Abstract
TP53 gene alteration confers inferior prognosis in refractory/relapse aggressive B-cell non-Hodgkin lymphoma (r/r B-NHL). From September 2016 to September 2020, 257 r/r B-NHL patients were assessed for eligibility for two trials in our center, assessing anti-CD19 and anti-CD22 chimeric antigen receptor (CAR19/22) T-cell cocktail treatment alone or in combination with autologous stem cell transplantation (ASCT). TP53 alterations were screened in 123 enrolled patients and confirmed in 60. CAR19/22 T-cell administration resulted in best objective (ORR) and complete (CRR) response rate of 87.1% and 45.2% in patients with TP53 alterations, respectively. Following a median follow-up of 16.7 months, median progression-free survival (PFS) was 14.8 months, and 24-month overall survival (OS) was estimated at 56.3%. Comparable ORR, PFS, and OS were determined in individuals with or without TP53 alterations, and in individuals at different risk levels based on functional stratification of TP53 alterations. CAR19/22 T-cell treatment in combination with ASCT resulted in higher ORR, CRR, PFS, and OS, but reduced occurrence of severe CRS in this patient population, even in individuals showing stable or progressive disease before transplantation. The best ORR and CRR in patients with TP53 alterations were 92.9% and 82.1%, respectively. Following a median follow-up of 21.2 months, 24-month PFS and OS rates in patients with TP53 alterations were estimated at 77.5% and 89.3%, respectively. In multivariable analysis, this combination strategy predicted improved OS. In conclusion, CAR19/22 T-cell therapy is efficacious in r/r aggressive B-NHL with TP53 alterations. Combining CAR-T cell administration with ASCT further improves long-term outcome of these patients.
Similar content being viewed by others
Introduction
Individuals with aggressive B-cell Non-Hodgkin’s Lymphoma (B-NHL) in either primary refractory or relapse status have poor prognosis. Salvage high-dose chemotherapy (HDT) with subsequent autologous stem cell transplantation (ASCT) is considered the standard therapeutic option for chemosensitive cases in the rituximab era1,2. However, in cases resistant to chemotherapy, the role of ASCT remains controversial and this salvage regimen does not show additional benefits, indicating a need for treatments with higher efficacy. Recently, chimeric antigen receptor (CAR) T-cell treatment has achieved unprecedented response in r/r B-NHL. In ZUMA-1, axicabtagene ciloleucel (Axi-cel), a first-in-class CD19-targeted CAR (CAR19) T-cell product, achieved an objective response rate (ORR) of 82% and a median overall survival (OS) greater than 2 years in r/r aggressive B-NHL following ≥2 lines of systemic therapies. Following a median follow-up of 55.1 months, median OS time and 4-year OS rate were 25.8 months, and 44%, respectively3,4. In particular, in high-risk cases, CAR T-cell treatment offers potential solutions5. In ZUMA-12, Axi-cel was administered as first-line treatment in high-risk large B-cell lymphoma (LBCL) patients, of whom about 60% had double- or triple-hit lymphoma (DHL/THL). An interim analysis indicated Axi-cel has significant clinical benefits in these unfavorable patients, with high treatment response rate and a manageable safety profile6.
However, in TP53-disrupted B-cell malignancies, CAR T-cell treatment has yielded controversial results. We previously reported an acute B-cell lymphoblastic lymphoma case who achieved minimal residual disease (MRD)-negative CR for 15 months after receiving a CAR19/22 T-cell treatment in the context of Li-Fraumeni syndrome, a rarely diagnosed autosomal dominant condition predisposing the carrier to malignant disease and commonly associated with germline TP53 mutations7. This study suggested a potentially effective role for CAR T-cell treatment in such patients7. However, relapse remains a challenge in patients with TP53-disrupted r/r B-cell acute lymphoblastic leukemia (B-ALL) after receiving CAR19 T-cell therapy, even consolidated with allogeneic hematopoietic stem cell transplantation8,9. The effect of CAR-T cell treatment, especially CAR-T with dual-targeting strategies, in r/r B-NHL cases with TP53 alterations remains unclear and needs to be systematically investigated.
The evolutionarily conserved TP53 gene, also called the ‘guardian of the genome’, represents a key tumor suppressor gene regulating cell cycle arrest, DNA repair pathways, apoptotic death, senescence, and autophagy in cells under stress conditions10,11,12. In humans, TP53 is the most frequently disrupted gene in malignant diseases being altered in 20–25% of individuals with aggressive B-NHL13,14,15. A higher incidence of TP53 mutation is likely to be found in r/r B-NHL16,17. Meanwhile, genomic instability caused by TP53 alterations induces chemoresistance and progression in cancer18,19. Multiple reports have shown disruption of TP53 is involved in lymphomagenesis and treatment resistance, and increased upon relapse in diffuse large B-cell lymphoma (DLBCL) and other lymphoid malignancies20,21,22. In DLBCL, TP53 gene alterations, including TP53 mutations and/or del(17p), are detected in approximately 30–50% of patients and mostly result in inferior outcome upon treatment with rituximab plus cyclophosphamide, hydroxydaunorubicin, vincristine, and prednisone (R-CHOP)13,14,23. However, even after high-dose therapy (HDT)/ASCT, the prognosis of these patients remains unfavorable. In the multicenter, open label, randomized, phase 3 DLCL04 trial, individuals with untreated DLBCL at high-risk were consolidated with HDT/ASCT as first-line treatment24. As the result, 5-year OS rates were 81 and 33% in wild type (TP53wt) and mutant (TP53mut) TP53 cases, respectively. The 5-year failure-free survival (FFS) rates were 73% for TP53wt patients and 19% for TP53mut cases25. Similarly, patients with TP53-disrupted mantle cell lymphoma (MCL) or Burkitt lymphoma (BL) may not benefit from intensive chemotherapy, ASCT, or other targeted treatment strategies26,27,28,29. Due to the poor outcome conferred by TP53 alterations, attempts to manage these patients are unfruitful30.
The safety and efficacy of two clinical studies examining CAR19/22 T-cell treatment alone (Trial A) or combined with ASCT (Trial B) in B-cell malignancies were examined in our recent report31,32. To assess the prognostic effect of TP53 gene disruption and develop a therapeutic strategy for these patients, the present work systemically assessed the efficacy and safety of these 2 regimens in this patient population with increased sample size and follow-up time.
Results
Enrollment and baseline features
From September 2016 to September 2020, 257 r/r B-NHL patients were assessed for eligibility for two trials. Supplemental Fig. 1 shows the schematic diagrams of the study procedures in both trials. TP53 alterations, including TP53 mutation and del(17p), were screened in 123 enrolled patients and confirmed in 60. Supplemental Fig. 2 shows a flowchart of patient enrollment and group assignment. In Trial A, 32 patients (48.5%) carried TP53 alterations (group B), while 34 (51.5%) did not (group A). In Trial B, 28 patients (49.1%) carried TP53 alterations (group C), while 29 (50.9%) did not (group D). The cutoff date for follow-up was April 30, 2021.
The patient baseline features are listed in Table 1. All features were balanced among the 4 groups (Table 1). Of the patients with TP53 alterations in both trials, 7 had prior ASCT, including 1 in Trial B. All had measurable disease, and 11 (18.3%) showed a stable (SD) or progressive (PD) disease at enrollment. Of note, although showing a SD/PD at enrollment, 5 patients (17.9% in group C) were enrolled in Trial B, a study involving ASCT.
Profiles of TP53 alterations
Heterozygous gene mutations and/or deletions in TP53 are depicted in Fig. 1a. Totally 42 (70.0%) individuals harbored TP53 mutation(s) or sole del(17p), with 27 (45.0%) and 15 (25.0%) showing TP53 mutation(s) and deletions, respectively (Fig. 1b). The remaining 18 (30.0%) cases had biallelic TP53 aberrations. Among the 51 mutations identified, 45 (88.0%) were in the DNA-binding domain (DBD; amino acids 101–294), as reflected in Fig. 1c. Compound heterozygous mutations were found in 6 patients (10.0%). Germline TP53 variations were validated in 2 patients (3.3%). In total, 40 (66.7%) cases had loss-of-function alterations inactivating TP53, with decreased copy number loss or truncations. Comparable TP53 mutation patterns were observed based on treatment strategies (trial A vs trial B) or different clinical outcomes (responders vs non-responders or no relapse vs relapse) (Supplemental Fig. 3).
Mutational profile of TP53 alterations. a Heatmap showing individual non-synonymous somatic mutations found in individuals administered CAR-T cell infusion (n = 60). Each row represents one type of TP53 alterations, and each column represents a patient with R/R B-NHL. The horizonal bar graph shows gene mutation frequencies. b Venn diagram demonstrates different TP53 alterations identified in 60 cases. Totally 42 (70.0%) individuals harbored TP53 mutation(s) or sole del(17p), with 27 (45.0%) and 15 (25.0%) showing TP53 mutation(s) and deletions, respectively. The remaining 18 (30.0%) cases had biallelic TP53 aberrations (TP53 mutation and del(17p) in the first and second alleles, respectively). c TP53 mutations are plotted above the protein divided into the main domains. Among the 51 mutations identified, 37 were missense mutations (yellow), 6 were splice-site mutations (blue), 4 were nonsense mutations (red), 3 were frameshift insertions or deletions (indels; purple), and 1 was a non-frameshift indel (green). Recurrent mutations were identified in 3 codons, including R273 (n = 6), R248 (n = 4) and R175 (n = 3). The x-axis indicates the amino acid position
Infusion and kinetics of CAR T cells and engraftment of hematopoietic stem cells (HSCs)
Patients in Trial A received 4.1 (1.4–8.9) × 106/kg CAR19 T cells and 6.0 (1.0–11.4) × 106/kg CAR22 T cells, and those in Trial B received similar doses, i.e., 4.0 (1.0–12.6) × 106/kg CAR19 T cells and 4.0 (0.8–10.0) × 106/kg CAR22 T cells. Median manufacturing times were 13 days (range: 8–20 days) and 12 days (range: 9–22 days) for CAR19 T and CAR22 T cells, respectively. Transduction efficiencies for CAR19 and CAR22 T cells averaged 46.2 ± 19.6% and 47.6 ± 20.4%, respectively. The mean viability rates of CAR-T cells were 92.7 ± 2.5% for CAR19 T cells and 93.1 ± 3.4% for CAR22 T cells. The CD4/CD8 ratios for CAR19 T and CAR22 T cells were 1.8 ± 0.1 and 1.8 ± 0.2 in totally 37 cases, respectively. Cell dosages (Table 1), median times to reach peak expansion, and median copies of peak expansion for CAR19 and CAR22 T cells in peripheral blood were similar between different groups in both 2 trials, suggesting comparable kinetics and expansion of CAR19 and CAR22 T cells in both trials (Supplemental Fig. 4). Additionally, the median dosage of autologous stem cells (CD34+ cells) in trial B was 7.4 (2.2–13.0) × 106/kg. Administration of the CAR19/22 T-cell cocktail was generally initiated at day +3 (range: days +2 to +6). All trial B patients had successful HSC engraftment. The median durations of neutrophil or platelet engraftment were 12 days (range: 7–33 days) and 16 days (range: 9–42 days), respectively.
Treatment effects of the CAR T-cell cocktail
In Trial A, 57 cases (87.7%, 95% CI: 77.6–93.6%) achieved best objective response (OR) to CAR19/22 T-cell therapy, including 31 (47.7%, 95% CI: 36.0–59.6%) with a CR (Supplemental Fig. 5). There was no marked difference in best OR rate (ORR, CR + PR) between cases with or without TP53 disruption (87.1% in group B vs. 88.2% in group A, P = 0.927, Fig. 2a). At the last follow up, 15 cases (48.4%, 95% CI: 32.0–65.2%) maintained their initial responses while 16 (51.6%, 95% CI: 34.8–68.0%) experienced disease progression.
Outcomes of r/r aggressive B-cell lymphoma cases according to TP53 alteration status after CAR19/22 T-cell infusion. a Best responses in r/r aggressive B-cell lymphoma cases with or without TP53 alterations. Kaplan–Meier analysis of DOR (b), PFS (c), and OS (d) in r/r aggressive B-cell lymphoma cases on the basis of TP53 alteration status. ORR, objective response rate; OR objective response; CR complete response; PR partial response; SD stable disease; DOR duration of response; W/O without
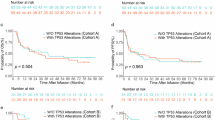
In patients with disrupted TP53 (group B), following a median follow-up of 16.7 months (range: 3.1–41.0 months), median DOR and OS were not reached (Fig. 2b, d). Median PFS was 14.8 months (95%CI: 5.1–NE) (Fig. 2c). In these cases, 24-month PFS and OS estimates were 48.4% (95% CI: 30.2–64.4%) and 56.3% (95% CI: 36.6–72.0%), respectively (Fig. 2c, d). Of note, DOR, PFS, and OS were comparable in the wild type and TP53 alteration groups when treated with CAR19/22 T-cell cocktail therapy (Fig. 2b–d). In addition, similar trends of best ORR, DOR, and survival were exhibited among the 54 patients in Trial A who had r/r DLBCL, irrespective of TP53 gene status (Supplemental Fig. 6a–d). Similarly, in each functional classification system of TP53 alterations, best ORR (Supplemental Fig. 7a) and survival features (Fig. 3a–h) were comparable in cases with different risk levels, suggesting CAR19/22 T-cell treatment overcame the negative effects of TP53 disruption in aggressive B-cell lymphoma.
Outcomes of r/r aggressive B-cell cases stratified by four functional classification systems of TP53 alterations after CAR19/22 T-cell infusion. In individuals with r/r aggressive B-cell lymphoma and concurrent TP53 mutations, PFS (a, c and e) and OS (b, d, and f) were compared according to functional classifications of TP53 mutations. Kaplan–Meier analysis of PFS (a) and OS (b) for the non-missense and missense mutation groups. Kaplan–Meier analysis of PFS (c) and OS (d) for the non-disruptive and disruptive mutation groups. Kaplan–Meier analysis of PFS (e) and OS (f) for EAp53 low-risk (<75) and EAp53 high-risk (≥75) mutation groups. Kaplan–Meier analysis of PFS (g) and OS (h) in the del(17p) and non-del(17p) groups
Superior effects of ASCT incorporating CAR19/22 T-cell treatment
Among the 28 individuals with r/r aggressive B-NHL and concurrent TP53 alterations (group C in Trial B), 26 (92.9%, 95%CI: 77.4–98.7%) showed best ORR when treated with ASCT incorporating CAR19/22 T-cell cocktail treatment (Trial B), including 23 (82.1%, 95%CI: 64.4–92.1%) CR cases (Fig. 4a). After a median follow-up of 21.2 (range: 4.0–48.7) months, median DOR, PFS, and OS were not reached (Fig. 4b–d). In these cases, 24-month PFS and OS estimates were 77.5% (95% CI: 56.5–89.3%) and 89.3% (95% CI: 70.4–96.4%) (Fig. 4c, d), respectively. At the last follow-up, 22 cases (78.6%, 95%CI: 60.5–89.8%) maintained the initial responses while 6 (21.4%, 95%CI: 10.2–39.5%) had disease progression. Surprisingly, in comparison with CAR19/22 T-cell cocktail treatment (group B), marked increased DOR (P = 0.040, Fig. 4b), PFS (P = 0.024, Fig. 4c) and OS (P = 0.012, Fig. 4d) were observed after CAR T-cell therapy incorporation in ASCT (group C). Similarly, comparable best ORR, DOR, PFS, and OS were detected in the wild type and TP53 alteration groups administered ASCT incorporated with CAR19/22 T-cell cocktail infusion (Fig. 5a–d). In each functional classification system of TP53 alterations, best ORR (Supplemental Fig. 7b) had no marked difference in trial B cases of distinct risk levels.
Outcomes of r/r aggressive B-cell lymphoma cases based on TP53 alteration status after ASCT combined with CAR19/22 T-cell infusion. a Best responses in r/r aggressive B-cell lymphoma cases with or without TP53 alterations. Kaplan–Meier analysis of DOR (b), PFS (c), and OS (d) is shown. ORR objective response rate; OR objective response; CR complete response; PR partial response; SD stable disease; DOR duration of response; W/O without
Likewise, in patients with r/r DLBCL and concurrent TP53 alterations, superior best response (P < 0.001, Supplemental Fig. 8a) and DOR (P = 0.039, Supplemental Fig. 8b), and trends for better PFS (P = 0.086, Supplemental Fig. 8c) and OS (P = 0.076, Supplemental Fig. 8d) were demonstrated when administered ASCT incorporating CAR19/22 T-cell cocktail infusion. Of note, in cases with a SD/PD at enrollment in Trial B, best ORR, and best CR rate were 100% (95%CI: 56.6–100%) and 80.0% (95%CI: 37.6–99.0%), respectively. Similar PFS (P = 0.892, Supplemental Fig. 9a) and OS (P = 0.510, Supplemental Fig. 9b) were obtained in patients with a PR or PD/SD at enrollment, suggesting that even in patients with a SD/PD at enrollment, durable remission could be obtained with CAR T-cell therapy incorporation in ASCT.
Predictive factors for response and survival
In cases with disrupted TP53, those with maintained OR at month 3 (R3m, i.e., “durable complete or partial response at month 3) (responders) had significantly extended PFS (P < 0.001, Supplemental Fig. 10a) and OS (P < 0.001, Supplemental Fig. 10b) when compared with patients who failed to have R3m (non-responders). Similarly, improved PFS and OS were found in cases with R6m compared to those who failed to have R6m (Supplemental Fig. 10c, d). Compared with non-responders, responders tended to have more persistent CAR19 (75.0% vs. 33.3%, P = 0.047) and CAR22 (87.5% vs. 31.4%, P = 0.0004) transgenes (Supplemental Fig. 11a) at month 3. Accordingly, fewer non-responders showed durable B-cell aplasia (BCA) at month 3 than responders (62.5% vs. 94.1%, P = 0.028, Supplemental Fig. 11b). Different TP53 alteration patterns exhibited comparable ORRs at month 3 (Supplemental Table 1). However, R3m was affected by CRS severity (≥ grade 3) after CAR19/22 T-cell treatment (P = 0.013, Supplemental Table 2), while being consistent in different subgroups administered ASCT incorporating CAR19/22 T-cell cocktail infusion (Supplemental Table 3).
Additionally, survival-associated clinical features were identified by univariable and multivariable analyses in individuals with aggressive r/r B-NHL and concurrent TP53 alterations (Table 2). OS was remarkably associated with R3m (HR14.50, 95%CI: 4.3–49.1, P < 0.0001), enrolled trial (HR 4.40, 95% CI: 1.2–16.0, P = 0.025) and performance status (HR 1.17, 95% CI: 1.0–3.1, P = 0.0498) in multivariable analysis (Table 2). In log-rank survival analysis, OS was significantly improved in patients who showed R3m (P < 0.0001, Supplemental Fig. 10b), received ASCT incorporating CAR19/22 T-cell cocktail treatment (P = 0.012, Fig. 4d), or showed an Eastern Cooperative Oncology Group performance status (ECOG PS) of 0–1 (P = 0.011, Supplemental Fig. 12).
Safety profiles
Comparable safety profiles were observed in both trials (Supplemental Table 4). The commonest adverse events were cytopenia, including neutropenia, lymphopenia, thrombocytopenia, and anemia. Anemia and severe thrombocytopenia were more common in Trial B than in Trial A due to 2 different conditioning regimens. No marked differences in other adverse effects were found between these 2 trials. Infection of grade 3 or higher was found in 4.54% Trial A and 7.14% Trial B cases. One patient in Trial A had grade 5 infection (invasive fungal infection) and succumbed to septic shock within 30 days.
Most patients in both groups developed CRS, with 90.9% (95%CI: 81.6–95.8%) in Trial A and 94.7% (95%CI: 85.6–98.6%) in Trial B (Supplemental Table 4). In Trial A cases, median onset of CRS occurred on day 4 (range: 2–8 days), with median resolution on day 10 (range: 6–24 days) post-infusion. In Trial B, median onset of CRS occurred on day 5 (range: 3–10 days), with median resolution on day 9 (range: 5–20 days). Group C patients had decreased incidence of severe CRS (grade ≥3) compared with group B cases (10.7% vs. 37.5%, P = 0.020, Supplemental Fig. 13). Similar incidence rates of immune effector cell-associated neurotoxicity syndrome (ICANS) were obtained in both trials, with 9.1% (95% CI: 4.2–18.4%) in Trial A and 19.3% (95% CI: 11.1–31.3%) in Trial B. In both trials, no patients died of CRS or developed severe ICANS (grade ≥3).
Discussion
TP53 represents the top candidate gene frequently disrupted in aggressive B-cell lymphomas including r/r DLBCL. Its alterations are implicated in treatment failure and remain clonally stable following multiple lines of therapies, suggesting a role in primary chemoresistance, and therefore have close correlations with disease progression and dismal survival rates. Salvage platinum-based chemotherapy with subsequent HDT/ASCT is presently considered as the standard treatment option for second-line chemo-sensitive patients. However, even consolidated with upfront ASCT at the time of first CR (CR1) after chemoimmunotherapy, patients with TP53 mutations have significantly reduced 5-year OS or FFS, indicating upfront ASCT cannot overcome the poor prognosis conferred by TP53 mutations. Since HDT/ASCT hardly provides durable disease control in these high-risk patients and is particularly unfit for chemo-refractory or ASCT ineligible patients, novel treatment strategies are warranted.
CAR T-cell infusion nowadays is becoming the preferred curative option for chemo-refractory or ASCT ineligible patients, or cases that relapse after ASCT. The ZUMA-1, JULIET and TRANSCEND trials indicated ORRs of 41–83% in chemo-refractory patients and ORRs of 53–76% in those with relapse within the first year post-ASCT. Moreover, several clinical trials, including ZUMA-7, BELINDA, and TRANSFORM, are actively assessing whether CAR T-cell therapy could replace salvage HDT/ASCT as second-line treatment in r/r LBCL. Interim analysis of the TRANSFORM study showed the superiority of lisocabtagene maraleucel (Liso-cel) over HDT/ASCT in event-free survival, PFS and CR rate, supporting the potential administration of Liso-cel in earlier lines of therapy in these patients. However, given the genetic heterogeneity of aggressive B-cell lymphomas, it is unclear whether unfavorable genetic aberrations exert uniformly poor outcomes even in the era of adoptive T-cell immunotherapy. Therefore, strategies that can boost the therapeutic effects of CAR T-cell infusion should be actively explored, especially for high-risk cases.
In this study, after CAR19/22 T-cell administration, comparable response and survival data were obtained in patients with or without TP53 alterations, as week as in patients at different risk levels stratified by four functional classification systems of TP53 alterations. These findings suggest CAR19/22 T-cell treatment overcame the unfavorable effect of TP53 disruption in r/r aggressive B-cell lymphoma. We hypothesized that combinational targeting of CD19 and other tumor-associated antigens represents a rational way to cope with TP53-disrupted B-cell lymphoma. Recently, a high incidence of CD19-negative relapse provoked by CD19-loss was observed in TP53-mutatant B-ALL administered CAR19 T cells9. In addition, TP53 mutation enriched in DLBCL with inconsistent expression of CD1933,34. Thus, CD19-negative relapse may be related to irregular CD19 expression in TP53-disrupted B-cell lymphoma and driven by CAR19 T-cell surveillance9,33,34. Previously, we reported that the CAR19/22 T-cell sequential infusion was highly active and well-tolerated in r/r B-cell malignant cases and could circumvent CD19 antigen escape31. Because CD22 and other B-cell markers are usually still expressed on CD19-negative tumor cells9,35, combinational targeting of CD19 and other tumor-associated antigens might be a feasible and superior solution than single-targeting of CD19 in TP53-disrupted B-cell lymphoma, although validation and investigation of underlying mechanism, including with or without ASCT, in prospective randomized control trials is warranted. Our preliminary underlying mechanism suggests that CAR19 and CAR22 T cells sequentially infused had consistent biological contributions, transcriptional patterns, and clinical relevance with the response or resistance to CAR-T cell therapy (unpublished data). However, the dual CAR targeting strategy includes co-administration or co-transduction of two separate CAR T-cells, T cells transduction using a bicistronic plasmid encoding both CARs, or utilization of a tandem CAR36. Novel dual-targeting approaches are being actively examined in preclinical and clinical studies, and the optimal strategy remains undefined and comparatively assessed for clinical benefits31,36,37.
Intriguingly, when ASCT was further combined with CAR19/22 T-cell sequential infusion, superior response and survival were obtained in TP53-disrupted B-cell lymphoma, even in patients with a SD/PD before transplantation, for whom, as indicated in the SCHOLAR-1 study, ASCT alone can hardly provide durable disease control1. In the present study, this combination strategy not only independently predicted improved OS, but also exhibited a reduced occurrence of severe CRS, suggesting potential synergistic effects of ASCT and CAR T-cell therapy. Indeed, multiple studies on metastatic melanoma and B-cell lymphoma have supported the notion that myeloablative ASCT can further augment the effectiveness of adoptive T-cell immunotherapy38,39,40,41. Myeloablative conditioning before the adoptive transfer of CAR T cells has elevated odds of conferring a beneficial cytokine profile to enhance T cell trafficking or the recruitment of innate immune cells into the microenvironment42. In addition, myeloablative conditioning eradicates malignant cells and restrains immunosuppressive elements in the microenvironment that impede the efficiency of CAR T-cell therapy43,44,45. Then, CAR T cells highly activated during hematopoietic reconstitution could further eliminate the residual tumors in both patients and transplants. Finally, reduced tumor load and suppressed regulatory factors, such as monocytes and macrophages, may decrease the rates of CRS and ICANS following CAR T-cell infusion46,47. Thus, this novel combination may result in enhanced response, decreased toxicity, reduced relapse, and sustained remission, although further investigation of similarities and differences comparing other dual CAR targeting strategies with or without ASCT is needed. Consistent with long-term outcomes of ZUMA-1 study as well as commercial anti-CD19 CAR T cell therapy4,48,49,50, three months or six months post CAR T-cell infusion were both feasible and efficient timepoints for predicting long-term outcome of CAR-T cell therapy in aggressive B-cell lymphomas. Besides, the present study also highlighted that better ECOG PS had extended survival which was consistent with real-world studies of axicabtagene ciloleucel51,52.
Taken together, this is the first clinical study investigating and comparing CAR19/22 T-cell cocktail and its combination with ASCT for effectiveness in TP53-disrupted r/r B-cell lymphoma. The results showed CAR19/22 T-cell cocktail was efficacious in this patient population; more importantly, the above findings highlighted great treatment benefits for ASCT combined with CAR T-cell therapy. This study also suggested that, besides TP53-disrupted B-cell lymphoma, this combination strategy could be applied for treating aggressive B-cell lymphoma with unfavorable clinicopathological or genetic features. Nevertheless, the present study had several limitations. It was not a randomized control trial, in which the advantages of this combination strategy over either CAR T-cell treatment or ASCT require further validation. In addition, although clinical features were consistent between subgroups, underlying selection bias could hardly be excluded in trials involving transplantation. Finally, varied prognostic relevance of TP53 alterations may underestimate the potentialities of this combination strategy. In the future, comprehensive genetic studies alongside outcome prediction would help optimize patient selection and achieve individualized treatment in the era of CAR T-cell therapy.
Materials and methods
Study design and enrollment
According to the intention-to-treatment principle and the availability of HSCs, r/r B-NHL cases were enrolled in two separate clinical trials examining CAR19/22 T-cell infusion (Trial A) and ASCT incorporating CAR19/22 T-cell therapy (Trial B), respectively. Inclusion and exclusion criteria of Trial A and Trial B are outlined in Supplementary Methods. Both trials had approval from the institutional review board of Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, and were registered with the Chinese Clinical Trial Registry (ChiCTR, ChiCTR-OPN-16008526, and 16009847). Signed informed consent was provided by each patient. Both trials were conducted based on the Declaration of Helsinki.
Clinical procedures
As previously reported27, leukapheresis was performed in each patient to collect cells for CAR 19/22 manufacturing. The third-generation CAR employed composed a single-chain variable fragment from a mouse monoclonal antibody targeting human CD19 or CD22, two costimulatory (CD28 and 4–1BB) domains, and the CD3ζ chain as the activation domain. CAR construct validation, as well as cell production and quality control steps, were described previously41,42. For patients enrolled in Trial A (CAR19/22 T-cell cocktail infusion), fludarabine (25 mg/m2) and cyclophosphamide (300 mg/m2) were administered for 3 days (days −4 to −2) with subsequent infusion of CAR19/22 T-cells. CAR19 and CAR22 T cells were administered on successive days from day 027. For Trial B patients (CAR19/22 T-cell cocktail infusion with ASCT), BEAM (300 mg/m2 of carmusitine, day −6; 200 mg/m2 of etoposide, days −5 to −2; 400 mg/m2 of cytarabine, days −5 to −2; 140 mg/m2 of melphalan, day −1) at the standard dosage was administered, with subsequent CAR19/22 T-cell infusion (days +2 to +6) following ASCT (day 0). In patients with CAR T following ASCT, CAR19 and CAR22 T cell infusion was carried out within 2–6 days after autologous stem cell infusion28. The detailed schematic diagram of study procedures is depicted in Supplemental Fig. 1.
Laboratory assessments and follow-up
In vivo expansion of CAR19 and CAR22 T cells was assessed by droplet digital polymerase chain reaction (ddPCR) as previously described53. Cytokine detection with specific kits was performed as directed by the manufacturer. Cytokine release syndrome (CRS) grading utilized a scale developed by Lee and collaborators. Immune effector cell-associated neurotoxicity syndrome (ICANS) and additional adverse events (AEs) were assessed according to the American Society for Transplantation and Cellular Therapy (ASTCT) Consensus and the National Cancer Institute Common Terminology Criteria for Adverse Events V4.03. Disease stages and treatment responses were examined based on the US National Comprehensive Cancer Network and Lugano Treatment Response Criteria. Follow-up was performed until patient death, loss to follow-up, or consent withdrawal.
Sequencing and mutational analysis
Panels for targeted sequencing covering the coding sequence (CDS) of the TP53 gene were designed online (Designstudio Sequencing, Illumina, USA) and shown in Supplemental Table 5. Library preparation was carried out with AmpliSeqTM Library PLUS for Illumina, and sequencing was performed on a NextSeqTM 550 system. Alignment and variant calling utilized the DNA Amplicon workflow (default parameters) on the BaseSpace Sequence Hub. The obtained variants underwent annotation with Annovar. Only exonic nonsynonymous or splice donor/acceptor site variants displaying a frequency below 0.001 in the gnomAD database were filtered for further analyses. The detailed procedures were described previously23,54.
Interphase fluorescence in situ hybridization (FISH)
Interphase FISH was performed to assess formalin-fixed, paraffin-embedded (FFPE) tissue sections or methanol and acetic acid-fixed cells for karyotyping. A commercially available 17p13.1 probe (Vysis, Downers, Grove, IL, USA) was utilized for del(17p) detection.
Function classification of TP53 alterations
Since distinct prognostic relevance with genetic variants has been demonstrated for the TP53 gene55,56, 4 functional classification systems were utilized to examine whether CAR T-cell treatment could help overcome the unfavorable prognosis resulting from TP53 gene disruption. In every functional classification system, TP53 alterations were stratified according to predicted effects on the protein. The first comparison involved missense TP53 mutations and non-missense mutations, which include nonsense mutations, splice site mutations, small insertions, and deletions57,58. Secondly, we classified TP53 gene mutations as ‘disruptive’ and ‘non-disruptive’ to assess whether the location of a specific TP53 mutation and the resulting amino acid change had a prognostic value in the current patients, as shown in individuals with AML and solid tumors59,60. The definitions of ‘disruptive mutation’ and ‘non-disruptive mutation’ were reported previously60. Thirdly, we used the evolutionary action score (EAp53), which performs the functional classification of missense mutations and has been validated in head and neck cancer or AML cases61. This system considers evolutionary sensitivity to sequence alteration and amino acid conservation, scoring mutations between 0 (TP53wt sequence) and 100. The EAp53 score of a specific TP53 missense mutation was obtained from the server of the German-Austrian AML Study Group (AMLSG) (http://mammoth.bcm.tmc.edu/EAp53), and a threshold of 75 was utilized to discriminate low-risk (<75) from high-risk (≥75) cases. Finally, we compared patients with or without del(17p).
Statistical analysis
Comparison of continuous variables utilized the unpaired two-sided student’s t-test. Categorical data were assessed by the χ2 test or Fisher’s exact test. Differences between ordinal variables were assessed by rank sum analysis. PFS and OS were assessed from the initial infusion to relapse and death, respectively. Duration of response (DOR) was estimated as the time from first response to first radiologically documented progressive disease or death. Follow-up was performed until patient death, loss to follow-up, or consent withdrawal. Objective response rates were presented with 95% confidence intervals (CIs) determined by the Clopper–Pearson method. Survival was assessed by generating Kaplan–Meier curves, and the log-rank test was utilized for comparisons. Univariable and multivariable analyses were carried out with the Cox regression proportional hazards model. Two-sided P < 0.05 was deemed statistically significant. SPSS 22.0 (SPSS, Chicago, IL, USA) was utilized for data analysis. The 95%CI of PFS was calculated with the survival (v3.2–11) package of R (v4.0.5; http://www.r-project.org). All data are available from the corresponding authors upon request.
Data availability
The additional data collected in this study are available from the corresponding authors on reasonable request.
References
Crump, M. et al. Outcomes in refractory diffuse large B-cell lymphoma: Results from the international SCHOLAR-1 study. Blood 130, 1800–1808 (2017).
Gisselbrecht, C. et al. Salvage regimens with autologous transplantation for relapsed large B-cell lymphoma in the rituximab era. J. Clin. Oncol. 28, 4184–4190 (2010).
Neelapu, S. S. et al. Axicabtagene ciloleucel CAR T-cell therapy in refractory large B-cell lymphoma. N. Engl. J. Med. 377, 2531–2544 (2017).
Locke, F. L. et al. Long-term safety and activity of axicabtagene ciloleucel in refractory large B-cell lymphoma (ZUMA-1): A single-arm, multicentre, phase 1–2 trial. Lancet Oncol. 20, 31–42 (2019).
Jacobson, C. et al. Long-term survival and gradual recovery of B cells in patients with refractory large B cell lymphoma treated with axicabtagene ciloleucel (Axi-Cel). Blood 136, 40–42 (2020).
Neelapu, S. S. et al. Interim analysis of ZUMA-12: A phase 2 study of axicabtagene ciloleucel (Axi-Cel) as first-line therapy in patients (Pts) with high-risk large B cell lymphoma (LBCL). Blood 136, 49–49 (2020).
Chen, L. et al. CAR T-cell therapy for a relapsed/refractory acute B-cell lymphoblastic lymphoma patient in the context of Li-Fraumeni syndrome. J. Immunother. Cancer 8, e000364 (2020).
Zhang, X. et al. Efficacy and safety of anti-CD19 CAR T-cell therapy in 110 patients with B-cell acute lymphoblastic leukemia with high-risk features. Blood Adv. 4, 2325–2338 (2020).
Pan, J. et al. Frequent occurrence of CD19-negative relapse after CD19 CAR T and consolidation therapy in 14 TP53-mutated r/r B-ALL children. Leukemia 34, 3382–3387 (2020).
Levine, A. J. p53: 800 million years of evolution and 40 years of discovery. Nat. Rev. Cancer 20, 471–480 (2020).
Levine, A. J. & Oren, M. The first 30 years of p53: Growing ever more complex. Nat. Rev. Cancer 9, 749–758 (2009).
Vousden, K. H. & Prives, C. Blinded by the light: The growing complexity of p53. Cell 137, 413–431 (2009).
Xu-Monette, Z. Y. et al. Mutational profile and prognostic significance of TP53 in diffuse large B-cell lymphoma patients treated with R-CHOP: Report from an International DLBCL Rituximab-CHOP Consortium Program Study. Blood 120, 3986–3996 (2012).
Zenz, T. et al. TP53 mutation and survival in aggressive B cell lymphoma. Int. J. Cancer 141, 1381–1388 (2017).
Pasqualucci, L. et al. Analysis of the coding genome of diffuse large B-cell lymphoma. Nat. Genet. 43, 830–837 (2011).
Morin, R. D. et al. Genetic landscapes of relapsed and refractory diffuse large B-cell lymphomas. Clin. Cancer Res. 22, 2290–2300 (2016).
Rushton, C. K. et al. Genetic and evolutionary patterns of treatment resistance in relapsed B-cell lymphoma. Blood Adv. 4, 2886–2898 (2020).
Qian, M. et al. TP53 germline variations influence the predisposition and prognosis of B-cell acute lymphoblastic leukemia in children. J. Clin. Oncol. 36, 591–599 (2018).
Wong, T. N. et al. Role of TP53 mutations in the origin and evolution of therapy-related acute myeloid leukaemia. Nature 518, 552–555 (2015).
Xu-Monette, Z. Y. et al. Dysfunction of the TP53 tumor suppressor gene in lymphoid malignancies. Blood 119, 3668–3683 (2012).
Miao, Y. et al. Genetic alterations and their clinical implications in DLBCL. Nat. Rev. Clin. Oncol. 16, 634–652 (2019).
Rosenthal, A. & Rimsza, L. Genomics of aggressive B-cell lymphoma. Hematol. Am. Soc. Hematol. Educ. Program 2018, 69–74 (2018).
Cao, Y. et al. Mutations or copy number losses of CD58 and TP53 genes in diffuse large B cell lymphoma are independent unfavorable prognostic factors. Oncotarget 7, 83294–83307 (2016).
Chiappella, A. et al. Rituximab-dose-dense chemotherapy with or without high-dose chemotherapy plus autologous stem-cell transplantation in high-risk diffuse large B-cell lymphoma (DLCL04): final results of a multicentre, open-label, randomised, controlled, phase 3 study. Lancet Oncol. 18, 1076–1088 (2017).
Chiappella, A. et al. Biodlcl04: The prognostic role of cell of origin profile, Myc, Bcl2, and Tp53 in untreated poor-risk diffuse large B-cell lymphoma. Hematol. Oncol. 35, 157–158 (2017).
Eskelund, C. W. et al. TP53 mutations identify younger mantle cell lymphoma patients who do not benefit from intensive chemoimmunotherapy. Blood 130, 1903–1910 (2017).
Ferrero, S. et al. KMT2D mutations and TP53 disruptions are poor prognostic biomarkers in mantle cell lymphoma receiving high-dose therapy: A FIL study. Haematologica 105, 1604–1612 (2020).
Delfau-Larue, M. H. et al. High-dose cytarabine does not overcome the adverse prognostic value of CDKN2A and TP53 deletions in mantle cell lymphoma. Blood 126, 604–611 (2015).
Eskelund, C. W. et al. Lenalidomide plus bendamustine-rituximab does not overcome the adverse impact of TP53 mutations in mantle cell lymphoma. Haematologica 103, e541–e543 (2018).
Chen, S. et al. Arsenic trioxide rescues structural p53 mutations through a cryptic allosteric site. Cancer Cell 39, 225–239 e228 (2021).
Wang, N. et al. Efficacy and safety of CAR19/22 T-cell cocktail therapy in patients with refractory/relapsed B-cell malignancies. Blood 135, 17–27 (2020).
Wei, J. et al. Long-term outcomes of relapsed/refractory double-hit lymphoma (r/r DHL) treated with CD19/22 CAR T-cell cocktail therapy. Clin. Transl. Med. 10, e176 (2020).
Kazantseva, M. et al. Tumor protein 53 mutations are enriched in diffuse large B-cell lymphoma with irregular CD19 marker expression. Sci. Rep. 7, 1566 (2017).
Evans, A. G. et al. Evolution to plasmablastic lymphoma evades CD19-directed chimeric antigen receptor T cells. Br. J. Haematol. 171, 205–209 (2015).
Fry, T. J. et al. CD22-targeted CAR T cells induce remission in B-ALL that is naive or resistant to CD19-targeted CAR immunotherapy. Nat. Med. 24, 20–28 (2018).
Cordoba, S. et al. CAR T cells with dual targeting of CD19 and CD22 in pediatric and young adult patients with relapsed or refractory B cell acute lymphoblastic leukemia: a phase 1 trial. Nat. Med. 27, 1797–1805 (2021).
Spiegel, J. Y. et al. CAR T cells with dual targeting of CD19 and CD22 in adult patients with recurrent or refractory B cell malignancies: a phase 1 trial. Nat. Med. 27, 1419–1431 (2021).
Dudley, M. E. et al. Adoptive cell therapy for patients with metastatic melanoma: Evaluation of intensive myeloablative chemoradiation preparative regimens. J. Clin. Oncol. 26, 5233–5239 (2008).
Sauter, C. S. et al. CD19 CAR T cells following autologous transplantation in poor-risk relapsed and refractory B-cell non-Hodgkin lymphoma. Blood 134, 626–635 (2019).
Bouchlaka, M. N., Redelman, D. & Murphy, W. J. Immunotherapy following hematopoietic stem cell transplantation: potential for synergistic effects. Immunotherapy 2, 399–418 (2010).
Wang, X. et al. Phase 1 studies of central memory-derived CD19 CAR T-cell therapy following autologous HSCT in patients with B-cell NHL. Blood 127, 2980–2990 (2016).
Gattinoni, L. et al. Removal of homeostatic cytokine sinks by lymphodepletion enhances the efficacy of adoptively transferred tumor-specific CD8+ T cells. J. Exp. Med. 202, 907–912 (2005).
Shimizu, J., Yamazaki, S. & Sakaguchi, S. Induction of tumor immunity by removing CD25+CD4+ T cells: A common basis between tumor immunity and autoimmunity. J. Immunol. 163, 5211–5218 (1999).
Turk, M. J. et al. Concomitant tumor immunity to a poorly immunogenic melanoma is prevented by regulatory T cells. J. Exp. Med. 200, 771–782 (2004).
Wrzesinski, C. & Restifo, N. P. Less is more: lymphodepletion followed by hematopoietic stem cell transplant augments adoptive T-cell-based anti-tumor immunotherapy. Curr. Opin. Immunol. 17, 195–201 (2005).
Giavridis, T. et al. CAR T cell-induced cytokine release syndrome is mediated by macrophages and abated by IL-1 blockade. Nat. Med. 24, 731–738 (2018).
Norelli, M. et al. Monocyte-derived IL-1 and IL-6 are differentially required for cytokine-release syndrome and neurotoxicity due to CAR T cells. Nat. Med. 24, 739–748 (2018).
Sesques, P. et al. Commercial anti-CD19 CAR T cell therapy for patients with relapsed/refractory aggressive B cell lymphoma in a European center. Am. J. Hematol. 95, 1324–1333 (2020).
Spiegel, J. Y. et al. Outcomes in large B-cell lymphoma progressing after axicabtagene ciloleucel (Axi-cel): Results from the U.S. Lymphoma CAR-T Consortium. J. Clin. Oncol. 37, 7517–7517 (2019).
Jacobson, C. et al. Long-term (≥4 year and ≥5 year) overall survival (OS) By 12- and 24-month event-free survival (EFS): An updated analysis of ZUMA-1, the pivotal study of axicabtagene ciloleucel (Axi-Cel) in patients (Pts) with refractory large B-cell lymphoma (LBCL). Blood 138, 1764–1764 (2021).
Vercellino, L. et al. Predictive factors of early progression after CAR T-cell therapy in relapsed/refractory diffuse large B-cell lymphoma. Blood Adv. 4, 5607–5615 (2020).
Nastoupil, L. J. et al. Standard-of-care axicabtagene ciloleucel for relapsed or refractory large B-cell lymphoma: Results from the US lymphoma CAR T consortium. J. Clin. Oncol. 38, 3119–3128 (2020).
Lou, Y. et al. Detection and quantification of chimeric antigen receptor transgene copy number by droplet digital PCR versus real-time PCR. J. Mol. Diagn. 22, 699–707 (2020).
Huang, L. et al. Integrated genomic analysis identifies deregulated JAK/STAT-MYC-biosynthesis axis in aggressive NK-cell leukemia. Cell Res. 28, 172–186 (2018).
Robles, A. I., Jen, J. & Harris, C. C. Clinical outcomes of TP53 mutations in cancers. Cold Spring Harb. Perspect. Med. 6, a026294 (2016).
Hainaut, P. & Pfeifer, G. P. Somatic TP53 mutations in the era of genome sequencing. Cold Spring Harb. Perspect. Med. 6, a026179 (2016).
Loizou, E. et al. A gain-of-function p53-mutant oncogene promotes cell fate plasticity and myeloid leukemia through the pluripotency factor FOXH1. Cancer Discov. 9, 962–979 (2019).
Oren, M. & Rotter, V. Mutant p53 gain-of-function in cancer. Cold Spring Harb. Perspect. Biol. 2, a001107 (2010).
Poeta, M. L. et al. TP53 mutations and survival in squamous-cell carcinoma of the head and neck. N. Engl. J. Med. 357, 2552–2561 (2007).
Dutta, S. et al. Functional classification of TP53 mutations in acute myeloid leukemia. Cancers 12, 637 (2020).
Neskey, D. M. et al. Evolutionary action score of TP53 identifies high-risk mutations associated with decreased survival and increased distant metastases in head and neck cancer. Cancer Res. 75, 1527–1536 (2015).
Acknowledgements
We are grateful to the faculty and staff of the Clinical and Laboratory Unit of the Department of Hematology, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, for clinical and technical support. Wuhan Bio-Raid Biotechnology CO., LTD. is acknowledged for cell manufacturing and quality-control. Dr. Pengcheng Wang of Hubei Clinical Research Center for Emergency and Resuscitation, Zhongnan Hospital of Wuhan University, is appreciated for kind assistance in statistical analysis. The current project was funded by the Key Program of the National Natural Science Foundation of China (81830008 and 81630006, to Dr. J.Z.), the National Natural Science Foundation of China (82070211 and 81670152, to Dr. L.H.; 82070217 and 81873427, to Dr. J.W.; 81770211 to Dr. M.X.), the Young Top-notch Talent Cultivation Program of Hubei Province (to Dr. L.H.) and CHEN XIAO-PING Foundation for the Development of Science and Technology of Hubei Province (CXPJJH12000009–113, to Dr. J.W.).
Author information
Authors and Affiliations
Contributions
All authors have read and approved the article. J.Z. and L.H. performed study design and supervision; T.Z., H.Z., and S.Z. supervised CAR T-cell production; N.W., H.Z., and S.Z. performed preclinical validation and quality control; L.H., Y.C., Y.X., F.M, J.W., Z.M., N.W, and Y.Z enrolled and treated the patients; J.W., Z.M., W.S., and X.Y. performed clinical data collection; J.W., M.X., and Z.M. analyzed data; J.W. and L.H. performed manuscript writing and revision; J.W. and Z.M. carried out data analysis; M.X., L.C., and Y.W. performed laboratory tests and patient response monitoring.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wei, J., Xiao, M., Mao, Z. et al. Outcome of aggressive B-cell lymphoma with TP53 alterations administered with CAR T-cell cocktail alone or in combination with ASCT. Sig Transduct Target Ther 7, 101 (2022). https://doi.org/10.1038/s41392-022-00924-0
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41392-022-00924-0
This article is cited by
-
Long-term follow-up demonstrates the curative potential of dual CD19/CD22 CAR-T-cell therapy alone or combined with autologous stem cell transplantation in TP53-altered relapsed/refractory B-cell non-Hodgkin lymphoma
Signal Transduction and Targeted Therapy (2026)
-
Prognostic impact of TP53 mutations in diffuse large B-cell lymphoma
Annals of Hematology (2026)
-
Sequential PD-1 inhibitors as consolidative therapy post-CD19 CART in relapsed/refractory NHL: a propensity score matching cohort study
Journal of Translational Medicine (2025)
-
Overcoming CAR-T bottlenecks in high-risk DLBCL: a molecular subtyping enhancement strategy
Cancer Cell International (2025)
-
Illuminating the impact of CD38-induced adenosine formation in B-cell lymphoma
Scientific Reports (2025)