Abstract
Background
Obesity is a major risk-factor for adverse pregnancy outcomes. While the 2017 American College of Cardiology/American Heart Association (ACC/AHA) classification of normal and abnormal blood pressure (BP) outside pregnancy has been suggested for use in pregnancy, the impact on adverse outcomes has not been examined specifically in women with obesity.
Methods
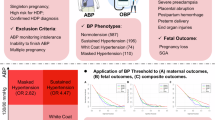
The UK Pregnancies Better Eating and Activity Trial (UPBEAT) enroled women with a body mass index (BMI) ≥ 30 kg/m2. In secondary analyses, maximal antenatal BP was categorised by 2017 ACC/AHA criteria: ‘Normal’ BP (systolic [sBP] <120 mmHg and diastolic [dBP] <80 mmHg), ‘Elevated’ BP (sBP 120–129 mmHg and dBP <80 mmHg), ‘Stage 1 hypertension’ (sBP 130–139 mmHg and/or dBP 80-89 mmHg), and ‘Stage 2 hypertension’ (sBP ≥140 mmHg and/or dBP ≥90 mmHg, non-severe [sBP 140-159 mmHg and/or dBP 90–109 mmHg] and severe (sBP ≥160 mmHg and/or dBP ≥110 mmHg). Main outcomes were preterm birth, postpartum haemorrhage (PPH), birthweight <10th centile (small-for-gestational age, SGA), and neonatal intensive care unit (NICU) admission. Associations with adverse outcomes were adjusted for UPBEAT intervention, maternal age, booking BMI, ethnicity, parity, smoking, alcohol, and previous pre-eclampsia or gestational diabetes. Diagnostic test properties (positive and negative likelihood ratios, -LR and +LR) were assessed as individual categories (vs. ‘Normal’ BP), and as threshold values.
Results
Severe ‘Stage 2 hypertension’ (vs. BP < 160/110 mmHg) was associated with PPH (RR 2.57 (1.35, 4.86)) and SGA (RR 2.52 (1.05, 6.07)) only in unadjusted analyses. No outcomes were associated with ‘Stage 1 hypertension’ or ‘Elevated BP’. All +LR were <5.0 and -LR ≥ 0.20, indicating that no BP threshold was useful as a diagnostic test to detect preterm birth, PPH, SGA, or NICU admission.
Conclusions
Among pregnant women with obesity, we found no evidence that lowering the antenatal BP considered to be abnormal (from 140/90 mmHg) would assist in identifying women and babies at risk.
Similar content being viewed by others
Introduction
In 2017, the American College of Cardiology (ACC) and American Heart Association (AHA), redefined what constitutes an abnormal blood pressure (BP) outside pregnancy [1]. This was done in recognition of the increased cardiovascular risks associated with a BP lower than the previous threshold for hypertension. ‘Normal BP’ was defined as a systolic BP (sBP) < 120 mmHg and a diastolic BP (dBP) < 80 mmHg. ‘Elevated BP’ was defined as sBP of 120–129 mmHg with a dBP <80 mmHg. ‘Stage 1 hypertension’ was defined as sBP 130–139 mmHg and/or dBP 80–89 mmHg. The prior threshold for hypertension (sBP ≥140 mmHg and/or dBP ≥90 mmHg) was relabelled as ‘Stage 2 hypertension’.
Within the United States or elsewhere, no clinical practice guidelines in pregnancy define BP according to the 2017 ACC/AHA criteria [2,3,4]. However, several studies have reported an association between ‘Elevated BP’ or ‘Stage 1 hypertension’ (as for ‘Stage 2 hypertension’) and a heightened risk of adverse pregnancy outcomes [5,6,7,8,9,10,11,12,13]. Recent systematic reviews of these data have demonstrated that despite these associations, lowering the threshold for abnormal BP in pregnancy would not aid clinicians in identifying mothers and babies at risk [14, 15]; all included studies had a minority of women with obesity.
With rising rates of overweight and obesity, and the heightened risk of hypertensive disease in pregnant women with obesity, it is important to evaluate whether the association of 2017 ACC/AHA BP categories with adverse pregnancy outcomes may be different among pregnant women with obesity, compared with the general maternity population. BP measurement is readily available and of low cost, allowing easy risk stratification to identify women at particular risk of adverse pregnancy outcomes and bringing the potential to mitigate that risk through preventative measures and/or enhanced surveillance.
The UK Pregnancies Better Eating and Activity Trial (UPBEAT) was a large, multicentre, randomised trial of women with obesity in early pregnancy, allocated to a behavioural intervention (vs standard care), to assess the impact on obesity-related adverse pregnancy outcomes [16]. We undertook a secondary analysis of UPBEAT data, to evaluate the relationship between BP categorised by ACC/AHA BP criteria and pregnancy outcomes in women with obesity.
Methods
Study design and participants
The methods of UPBEAT have been published previously [17]. In brief, between March 2009 and June 2014, 1555 women were recruited with maternal age ≥16 years, singleton pregnancy at 15+0-18+6 weeks’ gestational age, and body mass index (BMI) ≥ 30 kg/m2; women were excluded if they were taking metformin, or had diabetes mellitus or another condition (e.g., chronic hypertension currently treated with antihypertensive therapy) that increased the risk of adverse pregnancy outcomes. One participant was excluded after enrolment in another trial.
Intervention
Following written, informed consent, women were randomised to a complex behavioural intervention, focusing on a healthy diet and physical activity, or to standard antenatal care.
Outcomes and data collection
Antenatal registration data (including measurement of BP and proteinuria) were recorded from clinical records. Study visits were conducted at trial entry between 15+0-18+6 and then again at 27+0-28+6, and 34+0-36+6 weeks’ gestation, including blood collection for cardiovascular markers.
BP was measured according to a standardised protocol, using the automated Microlife BP3BTo-A BP monitor (Microlife, Widnau, Switzerland) validated for use in pregnancy and pre-eclampsia [18], with an appropriately-sized cuff. The last BP before delivery was recorded from clinical records.
The co-primary outcomes were gestational diabetes mellitus (GDM) and large-for-gestational age infants of which neither differed between trial arms, although the intervention (vs. usual care) resulted in less gestational weight gain and more physical activity [16].
Outcomes were abstracted from clinical records after birth. Pre-eclampsia was defined as gestational hypertension (i.e., systolic BP [sBP] ≥140 mmHg or diastolic BP [dBP] ≥90 mmHg, measured twice, at least four hours apart at ≥20 weeks) and new-onset proteinuria (i.e., ≥300 mg/24 h, dipstick proteinuria ≥2+, or a spot urine protein:creatinine ratio ≥30 mg/mmol) [16]. The World Health Organisation (WHO) classifies obesity as a BMI ≥ 30 kg/m2, with obesity further subdivided into obesity class I (BMI 30–34.9 kg/m2), obesity class II (BMI 35–39.9 kg/m2) and obesity class III (BMI ≥ 40 kg/m2) [19].
Ethical approval for UPBEAT was granted by the NHS Research Ethics Committee (reference 09/H0802/5). All methods were performed in accordance with the relevant guidelines and regulations.
This secondary analysis
Use of UPBEAT data for this project was approved by the UPBEAT Scientific Advisory Committee (Research Application Form reference 077). In this analysis, we included UPBEAT participants with data on BP from at least one study visit and the adverse pregnancy outcomes of interest. We sought to investigate whether adjusting BP thresholds for pregnant women with obesity would improve the prediction of adverse maternal and perinatal outcomes.
BP was classified according to the highest antenatal BP, using 2017 ACC/AHA criteria: ‘Normal’ (sBP <120 mmHg and dBP <80 mmHg). ‘Elevated’ (sBP 120–129 mmHg with dBP <80 mmHg), ‘Stage 1 hypertension’ (sBP 130–139 mmHg and/or dBP 80–89 mmHg), and ‘Stage 2 hypertension’ (sBP ≥140 mmHg and/or dBP ≥90 mmHg). ‘Stage 2 hypertension’ was further categorised into ‘non-severe’ (sBP 140-159 mmHg and/or dBP 90-109 mmHg) and ‘severe’ (sBP ≥160 mmHg and/or dBP ≥110 mmHg).
The main outcomes of interest were preterm birth (PTB), postpartum haemorrhage (PPH), birth weight <10th centile (small-for-gestational age, SGA), and neonatal intensive care unit (NICU) admission; none of these differed by trial arm in UPBEAT [16]. PTB was birth at <37+0 weeks’ gestation. PPH was an estimated blood loss ≥1000 mL. The following maternal core outcomes in hypertensive pregnancy were unavailable: stroke, eclampsia, blindness, pulmonary oedema, respiratory failure, hepatic haematoma or rupture, acute kidney injury or dialysis, elevated liver enzymes (aspartate or alanine transaminase >40IU/L), platelet count <100 × 109/L, and intensive care unit admission. The following fetal/neonatal core variables were unavailable: respiratory morbidity.
For each trial participant, maximum antenatal BP was categorised according to the 2017 ACC-AHA criteria. Baseline demographics and past medical and obstetric history were summarised for the trial cohort overall, and according to the ACC-AHA BP categories; frequencies and percentages were used for categorical variables, and medians and interquartile ranges (25th, 75th centiles) for continuous variables.
Statistical analysis
To assess the association between maximum BP and adverse pregnancy outcomes, we calculated adjusted risk ratios (aRR) using robust Poisson models. Confounders were: maternal age (yr), BMI (kg/m2), ethnicity (White British, Black, Asian and Other), parity (nulliparous/multiparous), smoking status (yes/no to ongoing in current pregnancy), alcohol use (yes/no to ongoing in current pregnancy), previous pre-eclampsia, and previous GDM; these were selected as variables related to BP level and outcomes, without being on the causal pathway.
The relationship between BP category and adverse outcomes were assessed in two ways. First, each BP category was treated as mutually exclusive from the others, and the risk ratio (RR) and 95% confidence interval (CI) [20] was calculated for each BP category relative to ‘Normal’ BP, using generalised estimating equations with a Poisson link function [21]. Second, analogous models were fit, but the lower limit of each category was treated as a BP cut off for the diagnosis of an abnormal BP, in the way that 140/90 mmHg is currently used; for example, for ‘Stage 1 hypertension’, the RR for each outcome was compared for women with sBP ≥130 mmHg and/or dBP ≥80 mmHg, and women with sBP <130 mmHg and dBP <80 mmHg. This analysis was repeated, adjusting for UPBEAT trial intervention group, maternal age, BMI at booking, ethnicity, parity, smoking status, alcohol use, previous pre-eclampsia, and previous GDM.
Also, for each new threshold for abnormal BP, diagnostic test properties were assessed, using sensitivity, specificity, and positive and negative likelihood ratios (+LR and -LR respectively). +LR was calculated as sensitivity/{1-specificity}, and -LR as {1-sensitivity}/specificity. LRs were considered diagnostically useful if +LR were ≥5.0 or -LR were <0.2 [22].
A sensitivity analysis was undertaken, restricting analyses to BP measurements taken under standardised conditions at study visits (and excluding BP measurements taken in routine clinical care, at antenatal care booking and again close to birth). We examined the impact on the association of each BP category (vs. ‘Normal’ BP) with adverse outcomes, as well as the diagnostic test properties of the BP threshold associated with each category.
All analyses were undertaken using R statistical software, with 95% confidence intervals (CIs) considered significant if they did not cross 1.0. No adjustment was made for multiple comparisons. As a secondary analysis of an existing dataset, no sample size calculation was undertaken.
Results
Of the 1554 women in UPBEAT, 1520 (97.8%) were included in this analysis (Fig. 1), following exclusion of 34 women with missing birth outcome data.
Table 1 (‘Overall’ column) shows that on average, UPBEAT participants were aged 30 years at booking, mostly White British, and more than half had a BMI consistent with at least class II obesity (≥35 kg/m2). Most women who were multiparous had a previous uncomplicated pregnancy, but family history was significant for at least one cardiovascular risk factor in almost half of women. Women had their first antenatal visit at an average of 10 weeks’ gestation, few conceived by artificial reproductive technologies, and just over 40% were nulliparous. Just over 10% were taking low-dose aspirin. Few reported being smokers or consuming alcohol. Half had been randomised to the intervention arm.
Table 1 (‘Antenatal BP’ columns) shows that few women were categorised as having ‘Normal’ BP (166, 10.9%) or ‘Elevated’ BP (252, 16.6%), with most women having ‘Stage 1 hypertension’ (614, 40.4%) or ‘Stage 2 hypertension’ (488, 32.1%; 28.0% non-severe and 4.1% severe). Many baseline and pregnancy characteristics differed according to BP category; women with ‘Normal’ BP or ‘Elevated’ BP had a lower mean BMI and were more likely to have WHO class I obesity (rather than III). Women with ‘Stage 1 hypertension’ or ‘Stage 2 hypertension’ were more likely to have a higher BMI, prior pre-eclampsia, and be on aspirin from their first antenatal visit.
Table 2 (‘Overall’ column) shows that on average, women delivered at 39 weeks’ gestation, with one-third undergoing labour induction and a similar number undergoing a Caesarean delivery. A clinical diagnosis of gestational hypertension or pre-eclampsia developed in 8.7% of women overall. There were no maternal deaths, abruption was rare, and a minority of women developed GDM or PPH. Most women delivered term, appropriately-grown babies who were not admitted to neonatal care (which was required most often for respiratory problems).
Table 2 (‘Antenatal BP’ columns) shows that many pregnancy characteristics differed by BP category, with higher BP associated with labour induction, instrumental vaginal birth or Caesarean section in labour, complications of gestational hypertension or PPH, and NICU admission. Placental abruption, stillbirth, and neonatal death were too infrequent to include in subsequent analyses of their relationship with BP category.
Table 3 shows that only Severe ‘Stage 2 hypertension’ was associated with higher risk of PPH (RR 2.57 (1.35, 4.86)) and SGA (RR 2.52 (1.05, 6.07), but only in unadjusted analyses. Elevated and ‘Stage 1 hypertension’ were not associated with outcomes. Adjusted and unadjusted values did not vary substantially.
Table 4 shows that only Severe ‘Stage 2 hypertension’ had a high specificity, and for all adverse outcomes. However, the sensitivity was very low (<10%). While ‘Normal’ BP had high sensitivity (>85%), specificity (<20%) was very low for the outcomes evaluated. None of the potential thresholds for abnormal BP (including the current 140/90 mmHg for ‘Stage 2 hypertension’) were useful as a diagnostic test to identify women at low or high risk of adverse outcomes (i.e., -LR ≥ 0.20 and +LR < 5.0); while this was based on point estimates, no lower limit of the 95% CI for -LR was <0.20, and no upper limit for +LR was ≥5.0.
In the sensitivity analysis restricted to BP measurements collected at study visits, the results were similar to those overall, in that only Severe ‘Stage 2 hypertension’ was associated with adverse outcomes—but in this case, the association was with PTB in adjusted analyses (aRR 6.29 (1.97, 20.08)) (Table S1), and the +LR was good (9.57 (1.62, 56.60)), suggesting that risk was meaningfully increased (Table S2).
Discussion
Principal findings
In this population of pregnant women with obesity enrolled in a randomised trial of a diet and lifestyle intervention, our analyses found no association of the ACC/AHA BP categories with the adverse pregnancy outcomes of PPH, preterm birth, birthweight <10th centile, or NICU admission. However, in sensitivity analyses restricted to study visit BP measurements, Severe ‘Stage 2 hypertension’ was associated with PTB, and with a good +LR.
Results in the context of what is known
Measuring BP in women with overweight and obesity, can represent challenges in standardisation, particularly when routine measurements are relied on in study settings. The ACC/AHA emphasise the importance of an appropriately sized BP cuff [1], as used in UPBEAT. Using a cuff size that is too small is likely to result in an overestimation of BP. For example, using a standard-sized cuff (vs. a larger one as dictated by arm circumference) resulted in an extra 7% of women misdiagnosed with hypertension [23]. Also, with the larger cylindrically-shaped cuffs, inaccurate BP measurements can result from an uneven fit over the distal end of the upper arm; overestimation of BP and overdiagnosis of hypertension is then more likely [24]. For this reason, troncoconical cuffs are suggested outside pregnancy for persons with a mid-arm circumference above 42 cm [24,25,26]. The UPBEAT trial used a standardised approach to measure BP, including an appropriate cuff size.
Several authors have reviewed the relationships of 2017 ACC/AHA BP criteria and adverse pregnancy outcomes, with varied results [14, 15]. Our findings contrast with data from large population-based studies, including women of all BMI in pregnancy [6, 27], that have demonstrated an association between higher BP category and higher risk of adverse pregnancy outcomes, including preterm birth, SGA infants, and NICU admission evaluated in our study. There was a large degree of heterogeneity in this review, particularly looking at the background risk of the women, explained by both their demographics, and their individual health characteristics.
The average BMI of women included varied across these reports, with few studies including a significant proportion of women with obesity. Of included studies that controlled for BMI in their analyses, and reported both unadjusted and adjusted analyses, adjustment reduced the strength of association between BP categories and adverse pregnancy outcome [6,7,8,9,10,11,12,13, 28,29,30,31,32,33,34]. However, all adjusted for multiple confounders that included BMI but also commonly maternal age, parity, and race/ethnicity. Of studies that reported only adjusted analyses, none adjusted only for BMI.
The pattern of associations seen consistently throughout these studies was not seen in this analysis restricted only to women with obesity. This could be influenced by the misclassification of women because of difficulty in accurately measuring BP in obesity, or perhaps masked by the multifactorial interaction of obesity with the pathophysiology of adverse pregnancy outcomes [35]. However, this analysis confirms that a different BP threshold need not be applied for women with obesity, despite the difficulties in accurate BP measurement and complex interplay of risk factors in this high-risk population.
Of note, our sensitivity analysis restricted to study visit BP measurements confirmed the importance of Severe ‘Stage 2 hypertension as a risk factor for adverse outcomes.
Wu reported the pregnancy outcomes of 47,874 women with a singleton pregnancy, who had BP in pregnancy of less than 140/90 mmHg in early pregnancy [34]. They also excluded women with multiple pregnancy, stillbirth, renal disease, pre-existing diabetes and thyroid dysfunction, leaving a relatively low-risk cohort of women. Approximately a quarter of these women were multiparous, and although they presented individual analyses by BMI category, the highest category was a BMI of at least 25 kg/m2, which accounted for only 14% of their cohort. Within this group, using blood pressures from <20 weeks in the pregnancy, an association was seen for the hypertensive disorders with ‘Stage 1 hypertension’. The other pregnancy outcomes seen in this study were not reported on by BMI category. Similar findings were observed by Hauspurg, in a secondary analysis of the Nulliparous Pregnancy Outcome Study: Monitoring Mothers-to-be [8]. Based on BP in early pregnancy, and including a larger proportion of women with overweight and obesity, an association was again seen. No other pregnancy outcomes were stratified by BMI.
Obesity is an important risk factor for both hypertension and cardiovascular disease outside pregnancy, as well as hypertension and many adverse pregnancy outcomes [36]. It is likely that this is through similar mechanisms by which obesity influences the risk of metabolic syndrome and cardiovascular disease outside pregnancy [35]. The contribution of adipose tissue to insulin resistance, cytokine release and inflammation are all proposed contributors to the link between obesity and pre-eclampsia, in the same way that obesity is linked to cardiovascular disease outside pregnancy [35, 37]. There are also multiple associations between the dietary and lifestyle factors that contribute to obesity and pre-eclampsia, including low rates of physical activity, and a sub-optimal diet, including a high intake of refined sugars [35].
Clinical implications
BP thresholds below the current 140/90 mmHg did not identify women at increased risk of adverse outcomes in pregnancy complicated by obesity. While our findings confirm the importance of severe ‘Stage 2 hypertension’, they do not support a lowering of BP thresholds in pregnant women with obesity to identify those at increased risk of adverse pregnancy outcomes.
Research implications
This analysis has shown that the relationship between BP and adverse pregnancy outcome is different in a cohort of only women with obesity, compared with previous observations in cohorts of pregnant women with heterogeneous BMI. Future work should aim to evaluate, as much as possible, the complex interplay between risk factors for adverse pregnancy outcomes and the associations and contributors to overweight and obesity.
Strengths and limitations
Categorisation of BP was based on the highest BP measurement available throughout the pregnancy. However, in the UPBEAT trial, nearly 20% of values were missing for the third study visit, which is the latest in gestation. Given that the expected trajectory of BP throughout pregnancy is a gradual rise throughout third trimester, this could have led to the misclassification into a lower BP category and overestimation of any BP category-outcome effects. The BP values used at the first antenatal appointment and at last appointment were also from clinical care, not from the standardised measurements, done as part of the trial; however, sensitivity analyses excluding them produced similar results for all but severe ‘Stage 2 hypertension’ for which the association with adverse outcome was strengthened. Detailed information about BP medication was not available at each visit, however given that BP was classified according to the maximum measurement, this is unlikely to have changed groupings; UK guidelines until 2019 did not recommend treatment of BP until 150/100 mmHg, so it is unlikely that treatment has changed classification of these women. Treated hypertension should overestimate the treatment effect for BP thresholds below Stage 2 hypertension. Also, the incidence of preeclampsia in this cohort was low given that all women had obesity. This may have related to the fact that before 2019, the UK used only a restrictive definition of pre-eclampsia (based on only hypertension and new-onset proteinuria), trial participants were more likely to have BP measured properly with the appropriately-sized cuff, and as hypertension was not a focus of UPBEAT, a medical record diagnosis of pre-eclampsia (which is less reliable) was used; of note, while the UPBEAT lifestyle intervention (vs. usual care) did result in reduced gestational weight gain and increased physical activity, there was no between-group difference in pre-eclampsia (and gestational hypertension was not reported). The cause of preterm birth (iatrogenic or spontaneous) was not available. We were limited by the information recorded in the original trial, which did not include indication for caesarean section or the number of antenatal visits recorded.
Conclusions
This analysis has not demonstrated that lowering the BP value considered to be abnormal (from 140/90 mmHg) in women with obesity would assist in identifying women and babies at risk.
Data availability
The datasets analysed during the current study are available in from the UPBEAT Consortium. https://www.medscinet.net/upbeat/default.aspx.
References
Whelton PK, Carey RM, Aronow WS, Casey DE Jr., Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018;71:e13–e115.
Gestational Hypertension and Preeclampsia: ACOG Practice Bulletin, Number 222. Obstet Gynecol. 2020;135:e237–e60.
ACOG Practice Bulletin No. 203: Chronic Hypertension in Pregnancy. Obstet Gynecol. 2019;133:e26–e50.
National Institute for Health and Care Excellence: Guidelines. Hypertension in pregnancy: diagnosis and management. London: National Institute for Health and Care Excellence (NICE). Copyright © NICE 2019; 2019.
MOMFIT: A randomized clinical trial of an intervention to prevent excess gestational weight gain in overweight and obese women. Am J Obstet Gynecol. 2017;216:S2–3.
Bello NA, Zhou H, Cheetham TC, Miller E, Getahun DT, Fassett MJ, et al. Prevalence of hypertension among pregnant women when using the 2017 American College of Cardiology/American Heart Association Blood Pressure Guidelines and Association with Maternal and Fetal Outcomes. JAMA Netw Open. 2021;4:e213808.
Greenberg VR, Silasi M, Lundsberg LS, Culhane JF, Reddy UM, Partridge C, et al. Perinatal outcomes in women with elevated blood pressure and stage 1 hypertension. Am J Obstet Gynecol. 2020;224:521.e1–e11.
Hauspurg A, Parry S, Mercer BM, Grobman W, Hatfield T, Silver RM, et al. Blood pressure trajectory and category and risk of hypertensive disorders of pregnancy in nulliparous women. Am J Obstet Gynecol. 2019;221:277.e1–.e8.
Hauspurg A, Sutton EF, Catov JM, Caritis SN. Aspirin effect on adverse pregnancy outcomes associated with stage 1 hypertension in a high-risk cohort. Hypertension. 2018;72:202–7.
He D, Wu S, Zhao H, Zheng Z, Zhang W. High normal blood pressure in early pregnancy also contribute to early onset preeclampsia and severe preeclampsia. Clin Exp Hypertens. 2018;40:539–46.
Hu J, Li Y, Zhang B, Zheng T, Li J, Peng Y, et al. Impact of the 2017 ACC/AHA guideline for high blood pressure on evaluating gestational hypertension-associated risks for newborns and mothers. Circ Res. 2019;125:184–94.
Huai J, Lin L, Juan J, Chen J, Li B, Zhu Y, et al. Preventive effect of aspirin on preeclampsia in high-risk pregnant women with stage 1 hypertension. J Clin Hypertens. 2021;23:1060–7.
Li Q, Zheng L, Gu Y, Jiang D, Wang G, Li J, et al. Early pregnancy stage 1 hypertension and high mean arterial pressure increased risk of adverse pregnancy outcomes in Shanghai, China. J Hum Hypertens. 2021;36:917–24.
Slade LJ, Mistry HD, Bone JN, Wilson M, Blackman M, Syeda N, et al. American College of Cardiology/American Heart Association blood pressure categories—a systematic review of the relationship with adverse pregnancy outcomes in the first half of pregnancy. Am J Obstetr Gynecol. 2022;228:418-29.e34.
Slade L, Wilson M, Mistry HD, Bone JN, Bello N, Blackman M, et al. The 2017 American College of Cardiology/American Heart Association blood pressure categories in the second half of pregnancy—a systematic review of their association with adverse pregnancy outcomes. Am J Obstet Gynecol. 2023;229;101–17.
Poston L, Bell R, Croker H, Flynn AC, Godfrey KM, Goff L, et al. Effect of a behavioural intervention in obese pregnant women (the UPBEAT study): a multicentre, randomised controlled trial. Lancet Diabetes Endocrinol. 2015;3:767–77.
Briley AL, Barr S, Badger S, Bell R, Croker H, Godfrey KM, et al. A complex intervention to improve pregnancy outcome in obese women; the UPBEAT randomised controlled trial. BMC Pregn Childbirth. 2014;14:74.
Clark K, Snowball O, Nzelu D, Kay P, Kametas NA. Validation of the microlife WatchBP Home blood pressure device in pregnancy for medium and large arm circumferences. Blood Press Monit. 2018;23:171–4.
Weir CB, Jan A. BMI classification percentile and cut off points. StatPearls. Treasure Island (FL): StatPearls Publishing. Copyright © 2023, StatPearls Publishing LLC; 2023.
Deeks JJ, Altman DG. Diagnostic tests 4: likelihood ratios. BMJ. 2004;329:168–9.
Zou GY, Donner A. Extension of the modified Poisson regression model to prospective studies with correlated binary data. Stat Methods Med Res. 2013;22:661–70.
Jaeschke R, Guyatt GH, Sackett DL. Users’ guides to the medical literature. III. How to use an article about a diagnostic test. B. What are the results and will they help me in caring for my patients? The Evidence-Based Medicine Working Group. JAMA. 1994;271:703–7.
Kho CL, Brown MA, Ong SL, Mangos GJ. Blood pressure measurement in pregnancy: the effect of arm circumference and sphygmomanometer cuff size. Obstet Med. 2009;2:116–20.
Palatini P, Benetti E, Fania C, Ermolao A, Spinella P, Battista F, et al. Effect of the shape of the cuff on blood pressure measurement in people with large arms. Blood Press. 2020;29:241–6.
Siddiqui M, Calhoun DA. Blood pressure measurement challenges in severely obese patients. Am J Hypertens. 2018;32:139–40.
Bonso E, Saladini F, Zanier A, Benetti E, Dorigatti F, Palatini P. Accuracy of a single rigid conical cuff with standard-size bladder coupled to an automatic oscillometric device over a wide range of arm circumferences. Hypertens Res. 2010;33:1186–91.
Reddy M, Rolnik DL, Harris K, Li W, Mol BW, Da Silva Costa F, et al. Challenging the definition of hypertension in pregnancy: a retrospective cohort study. Am J Obstet Gynecol. 2020;222:606.e1–.e21.
Darwin KC, Federspiel JJ, Schuh BL, Baschat AA, Vaught AJ. ACC-AHA diagnostic criteria for hypertension in pregnancy identifies patients at intermediate risk of adverse outcomes. Am J Perinatol. 2020;38:e249-e255.
Sutton EF, Hauspurg A, Caritis SN, Powers RW, Catov JM. Maternal outcomes associated with lower range stage 1 hypertension. Obstet Gynecol. 2018;132:843–9.
Porcelli BA, Diveley E, Meyenburg K, Woolfolk C, Rosenbloom JI, Raghuraman N, et al. A new definition of gestational hypertension? New-onset blood pressures of 130 to 139/80 to 89 mm Hg after 20 weeks of gestation. Am J Obstet Gynecol. 2020;223:442.e1–.e7.
Sabol BA, Porcelli B, Diveley E, Meyenburg K, Woolfolk C, Raghuraman N, et al. Defining the risk profile of women with stage 1 hypertension: a time to event analysis. Am J Obstet Gynecol. 2021;3:100376.
Sutton EF, Rogan SC, Lopa S, Sharbaugh D, Muldoon MF, Catov JM. Early pregnancy blood pressure elevations and risk for maternal and neonatal morbidity. Obstet Gynecol. 2020;136:129–39.
McLaren RA, Atallah F, Persad VVD, Narayanamoorthy S, Gougol N, Silver M, et al. Pregnancy outcomes among women with American College of Cardiology—American Heart Association defined hypertension. J Matern Fetal Neonatal Med. 2021:34:4072–102.
Wu D-D, Gao L, Huang O, Ullah K, Guo M-X, Liu Y, et al. Increased adverse pregnancy outcomes associated with stage 1 hypertension in a low-risk cohort: evidence from 47,874 cases. Hypertension. 2020;75:772–80.
Roberts JM, Bodnar LM, Patrick TE, Powers RW. The role of obesity in preeclampsia. Pregnancy Hypertens. 2011;1:6–16.
Schummers L, Hutcheon JA, Bodnar LM, Lieberman E, Himes KP. Risk of adverse pregnancy outcomes by prepregnancy body mass index: a population-based study to inform prepregnancy weight loss counseling. Obstet Gynecol. 2015;125:133–43.
Van Gaal LF, Mertens IL, De Block CE. Mechanisms linking obesity with cardiovascular disease. Nature. 2006;444:875–80.
Acknowledgements
We thank the UPBEAT participants for their participation in the trial. UPBEAT was supported by a National Institute for Health Research (NIHR) (UK) Programme Grant for Applied Research Programme (RP-0407-10452). Support was also provided from the Biomedical Research Centre at Guy’s and St.Thomas’ NHS Foundation Trust and King’s College London, the Chief Scientist Office Scotland, Guy’s and St Thomas’ Charity and Tommy’s Charity (Registered charity no. 1060508). KMG is supported by the UK Medical Research Council (MC_UU_12011/4), the National Institute for Health Research (NIHR Senior Investigator (NF-SI-0515-10042) and NIHR Southampton Biomedical Research Centre (NIHR203319)) and Alzheimer’s Research UK (ARUK-PG2022A-008). The views expressed are those of the author and not necessarily those of the NIHR or the Department of Health and Social Care. LP is supported by the Medical Research Council. The funders had no role in study design, data collection, data analysis, data interpretation or writing of the final report. For the purpose of Open Access, the author has applied a Creative Commons Attribution (CC BY) licence to any Author Accepted Manuscript version arising from this submission. PvD, LAM and HDM are funded by The PRECISE Network from the UK Research and Innovation Grand Challenges Research Fund GROW Award scheme (MR/P027938/1) and PRECISE-DYAD from the NIHR–Wellcome Partnership for Global Health Research Collaborative Award (reference 217123/Z/19/Z).
Author information
Authors and Affiliations
Consortia
Contributions
All authors (LS, NS, HDM, JNB, MW, MB, LP, KMG, PvD, and LAM) contributed to the study design and protocol. Data analysis was conducted by JB and MW. The manuscript was drafted by LS and reviewed and revised by LS, NS, HDM, JNB, MW, MB, LP, KMG, PvD, and LAM.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Slade, L., Syeda, N., Mistry, H. et al. Do lower antenatal blood pressure cut-offs in pregnant women with obesity identify those at greater risk of adverse maternal and perinatal outcomes? A secondary analysis of data from the UK Pregnancies Better Eating and Activity Trial (UPBEAT). Int J Obes 49, 1523–1531 (2025). https://doi.org/10.1038/s41366-025-01803-8
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41366-025-01803-8