Abstract
Background
No biological treatment has been approved for pediatric eosinophilic esophagitis (EoE) in France. For patients refractory to conventional treatments, although compassionate use of monoclonal antibodies has developed, experience remains limited.
Methods
We conducted a national multicenter study across French pediatric tertiary care centers where children (younger than 18 years) who presented with EoE were treated with biological therapies between January 2015 and December 2023. The main objective was to characterize this patient population, and the indications for prescribing biologics. The secondary goals were to assess these patients’ clinical, endoscopic, and histologic finding, as well as patient tolerance, and to compare our cohort at baseline with pediatric patients from two European registers of EoE treated with conventional therapies.
Results
Thirty-six patients were prescribed 37 biologics (omalizumab, n = 1; mepolizumab, n = 6; dupilumab, n = 30). At diagnosis, the mean patient age was 7.4 (±4.4) years, and most patients had at least one atopic comorbidity (91.7%, n = 33). Failure of first-line treatments was the main reason for starting biological therapy (75.7%, n = 28), prescribed as compassionate use (54.1%, n = 20). Dupilumab showed significant clinical (48%, p < 0.01) and histological (82.6%, p < 0.01) improvement. Compared with children treated with conventional therapies, patients in our cohort at baseline presented significantly more asthma, food allergies, and atopic dermatitis, as well as more fibrostenotic phenotype and digestive symptoms. No severe side effect was reported within a 6–12-month follow-up.
Conclusion
Dupilumab is the most frequently prescribed, and appears to be the most effective biotherapy, regarding clinical and histologic remission. All biologics were well-tolerated.
Impact
-
Pending marketing authorization, biological therapies for pediatric eosinophilic esophagitis are mainly prescribed after failure of first-line treatments and on a compassionate basis in France.
-
Dupilumab is the biotherapy most frequently used, is associated with clinical and histological efficacy and is well-tolerated.
-
Children and adolescents requiring biologics appear to be younger and more severe at diagnosis than naive pediatric patients in Europeans registries.
Similar content being viewed by others
Introduction
Eosinophilic esophagitis (EoE) is the most common cause of chronic esophagitis after peptic esophagitis, and it is the main cause of dysphagia in children and young adults.1 This disease has multifactorial pathophysiology that overlaps with environmental,2,3,4,5,6 genetic,7,8 and immunological factors.9 EoE belongs to the type 2 inflammatory disease family, with an inflammatory response to food allergens.10 In the pediatric population, EoE symptoms are related to age, with young children presenting fewer specific symptoms (e.g. vomiting, failure to thrive) compared with adolescents. These patients often suffer from other type 2 inflammatory diseases such as food allergies, asthma, atopic dermatitis (AD), or allergic rhinitis (AR), which significantly alter their quality of life.11 For these reasons, current EoE therapy research is particularly focused on understanding the effects of monoclonal antibodies that specifically target the inflammatory effectors involved in EoE pathogenesis; the developed biological agents include mepolizumab and dupilumab.12,13,14,15,16,17
Within this context, we aimed to describe a French cohort of pediatric patients, with EoE refractory to first-line treatments, who were administered biological treatments. We recorded the outcome after biologics, evaluated their tolerance, and compared their initial characteristics with European registers, the European Pediatric Eosinophilic Esophagitis Registry (pEEr),18 and EoE CONNECT, a registry of EUREOS, the European Consortium for Eosinophilic Diseases of the gastrointestinal tract.19
Materials and methods
Study design
We conducted a multicenter retrospective study by voluntary reporting in pediatric gastroenterology units affiliated with the French-speaking Group of Hepatology Gastroenterology and Nutrition (GFHGNP). Members of the French Society of Allergology were also asked to participate in the study. All patients younger than 18 years, with a diagnosis of EoE (defined as clinical signs of esophageal dysfunction and eosinophils ≥15 per high-power field [HPF] on at least one esophageal biopsy) and treated by biologics between January 2015 and December 2023 were eligible for inclusion. The exclusion criterion was eosinophilic gastrointestinal disorders beyond EoE (non-EoE EGIDs).
Data collection
Clinical, biologic, endoscopic, and histologic data from July 2023 to March 2024 were electronically collected using the secure, web-based application REDCap (Stony Brook, NY). Demographic data (age, sex), medical history (date of diagnosis and physician-diagnosed associated comorbidities, including history of AD and food allergy [FA], and previous EoE treatment), and clinical symptoms were collected at the time of diagnosis, initiation of biologics, and follow-up (6–12 months after initiation of biologics). Symptoms included chest pain, heartburn, abdominal pain, dysphagia, food impaction, regurgitations, vomiting, nausea, eating difficulties, needing a lot of water during a meal, failure to thrive, and chronic cough. For each prescribed biological agent, we collected the following data: type of molecule, date of initiation, dosage, chosen indication, and reason for initiating treatment (i.e., following marketing authorization indications or compassionate use, when a treatment is prescribed prior to marketing authorization). At the start of the study period, no biological therapy had been approved by the French marketing authorization (Autorisation de Mise sur le Marché) for prescription use in EoE. Regarding type 2 inflammation diseases, omalizumab had marketing authorization for severe allergic asthma among children older than 6 years and for idiopathic chronic urticaria for adolescents older than 12 years. Dupilumab had marketing authorization for severe asthma in children older than 6 years and severe AD in children older than 6 months. Complete histological remission was defined as eosinophilic infiltrate <5/HPF in all three esophageal stages. Partial remission was defined as a reduction in the eosinophil esophagus infiltrate between 5 and 15/HPF.
Study objectives
The main objective was to characterize the population of pediatric patients with EoE, and the indications for prescribing biological therapies. We also aimed to assess the efficacy of biological treatment on clinical symptoms, endoscopic and histological findings, and patient tolerance, and to compare our cohort’s demographic characteristics (sex, comorbidities, symptoms, and endoscopic findings at diagnosis) with pediatric patients with EoE treated with conventional therapies from the European registers pEEr and EoE CONNECT.18,19
Statistics
Qualitative data are expressed as frequencies and percentages. Quantitative variables are described as mean ± standard deviation in case of Gaussian data distributions, and they were tested with the Shapiro–Wilk test. Subgroup analyses were performed for patients treated by dupilumab, using the McNemar and Wilcoxon signed and ranked tests. SAS software version 9.4® (Cary, NC) was used for analyses. Statistical comparisons with the European registers were performed using the Mann–Whitney U test with GraphPad Prism 8.0 Software (San Diego, CA). P < 0.05 was considered statistically significant.
Ethics
Non opposition form was obtained from all patients or their parents or legal guardians prior to enrollment by the doctor treating the patient or one of the investigators. The study protocol was approved by the ethics committee of the GFHGNP (n°2023–50) and the Commission Nationale de l’Informatique et des Libertés (DEC23-100).
Results
Sample characteristics
Thirty-eight patients from 14 tertiary care hospital centers were eligible for inclusion, with a median of 2 patients per center (min: 1, max: 7). Two patients were excluded because of an eosinophilic gastrointestinal disease and normal esophageal biopsies before initiating biological treatment (Fig. 1). Among the 36 included patients, 1 patient received two different biological agents (mepolizumab, then dupilumab). At follow-up, clinical data, EoE Endoscopic Reference Score (EREFS), and histologic data were available for 32, 31, and 30 patients treated with biological agents, respectively.
At diagnosis, the mean patient age was 7.4 years, and most patients were male (75.0%, n = 27) (Table 1). Most patients presented with atopic disorders, including asthma (72.2%), FA (63.9%), AD (47.2%), or AR (38.9%). Five patients (13.9%) presented four atopic comorbidities, 11 patients (30.6%) had three atopic comorbidities, and 10 patients (27.8%) had two atopic comorbidities (5.6%). Only 3 patients reported no allergic comorbidities (8.3%). EoE symptoms were mainly dysphagia, food impaction, and feeding difficulties (Table 2). Endoscopic evaluation showed a median EREFS of 3.0 [interquartile range (IQR) 2.0; 4.0] and esophageal biopsies showed a median number of eosinophils/HPF of 23.3 [IQR 17.7; 32.7]. Most patients were prescribed proton pump inhibitors (PPIs, 97.2%, n = 35) for a median duration of 33.1 months, as well as budesonide (97.2%, n = 35) for a median duration of 14.7 months before initiating biologic therapy (Table 1). Almost half of the patients had empirical elimination diet (52.8%, n = 19) for a median duration of 4.9 months. In most cases, first-line treatments were initially combined (81.3%, n = 26/32 patients), with the most common combinations being PPI + budesonide (68.8%, n = 22/32), diet + PPI (25%, n = 8/32) and diet + budesonide (15.6%, n = 5/32)(Supplementary Table). Failure of first-line treatments was the main real-life reason for starting biological therapy (75.7%, n = 28). In the absence of authorization in France for EoE, the main reason declared for prescribing biologics was compassionate use (54.1% n = 20) pending a recommendation in EoE in France. The average time from EoE diagnosis to commencement of biologic therapy was 47.8 months ( ± 26.9). Symptoms and endoscopic findings present before starting the biological agent are detailed in Table 1.
Biological agents and follow-up
Omalizumab
One patient (male, 11 years) received omalizumab starting in February 2022 to treat severe asthma, at a dosage of 600 mg every 14 days. Heartburn was reduced from once or twice a day to once a month, after treatment. This patient did not present any other symptoms associated with EoE. However, after 16 months of omalizumab, although the number of asthma exacerbations was reduced, worsening of the obstructive ventilatory disorder led to switching to treatment with dupilumab. Endoscopic assessment was performed 9.6 months after starting treatment. EREFS was 2 and 0 before and after treatment, respectively. Complete histological remission was observed (0, 51, and 27 eosinophils/HPF before and 0, 0, and 1 eosinophils/HPF after omalizumab, in the proximal, mid-, and distal esophagus, respectively). The patient did not report any side effects while receiving omalizumab. Treatment with dupilumab was not included in the study because of complete remission prior to initiation.
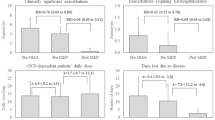
Mepolizumab
Mepolizumab was prescribed to 6 patients at the doses recommended for severe asthma, i.e., 40 mg monthly for patients aged 6–11 years (n = 2) and 100 mg weekly for patients older than 12 years (n = 4). Clinical efficacy was partial after 6–12 treatment months (Fig. 2a). The mean time to endoscopic control was 6.9 months. Histological response was absent in 3 patients, complete in 2, and partial in 1. EREFS was similar before and after treatment (median score 2.5 both before and after mepolizumab). Mean eosinophil counts were 35, 37, and 18 eosinophils/HPF before and 6, 9.5, and 4 eosinophils/HPF after mepolizumab, in the proximal, mid-, and distal esophagus, respectively (Fig. 2b). No side effects were reported. Two patients were still treated with mepolizumab at the time of data collection. Mepolizumab was suspended for complete remission in 3 patients and for treatment non-adherence in 1 patient.
Dupilumab
Thirty included patients received dupilumab, among whom 12 were followed prospectively. Eleven patients received dupilumab at recommended doses for severe AD: 5 patients were prescribed 200 mg/2 weeks; 6 patients were prescribed 300 mg/2 weeks. Dupilumab was also prescribed at recommended doses for severe asthma in 5 patients: 200 mg/4 weeks in 3 patients and 300 mg/4 weeks in 2 patients. For 4 patients (13.3%), dupilumab was administrated weekly (300 mg for 3 patients and 200 mg for 1 patient). Most patients (76.6%, n = 23) started dupilumab due to previous treatment failure. Compassionate use was indicated, in accordance with marketing authorization, for half (n = 15) of these patients, while severe asthma (26.7%, n = 8) and severe AD (16.7%, n = 5) were the second and third indications.
In terms of overall clinical efficacy, all patients’ symptoms improved after 6–12 months of dupilumab (Fig. 3a). Clinical improvement was significant (p = 0.0009), with complete resolution of symptoms in almost half of patients (48.0%, n = 12). Among these twelve patients, 6 (50%) were treated 300 mg every 2 weeks, 5 (41.7%) had 200 mg every two weeks and one (8.3%) received 200 mg monthly. Substantial improvement of food impaction (p = 0.01) and dysphagia (p = 0.0005) were observed on treatment.
a Clinical symptoms, before and 6-12 months after initiating dupilumab, food impaction: p = 0.011; dysphagia: p = 0.0005. b Eosinophils count per HPF at the proximal, mid- and distal esophagus, *p = 0.001, **p = 0.0001, ***p < 0.0001. EoE eosinophilic esophagitis, EREFS edema, rings, exudates, furrows, stenosis, HPF high power field.
Endoscopic control was performed at 7 months (mean 7.0 ± 4.5) and revealed a complete histological response for most patients (82.6%, n = 19), but was partial (8.7%, n = 2) or absent (8.7%, n = 2) for the others. Patients showing complete histological remission, mostly received 300 mg every 2 weeks (42.1%, n = 8) and 200 mg every 2 weeks (31.6%, n = 6). The median EREFS significantly decreased (3.0 vs. 0, p < 0.0001). For each esophageal stage, significant reduction of eosinophil counts before and after dupilumab are detailed in Fig. 3b.
Side effects were assessed in 26 patients and revealed good tolerance of dupilumab by most, who reported no adverse effect (76.9%, n = 20). Several patients reported pain at the injection site (11.5%, n = 3). One patient had blepharitis (3.8%) 3 months after starting dupilumab. One patient experienced a combination of abdominal pain, rash, and fever after the first injection, without the need to discontinue treatment. One patient (3.8%) experienced asthenia in the days following each injection. Side effects were not assessed in 4 patients because treatment had been started since less than 6 months. Dupilumab was still ongoing at the time of data collection for 25 patients (83.3%). Treatment was discontinued for 5 patients, due to complete remission for 3 patients, poor compliance for 1, and side effects for 2 (blepharitis in 1 patient who had severe active AD at the start of treatment).
Comparisons with pediatric patients with EoE from European Registries, treated with conventional therapies
We compared our cohort with pediatric patients, who were naïve to biologics, from the two European registers pEEr (n = 582)18 and EoE CONNECT (n = 254)19 (Table 2). Though age was not analyzed statistically, patients who required biologics in our cohort appeared younger at diagnosis (mean age 7.4 vs. 11.9 years). Patients did not differ on sex or AR frequency. However, our patients displayed significantly more FA, asthma, and AD compared with pEEr- and EoE CONNECT-registered patients. Our patients reported more symptoms than those on conventional therapies, including dysphagia, food impaction, vomiting, regurgitations, abdominal pain, and failure to thrive (Table 2). Finally, patients requiring biologics presented more exudates (p = 0.01), furrows (p = 0.0003), and a more frequent fibrostenotic phenotype (p = 0.0007) at baseline.
Discussion
Main results
This study is a rare real-world report of EoE treated with biological agents at a national level.20,21,22 Atopic comorbidities were observed in most patients. Biologics were indicated mainly because of previous medication failures, and were prescribed based on compassionate use for half the patients. Dupilumab was used most frequently, and reduced clinical symptoms, EREFS, and eosinophil counts on esophageal biopsies. All biologics were well-tolerated.
Patients requiring biologics were more severe at baseline
Patients in our cohort presented more atopic comorbidities and digestive symptoms than those in the two registers, who did not receive biologics. Similar to our cohort, Pelz et al. found that patients with EoE and FA were diagnosed at a younger age (6.05 vs. 8.09 years, p = 0.01) and had more EoE-related symptoms compared with patients with EoE without FA.23 Furthermore, in our cohort, esophageal eosinophil counts were neither predictive of symptom severity nor differed from biologics-naïve patients from the pEEr cohort. The sex ratio was similar between the cohort and registry groups, reflecting the absence of impact of this parameter on disease evolution. In Salvatore’s cohort, response to PPI therapy was better in older patients ( > 10 years, p = 0.03) which may partly explain the high non-response rate for patients with biologics in our cohort, who were younger at diagnosis.18 Finally, the more severe forms of EoE in our study could probably be explained by younger age at diagnosis and, therefore, a longer duration of disease progression. Indeed, it has been shown that EoE severity is linked to disease duration.24 Interestingly, younger age was associated with more frequent fibrostenotic phenotype in our cohort (25.0%) vs. EoE CONNECT (6.2%), which may explain the greater frequency of food impactions, dysphagia, and failure to thrive among our patients.
Positive effects of dupilumab
Dupilumab is a human monoclonal antibody that inhibits interleukin-4 and interleukin-13 signaling pathways, which are involved in type 2 inflammation.25,26 In France, dupilumab was initially approved in 2019 for severe asthma, and in 2020 for severe AD, among patients older than 12 years. This approval was progressively extended for both indications until 2023, with current approval for severe asthma from age 6 years and severe AD from age 6 months. Thus, this biological agent was prescribed for compassionate use in half of our French pediatric EoE cases resistant to first-line treatments, with a mean age of 11 years at the time of biotherapy initiation, the youngest of whom was 2 years old. Furthermore, 50% were indicated for atopic comorbidities. This could be explained by the paucity of studies available on the effects of dupilumab in patients with EoE who are younger than 12 years at the time of biological treatment prescription. Spergel et al. included 45 children and adolescents treated with dupilumab, mainly for atopic comorbidities associated with EoE.22 Our results are consistent with these cohort results, i.e., clinical and histological efficacy, with a significant reduction in EREFS, esophageal eosinophils count, and significant improvement in symptoms in all cases. Several pediatric case reports have consistently shown the effectiveness of dupilumab.21,27 After its 2022 approval by the United States Food and Drug Administration (FDA) for use in patients with EoE (who are older than 12 years, weigh more than 40 kg, and did not respond to 8 weeks of high-dose PPI), a survey of 42 patients during 2022 and 2023 showed that the primary reasons for starting dupilumab were non-response to topical corticosteroids and poor compliance with previous treatments.20 In 2024, the ESPGHAN EGID working group recommended the use of dupilumab for children older than 1 year and weighing over 15 kg in cases of conventional treatment failures.28 More recently, a randomized, phase III trial in children aged 1–11 years confirmed the efficacy of high-dose dupilumab (300 mg once weekly) vs. placebo, with a difference of esophageal eosinophils count peak of 65% between the two groups at 16 weeks (p < 0.001).13 Dupilumab used with lower dose (300 mg every 2 weeks) was also effective compared with placebo, with a reduction of 55% of the esophageal eosinophil count peak (p < 0.001), but it did not reach significance regarding most secondary endpoints (e.g. clinical scores, transcriptomic changes). Interestingly, the mean age (7.1 years vs. 7.4 years herein) and the presence of at least one atopic comorbidity (98% vs. 91.7% herein) were similar. The authors also detected comparable adverse effects during the treatment period (73–100% vs. 76.9% herein), which were not attributed to dupilumab. This publication was followed by extended FDA approval for dupilumab to children from age 1 year, weight over 15 kg, and refractory to 4 months of PPIs. Our study confirms, in a real-life setting, the efficacy of and tolerance to dupilumab in pediatric patients with EoE.
Given the heterogeneity of dupilumab dosages, we were unable to compare dosages in our cohort. Chehade et al. reported dupilumab dosing graded by weight according to higher- or lower-exposure regimen, corresponding to concentrations of 300 mg dose administered once weekly and once every 2 weeks, respectively.13 More precisely, the higher-exposure regimen, which was associated with significant benefits regarding histological, endoscopical, transcriptomic endpoints compared with placebo, included dosages ranging from 100 mg every 2 weeks (5–15 kg) to 300 mg once weekly ( ≥ 60 kg). In this study, although the majority of patients received doses corresponding to indications of allergic comorbidities, which are lower than the current FDA approved doses for EoE in children, dupilumab was effective.
Regarding tolerability, most reported side effects were pain at the injection site, without requiring treatment interruption. The only serious adverse reaction reported was blepharitis 3 months after starting dupilumab. This secondary effect appears rare, as it was not described in the two phase III trials conducted in adults and adolescents.12,13 However, blepharitis is specifically associated with AD, which was also present in our patient.29 Our series also emphasizes the importance of close monitoring and appropriate patient compliance with dupilumab treatment.30 Indeed, adolescents with EoE have been shown to have poor medication compliance and, thus, may start stopping their treatments on their own; this occurs far more frequently in real-world clinical contexts compared with randomized control studies.31
Strengths and limitations
Given the small numbers of patients treated with mepolizumab and omalizumab, we could provide only descriptions herein. Nevertheless, our mepolizumab results appear consistent with those of Assa’ad14 and Dellon,15 who concluded that there are significant reductions in esophageal eosinophils, although complete histological remission was low (33.3%) and symptom improvement was lacking.
Though the study was retrospective, we were able to include a prospective sample of 12 patients treated with dupilumab. However, the resulting dupilumab efficacy may have been influenced by a selection bias, due to the high frequency of atopic comorbidities in our cohort. Given the study design and the pediatric marketing authorization for using biotherapies in type 2 inflammatory diseases in France at the time of the study, we observed a high rate of comorbidities among patients receiving these biological agents. As for comparisons with the two European registers, we cannot exclude the possibility that patients from those cohorts may not have responded to first-line treatments or who relapsed after data collection. Another study limitation is that several histological evaluations could not be included due to anatomopathological report inaccuracies (i.e., only specified >15 eosinophils/HPF).
Conclusion
Pediatric patients with EoE refractory to first-line treatments present atopic comorbidities with more severe symptoms, more fibrostenotic phenotype, and likely younger age at diagnosis. Most of them are treated with biologics for compassionate use, pending marketing approval in France, and all were well-tolerated. Dupilumab was the most frequently prescribed among biologics and has been shown effective in terms of clinical symptoms and histological remission. Future studies should evaluate whether quality-of-life is better, especially for patients with severe EoE, with fewer symptoms, radiological exams, and endoscopies.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Lucendo, A. J. et al. Guidelines on eosinophilic esophagitis: evidence-based statements and recommendations for diagnosis and management in children and adults. U. Eur. Gastroenterol. J. 5, 335–358 (2017).
Alexander, E. S. et al. Twin and family studies reveal strong environmental and weaker genetic cues explaining heritability of eosinophilic esophagitis. J. Allergy Clin. Immunol. 134, 1084–1092.e1 (2014).
Jensen, E. T., Kuhl, J. T., Martin, L. J., Rothenberg, M. E. & Dellon, E. S. Prenatal, intrapartum, and postnatal factors are associated with pediatric eosinophilic esophagitis. J. Allergy Clin. Immunol. 141, 214–222 (2018).
Lucendo, A. J., Arias, A. & Tenias, J. M. Relation between eosinophilic esophagitis and oral immunotherapy for food allergy: a systematic review with meta-analysis. Ann. Allergy Asthma Immunol. 113, 624–629 (2014).
Jensen, E. T. & Dellon, E. S. Environmental factors and eosinophilic esophagitis. J. Allergy Clin. Immunol. 142, 32–40 (2018).
Jensen, E. T. et al. Maternal and infant antibiotic and acid suppressant use and risk of eosinophilic esophagitis. JAMA Pediatr. e234609. (2023)
Kottyan, L. C. & Rothenberg, M. E. Genetics of eosinophilic esophagitis. Mucosal. Immunol. 10, 580–588 (2017).
Sleiman, P. M. A. et al. GWAS identifies four novel eosinophilic esophagitis loci. Nat. Commun. 5, 5593 (2014).
Khokhar, D. et al. Eosinophilic esophagitis: Immune mechanisms and therapeutic targets. Clin. Exp. Allergy 52, 1142–1156 (2022).
Straumann, A., Bauer, M., Fischer, B., Blaser, K. & Simon, H. U. Idiopathic eosinophilic esophagitis is associated with a T(H)2-type allergic inflammatory response. J. Allergy Clin. Immunol. 108, 954–961 (2001).
Gómez de la Fuente, E. et al. Addressing the unmet needs in patients with type 2 inflammatory diseases: when quality of life can make a difference. Front Allergy 4, 1296894 (2023).
Dellon, E. S. et al. Dupilumab in adults and adolescents with eosinophilic esophagitis. N. Engl. J. Med 387, 2317–2330 (2022).
Chehade, M. et al. Dupilumab for eosinophilic esophagitis in patients 1 to 11 years of age. N. Engl. J. Med 390, 2239–2251 (2024).
Assa’ad, A. H. et al. An antibody against IL-5 reduces numbers of esophageal intraepithelial eosinophils in children with eosinophilic esophagitis. Gastroenterology 141, 1593–1604 (2011).
Dellon, E. S. et al. Mepolizumab for treatment of adolescents and adults with eosinophilic oesophagitis: a multicentre, randomised, double-blind, placebo-controlled clinical trial. Gut 72, 1828–1837 (2023).
Kliewer, K. L. et al. Benralizumab for eosinophilic gastritis: a single-site, randomised, double-blind, placebo-controlled, phase 2 trial. Lancet Gastroenterol. Hepatol. 8, 803–815 (2023).
Loizou, D. et al. A pilot study of omalizumab in eosinophilic esophagitis. PLoS ONE 10, e0113483 (2015).
Oliva, S. et al. Characterization of Eosinophilic Esophagitis From the European Pediatric Eosinophilic Esophagitis Registry (pEEr) of ESPGHAN. J. Pediatr. Gastroenterol. Nutr. 75, 325–333 (2022).
Laserna-Mendieta, E. J. et al. Differences between childhood- and adulthood-onset eosinophilic esophagitis: An analysis from the EoE connect registry. Dig. Liver Dis. 55, 350–359 (2023).
Nguyen, N. et al. One year into dupilumab: physician and patient experiences in initiating dupilumab for pediatric eosinophilic esophagitis. J. Pediatr. Gastroenterol. Nutr. 77, 536–539 (2023).
Syverson, E. P. & Rubinstein, E. Real world experience with dupilumab in eosinophilic esophagitis in children and young adults at a tertiary care pediatric medical center. JPGN Rep. 3, e180 (2022).
Spergel, B. L. et al. Improvement in eosinophilic esophagitis when using dupilumab for other indications or compassionate use. Ann. Allergy Asthma Immunol. 128, 589–593 (2022).
Pelz, B. J. et al. IgE-associated food allergy alters the presentation of paediatric eosinophilic esophagitis. Clin. Exp. Allergy J. Br. Soc. Allergy Clin. Immunol. 46, 1431–1440 (2016).
Schoepfer, A. M. et al. Delay in diagnosis of eosinophilic esophagitis increases risk for stricture formation in a time-dependent manner. Gastroenterology 145, 1230–1236 e1-2 (2013).
Gandhi, N. A., Pirozzi, G. & Graham, N. M. H. Commonality of the IL-4/IL-13 pathway in atopic diseases. Expert Rev. Clin. Immunol. 13, 425–437 (2017).
Le Floc’h, A. et al. Dual blockade of IL-4 and IL-13 with dupilumab, an IL-4Rα antibody, is required to broadly inhibit type 2 inflammation. Allergy 75, 1188–1204 (2020).
Castro, K. et al. Histologically remarkable eosinophilic esophagitis responsive to dupilumab in a gastrostomy tube-dependent pediatric patient on amino acid formula. JPGN Rep. 3, e250 (2022).
Amil-Dias, J. et al. Diagnosis and management of eosinophilic esophagitis in children: An update from the European Society for Paediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN). J. Pediatr. Gastroenterol. Nutr. 79, 394–437 (2024).
Neagu, N. et al. Dupilumab ocular side effects in patients with atopic dermatitis: a systematic review. J. Eur. Acad. Dermatol Venereol. JEADV 36, 820–835 (2022).
Buendia, M. A., Choksi, Y. A. & Hiremath, G. Relapse of eosinophilic esophagitis on dupilumab. JPGN Rep. 3, e273 (2022).
Mehta, P., Pan, Z., Zhou, W., Kwan, B. M. & Furuta, G. T. Medication adherence rates in adolescents with eosinophilic esophagitis are low and are associated with health habits. J. Pediatr. Gastroenterol. Nutr. 77, 532–535 (2023).
Acknowledgements
We express our gratitude to Dr. Mélanie Leroy and the FIMATHO clinical research team, including Marine Gonzalez, Sabrina Bennia, Katialine Groff, and Oumaima Lmouataz, for their generous support. We also thank the Groupe Francophone d’Hépatologie-Gastroentérologie et Nutrition Pédiatriques (GFHGNP) and the working group EoE/Food Allergy of the Societé Française d’Allergologie for their kind help.
Funding
Open access funding provided by Centre Hospitalier Universitaire de Lille.
Author information
Authors and Affiliations
Contributions
JS, SL, FG and LT brought substantial contributions to conception and design. JS, EC, FG and LT did acquisition of data, analysis and interpretation of data. JS, SL, MA, RE, CDL, AL, LBH, GD, EC, FG and LT drafted the article and revised it critically for important intellectual content. All co-authors approved of the final version of the manuscript to be published.
Corresponding author
Ethics declarations
Competing interests
Nicolas Caron: Consultant fees from Sanofi. Claire Dupont-Lucas: Consultant fees from Sanofi. Frederic Gottrand: Member of advisory board – Sanofi. Nicolas Kalach: Member of advisory board - Dr Falk and Sanofi. Stéphanie Lejeune: honoraria for communications (SANOFI), honoraria for training activities (SANOFI – NOVARTIS – STALLERGENES), funding for participation at conferences and congresses (SANOFI, ALK, GSK), research grant mobility (ASTRA ZENECA). Anaïs Lemoine: Grünenthal. The other authors have no conflict of interest to declare.
Patients consent
Non opposition form was obtained from all patients or their parents or legal guardians prior to enrollment by the doctor treating the patient or one of the investigators.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Soudant, J., Lejeune, S., Aumar, M. et al. A nationwide experience of biological treatments in children with eosinophilic esophagitis. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04011-2
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41390-025-04011-2