Abstract
Disordered eating and self-harm commonly co-occur in young people suggesting potential for shared underlying causes. Body image dissatisfaction (BID) has been recognised as a psychological correlate of body size, associated with both disordered eating and self-harm. However, the investigation into etiological pathways early in the lifecourse to provide detail on how body size and BID may foster disordered eating and self-harm remains largely unexplored. Employing data from two large population-based cohorts, the UK Biobank and the Avon Longitudinal Study of Parents And Children (ALSPAC), we conducted bidirectional Mendelian randomization (MR) to determine the causal direction of effect between genetically predicted prepubertal body size and two measures of BID indicating (i) desire to be smaller, and (ii) desire to be larger. We then used multivariable regression followed by counterfactual mediation analyses. Bidirectional MR indicated robust evidence that increased genetically predicted prepubertal body size increased desire to be smaller and decreased desire to be larger. Evidence for the reverse causal direction was negligible. These findings remained very similar across sensitivity analyses. In females and males, multivariable regression analyses demonstrated that being overweight increased the risk of disordered eating (risk ratio (RR), 95% confidence interval (CI): 1.19, 1.01 to 1.40 and 1.98, 1.28 to 3.05, respectively) and self-harm (RR, 95% CI: 1.35, 1.04 to 1.77 and 1.55, 0.86 to 2.81, respectively), while being underweight was protective against disordered eating (RR, 95% CI: 0.57, 0.40 to 0.81 and 0.81, 0.38 to 1.73, respectively). There was weak evidence of an increase in the risk of self-harm among underweight individuals. Mediation analyses indicated that the relationship between being overweight and subsequent disordered eating was largely mediated by the desire to be smaller. Our research carries important public health implications, suggesting distinct risk profiles for self-harm and disordered eating in relation to weight and body image. In addition, a better understanding of genetically predicted prepubertal BID may be valuable in the prevention and treatment of disordered eating and self-harm in adolescence.
Similar content being viewed by others
Introduction
Incidence rates of eating pathology and self-harm increase during adolescence and are associated with a higher risk of impaired physical health, mortality, and psychiatric comorbidity [1,2,3]. Whilst phenotypically distinct, disordered eating (weight-control behaviours, abnormal eating) and self-harm (intentionally harming oneself, with or without suicidal intent) have been shown to commonly co-occur in young people, suggesting the likelihood of shared underlying causes [2, 4,5,6]. Co-occurring disordered eating and self-harm may lead to more severe outcomes than either experience in isolation [4, 7, 8]. Furthermore, those who self-harm often report a history of eating disorders, suicide ideation, and body image dissatisfaction (BID) [9]. BID is defined as a negative subjective evaluation of the weight and shape of one’s own body [10, 11]. Individuals with higher levels of BID have been shown to be at greater risk of eating disorders [12, 13] and self-harm [14].
BID is a potential intervention target in psychological therapy. At the individual-level, BID may be managed effectively to prevent the development of adverse outcomes across an individual’s lifetime. This may be achieved using cognitive-behavioural therapy [15, 16] or self-esteem enhancement [17]. In addition, BID also holds promise as a potentially modifiable risk factor for population-based interventions. These may include media literacy [18, 19] and psychoeducation [20]. The examination of etiologic pathways early in the lifecourse, to provide more detail on how this risk factor fosters both disordered eating and self-harm in adolescence, remains largely unexplored, despite implications for prevention.
Sociocultural explanations of the development of BID propose that society promotes an appearance culture that emphasises the importance of physical attractiveness [21]. Along with emotional well-being and self-esteem, reporting satisfaction with body image is shown to decrease with obesity [22]. The Dual-Pathway model of disordered eating hypothesizes that a higher body mass index (BMI) leads to BID [23]. In addition, studies have shown that the association between BID and body weight is different between sexes [24,25,26]. Firstly, there appears to be stronger evidence of BID in overweight women in comparison to their normal weight counterparts, than in men [16, 27]. Secondly, boys are more likely to experience BID (utilised as a categorical variable) when they are below or above average weight and most satisfied when they consider themselves an average weight [25]. Conversely, in girls, BID linearly increases with body weight [26]. However, whilst high body weight is seen as a consistent biological factor correlated with BID, whether actual body size causes BID, BID leads to a change in body size, or whether both are occurring at the same time in the peri-pubertal phase, has yet to be determined.
Mendelian randomization (MR) uses genetic variants robustly associated with an exposure of interest to strengthen inference regarding the causal influence of an exposure on an outcome [28, 29]. In theory, this technique is less susceptible to the issues of confounding, including confounding by undiagnosed existing disease (reverse causation), which can affect more conventional epidemiological techniques. A study applying MR in a one-sample setting reported that a standard deviation increase in BMI genetic risk score was associated with a 9% increased odds of BMI (odds ratio (OR): 1.09, 95% confidence interval (CI): 1.01, 1.18) [30]. However, bidirectional MR was not performed and therefore evidence for a potential causal effect of BID on BMI was not determined. In the relationship between body size and disordered eating and self-harm, the role of BID could be as a confounder, where BID could independently lead to both changes in body size and disordered eating or self-harm. BID could also be a mediator, such that high or low body size may cause BID which then leads to increased risk of disordered eating or self-harm. In any single-mediator model there are three posited causal relationships and the direction of all three requires justification. In our case, we focus on the direction of causality between BMI and BID. We believe that reverse causation is unlikely for either path involving disordered eating or-self harm in adolescence since these dependent variables are such that we assume the population does not have the outcome when the mediating variable is measured (disordered eating and self-harm are extremely rare as manifestations of the same phenotypes, prepuberty).
Our work was guided by the hypothesis that prepubertal body size has a causal effect on BID which acts as a mediator between body size and both disordered eating and self-harm. We additionally expected to see an analogous relationship between body size and both disordered eating and self-harm. Using data from two large longitudinal cohorts, the UK Biobank and the Avon Longitudinal Study of Parents And Children (ALSPAC), this investigation set out to assess whether BID may have a causal role in the association between body size and both disordered eating and self-harm in adolescence, by employing a novel combination of epidemiological methods. Specifically, in addition to conventional epidemiological techniques, we used bidirectional two-sample MR to determine the direction of effect between genetically predicted body size and genetically predicted BID. Subsequently, we ran counterfactual mediation analyses accounting for intermediate confounding to infer the causal relationship between body size and both disordered eating and self-harm in adolescence, through the potential mediating effects of prepubertal BID.
Materials and methods
Data sources and instruments
UK Biobank
We used summary statistics derived from UK Biobank data for MR analyses [31]. Data were collected between 2006 and 2010 on individuals aged between 40 and 69 years old at baseline. Using a prospective cohort study design, data were collected from clinical examinations, assays of biological samples, detailed information on self-reported health characteristics, and genome-wide genotyping [32]. The UK Biobank study has obtained ethics approval from the Research Ethics Committee (REC; approval number: 11/NW/0382) and informed consent from all participants enrolled in UK Biobank.
The Avon Longitudinal Study of Parents And Children (ALSPAC)
We obtained data on children and adolescents from ALSPAC, a prospective population-based cohort study that recruited pregnant women living in the former county of Avon (UK) with expected delivery dates between 1 April 1991 and 31 December 1992 [33, 34]. There were 20,248 pregnancies identified as being eligible. The initial number of pregnancies enrolled was 14,541. Of the initial pregnancies, there was a total of 14,676 fetuses, resulting in 14,062 live births and 13,988 children who were alive at 1 year of age. When the oldest children were ~7 years of age, an attempt was made to bolster the initial sample with eligible cases who had failed to join the study originally. The total sample size for analyses using any data collected after the age of seven is therefore 15,447 pregnancies, resulting in 15,658 fetuses. Of these 14,901 children were alive at 1 year of age. The study website contains details of all the data that is available through a fully searchable data dictionary and variable search tool (www.bristol.ac.uk/alspac/researchers/our-data/). Consent for biological samples has been collected in accordance with the Human Tissue Act (2004). Ethical approval for the study was obtained from the ALSPAC Ethics and Law Committee and the local Research Ethics Committee. Informed consent for the use of data collected via questionnaires and clinics was obtained from participants following the recommendations of the ALSPAC Ethics and Law Committee at the time.
Weight-based body size—UK Biobank
Genetic variants strongly associated with childhood body size (using P ≤ 5 × 10–8 for non-false positives of a Type 1 error and r2 < 0.001 for independence of variants) were identified in a large-scale Genome-Wide Association Study (GWAS), previously undertaken in the UK Biobank study on 453,169 individuals, adjusting for age, sex, and genotyping chip [31]. The childhood body size measure employed recall questionnaire data, involving retrospective responses from adult participants who were asked whether, compared to the average, they were ‘thinner’, ‘about average’, or ‘plumper’, when they were aged 10 years old. This score has been independently validated in three distinct cohorts, providing verification that the genetic instruments can reliably separate childhood body size from adult body size [31, 35, 36].
Body size (based on BMI measurements)—ALSPAC
BMI was calculated using height (m) and weight (kg) measured at ALSPAC clinic sessions when participants were aged ~7 (mean age: 7.6 years). Further detail is provided in Supplementary Table 1. We grouped BMI into three body size age-specific categories (underweight (equivalent to the adult BMI cut point, ≤18.5 kg/m2), normal weight, and overweight (equivalent to the adult BMI cut point, ≥25 kg/m2) [37, 38]).
Body image dissatisfaction (BID)—ALSPAC
Perceived and desired body image were evaluated using the Stunkard figure rating scales [39] in a questionnaire administered to children (mean age: 10.7 years). The Stunkard figures are illustrations of different body types ranging from very thin (a value of 1) to very obese (a value of 5; Supplementary Fig. 1) [39]. Children were asked to self-select their perceived and desired body shape from the illustrated figures. BID scores were created by taking the difference between the perceived and desired body images (i.e. a score of zero indicated body satisfaction, whilst a negative score indicated body dissatisfaction (desire to be larger) and a positive score indicated body dissatisfaction (desire to be smaller)).
Outcomes—ALSPAC
Self-harm and disordered eating (fasting (not eating for at least one day), purging (vomiting or taking laxatives/other medications), and excessive exercise (that frequently interfered with daily routine/work) for the purpose of losing weight or avoiding gaining weight, as well as binge-eating (eating a very large amount of food, with loss of control, in a short period of time)) over the last year were assessed via self-report questionnaire during adolescence (mean age: 16.7 years). A thorough description of these variables as well as the questions that were employed to derive these variables are presented in Supplementary Table 2.
Confounders
Baseline and intermediate confounders were derived from the literature with support from specialists and clinicians. To guide the modelling strategy, variables were integrated into a directed acyclic graph (DAG) (Fig. 1). Baseline confounders included sex (in analyses that were not sex-stratified), birthweight, IQ, maternal education, ethnicity, father absence, weekly income, parent social class, maternal age, maternal BMI, Edinburgh Postnatal Depression Scale score (32 weeks gestation & 21 months), and stressful life events during childhood assessed using a questionnaire completed by mothers recording whether the child had experienced any of 16 upsetting events since the child was 5 years old. Except for IQ, all baseline confounders were collected at or prior to the data collection period with a mean age of 7.6 years. IQ was measured in a clinic with a mean age of 8.7 years. In including this measure as a baseline confounder, we have made the assumption that IQ did not fluctuate considerably between the ages of ~7 and 9 years. This assumption may not hold if IQ in this age range is affected by body size. Intermediate confounders (confounders of the mediator and outcome association which may be affected by the exposure) comprised self-reported measures of bullying victimization (relational and overt) and self-esteem measured at mean age of 8.7 years. Supplementary Table 3 contains further information on how several of the variables listed were derived and/or defined.
This graph illustrates the hypothesized role of prepubertal body size and body image dissatisfaction on disordered eating and self-harm in adolescence, and includes the intermediate confounders considered in the main analysis. The thick line indicates a direct effect. The thin lines indicate the indirect pathway. The dotted lines indicate pathways from intermediate confounders. Baseline confounders assumed to confound all paths: Sex; Birthweight; IQ; Indicators of SEP: Maternal education, ethnicity, father absence, weekly income, parent social class, Maternal age; Maternal BMI; Maternal depressive symptoms (32 weeks gestation & 21 months); Stressful life events.
Statistical analysis
Mediation is reliant on a theoretical model which makes a series of causal assumptions about the links between multiple variables. These causal claims are more challenging when more than one aspect of the model changes in tandem and the direction of causation may be different for different periods of the lifecourse. Thus, we sought to investigate evidence for causality using bidirectional MR to assess the direction of effect between body size and BID (Step 1). Using the appropriate regression model, we determined the confounder-adjusted relationships between exposure, mediator, and outcome (Step 2). Finally, we conducted mediation analyses using g-formula to identify the extent to which any causal relationship between body size and both disordered eating and self-harm in adolescence is mediated by prepubertal BID (Step 3). The three key steps are presented in Supplementary Fig. 2 and described in further detail below:
Step 1. Genetic analyses
Genome-wide Association Studies (GWAS)
We conducted GWAS analyses on 4011 children in ALSPAC who had complete genetic data available for the BID measure collapsed into two binary variables, indicative of (i) dissatisfaction (desire to be larger; n = 330) compared to satisfaction and dissatisfaction (desire to be smaller; n = 3681) and (ii) dissatisfaction (desire to be smaller; n = 938) and satisfaction and dissatisfaction (desire to be larger; n = 3073). These were performed using SNPTEST v2.5.6 [40]. Analyses were adjusted for age, sex, and the top 10 genetic principal components and restricted to participants of European ancestry. Children in ALSPAC were genotyped using the Illumina HumanHap550 quad genome-wide SNP genotyping platform. Imputation was performed using Impute V2.2.2 against the 1000 genomes phase 1 version 3 reference panel [41, 42]. Quality control measures included the removal of single nucleotide polymorphisms (SNPs) with ≥5% missing information, deviation from Hardy–Weinberg equilibrium (HWE) (P < 1.0 × 10−6) and minor allele frequency (MAF) ≤ 1.5% and >99.0% (due to the low case ratio, we increased the allele frequency threshold to exclude SNPs with a low minor allele count in the cases). We generated Manhattan plots which contain horizontal lines drawn at –log10(1 × 10−5) for “suggestive associations” and –log10(5 × 10−8) for the 'genome-wide significant' threshold and QQ plots (Supplementary Figs. 3 and 4) [43]. We used linkage disequilibrium (LD) clumping with an r2 threshold of 0.001 to select a set of independent instruments for each trait. This was performed using PLINK [44] and genotype data from European individuals from phase 3 (version 5) enrolled in the 1000 genomes project as a reference panel [45]. There were no genetic variants that reached genome-wide significance (P ≤ 5 × 10–8) due to the small sample sizes employed (Supplementary Tables 4B and 4C). We relaxed the conventional genome-wide significance p-value threshold for instrument selection to P ≤ 1 × 10–4 for the MR analysis. Applying MR in this study using a Robust Adjusted Profile Score (MR-RAPS) made it possible to employ genetic variants with a less stringent threshold [46, 47].
Mendelian randomization (MR)
We ran univariable bidirectional MR analyses to infer the causal direction of body size and BID, by estimating the genetically predicted effect of childhood body size on dissatisfaction (desire to be larger) and dissatisfaction (desire to be smaller) and then dissatisfaction (desire to be larger) and dissatisfaction (desire to be smaller) on childhood body size. We used two non-overlapping cohorts to minimise overfitting.
We used 1689 variants for the childhood body size exposure (Supplementary Table 4A) and 139 and 130 variants for the prepubertal BID (desire to be smaller) and BID (desire to be larger) exposures, respectively (Supplementary Table 4B and 4C).
We used MR-RAPS which maximises the profile likelihood of the ratio estimates and accounts for weak instrument bias, pleiotropy, and extreme outliers [48]. MR-RAPS is shown to be highly efficient with many weak genetic instruments by using an empirical, partially Bayes statistical analysis approach where instruments are weighted according to their strength [47, 48]. Weak instruments therefore bring less variation to the estimator. The inverse variance weighted (IVW) method was then employed as a sensitivity analysis, which takes SNP-outcome estimates and regresses them on the SNP-exposure associations [49]. MR-Egger and Weighted median were subsequently used as additional sensitivity analyses to assess the robustness of the results obtained. MR Egger is more robust to MR assumptions compared to the IVW method, including horizontal pleiotropy, whereby genetic variants influence multiple traits or disease outcomes via independent biological pathways [50].
The MR analyses were conducted using the TwoSampleMR R package [51]. Plots for this study were generated using the R package ‘qqman’ [52]. These analyses were undertaken using R (version 3.5.1).
Step 2. Regression analyses—ALSPAC
We estimated the crude and confounder-adjusted associations between body size at age 7 (mean age: 7.6 years) and both disordered eating and self-harm at 16 (mean age: 16.7 years) using Poisson regression to estimate risk ratios. Robust standard errors were used (modified Poisson) as Poisson models for binary outcomes suffer from under-dispersion. Adjusted models were controlled for the baseline confounders described. We then estimated the crude and adjusted relationships between (i) BMI and BID and (ii) BID and both disordered eating and self-harm using the appropriate regression models. We stratified all models by sex. The Likelihood Ratio test was used to measure evidence for effect modification by sex in the effect of BMI on BID.
To mitigate bias due to missing data, we used multiple imputation. This used a Fully Conditional Specification approach [53] with -mi impute chained- in Stata version 16 (StataCorp, 2019), comprising 25 cycles of regression-switching and produced 100 imputed datasets with imputation samples stratified by sex (further detail in Supplementary Table 5).
Step 3. Mediation analyses
We estimated the effect of body size on disordered eating and self-harm via BID by conducting parametric g-computation using the Stata package g-formula [54]. This package uses Monte Carlo simulation to simulate the outcome, mediators, and intermediate confounders under hypothetical interventions or “counter to the fact” scenarios [55].
The total causal effect (TCE) generated using this approach is the value of the outcome (disordered eating or self-harm) if all individuals had been exposed to a one-unit increase in BMI. The natural direct effect (NDE) is the direct (unmediated) effect of BMI on disordered eating or self-harm when BID takes the value it would be in absence of BMI. The natural indirect effect (NIE) is the effect of BMI on disordered eating or self-harm that operates by changing BID. We adjusted all direct and indirect paths for baseline confounders and the intermediate confounding effect. In order for these effects to have a causal interpretation, the following assumptions are required: that there is (i) no unmeasured confounding of the exposure-outcome relationship, (ii) no unmeasured confounding of the mediator-outcome relationship, and (iii) no unmeasured confounding of the exposure-mediator relationship [56].
Preliminary analysis uncovered two sparsely populated cells in the association between the three-category variables representing both BMI and BID—the number of children either being large and wanting to be larger, or small and wanting to be smaller, were in single digits (Supplementary Table 6). Consequently, to mitigate concerns about perfect prediction and prevent computational problems, we decided to split the sample by exposure and conduct two separate mediation analyses. Firstly, we focused on the sample of children who were either classified as normal or underweight and considered the binary BID variable 'desire to be larger' as the mediator. Following this, we switched our attention to the sample who were either considered normal or overweight and treated 'desire to be smaller' as the mediator. In both instances, separate mediation models were estimated for the disordered eating and self-harm outcomes, and for females and males (i.e. eight mediation models in total). Since we only dropped cases based on our exposure variable (BMI), this strategy would not be expected to introduce collider bias. We conducted sex-stratified analyses to provide insights into young male, as well as female, experiences of BID, disordered eating, and self-harm as (i) the published literature suggests experiences differ by sex, and (ii) information of young males in this area is sparse. The same approach to missing data, as described in Step 2, was employed for this section.
All analyses conducted in Steps 2 and 3 used Stata version 16 [57].
Results
The study sample comprised 2734 (52.6%) females and 2459 males (47.4%). Seven-hundred and thirty-one (22.6%) experienced disordered eating and 347 (10.5%) self-harmed in adolescence. Of those experiencing BID (32.1%), 1219 (73.1%) had a desire to be smaller, and 448 (26.9%) had a desire to be larger. The median BMI for children at age 7 was 15.8 kg/m2 (14.9–17.0 kg/m2) (Table 1).
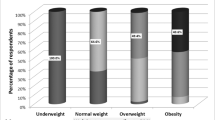
Of those with BID (desire to be smaller), individuals were more likely to be overweight than normal or low weight. Conversely, those with BID (desire to be larger), were more likely to be under or normal weight (Supplementary Table 7). Experiencing disordered eating was most common in those who were overweight (Table 2A) as well as those with BID (desire to be smaller) than in those with BID (desire to be larger) (Table 2B). These trends were stronger in females than they were in males.
Step 1. Genetic analyses (Mendelian randomization)
Of the children enrolled in ALSPAC of European ancestry, 4011 had complete data available on genotype, BID, age, sex, and the top 10 principal components. Results from MR-RAPS indicated strong evidence that having a larger genetically predicted prepubertal body size was associated with an increased log odds of BID (desire to be smaller) (β: 2.79; 95% CI: 2.15, 3.42; P = 1.194 × 10–17) (Fig. 2A, Supplementary Table 8A) and a decrease in BID (desire to be larger) (β: –2.93; 95% CI: –3.89, –1.98; P = 1.73 × 10–9) (Fig. 2B, Supplementary Table 8B). There was very little evidence of the effect of genetically predicted BID (desire to be smaller) and BID (desire to be larger) on prepubertal body size. The effect sizes in this direction were also very small. The directions of effect that were observed using MR-RAPS were reflected in the IVW, Weighted median, and MR-Egger estimates, with differing levels of strength (Fig. 2A, B, Supplementary Tables 8A and 8B).
A Forest plot displaying (i) the effects of childhood body size at age 10 (mean age: 10 years) on body image dissatisfaction (desire to be smaller) at age 10 (mean age: 10.7 years) and (ii) body image dissatisfaction (desire to be smaller) on childhood body size. B Forest plot displaying (i) the effects of childhood body size at age 10 (mean age: 10 years) on body image dissatisfaction (desire to be larger) at age 10 (mean age: 10.7 years) and (ii) body image dissatisfaction (desire to be larger) on childhood body size.
Step 2. Regression analyses
Adjusted analyses using imputed data indicated strong evidence in females (P < 0.001) and males (P = 0.007) that differences in BMI were associated with disordered eating. There was weaker evidence in females (P = 0.077) and very little evidence in males (P = 0.370) that differences in BMI were associated with self-harm. Females and males who experienced being overweight at age 7 (mean age: 7.6 years) had 1.19 (95% CI: 1.01, 1.40) and 1.98 (95% CI: 1.28, 3.05) times the risk of experiencing disordered eating, respectively, compared to their normal weight counterparts. Females and males experiencing being overweight also had 1.35 (95% CI: 1.04, 1.77) and 1.55 (95% CI: 0.86, 2.81) times the risk of experiencing self-harm, respectively. Further adjusted analyses indicated that females and males who experienced being underweight at age 7 had 0.57 (95% CI: 0.40, 0.81) and 0.81 (95% CI: 0.38, 1.73) times the risk of experiencing disordered eating and 1.09 (95% CI: 0.71, 1.65) and 1.14 (95% CI: 0.50, 2.59) times the risk of experiencing self-harm, respectively, compared to those of normal weight (Table 3).
There was strong evidence that being underweight increased BID (desire to be larger) and being overweight increased BID (desire to be smaller) (Supplementary Table 9). This effect was stronger in male participants, however, whilst there was evidence that the association between BMI and BID varied with sex in unadjusted estimates (P = 0.030), there was very little evidence of this when adjusting for selected confounders.
Step 3. Mediation analyses
In females, the effect of being underweight compared to normal weight on disordered eating was predominantly direct (RR: 0.55; 95% CI: 0.36, 0.83). There is a small proportion of this relationship mediated by BID (desire to be larger) (Table 4A). In contrast, the effect of being overweight compared to normal weight on disordered eating was largely indirect (RR: 1.22; 95% CI: 1.06, 1.41). BID (desire to be smaller) mostly mediated this association (Table 4B). There is suggestive evidence that in males, BID partially mediated the relationship between being underweight and experiencing disordered eating and being overweight and experiencing disordered eating. There is, however, lower power to detect evidence of this effect.
There is some evidence to suggest that in females, the effect of being overweight compared to normal weight on self-harm is mostly direct. There was very little mediating effect from BID (desire to be smaller). In males, the effect of being underweight compared to normal on self-harm is mostly indirect, with lower power to detect evidence of this effect. BID (desire to be larger) largely mediated this relationship. The remaining mediation effect estimates obtained reveal partial mediation of BID on the relationship between body size and self-harm.
Due to the opposite sign in the direction of effect in the relationship between the exposure and mediator and the mediator and outcome in some instances, the direct and indirect effect appeared larger than the total effect. This meant that we could not accurately calculate the proportion mediated [58].
Discussion
In this study, we employed MR and counterfactual mediation to examine the role of BID in the relationship between prepubertal body size and both disordered eating and self-harm in adolescence. Bidirectional MR indicated that higher genetically predicted childhood body size increased BID (desire to be smaller) and decreased BID (desire to be larger). In contrast, there was very little evidence of an effect of genetically predicted BID (a desire to be smaller or larger) on childhood body size.
In regression analyses, being overweight increased risk of disordered eating and self-harm in adolescence in both females and males. Conversely, being underweight appeared to be protective against disordered eating. There was more imprecision and thus weaker evidence for effects seen in males than females since disordered eating and self-harm are less common in adolescent males. The relationship between being overweight and disordered eating was largely mediated by BID (desire to be smaller). The relationship between being overweight and self-harm was only partially mediated by BID (desire to be smaller). There was little evidence of an increase in self-harm in underweight individuals. Our results additionally indicated strong evidence that being underweight increased BID (desire to be larger) and being overweight increased BID (desire to be smaller). The former of these appeared much stronger in males, however, there was little evidence that the association between body size and BID varied by sex upon conducting tests for interaction. Since high comorbidity of disordered eating and self-harm in adolescence has been reported previously [2, 4,5,6] and common risk factors include increased emotional dysregulation and impulsivity [5, 8], we expected to see an analogous relationship between body size and disordered eating and self-harm. However, our study has shown that risk profiles for disordered eating and self-harm differ in relation to weight-based risk measures.
Published findings regarding the association between being underweight and experiencing self-harm, suicidal ideation or suicide are conflicting. A systematic review and meta-analysis containing 38 observational studies indicated evidence that being underweight increased risk of completed suicide (HR: 1.21, 95% CI: 1.07, 1.36, p = 0.002) [59]. On the other hand, a population-based cohort study of male conscripts in Sweden showed that both low and high BMI was associated with increased risk of self-harm [60]. Studies investigating the association between BMI and suicidal ideation have reported different findings for males and females. For example, a study in young adults indicated an association between obesity and suicide risk for women, but not for men [61]. We found that being underweight, as well as overweight, compared to normal weight was more likely to increase self-harm in males relative to females. In addition, the effect of being overweight compared to normal weight on self-harm was only mediated to a small extent by BID (desire to be smaller). An alternative pathway not considered in our study may be that obesity increases risk of depression [62], which could be unrelated to BID. This may also result from the reverse cause, where depression could drive lower weight.
Disordered eating attitudes and behaviours are common among children and adolescents [63]. Those that are overweight during this life stage have been identified as a subset at especially high risk [64]. Whilst binge-eating disorder and night-eating syndrome are forms of disordered eating associated with overweight and obesity, they are also associated with weight gain over time [65, 66]. Binge-eating is reported to have the highest prevalence of comorbid obesity [63]. Results from our MR analyses show a one-directional causal relationship between being overweight and BID.
The majority of studies that have looked at the relationship between body size and body image have done so in female groups [67]. The few previous studies that have examined this relationship in women and men have identified a stronger effect of BID in overweight women compared to their normal weight counterparts, than in men [16, 27]. Conversely, we found a stronger relationship between being overweight and experiencing BID (desire to be smaller) in males than in females. However, tests for interaction indicated that there was very little evidence this association varied by sex. If this discrepancy were indeed real, it may be because the data we used were collected at a time (late 1990s to early 2000s) where changes in cultural attitudes toward the male body have been reported, and males may have felt under increasing pressure to conform to a cultural ideal of a lean, well-toned, muscular build [68]. In addition, counter to previous literature that suggests boys are more likely to experience BID when they are below or above average weight [25, 26], we identified a linear increase of BID with body weight in males as well as females.
This study is an important and novel analysis with several strengths. We used complimentary causal inference epidemiological methods to investigate the role of prepubertal body size and BID on disordered eating and self-harm. Specifically, we used the genetic epidemiological technique, MR (after running GWAS), as well as mediation analyses to assess causal pathways using g-formula. We also employed large population-based samples for this research. In addition, we conducted sex-stratified analyses. As a result, this study provides insight into young male experiences of BID, self-harm, and disordered eating which are largely unexplored in the published literature. Lastly, we examined disordered eating and self-harm over a key life period. In focusing on the age groups selected for this study, we were able to observe the exposure and mediator at a life stage where experiences of adolescent manifestations of self-harm and disordered eating had not begun. Intervention prospects in psychological therapy at younger ages for BID to mitigate disordered eating and self-harm in adolescence may additionally be more successful than those conducted in older age groups since the sense of self is still developing and undergoing significant change.
There are, however, limitations to this study. A consequence of the aforementioned strength is that this study is not likely to be generalisable to adult populations where behaviours have already been well-established. Exploration of these experiences in older populations is an important research area and should be independently explored. Disordered eating and self-harm in older adults have distinct characteristics and are associated with a high level of morbidity and mortality [69, 70]. Second, we used an imputed dataset under the assumption that data are missing at random, which, if incorrect, could lead to biased results. However, provided the outcome is unrelated to model missingness, it does not matter whether independent variables are missing not at random [71]. Third, in the ALSPAC sample it is not possible to determine if participants self-defined their disordered eating as self-harm in response to questions on self-harm. Fourth, enrolled ALSPAC participants are from the Southwest of England, more likely to be white, and ineligible for free school meals compared to the National Pupil Database (NPD) ‘Key Stage 4’ (KS4) sample [33]. The results obtained from this study may therefore not be generalisable to other communities in the United Kingdom or indeed globally. Moreover, since allele frequencies, risk factors, and diseases differ between ancestry subgroups, confounding may occur [72]. We have therefore conducted analyses in homogeneous populations of European ancestry and only depict effects within this single ancestry group. Fifth, genetic instruments for childhood body size were derived using recall data and may be more liable to bias. Earlier simulations and validation studies, however, have shown these instruments to effectively separate the effect of childhood body size from adulthood body size [31, 35, 36]. Lastly, due to sample size limitations, the GWAS evaluating BID contained SNPs that did not reach genome-wide significance. However, we were able to run MR-RAPS as the principal MR method. There is potential that the effect estimates for BID on body size may be impacted by weak instrument bias. This would bias the estimates towards the null since the context is a two-sample MR setting (with non-overlapping samples) [73].
Future research in this field would benefit from exploring effects in different age groups to provide more detail on how BID evolves over the lifecourse and how this interacts with disordered eating and self-harm at later stages in life. In addition, whilst novel MR methods are available to perform lifecourse research [74], the current limitation lies in the absence of adequately large datasets containing age-specific information with corresponding genetic data. These data would have the potential to greatly enhance our understanding of this research area.
Conclusions
This novel application of MR in a counterfactual mediation setting shows a causal effect of prepubertal body size on BID. It additionally suggests distinct risk profiles for disordered eating and self-harm in relation to weight and provides more detail on how risk in early life fosters both disordered eating and self-harm in adolescence. This has important public health implications. A better understanding of the mediating role of genetically predicted prepubertal BID in this context may be useful in the prevention and treatment of disordered eating and self-harm in adolescence.
Data availability
All individual-level data analysed in this study can be accessed via an approved application to ALSPAC (http://www.bristol.ac.uk/alspac/researchers/access/). Summary statistics on prepubertal body size are publicly available from the studies as referenced [31].
References
Treasure J, Duarte TA, Schmidt U. Eating disorders. Lancet. 2020;395:899–911.
Warne N, Heron J, Mars B, Moran P, Stewart A, Munafò M, et al. Comorbidity of self-harm and disordered eating in young people: Evidence from a UK population-based cohort. J Affect Disord. 2021;282:386–90.
Crow S, Eisenberg ME, Story M, Neumark-Sztainer D. Are body dissatisfaction, eating disturbance, and body mass index predictors of suicidal behavior in adolescents? A longitudinal study. J Consult Clin Psychol. 2008;76:887–92.
Brausch AM, Perkins NM. Nonsuicidal self-injury and disordered eating: differences in acquired capability and suicide attempt severity. Psychiatry Res. 2018;266:72–8.
Svirko E, Hawton K. Self-injurious behavior and eating disorders: the extent and nature of the association. Suicide Life Threat Behav. 2007;37:409–21.
Krug I, Arroyo MD, Giles S, Dang AB, Kiropoulos L, De Paoli T, et al. A new integrative model for the co-occurrence of non-suicidal self-injury behaviours and eating disorder symptoms. J Eat Disord. 2021;9:153.
Wright F, Bewick BM, Barkham M, House AO, Hill AJ. Co-occurrence of self-reported disordered eating and self-harm in UK university students. Br J Clin Psychol. 2009;48:397–410.
Warne N, Heron J, Mars B, Solmi F, Biddle L, Gunnell D, et al. Emotional dysregulation in childhood and disordered eating and self-harm in adolescence: prospective associations and mediating pathways. J Child Psychol Psychiatry. 2023;64:797–806.
Murray CD, Macdonald S, Fox J. Body satisfaction, eating disorders and suicide ideation in an Internet sample of self-harmers reporting and not reporting childhood sexual abuse. Psychol Health Med. 2008;13:29–42.
Satghare P, Mahesh MV, Abdin E, Chong SA, Subramaniam M. The relative associations of body image dissatisfaction among psychiatric out-patients in Singapore. Int J Environ Res Public Health. 2019;16:5162.
Xu X, Mellor D, Kiehne M, Ricciardelli LA, McCabe MP, Xu Y. Body dissatisfaction, engagement in body change behaviors and sociocultural influences on body image among Chinese adolescents. Body Image. 2010;7:156–64.
Stice E, Shaw HE. Role of body dissatisfaction in the onset and maintenance of eating pathology: A synthesis of research findings. J Psychosom Res. 2002;53:985–93.
Brechan I, Kvalem IL. Relationship between body dissatisfaction and disordered eating: mediating role of self-esteem and depression. Eat Behav. 2015;17:49–58.
Bornioli A, Lewis-Smith H, Smith A, Slater A, Bray I. Adolescent body dissatisfaction and disordered eating: Predictors of later risky health behaviours. Soc Sci Med. 2019;238:112458.
Farrell C, Shafran R, Lee M. Empirically evaluated treatments for body image disturbance: a review. Eur Eat Disord Rev. 2006;14:289–300.
Cash TF, Hicks KL. Being fat versus thinking fat: relationships with body image, eating behaviors, and well-being. Cogn Ther Res. 1990;14:327–41.
O’Dea JA. Evidence for a self-esteem approach in the prevention of body image and eating problems among children and adolescents. Eat Disord. 2004;12:225–39.
Grabe S, Ward LM, Hyde JS. The role of the media in body image concerns among women: a meta-analysis of experimental and correlational studies. Psychol Bull. 2008;134:460.
Irving LM, Berel SR. Comparison of media‐literacy programs to strengthen college women’s resistance to media images. Psychol Women Q. 2001;25:103–11.
Cash TF, Smolak L. Body image: a handbook of science, practice, and prevention. New York, NY: Guilford Press; 2011.
Keery H, Shroff H, Thompson JK, Wertheim E, Smolak L. The sociocultural internalization of appearance questionnaire - adolescents (SIAQ-A): psychometric analysis and normative data for three countries. Eat Weight Disord. 2004;9:56–61.
Wardle J, Cooke L. The impact of obesity on psychological well-being. Best Pract Res Clin Endocrinol Metab. 2005;19:421–40.
Stice E, Van Ryzin MJ. A prospective test of the temporal sequencing of risk factor emergence in the dual pathway model of eating disorders. J Abnorm Psychol. 2019;128:119–28.
Presnell K, Bearman SK, Stice E. Risk factors for body dissatisfaction in adolescent boys and girls: a prospective study. Int J Eat Disord. 2004;36:389–401.
Labre MP. Adolescent boys and the muscular male body ideal. J Adolesc Health. 2002;30:233–42.
Austin SB, Haines J, Veugelers PJ. Body satisfaction and body weight: gender differences and sociodemographic determinants. BMC Public Health. 2009;9:313.
Orbach S. Hunger strike: the anorectic’s struggle as a metaphor for our age. New York, NY: Taylor & Francis; 2018.
Davey Smith G, Ebrahim S. Mendelian randomization’: can genetic epidemiology contribute to understanding environmental determinants of disease? Int J Epidemiol. 2003;32:1–22.
Richmond RC, Davey Smith G. Mendelian randomization: concepts and scope. Cold Spring Harb Perspect Med. 2021;12:a040501.
Howe LJ, Trela-Larsen L, Taylor M, Heron J, Munafò MR, Taylor AE. Body mass index, body dissatisfaction and adolescent smoking initiation. Drug Alcohol Depend. 2017;178:143–9.
Richardson TG, Sanderson E, Elsworth B, Tilling K, Davey Smith G. Use of genetic variation to separate the effects of early and later life adiposity on disease risk: mendelian randomisation study. BMJ. 2020;369:m1203–m.
Bycroft C, Freeman C, Petkova D, Band G, Elliott LT, Sharp K, et al. The UK Biobank resource with deep phenotyping and genomic data. Nature. 2018;562:203–9.
Boyd A, Golding J, Macleod J, Lawlor DA, Fraser A, Henderson J, et al. Cohort profile: the ‘children of the 90s’–the index offspring of the Avon Longitudinal Study of Parents and Children. Int J Epidemiol. 2013;42:111–27.
Fraser A, Macdonald-Wallis C, Tilling K, Boyd A, Golding J, Davey Smith G, et al. Cohort profile: the Avon Longitudinal Study of Parents and Children: ALSPAC mothers cohort. Int J Epidemiol. 2013;42:97–110.
Brandkvist M, Bjørngaard JH, Ødegård RA, Åsvold BO, Davey Smith G, Brumpton B, et al. Separating the genetics of childhood and adult obesity: a validation study of genetic scores for body mass index in adolescence and adulthood in the HUNT Study. Hum Mol Genet. 2021;29:3966–73.
Richardson TG, Mykkänen J, Pahkala K, Ala-Korpela M, Bell JA, Taylor K, et al. Evaluating the direct effects of childhood adiposity on adult systemic metabolism: a multivariable Mendelian randomization analysis. Int J Epidemiol. 2021;50:1580–92.
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320:1240–3.
Cole TJ, Flegal KM, Nicholls D, Jackson AA. Body mass index cut offs to define thinness in children and adolescents: international survey. BMJ. 2007;335:194.
Stunkard A, Sorensen T, Schulsinger F. Use of the Danish Adoption Register for the study of obesity and thinness In: Kety SS, Rowland LP, Sidman RL, Matthysse SW, editors. The Genetics of Neurological and Psychiatric Disorders. New York: Raven Press; 1983.
Marchini J, Howie B, Myers S, McVean G, Donnelly P. A new multipoint method for genome-wide association studies by imputation of genotypes. Nat Genet. 2007;39:906–13.
Howie BN, Donnelly P, Marchini J. A flexible and accurate genotype imputation method for the next generation of genome-wide association studies. PLoS Genet. 2009;5:e1000529.
Howie B, Marchini J, Stephens M. Genotype imputation with thousands of genomes. G3. 2011;1:457–70.
Soumya Subhra P, Sarthok Rasique R, Kaustubh A. fastman: A fast algorithm for visualizing GWAS results using Manhattan and Q-Q plots. 2022. Available from: https://www.biorxiv.org/content/10.1101/2022.04.19.488738v1.
Chang CC, Chow CC, Tellier LC, Vattikuti S, Purcell SM, Lee JJ. Second-generation PLINK: rising to the challenge of larger and richer datasets. Gigascience. 2015;4:7.
Abecasis GR, Auton A, Brooks LD, DePristo MA, Durbin RM, Handsaker RE, et al. An integrated map of genetic variation from 1,092 human genomes. Nature. 2012;491:56–65.
Darrous L, Mounier N, Kutalik Z. Simultaneous estimation of bi-directional causal effects and heritable confounding from GWAS summary statistics. Nat Commun. 2021;12:7274.
Qingyuan Z, Jingshu W, Gibran H, Jack B, Dylan SS. Statistical inference in two-sample summary-data Mendelian randomization using robust adjusted profile score. Ann Stat. 2020;48:1742–69.
Zhao Q, Chen Y, Wang J, Small DS. Powerful three-sample genome-wide design and robust statistical inference in summary-data Mendelian randomization. Int J Epidemiol. 2019;48:1478–92.
Burgess S, Butterworth A, Thompson SG. Mendelian randomization analysis with multiple genetic variants using summarized data. Genet Epidemiol. 2013;37:658–65.
Bowden J, Davey Smith G, Burgess S. Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int J Epidemiol. 2015;44:512–25.
Hemani G, Zheng J, Elsworth B, Wade KH, Baird D, Haberland V et al. The MR-Base Collaboration. The MR-Base platform supports systematic causal inference across the human phenome. eLife 2018;7:e34408.
Turner SD. qqman: an R package for visualizing GWAS results using Q-Q and manhattan plots. J Open Source Softw. 2018;3:731.
van Buuren S. Multiple imputation of discrete and continuous data by fully conditional specification. Stat Methods Med Res. 2007;16:219–42.
Daniel RM, De Stavola BL, Cousens SN. gformula: estimating causal effects in the presence of time-varying confounding or mediation using the g-computation formula. Stata J. 2011;11:479+.
De Stavola BL, Daniel RM, Ploubidis GB, Micali N. Mediation analysis with intermediate confounding: structural equation modeling viewed through the causal inference lens. Am J Epidemiol. 2015;181:64–80.
Valeri L, Vanderweele TJ. Mediation analysis allowing for exposure-mediator interactions and causal interpretation: theoretical assumptions and implementation with SAS and SPSS macros. Psychol Methods. 2013;18:137–50.
Support ST StataCorp. 2019. Stata Statistical Software: Release 16. College Station, TX: StataCorp LLC. 2019.
Carter AR, Sanderson E, Hammerton G, Richmond RC, Davey Smith G, Heron J, et al. Mendelian randomisation for mediation analysis: current methods and challenges for implementation. Eur J Epidemiol. 2021;36:465–78.
Perera S, Eisen RB, Dennis BB, Bawor M, Bhatt M, Bhatnagar N, et al. Body mass index is an important predictor for suicide: results from a systematic review and meta-analysis. Suicide Life Threat Behav. 2016;46:697–736.
Nyberg J, Gustavsson S, Åberg MAI, Kuhn HG, Waern M. Late-adolescent risk factors for suicide and self-harm in middle-aged men: explorative prospective population-based study. Br J Psychiatry. 2020;217:370–6.
Branco JC, Motta J, Wiener C, Oses JP, Pedrotti Moreira F, Spessato B. et al. Association between obesity and suicide in woman, but not in man: a population-based study of young adults. Psychol Health Med. 2017;22:275–81.
Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BW, et al. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010;67:220–9.
Stabouli S, Erdine S, Suurorg L, Jankauskienė A, Lurbe E. Obesity and eating disorders in children and adolescents: the bidirectional link. Nutrients. 2021;13:4321.
Goldschmidt AB, Aspen VP, Sinton MM, Tanofsky-Kraff M, Wilfley DE. Disordered eating attitudes and behaviors in overweight youth. Obesity. 2008;16:257–64.
McCuen-Wurst C, Ruggieri M, Allison KC. Disordered eating and obesity: associations between binge-eating disorder, night-eating syndrome, and weight-related comorbidities. Ann N Y Acad Sci. 2018;1411:96–105.
Stice E, Presnell K, Shaw H, Rohde P. Psychological and behavioral risk factors for obesity onset in adolescent girls: a prospective study. J Consult Clin Psychol. 2005;73:195–202.
Schwartz MB, Brownell KD. Obesity and body image. Body Image. 2004;1:43–56.
Pope HG Jr, Olivardia R, Gruber A, Borowiecki J. Evolving ideals of male body image as seen through action toys. Int J Eat Disord. 1999;26:65–72.
Troya MI, Babatunde O, Polidano K, Bartlam B, McCloskey E, Dikomitis L, et al. Self-harm in older adults: systematic review. Br J Psychiatry. 2019;214:186–200.
Mulchandani M, Shetty N, Conrad A, Muir P, Mah B. Treatment of eating disorders in older people: a systematic review. Syst Rev. 2021;10:275.
Hughes RA, Heron J, Sterne JAC, Tilling K. Accounting for missing data in statistical analyses: multiple imputation is not always the answer. Int J Epidemiol. 2019;48:1294–304.
Sekula P, Del Greco MF, Pattaro C, Köttgen A. Mendelian randomization as an approach to assess causality using observational data. J Am Soc Nephrol. 2016;27:3253–65.
Zheng J, Baird D, Borges MC, Bowden J, Hemani G, Haycock P, et al. Recent developments in Mendelian randomization studies. Curr Epidemiol Rep. 2017;4:330–45.
Power GM, Sanderson E, Pagoni P, Fraser A, Morris T, Prince C et al. Methodological approaches, challenges, and opportunities in the application of Mendelian randomisation to lifecourse epidemiology: A systematic literature review. Eur J Epidemiol. 2024;39:501–20.
Acknowledgements
We are extremely grateful to all the families who took part in this study, the midwives for their help in recruiting them, and the whole ALSPAC team, which includes interviewers, computer and laboratory technicians, clerical workers, research scientists, volunteers, managers, receptionists, and nurses. We would like to thank the UK Biobank study and all participants who contributed to it, as well as the authors of the GWAS who made their summary statistics available for the benefit of this work. This research has been conducted using the UK Biobank Resource under Application Number 76538. We would also like to thank Professor Timothy M. Frayling for suggestions regarding the genetic components of this work.
Funding
The UK Medical Research Council and Wellcome (Grant ref: 217065/Z/19/Z) and the University of Bristol provide core support for ALSPAC. This publication is the work of the authors and Grace M. Power, Naomi Warne, Helen Bould, Francesco Casanova, Sam Jones, Tom G. Richardson, Jess Tyrrell, George Davey Smith, and Jon Heron will serve as guarantors for the contents of this paper. A comprehensive list of grants funding is available on the ALSPAC website (http://www.bristol.ac.uk/alspac/external/documents/grant-acknowledgements.pdf). GWAS data was generated by Sample Logistics and Genotyping Facilities at Wellcome Sanger Institute and LabCorp (Laboratory Corporation of America) using support from 23andMe. This work was in part supported by the Integrative Epidemiology Unit which receives funding from the UK Medical Research Council and the University of Bristol (MC_UU_00032/01 and MC_UU_00032/02). GDS conducts research at the NIHR Biomedical Research Centre at the University Hospitals Bristol NHS Foundation Trust and the University of Bristol. The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health. GMP is supported by the GW4 Biomed Doctoral Training Programme, awarded to the Universities of Bath, Bristol, Cardiff, and Exeter from the Medical Research Council (MRC)/UKRI (MR/N0137941/1). NW is supported by a fellowship awarded by The Prudence Trust. FC and JT are supported by an Academy of Medical Sciences (AMS) Springboard award, which is supported by the AMS, the Wellcome Trust, GCRF, the Government Department of Business, Energy and Industrial strategy, the British Heart Foundation and Diabetes UK [SBF004\1079]. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
GDS conceptualised the initial study design. GMP carried out data curation and formal analyses. GMP and JH designed the methodological approach. FC, SEJ, and JT helped with the methodological direction. Body size summary genetic data were obtained through a study led by TGR. GMP prepared the original draft. All authors (GMP, NW, HB, FC, SEJ, TGR, JT, JH, and GDS) contributed to the interpretation of the results and critical revision of the manuscript. This work was jointly supervised GDS and JH.
Corresponding author
Ethics declarations
Competing interests
TGR is an employee of GlaxoSmithKline outside of this research. All other authors declare no competing interests.
Ethics approval and consent to participate
The UK Biobank study have obtained ethics approval from the Research Ethics Committee (REC; approval number: 11/NW/0382) and informed consent from all participants enrolled in UK Biobank. Estimates were derived using data from the UK Biobank (app #76538). Ethical approval for the study was obtained from the ALSPAC ethics and law committee and the local research ethics committees. Informed consent for the use of data collected via questionnaires and clinics was obtained from participants following the recommendations of the ALSPAC Ethics and Law Committee at the time.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Power, G.M., Warne, N., Bould, H. et al. The role of body image dissatisfaction in the relationship between body size and disordered eating and self-harm: complimentary Mendelian randomization and mediation analyses. Mol Psychiatry 30, 521–531 (2025). https://doi.org/10.1038/s41380-024-02676-5
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41380-024-02676-5
This article is cited by
-
Weight discrimination and eating disorder symptoms in early adolescence: a prospective cohort study
Journal of Eating Disorders (2025)