Abstract
Background
Understanding how obesity impacts human mammary adipose tissue (MAT) biology is crucial for deciphering its role in mammary epithelium during both physiological and pathophysiological processes, including breast cancer. Hypertrophic mammary adipocytes and Crown-Like Structures are present in MAT of patients with obesity but whether these changes initiate a fibro-inflammatory response at the tissue level remains insufficiently explored.
Objective
We investigated the markers of adipose tissue dysfunction (immune cell infiltration, secretion pattern and fibrosis) in tumor-free MAT of patients with obesity versus patients who are lean.
Methods
Tumor-free MAT were obtained from 96 women with (n = 43) or without (n = 53) obesity who underwent mastectomy for breast cancer risk reduction or treatment. Immune and non-immune cell infiltration were determined using flow cytometry. Bulk transcriptomic was used to characterize the phenotype of CD206+ macrophages whose infiltration is increased in patients with obesity. Conditioned-medium were prepared from MAT to characterize their secretome and dose adipokines and cytokines by ELISA assay. The extra-cellular matrix (ECM) deposition was evaluated by Masson trichrome staining on cross-stained sections, 3D imaging of red picrosirius-stained tissues and measure of hydroxyproline content.
Results
We observed an increase of CD206+/HLA-DR+ macrophages in the stromal vascular fraction of MAT from patients with obesity compared to patients who are lean. Other immune cell infiltration and endothelial or adipose progenitor cell numbers were similar between groups. Bulk transcriptomics on CD206+ macrophages revealed a significant decrease in ECM component expression and processing in obesity. In addition, no heightened secretion of pro-inflammatory cytokines, TGF-β1 or MCP-1 was observed in the samples from patients with obesity. ECM characterization revealed an absence of fibrosis, with MAT of patients with obesity showing even a slightly reduced collagen secretion and deposition compared with their lean counterparts.
Conclusions
Obesity is not associated with inflammation nor fibrosis in MAT, highlighting its unique behavior.
Similar content being viewed by others
Introduction
Mammary epithelial cells are surrounded by a fat pad (called mammary adipose tissue or MAT), formed by adipocytes (and associated progenitors) and infiltrated by vascular endothelial cells, fibroblasts and immune cells embedded in extra-cellular matrix (ECM) [1]. MAT is considered as a white adipose tissue and possesses both metabolic (storage and release of lipids) and secretory functions [2]. MAT could be defined as an “organ-associated” adipose tissue (AT) (like dermal, bone-marrow, epicardial, or periprostatic AT) whose main primary function could be the regulation of proximal organ physiology [2]. It has been demonstrated that MAT plays an important role in the development of the mammary gland during puberty as well as during pregnancy, lactation and involution [3]. Note that most of these results were obtained using mouse models. In rodents, in addition to anatomical differences, the MAT is more diffuse throughout the gland and contains less connective tissue surrounding mammary epithelial cell structures than in human glands [4]. During these processes, adipocytes serve both as an energy reservoir and endocrine cells, and display dynamic changes in number, size and function [2, 3]. For example, during pregnancy and lactation, mammary adipocytes undergo de-differentiation into preadipocyte-like progenitors and re-differentiate into mammary adipocytes at the end of the process [5]. Altogether, these results highlight the plasticity of MAT.
Effect of obesity on these organ-associated AT including MAT remains poorly investigated as compared to “classical” adipose depots. This question is of importance for MAT since obesity has been associated with increased breast cancer (BC) occurrence in post-menopausal women [6]. In addition, regardless of menopausal status, obesity worsens the prognosis of BC by increasing the risk of relapse and cancer-specific mortality [7, 8]. Deciphering the changes induced by obesity in MAT might help to understand how it locally affects BC behavior and subsequent clinical consequences arising from this dialog. Two non-exclusive mechanisms have been implicated. First, the MAT distant from the tumor could be a source of metabolites and soluble factors able to favor BC progression [9]. Second, at the tumor invasive front, the profound phenotypic changes that occur in adipocytes towards transdifferentiated cells, that we named “Cancer-Associated Adipocytes” promote tumor progression through soluble and ECM-related factors as well as reprogramming of tumor metabolism [10,11,12,13]. These two mechanisms could both be affected by obesity, which could be responsible for MAT dysfunction and changes in its response to cancer stimuli. To answer this question, first deciphering the changes induced by obesity in MAT distant from the tumor is an important prerequisite.
In “classical” adipose depots such as sub-cutaneous and visceral ATs (respectively SAT and VAT), expansion occurs through a progressive increase in size (hypertrophy) and eventually in number (hyperplasia) of adipocytes [14]. However, adipocytes ultimately reach a size limit where they can no longer accommodate further growth, resulting in cellular stress. One consequence of this stress is the initiation of a fibro-inflammatory response [14, 15]. Infiltration and activation of innate immune cells (including macrophages) and accumulation of a myriad of cytokines (for example TNFα, IL-1β, IL-8 and IL-6) are observed [14, 15]. Part of these macrophages surrounds dead or dying adipocytes forming the so-called Crown-Like Structures (CLS) [14, 15]. In this context of obesity, adipocyte biology is altered at both metabolism and secretory levels [14, 15]. In turn, inflammation can trigger the myofibroblastic transition of adipocyte progenitors, promoting the development of AT fibrosis [16]. Whether this fibro-inflammatory response occurs in human MAT in obesity remains an open question. Mammary adipocyte size is increased in patients with overweight and obesity and a positive correlation exists between adipocyte size and BMI in all the studies including ours [17,18,19]. CLS are significantly increased in the MAT of patients with overweight/obesity compared to patients who are lean [17, 18] and we have demonstrated that the CD11c macrophages forming CLS were positive for IL6, highlighting their pro-inflammatory status [18]. However, it is important to note that the occurrence of CLS is a relatively rare event [18]. In human MAT, obesity is associated with increased accumulation of interstitial macrophages expressing the CD206 mannose receptor without increase in macrophages expressing CD11c [20]. Only two transcriptomic studies performed in MAT from individuals with normal weight or with obesity suggested enrichment in signaling pathways consistent with a pro-inflammatory state in MAT in obesity [21, 22], but these results have not been validated at cytokines expression levels. Determining cytokines expression levels is important since mRNA concentrations may not always accurately represent the expression levels of the bioactive proteins [23]. Concerning fibrosis, few data were obtained in human MAT distant from the tumors. While an increase in peri-cellular fibrosis has been reported in MAT from patients with obesity using picrosirius red-stained cross-sections [20], it was reported that the percentage of peri-cellular fibrosis was negatively correlated with adipocyte size in another study using a similar approach [19]. Collagen bundles present in the AT have been shown to increase in length using second harmonic generation in tumor-free MAT from patients with obesity compared to those who are lean [24]. Taken together, data obtained to date in humans are sparse and not sufficient to definitively assess that a fibro-inflammatory response is induced by obesity in MAT as classically observed in SAT and VAT [14]. By contrast, mouse models of obesity consistently show fat pads exhibiting more fibrillar and stiffer ECM, chronic inflammation affecting both its physiological function and role in cancer progression, but the differences with humans in anatomy, cellular and collagen content need to be kept in mind [25].
A better understanding of how obesity affects human MAT biology is mandatory to provide a foundation for further mechanistic inquiries on its paracrine role on mammary epithelium in both physiological and pathophysiological processes. Accordingly, the initial goal of this study was to characterize the cellular content, secretions and ECM organization of tumor-free MAT in women with or without obesity. The study showed that obesity is not associated with inflammation nor fibrosis in MAT, highlighting its peculiar behavior.
Material and methods
Tissue collection
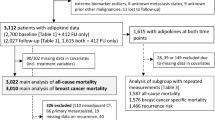
MAT samples were collected from patients undergoing mastectomy for BC or prophylactic surgery at the Toulouse-Oncopole University Cancer Institute or at the CHU Rangueil (for breast reduction surgery) between December 2017 and August 2024 (Toulouse, France). The clinical characteristics of the cohort are presented in Table S1. For patients with BC, MAT samples were collected in the quadrant opposite to the tumor, at a distance of at least 3 cm from the tumor. The patients with a history of homolateral breast surgery, chemotherapy, breast and/or axillary radiotherapy, hormone therapy were excluded. Samples were either obtained from patients who are lean (BMI between 18.5 and 25 kg/m²) or patients with obesity (BMI greater than 30 kg/m², except for 3 patients with overweight, with a BMI between 28 and 30 kg/m²). The sample size for the MAT analysis was determined to ensure the inclusion of women with a range of body mass index. The study was conducted in accordance to the guidelines and with the full approval of the national ethics committee (authorization AC-2016-2658, DC-2016-2656). All patients gave their informed consent to participate in biological studies.
Tissue processing
Surgical samples were immediately placed in 10 ml of Dulbecco’s Modified Eagle’s Medium and carried out to the laboratory within 1 h. Part of the samples were (1) fixed with 4% paraformaldehyde solution at RT to perform 3D microscopy analyses after picrosirius staining, (2) embedded in paraffin (Pathology Department) for Trichrome Masson staining, (3) immediately frozen in liquid nitrogen and stored at −80 °C for dosage of hydroxyproline content, or used as fresh samples to, (4) isolate the stroma vascular fraction (SVF) after collagenase digestion or, (5) prepare MAT-conditioned medium (MAT-CM) as previously [26].
Flow cytometry analysis of SVF and RNA-seq of the CD206+ macrophages isolated from SVF
Isolation of SVF and flow cytometry were performed as previously [27]. The antibodies used are listed in Table S2. CD206+ macrophages isolated from SVF of MAT samples from patients with or without obesity (n = 4 of each) were sorted using a FACS CantoTM II flow cytometer and Diva Pro software (BD Biosciences). After sorting, macrophages were resuspended in QIAzolTM lysis reagent (Qiagen) and stored (−80 °C) until analysis. After RNA extraction, RNA-seq libraries were prepared using the NEBNext® Ultra™ II Directional RNA Library Prep Kit for Illumina followed by a capture of the coding regions using the TWIST Human Core Exome following the manufacturer’s protocol. Paired-ended sequencing was performed on a Illumina NovaSeq6000 instrument by Integragen Genomics. For gene expression quantification, STAR was used to obtain the number of reads associated to each gene in the Gencode v31 annotation (restricted to protein-coding genes, antisense and lincRNAs). Raw counts for each sample were imported into R (v4.2.3). After filtering for genes quantified in at least 20% of samples, differentially expressed genes were identified using DESeq2, and multiple-test correction was performed using Benjamini–Hochberg control of false discovery rate [28]. Gene expression was considered significantly different if the p value was <0.05. Pathway enrichment analysis was performed with GeneAnalytics (https://geneanalytics.genecards.org/) [29] based upon Gene Ontology (GO) terms. Volcano plot was performed with GraphPad Prism (v9.5.1.733). Balloon plot was performed with ggplot2 package (v3.4.4). RNA-seq data have been deposited on SRA (Bioproject ID PRJNA1169556).
ELISA assays
A panel of secreted adipokines was quantified in MAT-CM from samples of patients with or without obesity with an ELISA kit as previously [26].
Masson’s Trichrome staining, collagen staining with Picrosirius Red, 3D collagen fiber and hydroxyproline quantification
Experiments and analysis were performed as previously [26].
Proteomic analysis
After centrifugation and supplementation with a protease inhibitor cocktail (Sigma-Aldrich), 5 ml of serum-free MAT-CM was incubated 2 h on ice with 0.1% sodium lauroyl sarcosinate and 7.5% trichloroacetic acid for protein precipitation then centrifuged 10 min at 10,000 × g. After 2 washes of the pellet with tetrahydrofuran, the resulting pellet was resuspended in a Laemmli buffer. Protein concentration was determined using DC protein assay kit (Biorad, Marnes-la-Coquette, France) following manufacturer instructions. Fifty µg of proteins were digested with trypsin using the S-Trap™ micro spin column (ProtiFi, NY USA). Tryptic peptides were analyzed by nano-LC using an UltiMate 3000 system coupled to an Orbitrap Q Exactive HF-X mass spectrometer (Thermo Scientific) operated in data-dependent acquisition mode, as previously [30]. Acquired data were searched with Mascot 2.7.7 against the Human UniProtKB database (release 20180213) with parameters as previously [31]. Proline 2.0 software (http://proline.profiproteomics.fr/) was used for the validation of identifications and the label-free quantification of identified proteins [32]. Proteins with a Welch’s t-test p value <0.05 and a fold change <0.66 and >1.5 were considered significantly varying. Heatmap from regulated proteins was performed with Perseus toolbox (v2.0). The data were deposited to the ProteomeXchange Consortium via the PRIDE partner repository with the dataset identifier PXD050896.
Statistics
Analyses were performed with GraphPad Prism (v9.5.1.733). For flow cytometry, two-way ANOVA was performed followed by the Bonferroni post-test. For ELISA assays and fibrosis analysis, comparisons between patients with or without obesity were performed using a paired t-test or Mann–Whitney test for data not normally distributed. Normal distribution of the data was determined using the Kolmogorov–Smirnov test. For correlation between macrophages number and BMI or correlation of Masson’s Trichrome staining and BMI, the univariate relationship was performed with Spearman’s correlation. p values <0.05 (*), <0.01 (**), <0.001 (***) and <0.0001 (****) were deemed as significant.
Results
Characterization of the stromal vascular fraction of MAT from patients with or without obesity
To investigate the impact of obesity on MAT, we used a cohort of 96 women who underwent mastectomy for BC treatment (n = 71), prophylactic surgery (n = 9) or reduction mammoplasty (n = 16). The clinicopathological data of the cohort are presented in Table S1. Based on BMI, patients were divided into 2 groups (with or without obesity). No differences were found between groups with respect to age, menopausal status or subtype of BC (Table S1). The total number of cells present in the stromal vascular fraction (SVF) (normalized per gram of fat tissue) was significantly higher in patients with obesity compared to those who are lean (Fig. 1a). We then measured the proportion of progenitors and immune cells in the SVF of MAT from patients with (n = 15) or without obesity (n = 20). Immunostaining followed by flow cytometry analyses using the immune cell marker CD45 and the endothelial and stemness marker CD34 allowed identification of non-immune cell subsets (mainly progenitors and endothelial cells as CD45−/CD34+) and immune cells (CD45+/CD34−) (Fig. 1b). The number of immune cells was significantly higher in patients with obesity compared to those who are lean, while the number of the non-immune cell subset was not different (Fig. 1b). Additional labeling with markers defining macrophages (CD14) and various macrophages subsets (CD206, HLA-DR) were performed. The proportion of macrophages (defined as CD45+/CD14+/CD34− cells) was increased in patients with obesity (Fig. 1c). Among macrophages, a significant increase in CD206+/HLA-DR+ subset was observed in the group with obesity whereas the proportion of CD206-/HLA-DR+ was unchanged between the two groups, these two populations being considered as resident and recruited macrophages respectively [33] (Fig. 1c). In addition, a positive correlation was observed between the number of macrophages and BMI (Fig. 1d). The proportion of total lymphocytes (defined as CD45+/low side scatter) and of various lymphocyte subsets were similar between the two groups (Fig. 1e). Finally, the percentage of adipose progenitor cells (defined as CD45-/CD34+/CD31− cells) in the SVF was similar between patients with or without obesity (Fig. 1f). When additional markers (MSCA1 and CD271) were used to characterize the sub-populations of adipose progenitors [27], the proportions of the various progenitor subsets (the adipogenic MSCA1+, myofibrogenic MSCA1−/CD271+, and immature MSCA1/CD271− subsets), were similar in all groups (Fig. 1f). Moreover, we compared the expression level of several genes in cells of the SVF fraction involved in the ECM and fibrosis (ACTA2, TGF-β1, col1A1, col3A1, col6A1, col6A2 and col6A3) in patients with or without obesity. Our results (obtained by RTqPCR) did not show any differences between the two groups with the exception of col6A3, whose expression was significantly reduced in patients with obesity (p < 0.05) (Supplementary Fig. 1). The number of endothelial cells (CD45−/CD34+/CD31+) was also unchanged between the two groups (Fig. 1f). Taken together, these data showed that the SVF fraction in patients with obesity exhibited slight modifications compared to lean ones with the noticeable increased infiltration by a CD206+ macrophages subset in accordance with a previous study [20].
a SVF cell count between patients with (n = 19) or without (w/o) (n = 26) obesity. b Number of non-immune (CD45−/CD34+) and immune (CD45+/CD34−) cells. c Number of total macrophages (CD45+/CD14+/CD34−) and macrophages subset (CD206+/HLA-DR+ or CD206−/HLA-DR+). d Correlation between macrophage number (as in c) and BMI (Pearson r = 0.5136, p = 0.0016). e Number of lymphocytes (CD45+/low side scatter or SSC), B (CD45+/CD3-/CD19+) and T lymphocytes (CD45+/CD3+/C19−) subdivided into helper (CD45+/CD3+/C19−/CD4+) and cytotoxic (CD45+/CD3+/CD19−/CD8+) T cells. f Number of adipose progenitor cells (CD45−/CD34+/CD31−) and subsets expressing or not CD271 or MSCA1, and endothelial cells (CD45−/CD34+/CD31+). The results, obtained from patients without (white open circle, n = 20) or with obesity (red filled circle, n = 15), were normalized per gram of fat tissue. g Volcano plot representing the log2 fold-change calculated from RNAseq data in obesity versus in normal weight condition and –log10 of the p value, showing under-represented (blue) and over-represented (red) RNA. h Balloon plot representing the hallmarks enriched in each gene categories. The size of the circles was setup according to the percentage of genes belonging to each hallmark differentially expressed and the color as a function of the GeneAnalytics score, which corresponds to the transformation of the binomial distribution p value. Pathways involved in ECM composition and regulation are in bold.
To investigate further the differences between these CD206+ macrophages in MAT of patients with or without obesity, their transcriptomes were sequenced. Among the 1582 differentially expressed genes identified in patients with obesity versus those who are lean (i.e. adjusted p < 0.05), 958 (60.6%) were down-regulated, while 624 (39.4%) were up-regulated (Fig. 1g). Gene ontology (GO)-based categories clustering on biological processes and pathway enrichment analysis highlighted that among the down-regulated pathways, most of them were associated to ECM organization, remodeling and cell-response to ECM, with ECM organization being the most down-regulated pathway in patients with obesity (Fig. 1h). Up-regulated pathways, that exhibited global low scores, were related to T cell function, small GTP-ases mediated transduction, and tryptophan metabolism (Fig. 1h). Within the ECM organization, the most down-regulated pathway, the detailed list of genes showed decrease in various collagen family members and proteases such as ADAMTSs (a disintegrin and metalloproteinase with thrombospondin motifs) and MMPs (matrix-metalloproteinase) (Table S3). Taken together, our results highlighted that one of the key features of the CD206+ macrophages identified was related to decreased secretion, processing and response to the ECM environment.
Absence of increased secretion of pro-inflammatory cytokines by MAT from patients with obesity compared to those who are lean
Adipocyte hypertrophy during AT expansion is usually associated with changes in secretion related to tissue dysfunction [14, 15]. Key among these changes is increased secretion of leptin and, in parallel, decreased secretion of adiponectin [14, 15]. Using MAT-conditioned media (MAT-CM), we found that significantly less adiponectin was secreted by MAT from patients with obesity than by MAT from patients who are lean (Fig. 2a), whereas leptin secretion was similar (Fig. 2b). In isolated adipocytes from MAT of patients with obesity, the mRNA levels of adiponectin were also decreased while the ones of leptin were significantly increased, as expected with adipocyte hypertrophy (Supplementary Fig. 2). To characterize the inflammatory state of MAT from patients with obesity, we quantified the secretion of several pro-inflammatory cytokines (IL-6, IL-8, IL1-β, TNF-α), the profibrotic protein TGF-β1, as well as the monocyte chemoattractant protein-1 (MCP-1/CCL2) and Plasminogen-activator 1 (PAI-1), both involved in the recruitment of immune cells [14, 15]. As shown in Fig. 2c–i, the amounts of these secreted proteins were similar between the two groups with the exception of PAI-1, for which an almost significant decrease (p = 0.0513) was observed in obesity.
Concentrations of adiponectin (a), leptin (b), IL-6 (c), IL-8 (d), IL-1β (e), TNF-α (f), TGF-β1 (g), MCP-1 (h), and PAI-1 (i), in the conditioned medium of MAT obtained from patients without (white open circle, n = 9) or with obesity (red filled circle, n = 9). Data are expressed as means ± SEM. *p < 0.05 (Mann–Whitney test).
Under-representation of ECM proteins in the conditioned medium of MAT from patients with obesity
We next analyzed by proteomics the MAT-CM of samples from patients with or without obesity, reflecting the compounds secreted by the cells composing the MAT. Among the 1791 proteins detected, 55 (3.1%) were enriched in obesity (i.e., adjusted p < 0.05 with a fold change >1.5) whereas 34 (1.9%) were less represented compared with samples of patients who are lean (Fig. 3a and Tables S4, S5 for the list of the proteins). The heatmap performed on differentially detected proteins to determine key features specific to MAT in obesity revealed two main clusters (Fig. 3b). Cluster analysis of under-represented proteins (31 out of 34) using GO on cellular components highlighted enrichment of proteins belonging to collagens and components of the ECM (Fig. 3c). A PPI network constructed using the STRING (v12.0) online database reinforced the connection of the collagen-containing-ECM proteins identified, with bridges indicating both functional and physical protein associations (Fig. 3d). Four types of different collagen chains (COL6A1, COL6A3, COL15A1, COL18A1) as well as fibrillin-1 (FBN1) and fibulin-2 (FBLN2) were identified as the hub proteins with the highest degree of connectivity (Fig. 3d). The analysis of the cluster related to over-regulated proteins (48 out of 55) with GO-based categories clustering (Fig. 3c) on cellular components showed that they were mainly enriched in the terms extracellular exosomes in accordance with our results that have shown increased exosomes secretion in AT in obesity [34]. Taken together, our main results suggested a decrease in ECM molecules secretion in samples obtained from patients with obesity compared to those who are lean.
a Volcano plot representing the log2 fold change of each protein in the MAT-CM of patients with obesity compared to that of patients who are lean and the p value (–log10). b Heatmaps of protein expression of MAT secretome belonging to the two main clusters differentially expressed in samples from patients with or without obesity. c Pathway enrichment analysis (GO-based categories clustering) performed with GeneAnalytics in the cluster identified for the under-represented (blue bars) or over-represented (red bars) proteins. Score has been calculated as a binomial transformation of the p Value for each pathway. Pathways involved in ECM composition and regulation are in bold. d Interaction networks of down-regulated proteins belonging to the collagen-containing-ECM in MAT-CM from patients with obesity, modelized using the STRING online database with a minimum required interaction score >0.4.
Absence of fibrosis in the MAT of patients with obesity
Our results highlighted that the MAT obtained from patients with obesity exhibited decrease in ECM protein secretion and were infiltrated by CD206+ macrophages exhibiting decrease in gene expression involved in ECM organization and remodeling. These results suggest that MAT in obesity does not exhibit fibrosis, which has been previously reported to occur in human ATs in obesity [35]. To investigate this hypothesis, we compared the collagen deposition with quantitative and qualitative approaches in MAT from patients with or without obesity. To quantify the collagen deposition, sections of paraffin-embedded samples were stained with Masson’s trichrome, which stains in blue the fibrillar collagens (Fig. 4a). The interstitial collagen deposition appeared to be decreased in samples from patients with obesity as shown in a picture from a representative experiment (Fig. 4a). Indeed, quantification of collagen staining indicated a decrease, while not significant (p = 0.075), in samples from the group with obesity compared to the other group (Fig. 4b). We also found a trend towards negative correlation between collagen quantification and BMI in our patient series (Fig. 4c). To further explore this issue, the quality of collagen fibers was investigated in term of diameter with picrosirius red, imaged the staining by 3D confocal microscopy (Fig. 4d, left) and reconstructed images of the fiber network in 3D (Fig. 4d, right). In the reconstructions, the diameter of collagen fibers appeared smaller in MAT in obesity (as shown by the maximum intensity projection) (Fig. 4d, right). Using Imaris software (v9.2), we observed a downward trend, although not significant, in the volume and number of branches of collagen fibers (Fig. 4e, f). To confirm the trend towards slight decrease in collagen deposition in the MAT in obesity, we quantified hydroxyproline (a major component of collagen comprising around 13.5% of its amino acid composition) content in MAT. This measurement represents a validated and quantitative method to evaluate fibrosis that we used in a previous study [26]. Our results showed a slight but significant decrease of this amino acid in MAT of patients with obesity compared with those without obesity (Fig. 4g). Together, these data using three different experimental approaches showed that obesity is not associated with an increase of fibrosis in MAT.
a Representative pictures of Trichrome Masson staining in MAT from patients with or without obesity (scale bars, 200 μm). b Quantification of the staining performed on the whole tissue sections obtained in patients without (n = 19) or with obesity (n = 13). Statistics were performed using Student’s t test. c Correlation between quantification of Trichrome Masson staining (as in b) and BMI (Pearson r = 0.5637, p = 0.0008). d Representative three-dimensional (3D) confocal images of Picrosirius Red staining (left panel) and 3D reconstruction of collagen fibers (right panel) in samples from patients with or without obesity. Reconstructed collagen fibers were color-coded according to their mean diameter (scale bars, 50 μm). e Quantification of collagen fiber volume or f number of branches in Picrosirius Red stained MAT samples from patients with or without obesity. g Hydroxyproline concentrations in MAT samples from patients with or without obesity. Data are expressed as means ± SEM; *p < 0.05 (Mann–Whitney test).
Discussion
The main aim of this study was to characterize the changes induced by obesity in human MAT and to assess whether the fibro-inflammatory response present in other adipose deposits was observed. Through highly complementary and diverse immunophenotyping, transcriptomic, proteomic and imaging approaches, we revealed that MAT in obesity exhibited an absence of fibrosis and even a slight decreased ECM remodeling, secretion and deposition, as well as an absence of inflammation.
Obesity is usually associated with altered ECM remodeling and excess ECM deposition in adipose depots, which could ultimately lead to fibrosis [35]. However, these ECM modifications have been better described in mouse models than in human conditions, and mainly in the major adipose deposits VAT and SAT. Our results are in apparent contradiction with those obtained in mice where MAT fibrosis in obesity has been systematically reported [25]. Mammary fat pad in diet-induced (HFD) or ob/ob mice (which have a mutation in the gene encoding leptin) exhibit increased α-SMA positive cells, fibronectin content and elevated linearity and stiffness of collagen [24]. However, it is worth mentioning that histologically, the mouse mammary stroma is dramatically different from the human [4]. In humans, the epithelium is closely associated with fibrous connective tissue separating it from AT while an interspersed connective tissue is present in small amounts in mouse mammary gland that contains a larger amount of fat [4]. Such a difference could explain the species-specific fibrotic stress response represented by the expansion of MAT. In humans, the data are sparse and contradictory as stated in the introduction.
One of the main advantages of our study was the use of combined approaches to address this issue. All the results obtained demonstrated an absence of fibrosis in MAT in obesity and rather suggest a slight decrease in matrix deposition in these tissues. Using collagen staining on MAT cross-sections with Trichrome Masson, that has been shown to correlate to picrosirius staining for quantification of collagen deposition [36], we found a decreased collagen deposition in patients with obesity versus those who are lean, with a negative correlation between the staining signal and BMI. These results were confirmed by 3D imaging after picrosirius staining, showing that the fibrillar collagen network in the MAT was substantially less dense in patients with obesity. The lack of significant decrease in collagen fiber volume may be explained by the small number of patients included (n = 5 in each group). Finally, the quantification of hydroxyproline showed a slight but significant decreased content in the MAT of patients with obesity. The results of the proteomic study showed an under-representation of ECM components in the MAT-CM in obesity compared to the samples of the other group. Among the under-represented proteins, two different alpha chains of the most abundant non-fibrillar collagen, collagen VI (COL6) were found (COL6A1 and COL6A3). COL6 is a highly enriched component in AT and the most highly expressed collagen in differentiated adipocytes [37]. The two other collagens found, collagen XV (COL15) and XVIII (COL18), share similarity in their primary structures and have been both implicated in the regulation of adipocyte differentiation [38]. Although not directly demonstrated here, our results suggest that part of the relative decrease in ECM content could be due to adipocytes. The transcriptomic analyses of CD206+ macrophages also highlighted a strong decrease in fibrillar and non-fibrillar collagen expression suggesting that macrophages also contribute to this absence of fibrosis in obesity although these results have not been validated at protein levels. Finally, in agreement with the lack of fibrosis, the number of myofibroblast precursors subset (MSCA1−/CD271+) that we previously described [27] was not altered in patients with obesity. Moreover, we found no increased expression of TGF-β1, a profibrotic cytokine inducing myofibrogenesis, as well as α-SMA, expressed by myofibroblasts, at the mRNA level in SVF fraction of MAT in obesity compared to the other group. This was confirmed at the protein level for TGF-β1 using ELISA assay. This coordinated cellular response leading to an absence of fibrosis in obesity might contribute to explain the relative healthy expansion of MAT found in our study. This study is in apparent contradiction with previous studies showing increased in collagen bundles and peri-cellular fibrosis in MAT of patients with obesity [24]. These differences are unlikely to be explained by differences in the BMI of the patients (comprised between 30 and 35 kg/m2 [19, 23] like in our cohort). However, it is important to note that our cohort includes patients from Europe whereas the two other studies were performed in the USA [19, 23]. Therefore, additional differences in terms of diet, lifestyle or even ethnic origin could explain these divergent results.
Evidence from mouse models deficient in ECM (such as COL6) or overexpressing ECM remodeling proteins (MMP14) has shown that reducing mechanical constraints allows AT expansion without inflammation [39]. We have previously demonstrated that mammary adipocyte size was increased in patients with overweight and obesity and that a positive correlation existed between adipocyte size and BMI [18]. According to adipocyte hypertrophy, leptin mRNA expression was increased, and adiponectin mRNA expression was decreased in isolated adipocytes from MAT of patients with obesity compared to those who are lean (Supplementary Fig. 2). We found that secretion of pro-inflammatory cytokines, including TNF-α, IL-6, IL-8, monocyte chemoattractant protein-1 (MCP-1) and PAI-1 was not increased in MAT-CM in obesity, and a decrease in PAI-1 was even observed, although not significant. While CLS, which contain IL6-positive CD11c macrophages, are significantly more numerous in the MAT of patients with overweight/obesity than in those who are lean [17, 18], their low frequency is probably not sufficient to alter the overall secretion of pro-inflammatory cytokines at tissue level. In line with these results, we also recently demonstrated that basal lipolysis was not increased in mammary adipocytes isolated from women with obesity [40] in opposition to the results obtained in other adipose depots [14, 15].
Taken together, our results highlight the very peculiar phenotype of human MAT in obesity that, in opposition to other adipose depots, displays a lack of fibrosis and inflammation. From a finalistic point of view, these results could be explained by the fact that adipocytes from MAT undergo pronounced size changes during lactation and subsequent involution, which is one of the most marked physiological examples of adipose adaptation to external signals [3], which could also modify their response to stress such as obesity. Of note, these results were obtained in cancer-free MAT and do not preclude changes that may occur in obesity in the vicinity of tumors. Convincing results have been obtained that demonstrate an increased desmoplastic reaction in tumors from patients with obesity relative to tumor from patients who are lean that was associated to collagen-dependent structural changes [24]. Recent results using bulk transcriptomic profile have also revealed an elevated and unresolved inflammation of the breast tumor microenvironment associated with obesity [41]. Therefore, additional experiments are clearly needed to characterize in depth the cellular and secretory changes of MAT induced by obesity both at distance and at proximity of the tumors.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Neville MC, Medina D, Monks J, Hovey RC. The mammary fat pad. J Mammary Gland Biol Neoplasia. 1998;3:109–16.
Zwick RK, Guerrero-Juarez CF, Horsley V, Plikus MV. Anatomical, physiological, and functional diversity of adipose tissue. Cell Metab. 2018;27:68–83.
Hovey RC, Aimo L. Diverse and active roles for adipocytes during mammary gland growth and function. J Mammary Gland Biol Neoplasia. 2010;15:279–90.
Parmar H, Cunha GR. Epithelial-stromal interactions in the mouse and human mammary gland in vivo. Endocr Relat Cancer. 2004;11:437–58.
Wang QA, Song A, Chen W, Schwalie PC, Zhang F, Vishvanath L, et al. Reversible de-differentiation of mature white adipocytes into preadipocyte-like precursors during lactation. Cell Metab. 2018;28:282–8.e3.
Renehan AG, Zwahlen M, Egger M. Adiposity and cancer risk: new mechanistic insights from epidemiology. Nat Rev Cancer. 2015;15:484–98.
Chan DSM, Vieira AR, Aune D, Bandera EV, Greenwood DC, McTiernan A, et al. Body mass index and survival in women with breast cancer-systematic literature review and meta-analysis of 82 follow-up studies. Ann Oncol. 2014;25:1901–14.
Neuhouser ML, Aragaki AK, Prentice RL, Manson JE, Chlebowski R, Carty CL, et al. Overweight, obesity, and postmenopausal invasive breast cancer risk: a secondary analysis of the women’s health initiative randomized clinical trials. JAMA Oncol. 2015;1:611–21.
Harris BHL, Macaulay VM, Harris DA, Klenerman P, Karpe F, Lord SR, et al. Obesity: a perfect storm for carcinogenesis. Cancer Metastasis Rev. 2022;41:491–515.
Dirat B, Bochet L, Dabek M, Daviaud D, Dauvillier S, Majed B, et al. Cancer-associated adipocytes exhibit an activated phenotype and contribute to breast cancer invasion. Cancer Res. 2011;71:2455–65.
Wang YY, Attané C, Milhas D, Dirat B, Dauvillier S, Guerard A, et al. Mammary adipocytes stimulate breast cancer invasion through metabolic remodeling of tumor cells. JCI Insight. 2017;2:e87489.
Wang YY, Lehuédé C, Laurent V, Dirat B, Dauvillier S, Bochet L, et al. Adipose tissue and breast epithelial cells: a dangerous dynamic duo in breast cancer. Cancer Lett. 2012;324:142–51.
Attané C, Muller C. Drilling for oil: tumor-surrounding adipocytes fueling cancer. Trends Cancer. 2020;6:593–604.
Kahn CR, Wang G, Lee KY. Altered adipose tissue and adipocyte function in the pathogenesis of metabolic syndrome. J Clin Invest. 2019;129:3990–4000.
Rosen ED, Spiegelman BM. What we talk about when we talk about fat. Cell 2014;156:20–44.
Marcelin G, Ferreira A, Liu Y, Atlan M, Aron-Wisnewsky J, Pelloux V, et al. A PDGFRα-mediated switch toward CD9high adipocyte progenitors controls obesity-induced adipose tissue fibrosis. Cell Metab. 2017;25:673–85.
Morris PG, Hudis CA, Giri D, Morrow M, Falcone DJ, Zhou XK, et al. Inflammation and increased aromatase expression occur in the breast tissue of obese women with breast cancer. Cancer Prev Res. 2011;4:1021–9.
Vaysse C, Lømo J, Garred Ø, Fjeldheim F, Lofteroed T, Schlichting E, et al. Inflammation of mammary adipose tissue occurs in overweight and obese patients exhibiting early-stage breast cancer. NPJ Breast Cancer. 2017;3:19.
Laforest S, Ennour-Idrissi K, Ouellette G, Gauthier MF, Michaud A, Durocher F, et al. Associations between markers of mammary adipose tissue dysfunction and breast cancer prognostic factors. Int J Obes. 2005;45:195–205.
Springer NL, Iyengar NM, Bareja R, Verma A, Jochelson MS, Giri DD, et al. Obesity-associated extracellular matrix remodeling promotes a macrophage phenotype similar to tumor-associated macrophages. Am J Pathol. 2019;189:2019–35.
Sun X, Casbas-Hernandez P, Bigelow C, Makowski L, Joseph Jerry D, Smith Schneider S, et al. Normal breast tissue of obese women is enriched for macrophage markers and macrophage-associated gene expression. Breast Cancer Res Treat. 2012;131:1003–12.
Coradini D, Gambazza S, Oriana S, Ambrogi F. Gene expression profile of normal breast tissue and body mass index. Breast Cancer. 2021;28:488–95.
de Sousa Abreu R, Penalva LO, Marcotte EM, Vogel C. Global signatures of protein and mRNA expression levels. Mol Biosyst. 2009;5:1512–26.
Seo BR, Bhardwaj P, Choi S, Gonzalez J, Andresen Eguiluz RC, Wang K, et al. Obesity-dependent changes in interstitial ECM mechanics promote breast tumorigenesis. Sci Transl Med. 2015;7:301ra130.
Colleluori G, Perugini J, Barbatelli G, Cinti S. Mammary gland adipocytes in lactation cycle, obesity and breast cancer. Rev Endocr Metab Disord. 2021;22:241–55.
Roumiguié M, Estève D, Manceau C, Toulet A, Gilleron J, Belles C, et al. Periprostatic adipose tissue displays a chronic hypoxic state that limits its expandability. Am J Pathol. 2022;192:926–42.
Estève D, Boulet N, Belles C, Zakaroff-Girard A, Decaunes P, Briot A, et al. Lobular architecture of human adipose tissue defines the niche and fate of progenitor cells. Nat Commun. 2019;10:2549.
Love MI, Huber W, Anders S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 2014;15:550.
Ben-Ari Fuchs S, Lieder I, Stelzer G, Mazor Y, Buzhor E, Kaplan S, et al. GeneAnalytics: an integrative gene set analysis tool for next generation sequencing, RNAseq and microarray data. Omics J Integr Biol. 2016;20:139–51.
Ayoub I, Dauvilliers Y, Barateau L, Vermeulen T, Mouton-Barbosa E, Marcellin M, et al. Cerebrospinal fluid proteomics in recent-onset Narcolepsy type 1 reveals activation of the complement system. Front Immunol. 2023;14:1108682.
Duguet F, Locard-Paulet M, Marcellin M, Chaoui K, Bernard I, Andreoletti O, et al. Proteomic analysis of regulatory T cells reveals the importance of Themis1 in the control of their suppressive function. Mol Cell Proteom. 2017;16:1416–32.
Bouyssié D, Hesse AM, Mouton-Barbosa E, Rompais M, Macron C, Carapito C, et al. Proline: an efficient and user-friendly software suite for large-scale proteomics. Bioinformatics. 2020;36:3148–55.
Bourlier V, Zakaroff-Girard A, Miranville A, De Barros S, Maumus M, Sengenes C, et al. Remodeling phenotype of human subcutaneous adipose tissue macrophages. Circulation. 2008;117:806–15.
Clement E, Lazar I, Attané C, Carrié L, Dauvillier S, Ducoux-Petit M, et al. Adipocyte extracellular vesicles carry enzymes and fatty acids that stimulate mitochondrial metabolism and remodeling in tumor cells. EMBO J. 2020;39:e102525.
Marcelin G, Silveira ALM, Martins LB, Ferreira AV, Clément K. Deciphering the cellular interplays underlying obesity-induced adipose tissue fibrosis. J Clin Invest. 2019;129:4032–40.
Marcos-Garcés V, Harvat M, Molina Aguilar P, Ferrández Izquierdo A, Ruiz-Saurí A. Comparative measurement of collagen bundle orientation by Fourier analysis and semiquantitative evaluation: reliability and agreement in Masson’s trichrome, Picrosirius red and confocal microscopy techniques. J Microsc. 2017;267:130–42.
Khan T, Muise ES, Iyengar P, Wang ZV, Chandalia M, Abate N, et al. Metabolic dysregulation and adipose tissue fibrosis: role of collagen VI. Mol Cell Biol. 2009;29:1575–91.
Xia T, Shen Z, Cai J, Pan M, Sun C. ColXV aggravates adipocyte apoptosis by facilitating abnormal extracellular matrix remodeling in mice. Int J Mol Sci. 2020;21:959.
Sun K, Tordjman J, Clément K, Scherer PE. Fibrosis and adipose tissue dysfunction. Cell Metab. 2013;18:470–7.
Rebeaud M, Bouche C, Dauvillier S, Attané C, Arellano C, Vaysse C, et al. A novel 3D culture model for human primary mammary adipocytes to study their metabolic crosstalk with breast cancer in lean and obese conditions. Sci Rep. 2023;13:4707.
Nguyen HL, Geukens T, Maetens M, Aparicio S, Bassez A, Borg A, et al. Obesity-associated changes in molecular biology of primary breast cancer. Nat Commun. 2023;14:4418.
Acknowledgements
This work benefited from the Toulouse Réseau Imagerie (TRI)-RIO Optical Imaging Platform at the Institute of Pharmacology and Structural Biology (Genotoul, Toulouse, France). We thank Mathilde Lacombe (IPBS, Toulouse) for her writing assistance. We thank Jessica Tran for her contribution in the hydroxyproline quantification experiments.
Funding
This study was funded by the Ligue Contre le Cancer (Comité Midi-Pyrénées), and by the Institut National Contre le Cancer (Programme d’actions intégrées de recherche (PAIR)—Obésités et Cancers, INCa_18711). This study was funded in part by the French Ministry of Research with the Investissement d’Avenir Infrastructures Nationales en Biologie et Santé program (ProFI, Proteomics French Infrastructure project, ANR-10-INBS-08) (to OBS). LO received a master fellowship (Program “Espoirs de la recherche”) from the Fondation pour la Recherche Médicale (FRM). MR received a PhD fellowship from the Ligue Nationale contre le Cancer and from the Fondation pour la Recherche Médicale (FRM). CA received a master fellowship from the Association pour la Recherche sur le Cancer (ARC).
Author information
Authors and Affiliations
Contributions
FF, MR and CB performed and analyzed most of the experiments presented in the manuscript and prepared the figures. SD and CA performed and prepared the figures of the imaging experiments (3D picrosirius staining). LO and RD performed the flow cytometry experiments with the help of JF under the supervision of AB. LO prepared the samples for proteomic analysis, FF, MDP and EMB performed the analysis of the proteomic data under the supervision of OBS. RN and FF performed the analysis of the RNA-seq. CF performed the Trichrome Masson staining which was analyzed by CV and DE. CA, CB and CV supervised the collection of human mammary adipose tissue samples and MM participated to tissue processing. AB, CV, FF, and CM supervised the study and wrote the manuscript. FF and MR performed the experiments required for the revision process. All the authors reviewed the manuscript. All the authors agreed with the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g., a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fallone, F., Rebeaud, M., Bouche, C. et al. Lack of fibro-inflammatory response in human mammary adipose tissue in obesity. Int J Obes 49, 809–818 (2025). https://doi.org/10.1038/s41366-024-01705-1
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41366-024-01705-1