Abstract
Fetal intracerebral hemorrhage is increasingly recognized on prenatal imaging. In this review, we discuss clinically relevant aspects of fetal intracerebral hemorrhage, including germinal matrix-intraventricular hemorrhage, as well as intraparenchymal hemorrhage. We discuss current clinical practice for prenatal counseling and postnatal management of fetal intracerebral hemorrhage, and offer practical recommendations for clinicians. We propose standardized terminology for classification of fetal intracerebral hemorrhage to be used in future research. We also highlight gaps in the literature and priorities for future research, namely the need for prospective large-scale studies to better understand underlying etiologies and neurodevelopmental outcomes in fetal intracerebral hemorrhage.
Impact statement
-
We discuss the diverse etiologies and outcomes of fetal intracerebral hemorrhage, and propose standardized terminology for classification.
-
We outline current practice and offer practical recommendations for management and counseling of fetal intracerebral hemorrhage, recognizing the need for capacity-building in the newly emerging subspecialty of fetal neurology.
-
We highlight gaps in the literature and research priorities in fetal intracerebral hemorrhage to promote collaborative research, and the development of interventions to improve pregnancy and child outcomes.
Similar content being viewed by others
Introduction
Intracranial hemorrhage (ICH) is increasingly diagnosed prenatally, in part due to the increasing availability and use of advanced prenatal diagnostic imaging.1 The timing of diagnosis of fetal ICH depends on the timing of hemorrhage, timing of imaging, indication for imaging, type of imaging, and whether there are conditions such as maternal trauma or illness. Often, the discovery of fetal ICH may be incidental.2 Fetal ICH can occur in different compartments, including epidural, subdural, subarachnoid, subpial, intraparenchymal, and intraventricular.3,4
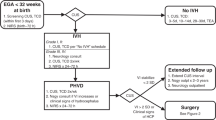
In this review, we will cover clinically relevant aspects of fetal intracerebral hemorrhage, specifically intraparenchymal hemorrhage (IPH), as well as germinal matrix-intraventricular hemorrhage (GMH-IVH) and its sequelae like periventricular hemorrhagic infarction (PVHI) (Fig. 1). We propose standardized terminology for classification of fetal intracerebral hemorrhage for use in future research. We also highlight gaps in the available fetal ICH literature to guide future research. Last, we discuss the state of current clinical practice and provide practical guidance for prenatal counseling and postnatal management of fetal intracerebral hemorrhage, recognizing the need for capacity-building in the newly emerging subspecialty of fetal neurology.5
a–c Intraventricular Hemorrhage (IVH); d–f Intraparenchymal Hemorrhage (IPH) without intraventricular hemorrhage. a Isolated intraventricular hemorrhage such as germinal matrix hemorrhage (GMH-IVH; arrow). b Intraventricular hemorrhage (solid arrow) with subsequent periventricular hemorrhagic infarction (PVHI; dotted arrow). c Intraventricular hemorrhage (solid arrow) with separate area of intraparenchymal hemorrhage (dotted arrow). d Intraparenchymal hemorrhage (dotted arrow) associated with a cerebral sinovenous thrombosis (CSVT), also known as a dural venous sinus thrombosis (DVST; solid open arrow). e Intraparenchymal hemorrhage (dotted arrow) in an arterial distribution suspicious for hemorrhagic transformation of an arterial infarct (Fetal Arterial Ischemic Stroke; FAIS). f intraparenchymal hemorrhage not associated with IVH, clot, nor consistent with hemorrhagic transformation of an arterial infarct suspected to be an idiopathic hemorrhage (Fetal Hemorrhagic Stroke; FHS). Illustrations are meant to reflect anatomy at ~25 gestational weeks. Refer to Fig. 2 for the corresponding proposed classification flowchart.
Terminology and classification
Defining specific patterns and subtypes of fetal intracerebral hemorrhage for prenatal application is necessary to advance understanding of pathophysiology, risk factors, and outcomes, including recurrence risk. A lack of consistency in the terminology used in the literature for different types of fetal ICH is a rate-limiting step in the advancement of our understanding of the underlying causes. The terminology used in this review for different patterns of fetal ICH are defined in Table 1.
We highlight GMH-IVH with subsequent PVHI as a distinct entity from IPH to emphasize the different risk factors and pathophysiology (Fig. 1). It is important to acknowledge that in the setting of severe and multiple areas of hemorrhage, it may not be possible to distinguish GMH-IVH with subsequent venous infarction with hemorrhage, and GMH-IVH associated with parenchymal hemorrhage by virtue of the same underlying etiology.
In order to provide a standardized fetal ICH classification, we propose a consensus-based approach to classifying fetal PVHI and IPH (Fig. 2). Our first proposed branch point is the presence of intraventricular blood, which may indicate a GMH-IVH, and then whether there is any parenchymal hemorrhage, and whether it is in the classic location for PVHI (periventricular) or distant from the ventricle, which would suggest a separate area of involvement. In the absence of intraventricular blood, we propose three categories based on pattern and etiology if these are possible to determine: primary parenchymal hemorrhage without communication with the lateral ventricle, venous hemorrhagic infarct, or arterial ischemic infarct with hemorrhagic transformation with lesions that do not communicate with the ventricle. Distinguishing these categories may only be possible on postnatal imaging, if ever.
Epidemiology
The incidence of many fetal neurological conditions is difficult to determine due to the lack of population-based screening after 20 gestational weeks. In many parts of the world, standardized ultrasound anatomy scans are performed at 18–20 gestational weeks, which may be the last time fetal imaging of the pregnancy is performed. Additional ultrasounds may be performed for specific concerns, such as fetal growth, trauma, vaginal bleeding, or a high-risk pregnancy due to multiple gestation, hypertension, diabetes, or other maternal conditions. There are limited epidemiologic data on fetal intracerebral hemorrhage, and studies predominantly report a subset of higher risk pregnancies. Furthermore, different types of fetal intracerebral or even ICH are often combined. Another challenge is that the fetal incidence and birth prevalence may differ given not every fetus with fetal intracerebral hemorrhage will be live born.3
Available data estimate an incidence for fetal ICH between 0.1 and 1/1000 pregnancies,6,7,8 while birth prevalence from one 2006 study was estimated to be 0.17–0.35/1000 live births.9
Etiopathogenesis
Diverse causes underlie fetal intracerebral hemorrhage (Table 2) suggesting heterogenous pathophysiology. Recognized causes include congenital infections (i.e., cytomegalovirus, parvovirus B19), autoantibody conditions such as fetal and neonatal autoimmune thrombocytopenia (FNAIT), maternal trauma, cerebral sinovenous thrombosis (CSVT, also known as dural venous sinus thrombosis (DVST)), deep medullary vein thrombosis,10 and coagulopathies such as those due to von Willebrand Factor,11 congenital factor deficiency (i.e., Factor X), or congenital amegakaryocytic thrombocytopenia due to MPL variant.12,13,14 IPH can also be due to genetic conditions that affect blood vessel integrity such as collagen vascular disorders, and the most frequently identified is COL4A1/2. Increasingly, a variety of monogenic causes are recognized to underlie a broad spectrum of pediatric cerebrovascular disease and vascular malformations, such as ACTA2, RASA1, and FOXC1, which can have a perinatal presentation.15 In one retrospective single-center study of fetal IPH, genetic disorders were more common (9/44) than congenital infection (2/44) and FNAIT (1/44), and the yield of genetic testing was 39% (9/23).16 In contrast, a recent single-center study of fetal cerebellar hypoplasia due to hemorrhage reported acquired etiologies like parvovirus B19 and FNAIT were common, but there were no known cases with genetic etiologies.17 Other small series of prenatally detected cerebellar hemorrhage have also reported parvovirus and intrauterine transfusion for fetal anemia as frequently identified etiologies16,18,19; however, a cause is not identified in many of the reported cases.19 A retrospective multicenter study of FNAIT reported fetal ICH as a complication in 43/592 (7%) pregnancies.20
The pathophysiology of fetal GMH-IVH has not been established. In the preterm population, GMH-IVH reflects the sensitivity of the highly vascular and friable germinal matrix to perturbations in blood flow and systemic blood pressure. Most commonly in the lateral ventricles, GMH-IVH is also frequently seen in the cerebellum of preterm infants. After 32–34 weeks the germinal matrix typically involutes, meaning that GMH-IVH is an injury typically diagnosed before 32–34 weeks’ gestation. An important exception to this timeline includes congenital anomalies and genetic syndromes that may delay germinal matrix maturity. For instance, congenital heart disease has been shown to delay germinal matrix maturity by ~2 weeks.21 However, the applicability and relevance of the pathophysiologic mechanisms of GMH-IVH in preterm infants to fetuses is not known. Despite this knowledge gap, potential complications of fetal GMH-IVH appear similar to preterm GMH-IVH.22 The complications of fetal GMH-IVH include post-hemorrhagic ventricular dilatation (PHVD) and PVHI, a venous infarction of the medullary veins that drain the white matter due to congestion at the level of the germinal matrix.23,24 When diagnosed remote from the timing of occurrence with chronic changes on MRI, PVHI is sometimes referred to as periventricular venous infarction. Commonly diagnosed on neuroimaging obtained in infancy or childhood following presentation with early handedness or motor asymmetry, remote PVHI can also be identified on prenatal imaging.25 When detected in a child that was born at term, the timing of the GMH-IVH and PVHI is presumed to be antenatal; however, in the absence of serial prenatal and postnatal imaging, determination of the precise timing of a remote venous hemorrhagic infarction cannot be made with certainty. Improved detection of intracerebral hemorrhage prenatally may shed light on this subgroup of children.
Vascular malformations
Developmental vascular malformations merit specific mention and underscore the importance of accurate diagnosis to inform prenatal counseling and care. Dural sinus malformations (DSMs) are rare vascular malformations in fetuses and infants characterized by venous lakes at the involved dural sinuses, often the torcula, commonly associated with thrombus that can be extensive. Of reported cases of prenatally and postnatally diagnosed torcular DSM (tDSM), parenchymal hemorrhage is present in 8/77 (10%) and other parenchymal injury suggesting prior ischemia in 14/63 (22%).26 Natural history data indicate that fetal tDSMs spontaneously involuted in 38/39 cases (97%) with continuation of pregnancy, with 5/38 (13%) initially increasing in size prior to spontaneous involution.26,27
Vein of Galen malformations (VGMs) occur when the anterior part of the prosencephalic vein of Markowski does not disappear in its usual developmental course, and instead enlarges due to high pressure of the choroidal feeders, forming a vascular malformation. Diffuse parenchymal injury and hemorrhage have been reported in VGMs.28 A recent systematic review of prenatally diagnosed VGMs reports 51 cases from 31 papers, though fetal MRI findings were not reported.29
Risk factors
Risk factors for fetal intracerebral hemorrhage are challenging to discern because of ascertainment bias due to the indication for fetal imaging. As above, a variety of potential fetal and maternal concerns may prompt additional imaging beyond the 20-week anatomy scan, and therefore may appear to be associated with fetal ICH without a causal link.
Male sex has been identified as a risk factor for fetal hemorrhage to varying degrees. In a systematic review of fetal GMH-IVH, the sex proportion among those with PVHI was equal.22 The proportions of males in several articles of fetal ICH (including extracerebral hemorrhage), have ranged from 57 to 77%.2,16,30 In delivered preterm infants, a preponderance of males with GMH-IVH and those with PVHI is acknowledged.23,24 Similarly, in term-born children diagnosed with remote PVHI, males are over-represented.31 Sex effects are also reported in animal models of perinatal hemorrhage and stroke,32 underscoring the importance of understanding how sex effects may influence the risk of hemorrhage, as well as outcomes.
Possible risk factors for fetal PVHI were evaluated in a systematic review of 80 studies comprising 105 fetuses with PVHI, including twin pregnancy, congenital anomalies, small for gestational age and/or intrauterine growth restriction. In over one-third there were no associated abnormalities.22 Twin-twin transfusion syndrome and intrauterine transfusion are common risk factors for fetal IPH.16
Neuroimaging
Prenatal sonography
The most common sonographic finding when fetal intracerebral hemorrhage is present is ventriculomegaly. The blood clot in GMH appears as an echogenic collection similar to the normal choroid plexus, and may be adherent to choroid plexus or separate.33 It can be challenging to estimate the amount of intraventricular blood present due to fetal motion, though more severe GMH-IVH tends to be associated with enlargement of the lateral ventricles over time. Progressive development of complex texture is typical over subsequent days, such as hyperechoic nodular ependyma or irregular, or heterogeneous echogenicity of the choroid plexus.33 Small GMH typically resolve spontaneously over time. Depending on the time interval between PVHI or IPH occurrence and ultrasound detection, there may be findings of increased echogenicity in the periventricular white matter or parenchyma, or evidence of cystic evolution and porencephaly.33,34 Fetal cerebellar hemorrhage in particular may be underestimated due to technical challenges in assessing the posterior fossa prenatally. Often when detected by ultrasound, fetal cerebellar hemorrhage is unilateral and associated with cerebellar hypoplasia. Neurosonography can provide greater resolution when a suspected intracranial abnormality is detected on routine sonography.34
Many studies have applied the Papile grading scheme from the preterm population to fetal GMH-IVH2,22; however, this approach is limited by the potential time interval between the occurrence of fetal GMH-IVH and when it is detected on prenatal imaging, which may be longer compared to preterm infants. In turn, this time interval likely impacts assessment of the amount of hemorrhage present in fetal GMH-IVH, as well as the ability to distinguish acute ventriculomegaly related to hemorrhage from fetal post-hemorrhagic ventricular dilatation. A recent paper proposed description of location of IVH, presence of parenchymal hemorrhage, ventriculomegaly and other associated findings rather than a grading system for fetal GMH-IVH.1
Systemic findings on ultrasound may also provide additional phenotypic clues pointing toward a specific syndrome or genetic etiology. For example, the presence of arthrogryposis may suggest a collagen vascular disorder, whereas organomegaly, hydrops and peritoneal calcifications can be seen in congenital infection.
Fetal MRI
The addition of fetal MRI has been found to improve diagnostic accuracy of suspected abnormalities on prenatal ultrasound;35,36 however, the diagnostic accuracy of fetal MRI for ICH has not been systematically evaluated. Recent studies have shown that identification of ICH on fetal MRI is often preceded by a different referral diagnosis based on ultrasound, most commonly ventriculomegaly. Only 6/57 (11%) cases of fetal ICH confirmed by fetal MRI in one study were preceded by a referral diagnosis of ICH based on ultrasound,3 whereas 12/22 (54%) were suspected to have fetal ICH based on ultrasound in a separate single-center study.2 In a series of 306 fetuses where ventriculomegaly was the only abnormality on ultrasound, five (2%) were found to have ICH on fetal MRI, which was confirmed postnatally.37 Other studies highlight the complementary nature of ultrasound and MRI for fetal intracerebral hemorrhage. Targeted neurosonography has shown superior sensitivity for detecting periventricular changes in the acute phase of PVHI, IVH, and basal ganglia or thalamic involvement compared to MRI in certain cases.34 Ultrasound is also reported as more reliable for determining the timing of IVH in some retrospective case series.38,39
Findings on fetal brain MRI that indicate acute or subacute hemorrhage include the presence of T1 hyperintense and T2 hypointense lesions, which may distort surrounding tissue due to local mass effect.16,33 The approximate timing of hemorrhage by T1- and T2-shortening combinations is difficult due to the high concentration of fetal hemoglobin. Chronic changes associated with hemorrhage include porencephaly, which may have areas of signal change suggestive of prior hemorrhage. An additional challenge posed by fetal MRI is the quality of hemosiderin specific sequences, as gradient echo (GRE) and susceptibility weighted imaging are particularly susceptible to motion artifact. Echo planar imaging (EPI) in fetal MRI is typically used for faster acquisition times, which may decrease sensitivity for hemorrhage.40,41,42 Examples of fetal ICH on fetal MRI and follow-up imaging are shown in Fig. 3.
Coronal T2-weighted MRI (a) at 33 gestational weeks showing mild ventriculomegaly with cysts at the bilateral caudothalamic grooves, and postnatal axial T2-weighted MRI in this case (b) showing small germinal matrix hemorrhage, septation in the right lateral ventricle and white matter hyperintensities due to congenital CMV. Axial echoplanar imaging (EPI) at 22 gestational weeks (c) in monochorionic twin showing bilateral germinal matrix-intraventricular hemorrhage (GMH-IVH), with cerebellar hemorrhage (d) on coronal T2-weighted MRI. GMH-IVH with right periventricular venous hemorrhagic infarction (e) at 31 gestational weeks due to COL4A2 variant, and postnatal axial T2-weighted MRI showing chronic changes (f). Twin with ventriculomegaly on coronal T2-weighted MRI (g) at 22 weeks and bilateral GMH confirmed on EPI (not shown), with postnatal follow-up MRI at 8 months (h) showing persistent severe ventriculomegaly despite ventriculoperitoneal shunting for post-hemorrhagic hydrocephalus with parenchymal volume loss and periventricular nodular heterotopia.
In one single-center retrospective study (n = 44) of fetal IPH, fetal MRI showed predominantly supratentorial and focal hemorrhage, with diffuse non-hemorrhagic injury in 43%.16 The frontal lobes (80%) and/or the parietal lobes (52%), and/or the deep gray nuclei (45%) were most commonly involved. IPH was commonly associated with GMH-IVH and ventriculomegaly; however, the authors reported that it was not possible to reliably grade severity of GMH-IVH or classify PVHI.16 Cortical malformations associated with IPH were seen in one-third of cases. Repeat fetal MRI after a median of 3 weeks showed expected evolution of hemorrhage in the majority (7/8), and one case showed a new finding of polymicrogyria overlying the IPH. The ratio of the maximal extent of hemorrhage to biparietal diameter was proposed to compare severity of hemorrhage on fetal MRI across different gestational ages.
The intrinsic characteristics of the hemorrhage can be helpful in determining etiology and guiding investigations. For instance, hemorrhage due to COL4A1/2 mutations classically results in a combination of IVH and frontal lobe parenchymal hemorrhage, often of different ages and resulting in porencephaly, which can be unilateral or bilateral.16,43 Multifocal white matter injury can also be seen and tends to accumulate over time. In FNAIT, fetal GMH-IVH, PVHI, IPH, and multi-compartment hemorrhage have been reported, with more than half (23/43) diagnosed <28 gestational weeks and multi-phasic hemorrhage occurring in 12% (5/43).20
Utility of postnatal imaging
Postnatal neuroimaging with MRI provides higher resolution images as well as hemosiderin specific sequences to fully visualize areas of parenchymal hemorrhage. Additionally, MRI allows for better visualization of the full-term cortical development; as many fetal MRI studies are performed mid-gestation, there may be malformations of cortical development either associated with or as a disruptive consequence of parenchymal hemorrhage, which will affect prognosis and investigations. New findings on neonatal MRI were frequent in cases of severe fetal IPH with or without IVH that underwent postnatal brain MRI in one study (6/13).16 These findings support the role of postnatal MRI to detect additional complications related to fetal IPH, such as recurrent hemorrhage, progression of ventriculomegaly, polymicrogyria, or additional white matter injury unrelated to fetal IPH.16 There are no systematic data on routine postnatal MRI after fetal intracerebral hemorrhage, and such data are requisite to quantify the probability of new clinically relevant findings. Although these data are limited currently, postnatal MRI is not thought to be needed after fetal low-grade GMH-IVH in neonates and infants that are otherwise clinically well. Postnatal vascular imaging (MRA, MRV, angiogram) may also be helpful diagnostically in cases of vascular malformation, and for endovascular intervention.
Outcomes
There is limited literature on outcomes after fetal ICH. This body of literature is retrospective and prone to selection bias. The generalizability of the rates of different pregnancy, perinatal, and neurological outcomes should be interpreted with caution. There are two systematic reviews and meta-analyses that report outcomes of fetal ICH, with most studies based on prenatal ultrasound. Sileo et al. report perinatal and neurodevelopmental outcomes in 193 fetuses from 16 studies inclusive of any type of ICH on prenatal imaging.44 Of these 16 studies, 12 overlap with the meta-analysis by Dunbar et al.22 that reports 240 cases of GMH-IVH and PVHI from 80 articles, including case reports and case series. Of the 4 studies included by Sileo et al.44 without overlap by Dunbar et al.,22 there is a retrospective series of FNAIT,20 2 small series on fetal cerebellar hemorrhage,18,19 and a series on fetal subdural hemorrhage.45 Whereas the meta-analysis by Sileo et al.44 combines Grade III GMH-IVH with PVHI (referred to as Grade IV), the Dunbar22 meta-analysis distinguishes between GMH-IVH with or without parenchymal hemorrhage. A few additional studies have been published since the publication of both meta-analyses. Here, we aim to integrate a discussion of this recent literature with the outcomes reported by meta-analysis.
Pregnancy and perinatal outcomes
Data on pregnancy outcomes report variable rates of termination of pregnancy (TOP), and do not describe reasons for termination when intracerebral hemorrhage is detected. Broadly, rates of TOP are higher when parenchymal hemorrhage is present. TOP is reported in 13/104 (13%) cases of GMH-IVH without parenchymal injury and 23/105 (22%) to 17/33 (52%) for PVHI.22 In one study of fetal IPH, TOP occurred in 16/44 (36%) of cases, and was strongly associated with maximal diameter of IPH.16 Meta-analysis data report TOP in 4/24 (17%) fetuses with infratentorial hemorrhage, and a more recent single-center study reported TOP in 2/16 (15%).17,44 Spontaneous intrauterine demise is low overall, but higher than population-level rates, occurring in 6/104 (6%) of cases of GMH-IVH without parenchymal injury, 9/105 (9%) with PVHI, 5/58 (9%) with IPH, and 2/24 (8%) with infratentorial hemorrhage.16,22,44
Preterm birth is common, both spontaneous and medically induced, occurring in 39/75 (52%) with GMH-IVH, 21/69 (30%) with PVHI,22 5/21 (24%) with IPH,16 and 2/16 (13%) with cerebellar hemorrhage.17 Medically induced indications for preterm delivery may include worsening severity of ventriculomegaly, and progressive ischemia or hemorrhage due to venous sinus thrombosis of vascular malformations. Whether preterm birth is spontaneous or medically induced is not typically reported, although would be informative to include in future studies. Postnatal mortality is often related to prematurity, systemic malformations, or other comorbidities, reported to occur in 8/104 (8%) with GMH-IVH, 7/105 (7%) with PVHI,22 and 2/21 (10%) with IPH.16 Antenatal counseling should highlight the risk of prematurity as a potentially important modifier of the risk of adverse neurodevelopmental outcomes.
Available data on the relationship between etiology of intracerebral hemorrhage and pregnancy outcome are limited to FNAIT. In a retrospective study of FNAIT,20 intrauterine demise occurred in 5/43 (12%) pregnancies complicated by fetal ICH. Preterm delivery occurred in 29/38 (76%), and perinatal or postnatal death occurred in 10/38 (26%) cases of fetal ICH due to FNAIT.
Neurological outcomes
Selected studies of neurological outcomes after fetal intracerebral hemorrhage are summarized in Table 3. The most common complication in surviving infants is motor impairment, seen in 22/80 (28%) of those without clear evidence of parenchymal hemorrhage, and 35/47 (75%) with PVHI and 12/13 (92%) with IPH.16,22 Many studies on isolated GMH-IVH have reported mild motor impairments (e.g., transient tone abnormalities, dyspraxia), whereas more severe impairment (e.g., cerebral palsy) may occur in parenchymal hemorrhage. The location and extent of parenchymal hemorrhage tends to correlate with the topology of motor impairment16; however, the relationship between fetal MRI findings, timing of hemorrhage, and the degree of functional motor impairment is not known. Cerebral palsy was reported in 2/16 (13%) cases of cerebellar hemorrhage in the meta-analysis by Sileo et al.,44 and there were no cases of motor impairment in a more recent single-center cohort.17
Little is known about cognitive and language outcomes after fetal intracerebral hemorrhage. Several factors likely contribute to variability in outcomes, including location of hemorrhage and its correlation with functional areas, involvement of critical brain areas (e.g., cerebellum, basal ganglia), and severity of ventriculomegaly. Underlying etiology additionally contributes to outcome in fetal IPH and fetal IVH, likely mediated in part by risk of recurrent hemorrhage and risk of prematurity, as well as medical complexity. However, the currently available literature has not specifically examined the influence of these factors on neurodevelopmental outcomes. Meta-analysis data indicate that developmental delay was present in 13/75 (21%) children with history of fetal grade III GMH-IVH, and 28/77 (57%) children with fetal PVHI, whereas none of the cases with grade I/II GMH-IVH had developmental delay.22 A single-center study reported intellectual disability or global developmental delay in 5/13 (38%) with IPH on fetal MRI.16 Neurodevelopmental delay was reported in 5/16 (31%) cases of cerebellar hemorrhage in the meta-analysis by Sileo et al.44 One small single center study of 10 patients evaluating outcome at a median 3.5 years (range 1–8) after isolated cerebellar hemorrhage found 6 had normal neurodevelopment and cognition, and three had mild dyspraxia and visuoperceptual impairment and one had autism spectrum disorder.17
Few studies have described epilepsy outcomes in fetal intracerebral hemorrhage. Epilepsy is reported in 3/74 (4%) with GMH-IVH, 13/50 (26%) with PVHI in a systematic review with a median follow up of 12 months (range 0–96),22 and 5/13 (38%) with IPH with a median follow up of 7 years.16
CSF diversion
Requirement for CSF shunting is reported in 31/77 (40%) of cases with fetal GMH-IVH without parenchymal injury, 34/57 (60%) with PVHI, and 2/21 (10%) with IPH.16,22 Progression of ventriculomegaly in utero is associated with shunt placement postnatally.22 The rates of shunting after fetal GMH-IVH and PVHI appear higher than the preterm population. It is uncertain to what extent ascertainment bias in the reported literature contributes to this difference, as cases with progressive or more severe fetal ventriculomegaly may be more likely to be identified. Another potential reason for the differential rates of CSF diversion in fetuses compared to the preterm population is the longer duration of progressive ventriculomegaly in utero before intervention is possible postnatally.
Recurrence risk
Fetal IPH and other ICH patterns may be associated with ongoing recurrence risk perinatally and postnatally if there is an underlying condition such as COL4A1, other collagen vascular disorders, and those with vascular anomalies.43,46 In contrast, the recurrence risk is near zero in perinatal arterial ischemic and hemorrhagic stroke.47
Current practice and practical guidance for pediatric neurologists
We surveyed pediatric neurologists that provide fetal consultations across the United States in 2023.5 Among 43 individual institutional responses, there was substantial variability in the landscape of current practice. The majority of respondents reported providing fetal neurologic consultation in collaborative care with a prenatal diagnosis center. Fewer than half of respondents (40%) reported having relevant subspecialty training, and annual consultation rates varied markedly across centers, indicating different levels of experience in centers with access to prenatal neurology consultation. Nearly all respondents indicated an interest in educational initiatives and ranked clinical practice guidelines as their top priority for this developing field. Recognizing the growing demand for fetal neurological care,5 and limited access,48 we outline practical considerations for management and counseling of fetal intracerebral hemorrhage to facilitate capacity-building, standardization of care, and collaborative research. These practical recommendations represent the current practice and consensus expert opinion of this international working group of pediatric neurologists that provide fetal neurological consultation and postnatal follow-up care.
Antenatal perinatal management
Fetal imaging
Fetal MRI is preferred following detection of suspected hemorrhage on fetal ultrasound. Imaging should be performed in a center with protocols optimized for fetal neuroimaging and interpreted by a neuroradiologist with expertise in fetal neuroimaging. Hemosiderin detection sequences should be included. After the diagnosis of intracerebral hemorrhage, longitudinal surveillance with serial fetal ultrasound is needed to monitor ventriculomegaly, and fetal head circumference, as well as to assess for new hemorrhage. Detailed anatomy scan is recommended to assess the extent of fetal abnormalities and determine whether a specific syndrome may be present.
Repeat fetal MRI may be informative in select cases, including when the initial MRI is obtained early in gestation and there are potential pregnancy management decisions, as well as to evaluate new parenchymal findings on fetal ultrasound, or to examine the extent of parenchymal hemorrhage and the secondary developmental consequences.
Family history
Elements of the family history that may support COL4A1/2-related disorders include ICH, porencephaly, unilateral cerebral palsy, focal epilepsy, renal disease, cataracts, and early-onset vascular dementia or stroke. It should be noted that over half of cases are de novo and due to variable penetrance and expressivity, family history is often unrevealing. A family history of bleeding disorders, vascular malformations, cutaneous vascular lesions, and stroke in the young should also be elicited.
Etiologic testing
There is no evidence base to recommend specific investigations; however, expert opinion recommends serological testing for infections such as CMV, parvovirus when cerebellar hemorrhage is present, other infectious etiologies as indicated case-by-case (i.e., Toxoplasma, LCMV and Zika virus), as well as parental antibody testing for FNAIT. Amniocentesis should be offered in all cases to enable testing for infection and genetic testing.
When evidence of parenchymal hemorrhage is present, genetic testing is recommended. If available, broad testing with exome or genome sequencing may be informative,11 and should be considered in all cases. If broad sequencing is not accessible and feasible, consider obtaining COL4A1/2 single gene testing or a cerebral small-vessel disease panel. Expectant parents should be counseled about the low pretest probability of genetic testing in the setting of isolated low-grade GMH-IVH without parenchymal hemorrhage. Practice patterns in some centers include offering broad sequencing to any pregnancy with an intracranial abnormality; however, access varies widely.
Fetal neurology consultations
Consultations should be conducted in collaboration with maternal-fetal medicine, to present the available diagnostic and prognostic information, as well as acknowledge uncertainties in etiology and prognosis. Studies of parents faced with a fetal diagnosis voice that having comprehensive information, delivered in plain language by a compassionate professional as key elements to reduce their stress.49,50,51,52,53 Parents should be explicitly reassured that they are not responsible for the ICH, which is often an unvoiced fear. Pediatric neurosurgery consultation should be obtained in cases of progressive ventriculomegaly where postnatal intervention may be needed.
Psychosocial support for expectant parents
Early support from a social worker and counselors/perinatal psychologists is advised to provide psychosocial support to expectant parents through the process of investigations. Perinatal palliative care and neonatology consultations should be considered in cases with anticipated lifelong consequences, and cases with uncertain consequences to facilitate discussions regarding perinatal planning, prognostic uncertainty, and family support. Referral to grief counseling is recommended as available for fetal demise and TOP.
Timing, location, mode of delivery
Cesarean section is recommended in FNAIT.54 There is otherwise no evidence available to guide mode of delivery and when to deliver the infant, however head size and risk of extension of hemorrhage should be considered in multidisciplinary discussion, and some centers routinely recommend cesarean section for fetal ICH independent of etiology. There is insufficient evidence to recommend scheduling early delivery in the case of progressive ventriculomegaly, and practice varies widely.55 Important considerations in planning the location of delivery include the need for specialized services like neurosurgery and tertiary level care. The indications for tertiary care delivery should be explained to expectant parents. For small, non-progressive hemorrhages with an otherwise healthy fetus, delivery at a specialized center is not required. If intensive care is anticipated post-delivery, it is recommended that the parent(s) meet with a neonatologist.
Postnatal recommendations
Neonatal evaluation
General examination should be performed with attention to the head circumference, fontanel, and sutures, as well as assessment for dysmorphisms, ocular findings, arthrogryposis, cutaneous vascular findings, and stigmata of congenital infection. A complete neurological examination should be performed. If encephalopathy is present or there are suspected clinical seizures, continuous electroencephalography (EEG) should be obtained as available.56 These signs could reflect new acute injury (i.e., hemorrhage, hypoxia-ischemia, ischemia) related or unrelated to the prenatal presentation, new postnatal infection, or an underlying genetic or metabolic disorder. Clinical signs such as a bulging fontanel or rapidly increasing head circumference should prompt neuroimaging (see below) and neurosurgical referral.
Neuroimaging
All infants with history of fetal GMH-IVH and/or IPH should have a postnatal cranial ultrasound, ideally prior to discharge from the birth hospitalization to establish a postnatal baseline and inform the need for ongoing monitoring of the ventricles. Surveillance of ventriculomegaly with serial ultrasound should be individualized in discussion with pediatric neurosurgery based on risk for progression to hydrocephalus. Postnatal MRI (3T if available) should be obtained in cases with parenchymal hemorrhage, whether confirmed on fetal imaging or suspected on postnatal cranial ultrasound. MRI should be performed within the first 3 months of age using the “feed and bundle” method, as feasible, to avoid need for anesthesia. Magnetic resonance angiography (MRA) and magnetic resonance venography (MRV) should be considered on a per-case basis. Resolution of fetal low-grade GMH-IVH on postnatal cranial ultrasound does not necessitate further imaging. In our experience some families may find follow-up MRI to confirm the absence of new hemorrhage or additional findings to be of substantial reassurance.
Other testing
The timing and type of investigations after delivery can be adjusted based on the timing of delivery, the condition of the infant, including associated anomalies, and the progression of findings antenatally. Genetic testing should be obtained in cases of parenchymal hemorrhage when there is not an otherwise apparent cause, such as multiple gestation or congenital infection, and genetic testing was not performed prenatally. Selection of exome or genome sequencing versus a cerebral small vessel gene panel may be based on regional access. CMV testing should be performed within 3 weeks of delivery if no confirmed etiology is otherwise established, and CMV was not definitively excluded with amniocentesis. Parvovirus testing should be performed in cases of prenatal cerebellar hemorrhage if not excluded prenatally.
Basic baseline coagulation studies, including platelets, INR, PT, PTT, should be obtained when parenchymal hemorrhage is present. Consultation with hematology can guide workup for a specific hematologic cause of hemorrhage, as well as guide the timing of specific tests that may be more reliable after the neonatal period. Further parental testing may be indicated in cases of FNAIT to prevent recurrence.
If findings are suggestive of collagen vascular disorder, including bilateral porencephaly, mixed hemorrhagic and ischemic findings, and hemorrhages of different ages,43,57 or there is a suggestive family history, then a comprehensive multi-system examination is warranted, including ophthalmological exam, renal ultrasound, creatine kinase (CK), and electrocardiogram in addition to confirmatory genetic testing.
Neurodevelopmental follow-up
Pediatric neurology follow-up is needed to monitor neurodevelopment, and for the occurrence of seizures. Close surveillance of head circumference is needed in children with risk of progressive ventriculomegaly after fetal ICH, and collaborative care with pediatric neurosurgery is recommended. A suggested schedule for neurological assessment could mirror other at-risk populations with follow-up at 3 months, 6 months, 12 months, 24 months, preschool age, and then at school age, with more frequent visits as needed when there are neurodevelopmental impairments or other neurological diagnoses requiring management such as epilepsy. Early intervention services with physical, occupational, speech and/or vision therapy should be implemented as needed to support neurodevelopment.
Practice and research gaps
Terminology
Formalized consensus across disciplines around terminology used to describe fetal intracerebral hemorrhage and associated imaging findings like cystic evolution is needed. Building consensus among pediatric neuroradiologists with expertise in fetal MRI, maternal-fetal medicine, and pediatric neurologists using a robust method like the Delphi technique,58,59 is a foundational step to address practice and research gaps.
Epidemiology
The incidence of fetal GMH-IVH with or without subsequent PVHI and fetal IPH are not well known. The reasons for the apparent male predominance are not known. Even less data is available on the incidence of less common pathologies, such as DSM.
Fetal imaging
Improved sensitivity of fetal MRI for blood products may improve diagnosis of fetal IPH. This may be of particular use for the detection of hemorrhage in cases of secondary disruptive malformations of cortical development such as schizencephaly and polymicrogyria. Use of consensus terminology will facilitate collaborative multicenter studies to describe the pattern and location of hemorrhage(s) on MRI, and associated findings, as well as how these factors relate to different etiologies and outcomes. Such datasets could be leveraged to develop and evaluate fetal GMH-IVH and IPH grading systems and compare the predictive value for outcomes with the Papile grading system in this population.1 The predictive value of imaging indices of preterm PHVD requiring neurosurgical intervention should also be evaluated in the fetal population.
Etiopathogenesis
The yield of genetic testing with targeted vasculopathy panels and whole exome or genome sequencing is not known. The yield of testing for non-genetic etiologies including congenital infections and FNAIT is not established and may vary regionally. Although prior studies have suggested a low likelihood of an identifiable etiology in low-grade fetal GMH-IVH, many of these studies are not contemporary, and it is possible that underlying genetic and non-genetic etiologies are underrecognized in this subgroup. Integrating placental pathology in studies of etiology may also provide important insights.
Mode and timing of delivery
The risk of extension in fetal ICH through a trial of labor and vaginal delivery is not known. However, a Cesarean section is routinely recommended in FNAIT because of suspected high risk of extension in this condition.54 How timing of delivery in cases with severe ventriculomegaly due to PHVD and timing to cerebrospinal fluid diversion may relate to outcome is not known. Mounting data in the preterm population show that earlier intervention for PHVD is associated with improved neurodevelopmental outcomes.60,61,62 Future studies examining the relationship between the duration of PHVD and outcome in the fetal population are needed. The influence of other clinical factors on clinical decision-making regarding medically-induced preterm delivery are not known.
Postnatal imaging
The yield of postnatal MRI is not established. For selected cases, such as arteriovenous malformation, or DSM, a postnatal neurovascular study may be needed to determine the etiology or neurovascular or surgical interventions. Neonatal MR angiogram/venogram (MRA/MRV) using a time-of-flight sequence may have low resolution without contrast, though the risk/benefit ratio of contrast in the neonatal period is not established.
Outcomes
Available literature on neurodevelopmental outcomes is limited. Prospective multicenter studies are needed to understand developmental and cognitive outcomes in childhood and adolescence, as well as risk of epilepsy, and rates of CSF diversion. How the location of hemorrhage and its correlation with functional areas, involvement of critical brain areas (e.g., cerebellum, basal ganglia), and severity of ventriculomegaly, relate to outcome will require larger sample populations to better understand. Given the prevalence of prematurity after fetal ICH, the influence of gestational age on clinical and neurodevelopmental outcomes of fetal ICH outcomes should be further evaluated. The rate of recurrent hemorrhage after fetal IPH is not known, and represents a critical gap in prognostication and care.
Conclusions
Fetal intracerebral hemorrhage is increasingly recognized, however, the available literature to date is limited by small studies, an incomplete understanding of underlying etiologies, and limited data regarding pregnancy, infant, and childhood outcomes. Given that many pregnancies of fetal ICH end in the context of fetal demise or pregnancy termination, additional research to understand factors that influence pregnancy outcomes are critically needed. Current data suggest favorable neurodevelopmental outcomes in isolated low-grade GMH-IVH, whereas cases with parenchymal hemorrhage are reported to be associated with neuromotor impairments in the vast majority. Cognitive and epilepsy outcomes are not well described. Progression of post-hemorrhagic ventricular dilatation is associated with postnatal shunt placement, although rates of hydrocephalus vary markedly by study.
Systematic investigation for an etiology as recommended in these practical guidelines will enable a more standardized approach in clinical practice, which will inform understanding of the relative frequency of different etiologies by imaging pattern. Prospective large-scale studies are needed and the practical recommendations outlined in this review may serve as the foundation for a registry to capture etiology and outcomes across populations.
References
Hadi, E. et al. Fetal intraventricular hemorrhage and periventricular hemorrhagic venous infarction: time for dedicated classification system. Ultrasound Obstet. Gynecol. 64, 285–293 (2024).
Eldad, K., Ya’ara, G., Simon, L. & Omer, B. Y. The association between fetal intracranial hemorrhages detected on MRI and neurodevelopment. Eur. J. Radiol. 173, 111380 (2024).
Gupta, V., Schlatterer, S. D., Bulas, D. I., du Plessis, A. J. & Mulkey, S. B. Pregnancy and child outcomes following fetal intracranial hemorrhage. Pediatr. Neurol. 140, 68–75 (2023).
Hausman-Kedem, M. et al. Clinical and neuroimaging patterns of perinatal intracranial haemorrhage in fetuses and term-born neonates: a prospective observational cohort study. Arch. Dis. Child. Fetal Neonatal Ed. https://doi.org/10.1136/archdischild-2024-327243 (2024).
Tarui, T. et al. Fetal neurology practice survey: current practice and the future directions. Pediatr. Neurol. 145, 74–79 (2023).
Kutuk, M. S. et al. Fetal intracranial hemorrhage related to maternal autoimmune thrombocytopenic purpura. Childs Nerv. Syst. 30, 2147–2150 (2014).
Elchalal, U. et al. Fetal intracranial hemorrhage (fetal stroke): does grade matter? Ultrasound Obstet. Gynecol. 26, 233–243 (2005).
Vergani, P. et al. Clinical significance of fetal intracranial hemorrhage. Am. J. Obstet. Gynecol. 175, 536–543 (1996).
Cardo, J. Prenatal cerebrovascular accidents: incidence, pathogenesis and risk factors. Rev. Neurol. 43, S121–S127 (2006).
Doneda, C. et al. Prenatal MR imaging detection of deep medullary vein involvement in fetal brain damage. Am. J. Neuroradiol. 32, E146–E149 (2011).
Hausman-Kedem, M. et al. Monogenic causes of apparently idiopathic perinatal intracranial hemorrhage. Ann. Neurol. 89, 813–822 (2021).
Germeshausen, M. & Ballmaier, M. CAMT-MPL: congenital amegakaryocytic thrombocytopenia caused by MPL mutations - heterogeneity of a monogenic disorder - a comprehensive analysis of 56 patients. Haematologica 106, 2439–2448 (2020).
Putbrese, B. & Kennedy, A. Findings and differential diagnosis of fetal intracranial haemorrhage and fetal ischaemic brain injury: what is the role of fetal MRI? Br. J. Radio. 90, 20160253 (2017).
Gano, D. et al. Fetal intracranial hemorrhage due to uniparental disomy and unmasked MPL-related congenital amegakaryocytic thrombocytopenia. Prenat. Diagn. https://doi.org/10.1002/pd.6737 (2024).
Ostrem, B. E. L., Godfrey, D., Caruso, P. A. & Musolino, P. L. Monogenic causes of cerebrovascular disease in childhood: a case series. Pediatr. Neurol. 149, 39–43 (2023).
Vassar, R. et al. Fetal intraparenchymal hemorrhage imaging patterns, etiology, and outcomes: a single center cohort study. Ann. Neurol. 96, 1137–1147 (2024).
Scelsa, B. et al. Prenatal diagnosis and neurodevelopmental outcome in isolated cerebellar hypoplasia of suspected hemorrhagic etiology: a retrospective cohort study. Cerebellum 21, 944–953 (2022).
Maisonneuve, E. et al. Fetal brain injury associated with parvovirus B19 congenital infection requiring intrauterine transfusion. Fetal Diagn. Ther. 46, 1–11 (2019).
Martino, F. et al. Prenatal MR imaging features of isolated cerebellar haemorrhagic lesions. Eur. Radio. 26, 2685–2696 (2016).
Tiller, H. et al. Fetal intracranial haemorrhages caused by fetal and neonatal alloimmune thrombocytopenia: an observational cohort study of 43 cases from an international multicentre registry. BMJ Open 3, e002490 (2013).
Jaimes, C. et al. Association of isolated congenital heart disease with fetal brain maturation. Am. J. Neuroradiol. 41, 1525–1531 (2020).
Dunbar, M. J., Woodward, K., Leijser, L. M. & Kirton, A. Antenatal diagnosis of fetal intraventricular hemorrhage: systematic review and meta‐analysis. Dev. Med Child Neurol. 63, 144–155 (2021).
Cizmeci, M. N. et al. Periventricular hemorrhagic infarction in very preterm infants: characteristic sonographic findings and association with neurodevelopmental outcome at age 2 years. J. Pediatr. 217, 79–85.e1 (2020).
Leijser, L. M. & de Vries, L. S. Preterm brain injury: Germinal matrix-intraventricular hemorrhage and post-hemorrhagic ventricular dilatation. Handb. Clin. Neurol. 162, 173–199 (2019).
Dunbar, M. J. & Kirton, A. Perinatal stroke: mechanisms, management, and outcomes of early cerebrovascular brain injury. Lancet Child Adolesc. Health 2, 666–676 (2018).
Yang, E. et al. Imaging features and prognostic factors in fetal and postnatal torcular dural sinus malformations, part II: synthesis of the literature and patient management. J. NeuroInterventional Surg. 10, 471 (2018).
Goldman-Yassen, A. E. et al. Torcular dural sinus malformation: fetal and postnatal imaging findings and their associations with clinical outcomes. Pediatr. Neurol. 135, 28–37 (2022).
Cornet, M. C. et al. Outcome of neonates presenting with severe cardiac failure due to cerebral arteriovenous fistula. Pediatr. Neurol. 131, 25–29 (2022).
Di Meglio, L. et al. A systematic review of prenatally diagnosed vein of Galen malformations: prenatal predictive markers and management from fetal life to childhood. Front. Pediatr. 12, 1401468 (2024).
Sanapo, L. et al. Fetal intracranial hemorrhage: role of fetal MRI. Prenat. Diagn. 37, 827–836 (2017).
Dunbar, M. J. et al. Population based birth prevalence of disease-specific perinatal stroke. Pediatrics 146, e2020013201 (2020).
Villapol, S. et al. Early sex differences in the immune-inflammatory responses to neonatal ischemic stroke. Int. J. Mol. Sci. 20, 3809 (2019).
Moradi, B., Ardestani, R. M., Shirazi, M., Eslamian, L. & Kazemi, M. A. Fetal intracranial hemorrhage and infarct: main sonographic and MRI characteristics: a review article. Eur. J. Obstet. Gynecol. Reprod. Biol. X 24, 100351 (2024).
Van der Knoop, B. J. et al. Additional value of advanced neurosonography and magnetic resonance imaging in fetuses at risk for brain damage. Ultrasound Obstet. Gynecol. 56, 348–358 (2020).
Hart, A. R. et al. Accuracy of in-utero MRI to detect fetal brain abnormalities and prognosticate developmental outcome: postnatal follow-up of the MERIDIAN cohort. Lancet Child Adolesc. Health 4, 131–140 (2020).
Griffiths, P. D. et al. Use of MRI in the diagnosis of fetal brain abnormalities in utero (MERIDIAN): a multicentre, prospective cohort study. Lancet 389, 538–546 (2017).
Griffiths, P. D. et al. Anatomical subgroup analysis of the MERIDIAN cohort: ventriculomegaly. Ultrasound Obstet. Gynecol. 50, 736–744 (2017).
Ghi, T. et al. Outcome of antenatally diagnosed intracranial hemorrhage: case series and review of the literature. Ultrasound Obstet. Gynecol. 22, 121–130 (2003).
Adiego, B. et al. Fetal intracranial hemorrhage. Prenatal diagnosis and postnatal outcomes. J. Matern Fetal Neonatal Med. 32, 21–30 (2019).
Afacan, O. et al. Fetal echoplanar imaging: promises and challenges. Top. Magn. Reson Imaging 28, 245–254 (2019).
Manganaro, L. et al. Fetal MRI: what’s new? A short review. Eur. Radio. Exp. 7, 41 (2023).
Manganaro, L. et al. Role of foetal MRI in the evaluation of ischaemic-haemorrhagic lesions of the foetal brain. J. Perinat. Med. 40, 419–426 (2012).
George, E. et al. Spectrum of fetal intraparenchymal hemorrhage in COL4A1/A2-related disorders. Pediatr. Neurol. 147, 63–67 (2023).
Sileo, F. G. et al. Perinatal and long‐term outcomes of fetal intracranial hemorrhage: systematic review and meta‐analysis. Ultrasound Obstet. Gynecol. 59, 585–595 (2022).
Folkerth, R. D., McLaughlin, M. E. & Levine, D. Organizing posterior fossa hematomas simulating developmental cysts on prenatal imaging: report of 3 cases. J. Ultrasound Med. 20, 1233–1240 (2001).
Vermeulen, R. J. et al. Fetal origin of brain damage in 2 infants with a COL4A1 mutation: fetal and neonatal MRI. Neuropediatrics 42, 1–3 (2011).
Curtis, C. et al. Thrombophilia risk is not increased in children after perinatal stroke. Blood 129, 2793–2800 (2017).
Agarwal, S., Venkatesan, C., Tarui, T. & Gano, D. Advancing the field of fetal neurology: a call for global collaborations. Indian Pediatr. 60, 795–799 (2023).
Hodgson, J. & McClaren, B. J. Parental experiences after prenatal diagnosis of fetal abnormality. Semin. Fetal Neonatal Med. 23, 150–154 (2018).
Hodgson, J. et al. Experiences of prenatal diagnosis and decision‐making about termination of pregnancy: a qualitative study. Aust. N. Zealand J. Obstet. Gynaecol. 56, 605–613 (2016).
Marokakis, S., Kasparian, N. A. & Kennedy, S. E. Prenatal counselling for congenital anomalies: a systematic review. Prenat. Diagn. 36, 662–671 (2016).
Larsson, A. K., Crang-Svalenius, E. & Dykes, A. K. Information for better or for worse: interviews with parents when their foetus was found to have choroid plexus cysts at a routine second trimester ultrasound. J. Psychosom. Obstet. Gynecol. 30, 48–57 (2009).
Field, N. K. et al. Communicating neurological prognosis in the prenatal period: a narrative review and practice guidelines. Pediatr. Res. https://doi.org/10.1038/s41390-025-03805-8 (2025).
Society for Maternal-Fetal Medicine (SMFM), Monteagudo, A. Intracranial hemorrhage. Am. J. Obstet. Gynecol. 223, B34–B37 (2020).
Agarwal, S. et al. Fetal cerebral ventriculomegaly: a narrative review and practical recommendations for pediatric neurologists. Pediatr. Neurol. 156, 119–127 (2024).
Wusthoff, C. J. et al. The American Clinical Neurophysiology Society Guideline on Indications for Continuous Electroencephalography Monitoring in Neonates. J. Clin. Neurophysiol. 42, 1–11 (2025).
Ozlu, C. et al. COL4A1/COL4A2 variants in 16 new pediatric patients: a case series of stroke, porencephaly, schizencephaly and other findings. Pediatr. Stroke 9, 29–75 (2024).
Nasa, P., Jain, R. & Juneja, D. Delphi methodology in healthcare research: how to decide its appropriateness. World J. Methodol. 11, 116–129 (2021).
Niederberger, M. & Spranger, J. Delphi technique in health sciences: a map. Front. Public Health 8, 457 (2020).
Cizmeci, M. N. et al. Assessment of brain injury and brain volumes after posthemorrhagic ventricular dilatation: a nested substudy of the randomized controlled ELVIS trial. J. Pediatr. 208, 191–197.e2 (2019).
Leijser, L. M. et al. Posthemorrhagic ventricular dilatation in preterm infants: when best to intervene? Neurology. 90, e698-e706 (2018).
Limbrick, Jr D. D. & de Vries, L. S. New insights into the management of post-hemorrhagic hydrocephalus. Semin. Perinatol. 46, 151597 (2022).
Cole, L. et al. Clinical Characteristics, Risk Factors, and Outcomes Associated With Neonatal Hemorrhagic Stroke: A Population-Based Case-Control Study. JAMA. 171, 230–238 (2017).
Papile, L. A., Burstein, J., Burstein, R. & Koffler, H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1500 gm. J Pediatr. 92, 529–534 (1978).
Kirton, A, & Wei, X. Teaching neuroimages: confirmation of prenatal periventricular venous infarction with susceptibility-weighted MRI. Neurology. 74, e48 (2010).
Pasternak, J. F., Mantovani, J. F, & Volpe, J. J. Porencephaly from periventricular intracerebral hemorrhage in a premature infant. Am. J. Dis. Child. 134, 673–675 (1980).
Kim, S. et al. Prenatal diagnosis and postnatal outcome of fetal intracranial hemorrhage: a single-center experience. Obstet. Gynecol. Sci. 67, 393–403 (2024).
Lecca, M. et al. Bi-allelic variants in the ESAM tightjunction gene cause a neurodevelopmental disorder associated with fetal intracranial hemorrhage. Am. J. Hum. Genet. 110, 681–690 (2023).
llves, N. et al. High Prevalence of Collagenopathies in Preterm- and Term-Born Children With Periventricular Venous Hemorrhagic Infarction. J. Child. Neurol. 38, 373–388 (2023).
Author information
Authors and Affiliations
Contributions
All authors were involved in drafting the article and revising it critically for important intellectual content. Each author has approved the final version for submission.
Corresponding author
Ethics declarations
Competing interests
S.B.M. and D.G. serve the Editorial Board of Pediatric Research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dunbar, M., Agarwal, S., Venkatesan, C. et al. Fetal intracerebral hemorrhage: review of the literature and practice considerations. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04000-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41390-025-04000-5