Abstract
Major depressive disorder (MDD) is a complex psychiatric disorder that affects the lives of hundreds of millions of individuals around the globe. Even today, researchers debate if morphological alterations in the brain are linked to MDD, likely due to the heterogeneity of this disorder. The application of deep learning tools to neuroimaging data, capable of capturing complex non-linear patterns, has the potential to provide diagnostic and predictive biomarkers for MDD. However, previous attempts to demarcate MDD patients and healthy controls (HC) based on segmented cortical features via linear machine learning approaches have reported low accuracies. In this study, we used globally representative data from the ENIGMA-MDD working group containing 7012 participants from 31 sites (N = 2772 MDD and N = 4240 HC), which allows a comprehensive analysis with generalizable results. Based on the hypothesis that integration of vertex-wise cortical features can improve classification performance, we evaluated the classification of a DenseNet and a Support Vector Machine (SVM), with the expectation that the former would outperform the latter. As we analyzed a multi-site sample, we additionally applied the ComBat harmonization tool to remove potential nuisance effects of site. We found that both classifiers exhibited close to chance performance (balanced accuracy DenseNet: 51%; SVM: 53%), when estimated on unseen sites. Slightly higher classification performance (balanced accuracy DenseNet: 58%; SVM: 55%) was found when the cross-validation folds contained subjects from all sites, indicating site effect. In conclusion, the integration of vertex-wise morphometric features and the use of the non-linear classifier did not lead to the differentiability between MDD and HC. Our results support the notion that MDD classification on this combination of features and classifiers is unfeasible. Future studies are needed to determine whether more sophisticated integration of information from other MRI modalities such as fMRI and DWI will lead to a higher performance in this diagnostic task.
Similar content being viewed by others
Introduction
Major depressive disorder (MDD) dramatically impacts the daily functioning of patients and is currently the leading cause of disability worldwide [1]. Therefore, early diagnosis and optimal allocation of the proper treatment are critical. Unfortunately, the current treatment strategies present a response rate and remission as low as of 36.8% after a first treatment [2,3,4]. Thus, as proposed in the realms of systems medicine, we expect that by identifying brain patterns that classify patients at the individual level, we may open new biomarker-based avenues for the development of more personalized and effective treatments.
Neuroimaging techniques, such as magnetic resonance imaging (MRI), enable a non-invasive macro-scale view of human brain structure at the millimeter level of resolution. Initial neuroimaging studies used univariate approaches to reveal structural brain differences in MDD compared to healthy controls (HC) [5,6,7], identifying reduced hippocampal and frontal lobe volume. However, these studies had limited sample sizes and the more recent large sample studies have reported small effect sizes [8,9,10,11], highlighting the absence of a single neuro-anatomical biomarker associated with MDD. The search for more complex biomarkers, which may include the interaction between different neuro-anatomical features, can be conducted via machine learning (ML) algorithms - especially deep learning (DL) algorithms - applied to the MDD vs HC classification task.
Like univariate approaches, ML and DL studies reported varying classification accuracies from 53–91% [12, 13]. The high variability of classification performances and the lack of consistent biomarkers can partly be explained by the small sample sizes, as it was demonstrated by Flint and colleagues [14]. Supplementing this, a study based on cortical and subcortical morphological features, reported high accuracy of 75% in the small sample, which was not replicated in an independent large UK Biobank dataset, achieving only 54% [15].
Another factor that may inflate classification accuracies are related to study-site effects. The site-effect corresponds to site-specific characteristics other than diagnosis – such as scanner type, acquisition protocol, demographic differences, and inclusion and exclusion criteria – which may bias classification accuracies. A study demonstrated how site effect may contribute to both inflated and deflated classification accuracies [16]. Hence, numerous ways to tackle site-effect and improve model generalizability exist, from linear and non-linear ComBat harmonization tools [17, 18] to embedding site confounders directly to the model [19]. However, to overcome the difficult point of the heterogeneity of MDD and the lack of replicability and generalization of the models, the investigation of very large samples of participants with global representation is fundamental.
Using a large-scale dataset from the ENIGMA-MDD consortium, we compared the classification performance of commonly used ML models to predict diagnosis based on cortical and subcortical parcellations of morphological features (surface areas, thicknesses, volumes) [20]. Overall, results showed a trend that may highlight the contribution of site-effects to classification performance. Specifically, there was a clear difference in classification performance dependent on the cross-validation splitting techniques used in training. Site-splitting generally performed at close to chance level for all classifiers, while mixing sites across splits achieved up to 62% balanced accuracy with an SVM. Of note, data harmonization using ComBat removed the site effect and resulted in a balanced accuracy of 52% with SVM. Based on these findings, we concluded that most commonly used ML classification algorithms could not successfully discriminate MDD from HC individuals based on morphological features organized in pre-defined Desikan-Killiany atlas parcellations. However, it remains unclear whether more fine-grained information of morphometric features, displayed in a vertex-wise organization, could outperform the classification based on parcellation atlas-distributed information.
There are some directions in improving classification based on morphological information. First, previous ML studies considered surface area, thickness, and volume characteristics only, while the information on the cortical shape, such as gyral and sulcal shape patterns, was not integrated into analyses. Cortical gyrification modalities are affected by genetic and non-genetic factors [21, 22], alterations of which were associated with MDD [23, 24]. Multimodal morphological feature analysis, including myelination, gray matter, and curvature, revealed a correlation between cortical differences and MDD-associated genes [25]. Therefore, the addition of shape modalities, such as cortical curvature and sulcal depth, to cortical thickness could enhance the classification performance, as demonstrated for sex and autism classification [26].
Cortical morphological features such as sulcal depth and gyrification, measured via local gyrification index (LGI) or curvature, have been investigated as potential biomarkers for MDD, although the literature remains limited and somewhat inconsistent. Some earlier studies have suggested that sulcal depth may be decreased in individuals with suicidality-associated MDD [25]. Even so, this study included only 39 healthy controls, 40 depressed patients without suicidality (patient controls), and 39 with suicidality (suicidal groups) were analyzed based on SBM to estimate the fractal dimension, gyrification index, sulcal depth, and cortical thickness; the small sample size and range of features assessed make it prone to both type I and type II error, relative to the studies we have performed in thousands of patients. In terms of gyrification, multiple studies have reported both hypo- and hyper-gyrification in various cortical regions, including the frontal, cingulate, insular, parietal, and temporal lobes [24, 27,28,29,30,31]. However, these findings are often region-constrained, based on small sample sizes, and lack consistent replication across cohorts and studies. These constraints highlight the need for coordinated multi-site analyses using harmonized data and advanced morphometric modeling approaches.
Hence, one promising direction is the use of more advanced classification algorithms. DL methods have gained popularity in the neuroimaging field as a promising tool for cortical surface reconstruction [32], image preprocessing [33], and cortical parcellation [34]. Furthermore, DL is widely evaluated as a predictive tool in psychiatry, showing higher or at least the same classification performance compared to linear models [26, 35,36,37,38,39]. The analysis of cortical morphometric features can be conducted via convolutional neural network (CNN) [40], designed to reveal complex patterns in 2D images. In order to apply such 2D CNN in the classification, it requires 3D cortical features to be initially projected into 2D image space. Nevertheless, this step may inevitably create distortion in spatial properties such as shape, area, distance, and direction. Several approaches were implemented before, such as latitude/longitude projection [41] and optimal mass transport (OMT) projection [26, 42], which preserves area. However, the impact of these projection methods on classification performance were never directly compared in the neuroimaging field.
The main goal of this study was to distinguish MDD from HC individuals based on integrated cortical morphological features, including sulcal depth, curvature, and thickness. These features were analyzed via SVM with linear kernel and CNN architecture of pre-trained DenseNet [43], which demonstrated its superiority over simpler models in autism vs HC classification task [26]. SVM was chosen as it is a robust shallow ML model, frequently used in neuroimaging settings [44,45,46]. We investigated classification performance of these two methods to understand the role of complex non-linear patterns in MDD manifestation. We used balanced accuracy, sensitivity, specificity and AUC as the classification performance metrics. Higher classification performance of the DenseNet model presume the presence of spatially complex patterns in brain morphology, which are relevant for classification. Furthermore, we aimed to estimate the relevance of integrating cortical thickness and shape characteristics (sulcal depth, curvature and thickness) into the analysis by training the models with all features combined and by considering them separately. Similar to our previous study [20], different cross-validation (CV) approaches were evaluated: Splitting the data by balancing age and sex distribution across all CV folds (Splitting by Age/Sex), and performing leave-sites-out CV in order to estimate the performance on the unseen during the training sites (Splitting by Site). This approach allowed us to estimate whether the model’s performance is influenced by demographic or site-related factors. The difference between results in both splitting strategies presumes the presence of the site effect we addressed by harmonizing the data in both splitting strategies via ComBat. In summary, we hypothesized that: (1) Integration of cortical thickness and shape characteristics would contribute positively to the classification performance, and (2) DenseNet could differentiate MDD from HC based on the provided features. Additionally, we compared two projection methods, latitude/longitude and OMT projections by performing auxiliary single-site sex classification based on three of the largest cohorts to explore whether classification performance may vary according to 2D projection method. We had no a priori hypothesis for the projection results.
Material and methods
Study participants and study design
We analyzed a large-scale multi-site sample provided by the ENIGMA-MDD working group, comprising 2772 MDD and 4240 HC individuals, from 30 cohorts worldwide. Details on inclusion/exclusion criteria and sample characteristics can be found in Supplementary Table 1. Subjects with missing information on demographic data or any of cortical surface mesh files (l(r).sulc, l(r).curv, l(r).thickness) were excluded from the analysis (476 and 6% excluded).
Image processing and analysis
Each site acquired structural T1-weighted MRI scans of participants and preprocessed them according to ENIGMA Consortium protocol (http://enigma.ini.usc.edu/protocols/imaging-protocols/). This pipeline includes the segmentation of T1-weighted MRI volumes, tessellation, topology correction, and spherical inflation of the white matter surface. Detailed information on the acquisition protocols and scanner model in each cohort can be found in Supplementary Table 2. Cortical meshes were generated during FreeSurfer preprocessing in every site. Cerebral cortex meshes were then extracted from the FreeSurfer unsmoothed fsaverage6 template, effectively removing intracranial volume (ICV) differences (Supplementary Fig. 1) and yielding 37,747 and 37,766 vertices for the left and right hemispheres, respectively. The preprocessing pipeline applied in this study is consistent across all subjects, regardless of age, as the core procedures do not differ fundamentally between adolescents and adults. We analyzed vertex-wise features, such as sulcal depth, curvature, and thickness, both as integrated features and separately (Fig. 1).
Left: Higher classification performance in MDD vs HC classification task can be achieved by implementing deep ML models, such as DenseNet, in comparison to a shallow ML model, for example, SVM. Furthermore, the analysis of integrated morphometric features can provide a more detailed description of cortical organization than separated features, leading to better differentiability of MDD from HC. The application of ComBat may improve the generalizability of results as site-related differences are removed. Right: Cortical sulcal depth, curvature, and thickness are first projected into the 2D grid and then transformed into 2D images using OMT projection. We split the data into 10 CV folds according to age and sex (Splitting by Age/Sex) and according to the site belonging (Splitting by Site). After the residualization step, where the age and sex effect are regressed out linearly, we train and test SVM and DenseNet on the diagnosis classification.
Considering the absence of well-established pre-trained on cortical meshes CNN models, we projected 3D cortical surfaces into 2D images and applied DenseNet, which was pre-trained on natural images. There are few studies applying different projection methods such as latitude/longitude project and area-preserving maps [e.g., 26, 41]. Of note, the latitude/longitude method, in which cortical mesh is first re-sampled to the sphere and consequently mapped to the 2D grid, creates strong area distortions in the edges and near the medial wall close to subcortical regions [41]. Both methods may (differentially) influence subsequent classification performances, but to the best of our knowledge, no studies to date have directly compared this in one study using the same samples. Thus, we applied both 2D projection methods to the cortical meshes, resulting in 224 × 224 pixels images for each hemisphere. The images were normalized to present mean of 0 and standard deviation of 1.
Data splitting
To assess potential biases in the model’s decision-making, we performed 10-fold cross-validation (CV) by splitting the data according to (1) demographic covariates, in which age and sex distribution were balanced and subjects from each site are equally distributed across all CV folds (Splitting by Age/Sex), and (2) site affiliation, where each site was contained only in one CV fold (Splitting by Site). In both strategies, 9 CV folds were used for training, while one remaining CV fold was used as a test set. This procedure was repeated iteratively until every CV fold was used as a test set. In the Splitting by Age/Sex strategy, effect of demographic factors on the classification performance is reduced, as the model is trained and tested on the same demographics. Nevertheless, the site-related differences may bias the decision-making of the classification models [20], which is directly addressed in Splitting by Site. This strategy demonstrates how well the model trained on one set of sites can be applied to the data from unseen sites. As the number of sites exceeds the number of folds, we distributed the sites across the folds to balance the number of subjects in every fold as close as possible by iteratively distributing the largest sites across all 10 folds. Smallest folds were added subsequently to further even the number of subjects in every fold. Overall, the difference in the classification results between these two splitting strategies may indicate the existence of the site effect. More detailed description of both splitting strategies can be found elsewhere [20].
MDD vs HC classification
After the data-splitting step, the primary analysis was carried out. Firstly, we residualized all features normatively, removing linear age and sex dependencies. To avoid data leakage, age and sex regressors were estimated on the healthy subjects from the training set (9 CV folds) and then applied to the training and test set (1 CV fold) for patients and HC. Next, the classification algorithms were trained on the training folds, and classification performance was estimated on the test fold. As demonstrated by Dinga and colleagues, accuracy alone should be avoided as it does not account for class frequencies [47]. Thus, the algorithms were evaluated according to categorical measures, including balanced accuracy, sensitivity, specificity, and rank-based measure – AUC, allowing for a broad overview of performance. For model-level assessment [48], we performed the classification using all features combined and then using features separately to assess the final classification performance. We evaluated the classification performance of a robust shallow model - SVM with linear kernel, and DL model - DenseNet pre-trained on natural images from ImageNet dataset [49], which has been shown to be a robust convolutional neural network for image classification in both natural images and neuroimaging contexts [26, 43]. When DenseNet was trained on a single data domain, left and right hemisphere images were propagated through corresponding left and right DenseNets, the fully connected layers of which were concatenated. The resulting feature vectors were then fed to the output layer. For the whole-brain all-features analysis, we combined the features extracted from every feature and hemisphere, concatenate them, and fed them to the output layer. For SVM, all considered images were flattened and then concatenated into a single array. In this study, we intentionally chose not to apply dimensionality reduction techniques (e.g., PCA or feature selection) prior to model training. This decision was driven by the goal of preserving the full anatomical interpretability of vertex-wise cortical features and directly evaluating the classification potential of the complete morphometric representation. To mitigate the risk of overfitting in this high-dimensional setting, we implemented nested 10-fold cross-validation for robust performance estimation and hyperparameter tuning. Specifically, for the SVM, nine values of the regularization parameter (C) were explored, resulting in 90 model evaluations across outer folds. For DenseNet, the grid search spanned 54 unique hyperparameter combinations, yielding 540 model evaluations (hyperparameters in Supplementary Table 3). The concept and implementation of analysis are illustrated in Fig. 1. To mitigate site-related differences, which may potentially bias the classification results, we additionally performed the analysis by harmonizing all features via ComBat. Variance explained by age and sex was preserved during this harmonization step. Next, we residualized features normatively, as described above, and trained/tested the models. Application of ComBat differed for both splitting strategies. In short, ComBat parameters estimated on the training set were applied to the test set directly for the Age/Sex splitting strategy. In splitting by Site, ComBat was applied twice: first, we used ComBat to harmonize the training sites; second, we applied ComBat to adjust the test sites to the harmonized training sites, i.e., using the training sites as the reference batch [50]. A more detailed description of the ComBat application can be found in our previous work [20].
Auxiliary analysis in projection methods
To explore and evaluate the potential impact of 2D projection methods on the classification performance, we compared both methods in their ability to classify healthy males from healthy females in 3 of the largest cohorts separately. The single-site classification was estimated via 10-fold CV on 411, 723, and 397 subjects, respectively. As usual, 9 CV folds were used for training, while one remaining CV fold was used as a test set. This procedure was repeated iteratively until every CV fold is used as a test set. To provide an initial perspective on the potential classification advantages of the pre-trained DenseNet, we presented the balanced accuracies obtained by two classifiers: an SVM with a linear kernel and the DenseNet [43]. Furthermore, using the hyperparameters found via the sex classification task (Supplementary Table 3), we presented the classification performance of both models.
Results
Participants and data splitting
We detected substantial differences in age (78% of pairwise comparisons between cohorts were significant, t-test, p < 0.05) and sex (47%, t-test, p < 0.05) across cohorts. The demographic and clinical profile is presented in Table 1. As expected, Splitting by Age/Sex resulted in more balanced CV folds with respect to number of subjects, age and sex distributions, while folds created by Splitting by Site were more uneven on these characteristics (Table 2).
MDD vs HC classification
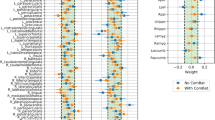
First, we compared the performance of SVM and DenseNet for different splitting strategies (Fig. 2). In Splitting by Age/Sex, SVM achieved 0.551 ± 0.021 in balanced accuracy, while DenseNet yielded 0.578 ± 0.022. In Splitting by Site, both SVM and DenseNet models performed worse, yielding 0.528 ± 0.039 and 0.512 ± 0.019, respectively. The minor difference in classification performances for different splitting strategies indicated a potential site effect, which we addressed by applying ComBat. In Splitting by Age/Sex, the balanced accuracy of SVM with ComBat dropped to 0.478 ± 0.019, while the performance of DenseNet did not change and yielded 0.561 ± 0.015. In splitting by Site with ComBat, the performance of both models was similar and close to random chance, balanced accuracy yielded 0.520 ± 0.019 and 0.508 ± 0.020 for SVM and DenseNet respectively. Thus, we did not observe an improvement of models’ performances after data harmonization by ComBat. A full panel of results, including all classification metrics, can be found in Supplementary Table 4.
Next, we explored if any of the considered feature modalities yields greater classification performance (Fig. 2). In Splitting by Age/Sex, all data modalities yielded similar range of accuracies: thickness (SVM: 0.549 ± 0.020; DenseNet: 0.576 ± 0.019) compared to sulcal depth (SVM: 0.543 ± 0.022; DenseNet: 0.562 ± 0.019), and curvature (SVM: 0.531 ± 0.015; DenseNet: 0.567 ± 0.019), observed for both classification models. In Splitting by Site, sulcal depth (SVM: 0.523 ± 0.016; DenseNet: 0.515 ± 0.020), curvature (SVM: 0.513 ± 0.033; DenseNet: 0.516 ± 0.025) and thickness (SVM: 0.522 ± 0.038; DenseNet: 0.515 ± 0.022) also exhibited similar range of classification accuracies. Both models performed similarly for all feature types. These results demonstrate that integration of shape modalities with cortical thickness did not benefit the classification models. Results from the exploratory analyses for each hemisphere and for each feature modality per hemisphere showed no improvements in performance of the models (Supplementary Table 5, Supplementary Fig. 3). In addition, we applied the main demographic and clinical stratifications used in the ENIGMA-MDD working group to assess post-hoc whether groups that are more homogeneous would achieve better classification metrics (Supplementary Table 6).
Auxiliary sex prediction task
As an initial step, we also conducted a sex classification to explore which projection method (latitude/longitude, OMT) yields higher classification performance for both SVM and DenseNet (Supplementary Fig. 2). There was no clear difference between projection methods; however, we observed a consistently higher classification performance of DenseNet compared to SVM for all types of features and hemispheres. Considering previous success of OMT projection as a projection method applied on cortical surface and its property to preserve distances between vertices [26], we conducted our main analysis with OMT projection.
Discussion
In this work, we evaluated the diagnostic classification performance of DenseNet and SVM models, trained on cortical maps projected via OMT, including sulcal depth, curvature, and thickness, from a multi-site global dataset. Our analysis included 7012 participants from 31 sites worldwide, allowing for a comprehensive and realistic overview of classification performances. Both models were evaluated in parallel using two different CV splitting strategies. In Splitting by Age/Sex, we obtained CV folds with comparable demographics; thus, the performance of the models should not be affected by these demographic variables. In Splitting by Site, sites were distributed across folds. Therefore, models were trained and tested on different sets of sites. This strategy is closer to application of diagnostic classification models in clinical practice, and allowed for realistic estimation of classification performance on unseen sites. Overall, the classification performances of both models were similar: In Splitting by Age/Sex, DenseNet achieved 58 vs 55% for SVM; in Splitting by Site, the difference was even more negligible, DenseNet achieved 51 vs 52% for SVM. Both models performed better in Splitting by Age/Sex, implying the presence of a confounding site effect, most likely arising from differences in scanner vendors or image acquisition parameters. In this sense, ComBat approximated the classification results of the two splitting strategies, but did not improve the accuracy of the models. Ultimately, the classification performances of both models for all integrated morphometric features, both in Splitting by Age/Sex and in Splitting by Site, revealed similar classification levels of single-features.
Cortical morphological maps as diagnostic biomarkers for MDD
To the best of our knowledge, this is the first study to combine cortical thickness, sulcal depth, and curvature features in order to classify MDD vs HC. Furthermore, previous ML studies with large samples only incorporated low-resolution atlas-based thickness characteristics. In our approach, we analyzed vertex-wise information, providing a richer and more detailed description of brain characteristics than atlas-derived regional measures. Even so, the integration of complementary cortical characteristics did not lead to higher classification performances compared to the accuracies obtained from the single cortical features, regardless of the data splitting strategy and the classification model. In Splitting by Site, no feature yielded an accuracy substantially higher than random chance accuracy, indicating the failure of both models to capture MDD-specific alterations. Furthermore, the analysis of finer-grained cortical maps, even for thickness alone, did not result in higher classification performance, compared to ML performance levels observed in our previous study [20]. Thus, the assumption that higher resolution would lead to greater classification performance did not hold in this study, as all results were close to the chance level, in line with previous attempts in classifying MDD [14, 15, 20]. Furthermore, stratification of the sample according to demographic (sex) and clinical characteristics (age of onset, antidepressant use, and number of depressive episodes) did not yield better differentiability between HC and MDD, in line with our previous study [20]. This new evidence suggests the absence of prominent gray matter alterations that alone may serve as diagnostic tool in patients with MDD. Combining features such as sulcal depth, curvature, and thickness in vertex-wise, unfolded cortical maps, and including them within a deep learning framework, is highly original. It advances prior work [24, 25, 27,28,29, 31] by integrating these complementary morphometric dimensions in a way few studies have, potentially clarifying whether these combined metrics can yield robust, clinically actionable biomarkers.
Although we combined complementary characteristics in the analysis, the interaction between thickness and shape was not addressed here. According to recent evidence, local cortical shape may correlate with thickness [51]. So, combined thickness-shape patterns should be further explored for the classification of MDD. Furthermore, reduced myelination was associated with MDD [52,53,54], which could lead to structural reorganization of cortical features, making it a potential classification aspect to be investigated. In addition, subcortical morphological characteristics may improve the classification by taking into account structural modifications in cortico-subcortical loops associated with MDD [8].
Integration of morphological characteristics with cytoarchitectonic and functional information may allow better contextualization of MDD-related alterations, as demonstrated in transdiagnostic study [55], with the potential to achieve higher classification performance [56, 57]. Brain topology can be described via the connectome - a whole-brain connectivity architecture of the brain. As nodes of brain connectome exhibited elevated susceptibility to brain disorders [58], graph analytical approaches could also lead to stronger differentiability between MDD and HC. Moreover, subject-specific parcellation schemes could be applied to compute structural and functional connectomes [59], and further analyzed by suitable sophisticated classification models taking into account the neural architecture e.g., with graph neural network [60].
Data splitting and site effect
Several multi-site psychiatric neuroimaging studies directly demonstrated how different splitting strategies might introduce unwanted biases in inflated classification performances [20, 36, 61]. In Splitting by Age/Sex, trained models are unbiased regarding demographic factors; while in Splitting by Site the site affiliation is controlled, therefore we addressed the generalizability of the models applied to unseen sites. Similar to the results from our previous study [20], the classification performance of both SVM and DenseNet was higher in Splitting by Age/Sex, up to 58%, compared to Splitting by Site, close to random chance. This discrepancy indicates the existence of hidden site-related biases influencing classification performance. As this nuisance-based phenomenon appears in multi-site mega-analyses [36, 62] for its better comprehension, we strongly encourage the application of different splitting strategies in future multi-site ML studies.
The low accuracy of both models in Splitting by Site strategy is either due to the presence of a strong site-effect, hindering the ability of the models to capture diagnosis-related differences, or due to the general inability of both models to find meaningful alterations associated with MDD. Therefore, we addressed site-effect via ComBat. Thus, the possibility remains that subject-level prediction based on cortical features is unfeasible. As Combat has never been applied to vertex-wise cortical projections, we visually inspected its effect on a single pixel for every feature type (Supplementary Fig. 4). The application of ComBat resulted in more homogenous value distribution across cohorts, in line with previous studies analyzing the effects on atlas-based features [17, 20]. Nevertheless, this harmonization step did not lead to improvement in accuracies. While demographic covariates were preserved, ComBat may over-correct the data [63], causing a part of MDD-related associations to be removed along with the site-effect. Against this, more careful consideration of the site-effect is required in the future studies.
In Splitting by Age/Sex, the balanced accuracy of both models dropped (SVM: 55–48%; DenseNet: 58–56%) when ComBat was applied. The decrease of model’s performances near the levels in Splitting by Site indicates that initial higher classifications are most likely driven by site-related biases. To further validate this assumption, we performed the classification with balanced ratio between HC and MDD in every site in Splitting by Age/Sex, which resulted in close to random chance accuracies in DenseNet and SVM. Noticeably, DenseNet was less affected by the application of ComBat in the original analysis, reflecting potential non-linear site-related differences that remained in the dataset after harmonization, which is in line with previous findings [64]. Therefore, we recommend ComBat only be applied when combining more linear models, such as SVM, while more sophisticated models alone should directly incorporate site information as an additional input.
SVM vs DenseNet
Previous ML mega-analyses based on structural MDD vs HC classifications considered only shallow linear and non-linear ML models, such as SVM, penalized logistic regression and decision tree [14, 15, 20]. In this study, we extended the diagnostic classification approach by comparing the performance of shallow linear model - SVM with a linear kernel to a highly non-linear deep DenseNet classifier applied to vertex-wise cortical information. The explorative results of sex classification applied to HC revealed higher classification performance of the DenseNet compared to the SVM (Supplementary Fig. 2) for all data modalities. The higher accuracy suggests that DenseNet was able to capture non-linear sex dependencies that were present in the cortical maps. The superiority of DenseNet over SVM in the sex classification task was in line with previous study conducted on the same vertex-wise cortical maps [26]. Conversely, another large sample study revealed no advantage of using any deep architectures over simpler models in predicting demographic factors [37]; therefore, further tests in even bigger samples are required. Nevertheless, in this study both models exhibited a similar range of accuracies, close to random chance, for the main task of MDD versus HC classification. Therefore, the application of DenseNet did not yield the expected improvement for detecting combined (nor separated) structural cortical features that discriminate patients from controls.
Similar performance of the linear SVM and non-linear DenseNet model may be due to the absence of non-linear interactions between different cortical regions, significant for the MDD detection. Furthermore, the analyzed sample is highly heterogeneous in terms of demographic and clinical covariates, potentially interfering with the main task and lowering the classification performance. In this vein, there are several possible directions for improving DenseNet performance. First, the considered model was pre-trained only on natural images from ImageNet. The model could be subsequently pre-trained on cortical projections from an independent large sample using immediate task, for example predicting sex as it was performed in Gao’s study [26]. Furthermore, one could use more than one intermediate task to optimize the weights of the neural network, for example, predicting demographic or clinical covariates. This approach is broadly known as multi-task learning [65], the usefulness of which in the neuroimaging domain was already demonstrated [19, 35].
Secondly, the multi-task approach could be used to “unlearn” undesired biases. In our analysis, site-related differences were removed via ComBat. One could train the network to perform the main task while unlearning the scanner parameters, as was successfully demonstrated by Dinsdale and colleagues [66]. Furthermore, one could replace the residualization step in the same manner by making the network unlearn age and sex dependencies. In line with our previous analysis, we linearly regressed out age and sex dependencies from the cortical features using normative approach [20]. Considering the greater performance of the DenseNet model in predicting sex, we can speculate the presence of non-linear male-female differences in cortical morphology. Thus, unlearning age- and sex-related dependencies could improve classification performance.
Further strengths and limitations
Here we were interested in using a pre-trained deep learning model—specifically, DenseNet—to see if it could effectively classify major depressive disorder (MDD) from healthy brains using finer-grained, unfolded cortical surface maps, and whether such information, when combined, could offer complementary classificatory value compared to previously examined features. This approach extends the methodology of our prior study [20], where we employed more conventional structural MRI-derived features such as cortical thickness, surface area, and subcortical volumes from whole-brain regions-of-interest (ROIs). Our current approach is original and methodologically relevant, particularly in light of increasing interest in surface-based neuroimaging analyses that go far beyond standard ROI measures. And by employing more detailed cortical maps from different sources—such as sulcal depth and curvature—and projecting them in unfolded 2D space, we sought to assess whether such refinements in cortical representation could provide additional or differentially informative patterns for diagnostic classification. While the classification performance did not surpass that of previous studies, this negative finding is itself valuable, helping to delineate the boundaries of what these finer-grained representations currently offer in this domain.
Although we did not apply dimensionality reduction in the present analysis, we acknowledge that this remains a promising avenue for future research. Prior work has employed PCA, spherical harmonic decomposition [67], surface eigenmodes [68], cortical gradients [69], and deep generative models such as variational autoencoders [70] to reduce feature dimensionality while preserving meaningful structure. The potential impact of these dimensionality reduction approaches on classification performance should be explored in dedicated follow-up studies.
A potential limitation of this study is the absence of modeling based on MDD subtypes. While studies have proposed various subtyping schemes to address the clinical and biological heterogeneity of MDD, there is a wide range of subtyping approaches and most were derived from small samples (e.g., [71]), with limited replication or independent validation. For this reason, we intentionally chose not to include a subtyping step. This decision avoids reliance on uncertain stratification and reflects a key strength of the approach: classification performance could have direct clinical applicability, independent of MDD subtype definitions. Nonetheless, we acknowledge that the presence of unmodeled heterogeneity within the MDD group may have contributed to the lack of discriminative performance observed. Another important limitation is the lack of detailed ethnic and genetic information across the full sample. Sociocultural and genetic diversity are known to influence both brain morphology and disease expression, and their absence may affect the generalizability of the findings. These remain open challenges for future research aiming to enhance the specificity and robustness of neuroimaging-based classifiers for MDD. In particular, large-scale studies incorporating diverse populations and robust subtyping frameworks may offer insights with broader international applicability.
Conclusion
In this study, we tested if more advanced classification algorithms applied to high-resolution morphometric shape characteristics can improve MDD vs HC classification. Splitting the data according to demographic variables and according to site allowed a comprehensive analysis of model’s performances and biases. We detected site effects, which we addressed at least partially with the ComBat harmonization tool, but did not increase classification metrics. Both shallow and deep ML models exhibited low, close to chance accuracies. Most importantly, the integration of high-resolution cortical thickness and shape features from vertices did not lead to greater classification performance over previously analyzed atlas-based cortical features. According to our results, it seems unlikely that structural MRI alone will provide diagnostic biomarkers of MDD. Thus, further investigation is required into the classification performance applied to the fusion of other MRI modalities, including fMRI and DWI.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to site restrictions but data may be available from the corresponding sites on reasonable request.
References
Friedrich MJ. Depression is the leading cause of disability around the world. JAMA. 2017;317:1517 https://doi.org/10.1001/jama.2017.3826
Machado M, Iskedjian M, Ruiz I, Einarson TR. Remission, dropouts, and adverse drug reaction rates in major depressive disorder: a meta-analysis of head-to-head trials. Curr Med Res Opin. 2006;22:1825–37. https://doi.org/10.1185/030079906X132415
Mendlewicz J. Towards achieving remission in the treatment of depression. Dialogues Clin Neurosci. 2008;10:371–5.
Rush AJ, Trivedi MH, Wisniewski SR, Nierenberg AA, Stewart JW, Warden D, et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D report. Am J Psychiatry. 2006;163:1905–17. https://doi.org/10.1176/ajp.2006.163.11.1905
Coffey CE, Wilkinson WE, Weiner RD, Parashos IA, Djang WT, Webb MC, et al. Quantitative cerebral anatomy in depression: a controlled magnetic resonance imaging study. Arch Gen Psychiatry. 1993;50:7–16. https://doi.org/10.1001/archpsyc.1993.01820130009002
Sheline YI, Gado MH, Kraemer HC. Untreated depression and hippocampal volume loss. Am J Psychiatry. 2003;160:1516–8. https://doi.org/10.1176/appi.ajp.160.8.1516
Zhang X, Yao S, Zhu X, Wang X, Zhu X, Zhong M. Gray matter volume abnormalities in individuals with cognitive vulnerability to depression: a voxel-based morphometry study. J Affect Disord. 2012;136:443–52. https://doi.org/10.1016/j.jad.2011.11.005
Ho TC, Gutman B, Pozzi E, Grabe HJ, Hosten N, Wittfeld K, et al. Subcortical shape alterations in major depressive disorder: findings from the ENIGMA major depressive disorder working group. Hum Brain Mapp. 2022;43:341–51. https://doi.org/10.1002/hbm.24988
Schmaal L, Hibar DP, Sämann PG, Hall GB, Baune BT, Jahanshad N, et al. Cortical abnormalities in adults and adolescents with major depression based on brain scans from 20 cohorts worldwide in the ENIGMA major depressive disorder working group. Mol Psychiatry. 2017;22:900–9. https://doi.org/10.1038/mp.2016.60
Schmaal L, Veltman DJ, van Erp TGM, Sämann PG, Frodl T, Jahanshad N, et al. Subcortical brain alterations in major depressive disorder: findings from the ENIGMA major depressive disorder working group. Mol Psychiatry. 2016;21:806–12. https://doi.org/10.1038/mp.2015.69
Winter NR, Leenings R, Ernsting J, Sarink K, Fisch L, Emden D, et al. Quantifying Deviations of Brain Structure and Function in Major Depressive Disorder Across Neuroimaging Modalities. JAMA Psychiatry. 2022;79:879–88.
Gao S, Calhoun VD, Sui J. Machine learning in major depression: from classification to treatment outcome prediction. CNS Neurosci Ther. 2018;24:1037–52. https://doi.org/10.1111/cns.13048
Kambeitz J, Cabral C, Sacchet MD, Gotlib IH, Zahn R, Serpa MH, et al. Detecting neuroimaging biomarkers for depression: a meta-analysis of multivariate pattern recognition studies. Biol Psychiatry. 2017;82:330–8. https://doi.org/10.1016/j.biopsych.2016.10.028
Flint C, Cearns M, Opel N, Redlich R, Mehler DMA, Emden D, et al. Systematic misestimation of machine learning performance in neuroimaging studies of depression. Neuropsychopharmacology. 2021;46:1510–7. https://doi.org/10.1038/s41386-021-01020-7
Stolicyn A, Harris MA, Shen X, Barbu MC, Adams MJ, Hawkins EL, et al. Automated classification of depression from structural brain measures across two independent community-based cohorts. Hum Brain Mapp. 2020;41:3922–37. https://doi.org/10.1002/hbm.25095
Solanes A, Palau P, Fortea L, Salvador R, González-Navarro L, Llach CD, et al. Biased accuracy in multisite machine-learning studies due to incomplete removal of the effects of the site. Psychiatry Res Neuroimaging. 2021;314:111313 https://doi.org/10.1016/j.pscychresns.2021.111313
Pomponio R, Erus G, Habes M, Doshi J, Srinivasan D, Mamourian E, et al. Harmonization of large MRI datasets for the analysis of brain imaging patterns throughout the lifespan. Neuroimage. 2020;208:116450 https://doi.org/10.1016/j.neuroimage.2019.116450
Radua J, Vieta E, Shinohara R, Kochunov P, Quidé Y, Green MJ, et al. Increased power by harmonizing structural MRI site differences with the ComBat batch adjustment method in ENIGMA. Neuroimage. 2020;218:116956 https://doi.org/10.1016/j.neuroimage.2020.116956
Ma Q, Zhang T, Zanetti MV, Shen H, Satterthwaite TD, Wolf DH, et al. Classification of multi-site MR images in the presence of heterogeneity using multi-task learning. Neuroimage Clin. 2018;19:476–86. https://doi.org/10.1016/j.nicl.2018.04.037
Belov V, Erwin-Grabner T, Aghajani M, Aleman A, Amod AR, Basgoze Z, et al. Multi-site benchmark classification of major depressive disorder using machine learning on cortical and subcortical measures. Sci Rep. 2024;14:1084 https://doi.org/10.1038/s41598-023-47934-8
Kremen WS, Prom-Wormley E, Panizzon MS, Eyler LT, Fischl B, Neale MC, et al. Genetic and environmental influences on the size of specific brain regions in midlife: the VETSA MRI study. Neuroimage. 2010;49:1213–23. https://doi.org/10.1016/j.neuroimage.2009.09.043
White T, Andreasen NC, Nopoulos P. Brain volumes and surface morphology in monozygotic twins. Cereb Cortex. 2002;12:486–93. https://doi.org/10.1093/cercor/12.5.486
Depping MS, Thomann PA, Wolf ND, Vasic N, Sosic-Vasic Z, Schmitgen MM, et al. Common and distinct patterns of abnormal cortical gyrification in major depression and borderline personality disorder. Eur Neuropsychopharmacol. 2018;28:1115–25. https://doi.org/10.1016/j.euroneuro.2018.07.100
Zhang Y, Yu C, Zhou Y, Li K, Li C, Jiang T. Decreased gyrification in major depressive disorder. Neuroreport. 2009;20:378–80. https://doi.org/10.1097/WNR.0b013e3283249b34
Li J, Seidlitz J, Suckling J, Fan F, Ji GJ, Meng Y, et al. Cortical structural differences in major depressive disorder correlate with cell type-specific transcriptional signatures. Nat Commun. 2021;12:1647 https://doi.org/10.1038/s41467-021-21943-5
Gao K, Fan Z, Su J, Zeng LL, Shen H, Zhu J, et al. Deep transfer learning for cerebral cortex using area-preserving geometry mapping. Cereb Cortex. 2021;31:3953–65. https://doi.org/10.1093/cercor/bhab394
Nixon NL, Liddle PF, Nixon E, Worwood G, Liotti M, Palaniyappan L. Biological vulnerability to depression: linked structural and functional brain network findings. Br J Psychiatry. 2014;204:283–9. https://doi.org/10.1192/bjp.bp.113.129965
Long J, Xu J, Wang X, Li J, Rao S, Wu H, et al. Altered local gyrification index and corresponding functional connectivity in medication-free major depressive disorder. Front Psychiatry. 2020;11:585401 https://doi.org/10.3389/fpsyt.2020.585401
Kang Y, Kang W, Kim A, Tae WS, Ham BJ, Han KM. Decreased cortical gyrification in major depressive disorder. Psychol Med. 2023;53:7512–24. https://doi.org/10.1017/S0033291723001216
Shen X, Reus LM, Cox SR, Adams MJ, Liewald DC, Bastin ME, et al. Subcortical volume and white matter integrity abnormalities in major depressive disorder: findings from UK Biobank imaging data. Sci Rep. 2017;7:5547 https://doi.org/10.1038/s41598-017-05507-6
Shen A, Shi K, Xia Q, Gong W, Huang Y, Wang Y, et al. Surface-based analysis of early cortical gyrification and thickness alterations in treatment-naïve, first-episode depressive patients during emerging adulthood. J Affect Disord. 2025;372:402–8. https://doi.org/10.1016/j.jad.2024.12.003
Cruz RS, Lebrat L, Bourgeat P, Fookes C, Fripp J, Salvado O DeepCSR: a 3D deep learning approach for cortical surface reconstruction. Proc IEEE/CVF Winter Conf Appl Comput Vis. 2021;806–15. https://doi.org/10.48550/arXiv.2010.11423
Henschel L, Conjeti S, Estrada S, Diers K, Fischl B, Reuter M. FastSurfer: a fast and accurate deep learning based neuroimaging pipeline. Neuroimage. 2020;219:117012 https://doi.org/10.1016/j.neuroimage.2020.117012
Williams LZJ, Fawaz A, Glasser MF, Edwards AD, Robinson EC Geometric deep learning of the Human Connectome Project multimodal cortical parcellation. In: Abdulkadir A, Kia SM, Habes M, Kumar V, Rondina JM, Tax C, Wolfers T, eds. Machine learning in clinical neuroimaging, lecture notes in computer science. Cham: Springer; 2021. pp. 103-12. https://doi.org/10.1007/978-3-030-87586-2_11
Pinaya WHL, Mechelli A, Sato JR. Using deep autoencoders to identify abnormal brain structural patterns in neuropsychiatric disorders: a large-scale multi-sample study. Hum Brain Mapp. 2019;40:944–54. https://doi.org/10.1002/hbm.24423
Qin K, Lei D, Pinaya WHL, Pan N, Li W, Zhu Z, et al. Using graph convolutional network to characterize individuals with major depressive disorder across multiple imaging sites. EBioMedicine. 2022;78:103977 https://doi.org/10.1016/j.ebiom.2022.103977
Schulz MA, Yeo BTT, Vogelstein JT, Mourao-Miranada J, Kather JN, Kording K, et al. Different scaling of linear models and deep learning in UK Biobank brain images versus machine-learning datasets. Nat Commun. 2020;11:4235 https://doi.org/10.1038/s41467-020-18037-z
Wen J, Thibeau-Sutre E, Diaz-Melo M, Samper-González J, Routier A, Bottani S, et al. Convolutional neural networks for classification of Alzheimer’s disease: overview and reproducible evaluation. Med Image Anal. 2020;63:101694 https://doi.org/10.1016/j.media.2020.101694
Yan W, Calhoun V, Song M, Cui Y, Yan H, Liu S, et al. Discriminating schizophrenia using recurrent neural network applied on time courses of multi-site fMRI data. EBioMedicine. 2019;47:543–52. https://doi.org/10.1016/j.ebiom.2019.08.023
LeCun Y, Bottou L, Bengio Y, Haffner P. Gradient-based learning applied to document recognition. Proc IEEE. 1998;86:2278–324. https://doi.org/10.1109/5.726791
Seong SB, Pae C, Park HJ. Geometric convolutional neural network for analyzing surface-based neuroimaging data. Front Neuroinform. 2018;12:42 https://doi.org/10.3389/fninf.2018.00042
Su Z, Wang Y, Shi R, Zeng W, Sun J, Luo F, et al. Optimal mass transport for shape matching and comparison. IEEE Trans Pattern Anal Mach Intell. 2015;37:2246–59. https://doi.org/10.1109/TPAMI.2015.2408346
Huang G, Liu Z, Van Der Maaten L, Weinberger KQ Densely connected convolutional networks. In: Proc IEEE Conf Comput Vis Pattern Recognit (CVPR). IEEE; 2017;2261-9. https://doi.org/10.1109/CVPR.2017.243
Lu X, Yang Y, Wu F, Gao M, Xu Y, Zhang Y, et al. Discriminative analysis of schizophrenia using support vector machine and recursive feature elimination on structural MRI images. Medicine (Baltimore). 2016;95:e3973 https://doi.org/10.1097/MD.0000000000003973
Sacchet MD, Prasad G, Foland-Ross LC, Thompson PM, Gotlib IH. Support vector machine classification of major depressive disorder using diffusion-weighted neuroimaging and graph theory. Front Psychiatry. 2015;6:21 https://doi.org/10.3389/fpsyt.2015.00021
Wottschel V, Chard DT, Enzinger C, Filippi M, Frederiksen JL, Gasperini C, et al. SVM recursive feature elimination analyses of structural brain MRI predicts near-term relapses in patients with clinically isolated syndromes suggestive of multiple sclerosis. Neuroimage Clin. 2019;24:102011 https://doi.org/10.1016/j.nicl.2019.102011
Dinga R, Penninx B, Veltman D, Schmaal L, Marquand A Beyond accuracy: measures for assessing machine learning models, pitfalls and guidelines. bioRxiv: [Preprint]. 2019. Available from: https://doi.org/10.1101/743138
Kohoutová L, Heo J, Cha S, Lee S, Moon T, Wager TD, et al. Toward a unified framework for interpreting machine-learning models in neuroimaging. Nat Protoc. 2020;15:1399–435. https://doi.org/10.1038/s41596-019-0289-5
Deng J, Dong W, Socher R, Li LJ, Li K, Fei-Fei L ImageNet: a large-scale hierarchical image database. In: Proc IEEE Conf Comput Vis Pattern Recognit (CVPR). IEEE; 2009. 248-55. https://doi.org/10.1109/CVPR.2009.5206848
Zhang Y, Jenkins DF, Manimaran S, Johnson WE. Alternative empirical Bayes models for adjusting for batch effects in genomic studies. BMC Bioinformatics. 2018;19:262 https://doi.org/10.1186/s12859-018-2263-6
Demirci N, Holland MA. Cortical thickness systematically varies with curvature and depth in healthy human brains. Hum Brain Mapp. 2022;43:2064–84. https://doi.org/10.1002/hbm.25776
Ho TC, Sisk LM, Kulla A, Teresi GI, Hansen MM, Wu H, et al. Sex differences in myelin content of white matter tracts in adolescents with depression. Neuropsychopharmacology. 2021;46:2295–303. https://doi.org/10.1038/s41386-021-01078-3
Sacchet MD, Gotlib IH. Myelination of the brain in major depressive disorder: an in vivo quantitative magnetic resonance imaging study. Sci Rep. 2017;7:2200 https://doi.org/10.1038/s41598-017-02062-y
van Velzen L, Kelly S, Isaev D, Aleman A, Aftanas L, Bauer J, et al. White matter disturbances in major depressive disorder: a coordinated analysis across 20 international cohorts in the ENIGMA MDD working group. Mol Psychiatry. 2020;25:1511–25. https://doi.org/10.1038/s41380-019-0477-2
Hettwer MD, Larivière S, Park BY, van den Heuvel OA, Schmaal L, Andreassen OA, et al. Coordinated cortical thickness alterations across six neurodevelopmental and psychiatric disorders. Nat Commun. 2022;13:6851 https://doi.org/10.1038/s41467-022-34367-6
Ayyash S, Davis AD, Alders GL, MacQueen G, Strother SC, Hassel S, et al. Exploring brain connectivity changes in major depressive disorder using functional-structural data fusion: a CAN-BIND-1 study. Hum Brain Mapp. 2021;42:4940–57. https://doi.org/10.1002/hbm.25590
Zhang YD, Dong Z, Wang SH, Yu X, Yao X, Zhou Q, et al. Advances in multimodal data fusion in neuroimaging: overview, challenges, and novel orientation. Inf Fusion. 2020;64:149–87. https://doi.org/10.1016/j.inffus.2020.07.006
Fornito A, Zalesky A, Breakspear M. The connectomics of brain disorders. Nat Rev Neurosci. 2015;16:159–72. https://doi.org/10.1038/nrn3901
Wig GS, Laumann TO, Cohen AL, Power JD, Nelson SM, Glasser MF, et al. Parcellating an individual subject’s cortical and subcortical brain structures using snowball sampling of resting-state correlations. Cereb Cortex. 2014;24:2265–78. https://doi.org/10.1093/cercor/bht056
Zhou J, Cui G, Zhang Z, Yang C, Liu Z, Wang L, et al. Graph neural networks: a review of methods and applications. arXiv:1812.08434. [Preprint]. 2019. https://doi.org/10.1016/j.aiopen.2021.01.001
Mårtensson G, Ferreira D, Granberg T, Cavallin L, Oppedal K, Padovani A, et al. The reliability of a deep learning model in clinical out-of-distribution MRI data: a multicohort study. Med Image Anal. 2020;66:101714 https://doi.org/10.1016/j.media.2020.101714
Nakano T, Takamura M, Ichikawa N, Okada G, Okamoto Y, Yamada M, et al. Enhancing multi-center generalization of machine learning-based depression diagnosis from resting-state fMRI. Front Psychiatry. 2020;11:594865 https://doi.org/10.3389/fpsyt.2020.594865
Bayer JMM, Thompson PM, Ching CRK, Liu M, Chen A, Panzenhagen AC, et al. Site effects how-to and when: an overview of retrospective techniques to accommodate site effects in multi-site neuroimaging analyses. Front Neurol. 2022;13:923988 https://doi.org/10.3389/fneur.2022.923988
Solanes A, Gosling CJ, Fortea L, Ortuño M, Lopez-Soley E, Llufriu S, et al. Removing the effects of the site in brain imaging machine-learning – measurement and extendable benchmark. Neuroimage. 2022;263:119800 https://doi.org/10.1016/j.neuroimage.2022.119800
Caruana R. Multitask learning. Mach Learn. 1997;28:41–75. https://doi.org/10.1023/A:1007379606734
Dinsdale N, Jenkinson M, Namburete A. Deep learning-based unlearning of dataset bias for MRI harmonisation and confound removal. Neuroimage. 2020;228:117689 https://doi.org/10.1016/j.neuroimage.2020.117689
Thompson PM, Toga AW. A surface-based technique for warping three-dimensional images of the brain. IEEE Trans Med Imaging. 1996;15:402–17. https://doi.org/10.1109/42.511745
Müller EJ, Munn BR, Aquino KM, Shine JM, Robinson PA. The music of the hemispheres: cortical eigenmodes as a physical basis for large-scale brain activity and connectivity patterns. Front Hum Neurosci. 2022;16:1062487 https://doi.org/10.3389/fnhum.2022.1062487
Margulies DS, Ghosh SS, Goulas A, Falkiewicz M, Huntenburg JM, Langs G, et al. Situating the default-mode network along a principal gradient of macroscale cortical organization. Proc Natl Acad Sci USA. 2016;113:12574–19. https://doi.org/10.1073/pnas.1608282113
Zhu X, Kim Y, Ravid O, He X, Suarez-Jimenez B, Zilcha-Mano S, et al. Neuroimaging-based classification of PTSD using data-driven computational approaches: a multisite big data study from the ENIGMA-PGC PTSD consortium. Neuroimage. 2023;283:120412 https://doi.org/10.1016/j.neuroimage.2023.120412
Yu C, Arcos-Burgos M, Licinio J, Wong ML. A latent genetic subtype of major depression identified by whole-exome genotyping data in a Mexican-American cohort. Transl Psychiatry. 2017;7:e1134 https://doi.org/10.1038/tp.2017.102
Acknowledgements
We would like to sincerely thank Vladimir Belov for his invaluable contributions to this work. ENIGMA MDD: This work was supported by NIH grants U54 EB020403 (PMT), R01MH116147 (PMT), and R01 MH117601 (NJ & LS), and the NSFC grants 61722313 (LLZ), and 62036013 (LLZ). LH was funded by the Rubicon award (grant number 452020227) from the Dutch NOW. AFFDIS: This study was funded by the University Medical Center Göttingen (UMG Startförderung) and VB and RGM are supported by German Federal Ministry of Education and Research (Bundesministerium für Bildung und Forschung, BMBF: 01 ZX 1507, “PreNeSt - e:Med”). Calgary: This study was supported by Alberta Children’s Hospital Foundation, Canadian Institutes for Health Research. Cardiff: This work was supported by a Medical Research Council (G 1100629) grant to DEJ Linden and a PhD studentship by Health Research Wales (HS/14/20) for DMEM. CSAN: This work was supported by grants from Johnson & Johnson Innovation (S.E.), the Swedish Medical Research Council (S.E.: 2017–00875, M.H.: 2013–07434, 2019–01138), the ALF Grants, Region Östergötland M.H., J.P.H.), National Institutes of Health (R.D.: R01 CA193522 and R01 NS073939), MD Anderson Cancer Support Grant (R.D.: P30CA016672). Dep-arrest clin: BCD is supported by a NHMRC CJ Martin fellowship (app 1161356). DCHS: supported by the Medical Research Council of South Africa. The DCHS was funded by the Bill and Melinda Gates Foundation (OPP1017641), and received additional support from the South African Medical Research Council. ENIGMA Central/USC: This work was supported by the National Natural Science Foundation of China (61722313 and 62036013). ETPB: Funding for this work was provided by the Intramural Research Program at the National Institute of Mental Health, National Institutes of Health (IRP-NIMH-NIH; ZIA-MH002857), by a NARSAD Independent Investigator to Dr. Zarate, and by a Brain & Behavior Mood Disorders Research Award to Dr. Zarate. Suported by the NIMH Intramural Research Program. FIDMAG: This work was supported by the Generalitat de Catalunya (2014 SGR 1573) and Instituto de Salud Carlos III (CPII16/00018) and (PI14/01151 and PI14/01148). PFC was supported by a Sara Borrell grant (CD19/00149, Instituto de Salud Carlos III) and a fellowship from “la Caixa” Foundation (ID 100010434, fellowship code LCF/BQ/PR22/11920017). FOR2107-Marburg: This work was funded by the German Research Foundation (DFG grant FOR2107, speaker Tilo Kircher KI588/14-1, KI588/14-2, KI588/20-1, KI588/22-1 to Tilo Kircher, NE 2254/1-2 to Igor Nenadic, and SFB/TRR 393, speaker Tilo Kircher, project grant no 521379614). FOR2107-Muenster: This work was funded by the German Research Foundation (DFG), Udo Dannlowski (co-speaker FOR2107, DA 1151/5-1, DA 1151/5-2, DA1151/9-1, DA1151/10-1 and DA1151/11-1, and SFB/TRR 393, project grant no 521379614) and the Interdisciplinary Center for Clinical Research (IZKF) of the medical faculty of Münster (grant Dan3/022/22 to UD). Houston: JCS has received research grants from Compass, Alkermes, and Allergan. Melbourne: This work was supported by National Health and Medical Research Council of Australia (NHMRC) Project Grants (1064643) to BJH and to CGD (1024570). Minnesota: The study was funded by the National Institute of Mental Health (K23MH090421), the National Alliance for Research on Schizophrenia and Depression, the University of Minnesota Graduate School, the Minnesota Medical Foundation, and the Biotechnology Research Center (P41 RR008079 to the Center for Magnetic Resonance Research), University of Minnesota, and the Deborah E. Powell Center for Women’s Health Seed Grant, University of Minnesota. Modal dilemma: This study was supported by the Brain and Behavior Research Foundation and by the National Health and Medical Research Council ID 1125504 to SLW. Munster: This work was funded by the German Research Foundation (SFB-TRR58, Project C09 to UD). NESDA: This study was supported by the Brain and Behavior Research Foundation and by the National Health and Medical Research Council ID 1125504 to SLW. QTIM: The QTIM dataset was supported by the Australian National Health and Medical Research Council (Project Grants No. 496682 and 1009064) and US National Institute of Child Health and Human Development (R01 HD050735). Singapore: KS was supported by National Healthcare Group, Singapore (SIG/15012) for the project. Stanford: IHG is supported in part by National Institutes of Health (R37MH101495). MDS is supported by the National Institute of Mental Health (Project Number R01MH125850), Dimension Giving Fund, Ad Astra Chandaria Foundation, Brain and Behavior Research Foundation (Grant Number 28972), BIAL Foundation (Grant Number 099/2020), Emergence Benefactors, The Ride for Mental Health, and Gatto Foundation. USFC, TIGER: UCSF Weill Institute for Neurosciences Weill Award for Investigators in the Neurosciences Impacted by COVID-19 Setbacks to TTY; this work was supported by the National Center for Complementary and Integrative Health (NCCIH) R21AT009173, R61AT009864, and 4R33AT009864-03 to TTY, by the National Center for Advancing Translational Sciences (CTSI), National Institutes of Health, through UCSF-CTSI UL1TR001872 to TTY, by the American Foundation for Suicide Prevention (AFSP) SRG-1-141-18 to TTY, by UCSF Research Evaluation and Allocation Committee (REAC) and J. Jacobson Fund to TTY, by the National Institute of Mental Health (NIMH) R01MH085734 and by the Brain and Behavior Research Foundation (formerly NARSAD) to TTY. Support for the TIGER study includes the Klingenstein Third Generation Foundation the National Institute of Mental Health K01MH117442, the Stanford Maternal Child Health Research Institute and the Stanford Center for Cognitive and Neurobiological Imaging; TCH receives partial support from the Ray and Dagmar Dolby Family Fund. TCH: This work is supported in part by the National Institute of Mental Health (K01MH117442), the Klingenstein Third Generation Foundation, Stanford Maternal Child Research Institute (Early Career Award, and K Support Award), the UCSF Research Evaluation and Allocation Committee (REAC), the Raschen-Tiedeman Fund, and the Moffitt Memorial Fund. SHIP is part of the Community Medicine Research net of the University of Greifswald, Germany, which is funded by the Federal Ministry of Education and Research (grants no. 01ZZ9603, 01ZZ0103, and 01ZZ0403), the Ministry of Cultural Affairs and the Social Ministry of the Federal State of Mecklenburg-West Pomerania. MRI scans in SHIP and SHIP-TREND have been supported by a joint grant from Siemens Healthineers, Erlangen, Germany and the Federal State of Mecklenburg-West Pomerania.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Consortia
Contributions
RGM conceived and designed the study, acquired, analyzed, and interpreted the data, and drafted the manuscript. TEG, LLZ, CRKC, AA, ARA, ZB, FB, BB, KB, RB, RC, CGC, EC, BCD, KC, UD, CGD, AD, JE, JWE, LF, PFC, ASG, IHG, HJG, NAG, DG, TH, JPH, LKMH, BJH, TCH, NJ, AJJ, AK, TK, BKD, SMK, TL, RL, ML, DEJL, FPM, DMAM, SM, EM, BAM, BM, IN, AO, YO, MLO, BWJHP, SP, EPC, MJP, JR, ERC, MDS, RS, AS, KS, JCS, DJST, FS, AS, SIT, YJT, AU, EV, YVG, HV, MW, HCW, SW, NW, KW, MJW, MJWu, TTY, CZ, EP, DJV, LS, and PMT acquired data, contributed to data analysis or interpretation, revised the manuscript for important intellectual content, and approved the final version for submission. LS and PMT helped conceive and design the study and supervised the project.
Corresponding author
Ethics declarations
Competing interests
PMT and NJ received a research grant from Biogen, Inc. for research unrelated to this manuscript. HJG has received travel grants and speakers’ honoraria from Fresenius Medical Care, Neuraxpharm, Servier and Janssen Cilag as well as research funding from Fresenius Medical Care unrelated to this manuscript. JCS has served as a consultant for Pfizer, Sunovion, Sanofi, Johnson & Johnson, Livanova, and Boehringer Ingelheim. The remaining authors declare no conflict of interest.
Ethics approval and consent to participate
The study was approved by the Ethics Committee of the University Medical Center Göttingen (UMG), Germany. The study was approved by the Ethics Committee of the University Medical Center Göttingen (UMG), Germany. In accordance with the current version of the Declaration of Helsinki, all methods in the participating cohorts were approved by the respective institutional review boards and local ethics committees, and written informed consent was obtained from all participants. For participants under 18 years of age, written informed consent was additionally provided by a parent and/or legal guardian.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Goya-Maldonado, R., Erwin-Grabner, T., Zeng, LL. et al. Classification of major depressive disorder using vertex-wise brain sulcal depth, curvature, and thickness with a deep and a shallow learning model. Mol Psychiatry (2025). https://doi.org/10.1038/s41380-025-03273-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41380-025-03273-w