Abstract
Background
Although germline genetic testing can inform medical management for patients with prostate cancer (PCa), data are limited regarding patient-reported outcomes (PROs) after germline genetic testing for PCa. Recall and comprehension of germline genetic testing results, uptake of post-test clinical recommendations, and psychological impact of germline genetic testing among patients with PCa were evaluated.
Methods
This is a secondary analysis of data from the PROCLAIM trial. PROs were analyzed overall and by germline genetic testing results. Differences between groups were determined by two-tailed Fisher’s exact test with significance set at p < 0.05.
Results
Among 494 patients with informative survey responses, 60% and 71% accurately recalled and interpreted their germline genetic testing results, respectively, with the highest rates among patients with negative results and the lowest among those with variant of uncertain significance-only (VUS) results. Among 42/55 (76%) patients with positive results for whom clinicians made germline genetic testing-informed recommendations, 39 (93%) completed or planned to complete >1 clinical recommendation. Conversely, no further recommendations were made for 160/221 (72%) and 211/218 (97%) patients with VUS and negative results, respectively. However, 57% (213/371) of these patients indicated that they or their family members intended to pursue clinical management strategies that were not recommended by their clinicians. Of the patients who responded to the survey, >90% of patients reported no post-germline genetic testing increase in their level of concern for themselves or their family members.
Conclusion
germline genetic testing for patients with PCa did not cause appreciable psychological harm to the tested patients. Furthermore, patients with positive results had a high uptake of clinician-recommended management strategies. Of note, there were inconsistencies in the understanding of VUS results, with some clinicians making recommendations not warranted by personal/family history; conversely, some patients pursued management strategies not recommended by their clinicians. This suggests that educational efforts are needed in the communication of germline genetic testing results and clinical recommendations to patients.
Similar content being viewed by others
Introduction
The complexity of current criteria for germline genetic testing (GGT) for men with prostate cancer (PCa), including conflicting guidelines published by various professional societies and consensus committees, has impeded implementation of GGT [1,2,3,4]. As a result, many patients with pathogenic or likely pathogenic germline variants (PGVs) in hereditary cancer genes have not been identified, resulting in missed opportunities for targeted therapy, cascade testing, clinical trials, as well as cancer screening and prevention [5,6,7,8].
The original publication from the PROstate Cancer Registry in Large Patient Population AIMed to Assess Efficacy in Germline Testing (PROCLAIM) trial (ClinicalTrials.gov ID NCT05447637) reported that 7.7% of unselected patients with PCa harbored >1 PGV [5]. A secondary aim of the PROCLAIM trial reported real-world clinical implications of universal GGT, demonstrating that GGT results informed clinician management recommendations, especially for patients with positive results [9]. The clinical benefits of GGT are, however, dependent on the accurate receipt, interpretation with explanation, and adherence of patients to guideline-informed clinical recommendations.
The collection of patient-reported outcomes (PROs) can evaluate how well patients understand physicians’ conveyance of GGT test results and their resulting decision-making. Two studies in patients with PCa that examined patient comprehension of GGT results and communication of results with family members were based on responses from just 12 and 109 patients [10, 11]. Thus, larger studies examining a broader range of PROs are needed. Here, the results of a prospective survey among a subset of patients enrolled in the PROCLAIM trial are presented. The survey assessed patient recall and comprehension of GGT results, uptake of post-test clinical recommendations, and the psychological impact of testing.
Methods
Study population
PROCLAIM (protocol 20191596) was approved by WCG IRB (Puyallup, WA). All patients had a diagnosis of PCa as the primary inclusion criterion, and were otherwise unselected for age at diagnosis, stage, or histology of cancer, or family history. All patients were recruited as previously described [5] and provided informed consent to have their de-identified data used in this study.
Germline genetic testing
Clinical GGT was performed by Invitae (now part of Labcorp) for all patients using a panel of 84 multi-cancer predisposition genes, as previously described [5, 12, 13]. GGT results were classified as positive if >1 PGV was detected, VUS-only if >1 variant of uncertain significance (VUS) but no PGVs were detected, and negative if no PGVs or VUSs were detected. Carrier findings (i.e., single PGVs in genes associated with autosomal recessive inheritance of cancer risk) were classified as positive and included in subsequent analyses to capture the diversity of clinical recommendations and PROs following universal GGT.
Data collection and management
As previously described [9], physicians were asked to enter patient data into electronic case report forms (CRFs) after they received GGT results and shared their post-test clinical recommendations with patients. Four weeks after physicians received the GGT results, patients were sent an electronic, semi-structured survey composed of 11 multiple-choice questions and one open-ended question related to their testing experience (Table S1). The survey questions were developed by a multidisciplinary team that included clinicians, genetic counselors, and an independent consultant experienced with PROs in cancer and genetics.
The patient survey assessed (1) patient recall and comprehension of test results, (2) patient recall and uptake of clinical recommendations, and (3) psychosocial impact. Clinical recommendations were divided into those for patients and those for family members. No reminders were sent to physicians regarding the CRFs, but patients who did not initially respond to the survey were sent an automated reminder after 2 weeks, and again 2 weeks later, if necessary. If patients still did not respond, a paper copy of the survey was mailed.
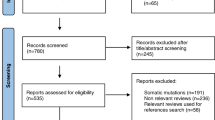
Survey respondents were excluded from this study as described in Fig. S1. Unless otherwise noted, only informative responses to multiple-choice questions were included in statistical analyses. Informative responses were defined as definitive answers and answers of “unsure” or “other.” Blank responses and two or more conflicting responses to a question requesting a single answer were excluded from analyses. For clinical recommendation uptake analyses, only recommendations that could be confirmed by the CRF were included.
Statistical analyses
All PROs were analyzed overall and by laboratory-confirmed GGT results. Laboratory-confirmed GGT results were compared with patient-reported GGT results to determine the accuracy of patient recall. The number of patients included in each analysis differed depending on how many patients provided informative responses to a particular question. Two-tailed chi-square or Fisher’s exact test was used to determine statistical differences between groups, with significance set at p < 0.05. For categorical variables with more than two levels, post hoc comparisons were conducted when the overall test was significant. To account for multiple comparisons, a Bonferroni correction was applied to all p values.
Results
Study patients
Among the 982 patients who enrolled in the PROCLAIM trial, 561 (57.1%) responded to the patient survey. Sixty-seven respondents were excluded based on blank or unevaluable responses, resulting in a cohort of 494 patients (50.3% of the original cohort) who provided informative responses (Fig. S1). Significant differences were detected between patients that provided informative survey responses and those who did not respond for race/ethnicity, with those providing informative responses more frequently White (85.6% vs. 65.6%, p < 0.001) and less frequently Black (8.9% vs. 27.6%, p < 0.001), to have had other non-prostate cancers (23.7% vs. 9.3%, p < 0.001) and a family history of cancer (30.2% vs. 20.2%, p = 0.011) (Table 1). The 55 patients with positive results had 57 PGVs in 18 genes (Fig. S2).
Patient recall of test results
Comparison of patient-recalled with laboratory-confirmed GGT results showed that 293 (60.2%) of 487 patients accurately recalled their test results: 171/214 (79.9%) with negative results, 35/55 (63.6%) with positive results, and 87/218 (39.9%) with VUS-only results (Fig. 1). Both patients with positive (p = 0.002) and negative (p = 0.010) results were significantly more accurate in recalling their results than those with VUS-only results; those with negative results also had a significantly higher rate of correctly recalling their test results compared to patients with positive results (p = 0.019). Of note, 82/487 (16.6%) patients were “unsure” of their test results. Patients with VUS-only results most frequently reported being unsure (41/221, 18.6%), followed by those with positive results (9/55, 16.4%) and negative results (32/218, 14.7%).
Patient comprehension of test results
The first component of comprehension assessed was whether patients correctly understood that they did (positive results) or did not (negative or VUS-only results) carry a genetic change associated with cancer risk. Overall, 338/474 (71.3%) patients demonstrated accurate understanding: 179/209 (85.6%) with negative results, 34/51 (66.7%) with positive results, and 125/214 (58.4%) with VUS-only results (Fig. 1). Accurate understanding was significantly more common among patients with negative results than those with positive results (p = 0.004) or VUS-only results (p < 0.001). An additional 101/474 (21.3%) patients were “unsure” what their test results meant, which was significantly more common among patients with VUS-only results than patients with negative results (31.8% versus 10.5%; p < 0.001). None of the demographic characteristics collected were significantly associated with comprehension (Supplementary Table S2).
When data on recall and comprehension were combined, 243/469 (51.8%) patients both accurately recalled their test results and understood what they meant in terms of cancer risk: 164 (79.2%) with negative results, 32 (62.7%) with positive results, and 47 (22.5%) with VUS-only results (Fig. 1). Patients with negative results had significantly higher rates of accurately recalling and understanding their results than patients with either positive results (p < 0.029) or VUS-only results (p < 0.001); patients with positive results also had significantly higher rates than patients with VUS-only results (p < 0.001).
The second component of comprehension assessed was whether patients understood GGT-based implications for follow-up. Of the 55 patients with positive results, 5 (9.1%) comprehended that they should meet with a non-prostate specialist, while 24 (43.6%) understood that family members should be tested. Conversely, the majority of patients with negative and VUS-only results understood that consulting with a non-prostate specialist (209/213, 98.1% and 219/219, 100%, respectively) or testing of their family members (206/213, 96.7% and 210/219, 95.9%) was not warranted. In total, 101 (20.7%) patients were “unsure” about the implications for follow-up of their results; those with VUS-only results were significantly more often unsure about their results compared to those with negative results (31.1% vs. 10.3%; p < 0.001), but not compared to those with positive results (31.1% vs. 20.0%, p = 0.134).
Patient uptake of clinical recommendations
Clinical recommendations for the patient and/or family members were made for 42/55 (76.4%), 61/221 (27.6%), and 7/218 (3.2%) of patients with positive, VUS-only, and negative results, respectively (Table 2). Receiving at least one recommendation for patient or family member management was significantly more common among patients with positive results compared to those with VUS-only or negative results (p ≤ 0.001 for both comparisons) (Table 2). For the 55 patients with positive results, the most frequent clinician recommendations were changes to follow-up care (31, 56.4%), and for family members to undergo GGT (36, 65.5%) or to meet with a genetic counselor (34, 61.8%). The most common recommendation for the 221 patients with VUS-only results was changes to follow-up care (51, 23.1%). For the 218 patients with negative results, the most frequent recommendation was for family members to undergo GGT (5, 2.3%).
Patients with positive results were significantly more often to have acted upon or intend to adhere to clinician recommendations (39/42, 92.9%) compared to those with negative results (4/7, 42.9%, p = 0.05), but not compared to those with VUS-only results (48/61, 78.7%, p = 0.52) (Table 2). For patients with positive results, treatment changes had the highest rate of uptake (4/7, 57.1%), followed by recommending that family members pursue GGT (19/36, 52.8%). For patients with VUS-only results, the most common recommendation pursued was to meet with a genetic counselor (12/36, 33.3%). For patients with negative results, only a single clinical recommendation (“other”) was made, and the patient pursued this recommendation. In accordance with VUS and negative results being non-actionable, no further recommendations (for either patient or family members) were made for 160/221 (72.4%) and 211/218 (96.8%) of patients with VUS-only and negative results, respectively (p < 0.001) (Table 2). Similar percentages of patients with VUS and negative results (64/160, 40.0% vs. 94/211, 44.5%, p = 1.0) understood that no further recommendations were made, however, the remaining 213/371 (~60%) of patients indicated that they or their family members had acted on or intended to pursue changes in clinical management that were not recommended by their clinician.
Psychosocial impact
Most patients (452/485, 93.2%) reported that their test results either reduced or did not change their concerns about their PCa diagnosis, treatment, and follow-up (Table 3). Patients with negative results (107/215, 49.8%) reported reduced concerns at a significantly higher rate than those with positive results (11/55, 20.0%, p = 0.0009). Conversely, patients with positive results (10/55, 18.2%) reported increased concerns at a significantly higher rate than those with negative results (9/215, 4.2%, p = 0.011).
Results were similar regarding the impact of post-test counseling/discussions with physicians, with a non-significant reduction in the percentage of patients reporting increased concern after these interactions (33/485, 6.8% pre-test versus 22/463, 4.8% post-test, p = 0.211), especially among patients with positive results (10/55, 18.2% versus 7/53, 13.2%, p = 0.60). Overall trends were also similar for how test results and post-test counseling/discussions impacted patient concerns for their family and their hereditary risk for PCa and other cancers (Table 4).
Discussion
This prospective study is, to our knowledge, the first to examine PROs in the context of universal testing for hereditary forms of PCa in the community setting, where the majority of cancer is treated and where GGT is likely to significantly increase over time [14]. Importantly, results from 494 survey respondents showed that universal GGT did not appear to cause undue psychosocial harm to patients. However, our results suggest that improvements are needed in how test results and clinical recommendations are communicated to improve both clinician and patient comprehension of the implications of test results and adherence to clinician recommendations.
Over 90% of patients with PCa and positive GGT results reported that they completed or planned to complete at least one clinical recommendation, suggesting they were motivated to take action, especially treatment recommendations or testing of family members (>50% uptake for each). Indeed, qualitative studies of men with PCa have found that they perceive the primary benefits of GGT to be therapeutic implications and familial impact [15, 16].
In contrast to the high rate of patients with positive results adherent to clinical recommendations (92.9%), patient recall and comprehension of positive test results were lower (62.7%). Moreover, for almost 25% of patients with positive results, no clinical recommendations were made, including patients with PGV in CHEK2 or PALB2, for which gene-specific clinical recommendations are available for both patients and family members. The omission of any recommendations for these patients may be the result of a lack of provider knowledge, as Loeb et al. recently showed that less than 40% of 132 U.S. urologists surveyed knew that hereditary PCa may be linked to pancreatic, colorectal, endometrial, and other cancers [17]. A recent study demonstrated that rates of GGT are increasing in men with PCa and that the proportion of tests ordered by urologists increased from 0% in 2015 to 8.3% in 2020 [18]. Together, these data highlight the critical need for additional educational resources so that urologists provide GGT-informed recommendations to their patients, ensuring that patients and family members with positive results are not deprived of available treatment and prevention strategies that could improve outcomes.
This need for improved understanding of GGT was even more apparent in patients with VUS-only results. In this group, only 22.5% of patients demonstrated both accurate recall and understanding of their results. Incorrect recall and interpretation of VUS results are common in patients who have undergone GGT with multi-gene hereditary cancer panels [10, 19]. In addition, given that the majority of VUS will eventually be reclassified as benign, physicians should not make any clinical decisions based on VUS results [20]. In this study, however, clinicians recommended changes to treatment and to follow-up for 3.2% and 23.1% of patients with VUS-only results, respectively, similar to results found in our earlier study evaluating the impact of GGT results on clinician recommendations [9]. Troublingly, in our current evaluation of PROs, 60% of patients with VUS-only results indicated that they would be making changes to management that were not clinically recommended. These results highlight the need for additional education for both clinicians and patients.
Finally, more than 90% of respondents reported that their GGT results did not increase their level of concern for themselves or their families. This is in line with results from a survey of 105 patients who underwent universal GGT for breast cancer in Australia [21], in which 83.8% of breast cancer patients reported reduced or unchanged levels of cancer-specific stress after GGT [21]. Interviews with 13 PCa patients who had undergone GGT revealed that for most patients, receiving test results was not nearly as impactful as receiving the original cancer diagnosis [11]. Additional pan-cancer studies also demonstrated that results of GGT for cancer predisposition do not have short-term or long-term psychological impact [22, 23].
Several study limitations may have impacted the interpretation of our data. Patients who responded to the survey differed from non-responders for a number of baseline characteristics, including a significantly lower proportion of Black men in the responders group. Although our study was not designed to investigate whether and how race/ethnicity and structural barriers, such access to healthcare, influenced patient comprehension of GGT results or uptake of GGT-informed clinical recommendations, other studies have noted that non-White individuals and individuals with income <$20,000 were less likely to be aware of or to have undergone genetic testing than White and individuals with higher incomes [24] and that non-White patients with positive GGT results had lower rates of genetic counseling for both patients and family members [25]. In conjunction, small sample sizes precluded more detailed evaluation of how clinical or demographic factors influenced patient recall and comprehension of GGT results or uptake of clinical recommendations. Future studies with larger sample sizes are needed to determine how patient demographics influence patient recall and comprehension of GGT results and uptake of clinical recommendations. Finally, our study did not measure clinician familiarity with GGT-informed patient management; thus, we were not able to evaluate why clinicians made recommendations for treatment and GGT for family members for only 12.7% and 65.5% of patients with positive results or recommended follow-up care changes for 23.1% of patients with VUS-only results. A survey of US urologists found that 33% of respondents did not perform GGT or refer their patients to genetic counselors, and only 4% received formal education in genetics [17]. Together, these data highlight the need for increased genetics education in the understanding and utilization of GGT in patients with PCa, which is especially important with the emergence of universal GGT for PCa, and ensuring optimal management for patients with not only positive, but also VUS-only and negative results as well.
In conclusion, this study demonstrated that while universal GGT for patients with PCa, including those with positive results, did not significantly increase patient concerns, improvements in the communication of GGT results and clinical recommendations to patients and strategies to increase patient comprehension are needed. Results from several studies that are evaluating the efficacy of new methods of clinician education [26], alternative delivery models for genetic counseling [7, 27,28,29,30], as well as an ongoing randomized controlled trial of a web-based tool versus traditional genetic counseling for GGT for patients with PCa [31] will be critical in improving the delivery of and response to GGT results in patients with PCa.
Data availability
When not prohibited by patient permissions or privacy laws, the de-identified individual data that underlie the results reported in this article may be made available to researchers. Researchers will be asked to submit a short proposal outlining objectives, research questions, and analytical methods, and submit institutional review board approval or determination of exempt status or nonhuman subjects research. For more information on how to access the data, please contact the corresponding author.
References
Giri VN, Knudsen KE, Kelly WK, Cheng HH, Cooney KA, Cookson MS, et al. Implementation of germline testing for prostate cancer: Philadelphia Prostate Cancer Consensus Conference 2019. J Clin Oncol. 2020;38:2798–811.
Eastham JA, Auffenberg GB, Barocas DA, Chou R, Crispino T, Davis JW, et al. Clinically localized prostate cancer: AUA/ASTRO Guideline, Part I: introduction, risk assessment, staging, and risk-based management. J Urol. 2022;208:10–18.
Schaeffer EM, Srinivas S, Adra N, An Y, Barocas D, Bitting R, et al. Prostate cancer, version 4.2023, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Cancer Netw. 2023;21:1067–96.
Tuffaha H, Edmunds K, Fairbairn D, Roberts MJ, Chambers S, Smith DP, et al. Guidelines for genetic testing in prostate cancer: a scoping review. Prostate Cancer Prostatic Dis. 2023. https://doi.org/10.1038/s41391-023-00676-0.
Shore N, Gazi M, Pieczonka C, Heron S, Modh R, Cahn D, et al. Efficacy of National Comprehensive Cancer Network Guidelines in identifying pathogenic germline variants among unselected patients with prostate cancer: the PROCLAIM trial. Eur Urol Oncol. 2023;6:477–83.
Nicolosi P, Ledet E, Yang S, Michalski S, Freschi B, O’Leary E, et al. Prevalence of germline variants in prostate cancer and implications for current genetic testing guidelines. JAMA Oncol. 2019;5:523–8.
Giri VN, Morgan TM, Morris DS, Berchuck JE, Hyatt C, Taplin M-E. Genetic testing in prostate cancer management: considerations informing primary care. CA Cancer J Clin. 2022;72:360–71.
Finch A, Clark R, Vesprini D, Lorentz J, Kim RH, Thain E, et al. An appraisal of genetic testing for prostate cancer susceptibility. npj Precis Oncol. 2022;6:43.
Shore N, Pieczonka C, Heron S, Gazi M, Cahn D, Belkoff LH, et al. Clinician-reported management recommendations in response to universal germline genetic testing in patients with prostate cancer. J Urol. 2024;212:832–43.
Giri VN, Obeid E, Hegarty SE, Gross L, Bealin L, Hyatt C, et al. Understanding of multigene test results among males undergoing germline testing for inherited prostate cancer: Implications for genetic counseling. Prostate. 2018;78:879–88.
Leader AE, Mercado J, Klein A, Hyatt C, Gross L, Brandt R, et al. Insight into how patients with prostate cancer interpret and communicate genetic test results: implications for families. J Community Genet. 2022. https://doi.org/10.1007/s12687-022-00603-1.
Lincoln SE, Kobayashi Y, Anderson MJ, Yang S, Desmond AJ, Mills MA, et al. A systematic comparison of traditional and multigene panel testing for hereditary breast and ovarian cancer genes in more than 1000 patients. J Mol Diagn. 2015;17:533–44.
Nykamp K, Anderson M, Powers M, Garcia J, Herrera B, Ho Y-Y, et al. Sherloc: a comprehensive refinement of the ACMG–AMP variant classification criteria. Genet Med. 2017;19:1105–17.
Szymaniak BM, Facchini LA, Giri VN, Antonarakis ES, Beer TM, Carlo MI, et al. Practical considerations and challenges for germline genetic testing in patients with prostate cancer: recommendations from the Germline Genetics Working Group of the PCCTC. JCO Oncol Pract. 2020;16:811–9.
Harrison C, Bartley N, Jacobs C, Best M, Vatter S, Meiser B, et al. Family communication and results disclosure after germline sequencing: a mixed methods study. Patient Educ Couns. 2023;114:107800.
Greenberg S, Slager S, Neil BO, Cooney K, Maughan B, Stopa N, et al. What men want: Qualitative analysis of what men with prostate cancer (PCa) want to learn regarding genetic referral, counseling, and testing. Prostate. 2020;80:441–50.
Loeb S, Byrne N, Walter D, Makarov DV, Wise DR, Becker D, et al. Knowledge and practice regarding prostate cancer germline testing among urologists: gaps to address for optimal implementation*,**. Cancer Treat Res Commun. 2020;25:100212
Roberts JL, Wang L, Rose B, Siebert T, Madlensky L, Nielsen SM, et al. Germline genetic testing for prostate cancer: ordering trends in the era of expanded hereditary cancer screening recommendations. Urol Oncol. 2024;211:e510.
Gould D, Walker R, Makari-Judson G, Seven M. Experiences of individuals with a variant of uncertain significance on genetic testing for hereditary cancer risks: a mixed method systematic review. J Community Genet. 2022;13:371–9.
Nicolosi P, Heald B, Esplin ED. What is a variant of uncertain significance in genetic testing? Eur Urol Focus. 2022;8:654–6.
De Silva DL, Stafford L, Skandarajah AR, Sinclair M, Devereux L, Hogg K, et al. Universal genetic testing for women with newly diagnosed breast cancer in the context of multidisciplinary team care. Med J Aust. 2023;218:368–73.
López-Fernández A, Villacampa G, Salinas M, Grau E, Darder E, Carrasco E, et al. Role of psychological background in cancer susceptibility genetic testing distress: It is not only about a positive result. J Genet Couns. 2023;32:778–87.
Culver JO, Ricker CN, Bonner J, Kidd J, Sturgeon D, Hodan R, et al. Psychosocial outcomes following germline multigene panel testing in an ethnically and economically diverse cohort of patients. Cancer. 2021;127:1275–85.
Tiner JC, Mechanic LE, Gallicchio L, Gillanders EM, Helzlsouer KJ. Awareness and use of genetic testing: an analysis of the Health Information National Trends Survey 2020. Genet Med. 2022;24:2526–34.
Liu YL, Maio A, Kemel Y, Salo-Mullen EE, Sheehan M, Tejada PR, et al. Disparities in cancer genetics care by race/ethnicity among pan-cancer patients with pathogenic germline variants. Cancer. 2022. https://doi.org/10.1002/cncr.34434.
Giri VN, Gross L, Cheng HH, Russo J, Paller CJ, Johnson JM, et al. Virtual genetics board for enhancing knowledge and practice of prostate cancer genetic testing: the ENGAGEMENT study. J Clin Orthod. 2022;40:184.
Stoll K, Kubendran S, Cohen SA. The past, present and future of service delivery in genetic counseling: Keeping up in the era of precision medicine. Am J Med Genet C Semin Med Genet. 2018;178:24–37.
Breen KE, Symecko H, Spielman K, Gebert R, Shah IH, Pundock S, et al. Clinical impact of a rapid genetic testing model for advanced prostate cancer patients. J Urol. 2023;209:918–27.
Abusamra SM, Solorzano MA, Luke M, Quarles J, Jacobs MF, Das S, et al. Satisfaction with clinician-led germline genetic counseling in patients with prostate cancer. J Urol. 2022;208:1007–17.
Scheinberg T, Goodwin A, Ip E, Linton A, Mak B, Smith DP, et al. Evaluation of a mainstream model of genetic testing for men with prostate cancer. JCO Oncol Pract. 2021;17:e204–16.
Loeb S, Cheng HH, Leader A, Gross L, Nolasco TS, Byrne N, et al. Technology-enhanced AcceleRation of Germline Evaluation for Therapy (TARGET): a randomized controlled trial of a pretest patient-driven webtool vs. genetic counseling for prostate cancer germline testing. Contemp Clin Trials. 2022;119:106821.
Funding
This study was funded by Invitae Corp., now part of Labcorp.
Author information
Authors and Affiliations
Contributions
NDS was the principal investigator of the PROCLAIM trial, contributed clinical and patient survey data and reviewed the manuscript; CMP, SH, MG, DJC, LHB, ADB, BM, JV, DM, RB-T, AE, PD, and DRW contributed patients, clinical and patient survey data and reviewed the manuscript; MKH provided clinical research support and database management; KWA contributed to the original manuscript draft, BH, RLN, and EDE reviewed and revised the manuscript, KEH and BB provided statistical support and reviewed and revised the manuscript, SMN provided overall project supervision, data collection and analysis, manuscript drafting and revision.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval for PROCLAIM was approved by WCG IRB (Puyallup, WA; protocol 20191596). All patients provided informed consent to have their de-identified data used in this study. This study was performed in accordance with the Declaration of Helsinki.
Competing interests
NS is a consultant or advisor for AbbVie, Amgen, Astellas Pharma, AstraZeneca, Bayer, Bristol Myers Squibb, Boston Scientific, Clovis Oncology, Cold Genesys, Dendreon, EMD Serono, Merck, Exact Imaging, Exact Sciences, FerGene, Foundation Medicine, GConcology, Genentech, GenesisCare, Genomic Health, Guardant Health, Invitae, Janssen, MDxHealth, Merck, Moivant, Myriad Genetics, Nymox, Pacific Edge, Phosphorus, Pfizer, Propella, Sanofi Genzyme, Sesen Bio, Tolmar, and UroGen Pharma. CMP has received research funding from Astellas Pharma, AstraZeneca, Bayer, Dendreon, Eli Lilly, Invitae, Janssen, Merck, Myovant Sciences, Myriad Genetics, Pfizer, and Veru, and is a consultant for Astellas Pharma, AstraZeneca, Bayer, Dendreon, Foundation Medicine, Janssen, Large Urology Group Practice Association, Merck, Myovant Sciences, Pfizer, Sun, and UroGPO. DJC is a consultant for Janssen and AstraZeneca. LHB is a consultant for Marius Pharmaceuticals. ADB is a speaker for Astellas Pharma, Janssen, Myovant Sciences, and Pfizer. BM is a consultant for NeoTract/Teleflex, Calyxo, MagForce USA, and UroDev Medical, and is Medical Director and an equity holder for Convergent Genomics. DM is a consultant for Astellas Pharma, AstraZeneca, Clovis Oncology, Decipher, Janssen, and Myriad Genetics. AE is a consultant for Myriad Genetics and an investigator for Palette Life Sciences. PD is a speaker for Astellas Pharma, Bayer, Dendreon, Exact Imaging, Janssen, Myovant, and Pfizer; and a consultant for Dendreon, Exact Imaging, and Myovant. DRW is a consultant for Foundation Medicine, Janssen, Labcorp, Leap Therapeutics, Myovant, and Pfizer. KWA, BH, KEH, and RLN were employees of Invitae Corp., now part of Labcorp. BB, EDE, and SMN are current employees of Labcorp. EDE is an advisor and stockholder of Taproot Health, Exir Bio, and ROMTech.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Shore, N.D., Pieczonka, C.M., Heron, S. et al. Using patient-reported outcomes from the PROCLAIM trial to assess the impact of universal germline genetic testing for prostate cancer patients. Prostate Cancer Prostatic Dis (2025). https://doi.org/10.1038/s41391-025-01013-3
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41391-025-01013-3
This article is cited by
-
Best of 2025 in prostate cancer and prostatic diseases
Prostate Cancer and Prostatic Diseases (2026)