: a multi-country study. Int J Obes 49, 295–305 (2025). https://doi.org/10.1038/s41366-024-01657-6
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41366-024-01657-6