Abstract
Obesity has emerged as a critical public health challenge globally, with substantial health and economic repercussions. This study aimed to evaluate the literature on the clinical and economic burdens associated with obesity, specifically in low- and middle-income countries (LMICs). A systematic review following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines was performed. The CINAHL, MEDLINE, PubMed, Web of Science and Scopus databases were systematically searched for studies published from inception to March 28, 2025. The costs of illness for all included studies were converted to 2024 United States (US) dollars, using country-specific gross domestic product inflators. Conversion to US dollars was based on purchasing power parity (PPP). The quality of all included studies was assessed via the Newcastle‒Ottawa Scale (NOS). Of the total of 676 reports identified by the search strategy, six studies were prevalence-based, four studies were survey-based, and three model-based studies (n = 13) were eligible for inclusion on the basis of predefined inclusion criteria. These studies published data from Brazil, Ghana, China, Iran, South Africa, Mexico, and Thailand. Three of the 13 studies reported indirect costs. Two studies reported the clinical impact of obesity. Methodological quality was deemed moderate. The annual direct and indirect costs associated with obesity for a population in LMICs ranged from USD 0.2 billion to USD 12.56 billion and USD 223 million to USD 227.5 million, respectively. Hospitalisation was the main cost driver in five of the included studies. One study reported the total number of hospitalisations/number of person-years for men and women as 803/9207 and 2354/25,173, respectively. This is the first systematic review to summarise the clinical and economic burdens associated with obesity in LMICs. The clinical and economic burden of obesity on individuals and healthcare systems is significant, necessitating effective prevention and management strategies. To increase the accuracy and comparability of findings, future research should adopt a standardised cost-of-illness methodology. This approach will provide clearer insights into the economic impact of obesity and facilitate more effective public health interventions.
Similar content being viewed by others
Introduction
The World Health Organization (WHO) classifies obesity as a chronic, multifactorial disease characterized by excessive fat accumulation that presents a risk to health, operationalized as a body mass index (BMI) of 30 kg/m² or higher [1]. This metric is calculated by dividing an individual’s weight in kilograms by the square of their height in meters [2]. Obesity ranks as the fifth leading cause of mortality globally and is a major contributor to the rise of non-communicable diseases (NCDs) such as cardiovascular disease, type 2 diabetes, and certain forms of cancer [3]. Although obesity is often associated with high-income nations, it is increasingly prevalent across low- and middle-income countries (LMICs), where the shift from traditional to modern dietary patterns, combined with urbanization and sedentary lifestyles, is accelerating the public health crisis [4].
In 2014, the WHO estimated that over 600 million out of approximately 1.9 billion were people with obesity, with eight of the ten countries most affected being LMICs, including Brazil, China, Egypt, India, Indonesia, Mexico, Pakistan, and Russia [5, 6]. LMICs are nations classified by the World Bank based on gross national income (GNI) per capita, currently defined as those with a GNI per capita of $13,845 or less in 2024 (World Bank, 2024). Notably, 62% of the world’s population with obesity resides in LMICs [6]. Over the past three decades, age-standardised obesity rates have increased significantly, increasing from 3.2% to 10.8% in men and from 6.4% to 14.9% in women [7]. Specifically, in LMICs such as India, Bangladesh, and Nepal, the prevalence of obesity among women increased from 10.6% to 14.8%, from 2.7% to 8.9%, and from 1.6% to 10.1%, respectively, between 1996 and 2006 [8]. Interestingly, recent studies suggest that the prevalence of obesity in LMICs is lower than that in high-income countries [9].
Historically, undernutrition has dominated the public health discourse in LMICs. However, many of these countries are now experiencing a rapid epidemiological transition, where underweight and micronutrient deficiencies coexist with overnutrition and diet-related NCDs [10]. Urbanization, aggressive marketing of ultra-processed foods, declining physical activity, and increasing substance use such as tobacco and alcohol are driving this shift [11]. As a result, conditions like obesity, hypertension, and diabetes are emerging more rapidly in LMICs than in high-income settings. For example, cardiovascular diseases now account for a significant share of mortality in Ethiopia and Kenya, often linked to overweight and obesity [12].
Although obesity rates have started to stabilize in some high-income countries, this trend is not evident in the majority of LMICs, where rates continue to rise. Notably, urban areas in Rwanda, Zambia, and Brazil have shown renewed surges in obesity prevalence after initial periods of stabilization [13]. Among adolescents in LMICs including those in Egypt, Mexico, Vietnam, and Nigeria obesity rates are increasing at alarming rates [13]. A 2021 study spanning seven LMICs reported a consistent rise in overweight among adolescents, highlighting a troubling trajectory that portends a future wave of adult obesity and associated health complications [14]. Without comprehensive prevention programs, this trend is expected to continue, albeit at a potentially slower pace. However, even modest increases in obesity among youth populations can translate into significant public health costs in the long term, given the chronic nature of obesity and its complications [15].
Obesity is associated with several chronic lifestyle conditions, including hypertension, diabetes, cancer, and heart disease [16, 17]. These conditions contribute to disability, significant healthcare expenditures, and increased mortality rates. Obesity is reported to reduce life expectancy by an average of 5–8 years for women and 13–20 years for men [16]. Additionally, it is linked to various health issues, such as pain, fatigue, sleep disorders, and depressive moods [18]. Studies estimate that obesity can reduce life expectancy by 5–8 years in women and 13–20 years in men [19]. Moreover, obesity is associated with physical limitations such as chronic fatigue, sleep disturbances, joint pain, and depressive symptoms. For example, in Nigeria, patients with obesity undergoing cardiac surgery had significantly longer hospital stays compared to their non-obese counterparts, placing strain on already limited healthcare infrastructure [20]. Across LMICs, obesity-related disability-adjusted life years (DALYs) have been on a steady rise since 1990, and projections suggest they could double over the next four decades without effective intervention [21].
Despite the growing burden of obesity in LMICs, there is a lack of comprehensive synthesis evaluating its clinical and economic impacts in these settings. Although multiple studies have estimated the burden of obesity globally, significant variability in methods such as diagnostic criteria, cost components, population selection, and analytical approaches has led to inconsistent findings [22]. Most existing systematic reviews are either outdated, limited to high-income countries, or lack rigorous methodological assessments, such as quality appraisal, standardized cost conversions, or inclusion of both direct and indirect costs [22,23,24,25]. Furthermore, few reviews have focused specifically on LMICs, despite the rapidly increasing prevalence and unique contextual factors in these countries. Given the double burden of malnutrition and non-communicable diseases now faced by LMICs, a systematic review focused on these countries is urgently needed.
Methods
A systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [26]. The review has been registered with PROSPERO, the International Prospective Register of Systematic Reviews, under the registration number CRD42022331948. This registration ensures transparency and helps prevent duplication of research efforts.
Search strategy
The literature search in this systematic review used the CINAHL, MEDLINE, PubMed, Web of Science, and Scopus databases and included articles published from inception to the 28th of March 2025. The search terms used were obesity, overweight, obesity, unhealthy weight, high BMI, cost, expense, affordability, financial burden, health care costs, healthcare resource utilisation, emergency department visit, physician visits, hospitalisation, LMICs, low-income countries, middle-income countries, developing countries, Africa, Asia, Latin America, South America, and Central America. In addition to these databases, hand searches of the references of the included studies were also performed. The terms were matched with terms in the Medical Subject Heading (MeSH) database. All references were downloaded to EndNote, and duplicates were removed. The search was performed independently by two reviewers (TG & CM) to avoid the presence of bias in the selection and exclusion of studies. Disagreements were resolved by discussion with a third reviewer (FF). The details of the searching strategy with key words and initial hits are provided in Appendix A to ensure reproducibility and transparency of the work.
Inclusion and exclusion criteria
On the basis of the predefined eligibility criteria, the reviewers (TG & CM) identified publications independently to be included in this review. Discrepancies were solved with the agreement of the reviewers (FF). The inclusion criteria for the search were studies on economic consequences or burdens of obesity (e.g., healthcare costs, societal costs, and treatment costs), the WHO’s recommendations for the definition of obesity (BMI ≥ 30 kg/m2), studies on humans related to obesity, studies published in the English language, and studies conducted in LMICs. The exclusion criteria included studies not related to the economic consequences of obesity; studies that did not calculate the burden of obesity; studies that characterised full economic evaluations, reviews, meta-analyses, cost-effectiveness studies, letters, notes, editorials and conferences; reports; letters to the editors; comments; opinions; protocols; studies with insufficient methodological details; and studies not published in the English language. These criteria ensured a focused selection of studies relevant to the clinical and economic impact of obesity in LMICs.
Data extraction, quality assessment and reporting
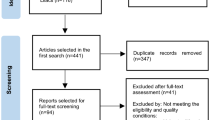
The study selection process is illustrated in the PRISMA flow diagram (Fig. 1). Data extraction was performed by one reviewer (TG) and entered into a standardised data extraction table in Microsoft Excel. To ensure accuracy, the extracted data were independently verified by two additional reviewers (TG & CM). The following information was extracted from the selected studies: general details such as the first author and publication year, study country, type of cost analysis, sample size, socioeconomic status, BMI, study period, and study perspective. For cost-related data, we gathered information on the currency and cost year, along with mean or median total costs and costs attributable to obesity. The quality of the included studies was assessed via the Newcastle‒Ottawa Scale (NOS) by two reviewers (TG & CM). The NOS consists of nine items categorised into three dimensions: selection of the population, comparability of groups, and outcomes or exposures of interest [27]. Each study was scored on a scale with a maximum of nine points, where a score of ≥ 6 indicated high quality, 3 to 6 indicated moderate quality, and ≤ 3 indicated low quality. Any disagreements in scoring were resolved through consultation with a third reviewer (FF).
Data analysis
In this study, summary descriptive statistics were utilised to outline the background and types of costs associated with obesity. Both healthcare and nonhealthcare costs were further analysed through quantitative methods. A comparison of costs across countries was conducted on the basis of the methodologies used in each included study. To facilitate these comparisons, costs were converted to US dollars (US$) via country-specific gross domestic product (GDP) deflators [28] and purchasing power parities (PPP) [29]. These conversions were performed as of August 2024. Estimated cost values were adjusted by multiplying them by the 2024 GDP coefficient, then dividing by the GDP of the reference year for each study, and finally adjusted by the PPP conversion factor for 2024. This approach ensured a standardised framework for comparing costs across different countries, taking into account economic variations.
Results
The literature search retrieved 676 potentially relevant studies from PubMed (n = 167), Medline & CINHAL (n = 167), Scopus (n = 98) and Web of Science (n = 244) (see the PRISMA flowchart in Fig. 1). Of these, 182 were duplicates. After screening the titles and abstracts, 452 publications were excluded, leaving 42 articles for further full-text review. Thirteen studies met the inclusion criteria and were included in the review. The studies included in this systematic review were deemed to be of moderate quality (Appendix B).
Characteristics of the included studies
The characteristics of each included study are detailed in Table 1. The studies reported data from various countries: Brazil (n = 6), Ghana (n = 1), China (n = 2), South Africa (n = 1), Mexico (n = 1), Iran (n = 1), and Thailand (n = 1). Among the 13 studies, three [30,31,32] were conducted from a societal perspective, whereas the remaining studies [33,34,35,36,37,38,39,40] focused on the health system perspective. Additionally, two studies [41, 42] specifically reported the clinical impact of obesity. Economic impact was assessed via different methodologies: prevalence-based [32, 33, 35, 37, 41], survey-based [30, 31, 36, 39], and modelling [34, 38, 40]. These studies were published between 2012 and 2022 and adopted varying time horizons, ranging from 6 months to 50 years.
Summary of findings
The key findings from the included studies are summarised in Table 2. The annual costs related to obesity in low- and middle-income countries (LMICs) are estimated to be between US$ 544 million and USD 12.56 billion for direct expenses and between USD 203 million and USD 227.5 million for indirect expenses. In Brazil, hospitalisation costs for individuals with class III obesity were found to be twice as high, with indirect costs nearly double those of individuals with a normal BMI [18]. Specifically, the annual physician and hospitalisation costs for class III obesity patients were reported at USD 188.14 and USD 1,839.70, respectively. In Ghana, a cost of illness study estimated that the annual direct healthcare costs for female and male patients were USD5,530 and USD4923, respectively [22]. Moreover, in rural Yunnan Province, China, the direct cost for individuals aged 35 years and older was estimated at USD 3.774 billion, whereas the indirect cost was estimated at USD 203 million [19]. These findings highlight the substantial economic burden of obesity across different LMICs. Three studies from Brazil, China, and Thailand estimated the indirect costs associated with obesity [18,19,20]. In Brazil, the average annual indirect cost estimate for individuals with class III obesity is USD 970.00 [18]. This study utilised the Work Productivity and Activity Impairment-General Health Questionnaire, a validated instrument that measures absenteeism, presenteeism, overall work productivity loss, and activity impairment. In China, the indirect cost related to obesity is estimated at USD 203 million [19], whereas in Thailand, it is estimated at USD 227 million [20]. Table 3 summarizes the cost components included across the studies. Hospitalisation emerged as the primary cost driver in six of the included studies [18,19,20,21, 23, 24]. In Brazil, the average length of hospital stay for obesity-related diseases was reported to be 7.9 days for men and 6.8 days for women [29]. The burden of hospitalisation associated with obesity was notably substantial in both Brazil [29] and Iran [30], underscoring the need for effective management strategies to address this issue.
Discussion
This systematic review provides valuable insights into the clinical and economic impact of obesity in LMICs, highlighting significant variations in costs across different nations. The review identified only 13 studies that met the inclusion criteria, indicating a limited but crucial body of literature on this topic. The estimated annual costs associated with obesity, including both direct and indirect expenses, varied widely from US$544 million to US$12.56 billion for direct costs and US$ 223 million to US$227.5 million for indirect costs. These figures emphasise the substantial economic burden of obesity, with hospitalisation identified as the primary cost driver. One critical point is the heterogeneity among the studies, stemming from differences in methodological approaches, perspectives, and target populations. Beyond these high-level factors, heterogeneity also appeared to arise from variations in how obesity was defined and measured across studies, the types of cost components included, and the timeframes over which costs were assessed. Additionally, some studies employed national datasets while others relied on sub-national or hospital-level data, leading to differences in representativeness and scale. Economic modelling techniques and assumptions such as discount rates, cost inflation adjustments, and currency conversions also varied, further complicating cross-study comparisons [43]. These methodological disparities underscore the challenge of synthesising findings across settings and reinforce the need for unified costing frameworks to better inform policy responses in LMICs.
This systematic review aligns with the literature indicating that individuals with obesity experience significantly greater healthcare resource utilisation than those with a normal BMI [44, 45]. The current review highlights the multifaceted costs of obesity, including humanistic impacts such as binge eating, anxiety, and depression, as well as societal costs linked to lost productivity, which encompasses both directly missed workdays and the reduction of future earnings due to morbidity and mortality [30,31,32]. Despite limited discussion across studies, productivity costs particularly in LMICs represent a substantial but often underreported component of the economic burden. The studies included in this review employed the human capital approach, which estimates productivity loss by assigning a monetary value to time lost from work due to illness or premature death. This method typically involved calculating missed workdays multiplied by the average daily wage for morbidity-related losses and projecting lost future income for mortality-related losses, adjusted with discount rates. However, assumptions varied across studies regarding the inclusion of caregiver absenteeism, time per outpatient visit, and wage metrics, contributing to variability in estimates. The underrepresentation of broader productivity impacts, such as reduced job performance and long-term employment limitations, suggests a need for more comprehensive methodologies. Given these findings, it is crucial for public health authorities to prioritise preventive interventions aimed at reducing obesity. Strategies should focus on promoting physical activity and encouraging healthy lifestyle choices [46]. These interventions could help reduce direct costs related to physician services, hospitalisation, and outpatient care, ultimately benefiting both individuals and the wider economy [22]. This comprehensive approach can help address the growing obesity epidemic and its associated burdens in LMICs.
Dee et al. [47] found that, in high-income countries, the indirect costs of overweight and obesity such as lost productivity tended to surpass direct medical expenses. However, in contrast, two studies included in the current review [30, 31] found that direct healthcare costs related to obesity were greater than the indirect costs. Notably, only a few studies in this review [30,31,32] considered indirect costs, suggesting that the full economic burden from productivity losses may be underestimated. Additionally, while Dee et al.’s findings were based on high-income settings, the present review focuses on LMICs, where estimating indirect costs is particularly challenging. Many individuals in LMICs are employed in the informal sector, where income is often unstable and difficult to measure [48, 49]. Furthermore, cultural perceptions of obesity may influence healthcare-seeking behaviors and the distribution of health resources, potentially leading to higher direct spending [50]. These contextual factors may help explain why, in LMICs, direct costs appear to outweigh indirect ones.
In this systematic review, five studies employed a prevalence-based approach to estimate the costs associated with obesity [32, 33, 35, 37, 41]. This method allows for the estimation of costs incurred over a specified period, measuring the economic burden of obesity without considering when the condition first developed [51]. While prevalence-based cost-of-illness analyses provide valuable insights, it is essential to acknowledge potential limitations. The reported cost estimates may not fully reflect the current economic impact or be entirely applicable to the specific population under study. This variability highlights the need for caution when interpreting the results, as the estimates may lack accuracy and timeliness. Future research should consider incorporating more dynamic modelling approaches that account for the temporal aspects of obesity-related costs to improve the precision and relevance of findings.
The variation in healthcare systems across countries poses a critical challenge to generalising obesity cost estimates, as most studies in this review offer country-specific data that reflect distinct healthcare infrastructures and economic conditions within LMICs. This limits the transferability of findings across settings and underscores the need for robust multinational studies. The World Obesity Atlas exemplifies such efforts, providing a globally harmonised model that estimated the economic impact of overweight and obesity at US$1.96 trillion in 2020, or 2.4% of global GDP, with projections rising to nearly 3% by 2035 [52]. These figures capture both direct and indirect costs, including productivity losses and premature mortality, and highlight the disproportionate burden on LMICs, which are expected to house two-thirds of adults with severe obesity by 2030 [43]. This disparity reveals the limitations of isolated national studies and demonstrates the value of cross-country analyses like those used in the World Obesity Atlas and Global Burden of Disease project. Integrating such global models with local data enables more accurate forecasting, promotes international benchmarking, and supports the development of context-specific, scalable interventions ultimately enhancing the global response to the growing obesity epidemic.
This systematic review is the first to comprehensively assess both the clinical and economic burden of obesity in LMICs, offering valuable and policy-relevant insights into an underexplored area of global health. The study followed a structured and transparent methodology, drawing from five major databases; however, this may have limited the inclusion of relevant studies indexed elsewhere [53]. The exclusion of non-English publications could also have led to the omission of important research from non-English-speaking LMICs. Significant heterogeneity in study designs, outcome measures, and costing approaches prevented meta-analysis and highlighted the urgent need for standardized reporting guidelines in obesity research. Only two [41, 42] of the thirteen included studies focused on clinical outcomes, restricting insights into the broader health impacts of obesity. Moreover, the reliability of cost estimates is constrained by the generally moderate to low quality of included studies, as assessed using the Newcastle-Ottawa Scale. In spite of these limitations, we believe that this review was systematic in nature and summarizes all available and relevant clinical and economic burden results from the literature.
Conclusion
This is the first systematic review to summarise the clinical and economic burdens associated with obesity in LMICs. The clinical and economic burden of obesity on individuals, families, healthcare systems and society is significant. In addition, obesity in LMICs is associated with significant direct healthcare costs. These findings underscore the need for effective prevention and management strategies to reduce the associated burden. However, the studies included in this review utilised diverse approaches, and many presented methodological shortcomings related to resource use measurement and cost allocation. To increase the validity and comparability of findings, future research should adopt a standardised cost-of-illness methodology. This would help ensure more accurate assessments of the economic impact of obesity, facilitating evidence-informed decision-making for public health interventions. By addressing these methodological challenges, we can better understand the true burden of obesity and develop more effective strategies to mitigate its impact.
References
World Health Organisation Obesity: preventing and managing the global epidemic (Report of a WHO Consultation: WHO Technical Report Series 894). Geneva: World Health Organisation; 2000.
Ataey A, Jafarvand E, Adham D, Moradi-Asl E. The relationship between obesity, overweight, and the human development index in world health organisation eastern mediterranean region countries. J Prev Med Public Health. 2020;53:98.
WHO. Obesity and overweight. 2016. http://www.who.int/mediacentre/factsheets/fs311/en/. WHO. Obesity and overweight. 2020. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight.
Ahmed SK. Mohammed RA. Obesity: prevalence, causes, consequences, management, preventive strategies and future research directions. Metab Open. 2025;27:100375
World Health Organisation. Obesity and overweight. 2015. http://www.who.int/mediacentre/factsheets/fs311/en/.
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:766–81.
NCD Risk Factor Collaboration. Trends in adult body-mass index in 200 countries from 1975–2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participants. Lancet. 2016;387:1377–96.
Balarajan Y, Villamor E. Nationally representative surveys show recent increases in the prevalence of overweight and obesity among women of reproductive age in Bangladesh, Nepal, and India. J Nutr. 2009;139:2139–44.
Fan H, Zhang X. Recent trends in overweight and obesity in adolescents aged 12 to 15 years across 21 countries. Pediatr Obes. 2022;17:e12839.
Mamun AA, Finlay JE. Shifting of undernutrition to overnutrition and its determinants among women of reproductive ages in the 36 low to medium income countries. Obes Res Clin Pract. 2015;9:75–86. https://doi.org/10.1016/j.orcp.2014.03.001.
Leocádio PCL, Lopes SC, Dias RP, Alvarez-Leite JI, Guerrant RL, Malva JO, et al. The transition from undernutrition to overnutrition under adverse environments and poverty: the risk for chronic diseases. Front Nutr. 2021;8:676044.
Keino BC, Carrel M. Spatial and temporal trends of overweight/obesity and tobacco use in East Africa: subnational insights into cardiovascular disease risk factors. Int J Health Geogr. 2023;22:20.
Jaacks LM, Slining MM, Popkin BM. Recent underweight and overweight trends by rural-urban residence among women in low- and middle-income countries. J Nutr. 2015;145:352–7.
GBD 2021 Adolescent BMI Collaborators. Global, regional, and national prevalence of child and adolescent overweight and obesity, 1990–2021, with forecasts to 2050: a forecasting study for the Global Burden of Disease Study 2021. Lancet. 2025;405:785–812.
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in underweight and obesity from 1990 to 2022: a pooled analysis of 3663 population-representative studies with 222 million children, adolescents, and adults. Lancet. 2024;403:1027–50.
Fontaine KR, Redden DT, Wang C, Westfall AO, Allison DB. Years of life lost due to obesity. JAMA. 2003;289:187–93.
Peeters A, Barendregt JJ, Willekens F, Mackenbach JP, Al Mamun A, Bonneux L. Obesity in adulthood and its consequences for life expectancy: a life-table analysis. Ann Intern Med. 2003;138:24–32.
Klages KL, Berlin KS, Cook JL, Merchant TE, Wise MS, Mandrell BN, et al. Health-related quality of life, obesity, fragmented sleep, fatigue, and psychosocial problems among youth with craniopharyngioma. Psychooncology. 2022;31:779–87.
Peeters A, Barendregt JJ, Willekens F, Mackenbach JP, Al Mamun A, Bonneux L. NEDCOM, the Netherlands Epidemiology and Demography Compression of Morbidity Research Group. Obesity in adulthood and its consequences for life expectancy: a life-table analysis. Ann Intern Med. 2003;138:24–32.
Saker Z, Saab M, Rabah A. The impact of body mass index on the duration of hospital stay after cardiac surgery. Cureus. 2025;17:e84985.
Wang J, Huang Y, Feng N, Xu L, Du X, Chen M, et al. Global disease burden attributable to high body mass index in young adults from 1990 to 2019, with projections to 2050: a systematic analysis for the Global Burden of Disease Study 2019. Diabetes Metab Res Rev. 2024;40:e70007.
Tremmel M, Gerdtham UG, Nilsson PM, Saha S. Economic burden of obesity: a systematic literature review. Int J Environ Res Public Health. 2017;14:435.
Withrow D, Alter DA. The economic burden of obesity worldwide: a systematic review of the direct costs of obesity. Obes Rev. 2011;12:131–41.
Specchia ML, Veneziano MA, Cadeddu C, Ferriero AM, Mancuso A, Ianuale C, et al. Economic impact of adult obesity on health systems: a systematic review. Eur J Public Health. 2015;25:255–62.
Nagi MA, Ahmed H, Rezq MA, Sangroongruangsri S, Chaikledkaew U, Almalki Z, et al. Economic costs of obesity: a systematic review. Int J Obes. 2024;48:33–43.
Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–9.
Wells GA, Tugwell P, O’Connell D, Welch V, Peterson J, Shea B, et al. The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2015. https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
The World Bank. GDP deflator. 2023. https://data.worldbank.org/indicator/NY.GDP.DEFL.ZS.
The World Bank. Official exchange rate. 2023. https://data.worldbank.org/indicator/PA.NUS.FCRF.
Kudel I, Alves JS, de Menezes Goncalves T, Kull K, Nørtoft E. The association between body mass index and health and economic outcomes in Brazil. Diabetol Metab Syndr. 2018;10:1–11.
Li Q, Cai L, Cui W, Wang G, He J, Golden AR. Economic burden of obesity and four obesity-related chronic diseases in rural Yunnan Province, China. Public Health. 2018;164:91–8.
Pitayatienanan P, Butchon R, Yothasamut J, Aekplakorn W, Teerawattananon Y, Suksomboon N, et al. Economic costs of obesity in Thailand: a retrospective cost-of-illness study. BMC Health Serv Res. 2014;14:146.
Bahia L, Coutinho ESF, Barufaldi LA, de Azevedo Abreu G, Malhão TA, Ribeiro de Souza CP, et al. The costs of overweight and obesity-related diseases in the Brazilian public health system: cross-sectional study. BMC Public Health. 2012;12:1–7.
Lartey S, Si L, Lung T, Magnussen CG, Boateng GO, Minicuci N, et al. Impact of overweight and obesity on life expectancy, quality-adjusted life years and lifetime costs in the adult population of Ghana. BMJ Glob Health. 2020;5:e003332.
Boachie MK, Thsehla E, Immurana M, Kohli-Lynch C, Hofman KJ. Estimating the healthcare cost of overweight and obesity in South Africa. Glob Health Action. 2022;15:2045092.
Shi J, Wang Y, Cheng W, Shao H, Shi L. Direct health care costs associated with obesity in Chinese population in 2011. J Diabetes Complications. 2017;31:523–8.
de Oliveira ML, Santos LMP, da Silva EN. Direct healthcare cost of obesity in Brazil: an application of the cost-of-illness method from the perspective of the public health system in 2011. PLoS ONE. 2015;10:e0121160.
Rtveladze K, Marsh T, Webber L, Kilpi F, Levy D, Conde W, et al. Health and economic burden of obesity in Brazil. PLoS ONE. 2013;8:e68785.
Canella DS, Novaes HM, Levy RB. Medicine expenses and obesity in Brazil: an analysis based on the household budget survey. BMC Public Health. 2015;16:1–8.
Rtveladze K, Marsh T, Barquera S, Romero LMS, Levy D, Melendez G, et al. Obesity prevalence in Mexico: impact on health and economic burden. Public Health Nutr. 2014;17:233–9.
Sichieri R, Nascimento SD, Coutinho W. The burden of hospitalisation due to overweight and obesity in Brazil. Cad Saude Publica. 2007;23:1721–7.
Ramezankhani A, Azizi F, Hasheminia M, Hadaegh F. The impact of general and central obesity for all-cause hospitalisation among Iranian adults: a 20 year follow-up—results from the TLGS cohort. BMC Public Health. 2023;23:903.
Okunogbe A, Nugent R, Spencer G, Powis J, Ralston J, Wilding J. Economic impacts of overweight and obesity: current and future estimates for 161 countries. BMJ Glob Health. 2022;7:e009773.
Kleinman N, Abouzaid S, Andersen L, Wang Z, Powers A. Cohort analysis assessing medical and nonmedical cost associated with obesity in the workplace. J Occup Environ Med. 2014;56:161–70.
Van Nuys K, Globe D, Ng-Mak D, Cheung H, Sullivan J, Goldman D. The association between employee obesity and employer costs: evidence from a panel of U.S. employers. Am J Health Promot. 2014;28:277–85.
Shrestha N, Pedisic Z, Neil-Sztramko S, Kukkonen-Harjula KT, Hermans V. The impact of obesity in the workplace: a review of contributing factors, consequences and potential solutions. Curr Obes Rep. 2016;5:344–60.
Dee A, Kearns K, O’Neill C, Sharp L, Staines A, O’Dwyer V, et al. The direct and indirect costs of both overweight and obesity: a systematic review. BMC Res Notes. 2014;7:1–9.
Ungar WJ, Coyte PC. Measuring productivity loss days in asthma patients. Health Econ. 2000;9:37–46.
Russell S. The economic burden of illness for households in developing countries: a review of studies focusing on malaria, tuberculosis, and HIV/AIDS. Am J Trop Med Hyg. 2004;71:147–55.
James CD, Hanson K, McPake B, Balabanova D, Gwatkin D, Hopwood I, et al. To retain or remove user fees? Reflections on the current debate in low- and middle-income countries. Appl Health Econ Health Policy. 2006;5:137–53.
Habetha S, Bleich S, Weidenhammer J, Fegert JM. A prevalence-based approach to societal costs occurring in consequence of child abuse and neglect. Child Adolesc Psychiatry Ment Health. 2012;6:1–10.
Lobstein T, Jackson-Leach R, Powis J, Brinsden H, Gray M. World obesity atlas 2023. World Obesity Federation; 2023. https://coilink.org/20.500.12592/hrmxx8.
Freeman P, Robbins A. Editorial: The publishing gap between rich and poor: the focus of AuthorAID. J Public Health Policy. 2006;27:196–203.
Author information
Authors and Affiliations
Contributions
TG, CM, and FF conceptualised the study. TG and CM carried out the literature search, data extraction and risk of bias assessment with support from FF. TG conducted the narrative synthesis and statistical analyses and wrote the first draft of the manuscript. FF, FN-O, FC, ZH, and UU critically reviewed the manuscript. TG, CM, FF, FN-O, FC, ZH, and UU approved the manuscript. FF is responsible for the overall content as guarantor.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The study is a systematic review. For this study, ethical approval was not needed.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fatoye, F., Mbada, C., Niyi-Odumosu, F. et al. The clinical and economic burden of obesity in low- and middle-income countries: a systematic review. Int J Obes 49, 2453–2461 (2025). https://doi.org/10.1038/s41366-025-01913-3
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41366-025-01913-3