Abstract
Early identification of relapsing/refractory diffuse large B-cell lymphoma (DLBCL) represents an unmet clinical need. A real-life cohort of newly diagnosed DLBCL (n = 120) treated with R-CHOP was investigated. Using the standardized uptake value (SUV) threshold of 4.0, PET/CT radiomics variables (SUVmax, tMTV, tTLG and Dmax) were collected. Circulating tumor DNA (ctDNA) analysis by CAPP-seq yielded baseline ctDNA levels and LymphGen molecular clustering. The best cut-off for both PET/CT parameters and ctDNA levels were identified by max-stat statistics. tMTV, tTLG and Dmax retained independent prognostic value when adjusted for ctDNA levels and were grouped together in a variable named high-risk PET. By multivariate analysis, ctDNA-high and high-risk PET independently predicted PFS and were combined into a 2-factor prognostic model (C-indices: 0.712 for PFS and 0.696 for OS). Molecular clustering, by capturing high-risk biological features of DLBCL, further improved outcome prediction. Consistently, BN2/EZB/ST2 clusters maintained an independent association with better PFS when adjusted for the 2-factor model variables and were therefore included in a 3-factor prognostic score (C-indices: 0.745 for PFS and 0.746 for OS), that identified a very high-risk group of patients (n = 22, 40-month PFS 12.1%) which should be prioritized for early response evaluation and for access to novel agents.
Similar content being viewed by others
Introduction
Diffuse large B-cell lymphoma (DLBCL) accounts for up to 30–35% of all cases of non-Hodgkin lymphomas (NHL) and represents a heterogeneous disease with different biological features, clinical behavior, and treatment response. Front-line R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone) chemoimmunotherapy allows the achievement of long-term disease control in about 60% of patients [1, 2]. After several unsuccessful attempts to improve R-CHOP, the pola-R-CHP regimen (polatuzumab vedotin, rituximab, cyclophosphamide, doxorubicin, and prednisone) showed a survival benefit over R-CHOP in intermediate-risk and high-risk DLBCL [3,4,5]. Despite this improvement, relapsing/refractory DLBCL patients still pose an unmet clinical need also because they are not easily identified a priori [1,2,3,4].
Baseline [18F]FDG-PET/CT features, namely standardized uptake volume (SUVmax), maximum distance between tumor lesions (Dmax), metabolic tumor volume (MTV) and total lesion glycolysis (TLG), have been recently included in different prognostic models to refine outcome prediction in DLBCL patients. These models are able to identify high-risk DLBCL and, in some cases, can outperform the international prognostic index (IPI) risk score [6,7,8,9].
Liquid biopsy, here intended as the analysis of circulating tumor DNA (ctDNA), is regarded as a minimally invasive strategy to estimate tumor burden and to predict outcome in DLBCL patients [10]. In particular, the analysis of ctDNA levels is a powerful tool to predict outcome at the time of diagnosis and during the course of R-CHOP therapy [11]. Also, ctDNA has been shown as a reliable option to biologically classify DLBCL patients into molecular clusters in a non-invasive manner [12], recapitulating DLBCL molecular clusters identified on tissue [13,14,15,16].
On these grounds, baseline [18F]FDG-PET/CT parameters, ctDNA levels and molecular clusters on the liquid biopsy individually represent powerful biomarkers able to stratify clinical risk in DLBCL. However, their integration has not been extensively evaluated and might generate prognostic models able to further refine outcome prediction for this lymphoma.
Materials and methods
Patients and samples
A real-life cohort of 120 newly diagnosed DLBCL patients consecutively referring to our institution were included in the study. Patients had a diagnosis of DLBCL not otherwise specified (NOS) [17, 18] and were treated with R-CHOP-based therapy. All cases were provided at baseline with: i) [18F]FDG-PET/CT scans; ii) ctDNA from plasma; and iii) germline gDNA extracted from granulocytes for comparative purposes. Patients provided informed consent in accordance with Institutional Review Board requirements and the Declaration of Helsinki. The study was approved by the Ethical Committee of the Ospedale Maggiore della Carità di Novara associated with the Università del Piemonte Orientale (study number CE 120/19).
[18F]FDG-PET/CT analysis
All PET/CT scans were acquired using the same protocol, following the procedural guidelines described by the European Nuclear Medicine Association (EANM) [19]. Specifically, each patient fasted for at least 6 hours before the examination and was injected with 2.5–3 Mbq/kg of [18F]FDG with a blood glucose level below 200 mg/dL. After 60 ± 10 minutes, total-body images from the nasion to the proximal third of the femurs were acquired. Non-contrast low-dose CT co-registration images were gathered to perform the attenuation correction processing, and then the images were reconstructed on the three spatial axes: axial, sagittal, and coronal. Subsequently, using the free software LIFEx v 7.4.0 [20], a semi-automatic segmentation was conducted on all evident lesions in each PET/CT scan using specific automatic segmentation tools available in the software and, when necessary, performing the manual exclusion of activity related to the presence of radioactive urine in the renal excretory or physiological uptake in the cardiac area with the aid of co-registration CT images. Data were then collected by two independent nuclear radiologists (any possible conflict was resolved by consensus) using the SUVmax ≥4.0 threshold, since the current literature suggests that a SUVmax ≥4.0 may represent a more robust, reliable, and reproducible threshold when compared to a SUVmax ≥41% [19, 21,22,23,24,25,26]. Finally, for each patient the SUVmax of the hottest lesion, the total (t) MTV, the tTLG and the distance between the two farthest hypermetabolic lesions (Dmax) were collected [19,20,21,22,23,24,25,26,27,28].
Molecular characterization of the DLBCL cohort on ctDNA
The LyV4.0 CAncer Personalized Profiling by deep Sequencing Assay (CAPP-seq) was used for the study and comprised a panel of 109 genes (199411 bp) relevant in DLBCL based on previous studies[13, 14, 16]. The genomic regions included in the panel are shown in Table S1. The number of the libraries loaded in the MiSeq/NextSeq550 instruments was tailored to obtain at least a coverage >2000× in >80% of the region of interest. A background error-suppressed approach was used for variant calling. The limit of quantification of the LyV4.0 CAPP-seq assay was 0.09%, which represented the analytical background noise threshold over which the assay produced a signal distinguishable from “blank”. The analytical sensitivity of the LyV4.0 CAPP-seq was 0.1%, representing the smallest detectable allele frequency [29,30,31]. Copy-number analysis was performed in 89 cases using the CNVkit software toolkit (version 0.9.10) in Python 3.11.4 [32]. A reference file was built from 31 minimal residual disease-negative samples; read depths were median-centered and bias-corrected (GC-content, sequence repeats, target density) to produce normalized log2 read-depth values for each bin. The results of CNVkit were internally validated by comparison to ichorCNA [33]. We applied the GISTIC algorithm on the segmented data using the GISTIC2.0 GenePattern module (version 6.15.30) to identify statistically significant copy number abnormalities (CNAs) [34].
ctDNA quantitation and molecular clusters classification
ctDNA levels were reported as haploid genome equivalents per mL of plasma (hGE/mL), determined as the product of total cfDNA concentration and the mean allele fraction of somatic mutations. This value was expressed as a base-10 logarithm (log hGE/mL) [11].
The LymphGen probabilistic classification tool was used to classify the DLBCL cases of this cohort into the previously described genetics subtypes [14]. We consider a patient assigned to a specific cluster when the tool considers the case as “core” or “extended” subtype [14].
Statistical analysis
The primary endpoint of the clinical study was progression-free survival (PFS) and the secondary endpoint was overall survival (OS) [35]. Survival analysis was performed using the Kaplan-Meier method and compared between strata using the Log-rank test. The maximally selected rank statistics was used to identify the best cut-off values in predicting PFS for ctDNA levels and for each [18F]FDG-PET/CT variable. The adjusted effects of molecular clusters, [18F]FDG-PET/CT parameters and ctDNA levels on PFS and OS were estimated by Cox regression. Internal validation of the multivariate analysis was performed using the bootstrap approach with 1000 bootstrap samples. Chi-square and Mann-Whitney tests were used to compare dichotomous and continuous variables, respectively. P-values were adjusted according to Benjamini-Hochberg correction. The C-indices were internally validated with 1000 bootstrap samples and the means between groups were compared with the T-test. The analysis was performed with the Statistical Package for the Social Sciences (SPSS) software v.24.0 (Chicago, IL) and RStudio Version 1.2.1335 2009-2019, Inc. Statistical significance was defined as p-value < 0.05.
Results
Patient characteristics and prognostic impact of ctDNA levels and PET/CT parameters
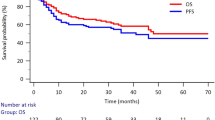
The cohort included 120 newly diagnosed DLBCL patients referring to our institution and homogenously treated with R-CHOP-based therapy. The median age of the study cohort was 67 years, 87 (72.5%) patients presented an Ann Arbor stage III/IV and 68 (56.7%) presented an IPI ≥ 3 (Table 1). After a median follow-up of 56 months, the 40-month PFS and OS were 65.1% and 75.6%, respectively (Fig. S1A, B).
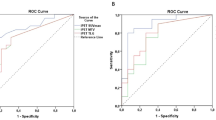
A recursive partitioning approach was used to maximize the log-rank statistics for PFS in the 120 DLBCL patients enrolled in the present study. The list of all PET/CT parameters for each individual patient is represented in Table S2. Consistently, the optimal cut-off of SUVmax, tMTV, Dmax and tTLG for predicting PFS were 17.66, 639.20 cm3, 39 cm and 7138.34, respectively (Fig. S2A–D). For all PET/CT parameters, these cut-off values segregated patients for significantly different PFS and OS. In detail, patients with a SUVmax >17.66 (N = 78) had a 40-month PFS and OS of 57.9% and 70.5% compared to 78.6% and 84.8% for patients with a SUVmax ≤17.66 (N = 42) (p = 0.023 and p = 0.056, respectively) (Figs. 1A and S3A). Patients with a tMTV >639.20 cm3 (N = 39) had a 40-month PFS and OS of 36.8% and 51.6% compared to 78.8% and 86.3% for patients with a tMTV ≤639.20 cm3 (N = 81) (p < 0.001 and p = 0.0023, respectively) (Figs. 1B and S3B). Patients with a tTLG >7138.34 (N = 33) had a 40-month PFS and OS of 34.5% and 51.0% compared to 76.7% and 84.5% for patients with a tTLG ≤7138.34 (N = 87) (p < 0.001 and p = 0.0016, respectively) (Figs. 1C and S3C). Patients with a Dmax >39 cm (N = 51) had a 40-month PFS and OS of 47.6% and 65.2% compared to 78.0% and 83.3% for patients with a Dmax ≤39 cm (N = 69) (p = 0.018 and p = 0.082, respectively (Figs. 1D and S3D).
Kaplan-Meier estimates of PFS according to cut-off values of (A) SUVmax, (B) tMTV, (C) tTLG and (D) Dmax. Patients with values under the respective cut-off for each PET/CT parameter are represented by the blue curves and patients above the cut-off are represented by the red curves. E Correlation map comparing clinical, metabolic and molecular features. The red color scale of -log10 (p) points to a co-occurrence between two variables. The blue color scale of -log10 (p) points to a mutual exclusivity between two variables. The intensity of the color corresponds to the strength of the correlation. The white boxes denote non-significant correlations.
By using the same approach utilized for PET/CT parameters, a threshold of 2.68 Log10hGE was identified as the optimal cut-off that maximizes the log-rank statistics for PFS (Fig. S2E). The complete list of variants identified on ctDNA, of ctDNA levels and of CNVs for each patient are reported in Tables S3 and S4. Patients with ctDNA levels >2.68 Log10hGE (N = 43), termed ctDNA-high, had a 40-month PFS and OS of 42.9% and 55.4% compared to 77.4% and 86.5% for ctDNA-low patients (p < 0.001 and p < 0.001, respectively) (Fig. 2A, B). The C-index based on ctDNA levels was 0.630 for PFS and 0.648 for OS (Table 2).
Kaplan-Meier estimates of (A) PFS and (B) OS according to ctDNA levels. Patients with ctDNA levels ≤ 2.68 log hGE/mL are represented by the blue curves and patients with ctDNA levels > 2.68 log hGE/mL are represented by the red curves. Kaplan-Meier estimates of (C) PFS and (D) OS according to the presence of at least one PET/CT variable above the respective cut-off value (high-risk PET). Low-risk PET patients are represented by the blue curves and high-risk PET patients are represented by the red curves.
Correlations of PET/CT parameters and ctDNA levels with baseline clinical characteristics
The correlations between PET/CT variables and clinical or biological features, namely IPI score, Ann Arbor stage, cell of origin (COO), LDH, extranodal involvement and molecular clusters identified on ctDNA (A53, BN2, EZB, MCD, ST2) [14], were investigated and p-values were adjusted for Benjamini-Hochberg correction. A high tMTV directly correlated with an advanced Ann Arbor stage (p = 0.005), elevated LDH level (p < 0.001), and a higher IPI score (p = 0.004). Higher values of tTLG directly correlated with an advanced Ann Arbor stage (p = 0.022), elevated LDH level (p < 0.001), and a higher IPI score (p = 0.016). Finally, values of Dmax greater than the respective cut-off directly correlated with an advanced Ann Arbor stage (p < 0.001) and a higher IPI score (p < 0.001) (Fig. 1E).
Higher ctDNA levels directly correlated with an advanced Ann Arbor stage (p = 0.016), elevated LDH level (p < 0.001), a higher IPI score (p = 0.049), MCD cluster (p = 0.030) and BN2 cluster (p = 0.016) (Fig. 1E).
Moreover, by evaluating the relationship between PET/CT variables and ctDNA levels, ctDNA levels >2.68 Log10hGE directly correlated with higher values of tMTV (p < 0.001), tTLG (p < 0.001) and Dmax (p = 0.016), while there was not a significant correlation with higher SUVmax values (Fig. 1E).
Integration between ctDNA levels and PET/CT parameters
After assessing the individual prognostic impact of ctDNA levels and each PET/CT parameter, we proceeded to investigate whether their integration would improve outcome prediction. In four different bivariate Cox regression analyses including each single PET/CT feature together with ctDNA levels, tMTV (HR 2.42, 95% CI 1.28-4.58, p = 0.007), tTLG (HR 2.42, 95% CI 1.28-4.60, p = 0.007) and Dmax (HR 1.97, 95% CI 1.07-3.65, p = 0.031) maintained an independent association with a shorter PFS, while SUVmax (HR 1.84, 95% CI 0.91-3.69, p = 0.087) lost its prognostic value (Fig. S4A–D). In all the above-mentioned bivariate analyses, ctDNA levels also retained independent association with shorter PFS (Fig. S4A–D). Therefore, patients with at least one PET/CT value (namely tMTV, tTLG or Dmax) above the respective cut-off were grouped as high-risk PET patients (N = 67). More precisely, 18 patients have all the three PET/CT variables above the respective cut-off, 20 patients have two PET/CT variables above the respective cut-off and 29 patients have only one PET/CT variable above the respective cut-off. High-risk PET patients had a significantly worse outcome compared to low-risk PET patients, with a 40-month PFS and OS of 45.4% and 62.2% compared to 90.4% and 92.3% (p < 0.001 and p = 0.007, respectively) (Fig. 2C, D). The C-index for the high-risk PET variable was 0.685 for PFS and 0.645 for OS (Table 2).
By multivariate analysis, ctDNA-high (HR 2.04, 95% CI 1.10-3.78, p = 0.024) and high-risk PET (HR 3.84, 95% CI 1.78-8.28, p < 0.001) independently predicted PFS (Fig. 3A). Relying on β coefficients, 1 point was assigned to ctDNA-high patients and 2 points were assigned to high-risk PET patients. Patients were then grouped into three risk classes, according to their total score, and presented significantly different outcomes (p < 0.001 for both PFS and OS). Low-risk DLBCL (0 points, N = 44) were both ctDNA-low and low-risk PET and presented a 40-month PFS and OS of 93.0% and 95.3%. Intermediate-risk DLBCL (1 and 2 points, N = 42) were either ctDNA-high or high-risk PET and presented a 40-month PFS and OS of 61.5% and 75.4%. High-risk DLBCL (3 points, N = 34) were both ctDNA-high and high-risk PET and presented a 40-month PFS and OS of 33.6% and 49.8% (Fig. 3B, C). Importantly, when compared to ctDNA-high and high-risk PET variables alone, the novel 2-factor prognostic model improved the C-index for both PFS and OS (0.712 and 0.696, respectively) (Table 2).
A Multivariate analysis of PFS including ctDNA-high and high-risk PET variables with β coefficients and points assigned to each variable. The table shows how the patients were grouped based on their total score. Kaplan-Meier estimates of (B) PFS and (C) OS according to the two-variable score. Low-risk patients (0 points, both ctDNA-low and low-risk PET) are represented by the blue curves, intermediate-risk patients (1 and 2 points, either ctDNA-high or high-risk PET) are represented by the yellow curves, high-risk patients (3 points, both ctDNA high and high-risk PET) are represented by the red curves.
Molecular clusters on liquid biopsy improve outcome prediction
Since molecular clusters identified on liquid biopsy harbor prognostic relevance in DLBCL patients (Table S5) [12], we tried to integrate this biological feature into the 2-factor prognostic score. As expected, A53 (40-month PFS 0%) and MCD (40-month PFS 33.3%) clusters were associated with a worse outcome, whereas patients belonging to BN2 (40-month PFS 83.3%), EZB (40-month PFS 83.3%) or ST2 (40-month PFS 75.0%) clusters were associated with a better outcome after R-CHOP (Fig. S5A, B). By combining the molecular clusters associated with favorable outcomes (BN2, EZB and ST2 clusters; N = 33), patients belonging to this group presented a 40-month PFS and OS of 81.3% and 90.0% compared to 59.3% and 70.3% for patients belonging to other molecular clusters or not classified (N = 87) (p = 0.044 and p = 0.028, respectively) (Fig. S5C, D).
In multivariate analysis, BN2/EZB/ST2 clusters (HR 0.27, 95% CI 0.12-0.62, p = 0.02) maintained an independent association with a better PFS even when adjusted for ctDNA-high (HR 2.77, 95% CI 1.45-5.27, p = 0.002) and for high-risk PET (HR 3.90, 95% CI 1.79-8.48, p < 0.001) (Fig. 4A).
A Multivariate analysis with bootstrapping validation of PFS including ctDNA-high, high-risk PET and BN2/EZB/ST2 variables with β coefficients and points assigned to each variable. The table shows how the patients were grouped based on their total score. Kaplan-Meier estimates of (B) PFS and (C) OS according to the three-variable score. Low-risk patients (−1.5 to 0.5 points) are represented by the blue curves, intermediate-risk patients (1–1.5 points) are represented by the yellow curves, high-risk patients (2.5 points) are represented by the red curves.
A novel 3-factor prognostic model was therefore devised. According to the β coefficients, 1 point was assigned to ctDNA-high, 1.5 points to high-risk PET and −1.5 points to BN2/EZB/ST2 patients. Three different groups with unique PFS and OS were identified. Low-risk DLBCL (−1.5 to 0.5 points, N = 57) presented a 40-month PFS and OS of 91.1% and 94.6%, intermediate-risk DLBCL (1 to 1.5 points, N = 41) presented a 40-month PFS and OS of 58.1% and 74.6%, and high-risk DLBCL (2.5 points, N = 22) presented a 40-month PFS and OS of 12.1% and 27.3%, respectively (both p < 0.001) (Fig. 4B, C). Notably, the variables of the 3-factor prognostic model were all frequently selected by internal 1000X bootstrap validation (bootstrap selection ranging from 85.0% to 96.4%; Fig. 4A). Importantly, when compared to the previous 2-factor prognostic model, the addition of molecular clusters into the 3-factor prognostic model significantly improved, after internal 1000X bootstrap validation, the C-statistics both for PFS (mean C-index 0.745, 95% CI 0.668- 0.799, p < 0.0001) and for OS (mean C-index 0.746, 95% CI 0.649-0.813, p < 0.0001) (Table 2). Also, eight random training-validation splits of the dataset using 80 patients as training and 40 patients as validation were performed. In all 8 iterations, the progression-free survival curves of the 3-factor prognostic model maintained statistical significance (Fig. S6).
Finally, the variables of the 3-factor prognostic model were compared with the prognostic markers currently used in the clinical practice to predict outcome in newly diagnosed DLBCL, namely IPI and COO. In multivariate analysis, both IPI ≥ 3 (HR 0.85, 95% CI 0.41–1.76, p = 0.662) and non-GC COO (HR 1.58, 95% CI 0.72–3.47, p = 0.259) lost their prognostic impact, whereas ctDNA-high (HR 2.45, 95% CI 1.22–4.96, p = 0.012) and a high-risk PET (HR 6.50, 95% CI 2.38–18.03, p < 0.001) maintained an independent association with a shorter PFS and BN2/EZB/ST2 clusters (HR 0.32, 95% CI 0.13–0.83, p = 0.020) maintained an independent association with a better PFS (Table 3).
Discussion
The present study employed a multilayered approach integrating three distinct prognostic markers for DLBCL - i.e. PET/CT radiomics, ctDNA levels, and molecular clusters from liquid biopsy - into a novel 3-factor prognostic model that stratifies patient outcomes with a greater accuracy than clinical prognostic biomarkers.
Different PET/CT radiomics features have been demonstrated capable of predicting outcomes in DLBCL [6,7,8, 27, 28]. The bidimensional parameters, i.e. SUVmax, have an established prognostic value, but the tridimensional parameters, namely tMTV, tTLG and Dmax, may capture also spatial heterogeneity and disease dissemination [27, 28]. Various approaches have been employed to assess the prognostic impact of tMTV, tTLG and Dmax, considering them as either continuous or dichotomic variables. However, no clear cut-off has been established to date, due to heterogeneity across studies in the cut-off values, which largely depends on the study population, software platforms for analysis, and statistical approaches adopted [6,7,8,9, 36,37,38,39,40]. To ensure consistent analysis of all available data, this study employed the maximally selected rank statistics to determine the optimal cut-off values to predict PFS for each PET/CT variable. The cut-off values identified in this study need further validation in additional DLBCL patient cohorts to confirm their prognostic significance and their potential for implementation in the clinical practice.
In order to test the independent prognostic value of each PET/CT parameter with ctDNA levels, max-stat statistics was also applied to ctDNA levels and the 2.68 log hGE/mL cut-off (very close to the previously reported value of 2.5 log hGE/mL) [11] was identified as the optimal value to predict DLBCL outcome. Importantly, in the multivariate analysis of the 3-factor prognostic model, use of the 2.5 log hGE/mL cut-off allowed to achieve superimposable outcome results (Table S7). Subsequently, by multivariate analysis, the tridimensional PET/CT parameters (i.e. tMTV, tTLG and Dmax) retained their prognostic significance after adjustment for ctDNA levels, whereas the bidimensional PET/CT parameter SUVmax lost its prognostic impact. This finding highlights the importance of capturing the anatomical heterogeneity of DLBCL by considering the potential impact of all individual lesions identified during PET/CT staging (by using tMTV, tTLG and Dmax), rather than focusing solely on the most metabolically active lesion (by using SUVmax). Therefore, patients with at least one PET/CT parameter among tMTV, tTLG and Dmax above the respective cut-off value were grouped as high-risk PET patients.
An early identification of relapsing/refractory DLBCL patients a priori before re-treatment represents a major unmet clinical need. To address this issue, we integrated the three prognostic markers investigated in this cohort, namely PET/CT parameters (tMTV, tTLG and Dmax), ctDNA levels and molecular clusters. Initially, the 2-factor prognostic model validated the independent prognostic value of high-risk PET and ctDNA-high levels. However, PET/CT scans and ctDNA levels merely represent a phenotypic expression of an underlying molecular landscape, that varies among patients and influences their clinical presentation.
To address the molecular heterogeneity of DLBCL, we took advantage of the recent demonstration that ctDNA analysis with the LymphGen tool allows to classify a fraction of DLBCL into distinct molecular clusters, thereby providing insights into the intrinsic disease biology [12, 14]. Importantly, the molecular profiles and outcomes of the clusters identified in this study were consistent with previous findings. For instance, the A53 cluster showed an enrichment of CNVs compared to non A53 patients (p = 0.038) and the MCD cluster was associated with poor outcomes [14]. Notably, the percentage of classified patients in our cohort (i.e. 38.4%) is in line with previous studies using targeted panels and classifying approximately 40% of patients [41, 42]. In the current cohort, both the proportion of classifiable patients and the clinical impact of the clusters identified on ctDNA closely mirrored those observed on the tissue biopsy.
The greatest improvement in outcome prediction documented by C-statistics was achieved by incorporating molecular clusters into the 3-factor prognostic model, further supporting the notion that the underlying DLBCL biology enhances outcome prediction. Previous studies have investigated the integration of liquid biopsy with PET/CT, but they included only one liquid biopsy biomarker (i.e. ctDNA levels) with only one PET/CT parameter (i.e. tMTV) [39, 43]. To the best of our knowledge, this study is the first to demonstrate that multiple PET/CT parameters (i.e. tMTV, tTLG and Dmax) and multiple liquid biopsy biomarkers (i.e. ctDNA levels and molecular clusters), if integrated simultaneously into a single prognostic score, significantly improve DLBCL outcome prediction compared to using each biomarker individually. Importantly, the variables of the 3-factor prognostic model outperformed the prognostic impact of clinical parameters routinely used in the clinical practice, namely IPI and COO.
This study aimed at demonstrating the feasibility of integrating liquid biopsy with PET/CT parameters, rather than validating a specific prognostic score. Based on sample power analysis, a single cohort of at least 114 DLBCL patients was required to demonstrate that, compared to ctDNA levels only, the integration of PET/CT parameters, ctDNA levels and molecular clusters can improve this sensitivity in predicting cure from 72.5% to 85% (assuming a type I error rate of α = 0.05 and 90% power) [11]. Accordingly, a training-validation design was not employed, and all 120 DLBCL patients were included in the analysis. Nevertheless, to mitigate the lack of an external validation, we have performed extensive internal validation through multiple bootstrapping analyses and all retained statistical significance.
The present study also provides the background for dynamic investigations of the multilayered biomarker assessment utilized herein. In fact, in addition to the static baseline evaluation at diagnosis, monitoring the dynamic changes in ctDNA levels and PET/CT parameters during treatment and at therapy completion might offer potential valuable prognostic insights. This approach may help anticipate disease progression or early relapse, even when traditional radiologic and metabolic assessments based on the Lugano criteria suggest a favorable response [35, 44]. Notably, recent evidence has documented that molecular clusters identified at diagnosis on the tissue biopsy enhance the prognostic accuracy of end-of-therapy (EOT) PET/CT when solely based on the Deauville score [45].
Liquid biopsy biomarkers are minimally invasive and capture information from all disease sites, and PET/CT scans are already used for staging and evaluating response assessment in DLBCL. The assessment of these prognostic markers in the clinical practice and combining them in a prognostic score is devoid of major hurdles for patients, appears to be feasible, and might help identify DLBCL patients who may benefit most from standard chemoimmunotherapy, as well as cases at high risk of early relapse who should be prioritized for the access to innovative treatment strategies. Dedicated clinical trials combining liquid biopsy biomarkers with PET/CT parameters during the first cycle of standard chemoimmunotherapy might be pivotal to identify high-risk DLBCL patients who may benefit the most from an early switch to bispecific monoclonal antibodies and/or CAR-T cell therapy.
Data availability
Data files will be made available upon reasonable request to the corresponding authors.
References
Sehn LH, Salles G. Diffuse Large B-Cell Lymphoma. N Engl J Med. 2021;384:842–58.
Susanibar-Adaniya S, Barta SK. 2021 Update on Diffuse large B cell lymphoma: A review of current data and potential applications on risk stratification and management. Am J Hematol. 2021;96:617–29.
Lue JK, O’Connor OA. A perspective on improving the R-CHOP regimen: from Mega-CHOP to ROBUST R-CHOP, the PHOENIX is yet to rise. Lancet Haematol. 2020;7:e838–e850.
Tilly H, Morschhauser F, Sehn LH, Friedberg JW, Trněný M, Sharman JP, et al. Polatuzumab vedotin in previously untreated diffuse large B-cell lymphoma. N Engl J Med. 2022;386:351–63.
Lenz G, Tilly H, Ziepert M, Altmann B, Herbaux C, Frontzek F, et al. Pola-R-CHP or R-CHOEP for first-line therapy of younger patients with high-risk diffuse large B-cell lymphoma: a retrospective comparison of two randomized phase 3 trials. Leukemia. 2024;38:2709–11.
Zhang YY, Song L, Zhao MX, Hu K. A better prediction of progression-free survival in diffuse large B-cell lymphoma by a prognostic model consisting of baseline TLG and %ΔSUVmax. Cancer Med. 2019;8:5137–47.
Mikhaeel NG, Heymans MW, Eertink JJ, de Vet HCW, Boellaard R, Dührsen U, et al. Proposed new dynamic prognostic index for diffuse large B-cell lymphoma: international metabolic prognostic index. J Clin Oncol. 2022;40:2352–60.
Eertink JJ, Zwezerijnen GJC, Heymans MW, Pieplenbosch S, Wiegers SE, Dührsen U, et al. Baseline PET radiomics outperforms the IPI risk score for prediction of outcome in diffuse large B-cell lymphoma. Blood. 2023;141:3055–64.
Eertink JJ, van de Brug T, Wiegers SE, Zwezerijnen GJC, Pfaehler EAG, Lugtenburg PJ, et al. 18F-FDG PET baseline radiomics features improve the prediction of treatment outcome in diffuse large B-cell lymphoma. Eur J Nucl Med Mol Imaging. 2022;49:932–42.
Lauer EM, Mutter J, Scherer F. Circulating tumor DNA in B-cell lymphoma: technical advances, clinical applications, and perspectives for translational research. Leukemia. 2022;36:2151–64.
Kurtz DM, Scherer F, Jin MC, Soo J, Craig AFM, Esfahani MS, et al. Circulating tumor DNA measurements as early outcome predictors in diffuse large B-cell lymphoma. J Clin Oncol. 2018;36:2845–53.
Moia R, Talotta D, Terzi Di Bergamo L, Almasri M, Dondolin R, Salehi M, et al. Molecular clustering on ctDNA improves the prognostic stratification of DLBCL patients compared to ctDNA levels. Blood Adv. 2025;9:1692–701.
Lacy SE, Barrans SL, Beer PA, Painter D, Smith AG, Roman E, et al. Targeted sequencing in DLBCL, molecular subtypes, and outcomes: a Haematological Malignancy Research Network report. Blood. 2020;135:1759–71.
Wright GW, Huang DW, Phelan JD, Coulibaly ZA, Roulland S, Young RM, et al. A probabilistic classification tool for genetic subtypes of diffuse large B cell lymphoma with therapeutic implications. Cancer Cell. 2020;37:551–.e514.
Chapuy B, Stewart C, Dunford AJ, Kim J, Kamburov A, Redd RA, et al. Molecular subtypes of diffuse large B cell lymphoma are associated with distinct pathogenic mechanisms and outcomes. Nat Med. 2018;24:679–90.
Schmitz R, Wright GW, Huang DW, Johnson CA, Phelan JD, Wang JQ, et al. Genetics and pathogenesis of diffuse large B-cell lymphoma. N Engl J Med. 2018;378:1396–407.
Alaggio R, Amador C, Anagnostopoulos I, Attygalle AD, Araujo IBO, Berti E, et al. The 5th edition of the World Health Organization Classification of Haematolymphoid Tumours: Lymphoid Neoplasms. Leukemia. 2022;36:1720–48.
Campo E, Jaffe ES, Cook JR, Quintanilla-Martinez L, Swerdlow SH, Anderson KC, et al. The International Consensus Classification of Mature Lymphoid Neoplasms: a report from the Clinical Advisory Committee. Blood. 2022;140:1229–53.
Boellaard R, Delgado-Bolton R, Oyen WJ, Giammarile F, Tatsch K, Eschner W, et al. FDG PET/CT: EANM procedure guidelines for tumour imaging: version 2.0. Eur J Nucl Med Mol Imaging. 2015;42:328–54.
Nioche C, Orlhac F, Boughdad S, Reuzé S, Goya-Outi J, Robert C, et al. LIFEx: A freeware for radiomic feature calculation in multimodality imaging to accelerate advances in the characterization of tumor heterogeneity. Cancer Res. 2018;78:4786–9.
Ilyas H, Mikhaeel NG, Dunn JT, Rahman F, Møller H, Smith D, et al. Defining the optimal method for measuring baseline metabolic tumour volume in diffuse large B cell lymphoma. Eur J Nucl Med Mol Imaging. 2018;45:1142–54.
Burggraaff CN, Rahman F, Kaßner I, Pieplenbosch S, Barrington SF, Jauw YWS, et al. Optimizing workflows for fast and reliable metabolic tumor volume measurements in diffuse large B cell lymphoma. Mol Imaging Biol. 2020;22:1102–10.
Zhao S, Wang J, Jin C, Zhang X, Xue C, Zhou R, et al. Stacking ensemble learning-based [18F]FDG PET radiomics for outcome prediction in diffuse large B-cell lymphoma. J Nucl Med. 2023;64:1603–9.
Knaup H, Weindler J, van Heek L, Voltin CA, Fuchs M, Borchmann P, et al. PET/CT reconstruction and its impact on [measures of] metabolic tumor volume. Acad Radio. 2024;31:3020–5.
van Heek L, Weindler J, Gorniak C, Kaul H, Müller H, Mettler J, et al. Prognostic value of baseline metabolic tumor volume (MTV) for forecasting chemotherapy outcome in early-stage unfavorable Hodgkin lymphoma: Data from the phase III HD17 trial. Eur J Haematol. 2023;111:881–7.
Barrington SF, Zwezerijnen BGJC, de Vet HCW, Heymans MW, Mikhaeel NG, Burggraaff CN, et al. Automated segmentation of baseline metabolic total tumor burden in diffuse large B-cell lymphoma: which method is most successful? A Study on Behalf of the PETRA Consortium. J Nucl Med. 2021;62:332–7.
Cottereau AS, Nioche C, Dirand AS, Clerc J, Morschhauser F, Casasnovas O, et al. 18F-FDG PET dissemination features in diffuse large B-cell lymphoma are predictive of outcome. J Nucl Med. 2020;61:40–45.
Frood R, Burton C, Tsoumpas C, Frangi AF, Gleeson F, Patel C, et al. Baseline PET/CT imaging parameters for prediction of treatment outcome in Hodgkin and diffuse large B cell lymphoma: a systematic review. Eur J Nucl Med Mol Imaging. 2021;48:3198–220.
Rossi D, Diop F, Spaccarotella E, Monti S, Zanni M, Rasi S, et al. Diffuse large B-cell lymphoma genotyping on the liquid biopsy. Blood. 2017;129:1947–57.
Spina V, Bruscaggin A, Cuccaro A, Martini M, Di Trani M, Forestieri G, et al. Circulating tumor DNA reveals genetics, clonal evolution, and residual disease in classical Hodgkin lymphoma. Blood. 2018;131:2413–25.
Diop F, Moia R, Favini C, Spaccarotella E, De Paoli L, Bruscaggin A, et al. Biological and clinical implications of BIRC3 mutations in chronic lymphocytic leukemia. Haematologica. 2020;105:448–56.
Talevich E, Shain AH, Botton T, Bastian BC. CNVkit: genome-wide copy number detection and visualization from targeted DNA sequencing. PLoS Comput Biol. 2016;12:e1004873.
Rothwell DG, Ayub M, Cook N, Thistlethwaite F, Carter L, Dean E, et al. Utility of ctDNA to support patient selection for early phase clinical trials: the TARGET study. Nat Med. 2019;25:738–43.
Beroukhim R, Getz G, Nghiemphu L, Barretina J, Hsueh T, Linhart D, et al. Assessing the significance of chromosomal aberrations in cancer: methodology and application to glioma. Proc Natl Acad Sci USA. 2007;104:20007.
Cheson BD, Fisher RI, Barrington SF, Cavalli F, Schwartz LH, Zucca E, et al. Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: the Lugano classification. J Clin Oncol. 2014;32:3059–68.
Sasanelli M, Meignan M, Haioun C, Berriolo-Riedinger A, Casasnovas RO, Biggi A, et al. Pretherapy metabolic tumour volume is an independent predictor of outcome in patients with diffuse large B-cell lymphoma. Eur J Nucl Med Mol Imaging. 2014;41:2017–22.
Vercellino L, Cottereau AS, Casasnovas O, Tilly H, Feugier P, Chartier L, et al. High total metabolic tumor volume at baseline predicts survival independent of response to therapy. Blood. 2020;135:1396–405.
Cottereau AS, Lanic H, Mareschal S, Meignan M, Vera P, Tilly H, et al. Molecular profile and FDG-PET/CT total metabolic tumor volume improve risk classification at diagnosis for patients with diffuse large B-cell lymphoma. Clin Cancer Res. 2016;22:3801–9.
Le Goff E, Blanc-Durand P, Roulin L, Lafont C, Loyaux R, MBoumbae DL, et al. Baseline circulating tumour DNA and total metabolic tumour volume as early outcome predictors in aggressive large B-cell lymphoma. A real-world 112-patient cohort. Br J Haematol. 2023;202:54–64.
Ceriani L, Milan L, Chauvie S, Zucca E. Understandings 18 FDG PET radiomics and its application to lymphoma. Br J Haematol. 2025;206:1546–59.
Rivas-Delgado A, Nadeu F, Enjuanes A, Casanueva-Eliceiry S, Mozas P, et al. Mutational landscape and tumor burden assessed by cell-free DNA in diffuse large B-cell lymphoma in a population-based study. Clin Cancer Res. 2021;27:513–21.
Wilson WH, Wright GW, Huang DW, Hodkinson B, Balasubramanian S, Fan Y, et al. Effect of ibrutinib with R-CHOP chemotherapy in genetic subtypes of DLBCL. Cancer Cell. 2021;39:1643–.e3.
Dean EA, Kimmel GJ, Frank MJ, Bukhari A, Hossain NM, Jain MD, et al. Circulating tumor DNA adds specificity to PET after axicabtagene ciloleucel in large B-cell lymphoma. Blood Adv. 2023;7:4608–18.
Soscia R, Assanto GM, Starza ID, Moia R, Talotta D, Bellomarino V, et al. Molecular measurable residual disease by immunoglobulin gene rearrangements on circulating tumor DNA predicts outcome in diffuse large B-cell lymphoma. Haematologica. 2024.
Mendeville MS, Janssen J, Los-de Vries GT, van Dijk E, Richter J, Nijland M, et al. Integrating genetic subtypes with PET scan monitoring to predict outcome in diffuse large B-cell lymphoma. Nat Commun. 2025;16:109.
Acknowledgements
This work was supported by: ‘Molecular bases of disease dissemination in lymphoid malignancies to optimize curative therapeutic strategies’ (5×1000 No. 21198), Associazione Italiana per la Ricerca sul Cancro (AIRC) Foundation Milan, Italy; the AGING Project – Department of Excellence – DIMET, Università del Piemonte Orientale, Novara, Italy; PNRR-MCNT2-2023-12378037, Italian MoH, Rome, Italy; AIL Novara VCO, Novara, Italy.
Author information
Authors and Affiliations
Contributions
R.D., G.G., and R.M. designed the study, interpreted data, and wrote the manuscript; F.G., and G.M.S. analyzed PET/CT parameters and contributed to data interpretation and manuscript preparation; M.A., L.T.D.B., C.C., A.B., M.S., D.T., J.N., B.A.D., and L.C. performed molecular studies, interpreted data and contributed to manuscript revision; R.B., G.M.R., M.B., S.M., N.M., J.G., F.M., A.A., F.M., M.L., A.L., A.M.M., W.A.E., N.M.D., E.S., C.D., S.R., and R.L.B. provided study material and contributed to manuscript revision; M.G., G.A.P., V.G., R.F., and D.R. contributed to data interpretation and manuscript preparation.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics
The study was approved by local Ethical Committees (study number CE 120/19 for the training cohort; Approval n. IRB-05-2010 for the validation cohort)
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Dondolin, R., Garrou, F., Almasri, M. et al. Integration of [18F]FDG-PET radiomics with liquid biopsy improves outcome prediction in newly diagnosed diffuse large B-cell lymphoma. Leukemia 39, 2207–2214 (2025). https://doi.org/10.1038/s41375-025-02688-2
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41375-025-02688-2