Abstract
Background
Body weight and health-outcome results of highly effective new GLP-1R agonist medicine trials are usually presented in scientific reports in the form of standard graphs and tables. These representations are not easily translated to what the average participant looked like or their health risks at the outset of the study and how improvements in adiposity and clinical measures changed with treatment. Two recently developed methods for visually presenting complex weight and health-risk information that encapsulate substantial amounts of clinical trial observations were recently developed that can potentially supplement and give new insights into conventional GLP-1R agonist scientific reports. The current study aim was to put these visual presentations into a demonstration format to explore if and to what extent they convey new or useful information beyond traditional graphical and tabular approaches.
Methods
The first developed approach was the capability of generating, with manifold regression, humanoid avatars with accurate anthropometric dimensions. The second developed approach, body roundness index (BRI), associates a person’s shape phenotype with high-risk adiposity components and multiple health outcomes; BRI can be displayed in a visual format. These two approaches were applied to produce visual representations of body size and shape in Surmount 1 average male and female participants (maximal-tolerated dose group) at baseline and after 72-weeks of tirzepatide treatment.
Results
Developed images revealed clear excess adiposity and high health-risk (BRI) at baseline with marked improvements, although not to within the healthy BMI (<25 kg/m2) and BRI ranges at 72 weeks, observations not evident in the published report. Avatar analyses revealed sexual dimorphism in regional shape (volume) changes with weight loss.
Conclusions
Visual presentation of new weight loss medicine trial results can supplement standard published reports by condensing substantial amounts of complex technical information in an easily understood format that can potentially yield new study insights.
Similar content being viewed by others
Introduction
The recent introduction of highly effective glucagon-like peptide 1 receptor (GLP-1R) agonists for managing excess adiposity is revolutionizing multiple aspects of clinical medicine [1]. Publications reporting these breakthrough drugs describe relative weight loss, beneficial medical effects, and adverse events in a standardized format [2,3,4,5]. Typically, the responses to active drug relative to placebo are summarized in tables and graphically as percent (%) or absolute weight changes over the specified protocol time-period. While these communication formats provide useful technical information, they fail to adequately convey a more holistic impression of exactly what the average participant looked like at the beginning and end of the study, or how their body shape shifted from an unhealthy to a healthier state.
To improve the visual representation of these groundbreaking results, we developed two novel imaging approaches that convey the average study participant’s three-dimensional (3D) optical image [6, 7] and health-related shape index [8] at baseline and at the end of the specified treatment protocol. The first approach allows the user to generate a participant’s 3D avatar using manifold regression analysis at the two key study timepoints [9]. Model predictor variables are easily acquired demographic and other characteristics and the developed avatars can be analyzed using software created specifically for this purpose [10, 11]. An earlier study demonstrated the accuracy of the predicted humanoid avatar body circumferences and other anthropometric dimensions relative to comparable ground-truth measurements [6].
The second novel method involved the development of a body roundness index (BRI) based on physics concepts that can be visually portrayed in simplified form [8]. The BRI establishes a participant’s shape and health risks relative to the healthy range. Multiple studies have now confirmed the predictive value of the BRI for morbidity and mortality endpoints [12,13,14].
Accordingly, the aim of the current study was to put these visual presentations into a demonstration format to explore if and to what extent they conveyed new or useful information beyond the traditional graphical approaches. To accomplish this aim, 3D avatars and corresponding BRIs were developed at baseline and 72 weeks with data from the pivotal phase 3 trial of the GLP-1R agonist tirzepatide [2].
Methods
Protocol
The 3D and BRI visual images were developed from data reported from the pivotal phase 3 study of tirzepatide, a novel glucose-dependent insulinotropic polypeptide and GLP-1R agonist for the treatment of people with obesity [2, 15, 16]. The study, Surmount 1, was a 72-week double-blind, randomized controlled trial of three weekly subcutaneous doses of tirzepatide (5, 10, and 15 mg) and placebo (ClinicalTrials.gov number, NCT04184622). The participant data presented in the current report is from the maximal tolerated dose (MTD) group combined from 10 and 15 mg dose groups [16]. The data reported herein were acquired from a post-hoc analysis presented at ENDO 2024 [16] and the 2024 European Association for the Study of Diabetes annual meeting [15]. Evaluated data included mean age, weight, and BMI at baseline and % weight loss at 72-weeks for males and females. A detailed analysis plan emerging from the publicly presented data is provided in Supplementary Information I. Waist circumference data was available at baseline, but not at follow-up. Accordingly, we derived values for the 72-week waist circumferences as described in Supplementary Information II. The sample was race/ethnically diverse and data was not extracted for individual groups.
Participants and Ethics
The participants enrolled in the study had a baseline BMI of ≥30 kg/m2 or ≥27 kg/m2 with minimally one weight-related comorbidity [2], other than diabetes. Additional baseline participant details are presented in the pivotal phase 3 study publication [2].
The study protocol was approved by local institutional review boards and the trial complied with the International Conference on Harmonization Good Clinical Practice guidelines and the Declaration of Helsinki. All participants provided written informed consent (2). The developments reported in the current investigation were approved by the Pennington Biomedical Research Center Institutional Review Board under the activities of National Institute of Health grant R01DK109008.
Image generation
Manifold regression models were used to predict the 3D humanoid avatars, as previously described [6, 7, 9], with four covariates including age, weight, height, and waist circumference at baseline and 72 weeks. The manifold regression analyses were performed in R version 4.2.1 (https://stat.ethz.ch/pipermail/rannounce/2020/000658.html; R Core Team, 2020). In this process, a shape model of the 3D avatars was created using principal components (PCs) that describe variations in the avatar’s shapes. The PCs used are core features of the shapes that capture the most important variations. These PCs were then adjusted based on individual features such as weight and height using a manifold equation. The person’s 3D shape is then generated after adjusting for the selected individual features. The 3D avatar can be processed further using Universal Software [10, 11] to acquire anthropometric body dimensions (6 circumferences, 7 volumes, and 7 surface areas) at standard anatomic locations that we showed in an earlier report are accurate relative to ground-truth measurements from a 20-camera 3D optical scanner [6]. Only the predicted changes in body volumes are presented in the current report in association with the 3D avatars; circumference and surface area observations are presented in Supplementary Information III.
The BRI models human body shape as an ellipse or an oval that captures body girth (waist circumference) in relation to height [8, 17]. The deviations of ellipses from circles are characterized by their eccentricity, a unitless term that quantifies their degree of circularity; values range between 0 and 1, with 0 characterizing a perfect circle, and 1, a vertical line. Since small differences in eccentricity can be difficult to distinguish, the values are mapped onto a range from 1 to 20. Larger values of BRI are associated with rounder individuals while values closer to 1 correspond to more narrowly shaped, lean individuals. The BRI is represented as a normalized elliptical image of body shape with varying degrees of roundness. A healthy zone is indicated in green, and a solid black line marks the individual’s current zone, providing a clear visual portrayal of their degree of adiposity and associated health risks.
Our analyses included baseline and 72-week 3D humanoid and corresponding BRI images for the average Surmount 1 male and female participants based on their respective ages, weights, heights, and waist circumferences.
Results
Sample
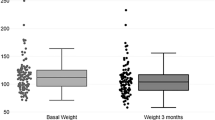
Surmount-1 included 2539 participants, 825 males and 1714 females [2](Jastreboff). The reported weight changes at 72 weeks included 813 males and 1699 females, retention rates of 98.5% and 99.1%, respectively [15, 16]. Baseline and 72-week sample characteristics are presented in Table 1. The sample sizes of the MTD groups were unavailable. Body mass index in the males at baseline in the MTD group was 37.6 kg/m2 and decreased by 18.1–30.8 kg/m2 at 72-weeks. Corresponding results in females were 38.2 kg/m2, 24.6%, and 28.8 kg/m2. According to our estimates, waist circumference decreased by 17.0 cm in the males and 21 cm in the females at 72-weeks.
Image analyses
The developed 3D avatars for males and females are shown in Figs. 1, 2, respectively, along with corresponding BRIs. The baseline and 72-week images are superimposed in Fig. 3, showing the changes in body size and shape over the course of the treatment protocol. Body mass index and waist circumference data are presented within each figure at the corresponding timepoints.
The participant age, weight, height, and waist circumference (WC) as outlined in Table 1 were used to generate the 3D images with manifold regression. BMI is body mass index. Waist circumference at the 72-week evaluation was predicted using a multiple regression model shown in Supplementary Information II. Data were reported earlier by Chao et al. [16] and Garcia-Perez [15].
The male image in Fig. 1 clearly shows excess weight at baseline consistent with a BMI of 37.6 kg/m2 (obesity is defined as BMI ≥ 30 kg/m2) and BRI at the “unhealthy” level of 7.6, clearly outside of the healthy range of about 4-5 shown by the green ellipse. While the relative BMI reduction of 18.1% is substantial, the 72-week image still shows some degree of excess weight, again consistent with a BMI in the obese range of 30.8 kg/m2 while BRI, shown outside the healthy green ellipse is at 5.2. The male images, combined with the objective measurements, thus shows that the average male in the reported study [2, 16] had substantial improvements in body size and shape along with the BRI health marker, but some remaining progress is needed if the target is to be at what are recognized as a “healthy” weights (BMI < 25 kg/m2) and shapes (BRI < 4-5).
The female image in Fig. 2 also clearly shows excess weight at baseline consistent with a BMI even higher than the male at 38.2 kg/m2 and BRI at the “unhealthy” level of 7.6, also clearly outside of the healthy range shown by the green ellipse. The female’s relative BMI reduction of 24.6% is substantial, and the 72-week image still shows a small degree of excess weight, although now BMI has moved from the obesity into an “overweight” level (>27 kg/m2) of 28.8 kg/m2; BRI also moved into the edge of the healthy green ellipse at a level of 4.5. The female images, combined with the objective measurements, shows that the average female in the reported study [2, 16] had substantial improvements in body size and shape along with the BRI health marker, moving closer to what might be considered target BMIs and BRIs.
The 3D avatars processed with the Universal Software are shown in Fig. 4 along with pie charts showing the percentage of total volume changes for each of 6 body regions with weight loss. More than half of total body volume changes were derived from the trunk and about one-third were derived from the legs in both the male and female. A larger percentage of total volume changes in the male were from the trunk (61%) compared to the female (53%); by contrast, legs in the female contributed a greater percentage of total volume changes (36%) compared to the male (30%). The before-after images thus suggest the presence of a sexual dimorphism in shape changes with weight loss in the context of the current study experimental conditions.
Pie-charts showing the percentage of total volume changes in four designated regions; right and left arm and leg volumes were combined for presentation of total arm and leg volumes, respectively. Additional circumference, volume, and surface area data is presented in Supplementary Information III.
Discussion
Extending the usual graphical portrayals of longitudinal weight loss drug effects and tabular presentation of health measure improvements [2,3,4,5], the current study presents visual images that capture these kinds of observations in an easy to understand and assimilate format. The presented images provide a sense of what the average male and female participants looked like at baseline, prior to drug treatment, and how they appeared after approximately one year following medication use, along with the extent to which their heath-risks diminished. The average male and female participants in the Surmount 1 study began the protocol with similar baseline BMIs [16], but the female participants lost relatively more weight and had greater health improvements, at least according to BRI, than the male, findings clearly evident from the images shown in Figs. 1, 2. Consistent with the reductions in BRI, cardiovascular disease risk factors improved in Surmount 1, although sex differences could not be ascertained as male and female observations were pooled in the pivotal publication [2]. The avatar-predicted changes in body shape with weight loss also differed between the male and female, the male losing more volume (i.e., mass) from the trunk and less from the legs than the female. As shown by the images, baseline BMIs were quite high (~37–38 kg/m2, Class II obesity) and, as depicted by the avatars, body size and shape remained in the overweight-obese range following 72 weeks of medication treatment.
Are the 3D avatar body size and shape estimates accurate? We validated the manifold regression approach in an earlier study by comparing predicted avatar dimensions to those acquired with a 20-camera 3D-optical system and we found close agreement for evaluated circumferences, volumes, and surface areas [6]. In that cross-sectional study, we also found that avatar predication covariates beyond sex, weight, height, and age were important in refining avatar features. These additional model covariates include measured variables such as circumferences derived from a flexible tape and impedances evaluated with bioimpedance analysis systems. This highlights the importance of collecting and publishing such clinical trial data, which can be used in follow-up studies such as the current report. Accurate 3D avatars, using these types of covariates, could be employed to estimate changes in body composition with weight loss [7, 18], incorporated as a visual supplement when reporting the results generated by dynamic energy balance weight loss prediction models [8], and serve a role as part of human heat thermoregulation models introduced for medical and public health applications [19].
The 3D avatars and health-risk images presented in this report can also potentially serve a useful purpose as part of weight loss treatment plans. Horne et al. [20]. observed that visualizing a future “self” as a personalized avatar reinforced motivation to modify behavior, an effect that might build self-confidence and promote participation in a weight loss program. Further research is needed, however, to examine the psychological effects of exposing people who are overweight and obese to images that emphasize their body size and shape. Individuals categorized as overweight and obese are already at a heighted risk of experiencing negative body image perceptions due to weight stigma and weight bias [21]. The visual tools described herein may draw further attention to aspects of their physical appearance, exacerbating feelings of body dissatisfaction [22]. Moreover, appearance-related motivations for exercise have been linked to disordered eating behaviors and poor adherence to health regimes [23]. When individuals fail to achieve their desired weight loss or appearance goal in the short term, they often abandon behavior change altogether, suggesting that using appearance as the primary driver for health behavior change might be an ineffective strategy [24]. The role of 3D avatars in weight control management thus remains a topic worthy of future study.
The focus of this report was on Surmount 1 (tirzepatide) and an assumption is that weight loss in participants proceeded mainly through caloric restriction. As such, the composition of weight change is anticipated to resemble that of non-pharmacologic measures that promote negative energy balance [25]. What if all or most of the weight loss was fat with sparing of lean tissues such as skeletal muscle? This possibility arises through newer muscle-sparing weight loss medicines [26] or protocols that include intensive protein supplementation and physical activity regimens [27]. How would physical appearance differ from that reported here? Our modeling approach, as reported here, allows for variation in the composition of weight change and generation of avatars with specified body composition. We anticipate forthcoming studies that will present an opportunity to explore these kinds of questions.
The current study and approach has several limitations. Waist circumference measurements were unavailable at the 72-week evaluation and had to be estimated using equations derived as reported in Supplementary Information II. We did not include race or ethnicity as covariates in the manifold regression models as the available Surmount 1 data only included pooled averages for all males and all females in the MTD groups. While we did not include race or ethnicity information when predicting humanoid avatars in the current study, the question arises if adding these kinds of covariates is feasible. Our current manifold regression model sample includes information on participant demographics that we can include in predictions, although increasing model accuracy across diverse samples, cultures, and geographic regions requires larger and more varied development groups. The mean data used in manifold prediction models reflected different sample sizes at baseline and 72-weeks and the sizes of the MTD groups were not reported in the presentation of Chao et al. [16]. Our avatar predictions are founded on the assumption that people in the post-weight loss state have similar anthropometric features to their never-weight loss counterparts, a hypothesis that could be evaluated in future studies by including actual 3D-optical evaluations in the protocol. Lastly, the body regions designated by Universal Software were designed to match those of other methods such as dual-energy X-ray absorptiometry. These kinds of image landmarks are easily moved should different regional estimates be of interest in future studies.
In conclusion, humanoid avatar and health-risk images were generated in the current report to present a visual representation of typically complex graphical and text data characteristic of advanced stage weight loss drug trials. Images such as these encapsulate treatment outcomes in a simple format that is easy to understand, even for people not familiar with the nuances of scientific publications. These images have the potential to serve as additional communicated outcomes of weight loss clinical trials that can be shared with professional and public audiences for educational purposes.
Data availability
Data described in the manuscript will be made available on request, pending application and approval by the investigators.
References
Couzin-Frankel J 2023 Breakthrough of the Year. Science. Available at: https://www.science.org/content/article/breakthrough-2023#:~:text=weight%20loss%20itself.-,For%20these%20reasons%2C%20Science%20has%20named%20GLP%2D1%20drugs%20the,anxieties%2C%20this%20sea%20change%20brings. Last updated 14 December 2023. Accessed: 27 February 2025.
Jastreboff AM, Aronne LJ, Ahmad NN, Wharton S, Connery L, Alves B, et al. Tirzepatide once weekly for the treatment of obesity. N Engl J Med. 2022;387:205–216.
Ryan DH, Lingvay I, Deanfield J, Kahn SE, Barros E, Burguera B, et al. Long-term weight loss effects of semaglutide in obesity without diabetes in the SELECT trial. Nat Med. 2024;30:2049–2057.
Wilding JPH, Batterham RL, Calanna S, Davies M, Van Gaal LF, Lingvay I, et al. Once-weekly semaglutide in adults with overweight or obesity. N Engl J Med. 2021;384:989–1002.
Wilding JPH, Batterham RL, Davies M, Van Gaal LF, Kandler K, Konakli K, et al. Weight regain and cardiometabolic effects after withdrawal of semaglutide: The STEP 1 trial extension. Diab Obes Metab. 2022;24:1553–64.
McCarthy C, Wong MC, Brown J, Ramirez S, Yang S, Bennett JP, et al. Accurate prediction of three-dimensional humanoid avatars for anthropometric modeling. Int J Obes ((Lond)). 2024;48:1741–47.
Wong MC, Ng BK, Tian I, Sobhiyeh S, Pagano I, Dechenaud M, et al. A pose-independent method for accurate and precise body composition from 3D optical scans. Obes (Silver Spring). 2021;29:1835–47.
Thomas DM, Martin CK, Heymsfield S, Redman LM, Schoeller DA, Levine JA. A simple model predicting individual weight change in humans. J Biol Dyn. 2011;5:579–99.
Wong MC, McCarthy C, Fearnbach N, Yang S, Shepherd J, Heymsfield SB. Emergence of the obesity epidemic: 6-decade visualization with humanoid avatars. Am J Clin Nutr. 2022;115:1189–93.
Sobhiyeh S, Dunkel A, Dechenaud M, Mehrnezhad A, Kennedy S, Shepherd J, et al. Digital anthropometric volumes: Toward the development and validation of a universal software. Med Phys. 2021;48:3654–64.
Sobhiyeh S, Kennedy S, Dunkel A, Dechenaud ME, Weston JA, Shepherd J, et al. Digital anthropometry for body circumference measurements: Toward the development of universal three-dimensional optical system analysis software. Obes Sci Pr. 2021;7:35–44.
Liu Y, Liu X, Guan H, Zhang S, Zhu Q, Fu X, et al. Body Roundness Index Is a Superior Obesity Index in Predicting Diabetes Risk Among Hypertensive Patients: A Prospective Cohort Study in China. Front Cardiovasc Med. 2021;8:736073.
Zeng D, Zeng Q, Li S, Lu J, Cheng N. Evaluating body roundness index and systemic immune inflammation index for mortality prediction in MAFLD patients. Sci Rep. 2025;15:330.
Zhang X, Ma N, Lin Q, Chen K, Zheng F, Wu J, et al. Body roundness index and all-cause mortality among US adults. JAMA Netw Open. 2024;7:e2415051.
Body weight reduction with tirzepatide by sex: a subgroup analysis of the SURMOUNT clinical trials. European Association for the Study of Diabetes (EASD) 60th Annual Meeting; Madrid, Spain, 2024.
Chao A, Taylor R, Mojdami D, Forrester T, Chigutsa F, Malik R Body Weight Reduction Associated With Tirzepatide by Sex: A Subgroup Analysis of the SURMOUNT Clinical Trials. Eli Lilly. Available at: https://medical.lilly.com/us/products/assets/vaultpdf/en/c5fca87576d4c2abd35a08d9bd1b72f5bb73c3610a9deb3ac9189eb9306b7dda/body-weight-reduction-associated-with-tirzepatide-by-sex-a-subgroup-analysis-of-the-surmount-clinical-trials. Last updated 2024. Accessed: 27 February 2025.
Thomas DM, Bredlau C, Bosy-Westphal A, Mueller M, Shen W, Gallagher D, et al. Relationships between body roundness with body fat and visceral adipose tissue emerging from a new geometrical model. Obes (Silver Spring). 2013;21:2264–71.
Marazzato F, McCarthy C, Field RH, Nguyen H, Nguyen T, Shepherd JA, et al. Advances in digital anthropometric body composition assessment: neural network algorithm prediction of appendicular lean mass. Eur J Clin Nutr. 2024;78:452–54.
Xu X, Rioux TP, Castellani MP. Three dimensional models of human thermoregulation: a review. J Therm Biol. 2023;112:103491.
Horne M, Hardy M, Murrells T, Ugail H, Hill AJ. Using personalized avatars as an adjunct to an adult weight loss management program: randomized controlled feasibility study. JMIR Form Res. 2022;6:e36275.
Puhl R, Brownell KD. Bias, discrimination, and obesity. Obes Res. 2001;9:788–805.
Grogan S, Storey E, Brownbridge K, Gill S, Templeton C, Gill J, et al. Whole body scanning as a tool for clothing sizing: effects on women’s body satisfaction. J Text Inst. 2019;111:862–8.
Tylka TL, Homan KJ. Exercise motives and positive body image in physically active college women and men: Exploring an expanded acceptance model of intuitive eating. Body Image. 2015;15:90–7.
Stewart TM. Why thinking we’re fat won’t help us improve our health: Finding the middle ground. Obes (Silver Spring). 2018;26:1115–16.
Heymsfield SB, Gonzalez MC, Shen W, Redman L, Thomas D. Weight loss composition is one-fourth fat-free mass: a critical review and critique of this widely cited rule. Obes Rev. 2014;15:310–21.
Heymsfield SB, Coleman LA, Miller R, Rooks DS, Laurent D, Petricoul O, et al. Effect of bimagrumab vs placebo on body fat mass among adults with type 2 diabetes and obesity: a phase 2 randomized clinical trial. JAMA Netw Open. 2021;4:e2033457.
Mechanick JI, Butsch WS, Christensen SM, Hamdy O, Li Z, Prado CM, et al. Strategies for minimizing muscle loss during use of incretin-mimetic drugs for treatment of obesity. Obes Rev. 2025;26:e13841.
Acknowledgements
We extend our appreciation to Ms. Melanie Peterson for her assistance in the preparation of this manuscript.
Funding
This work was partially supported by National Institutes of Health NORC Center Grants P30DK072476, Pennington/Louisiana, P30DK040561, Harvard, and R01DK109008, Shape UP! Adults.
Author information
Authors and Affiliations
Contributions
Authors’ contributions to manuscript: SR, RY, MH, SK, JB, JS, DT, and SBH designed research; SR, RY, MH, and SK conducted research; SR, RY, MH, SK, JB, JS, DT, and SBH wrote the paper and had primary responsibility for final content.
Corresponding author
Ethics declarations
Competing interests
SBH participates in Medical Advisory Boards of Tanita Corporation, Medifast, Lilly, and Regeneron; he serves on a Novo Nordisk data safety monitoring committee.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ramirez, S., Yang, R., Habibovic, M. et al. Visual demonstration of weight loss and health risk improvement with a dual GIP and GLP-1 receptor agonist. Int J Obes 49, 2005–2010 (2025). https://doi.org/10.1038/s41366-025-01842-1
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41366-025-01842-1