Abstractl
Background/Objectives
Studies have shown widespread alterations in different components of the cholinergic system in schizophrenia, but to date the evidence has not been systematically reviewed and summarized. Here, we systematically review imaging and post-mortem studies on the central cholinergic system in schizophrenia/schizoaffective disorder.
Subjects/Methods
Searches were performed in Embase and Medline. Study designs included cross-sectional case control studies comparing individuals with schizophrenia/schizoaffective disorder to control population. Risk of bias was assessed with the NIH/NHLBI tool for Quality Assessment of Case-Control Studies. The current study followed the PRISMA 2020 guidelines (PROSPERO: CRD42023402126).
Results
A total of 3259 studies were screened and 61 met eligibility criteria for the systematic review, including 8 in vivo neuroimaging and 53 post-mortem studies. About 74% of these studies described significant alterations, most often reductions in either muscarinic or nicotinic receptor levels in schizophrenia. We also conducted 3 meta-analyses showing reductions in M1/M4 muscarinic receptors in the striatum (g = −0.809, k = 3, n = 108), hippocampus (g = −0.872, k = 3, n = 84), and fronto-cingulate cortex (g = −0.438, k = 4, n = 295). Six neuroimaging studies reported associations with clinical symptom severity measures, and four investigations with cognitive dysfunction.
Conclusions
Our review demonstrates a widespread decrease in muscarinic and nicotinic receptor levels in schizophrenia, evident in both neuroimaging and post-mortem studies. Our meta-analyses show large to moderate effects for the reductions in M1/M4 muscarinic receptors in the striatum, hippocampus, and fronto-cingulate cortex. Limitations and future directions for the field are discussed.
Similar content being viewed by others
Introduction
Since the mid-20th century, researchers have hypothesized that the cholinergic system could be targeted for the treatment of schizophrenia [1]. Observations that anticholinergic drugs could produce psychotic symptoms further suggested that abnormal cholinergic function might underly the pathophysiology of schizophrenia [2, 3]. A growing body of literature using neuroimaging or post-mortem samples now shows changes in cholinergic neurotransmission in this disorder, and multiple cholinergic agents are being developed and tested for the treatment of schizophrenia [4,5,6,7,8,9].
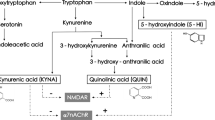
Cholinergic neurotransmission involves acetylcholine release and complex pre- and post-synaptic molecular apparatus (see Fig. 1). The cholinergic system is essential for synaptic plasticity, modulation of excitation-inhibition balance and oscillations, as well as the coordination of functional networks [10, 11]. This system modulates a wide variety of neurobehavioral functions from sensory processing and perception to cognition, memory, emotional regulation, and motivation [12,13,14,15,16]. Since disruptions of these functions are thought to manifest as symptoms of schizophrenia, abnormal cholinergic signaling may partly underly the clinical presentation of schizophrenia [17,18,19,20,21]. Moreover, the cholinergic system modulates dopamine release in the striatum, where the cholinergic receptors are localized on most GABAergic interneurons as well as dopamine and glutamate terminals [22,23,24,25,26]. Specifically, activation of the M1 and M4 receptors dampens striatal dopamine release whereas the activity of various nicotinic receptor subtypes facilitate dopamine release in this brain region [27,28,29]. Consequently, some of the effects of abnormal cholinergic signaling in schizophrenia may be mediated via modulation of dopamine release [18,19,20].
Acetylcholine is synthesized from choline and acetyl-coA by choline acetyltransferase, packed into vesicles by a vesicular acetylcholine transporter, and, after release, broken down by acetylcholinesterase. The effects of released acetylcholine are conveyed by nicotinic ligand-gated ion channels and muscarinic metabotropic (G-protein coupled) receptors. There are 5 muscarinic receptor subtypes: M1–M5. Muscarinic M2 receptors can act as pre-synaptic auto-receptors on cholinergic neurons, while the other subtypes act mainly as heteroreceptors on other cholinoceptive neuronal types (both pre- and post-synaptically). Nicotinic receptor subunits include α3, α4, α5, α6, α7, β2, and β4. The most common nicotinic receptors in the brain are the heteromeric α4β2 and the penta-homomeric α7 receptors, which are located both on cholinergic and cholinoceptive neurons (e.g., pre- and post-synaptically on dopamine neurons). Cortical and hippocampal innervation is primarily provided by projections from the basal forebrain and brainstem cholinergic nuclei, while the majority of acetylcholine release in the striatum is accounted for by cholinergic interneurons. Some evidence suggests that cholinergic neurotransmission also occurs by slow volume transmission across extracellular space, in addition to the classical synaptic transmission. Image created in BioRender.com.
In addition to post-mortem and imaging studies, the involvement of the cholinergic system in schizophrenia is also supported by pharmacological studies. Anticholinergic agents can induce psychotic-like experiences and cognitive deficits in healthy controls [30]. In schizophrenia, anticholinergic activity can exacerbate psychotic symptoms as well as worsen cognitive, brain structural, and functional impairments [30,31,32]. Most prominently, many recent clinical trials of cholinergic agents have shown promising results in the treatment of this disorder [8, 9]. Specifically, the brain-penetrant muscarinic (M1/M4) agonist xanomeline (combined with the peripheral blocker trospium) has demonstrated efficacy in improving positive, negative, and cognitive symptoms of schizophrenia [8, 33, 34]. These pharmacological findings lend additional credibility for the postulated cholinergic involvement in this mental health disorder.
Given recent developments in cholinergic therapeutic agents and increased interest in this system in schizophrenia, it is important to systematically summarize the existing evidence for the involvement of the cholinergic system in the pathophysiology of schizophrenia. Changes in the cholinergic system in schizophrenia have been studied in post-mortem samples as well as in vivo using positron emission tomography (PET) and single photon emission computed tomography (SPECT) [4, 5, 35]. There are multiple narrative reviews describing cholinergic alterations in schizophrenia [33, 36,37,38]. However, the human experimental data on the topic has never been systematically reviewed. Therefore, we conducted a systematic review (and meta-analyses when feasible) to identify, summarize, and combine the broad literature quantifying neuronal cholinergic alterations in the brain of individuals with schizophrenia.
Methods
To better understand the potential alterations associated with schizophrenia, we systematically reviewed the human empirical data on the brain cholinergic system in this disorder relative to controls. The systematic review process used in the current protocol follows the PRISMA 2020 guidelines (see supplementary material) and was registered in PROSPERO in March 2023 (https://www.crd.york.ac.uk/prospero/display_record.php?ID = CRD42023402126) [39].
Search strategy
Systematic searches were performed in Ovid Embase and Medline (see Supplementary Table S1 for example of Ovid Embase search strategy; last search: June 2024).
Inclusion and exclusion criteria
Sources needed to include original, peer-reviewed data where direct experimental measures of the cholinergic system in the human brain (e.g., cholinergic receptors, transporters, enzymes (protein or mRNA expression levels), or neuronal counts) were compared between a sample of persons with schizophrenia or schizoaffective disorder and a control sample. The diagnosis of schizophrenia or schizoaffective disorder needed to be confirmed using a validated diagnostic assessment tool that adheres to either the Diagnostic and Statistical Manual of Mental Disorders’ (DSM-III or higher; American Psychiatric Association) or the International Classification of Diseases’ (ICD-9 or higher; World Health Organization) diagnostic criteria. Included study designs encompassed cross-sectional, case control, and cohort studies (with control groups). Control trials studies were only eligible if they reported baseline measures of cholinergic markers in comparison to a control group. Sources were limited to the English language. Sources were ineligible if they included purely DNA sequencing without measuring cholinergic expression markers; measured the cholinergic system outside of the brain (e.g., blood cells) or in non-neuronal cells; or utilized animal models. Reviews, meta-analyses, and conference presentations were not eligible.
Data extraction
All collected sources were uploaded into Covidence (https://www.covidence.org), an online software that facilitates the systematic review process. Two members of the research team reviewed and screened the titles and abstracts of the collected sources according to the predefined inclusion and exclusion criteria (ZS & RH). The remaining sources underwent full-text review/screening by two members according to the predefined criteria (ZS & JM). Data on general study characteristics, methodology, sample composition, and relevant quantitative results were extracted from the included sources and recorded in a customized data extraction spreadsheet independently by two of three members of the team (ZS, RA & JM). At each step, disagreements of relevant data were resolved through discussion by two members of the research team, until consensus was reached.
Risk of bias assessment
The quality of eligible sources was determined using the NIH/NHLBI tools for Quality Assessment of Case-Control Studies (https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools). Two reviewers independently assessed the quality of each included source (ZS, RA, JM). Disagreements were resolved through discussion, until consensus was reached.
Data synthesis
We performed a narrative synthesis of the findings. General data synthesis described the following characteristics: study characteristics (i.e., author names, year, study type), smoking status, medications, sample/group characteristics (i.e., specific diagnosis, sample size, demographics), component of the cholinergic system quantified (including relevant methodological information, such as ligand/probe, etc.), and study results (i.e., between-group differences in cholinergic system components). Results were tabulated according to these measures.
We also stratified the results according to the study type, methodology, cholinergic components assessed (e.g., receptors, transporters, enzymes, mRNA expression, and neuronal counts) and the brain regions assessed. We reported findings narratively and conducted a meta-analysis when ≥ 3 studies showing effect sizes per methodological assay/measure were available for a given brain region.
Meta-analytical statistics
When 3 or more studies using the same cholinergic probe/assay in the same brain region were identified, meta-analyses were performed using the metafor package in R with random effect modeling, unbiased estimator, and Hedge’s g statistics, which is more robust with small sample sizes [40]. R code is available upon request. The Q-Statistic was used to test heterogeneity and publication bias was visually evaluated with funnel plots.
Results
A total of 61 studies met eligibility criteria for the current systematic review, including eight in vivo neuroimaging studies and 53 post-mortem investigations (see Supplementary Fig. S1 for PRISMA diagram). Of the total 61 included investigations, 45 showed alterations in the cholinergic system in schizophrenia (see Table 1 for details).
In vivo neuroimaging studies
There are eight neuroimaging studies on the cholinergic system in schizophrenia: one study used [123I]IQNB, a non-selective muscarinic receptor antagonist; two studies used [123I]5-IA-85380, a nicotinic β2* agonist; three studies used [18F]-ASEM, a nicotinic α7 receptor antagonist; one study used 2-[18F]FA, an α4β2 agonist; and one study used [18F]VAT, a vesicular acetylcholine transporter inhibitor [4, 7, 35, 41,42,43,44,45]. See Fig. 2a for a visual summary of neuroimaging findings in schizophrenia.
Each panel displays a visual summary in the form of brain maps with corresponding tables, highlighting the main findings from the systematic review [55, 56]. Panel a) shows in vivo neuroimaging evidence. Panels b) and d) display findings on post-mortem muscarinic receptors and mRNA, respectively. Panel c) highlights findings on post-mortem nicotinic receptors as well as mRNA. k = #: # of studies represented in the panel. ↑ Higher in schizophrenia relative to controls, ↓ Lower in schizophrenia relative to controls, ~ No group difference, 6–46 Brodmann Areas #, FC Frontal Cortex, PC Parietal Cortex, CC Cingulate Cortex, ACC Anterior Cingulate Cortex, PCC Posterior Cingulate Cortex, TC Temporal cortex, STG Superior Temporal Gyrus, OC Occipital Cortex, Cau Caudate, Put Putamen, Str Striatum (caudate/putamen), Tha Thalamus, Hip Hippocampus, Ms Muscarinic receptors (combined subtypes), M# Muscarinic receptor subtype #, Ns Nicotinic receptors (combined subtypes), α# α nicotinic receptor subunit/subtype #, β2 β2 nicotinic receptor subunits, vAChT Vesicular Acetylcholine Transporters. *Confounds, including a large smoking and age mismatch between groups, render findings inconclusive.
Six of the seven studies on muscarinic or nicotinic receptors (density or availability thereof) found reductions in schizophrenia relative to controls [4, 7, 35, 43,44,45]. One study compared older patients with schizophrenia who smoked to younger healthy controls who mostly did not smoke, thus not allowing to conclude on effect of illness [42]. The report on vesicular acetylcholine transporters did not find evidence for a group difference [41]. The small number of in vivo studies, their use of a variety of radioligands, regions-of-interest, or shared participants (follow-up reports of the same study) precluded us from conducting a meta-analysis for the neuroimaging investigations.
Associations with symptoms of schizophrenia
Six neuroimaging studies also reported significant associations between lower cholinergic receptor levels and more severe clinical or cognitive symptoms, while one of the investigations on receptors did not report this type of analysis [4, 7, 35, 42,43,44,45]. Higher levels of positive symptoms were associated with lower levels of muscarinic receptors in the frontal cortex as well as caudate/putamen [4]. Similarly, higher levels of positive symptoms correlated with lower levels of α7 nicotinic receptor in widespread cortical and subcortical regions in individuals with recent-onset psychosis (schizophrenia spectrum and bipolar I disorder) [43]. A negative correlation was also found between negative symptoms and β2* nicotinic receptor availability in the striatum, frontal, and parietal cortex [7]. Additionally, a negative correlation was shown between β2* nicotinic receptor availability in frontal and parietal cortices and cognitive deficits in smokers with schizophrenia [7]. Similarly, α7 nicotinic receptor availability negatively correlated with cognitive deficits in the temporal, occipital and cingulate cortices as well as the striatum and hippocampus, in recent-onset psychosis [35, 43]. Lastly, the study assessing vesicular acetylcholine transporters, although not showing group differences, found higher transporter levels in many brain cortical and subcortical regions to correlate with higher positive symptoms and with lower cognitive ability in individuals with schizophrenia [41].
Post-mortem studies
Constituents of the cholinergic system in post-mortem samples have been quantified using autoradiography, in situ hybridization, Western blots, enzyme assays, and PCR [5, 46,47,48,49]. Of the 53 eligible post-mortem studies, 30 measured muscarinic receptor proteins, mRNA, or the coupling of receptors with intracellular targets; 17 assessed nicotinic receptor protein and/or mRNA; five reported directly on neuronal cholinergic/cholinoceptive populations; and four investigated cholinergic enzymes. Notably, three studies assessed cholinergic receptors along with either enzymes or neuronal populations. M1/M4 receptors were the most widely studied target using [3H]pirenzepine. Other commonly studied targets were the nicotinic α7 and muscarinic M2/M4 receptors, using [125I]α-bungarotoxin and [3H]AF-DX 384, respectively. In terms of brain regions, a majority of studies have focused on the frontal and cingulate cortices, striatum, and hippocampus.
Muscarinic receptors
A total of 30 studies investigated muscarinic receptor expression, protein, or coupling measures. Twenty reported decreases in the post-mortem brain in schizophrenia compared to controls, whereas three investigations showed bidirectional changes, only two evidenced an increase, and five studies found no group differences. Figure 2b and d provide visual representations of muscarinic receptor and mRNA findings, respectively. The most used cholinergic probe in post-mortem schizophrenia literature is [3H]pirenzepine, a pseudo-selective muscarinic antagonist. This tracer has the highest affinity for the muscarinic M1 receptor, followed by the muscarinic M4 receptor [50]. In post-mortem human cortex, where the ratio of M1 to M4 receptors is also relatively higher, the majority of [3H]pirenzepine binding is attributable to M1 receptors (≳80%) [38, 51]. Whereas M4 receptors are relatively more abundant in the striatum, resulting in a more mixed [3H]pirenzepine signal to which both M1 and M4 receptor levels contribute [38, 52].
Meta-analytical findings
There was a sufficient number of independent investigations assessing [3H]pirenzepine binding in the striatum (k = 3, n = 108), hippocampus (k = 3, n = 84), and the fronto-cingulate cortex (k = 4, n = 295) to conduct meta-analyses. Random effect models yielded large effect sizes in the striatum (g = −0.809 [CI: −1.492, −0.125], p < 0.05) and the hippocampus (g = −0.872 [CI: −1.326, −0.418], p < 0.001), and a medium effect size in the fronto-cingulate cortex (g = −0.438 [CI: −0.670, −0.206], p < 0.001), in schizophrenia relative to controls. See Fig. 3 for forest plots and effect size contributions.
Forest plots of Random Effect (RE) meta-analyses of [3H]pirenzepine binding assays, representing M1/M4 receptor density, in the post-mortem (a) striatum, (b) hippocampus, and (c) fronto-cingulate cortex of individuals with schizophrenia relative to controls. Percent contribution to pooled effect size (Hedge’s g) shown as a square. Whiskers show confidence intervals (95%). For the meta-analysis in fronto-cingulate cortex (c), Zavitsanou and colleagues (2004) assessed anterior cingulate region and the other three studies assessed Brodmann Area 9.
Due to the low number of studies included in each meta-analysis (k = 3–4), publication bias was only assessed visually with funnel plots. The funnel plots from our meta-analyses did not highlight significant asymmetry beyond what could be expected from the random distribution of three unbiased publications (see Supplementary Fig. S2). Furthermore, no significant heterogeneity in effect sizes across studies included were found, suggesting the investigations are assessing the same underlying effect and variations in effect sizes could be attributed to sampling error rather than differences in study populations (striatum: Q(df = 2) = 4.67 (p = 0.10); hippocampus: Q(df = 2) = 2.00 (p = 0.37); and fronto-cingulate cortex: Q(df = 3) = 0.92 (p = 0.82)).
Nicotinic receptors
There were 17 studies on nicotinic receptors, and 12 of them found changes in schizophrenia. Changes in nicotinic receptor subtypes in post-mortem schizophrenia samples were less unidirectional than those of muscarinic receptors, with certain subtypes downregulated in a region but upregulated in another (see Table 1). For instance, α4β2 receptor levels may be decreased in the hippocampus, whereas the same receptor may be increased in the cingulate cortex [53, 54]. See Fig. 2c for a visual summary of nicotinic receptor and mRNA findings in schizophrenia [55, 56].
Cholinergic enzymes and neurons
Four studies investigated cholinergic enzymes (e.g., choline acetyltransferase and acetylcholinesterase) in the post-mortem brain of individuals with schizophrenia [48, 57,58,59]. Only one study reported increased choline acetyltransferase in the occipital cortex and angular gyrus of patients with schizophrenia relative to controls [57]. The remaining three studies did not find group differences.
Four of the five eligible histological studies found reductions in cholinergic or cholinoceptive neuron/cell populations in schizophrenia relative to controls, in the striatum and specific subregions of frontal and occipital cortices [47, 48, 58, 59].
Risk of bias
The majority of studies included in our review were rated as fair in design quality and risk of bias assessments (see Supplementary Table S2) because they did not statistically control for potential confounds (e.g., smoking, medications) in their analyses. Many also did not include sample size justification or power analysis. This may reflect the inherent limitations of the field that we reviewed. Sample sizes in post-mortem and nuclear imaging studies are often limited by feasibility, which in turn, limits the statistical power to account for confounds.
Discussion
Cholinergic alterations in schizophrenia
We systematically reviewed and conducted meta-analyses to summarize the evidence of alterations to the cholinergic system in the brain of individuals with schizophrenia. Our findings establish that multiple components of the cholinergic system across several cortical and subcortical brain regions are affected in schizophrenia. Evidence from in vivo neuroimaging studies demonstrate significant regional decreases in cholinergic receptor availabilities (i.e., muscarinic receptors as well as nicotinic α7 and β2* receptors). Likewise, the majority of reported changes in post-mortem schizophrenia samples are decreases in markers of the cholinergic system, with few exceptions.
The most studied regions in post-mortem studies were the striatum, hippocampus, as well as the frontal and cingulate cortices. We conducted meta-analyses of M1/M4 muscarinic receptor densities in these regions and found a significant decrease with large effect sizes in the striatum (g = −0.809) and hippocampus (g = −0.872), as well as a medium effect size in the fronto-cingulate cortex (g = −0.438). Importantly, the small number of studies included in each meta-analysis (k = 3–4) is a limitation and warrants further research. These findings remain of particular interest considering the efficacy of agents targeting muscarinic receptors in reducing symptoms of schizophrenia [8, 9, 60]. Both xanomeline (M1/M4 agonist) and emraclidine (M4 positive allosteric modulator) have shown significant therapeutic effects in human clinical trials [8, 9]. Furthermore, it is noteworthy to mention that many studies included in this review used pseudo-selective probes and assays [51, 53, 61, 62]. Specifically, our meta-analyses rely on [3H]pirenzepine binding assays that do not allow complete separation of signal from M1 and M4 receptors [61, 63]. Regarding our findings in the fronto-cingulate cortex, other lines of evidence suggest that only M1 levels would be altered. In Brodmann Area 9, one of the regions included in that meta-analysis, Western Blots and PCR experiments have shown a decrease in M1 receptors and mRNA, but unchanged M4 receptor levels [5]. As for the findings in the striatum and hippocampus, lower [3H]pirenzepine binding could reflect lower M4 levels because M1 mRNA expression was found to be unchanged in those brain structures [63, 64]. Consistent with this, there is evidence that M4 mRNA levels are decreased in the hippocampus, whereas data on the striatum are lacking [64]. However, the attribution of [3H]pirenzepine signal remains speculative in those brain regions, since mRNA and protein levels do not always correspond [65]. In the future, it may be feasible to quantify individual muscarinic receptor subtypes in vivo with selective radiotracers [66, 67].
Cholinergic system and symptoms of schizophrenia
The cholinergic system is crucial to multiple neuronal circuits that support neurobehavioral functions affected in schizophrenia (e.g., cognitive processes, sensory processing, motivation, and emotional regulation) [12,13,14,15,16]. The majority of in vivo studies we identified in this review show a link between symptoms of schizophrenia and alterations in the cholinergic system. On one hand, greater positive symptom severity has been found to correlate with lower muscarinic receptors, lower α7 nicotinic, as well as increased vesicular acetylcholine transporters [4, 41, 43]. On the other hand, greater negative symptom severity has been associated with less β2* nicotinic receptors as well as lower M1 muscarinic receptors [7, 45, 68]. Additionally, greater cognitive deficits may correlate with lower α7 nicotinic and M1 muscarinic receptors [43, 44, 68]. Greater cognitive impairments may also correlate with lower choline acetyltransferase activity and increased vesicular acetylcholine transporters [41, 48]. Although these associations need to be replicated in larger samples, they lend credibility to the cholinergic involvement in the pathophysiology of schizophrenia. The implication of the cholinergic system in schizophrenia is further supported by clinical trials showing promising therapeutic effects of novel cholinergic agents [8, 9, 34].
Changes in striatal cholinergic system
The striatum has the densest cholinergic innervation and is a crucial site of cholinergic influence on neurobehavioral functions, such as learning, attention, decision-making, emotional regulation, and motivation [18, 41, 69,70,71]. Our meta-analytical post-mortem results emphasize a large decrease in M1/M4 muscarinic receptors in the striatum, suggesting a breakdown of cholinergic modulation in this region in schizophrenia. These two muscarinic receptor subtypes localize to multiple neuronal populations in the striatum, but most prominently post-synaptically on medium spiny neurons [72,73,74,75]. Both M1 and M4 are essential to the balanced control of dopaminergic neurotransmission in the striatum, which is associated with clinical symptom severity in schizophrenia [27, 28, 76,77,78]. Hence, it is not surprising that striatal muscarinic receptor availability is negatively correlated with positive symptoms [4]. Results are less consistent for nicotinic receptors in the striatum in schizophrenia. Some evidence suggests total nicotinic receptors may be increased in this region, while combined levels of β2* subunits may be unchanged, and α7/α4β2 receptor subtypes may be decreased [43, 79, 80]. Interestingly, lower α7 nicotinic receptor availability in the striatum is also associated with greater positive symptoms [43]. Studies of pre-synaptic markers of cholinergic innervation in the striatum have yielded opposing results and more research is required to conclude on whether it may be altered in schizophrenia [41, 46, 47, 81].
Alterations in the cholinergic system in the frontal and cingulate cortices
Our meta-analysis demonstrated significant reductions in muscarinic M1/M4 receptors in the fronto-cingulate cortex (combining data from Brodmann Area 9 and anterior cingulate) in schizophrenia. The frontal and cingulate cortices are essential to cognition, decision-making, social behavior, attention, and self-referential thought, whose function is disrupted in schizophrenia [82,83,84,85,86,87]. In the frontal cortex, there is evidence for a decrease in the number of cortical neurons displaying M1 receptors in schizophrenia relative to controls, and impaired M1 signaling correlates with cognitive deficits and negative symptoms in vivo in psychosis [68, 88]. Total muscarinic receptor availability in the frontal cortex also correlates with positive symptoms of schizophrenia [4]. Overall, alterations in muscarinic receptors in schizophrenia show a subtype-specific pattern with some, but not all, subtype-specific mRNA findings being concordant with receptor alterations [5, 6, 49, 89,90,91,92]. The nicotinic α7 receptors, which modulate excitatory neurotransmission, may be decreased in frontal and cingulate cortices, and lower α7 receptor availability may also be linked to greater positive symptom severity [43, 93]. Pre-synaptic markers of cholinergic innervation seem unchanged in the fronto-cingulate cortex in schizophrenia, but higher vesicular acetylcholine transporters in that region may be correlated with increased positive symptoms and poorer working memory performance [41, 58]. In summary, the literature shows region-specific muscarinic M1 and nicotinic α7 receptors abnormality in the fronto-cingulate cortex and associations with schizophrenia symptoms.
Cholinergic changes in the hippocampus
Our review indicates that specific components of the cholinergic system may also be altered in the hippocampus, specifically a large decrease in M1 and/or M4 receptors [54, 61, 64]. M1 receptors are primarily located on soma and dendrites of pyramidal and granule cells, where they potentiate NMDA and AMPA receptor signaling, and exert essential procognitive effects [94,95,96,97,98]. Research suggests that M4 muscarinic receptors localize to GABAergic interneurons and glutamatergic fibers in the hippocampus, modulate hippocampal circuits, and are vital to cognitive function [94, 99,100,101]. Thus, a breakdown of M1 or M4 signaling in schizophrenia may contribute to related cognitive impairments [102].
Total nicotinic receptors in the hippocampus may also be lower in schizophrenia [54]. Conversely, in vivo data suggest reductions in hippocampal α7 nicotinic receptors, which is supported by post-mortem mRNA changes [43, 103, 104]. The α7 is the most expressed nicotinic subtype in the hippocampus, localizing ubiquitously pre- and post-synaptically on interneurons, pyramidal cells and projection terminals [105]. α7 nicotinic receptors can enhance GABA and glutamate release and play a crucial role in cognitive functioning, with association with cognitive deficits in first-episode psychosis [43, 106]. Interestingly, nicotine use may have a differential effect on the expression of the α7 receptors in schizophrenia relative to controls, suggesting aberrant regulation in schizophrenia specifically [7, 103]. There is also evidence for lower surface availability of α7 receptors suggestive of altered assembly or trafficking in schizophrenia [103].
Similarly to the striatum, it is unclear whether pre-synaptic markers of cholinergic innervation in the hippocampus are altered in schizophrenia due to conflicting results [41, 81, 107]. Nonetheless, there is evidence that higher levels of hippocampal vesicular acetylcholine transporters are associated with poorer working memory performance and increased positive symptoms [41]. In sum, hippocampal cholinergic activity may be dysregulated in schizophrenia, and diverse cholinergic alterations are plausibly contributing to cognitive deficits and positive symptoms associated with the disorder.
Confounding factors, limitations, and future directions
Some limitations have been identified in the current literature about the cholinergic system in schizophrenia and future directions are suggested in this review (see Table 2). Although muscarinic M1/M4 receptors are the most studied components of the cholinergic system in schizophrenia, there is only one study that assessed their levels separately with Western Blots [5]. There is a lack of studies on pre-synaptic cholinergic function in schizophrenia in general, and even less investigations assessing how pre- and post-synaptic markers might be related. Only one study has investigated pre- and post-synaptic cholinergic markers in the same sample. That study found unchanged choline acetyltransferase in both patients with and without a deficits in M1/M4 receptors, suggesting that at least some part of the pre-synaptic cholinergic system is intact in patients with post-synaptic deficits [59]. In the future, systematic investigations including both pre- and post-synaptic markers should be conducted to assess whether one could be related to the other. This would also serve as a preliminary step in determining whether a primary cholinergic deficit might be driving the other cholinergic changes seen in schizophrenia. The difficulty in distinguishing illness from medication effects in the current literature is complicated by the cholinergic affinities of many antipsychotics (e.g., clozapine) and the use of anticholinergics to treat related pyramidal side effects. Many regional cholinergic alterations seem to be significant for individuals with schizophrenia regardless of their medication, while others may only be found in patients treated with benztropine, an anticholinergic medication [108]. Additionally, schizophrenia patients may be particularly vulnerable to the adverse cognitive effects of anticholinergic drugs, perhaps because of a primary cholinergic deficit in this illness [109]. This points to the importance of careful consideration when using anticholinergic medications in this disorder [110]. Furthermore, current knowledge highlights that smoking is a risk factor for schizophrenia and a predictor of relapse of psychotic episodes, but how smoking affects the cholinergic system in schizophrenia needs to be further explored [111,112,113,114]. This is of particular importance given the high prevalence of smoking in schizophrenia [115]. Findings regarding nicotinic receptors especially must be interpreted with caution because smoking status was not available in many of the included studies and some data suggest that nicotine may affect gene expression and upregulate certain nicotinic subtypes [103].
The potential cholinergic contribution in the pathogenesis of schizophrenia is supported by correlations between cholinergic markers and clinical symptoms, as well as cholinergic involvement in the neurobehavioral functions known to be impaired in schizophrenia [4, 17,18,19,20,21, 43]. However, current study designs do not allow to ascertain if cholinergic alterations could underly some of the other neuronal changes seen in schizophrenia, such as increased dopamine synthesis. There are very little data in early course psychosis, clinical high-risk, or in relatives of individuals with schizophrenia. It is also unclear whether cholinergic disruptions could drive symptoms only in a subgroup of individuals with schizophrenia [116].
Conclusion
To the best of our knowledge, the present study represents the first systematic review and meta-analyses of the broad literature of human brain studies on cholinergic alterations in schizophrenia. Widespread cholinergic alterations are reported, especially reductions in M1/M4 muscarinic receptors in the striatum, hippocampus, and fronto-cingulate cortex. In vivo studies also suggest reductions in cholinergic receptors and associations with symptom severity. Whether these cholinergic alterations are central to the pathophysiology of schizophrenia or are secondary to the effects of medications and/or smoking needs to be clarified by further research. Despite these limitations, current evidence strongly supports the continued development of cholinergic agents for treating schizophrenia symptoms, both as primary antipsychotic medications and as adjuvants aiming at reducing more specific symptom clusters, such as cognitive deficits. Future research should focus on disentangling illness, medication, and smoking effects as well as investigating the pre-synaptic and post-synaptic cholinergic system across different stages of illness. The continued development of more specific in vivo radioligands is also needed and could be used to identify or confirm potential cholinergic biomarkers or subgroups with particular cholinergic impairments. The current review highlights the cholinergic system as a plausible contributor to the pathophysiology of schizophrenia as well as a promising target for novel treatments.
References
Fulcher JH Jr, Gallagher WJ, Pfeiffer CC. Comparative lucid intervals after amobarbital, CO2, and arecoline in the chronic schizophrenic. Arch Neurol Psychiatry. 1957;78:392–5.
Tandon R, Mann NA, Eisner WH, Coppard N. Effect of anticholinergic medication on positive and negative symptoms in medication-free schizophrenic patients. Psychiatry Res. 1990;31:235–41.
Singh M, Kay SR. Therapeutic antagonism between anticholinergic antiparkinsonism agents and neuroleptics in schizophrenia. Neuropsychobiology. 1979;5:74–86.
Raedler TJ, Knable MB, Jones DW, Urbina RA, Gorey JG, Lee KS, et al. In vivo determination of muscarinic acetylcholine receptor availability in schizophrenia. Am J Psychiatry. 2003;160:118–27.
Dean B, McLeod M, Keriakous D, McKenzie J, Scarr E. Decreased muscarinic1 receptors in the dorsolateral prefrontal cortex of subjects with schizophrenia. Mol Psychiatry. 2002;7:1083–91.
Zavitsanou K, Katsifis A, Mattner F, Huang XF. Investigation of M1/M4 muscarinic receptors in the anterior cingulate cortex in schizophrenia, bipolar disorder, and major depression disorder. Neuropsychopharmacology. 2004;29:619–25.
Esterlis I, Ranganathan M, Bois F, Pittman B, Picciotto MR, Shearer L, et al. In vivo evidence for β2 nicotinic acetylcholine receptor subunit upregulation in smokers as compared with nonsmokers with schizophrenia. Biol Psychiatry. 2014;76:495–502.
Brannan SK, Sawchak S, Miller AC, Lieberman JA, Paul SM, Breier A. Muscarinic cholinergic receptor agonist and peripheral antagonist for schizophrenia. N Engl J Med. 2025;384:717–26.
Krystal JH, Kane JM, Correll CU, Walling DP, Leoni M, Duvvuri S, et al. Emraclidine, a novel positive allosteric modulator of cholinergic M4 receptors, for the treatment of schizophrenia: a two-part, randomised, double-blind, placebo-controlled, phase 1b trial. Lancet. 2022;400:2210–20.
Huerta PT, Lisman JE. Heightened synaptic plasticity of hippocampal CA1 neurons during a cholinergically induced rhythmic state. Nature. 1993;364:723–5.
Fisahn A, Pike FG, Buhl EH, Paulsen O. Cholinergic induction of network oscillations at 40 Hz in the hippocampus in vitro. Nature. 1998;394:186–9.
Mohebi A, Collins VL, Berke JD. Accumbens cholinergic interneurons dynamically promote dopamine release and enable motivation. eLife. 2023;12:e85011.
Jimenez-Martin J, Potapov D, Potapov K, Knöpfel T, Empson RM. Cholinergic modulation of sensory processing in awake mouse cortex. Sci Rep. 2021;11:17525.
Rokem A, Silver M. The benefits of cholinergic enhancement during perceptual learning are long-lasting. Front Comput Neurosci. 2013;7:66. https://www.frontiersin.org/articles/10.3389/fncom.2013.00066
Mineur YS, Obayemi A, Wigestrand MB, Fote GM, Calarco CA, Li AM, et al. Cholinergic signaling in the hippocampus regulates social stress resilience and anxiety- and depression-like behavior. Proc Natl Acad Sci USA. 2013;110:3573–8.
Gratton C, Yousef S, Aarts E, Wallace DL, D’Esposito M, Silver MA. Cholinergic, but not dopaminergic or noradrenergic, enhancement sharpens visual spatial perception in humans. J Neurosci. 2017;37:4405–15.
Dean B, Bakker G, Ueda HR, Tobin AB, Brown A, Kanaan RAA. A growing understanding of the role of muscarinic receptors in the molecular pathology and treatment of schizophrenia. Front Cell Neurosci. 2023;17:1124333.
Acharya S, Kim KM. Roles of the functional interaction between brain cholinergic and dopaminergic systems in the pathogenesis and treatment of schizophrenia and parkinson’s disease. Int J Mol Sci. 2021;22:4299.
Raedler TJ, Bymaster FP, Tandon R, Copolov D, Dean B. Towards a muscarinic hypothesis of schizophrenia. Mol Psychiatry. 2007;12:232–46.
Tandon R. Cholinergic hyperactivity and negative schizophrenic symptoms: a model of cholinergic/dopaminergic interactions in schizophrenia. Arch Gen Psychiatry. 1989;46:745.
Tandon R. Cholinergic aspects of schizophrenia. Br J Psychiatry. 1999;174:7–11.
Bernard V, Levey AI, Bloch B. Regulation of the subcellular distribution of M4 muscarinic acetylcholine receptors in striatal neurons in vivo by the cholinergic environment: evidence for regulation of cell surface receptors by endogenous and exogenous stimulation. J Neurosci. 1999;19:10237–49.
Xiao C, Zhou C, Jiang JH, Yin C. Neural circuits and nicotinic acetylcholine receptors mediate the cholinergic regulation of midbrain dopaminergic neurons and nicotine dependence. Acta Pharmacol Sin. 2019;41:1–9.
Wang L, Shang S, Kang X, Teng S, Zhu F, Liu B, et al. Modulation of dopamine release in the striatum by physiologically relevant levels of nicotine. Nat Commun. 2014;5:3925.
Marchi M, Risso F, Viola C, Cavazzani P, Raiteri M. Direct evidence that release-stimulating α7* nicotinic cholinergic receptors are localized on human and rat brain glutamatergic axon terminals. J Neurochem. 2002;80:1071–8.
Drenan RM, Grady SR, Steele AD, McKinney S, Patzlaff NE, McIntosh JM, et al. Cholinergic modulation of locomotion and striatal dopamine release is mediated by α6α4* nicotinic acetylcholine receptors. J Neurosci. 2010;30:9877–89.
Tzavara ET, Bymaster FP, Davis RJ, Wade MR, Perry KW, Wess J, et al. M4 muscarinic receptors regulate the dynamics of cholinergic and dopaminergic neurotransmission: relevance to the pathophysiology and treatment of related CNS pathologies. FASEB J. 2004;18:1410–2.
Gerber DJ, Sotnikova TD, Gainetdinov RR, Huang SY, Caron MG, Tonegawa S. Hyperactivity, elevated dopaminergic transmission, and response to amphetamine in M1 muscarinic acetylcholine receptor-deficient mice. Proc Natl Acad Sci USA. 2001;98:15312–7.
Exley R, McIntosh JM, Marks MJ, Maskos U, Cragg SJ. Striatal α5 nicotinic receptor subunit regulates dopamine transmission in dorsal striatum. J Neurosci. 2012;32:2352–6.
Veselinović T, Vernaleken I, Janouschek H, Kellermann T, Paulzen M, Cumming P, et al. Effects of anticholinergic challenge on psychopathology and cognition in drug-free patients with schizophrenia and healthy volunteers. Psychopharmacology (Berl). 2015;232:1607–17.
Wojtalik JA, Eack SM, Pollock BG, Keshavan MS. Prefrontal gray matter morphology mediates the association between serum anticholinergicity and cognitive functioning in early course schizophrenia. Psychiatry Res. 2012;204:61–7.
Schreiber SR, Wojtalik JA, Walker CP, Cho RY, Eack SM, Keshavan MS. Serum anticholinergicity is associated with reduced prefrontal brain function in early course schizophrenia. Psychiatry Res Neuroimaging. 2018;281:31–4.
Yohn SE, Weiden PJ, Felder CC, Stahl SM. Muscarinic acetylcholine receptors for psychotic disorders: bench-side to clinic. Trends Pharmacol Sci. 2022;43:1098–112.
Sauder C, Allen LA, Baker E, Miller AC, Paul SM, Brannan SK. Effectiveness of KarXT (xanomeline-trospium) for cognitive impairment in schizophrenia: post hoc analyses from a randomised, double-blind, placebo-controlled phase 2 study. Transl Psychiatry. 2022;12:1–8.
Coughlin JM, Du Y, Crawford JL, Rubin LH, Azad BB, Lesniak WG, et al. Use of 18 F-ASEM PET to determine the availability of the α7-nicotinic acetylcholine receptor in recent-onset psychosis. J Nucl Med. 2019;60:241–3.
Gibbons A, Dean B. The cholinergic system: an emerging drug target for schizophrenia. Curr Pharm Des. 2016;22:2124–33.
Raedler TJ, Tandon R. Cholinergic mechanisms in schizophrenia: current concepts. Curr Psychos Ther Rep. 2006;4:20–6.
Scarr E, Dean B. Muscarinic receptors: do they have a role in the pathology and treatment of schizophrenia? J Neurochem. 2008;107:1188–95.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw. 2010;36:1–48.
Weinstein JJ, Moeller SJ, Perlman G, Gil R, Van Snellenberg JX, Wengler K, et al. Imaging the vesicular acetylcholine transporter in schizophrenia: a positron emission tomography study using [18F]-VAT. Biol Psychiatry. 2024;96:352–64. https://www.sciencedirect.com/science/article/pii/S0006322324000623
Brašić JR, Cascella N, Kumar A, Zhou Y, Hilton J, Raymont V, et al. Positron emission tomography experience with 2-[18F]fluoro-3-(2(S)-azetidinylmethoxy)pyridine (2-[18F]FA) in the living human brain of smokers with paranoid schizophrenia. Synapse. 2012;66:352–68.
Wong NR, Rubin LH, Harrington CK, Jenkins KR, Shinehouse LK, Yoon M, et al. Hippocampal availability of the α7 nicotinic acetylcholine receptor in recent-onset psychosis. JAMA Netw Open. 2024;7:e2427163.
Wong DF, Kuwabara H, Horti AG, Roberts JM, Nandi A, Cascella N, et al. Brain PET imaging of α7-nAChR with [18F]ASEM: reproducibility, occupancy, receptor density, and changes in schizophrenia. Int J Neuropsychopharmacol. 2018;21:656–67.
D’Souza DC, Esterlis I, Carbuto M, Krasenics M, Seibyl J, Bois F, et al. Lower β2*-nicotinic acetylcholine receptor availability in smokers with schizophrenia. Am J Psychiatry. 2012;169:326–34.
Holt DJ, Bachus SE, Hyde TM, Wittie M, Herman MM, Vangel M, et al. Reduced density of cholinergic interneurons in the ventral striatum in schizophrenia: an in situ hybridization study. Biol Psychiatry. 2005;58:408–16.
Holt DJ, Herman MM, Hyde TM, Kleinman JE, Sinton CM, German DC, et al. Evidence for a deficit in cholinergic interneurons in the striatum in schizophrenia. Neuroscience. 1999;94:21–31.
Powchik P, Davidson M, Haroutunian V, Gabriel SM, Purohit DP, Perl DP, et al. Postmortem studies in schizophrenia. Schizophr Bull. 1998;24:325–41.
Scarr E, Keriakous D, Crossland N, Dean B. No change in cortical muscarinic M2, M3 receptors or [35S] GTPγS binding in schizophrenia. Life Sci. 2006;78:1231–7.
Moriya H, Takagi Y, Nakanishi T, Hayashi M, Tani T, Hirotsu I. Affinity profiles of various muscarinic antagonists for cloned human muscarinic acetylcholine receptor (mAChR) subtypes and mAChRs in rat heart and submandibular gland. Life Sci. 1999;64:2351–8.
Gibbons AS, Scarr E, Boer S, Money T, Jeon WJ, Felder C, et al. Widespread decreases in cortical muscarinic receptors in a subset of people with schizophrenia. Int J Neuropsychopharmacol. 2013;16:37–46.
Flynn DD, Ferrari-DiLeo G, Mash DC, Levey AI. Differential regulation of molecular subtypes of muscarinic receptors in alzheimer’s disease. J Neurochem. 1995;64:1888–91.
Marutle A, Zhang X, Court J, Piggott M, Johnson M, Perry R, et al. Laminar distribution of nicotinic receptor subtypes in cortical regions in schizophrenia. J Chem Neuroanat. 2001;22:115–26.
Freedman R, Hall M, Adler LE, Leonard S. Evidence in postmortem brain tissue for decreased numbers of hippocampal nicotinic receptors in schizophrenia. Biol Psychiatry. 1995;38:22–33.
Mowinckel AM ggseg/ggsegBrodmann: first release [Internet]. Zenodo 2021 [cited 2025 Jan 16]. Available from: https://zenodo.org/records/5668078.
Mowinckel AM, Vidal-Piñeiro D. Visualization of brain statistics with R packages ggseg and ggseg3d. Adv Methods Pract Psychol Sci. 2020;3:466–83.
Toru M, Watanabe S, Shibuya H, Nishikawa T, Noda K, Mitsushio H, et al. Neurotransmitters, receptors and neuropeptides in post-mortem brains of chronic schizophrenic patients. Acta Psychiatr Scand. 1988;78:121–37.
Haroutunian V, Davidson M, Kanof PD, Perl DP, Powchik P, Losonczy M, et al. Cortical cholinergic markers in schizophrenia. Schizophr Res. 1994;12:137–44.
Dean B, Pavey G, Scarr E. Higher levels of α7 nicotinic receptors, but not choline acetyltransferase, in the dorsolateral prefrontal cortex from a sub-group of patients with schizophrenia. Schizophr Res. 2020;222:283–90.
Shekhar A, Potter WZ, Lightfoot J, Lienemann J, Dubé S, Mallinckrodt C, et al. Selective muscarinic receptor agonist xanomeline as a novel treatment approach for schizophrenia. Am J Psychiatry. 2008;165:1033–9.
Crook JM, Tomaskovic-Crook E, Copolov DL, Dean B. Decreased muscarinic receptor binding in subjects with schizophrenia: a study of the human hippocampal formation. Biol Psychiatry. 2000;48:381–8.
Martin-Ruiz CM, Haroutunian VH, Long P, Young AH, Davis KL, Perry EK, et al. Dementia rating and nicotinic receptor expression in the prefrontal cortex in schizophrenia. Biol Psychiatry. 2003;54:1222–33.
Dean B, Crook JM, Pavey G, Opeskin K, Copolov DL. Muscarinic1 and 2 receptor mRNA in the human caudate-putamen: no change in M1 mRNA in schizophrenia. Mol Psychiatry. 2000;5:203–7.
Scarr E, Sundram S, Keriakous D, Dean B. Altered hippocampal muscarinic M4, but not M1, receptor expression from subjects with schizophrenia. Biol Psychiatry. 2007;61:1161–70.
Hansen JY, Markello RD, Tuominen L, Nørgaard M, Kuzmin E, Palomero-Gallagher N, et al. Correspondence between gene expression and neurotransmitter receptor and transporter density in the human brain. Neuroimage. 2022;264:119671.
Li W, Wang Y, Lohith TG, Zeng Z, Tong L, Mazzola R, et al. The PET tracer [11C]MK-6884 quantifies M4 muscarinic receptor in rhesus monkeys and patients with Alzheimer’s disease. Sci Transl Med. 2022;14:eabg3684.
Naganawa M, Nabulsi N, Henry S, Matuskey D, Lin SF, Slieker L, et al. First-in-human assessment of 11 C-LSN3172176, an M1 muscarinic acetylcholine receptor PET radiotracer. J Nucl Med. 2021;62:553–60.
Bakker G, Vingerhoets C, Boucherie D, Caan M, Bloemen O, Eersels J, et al. Relationship between muscarinic M1 receptor binding and cognition in medication-free subjects with psychosis. Neuroimage Clin. 2018;18:713–9.
McDermott TJ, Berg H, Touthang J, Akeman E, Cannon MJ, Santiago J, et al. Striatal reactivity during emotion and reward relates to approach–avoidance conflict behaviour and is altered in adults with anxiety or depression. J Psychiatry Neurosci. 2022;47:E311–22.
Xue B, Chen EC, He N, Jin DZ, Mao LM, Wang JQ. Integrated regulation of AMPA glutamate receptor phosphorylation in the striatum by dopamine and acetylcholine. Neuropharmacology. 2017;112:57–65.
Laurent V, Bertran-Gonzalez J, Chieng BC, Balleine BW. δ-Opioid and dopaminergic processes in accumbens shell modulate the cholinergic control of predictive learning and choice. J Neurosci. 2014;34:1358–69.
Alcantara AA, Mrzljak L, Jakab RL, Levey AI, Hersch SM, Goldman-Rakic PS. Muscarinic M1 and M2 receptor proteins in local circuit and projection neurons of the primate striatum: anatomical evidence for cholinergic modulation of glutamatergic prefronto-striatal pathways. J Comp Neurol. 2001;434:445–60.
Mao LM, He N, Jin DZ, Wang JQ. Regulation of phosphorylation of AMPA glutamate receptors by muscarinic M4 receptors in the striatum In vivo. Neuroscience. 2018;375:84–93.
Hersch SM, Gutekunst CA, Rees HD, Heilman CJ, Levey A. Distribution of M1-M4 muscarinic receptor proteins in the rat striatum: light and electron microscopic immunocytochemistry using subtype- specific antibodies. J Neurosci. 1994;14:3351–63.
Bernard V, Normand E, Bloch B. Phenotypical characterization of the rat striatal neurons expressing muscarinic receptor genes. J Neurosci. 1992;12:3591–600.
Abi-Dargham A, Gil R, Krystal J, Baldwin RM, Seibyl JP, Bowers M, et al. Increased striatal dopamine transmission in schizophrenia: confirmation in a second cohort. Am J Psychiatry. 1998;155:761–7.
Heinz A. Dopaminergic dysfunction in alcoholism and schizophrenia – psychopathological and behavioral correlates. Eur Psychiatry. 2002;17:9–16.
Zhang W, Yamada M, Gomeza J, Basile AS, Wess J. Multiple muscarinic acetylcholine receptor subtypes modulate striatal dopamine release, as studied with M1-M5 muscarinic receptor knock-out mice. J Neurosci. 2002;22:6347–52.
Durany N, Zöchling R, Boissl KW, Paulus W, Ransmayr G, Tatschner T, et al. Human post-mortem striatal α4β2 nicotinic acetylcholine receptor density in schizophrenia and Parkinson’s syndrome. Neurosci Lett. 2000;287:109–12.
Court JA, Martin-Ruiz C, Graham A, Perry E. Nicotinic receptors in human brain: topography and pathology. J Chem Neuroanat. 2000;20:281–98.
Bird ED, Barnes J, Iversen LL, Spokes EG, Mackay AV, Shepherd M. Increased brain dopamine and reduced glutamic acid decarboxylase and choline acetyltransferase activity in schizophrenia and related psychoses. Lancet. 1977;310:1157–9.
Noudoost B, Moore T. Control of visual cortical signals by prefrontal dopamine. Nature. 2011;474:372–5.
Jiang Y, Duan M, Chen X, Zhang X, Gong J, Dong D, et al. Aberrant prefrontal-thalamic-cerebellar circuit in schizophrenia and depression: evidence from a possible causal connectivity. Int J Neural Syst. 2019;29:1850032.
Senkowski D, Gallinat J. Dysfunctional prefrontal gamma-band oscillations reflect working memory and other cognitive deficits in schizophrenia. Biol Psychiatry. 2015;77:1010–9.
Yoshimura S, Ueda K, Suzuki SI, Onoda K, Okamoto Y, Yamawaki S. Self-referential processing of negative stimuli within the ventral anterior cingulate gyrus and right amygdala. Brain Cogn. 2009;69:218–25.
Zinchenko O, Arsalidou M. Brain responses to social norms: meta‐analyses of fMRI studies. Hum Brain Mapp. 2017;39:955–70.
Marinkovic K, Beaton LE, Rosen BQ, Happer JP, Wagner LC. Disruption of frontal lobe neural synchrony during cognitive control by alcohol intoxication. J Vis Exp. 2019; https://doi.org/10.3791/58839.
Scarr E, Hopper S, Vos V, Suk Seo M, Everall IP, Aumann TD, et al. Low levels of muscarinic M1 receptor–positive neurons in cortical layers III and V in Brodmann areas 9 and 17 from individuals with schizophrenia. J Psychiatry Neurosci. 2018;43:338–46.
Seo MS, Scarr E, Dean B. An investigation of the factors that regulate muscarinic receptor expression in schizophrenia. Schizophr Res. 2014;158:247–54.
Scarr E, Craig JM, Cairns MJ, Seo MS, Galati JC, Beveridge NJ, et al. Decreased cortical muscarinic M1 receptors in schizophrenia are associated with changes in gene promoter methylation, mRNA and gene targeting microRNA. Transl Psychiatry. 2013;3:1–9.
Mancama D, Arranz MJ, Landau S, Kerwin R. Reduced expression of the muscarinic 1 receptor cortical subtype in schizophrenia. Am J Med Genet B Neuropsychiatr Genet. 2003;119B:2–6.
Deng C, Huang XF. Decreased density of muscarinic receptors in the superior temporal gyrus in schizophrenia. J Neurosci Res. 2005;81:883–90.
Rousseau SJ, Jones IW, Pullar IA, Wonnacott S. Presynaptic alpha7 and non-alpha7 nicotinic acetylcholine receptors modulate [3H]D-aspartate release from rat frontal cortex in vitro. Neuropharmacology. 2005;49:59–72.
Levey A, Edmunds S, Koliatsos V, Wiley R, Heilman C. Expression of M1-M4 muscarinic acetylcholine receptor proteins in rat hippocampus and regulation by cholinergic innervation. J Neurosci. 1995;15:4077–92.
Dennis SH, Pasqui F, Colvin EM, Sanger H, Mogg AJ, Felder CC, et al. Activation of muscarinic M1 acetylcholine receptors induces long-term potentiation in the hippocampus. Cereb Cortex. 2016;26:414–26.
Marino MJ, Rouse ST, Levey AI, Potter LT, Conn PJ. Activation of the genetically defined M1 muscarinic receptor potentiates N-methyl-D-aspartate (NMDA) receptor currents in hippocampal pyramidal cells. Proc Natl Acad Sci USA. 1998;95:11465–70.
Zhao LX, Ge YH, Xiong CH, Tang L, Yan YH, Law PY, et al. M1 muscarinic receptor facilitates cognitive function by interplay with AMPA receptor GluAl subunit. FASEB J. 2018;32:4247–57.
Yamasaki M, Matsui M, Watanabe M. Preferential localization of muscarinic M1 receptor on dendritic shaft and spine of cortical pyramidal cells and its anatomical evidence for volume transmission. J Neurosci. 2010;30:4408–18.
Dasari S, Gulledge AT. M1 and M4 receptors modulate hippocampal pyramidal neurons. J Neurophysiol. 2011;105:779–92.
Shirey JK, Xiang Z, Orton D, Brady AE, Johnson KA, Williams R, et al. An allosteric potentiator of M4 mAChR modulates hippocampal synaptic transmission. Nat Chem Biol. 2008;4:42–50.
Romanelli Ferreira A, Fürstenau L, Blanco C, Kornisiuk E, Sánchez G, Daroit D, et al. Role of hippocampal M1 and M4 muscarinic receptor subtypes in memory consolidation in the rat. Pharmacol Biochem Behav. 2003;74:411–5.
Thorn CA, Popiolek M, Stark E, Edgerton JR. Effects of M1 and M4 activation on excitatory synaptic transmission in CA1. Hippocampus. 2017;27:794–810.
Mexal S, Berger R, Logel J, Ross RG, Freedman R, Leonard S. Differential regulation of α7 nicotinic receptor gene (CHRNA7) expression in schizophrenic smokers. J Mol Neurosci. 2010;40:185–95.
Thomsen MS, Weyn A, Mikkelsen JD. Hippocampal α7 nicotinic acetylcholine receptor levels in patients with schizophrenia, bipolar disorder, or major depressive disorder. Bipolar Disord. 2011;13:701–7.
Fabian-Fine R, Skehel P, Errington ML, Davies HA, Sher E, Stewart MG, et al. Ultrastructural distribution of the alpha7 nicotinic acetylcholine receptor subunit in rat hippocampus. J Neurosci. 2001;21:7993–8003.
Kanno T, Yaguchi T, Yamamoto S, Nagata T, Yamamoto H, Fujikawa H, et al. Bidirectional regulations for glutamate and GABA release in the hippocampus by α7 and non-α7 ACh receptors. Biochem Biophys Res Commun. 2005;338:742–7.
McGeer PL, McGeer EG. Possible changes in striatal and limbic cholinergic systems in schizophrenia. Arch Gen Psychiatry. 1977;34:1319–23.
Crook JM, Tomaskovic-Crook E, Copolov DL, Dean B. Low muscarinic receptor binding in prefrontal cortex from subjects with schizophrenia: a study of Brodmann’s areas 8, 9, 10, and 46 and the effects of neuroleptic drug treatment. Am J Psychiatry. 2001;158:918–25.
Eum S, Hill SK, Rubin LH, Carnahan RM, Reilly JL, Ivleva EI, et al. Cognitive burden of anticholinergic medications in psychotic disorders. Schizophr Res. 2017;190:129–35.
Eack SM, Wojtalik JA, Keshavan MS. Anticholinergic medications in the treatment of psychoses: pharmacological subtraction is better than addition. Schizophr Res. 2023;262:40–1.
Tang YL, George T, Mao PX, Cai ZJ, Chen Q. Cigarette smoking in Chinese male inpatients with schizophrenia: a cross-sectional analysis. J Psychiatr Res. 2007;41:43–8.
Wium-Andersen MK, Ørsted DD, Nordestgaard BG. Tobacco smoking is causally associated with antipsychotic medication use and schizophrenia, but not with antidepressant medication use or depression. Int J Epidemiol. 2015;44:566–77.
Hui CL, Tang JY, Leung CM, Wong GH, Chang WC, Chan SK, et al. A 3-year retrospective cohort study of predictors of relapse in first-episode psychosis in Hong Kong. Aust N Z J Psychiatry. 2013;47:746–53.
Wootton RE, Richmond RC, Stuijfzand BG, Lawn RB, Sallis HM, Taylor GMJ, et al. Evidence for causal effects of lifetime smoking on risk for depression and schizophrenia: a mendelian randomisation study. Psychol Med. 2020;50:2435–43.
Ziaaddini H, Kheradmand A, Vahabi M. Prevalence of cigarette smoking in schizophrenic patients compared to other hospital admitted psychiatric patients. Addict Health. 2009;1:38–42.
Scarr E, Cowie TF, Kanellakis S, Sundram S, Pantelis C, Dean B. Decreased cortical muscarinic receptors define a subgroup of subjects with schizophrenia. Mol Psychiatry. 2009;14:1017–23.
Alnafisah RS, Reigle J, Eladawi MA, O’Donovan SM, Funk AJ, Meller J, et al. Assessing the effects of antipsychotic medications on schizophrenia functional analysis: A postmortem proteome study. Neuropsychopharmacology. 2022;47:2033–41.
Crook JM, Dean B, Pavey G, Copolov D. The binding of [3H]AF-DX 384 is reduced in the caudateputamen of subjects with schizophrenia. Life Sci. 1999;64:1761–71.
Dean B, Crook JM, Opeskin K, Hill C, Keks N, Copolov DL. The density of muscarinic M1 receptors is decreased in the caudate-putamen of subjects with schizophrenia. Mol Psychiatry. 1996;1:54–8.
Dean B, Gray L, Keriakous D, Scarr E. A comparison of M1 and M4 muscarinic receptors in the thalamus from control subjects and subjects with schizophrenia. Thalamus Relat Syst. 2004;2:287–95.
Dean B, Soulby A, Evin GM, Scarr E. Levels of [3H]pirenzepine binding in Brodmann’s area 6 from subjects with schizophrenia is not associated with changes in the transcription factor SP1 or BACE1. Schizophr Res. 2008;106:229–36.
Dean B, Thomas N, Lai CY, Chen WJ, Scarr E. Changes in cholinergic and glutamatergic markers in the striatum from a sub-set of subjects with schizophrenia. Schizophr Res. 2015;169:83–8.
Dean B, Hopper S, Conn PJ, Scarr E. Changes in BQCA allosteric modulation of [3H]NMS binding to human cortex within schizophrenia and by divalent cations. Neuropsychopharmacology. 2016;41:1620–8.
Dean B, Duce J, Li QX, Masters CL, Scarr E. Lower levels of soluble β-amyloid precursor protein, but not β-amyloid, in the frontal cortex in schizophrenia. Psychiatry Res. 2024;331:115656.
Hopper S, Pavey GM, Gogos A, Dean B. Widespread changes in positive allosteric modulation of the muscarinic M1 Receptor in some participants with schizophrenia. Int J Neuropsychopharmacol. 2019;22:640–50.
Matsumoto I, Inoue Y, Iwazaki T, Pavey G, Dean B. 5-HT2A and muscarinic receptors in schizophrenia: A postmortem study. Neurosci Lett. 2005;379:164–8.
McLeod MC, Scarr E, Dean B. Effects of benzodiazepine treatment on cortical GABAA and muscarinic receptors: Studies in schizophrenia and rats. Psychiatry Res. 2010;179:139–46.
Newell KA, Zavitsanou K, Jew SK, Huang XF. Alterations of muscarinic and GABA receptor binding in the posterior cingulate cortex in schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2007;31:225–33.
Salah-Uddin H, Scarr E, Pavey G, Harris K, Hagan JJ, Dean B, et al. Altered M(1) muscarinic acetylcholine receptor (CHRM1)-Gα(q/11) coupling in a schizophrenia endophenotype. Neuropsychopharmacol Off Publ Am Coll Neuropsychopharmacol. 2009;34:2156–66.
Watanabe S, Nishikawa T, Takashima M, Toru M. Increased muscarinic cholinergic receptors in prefrontal cortices of medicated schizophrenics. Life Sci. 1983;33:2187–96.
Zavitsanou K, Katsifis A, Yu Y, Huang XF. M2/M4 muscarinic receptor binding in the anterior cingulate cortex in schizophrenia and mood disorders. Brain Res Bull. 2005;65:397–403.
Court J, Spurden D, Lloyd S, McKeith I, Ballard C, Cairns N, et al. Neuronal nicotinic receptors in dementia with Lewy bodies and schizophrenia: α-bungarotoxin and nicotine binding in the thalamus. J Neurochem. 1999;73:1590–7.
Guan ZZ, Zhang X, Blennow K, Nordberg A. Decreased protein level of nicotinic receptor α7 subunit in the frontal cortex from schizophrenic brain. Neuroreport. 1999;10:1779–82.
Guillozet-Bongaarts AL, Hyde TM, Dalley RA, Hawrylycz MJ, Henry A, Hof PR, et al. Altered gene expression in the dorsolateral prefrontal cortex of individuals with schizophrenia. Mol Psychiatry. 2014;19:478–85.
Hemby SE, Ginsberg SD, Brunk B, Arnold SE, Trojanowski JQ, Eberwine JH. Gene expression profile for schizophrenia: Discrete neuron transcription patterns in the entorhinal cortex. Arch Gen Psychiatry. 2002;59:631–40.
Mathew SV, Law AJ, Lipska BK, Dávila-García MI, Zamora ED, Mitkus SN, et al. α7 nicotinic acetylcholine receptor mRNA expression and binding in postmortem human brain are associatedwith genetic variation in neuregulin 1. Hum Mol Genet. 2007;16:2921–32.
De Luca V, Likhodi O, Van Tol HHM, Kennedy JL, Wong AHC. Regulation of α7-nicotinic receptor subunit and α7-like gene expression in the prefrontal cortex of patients with bipolar disorder and schizophrenia. Acta Psychiatr Scand. 2006;114:211–5.
Severance EG, Yolken RH. Novel α7 nicotinic receptor isoforms and deficient cholinergic transcription in schizophrenia. Genes Brain Behav. 2008;7:37–45.
Impagnatiello F, Guidotti AR, Pesold C, Dwivedi Y, Caruncho H, Pisu MG, et al. A decrease of reelin expression as a putative vulnerability factor in schizophrenia. Proc Natl Acad Sci. 1998;95:15718–23.
Kunii Y, Zhang W, Xu Q, Hyde TM, McFadden W, Shin JH, et al. CHRNA7 and CHRFAM7A mRNAs: Co-localized and their expression levels altered in the postmortem dorsolateral prefrontal cortex in major psychiatric disorders. Am J Psychiatry. 2015;172:1122–30.
German DC, Manaye KF, Wu D, Hersh LB, Zweig RM. Mesopontine cholinergic and non-cholinergic neurons in schizophrenia. Neuroscience. 1999;94:33–8.
Acknowledgements
The current systematic review was supported by the Canadian Institutes of Health Research (support provided to LT and SG; Grant #173227), the Emerging Research Innovators in Mental Health (eRIMh) Program (support provided to LT and SG), and the Vanier Canada Graduate Scholarship Program (scholarship provided to ZS; Award #455165).
Author information
Authors and Affiliations
Contributions
ZS: protocol development, search, abstract screening, full-text review, data extraction and risk of bias assessment, analyses, original draft, writing, figures and tables. JM: full-text review, data extraction, risk of bias assessment, figures. RA: data extraction and risk of bias assessment. RH: abstract screening, figures. MS: protocol development, reviewing, editing. MK: protocol development, reviewing, editing. LT: conceptualization, writing, reviewing, editing, analyses, supervision. SG: conceptualization, writing, reviewing, editing, supervision.
Corresponding authors
Ethics declarations
Competing interests
MS received honoraria/has been a consultant for AbbVie, Boehringer-Ingelheim, Otsuka. SG received honoraria/has been a consultant for Boehringer-Ingelheim (Canada) Ltd. RH previously owned shares in Karuna Therapeutics and received two knowledge dissemination grants from Otsuka to organize local trainee conferences.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Saint-Georges, Z., MacDonald, J., Al-Khalili, R. et al. Cholinergic system in schizophrenia: A systematic review and meta-analysis. Mol Psychiatry 30, 3301–3315 (2025). https://doi.org/10.1038/s41380-025-03023-y
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41380-025-03023-y