Abstract
Meta-analysis conducted to evaluate the effectiveness of high-dose (≥800 IU/day) and low-dose (<800 IU/day) vitamin D supplementation on preterm infants. Study quality was evaluated using the Revised Cochrane risk-of-bias tool 2 for randomized trials. 21 studies included 1130 infants. Regarding short-term (before 40 weeks’ postmenstrual age [PMA] or at discharge) outcomes, high-dose vitamin D supplementation was associated with increased serum 25-hydroxyvitamin D (25[OH]D) levels (mean difference 15.62 [13.35–17.88]) and growth velocities, as well as decreased vitamin D deficiency (VDD), skeletal hypomineralization, and mortality. In the subgroup analysis of high-dose supplementation stratified by dosage, 800 IU/day significantly increased serum 25(OH)D levels (mean difference 13.99 [9.03–18.95]) and reduced the risk of VDD (risk difference −0.21 [−0.32 to −0.10]) compared to 400 IU/day, without increasing the risk of vitamin D excess. The long-term outcomes assessed after 40 weeks’ PMA or at follow-up visits showed no significant differences in vitamin D status or neurodevelopmental outcomes between the high-dose and low-dose groups. The certainty of the evidence ranges from moderate to very low. High-dose vitamin D supplementation improved short-term outcomes by increasing serum 25(OH)D levels, promoting growth, and reducing mortality. Among the high-dose regimens, 800 IU/day appeared to be the most appropriate dose.
Similar content being viewed by others
Introduction
Vitamin D is important for normal bone mineralization. However, preterm infants are vulnerable to vitamin D deficiency (VDD) due to several factors, including decreased transplacental transfer of vitamin D, limited synthesis resulting from prolonged hospitalization, prolonged parenteral nutrition use, and minimal fat mass for the storage of vitamin D and its metabolites [1, 2]. Inadequate vitamin D levels lead to increased risks of metabolic bone disease or rickets in preterm infants [3]. In addition, VDD may be associated with lung maturation, respiratory distress syndrome (RDS), bronchopulmonary dysplasia (BPD), and immune function [4,5,6].
The recommended dose of vitamin D for preterm infants differs among advisory bodies. The American Academy of Pediatrics recommends a vitamin D intake of 200–400 IU/day (to convert to μg /day, multiply by 0.025) [3]. In contrast, the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition guidelines suggest a higher intake (800–1000 IU/day) to prevent VDD [2]. These differences may stem from variations in the emphasis on the risks associated with vitamin D deficiency versus excess, differences in the interpretation of results, and regional differences in factors related to vitamin D synthesis. As differing guidelines, there is a growing need for clear and integrated evidence-based recommendations to optimize the health and development of preterm infants in clinical practice. Therefore, it is essential to establish guidelines for vitamin D supplementation that compare high- and low-dose, aiming to identify an optimal regimen that yields better outcomes while minimizing side effects.
Two previous meta-analyses have investigated the effects of varying doses of vitamin D supplementation in preterm infants [7, 8], but their findings remain inconsistent. Yang et al. reported that high-dose supplementation (800–1000 IU/day) did not significantly increase serum 25-hydroxyvitamin D (25[OH]D) levels, compared to the low-dose (400 IU/day) [7]. However, it was associated with improved growth and immune function [7]. In contrast, Kumar et al. found no significant benefits of high-dose supplementation (800–1600 IU/day) on mortality, morbidity, or growth, despite an increase in vitamin D levels [8]. However, these prior studies did not separately evaluate short-term (during hospitalization) and long-term (post-discharge) outcomes, nor did they provide sufficient insight into the dose-response relationship for different clinical endpoints. Given the critical role of vitamin D in skeletal development, growth, and neurodevelopment, it is important to determine whether higher doses confer added benefits−or introduce risks beyond simply correcting deficiency. This is particularly important in preterm infants, who are at increased risk for vitamin D deficiency and its associated complications.
This study aimed to (1) evaluate the short-term and long-term effectiveness and safety of high-dose (≥800 IU/day) and low-dose (<800 IU/day) vitamin D supplementation on preterm infants and (2) provide evidence to help determine the optimal dosage strategy for vitamin D supplementation.
Methods
This meta-analysis was conducted based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA guidelines) [9]. The Research protocol was registered and updated in the International Prospective Register of Systematic Reviews. (CRD 42023387565).
Literature search
The MEDLINE, EMBASE, and Cochrane Library databases were systematically searched for articles published through November 30th, 2024. Medical subject words (MeSH) and free-text terms were used for retrieval. The search terms employed encompassed phrases such as “Infant,” “Premature,” and “Vitamin D.” Supplementary Fig. 1 provides detailed information.
Study selection
EndNote software was employed for literature management. Qualified studies were identified and cross-checked by two researchers (S.H.S. and H.J.K.). In cases where consensus was needed, a third reviewer (J.S.H.) was consulted.
Inclusion criteria
The Population, Intervention, Comparison, Outcomes, and Study (PICOS) design criteria was used in searching the literature [10, 11]. The population(P) of interest consisted of preterm infants (gestational age < 37 weeks); The intervention (I) was high-dose vitamin D3 (≥800 IU/day) supplementation started during neonatal intensive care unit (NICU) stay after birth; the comparison (C) was low-dose vitamin D3 (<800 IU/day) supplementation started during NICU stay after birth; the outcomes (O) include short-term (before 40 weeks’ postmenstrual age [PMA] or at discharge) and long-term (after 40 weeks’ PMA or at the outpatient clinic follow-up) outcomes. Short-term outcomes include serum 25(OH)D level, VDD(serum 25[OH]D level < 20 ng/mL, to convert to nmol/L, multiply by 2.5) [12], vitamin D excess (VDE), skeletal bone mineralization, clinical outcomes (growth, RDS, BPD, late-onset sepsis [LOS], length of hospital stay, and mortality), biochemical markers (parathyroid hormone [PTH], calcium [Ca], phosphorus, alkaline phosphatase [ALP], osteocalcin, and urine calcium/creatinine ratio [uCa/Cr]). Long-term outcomes include serum 25(OH)D level, bone mineral density, mortality, and neurodevelopment; the study design(S) was a randomized controlled trial.
Exclusion criteria
The studies of usage of different forms of vitamin D (example: vitamin D2), selective vitamin D supplementation based on limited criteria (example: vitamin D level <20 ng/mL), or enteral vitamin D supplementation for the treatment of any disease were excluded.
Data extraction
A predefined data extraction form was used. Ambiguities in data extraction were resolved after discussion with a third reviewer. The following information was extracted: (1) First author and year of publication; (2) country; (3) gestational age at birth; (4) vitamin D dose; (5) sample size; (6) starting point of supplementation; (7) duration or endpoint of supplementation; (8) timing of outcome assessment; (9) primary outcomes: short- and long-term outcomes. Data was extracted by two independent reviewers (S.H.S. and H.J.K.) and reexamined by a third reviewer (H.J.S.).
Quality assessment
The quality of the included studies was evaluated and cross-checked by two researchers according to the Revised Cochrane risk-of-bias (ROB) tool 2 for randomized trials [13, 14], and a third reviewer was consulted when necessary. A sensitivity analysis was conducted to determine whether the ROB, funding/conflict of interest status, feeding type, publication year, and Mantel-Haenszel analysis as odds ratio influenced the statistical results (Supplementary Table 1). For sensitivity analysis based on feeding type, studies were categorized into two groups: 1) “feeding clearly described and total vitamin D intake estimated” – this group included studies either quantified total vitamin D intake from all sources (supplementation and feeding), or involved exclusively breastfed infants (assuming negligible vitamin D intake from breast milk) or infants fed with formula clearly stated to contain no vitamin D, 2) “feeding type mentioned, but vitamin D intake not estimated” – this group included studies that described the feeding type (e.g., breast milk or formula) and. in some cases, mentioned the use of vitamin D-containing fortifiers or preterm formula, but did not specify the vitamin D content of the feeding source or provide sufficient information to estimate the total vitamin D intake. A funnel plot was used to investigate publication bias.
Statistical analysis
The outcomes of this review were categorized into short- and long-term outcomes. The definitions of outcome measures in each study are provided in Supplementary Table 2. Statistical analysis was performed using RevMan Web and stata/MP 15.0, and P < 0.05 was considered to be statistically significant. The risk difference (RD) and mean difference (MD) were used as outcome estimation measures for categorical and continuous outcomes, respectively. The outcomes were analyzed using a fixed-effects model due to the homogeneity of the preterm infant populations in each study. The results were visually presented using forest plots. The I2 statistic and Cochran’s Q test were used to assess the statistical heterogeneity. Data that were initially presented as median, interquartile range, and minimum and maximum values were transformed into mean and standard deviation values according to the Cochrane Handbook [14]. The certainty of evidence for each outcome was assessed independently by two review authors using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) System [15]. GRADEPro GDT, a web-based tool, was used to create a “Summary of Findings” table to report the certainty of evidence.
Results
Study selection
A total of 6873 studies were identified (Fig. 1). Following the removal of duplicates and the subsequent screening of titles, abstracts, and full texts, 21 studies from nine countries (Canada, Egypt, Finland, India, Iran, Israel, Turkey, UK and USA), reporting on 1,130 infants met the final inclusion criteria [16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36]. Three separate studies from one cohort were included, each investigating different outcomes with intervals of several years [20, 25, 35].Additionally, for one study [28], only the abstract was available. The baseline characteristics of studies are summarized in Table 1.
Search strategy flow diagram of literature search and filtering results for a systematic review of the short-term (before 40 weeks’ postmenstrual age or at discharge) and long-term (after 40 weeks’ postmenstrual age or at the outpatient clinic follow-up) effects of vitamin D supplementation for preterm infants, according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 guidelines.
Short-term outcomes
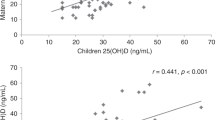
The Serum 25(OH)D levels and associated outcomes are presented in Fig. 2A, B, Supplementary Fig. 2, and Table 2A. Serum 25(OH)D levels were significantly increased in the high-dose group compared to the low-dose group (MD 15.62; 95% confidence interval [CI] 13.35-17.88; I2 = 90% [95% CI 88–98]; low certainty of evidence; 13 trials, 739 participants) [16, 19, 21,22,23, 25, 28, 30,31,32,33,34, 36]. In addition, the risk of VDD was significantly lower in the high-dose group (RD−0.29; 95% CI−0.37 to −0.22; I2 = 78% [95% CI 48–91]; moderate certainty of evidence; 5 trials, 449 participants) [23, 28, 31, 32, 36]. Moreover, significant difference was not found in the risk of VDE (RD 0.04; 95% CI 0.00–0.08; I2 = 21% [95% CI 0–88]; low certainty of evidence; 4 trials, 302 participants) [16, 19, 23, 36].
A Short-term outcomes: continuous variables. B Short-term outcomes: categorical variables. C Subgroup analysis of serum 25-hydroxyvitamin D levels according to different doses among the high-dose vitamin D supplementation group. D Subgroup analysis of categorical variables according to different doses among the high-dose vitamin D supplementation group. CI confidence interval, MD mean difference, RD risk difference; 25(OH)D 25-hydroxyvitamin D.
Skeletal hypomineralization is presented in Fig. 2B, Supplementary Fig. 2, and Table 2A. The RD for skeletal hypomineralization was −0.18, indicating that the high-dose group had a significantly lower risk compared to the low-dose group (95% CI−0.28 to −0.08; I2 = 94% [95% CI 87–97]; low certainty of evidence; 4 trials; 168 participants) [17, 19, 31, 34].
Clinical outcomes are presented in Fig. 2A, B, Supplementary Fig. 2, and Table 2A. Weight gain velocity (g/day), length gain velocity (cm/week), and head circumference gain velocity (cm/week) all demonstrated a significant increase in the high-dose group compared to the low-dose group (weight: MD 2.57; 95% CI 1.10–4.04; length: MD 1.01; 95% CI 0.22-1.80; head: MD 0.57, 95% CI 0.13–1.02; all three outcomes: I2 = 0%; low certainty of evidence; 2 trials; 112 participants) [30, 31]. The significant differences in clinical outcomes, including RDS, BPD, LOS, and length of hospital stay were not found. However, the risk of mortality was significantly lower in the high-dose group (RD−0.13; 95% CI−0.25 to −0.02; I2 = 0%; low certainty of evidence; 2 trials; 114 participants) [16, 25].
Biochemical markers are presented in Supplementary Fig. 2. The PTH level(pg/mL, to convert to pmol/L, multiply by 0.106) was significantly lower in the high-dose group (MD−15.76; 95% CI−21.96 to −9.56; I2 = 84% [95% CI 61–94]; 4 trials, 302 participants) [19, 23, 31, 36]. The levels of the other biochemical markers, did not differ.
To identify the optimal high-dose, the high-dose group was divided into three subgroups, and a subsequent subgroup analysis was performed (Figs. 2C, D, Supplementary Fig. 2). All three high-dose groups (800 IU [16, 19, 23, 25, 27, 30, 33], 960–1000 IU [22, 23, 31, 34, 36], and 2000 IU [24]) demonstrated a significant elevation in serum 25(OH)D levels compared to the low-dose group. The risk of VDD significantly decreased in both the 800 IU [23, 28, 32] and 1000 IU [23, 31] groups compared to the low-dose group. However, the risk of VDE showed a significant increase exclusively in the 1000 IU subgroup [23, 36] (RD 0.07; 95% CI 0.01–0.12; I2 = 48%; 2 trials; 179 participants) and not in the 800 IU group [16, 19, 23].
Long-term outcomes
The Serum 25(OH)D levels and associated outcomes are presented in Fig. 3A, Supplementary Fig. 3, and Table 2B. The significant differences in serum 25(OH)D levels were not found between the low-dose and high-dose groups. In a single study focusing on long-term follow-up of VDD and VDE [32], VDD showed a significant decrease in the high-dose group (RD−0.23; 95% CI−0.40 to −0.05; low certainty of evidence; 80 participants), and VDE did not show a significant difference.
Bone mineral density is presented in Fig. 3A, Supplementary Fig. 3, and Table 2B. Bone mineral density (mg/cm2) at corrected age 3 months displayed no significant difference (MD 0.33; 95% CI−5.47 to 6.12; I2 = 62%; very low certainty of evidence; 2 trials; 107 participants) [21, 32]. Bone mineral density at 9–11 years was reported in one study [22], and significant differences were not found between the two groups.
Clinical outcomes are presented in Fig. 3B, Supplementary Fig. 3, and Table 2B. In one study reporting on mortality and neurodevelopmental outcomes at 2 years of age [35], significant differences were not found in terms of mortality, cognitive and language impairment, and total neurodevelopmental impairment.
Quality assessment and certainty of the evidence
All outcome parameters analyzed are summarized in Table 2. The ROB values are shown in Supplementary Fig. 4. Overall, 25% of the studies had a low risk, 25% raised concerns, and 50% had a high risk. Six studies had concerns regarding bias in the randomization process [17, 20, 24, 29, 33, 34], 9 studies had concerns regarding bias in deviations from the intended interventions [17, 21, 23, 24, 29, 30, 32, 35, 36], and 10 studies had a high risk of bias due to missing outcome data [20, 23,24,25,26, 29, 30, 32, 35, 36]. Bias in the measurement of the outcomes was determined to be low across all studies. However, for bias in the selection of the reported results, one was found to have some concerns [25]. To determine the robustness of the ROB, a sensitivity test that excluded the high-risk studies was conducted (Supplementary Table 1). Following the sensitivity analysis for serum 25(OH)D levels, the MD score between the high-dose and low-dose groups decreased (MD 8.11; 95% CI 5.07–11.15). In addition, there was no significant difference in mortality following the sensitivity analysis. Based on the risk of bias, the certainty of the evidence ranges from moderate to very low (Table 2). When analyzing the publication bias concerning different doses of vitamin D supplementation on serum 25(OH)D levels, we visually evaluated the symmetry of the funnel plot shape and found no evidence of asymmetry (Supplementary Fig. 5).
Discussion
This is the first meta-analysis to simultaneously analyze the short- and long-term outcomes of vitamin D supplementation and suggest an optimal dose for preterm infants. In this study, high-dose vitamin D supplementation showed short-term benefits by increasing serum 25(OH)D levels and growth velocity, and by reducing the risk of VDD, bone hypomineralization, and mortality. Among the high-dose groups, supplementation with 800 IU/day improved serum 25(OH)D levels without increasing the risk of VDE. However, in the long-term, significant differences in serum 25(OH)D levels or clinical outcomes were not found between the high-dose and low-dose groups.
Vitamin D is an essential micronutrient that regulates bone health [37]. Prevention of VDD early in life is important due to its effects on skeletal and non-skeletal health [38, 39]. Our meta-analysis indicates that high-dose vitamin D supplementation is more beneficial for increasing serum 25(OH)D levels and decreasing the risk of VDD and skeletal hypomineralization without VDE before 40 weeks’ PMA or at discharge. Notably, this result is inconsistent with the results of the meta-analysis by Yang et al. [7]. Regarding serum 25(OH)D levels, the meta-analysis included only 5 studies up to 2016 in Yang’s research, whereas our study includes 13 studies up to 2024. Additionally, while the study by Yang et al. did not distinguish between the time points of the outcomes measurements, our study analyzed the short- and long-term outcomes separately. These factors may have contributed to the disparities in our respective results.
Unlike the short-term outcomes, there was insufficient evidence to suggest significant differences in serum 25(OH)D levels and bone mineral density in the long-term. Several possibilities should be considered when interpreting these results. Firstly, for long-term outcomes, only 4 studies were included to evaluate serum 25(OH)D levels. The limited number of studies may have made it challenging to provide an accurate evaluation. Secondly, the timing of the long-term outcomes evaluation varied greatly, ranging from a corrected age of 3 to 12 months. Furthermore, in some studies, the duration of vitamin D supplementation was either inadequately described or was shorter than the latest evaluation time. Thirdly, although medical staff can accurately supplement vitamin D during hospitalization, vitamin D supplementation may be affected by parental compliance after discharge. Fourthly, after discharge, environmental factors such as exposure to sunlight (ultraviolet B-mediated vitamin D formation) [40, 41], the introduction of solid foods containing vitamin D, and the accrual of fat mass (where vitamin D and its metabolites are stored) [42] could affect serum vitamin D levels.
This study showed that high-dose supplementation was more effective in the growth of weight, length, and head circumference over a short-term period. The positive relationship in our study is in line with previous meta-analyses showing that vitamin D supplementation during pregnancy or early infancy was associated with improved infant growth [43, 44]. Notably, vitamin D levels may be related to the levels of insulin-like growth factor 1, which plays a pivotal role in height and weight gain [45, 46]. Moreover, vitamin D plays an important role in the modulation of immune function and oxidative stress, factors that may be linked to growth [6, 47].
In this study, the mortality risk was significantly lower in the high-dose group. The association between vitamin D levels and pulmonary development has been well established [48, 49], and one possible hypothesis is that high-dose vitamin D supplementation is more beneficial for lung maturation and survival. However, following the sensitivity analysis according to the ROB or feeding type, the statistical significance of mortality disappeared. Therefore, the effect of high-dose vitamin D supplementation on mortality may have been overinterpreted. In terms of morbidity (RDS, BPD, late-onset sepsis [LOS], and length of hospital stay), the significant differences were not found in this study. Infants who had not reached enteral feeding were often excluded from study enrollment due to the impracticality of administering vitamin D supplementation. This exclusion may have introduced selection bias, potentially affecting the evaluation of morbidity and mortality outcomes.
When a subgroup analysis of high-dose supplementation stratified by dosage was conducted on the high doses, 800 IU/day was associated with a significant increase in serum 25(OH)D levels and a decrease in VDD during the short-term period. However, an increase in VDE was observed solely in the high-dose group at 1000 IU/day but not at 800 IU/day. To mitigate side effects, it is advisable to keep vitamin D doses as low as possible while still achieving the desired therapeutic effects. Consequently, a vitamin D dose of 800 IU/day could be recommended as the optimal dose to improve short-term outcomes. However, vitamin D levels and complications should be closely monitored simultaneously.
Limitations
This study had some limitations. Firstly, although 21 studies were included, the number of studies and sample sizes, especially when considering short-term and long-term outcomes, was very small. Accordingly, it is difficult to accurately evaluate the clinical or long-term outcomes in a small number of studies. Secondly, five (25%) of the included studies had ‘some concerns’, and 10 studies (50%) had a high ROB. When a sensitivity analysis was performed by excluding high-risk studies, the MD of serum 25(OH)D decreased from 15.62 to 8.11, though statistical significance was retained (Supplementary Table 1). This suggests that the effect of high-dose vitamin D supplementation on serum 25(OH)D levels may have been overestimated due to selective reporting bias in the high-risk studies. Regarding other outcomes, it is important to acknowledge that sensitivity analysis is limited in its interpretability due to the small number of studies available. Third, this meta-analysis had limited availability and inconsistency of data regarding feeding type and background vitamin D intake. Several included studies did not report detailed information on the vitamin D content from feeding sources such as breast milk, formula, or fortifiers. Although a sensitivity analysis was conducted based on whether total vitamin D intake could be estimated, the number of studies in each subgroup was small, with some subgroups containing only a single study. This limits the ability to assess whether the efficacy of high-dose supplementation differs by feeding context and highlights the need for future trials to report total vitamin D exposure more comprehensively.
Conclusion
High-dose (≥800 IU/day) vitamin D supplementation for preterm infants was associated with positive short-term outcomes, encompassing improvements in vitamin D levels, growth, and reduced mortality. However, the benefits of high-dose supplementation did not persist in the long-term outcomes. Among the high-dose supplementation, 800 IU/day appeared to be the most appropriate dose. By identifying the optimal and safest dose of vitamin D supplementation for preterm infants, this study could help alleviate the clinical confusion resulting from current guidelines that recommend different doses.
Data availability
The data underlying this meta-analysis are derived from previously published studies, which are all publicly available. No new datasets were generated or analyzed for the current study.
References
Abrams SA, Committee on Nutrition. Calcium and vitamin D requirements of enterally fed preterm infants. Pediatrics. 2013;131:e1676–83.
Agostoni C, Buonocore G, Carnielli VP, De Curtis M, Darmaun D, Decsi T, et al. Enteral nutrient supply for preterm infants: commentary from the European Society of Paediatric Gastroenterology, Hepatology and Nutrition Committee on Nutrition. J Pediatr Gastroenterol Nutr. 2010;50:85–91.
Abrams SA. Vitamin D in preterm and full-term infants. Ann Nutr Metab. 2020;76:6–14.
Kim YJ, Lim G, Lee R, Chung S, Son JS, Park HW. Association between vitamin D level and respiratory distress syndrome: A systematic review and meta-analysis. PLoS One. 2023;18:e0279064.
Çetinkaya M, Çekmez F, Erener-Ercan T, Buyukkale G, Demirhan A, Aydemir G, et al. Maternal/neonatal vitamin D deficiency: a risk factor for bronchopulmonary dysplasia in preterms?. J Perinatol. 2015;35:813–7.
Sava F, Treszl A, Hajdú J, Toldi G, Rigó J Jr, Tulassay T, et al. Plasma vitamin D levels at birth and immune status of preterm infants. Immunobiology. 2016;221:1289–92.
Yang Y, Li Z, Yan G, Jie Q, Rui C. Effect of different doses of vitamin D supplementation on preterm infants - an updated meta-analysis. J Matern Fetal Neonatal Med. 2018;31:3065–74.
Kumar M, Shaikh S, Sinha B, Upadhyay RP, Choudhary TS, Chandola TR, et al. Enteral Vitamin D supplementation in preterm or low birth weight infants: a systematic review and meta-analysis. Pediatrics. 2022;150:e2022057092K.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100.
Higgins JPT, Green S Cochrane handbook for systematic reviews of interventions. John Wiley & Sons, (2011).
Brown P, Brunnhuber K, Chalkidou K, Chalmers I, Clarke M, Fenton M, et al. How to formulate research recommendations. BMJ. 2006;333:804–6.
Ross AC, Manson JE, Abrams SA, Aloia JF, Brannon PM, Clinton SK, et al. The 2011 report on dietary reference intakes for calcium and vitamin D from the Institute of Medicine: what clinicians need to know. J Clin Endocrinol Metab. 2011;96:53–8.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898.
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane Handbook for Systematic Reviews of Interventions. 2nd ed. Wiley-Blackwell, (2019).
Guyatt GH, Oxman AD, Vist G, Kunz R, Brozek J, Alonso-Coello P, et al. GRADE guidelines: 4. Rating the quality of evidence-study limitations (risk of bias). J Clin Epidemiol. 2011;64:407–15.
Abdel-Hady H, Yahia S, Megahed A, Mosbah A, Seif B, Nageh E, et al. Mediators in preterm infants with late-onset sepsis: a randomized controlled trial. J Pediatr Gastroenterol Nutr. 2019;68:578–84.
Alizade P, Naderi F, Sotoudeh K. A randomized clinical trial of prophylactic effects of vitamin D on different indices of osteopenia of prematurity. Iran J Public Health. 2006;35:58–63.
Aly H, Mohsen L, Bhattacharjee I, Malash A, Atyia A, Elanwary S, et al. Vitamin D supplementation and T cell regulation in preterm infants: a randomized controlled trial. J Pediatr Gastroenterol Nutr. 2019;69:607–10.
Anderson-Berry A, Thoene M, Wagner J, Lyden E, Jones G, Kaufmann M, et al. Randomized trial of two doses of vitamin D3 in preterm infants <32 weeks: Dose impact on achieving desired serum 25(OH)D3 in a NICU population. PLoS One. 2017;12:e0185950.
Aristizabal N, Holder MP, Durham L, Ashraf AP, Taylor S, Salas AA. Safety and efficacy of early Vitamin D supplementation in critically ill extremely preterm infants: an ancillary study of a randomized trial. J Acad Nutr Diet. 2023;123:87–94.
Backström MC, Mäki R, Kuusela AL, Sievänen H, Koivisto AM, Ikonen RS, et al. Randomised controlled trial of vitamin D supplementation on bone density and biochemical indices in preterm infants. Arch Dis Child Fetal Neonatal Ed. 1999;80:F161–6.
Backström MC, Mäki R, Kuusela AL, Sievänen H, Koivisto AM, Koskinen M, et al. The long-term effect of early mineral, vitamin D, and breast milk intake on bone mineral status in 9- to 11-year-old children born prematurely. J Pediatr Gastroenterol Nutr. 1999;29:575–82.
Bozkurt O, Uras N, Sari FN, Atay FY, Sahin S, Alkan AD, et al. Multi-dose vitamin d supplementation in stable very preterm infants: Prospective randomized trial response to three different vitamin D supplementation doses. Early Hum Dev. 2017;112:54–9.
Evans JR, Allen AC, Stinson DA, Hamilton DC, St John Brown B, Vincer MJ, et al. Effect of high-dose vitamin D supplementation on radiographically detectable bone disease of very low birth weight infants. J Pediatr. 1989;115:779–86.
Fort P, Salas AA, Nicola T, Craig CM, Carlo WA, Ambalavanan N. A Comparison of 3 Vitamin D dosing regimens in extremely preterm infants: a randomized controlled trial. J Pediatr. 2016;174:132–8.e1.
Golan-Tripto I, Bistritzer J, Loewenthal N, Staretz-Chacham O, Dizitzer Y, Goldbart A. The effect of vitamin D administration on vitamin D status and respiratory morbidity in late premature infants. Pediatr Pulmonol. 2020;55:3080–7.
Hanson C, Jones G, Lyden E, Kaufmann M, Armas L, Anderson-Berry A. Vitamin D metabolism in the premature newborn: A randomized trial. Clin Nutr. 2016;35:835–41.
Kishore SS, Gadiraju M. Study of daily vitamin D supplementation in preterm infants: a randomized trial. J Pediatr Gastroenterol Nutr. 2019;68:1167.
Kislal FM, Dilmen U. Effect of different doses of vitamin D on osteocalcin and deoxypyridinoline in preterm infants. Pediatr Int. 2008;50:204–7.
Koo WW, Krug-Wispe S, Neylan M, Succop P, Oestreich AE, Tsang RC. Effect of three levels of vitamin D intake in preterm infants receiving high mineral-containing milk. J Pediatr Gastroenterol Nutr. 1995;21:182–9.
Mathur NB, Saini A, Mishra TK. Assessment of adequacy of supplementation of Vitamin D in very low birth weight preterm neonates: a randomized controlled trial. J Trop Pediatr. 2016;62:429–35.
Natarajan CK, Sankar MJ, Agarwal R, Pratap OT, Jain V, Gupta N, et al. Trial of daily vitamin D supplementation in preterm infants. Pediatrics. 2014;133:e628–34.
Pittard WB 3rd, Geddes KM, Hulsey TC, Hollis BW. How much vitamin D for neonates?. Am J Dis Child. 1991;145:1147–9.
Robinson MJ, Merrett AL, Tetlow VA, Compston JE. Plasma 25-hydroxyvitamin D concentrations in preterm infants receiving oral vitamin D supplements. Arch Dis Child. 1981;56:144–5.
Salas AA, Woodfin T, Phillips V, Peralta-Carcelen M, Carlo WA, Ambalavanan N. Dose-response effects of early Vitamin D supplementation on neurodevelopmental and respiratory outcomes of extremely preterm infants at 2 years of age: a randomized trial. Neonatology. 2018;113:256–62.
Tergestina M, Rebekah G, Job V, Simon A, Thomas N. A randomized double-blind controlled trial comparing two regimens of vitamin D supplementation in preterm neonates. J Perinatol. 2016;36:763–7.
Thorne-Lyman A, Fawzi WW. Vitamin D during pregnancy and maternal, neonatal and infant health outcomes: a systematic review and meta-analysis. Paediatr Perinat Epidemiol. 2012;26:75–90.
Wagner CL, Greer FR, American Academy of Pediatrics Section on Breastfeeding, American Academy of Pediatrics Committee on Nutrition. Prevention of rickets and vitamin D deficiency in infants, children, and adolescents. Pediatrics. 2008;122:1142–52.
Misra M, Pacaud D, Petryk A, Collett-Solberg PF, Kappy M. Vitamin D deficiency in children and its management: review of current knowledge and recommendations. Pediatrics. 2008;122:398–417.
Matsuoka LY, Wortsman J, Hollis BW. Suntanning and cutaneous synthesis of vitamin D3. J Lab Clin Med. 1990;116:87–90.
Kimlin MG, Schallhorn KA. Estimations of the human ‘vitamin D’ UV exposure in the USA. Photochem Photobiol Sci. 2004;3:1067–70.
Didriksen A, Burild A, Jakobsen J, Fuskevag OM, Jorde R. Vitamin D3 increases in abdominal subcutaneous fat tissue after supplementation with vitamin D3. Eur J Endocrinol. 2015;172:235–41.
Huey SL, Acharya N, Silver A, Sheni R, Yu EA, Peña-Rosas JP, et al. Effects of oral vitamin D supplementation on linear growth and other health outcomes among children under five years of age. Cochrane Database Syst Rev. 2020;12:CD012875.
Ma K, Wei SQ, Bi WG, Weiler HA, Wen SW. Effect of Vitamin D supplementation in early life on children’s growth and body composition: a systematic review and meta-analysis of randomized controlled trials. Nutrients. 2021;13:524.
Gou Z, Li F, Qiao F, Maimaititusvn G, Liu F. Causal associations between insulin-like growth factor 1 and vitamin D levels: a two-sample bidirectional Mendelian randomization study. Front Nutr. 2023;10:1162442.
Ameri P, Giusti A, Boschetti M, Murialdo G, Minuto F, Ferone D. Interactions between vitamin D and IGF-I: from physiology to clinical practice. Clin Endocrinol. 2013;79:457–63.
Walker VP, Zhang X, Rastegar I, Liu PT, Hollis BW, Adams JS, et al. Cord blood vitamin D status impacts innate immune responses. J Clin Endocrinol Metab. 2011;96:1835–43.
Fang K, He Y, Mu M, Liu K. Maternal vitamin D deficiency during pregnancy and low birth weight: a systematic review and meta-analysis. J Matern Fetal Neonatal Med. 2021;34:1167–73.
Lai G, Wu C, Hong J, Song Y. 1,25-Dihydroxyvitamin D(3) (1,25-(OH)(2)D(3)) attenuates airway remodeling in a murine model of chronic asthma. J Asthma. 2013;50:133–40.
Funding
This work was supported by the Korea University Anam Hospital grant [grant number O2207711], the Korea University grant, and the National Research Foundation of Korea(NRF) grant funded by the Korea government(MSIT) [grant number RS-2025-00522231]. Open Access funding enabled and organized by Seoul National University.
Author information
Authors and Affiliations
Contributions
All authors had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Conception and/or design: Shin SH, Heo JS. Acquisition, analysis, or interpretation of data: All authors. Drafting of the manuscript: Shin SH, Heo JS. Critical review of the manuscript for important intellectual content: Kim HJ, Heo JS. Statistical analysis: Kim HJ, Heo JS. Obtained funding: Heo JS. Administrative, technical, or material support: Shin SH, Heo JS. Supervision: Kim HJ, Heo JS.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Ethical approval was not requested because this study retrieved and synthesized data from already published studies.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shin, S.H., Kim, H.J. & Heo, J.S. Short-term and long-term effects of vitamin D supplementation for preterm infants: a systematic review and meta-analysis. J Perinatol (2025). https://doi.org/10.1038/s41372-025-02440-9
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41372-025-02440-9