Abstract
The metabolic pathway of sulfur-containing amino acids in organisms begins with methionine, which is metabolized to produce important sulfur-containing biomolecules such as adenosylmethionine, adenosylhomocysteine, homocysteine, cystine, and hydrogen sulfide (H2S). These sulfur-containing biomolecules play a wide range of physiological roles in the body, including anti-inflammation, antioxidant stress, DNA methylation, protein synthesis, etc., which are essential for maintaining cellular function and overall health. In contrast, dysregulation of the metabolic pathway of sulfur-containing amino acids leads to abnormal levels of sulfur-containing biomolecules, which produce a range of pathological consequences in multiple systems of the body, such as neurodegenerative diseases, cardiovascular diseases, and cancer. This review traces the milestones in the development of these sulfur-containing biomolecules from their initial discovery to their clinical applications and describes in detail the structure, physiochemical properties, metabolism, sulfide signaling pathway, physiopathological functions, and assays of sulfur-containing biomolecules. In addition, the paper also explores the regulatory role and mechanism of sulfur-containing biomolecules on cardiovascular diseases, liver diseases, neurological diseases, metabolic diseases and tumors. The focus is placed on donors of sulfur-containing biological macromolecule metabolites, small-molecule drug screening targeting H2S-producing enzymes, and the latest advancements in preclinical and clinical research related to hydrogen sulfide, including clinical trials and FDA-approved drugs. Additionally, an overview of future research directions in this field is provided. The aim is to enhance the understanding of the complex physiological and pathological roles of sulfur-containing biomolecules and to offer insights into developing effective therapeutic strategies for diseases associated with dysregulated sulfur-containing amino acid metabolism.
Similar content being viewed by others
Introduction
Sulfur is an essential element in biological systems and is vital to life. In healthy individuals, sulfur is absorbed in the digestive tract in the form of sulfur-containing amino acids, of which methionine is an essential amino acid. Endogenous sulfur-containing amino acid metabolism begins with the dietary intake of methionine, and through methionine cycle pathway, S-adenosylmethionine (SAM), S-adenosylhomocysteine (SAH), homocysteine (Hcy) and methionine are produced successively. Cystathionine and cysteine are produced from Hcy via the Hcy trans-mercapto pathway. Cysteine on the one hand produces taurine and sulfur dioxide through cysteine oxidative metabolism pathway, and on the other hand produces cystathionine, cystine, cysteine and hydrogen sulfide (H2S) through cysteine trans-mercapto pathway. H2S is eventually metabolized to sulfate or dimethyl sulfide and excreted from the body. Therefore, this metabolic pathway leads to the production of key intermediate metabolites such as SAM, SAH, Hcy, cystathionine, cysteine, and cystine, as well as terminal metabolites such as H2S, taurine, and sulfur dioxide.
A review of the research history reveals key milestones in the study of sulfur-containing amino acids and H2S (Fig. 1). In 1899-1900, Morner and Embden isolated cystine from scleroprotein, marking the identification of sulfur-containing amino acids. Later research demonstrated that cystine and cysteine are interconvertible through oxidation and reduction reactions.1,2,3 In the 1930s, methionine was recognized as an essential amino acid in protein synthesis.4,5 Hcy was identified in 1932 by Du Vigneaud and later recognized as an intermediate in the methionine metabolic pathway, forming cysteine through the transsulfuration pathway.6,7,8 In 1953, Giulio Cantoni described the formation and function of SAM, pivotal for methylation reactions.9 SAH, a product of SAM transmethylation, was synthesized by Baddiley and Jamieson in 1953.10 In the 1960s, scientists gradually elucidated the specific steps of methionine metabolism, revealing that methionine enters the methylation pathway via SAM, is then converted to Hcy through SAH, and subsequently re-enters the methionine cycle through remethylation reactions. H2S production in mammals was known biochemically by the early 1990s. Subsequent studies confirmed the presence of H2S-producing enzymes in the brain11 and blood vessels,12 gradually demonstrating that H2S plays important roles across various physiological systems. H2S is now recognized as the third gasotransmitter, following nitric oxide (NO) and carbon monoxide (CO).13,14
Timeline of major advancements in the study of sulfur-containing biomolecules produced by metabolism of sulfur-containing amino acids. In 1810, Wollaston identified cystine; in 1899-1900, Morner and Embden isolated cystine, showing cysteine’s interconvertibility; in 1922, Mueller isolated methionine; in the 1930s, methionine was recognized as essential for protein synthesis; in 1932, Du Vigneaud identified homocysteine; in 1953, Cantoni described SAM formation and Baddiley and Jamieson discovered SAH; and in the 1960s, methionine metabolism pathways were further elucidated. H2S, first observed by Ulysse Gayon in 1877 from bacteria in spoiled eggs, was linked to sulfur amino acid metabolism. In the 1930s and 1940s, Du Vigneaud discovered the transsulfuration pathway. By the 1960s and 1970s, enzymes like CBS, CSE, and 3-MST were identified. In the 1980s, sulfides were found in deep-sea vents. By the early 1990s, H2S production in mammals was known, with its biological effects explored later
In a healthy state, these sulfur-containing biomolecules participate in protein synthesis, as well as the synthesis and degradation of fatty acids, and are involved in key energy metabolism processes such as the citric acid cycle. They exert neurotransmitter, modulatory, and hormone-like biological effects, protect cells from environmental toxins and drug-induced damage, and play a critical role in the oxidant-antioxidant homeostasis.15,16,17,18,19,20 Through these diverse functions, sulfur-containing biomolecules play a crucial role in maintaining life activities, regulating physiological processes, protecting cells from damage, and are important substances in regulating homeostasis in the body. And disruption of sulfur-containing amino acid metabolic pathways is closely linked to the development of many diseases. It is well known that long-term induced hypermethioninemia leads to hyperhomocysteinemia, which affects methylation and metabolic processes. Clinical studies have confirmed that hyperhomocysteinemia is not only an independent risk factor for the development of cardiovascular and cerebrovascular diseases, such as atherosclerosis, acute myocardial infarction, stroke, coronary artery lesions, and peripheral vascular disease, but also increases the risk of neurodegenerative disorders and tumors, and impairs the efficacy of antifolate drugs.21 In contrast, H2S has a protective effect on the development of many diseases. It prevents cardiovascular diseases such as myocardial infarction, myocardial ischemia-reperfusion (IR) injury, cardiac hypertrophy, and atherosclerosis,22 reduces renal IR injury,23 attenuates non-alcoholic fatty liver disease (NAFLD) and hepatic fibrosis,24 reduces brain injury, promotes neurofunctional recovery, alleviates neurodegenerative diseases,25 promotes dendritic development of Purkinje cells and protects the cerebellum from oxidative stress damage. H2S presents a complex regulatory mechanism in tumors. In tumors such as breast,26 colorectal,27 and prostate cancers,28 H2S may promote tumor growth through pro-angiogenic and anti-apoptotic effects. Nevertheless, it has also been found that H2S may have anti-tumor properties by inducing apoptosis and inhibiting cell proliferation.29,30,31 The role of H2S in diseases may vary due to individual differences, disease types, and disease stages. Therefore, further research is still needed to better understand the effect of H2S in the occurrence and progression of specific diseases.
This paper summarizes the structure, physicochemical properties, metabolic processes, signaling pathways, physiological and pathophysiological functions of sulfur-containing biomolecules. Furthermore, novel mechanisms such as disulfide stress, disulfidptosis, and protein sulfhydration are discussed, highlighting their diverse roles in cellular regulation and disease progression. Moreover, the detection methods were also described, with an emphasis on innovative techniques such as fluorescence probes and mass spectrometry, which allow for highly sensitive and real-time monitoring of H₂S in biological systems. In addition, this paper summarizes the currently developed donors of sulfur-containing biomacromolecule metabolites and the screening of small molecule drugs targeting hydrogen sulfide-producing enzymes. These advances open new therapeutic avenues, particularly in modulating the sulfide metabolism to address diseases like cancer, neurodegenerative disorders, and metabolic diseases. We also focus on recent advances in preclinical and clinical studies of sulfur-containing biomacromolecule metabolites, noting the critical need to overcome existing research gaps. To this end, we propose strategies such as advancing clinical trials and further exploring large animal models, which will help bridge the gap between preclinical findings and human therapeutic applications. This holistic approach provides a new research orientation in the treatment of sulfur-containing biomacromolecule metabolism imbalance-related diseases.
Chemical biology of sulfides
Methionine
Amino acids are the fundamental elements of proteins and are involved in various critical biological processes in the body, such as metabolism,32,33,34 growth and development,35,36,37 and immune function.36,38,39,40 In prokaryotes, nearly all proteins are initiated with N-formylmethionine, whereas in eukaryotes, protein synthesis starts with methionine.41 For humans, methionine is the only sulfur-containing essential amino acid. Methionine exists in two isomeric forms, L-methionine and D-methionine, with the former being the predominant form found in nature.42 Methionine has a slightly distinctive odor and is unstable in strong acids, which can lead to demethylation. Additionally, it is soluble in water, dilute acids, and dilute bases, while being sparingly soluble in ethanol.42 The metabolism of methionine begins with its breakdown by methionine adenosyltransferase (MAT), producing the universal methyl donor SAM. SAM then donates its methyl group via the action of methyltransferase (MT), resulting in the formation of SAH. SAH is hydrolyzed by adenosylhomocysteinase (AHCY) into Hcy and adenosine. Hcy can either enter the transsulfuration pathway or be remethylated back to methionine via the methionine synthase (MS) pathway or the betaine-homocysteine S-methyltransferase (BHMT) pathway, thereby completing the methionine cycle41,43,44 (Fig. 2). In addition to serving as a precursor for protein synthesis, methionine’s broader physiological functions are primarily mediated through the intermediate products of the methionine cycle, such as the methylation processes dependent on its derivative SAM. Furthermore, elevated levels of Hcy, a byproduct of methionine metabolism, are associated with cardiovascular diseases and neurodegenerative disorders.45 Methionine can also be converted into cysteine, which is involved in the synthesis of glutathione. Glutathione is a critical intracellular antioxidant that scavenges free radicals and protects cells from oxidative stress-induced damage. Therefore, methionine plays a key role in maintaining cellular redox balance.16,46,47,48 The current limitations in methionine research primarily lie in the incomplete understanding of its complex role in various diseases. While methionine is associated with several metabolic disorders and cancers, the specific pathological effects of its excess or deficiency remain unclear. Existing therapeutic strategies mainly focus on regulating homocysteine levels, with limited effective interventions targeting methionine itself.
Generation and metabolism of sulfur-containing biomolecules. The metabolism of methionine begins with its breakdown by methionine adenosyltransferase (MAT), producing S-adenosylmethionine (SAM). Subsequently, SAM is converted to S-adenosylhomocysteine (SAH) through the action of methyltransferase (MT). SAH is then hydrolyzed by adenosylhomocysteinase (AHCY) to homocysteine (Hcy). Hcy can enter the transsulfuration pathway or be recycled back into methionine via the methionine synthase (MS) pathway or the betaine-homocysteine S-methyltransferase (BHMT), completing the methionine cycle. Within the MS pathway, Hcy also participates in the folate cycle. Additionally, SAM can contribute to methionine salvage pathways via MAT to replenish methionine levels. In the transsulfuration pathway, Hcy can be converted to cysteine (Cys) via cystathionine β-synthase (CBS) and cystathionine γ-lyase (CSE), leading to hydrogen sulfide (H2S) production. Hcy can also be directly converted to H2S by CSE. Furthermore, Cys and cystine can interchange with each other. D-amino acid oxidase (DAO), located in peroxisomes, can utilize D-cysteine (D-Cys) as a substrate to produce 3-mercaptopyruvate (3-MP), which can then be converted to H2S by 3-mercaptopyruvate sulfurtransferase (3-MST). The metabolism of H2S in the body can occur through simple gas exhalation, as well as via oxidation (which occurs in the mitochondria), methylation, and clearance by methemoglobin. Created with BioRender.com
S-adenosylmethionine
As early as 1951, Giulio Cantoni49 discovered SAM which is formed when methionine binds to the adenosyl group of ATP. SAM is a typical sulfonium compound, where the sulfur atom is covalently bonded to three substituents arranged in a trigonal pyramidal geometry, with a lone pair of electrons also associated with the sulfur atom.50 The high-energy sulfonium ion present in SAM enables it to transfer its methyl group to a variety of substrates via substitution reactions, including proteins, DNA, RNA, and metals.51 The most prominent metabolic function of SAM is its role as a methyl donor, with over 90% of the SAM produced being consumed in methylation reactions.52,53,54 DNA methyltransferases (DNMTs) transfer the methyl group from SAM to DNA, typically adding the methyl group to the 5th carbon of cytosine, forming 5-methylcytosine. This DNA methylation plays a crucial role in the regulation of gene expression and is often associated with gene silencing.55 SAM is also involved in RNA methylation modifications, such as N6-methyladenosine (m6A) modification in mRNA. This modification influences mRNA stability and translation efficiency, thereby regulating gene expression.56 SAM is also a critical methyl donor for histone methylation. Histone methylation is carried out by histone methyltransferases (HMTs) and typically occurs on lysine or arginine residues. This modification affects chromatin structure and regulates gene expression.57 SAM also participates in the synthesis of polyamines. In this pathway, SAM is decarboxylated by SAM decarboxylase, generating decarboxylated SAM (dcSAM). Subsequently, spermidine synthase catalyzes the addition of the first aminopropyl group from dcSAM to putrescine, forming spermidine (SPD). SPD is then converted into spermine (SPM) by spermine synthase through the addition of a second aminopropyl group. Both reactions generate 5′-methylthioadenosine as a byproduct.58,59,60 SPD and SPM are involved in various cellular processes, such as the regulation of autophagy pathways, mTOR signaling, and oxidative stress and antioxidant pathways.61,62,63 Methylthioadenosine (MTA) inhibits both spermidine synthase and spermine synthase. As a result, MTA can be recycled into methionine through the methionine salvage pathway.64 MTA is phosphorylated by MTA phosphorylase (MTAP), and subsequently converted into adenine and 5-methylthioribose-1-phosphate, the latter of which is further metabolized into methionine. In the absence of MTAP, endogenous MTA cannot be salvaged into methionine, leading to the accumulation of dcSAM and MTA, both of which inhibit methylation reactions.65,66,67 In addition, SAM mediates radical-based chemical reactions. Several SAM-dependent radical enzymes exist in the body, and the SAM radical enzyme family can form characteristic [4Fe-4S] clusters. These clusters provide the electrons necessary for the reductive cleavage of SAM, generating a 5’-deoxyadenosyl radical, which initiates radical mechanisms.68,69 Despite its critical involvement in methylation reactions, the precise mechanisms by which SAM dysregulation contributes to diseases such as cancer, neurodegenerative disorders, and liver diseases are still not fully elucidated. Moreover, while SAM supplementation has shown promise in some clinical settings, its therapeutic application is limited by the lack of standardized dosing and concerns over potential side effects.
S-adenosylhomocysteine
AHCY is the only enzyme that catalyzes the reversible hydrolysis of SAH into adenosine and homocysteine, thereby maintaining methylation homeostasis within the methionine cycle.70 Excessive accumulation of SAH within the cell can inhibit the activity of SAM-dependent methyltransferases.71 Therefore, the ratio of SAM/SAH is often used as an indicator of cellular methylation capacity, with a decrease in this ratio signaling a reduction in cellular methylation potential.72 Previous Study has shown that SAH can reduce the expression of DNA methyltransferase DNMT1 protein, lead to demethylation of the CpG islands in the NF-κB gene promoter region, and increase NF-κB expression, trigger the expression of pro-inflammatory senescence-associated secretory phenotype (SASP) factors, and thus induce cellular senescence in rat aortic smooth muscle cells.73 Additionally, inhibition of AHCY can induce endothelial cell senescence by downregulating hTERT expression, which is linked to reduced histone methylation in the hTERT promoter region.74 Notably, AHCY inhibition can also promote the development of atherosclerosis; it leads to downregulation of DNMT1 expression, which subsequently triggers the Drp1-mitochondrial reactive oxygen species (mtROS) pathway, ultimately resulting in atherosclerosis.75 Conversely, overexpression of AHCY can rescue cell function by activating the Nrf2-HO-1 signaling pathway. Transplantation of diabetic bone marrow mesenchymal stem cells with AHCY overexpression can enhance angiogenesis and mitigate adverse cardiac remodeling in rats.76
Homocysteine
Hcy is a sulfur-containing, non-proteinogenic amino acid derived from methionine and is a homolog of cysteine,77 with an additional methylene group (-CH2-) preceding the thiol group (-SH) on its side chain. Homocysteine is converted back to methionine via the MS pathway and the BHMT pathway, thus fulfilling a biological function of protecting methionine. In the MS pathway, 5,10-methylene tetrahydrofolate (5,10-MTHF) is converted into 5-methyl tetrahydrofolate (5-MTHF) by methylenetetrahydrofolate reductase (MTHFR). 5-MTHF then donates a methyl group to Hcy under the catalysis of MS, forming methionine. Subsequently, 5-MTHF is converted into tetrahydrofolate (THF). THF can be reconverted into 5,10-MTHF to complete the folate cycle, a process that requires normal levels of folate and vitamin B12.78,79 This also demonstrates the role of Hcy as an essential substrate in the folate cycle. In the BHMT pathway, Hcy uses betaine as a methyl donor, ultimately producing methionine and dimethylglycine (DMG).80 Betaine is a metabolite of choline, and the process is also a necessary step in the catabolism of choline.81 Another important physiological function of Hcy is its entry into the transsulfuration pathway. As early as the 1930s and 1940s, Du Vigneaud began studying the oxidation of sulfur-containing amino acids in tissues and whole animals, ultimately discovering the transsulfuration pathway.7,8 Through this pathway, Hcy can produce cysteine as well as the important gaseous signaling molecule H2S. Notably, SAM indirectly participates in the transsulfuration pathway by inhibiting MTHFR82 and activating CBS.83 When SAM is depleted, Hcy is remethylated back to methionine to regenerate SAM. Conversely, when SAM levels are high, Hcy is directed toward the transsulfuration pathway. Elevated levels of Hcy are considered an independent risk factor for the development of cardiovascular diseases. Hcy can induce endothelial dysfunction and is associated with atherosclerotic vascular diseases and ischemic heart attacks.84,85,86 Additionally, high Hcy levels are well-established risk factors for neurological disorders such as dementia and cognitive impairment.87,88,89 While elevated Hcy levels are associated with cardiovascular, neurodegenerative, and metabolic disorders, the direct causality between Hcy and these diseases remains unclear. Furthermore, therapeutic approaches targeting Hcy metabolism, such as supplementation with B vitamins, show inconsistent results, highlighting the need for more effective and standardized treatments.90,91
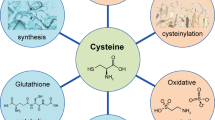
Cystine
Cystine is a dimer formed by the linkage of two cysteine molecules through a disulfide bond. Cystine has better solubility in acidic and alkaline solutions but is relatively unstable, easily reduced back to two cysteine molecules in a reductive environment. The primary physiological function of cystine is its reduction to cysteine, which then participates in the synthesis of glutathione. Under the catalysis of γ-glutamylcysteine synthetase (GCL) and in the presence of ATP, glutamate and cysteine form γ-glutamylcysteine. This step is the rate-limiting step in glutathione synthesis and serves as a key regulatory point in the process.92 Subsequently, γ-glutamylcysteine combines with glycine under the catalysis of glutathione synthetase, forming glutathione. This reaction also requires ATP for energy.93 The function of the cystine/glutamate antiporter (system x(c)(-)) is crucial for maintaining glutathione levels,94 and plays a significant role in ferroptosis.95,96,97
Hydrogen sulfide
H2S is a colorless, rotten egg flavor, soluble in water gas.98 H2S is a weak acid with an equilibrium state: in a 140 mM NaCl solution at pH 7.4, 14% of the free sulfide is H2S gas, 86% is HS,- and a trace amount of S.2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122 CBS and CSE mediate the transsulfuration pathway to produce H2S (Fig. 2). CBS first catalyzes the β-substitution reaction of L-homocysteine (L-Hcy) with L-serine to produce cystathionine, followed by α, γ-elimination reactions of CSE, which catalyzes the production of cystathiones to produce L-cysteine (L-Cys), α-ketobutyric acid, and NH3.123 L-Cys and water can further react to generate H2S. It should be noted that in this reaction, CBS generates H2S and serine through β-elimination reaction, while CSE generates H2S and pyruvate through α, β-elimination reaction.124 Additionally, both CBS and CSE can catalyze β-substitution reactions, resulting in the condensation of two L-Cys molecules to produce H2S and lanthionine, or the condensation of L-Hcy and L-Cys through β, γ-substitution reactions to produce H2S and cystathionine. Among them, CBS catalyzed the condensation of L-Hcy and L-Cys more predominantly, and L-Hcy and L-Cys were the most suitable substrates for the enzymatic reaction of CB.29 CSE can also catalyze the reaction of L-Hcy with water via α, γ-elimination reactions to produce homoserine, α-ketobutyrate, and NH3, or it can condense two molecules of L-Hcy through γ-substitution reaction to ultimately generate H2S.125 CBS is considered the main H2S synthesizing enzyme in the central nervous system, but it is also expressed in other organs such as the kidneys, liver, and lymphocyte.126 Compared to CBS, CSE has a wider distribution in mammalian tissues, mainly expressed in the periphery, responsible for H2S production in peripheral tissues,127 and is highly expressed in the cardiovascular and respiratory system.128 The third key enzyme for H2S generation is 3-MST, which catalyzes the synthesis of endogenous H2S using 3-mercaptopyruvate (3-MP) as a substrate129 (Fig. 2). 3-MP is produced from L-Cys by cysteine aminotransferase (CAT) with α-ketoglutarate as a coenzyme. 3-MST can remove sulfur from 3-MP, resulting in the creation of a persulfide on the enzyme (3-MST-ssh). H2S can be liberated from 3-MST-SSH through endogenous reducing agents like thioredoxin (Trx) or dihydrolipoic acid (DHLA).130,131 3-MST exhibits high activity in various tissues, such as kidney proximal renal tubular epithelial cells, cardiac cells and liver cells. Currently, 3-MST is believed to be the main enzyme in mitochondria that catalyzes H2S production.131,132
Studies129 have shown that D-amino acid oxidase (DAO) also contributes to endogenous H2S production (Fig. 2). DAO utilizes D-cysteine (D-Cys) as a substrate to produce 3-MP, which is then converted to H2S by the action of 3-MS.133 It is worth noting that, unlike the best H2S production under alkaline conditions using L-Cys as a substrate, D-Cys has the best H2S production under neutral conditions, specifically at pH 7.4. Furthermore, the endogenous H2S generation pathway using D-Cys as a substrate primarily functions in the cerebellum and kidneys, which are 7-and 80-fold higher than the source of L-Cys as a substrate generation pathway, respectively. Meanwhile, DAO is localized in peroxisomes, while 3-MST mainly exists in mitochondria. The two exchange various metabolites through specific forms of vesicular transport,134 that is, 3-MST and DAO produce H2S through organelle interactions.
Metabolism of H2S can occur through simple gaseous exhalation,135 or through oxidation, methylation, and scavenging by methemoglobin (Fig. 2). Research have shown that after intravenous injection of sodium sulfide in rats, a significant amount of exhaled H2S gas can be detected. This finding was subsequently confirmed in humans, where an increase in exhaled H2S gas was observed during intravenous injection of sodium sulfide.136,137 The final products of protein hydrolysis by oral microbial organisms often include H2S gas, which is also considered a potential underlying cause of halitosis.138 Increased levels of H2S in exhaled gas have also been observed in newborns and children with sepsis. Therefore, endogenous H2S can be eliminated in the form of gas. Considering that the production and metabolism of endogenous H2S can alter under various pathological and physiological conditions, it may be worth exploring exhaled H2S gas as one of the diagnostic indicators. However, it is important to note that exhaled H2S is a minor (<1%) route of elimination in the human bod,137 and attention should still be paid to other metabolic pathways.
The metabolism of H2S primarily occurs through mitochondrial oxidation. Sulfide:quinone oxidoreductase (SQR) is located in the inner membrane of the mitochondria and initiates the irreversible oxidation of H2S. Through the oxidation of H2S, SQR introduces electrons into the electron transport chain by transferring electrons from H2S to the oxidized form of coenzyme Q (CoQ), eventually resulting in ATP production.139 At the same time, H2S is oxidized to sulfur atoms and bound to the SQR to produce SQR persulfide (SQR-SSH). Subsequently, there are two pathways for further metabolism of SQR-SSH. The first pathway involves the transfer of sulfur atoms from SQR-SSH to sulfite (SO32-), forming thiosulfate (S2O32-), the sulfur atoms are transferred by thiosulfate sulfotransferase (TST) to reduced glutathione (GSH) to form Glutathione persulfide(GSSH) while regenerating SO3.2- In another pathway, sulfur atoms in SQR-SSH are transferred directly to GSH to form GSSH, which is then oxidized to SO32− by persulfide dioxygenase (ETHE1). SO32- can be further oxidized to sulfate (SO42-) by sulfite oxidase (SO) and excreted by the kidneys.140,141 Notably, rhodanese (Rhd) can transfer sulfur from GSSH to SO32-, which in turn generates S2O32-, most of which is further metabolized to sulfate by thiosulfate reductase (TR) and SO.142
Methylation is another pathway for the metabolism of H2S. Unlike oxidation, methylation of H2S occurs in the cytoplasm and is catalyzed by Thiol S-methyltransferase (TSMT).143 Methylation of H2S produces methanethiol (CH3SH), which can be further methylated to produce a relatively non-toxic compound, dimethyl sulfide (CH3SCH3). Both methylation products are sufficiently volatile to be excreted by respiration. On this basis, the conversion of CH3SH to CH3SCH3 is slower than the initial conversion of H2S to CH3SH, so the methylation of H2S is much slower than oxidation.143 TSMT is a widely distributed enzyme, with the highest activity in the mucosa of the colon and cecum. Additionally, it has also been reported to be active in the live144 and brain.145
H2S can also be eliminated by methemoglobin. H2S can rapidly bind to the Fe3+ in methemoglobin (MetHb), eventually producing heme-bound polysulfides and free thiosulfate, with Fe3+ reduced to Fe.2+ This process does not interfere with the function of hemoglobin as an oxygen carrier in the blood.146 Furthermore, based on the inherent binding characteristics of MetHb and H2S, Yuto Suzuki147 have designed and developed MetHb-albumin clusters as an antidote for H2S poisoning. Clusters of MetHb-albumin contain a ferric Hb core coated with three human serum albumins covalently. Rat cardiomyocytes (H9c2) death exposed to H2S can be inhibited by MetHb-albumin clusters while maintaining mitochondrial function. Additionally, they can restore cytochrome c oxidase activity in mice with lethal H2S toxicity.
SAM interacts with nucleic acids and plays a crucial role in cellular methylation processes. SAM serves as an essential methyl donor for DNMT, facilitating DNA methylation reactions.148 Additionally, SAM is involved in the methylation of RNA, particularly in RNA modifications, where it plays a critical role in regulating RNA stability, processing, and function.149 The thiol group (-SH) of cysteine can bind to metal ions such as copper, iron, and zinc, forming chelates that influence the biological functions of these metal ions. For example, cysteine’s interaction with copper ions can inhibit copper-induced oxidative reactions, thereby protecting cells from oxidative damage caused by metals.150,151 Chemical interaction of H2S with nitric oxide (NO) could generate several intermediates, including nitrosothiol, thionitrous acid, nitroxyl, nitrosopersulifide, polysulfides, SULFI/NO, etc.152 These intermediates play a number of biological roles. For example, nitroxyl and SULFI/NO exert positive inotropic effects. Nitroxyl reduces blood pressure in spontaneously hypertensive rats153 and attenuates myocardial ischemia-reperfusion injury.154 Polysulfides modulate the release of neurotransmitters.155 In addition, H2S may interact with other reactive species (e.g., oxygen, nitrogen, sulfur and selenium), leading to the formation of numerous products, contributing mostly to the redox biology of the cell. H₂S also interacts with proteins. For instance, H₂S can undergo sulfhydration reactions with cysteine residues within proteins, leading to the formation of sulfhydryl modifications.156 Moreover, H₂S may interact with the metal centers of target proteins,157 forming metal-sulfide complexes that regulate the activity of metal ions. This interaction is particularly significant in redox reactions. The interactions of sulfur-containing biomolecules with other biomolecules and the subsequent generation of intermediates and products which might be new signal molecules are becoming a new research field. More and more studies are conducted to clarify the exact production mechanisms and biological importance of these hybrid molecules.
Detection of sulfide metabolites
The methylene blue colorimetric method is the simplest technique for detecting sulfide metabolite H2S release. It has been applied in studies to measure H2S production in the human internal mammary artery158 and human uterine artery,159 as well as to assess H2S levels in the serum of children with Kawasaki disease.160 The principle of this method is based on the reaction of H2S with N,N-dimethyl-p-phenylenediamine solution, resulting in the formation of methylene blue. The methylene blue colorimetric assay is simple, uses relatively inexpensive reagents, has a short detection time, and is suitable for high-throughput screening. However, this method can only accurately detect H2S concentrations above 1 μM and is unable to measure H2S levels in the nmol/L range, with significant variability in the results.161 The sulfur-sensitive electrode method is characterized by a wide measurement range, as well as good stability and reproducibility.162,163 In recent years, it has been applied to measure H2S levels in various tissues, including the heart,164 brain,165 liver,166 and stomach167 of rats. However, during detection, Ag2S can form on the electrode surface, leading to decreased sensitivity and altered performance. In recent years, numerous sensitive, real-time monitorable, and structurally novel fluorescent probes for H2S detection have been reported, including probes selectively reduced by H2S,168,169,170 probes reacting with H2S via nucleophilic reactions,171,172,173,174,175 and probes using ligand metals to trap H2S.176,177 These fluorescent probes have great potential as tools for the detection of H2S in biological samples. Gas chromatography (GC) and high-performance liquid chromatography (HPLC) have been extensively reported for the determination of endogenous H2S. GC can be combined with chemiluminescence detection for the analysis of H2S levels in biological samples. And it can also be coupled with mass spectrometry (GC-MS) to detect sulfides and thiosulfates in sample.178,179 This method demonstrates high detection sensitivity; however, the derivatization process may influence the concentration of original sulfides in the samples. Additionally, the settings of the instrumental parameters can impact the results, necessitating a high level of proficiency from the operators. The basic operation of HPLC involves the rapid derivatization of sulfides in the sample with an excess of monobromobimane (MBB) under mild conditions, yielding sulfide-dibimane. Dibimane is a hydrophobic molecule, and sulfide-dibimane is more hydrophobic than most physiological thiols. Based on this property, sulfide-dibimane was separated by reverse phase-HPLC with gradient elution and analyzed by fluorescence detector.180 This method exhibits high sensitivity, low detection limits (0.02 pM), good selectivity, and the ability to rapidly capture active sulfides without releasing chemically bound sulfur that may be present in biological matrices. However, the method still has non-negligible drawbacks, such as expensive reagents, stringent reaction conditions, and long analysis times. Despite the various disadvantages of chromatography, this method is commonly employed in the detection of clinical plasma samples181,182 (Table 1).
Sulfide catabolism and diseases
Cardiovascular disease
The surviving heart after myocardial infarction (MI) undergoes continuous changes with myocardial fibrosis as the main pathological process.183,184,185 Early myocardial fibrosis can reduce expansion of the infarcted area and prevent ventricular rupture; however, prolonged fibrosis can lead to stiffening of the ventricular wall, progressive impairment of heart function, and eventually heart failure.186 Studies have shown that feeding mice a high L-methionine diet can induce hyperhomocysteinemia, increase MI risk, and promote myocardial fibrosis and cardiomyocyte apoptosis.187 The underlying mechanism involves the propensity of Hcy to undergo auto-oxidation, generating reactive oxygen species (ROS), which can reduce plasma membrane fluidity and compromise cellular integrity. This results in structural and functional damage to cells. The SAM/SAH ratio is critical for the regulation of methylation. In MI models, SAM concentration and the SAM/SAH ratio decrease progressively in a time-dependent manner, offering new insights into the potential pathophysiological mechanisms underlying myocardial infarction.188 However, the concentration changes of SAM and SAH are often measured at specific time points following myocardial infarction, which may overlook the impact of long-term and chronic changes on DNA methylation and myocardial repair processes. Moreover, it remains unclear whether alterations in the SAM/SAH ratio have a sustained effect on cardiac function and long-term prognosis. Notably, H2S can mitigate myocardial fibrosis following MI. In myocardial tissue from MI rat models, myocardial fibrosis develops, with reduced expression of CSE and downregulation of endogenous H2S levels. H2S intervention can inhibit excessive activation of the endoplasmic reticulum stress-autophagy axis, activate the PI3K/AKT pathway, reduce apoptosis, and thereby improve myocardial remodeling189 (Fig. 3). Overexpression of CSE can similarly inhibit endoplasmic reticulum stress and activate the PI3K/AKT signaling pathway.190 The mitochondria-targeted H2S donor AP39 can restore mitochondrial H2S homeostasis in MI rats, improve myocardial fibrosis and cardiac function, inhibit PINK1 expression and mitophagy, and reduce ROS production and iron accumulation, thereby counteracting ferroptosis in cardiomyocytes.191 GSH plays a crucial role in counteracting ROS production and ferroptosis. The key functional component of GSH is the thiol (-SH) group of cysteine, which allows GSH to be oxidized into glutathione disulfide (GSSG) to directly neutralize free radicals and peroxides that accumulate in cells during oxidative stress, thereby exerting a protective effect in MI192,193 (Fig. 4). It is important to note that although H2S may be involved in myocardial protection through pathways such as the PI3K/AKT signaling pathway, and mitochondrial autophagy, existing studies show inconsistent results and lack systematic validation. Additionally, many studies focus primarily on short-term effects, overlooking the long-term impact of H2S after myocardial infarction and its potential for clinical translation.
Sulfide signaling pathway. SAM and Hcy promote the activation of caspases, leading to apoptosis, while H2S exerts an inhibitory effect. In the ERK1/2 pathway, SAH, Hcy, and H2S demonstrate a promoting role. Both SAM and H2S activate the PI3K/Akt pathway. H2S inhibits RhoA, β-catenin, and TGF-β/Smad signaling, whereas Hcy promotes β-catenin nuclear translocation but downregulate its protein expression. Additionally, SAM and H2S can suppress the activity of the STAT pathway. SAH enhances NF-κB pathway, while H2S has the opposite effect. Furthermore, H2S promotes the activation of Nrf2. Created with BioRender.com
Role of sulfur-containing biomolecules in cardiovascular diseases, liver diseases, brain-related diseases, metabolic disease and tumors. In cardiovascular diseases, they are implicated in conditions such as myocardial infarction ischemia-reperfusion, atherosclerosis, and myocardial hypertrophy. In liver diseases, they are involved in the pathogenesis of non-alcoholic fatty liver disease, liver fibrosis, and hepatocellular carcinoma. Sulfur-containing molecules also contribute to brain-related diseases, including hypoxic-ischemic brain injury, neurodegenerative diseases like Alzheimer’s disease (AD), Parkinson’s disease (PD), Huntington’s disease (HD), and amyotrophic lateral sclerosis (ALS), as well as multiple sclerosis. In metabolic diseases, they are involved in obesity, diabetes, and diabetic nephropathy. Furthermore, sulfur-containing biomolecules have been linked to various cancers, including non-small cell lung cancer, breast cancer, colon cancer, ovarian cancer, and bladder cancer. Created with BioRender.com
Myocardial ischemia-reperfusion (I/R) is the restoration of coronary artery blood flow after a period of coronary artery occlusion.194 Reperfusion has the potential to save ischemic myocardium. However, the influx of oxygen during reperfusion prompts reactivation of the aerobic metabolic electron transport chain, disrupting the dynamic balance between endogenous pro-oxidant and antioxidant functions.195,196,197 This leads to a significant increase in oxidative stress in vivo, which induces a pro-inflammatory immune cascade response, ultimately resulting in myocardial cell damage and death.198,199,200 Recent studies have identified a specific type of oxidative stress termed disulfide stress, which arises from the abnormal accumulation of intracellular disulfides, such as cystine. SLC7A11 is a cystine/glutamate antiporter that transports extracellular cystine into cells, where it is reduced to cysteine through NADPH consumption. Cysteine serves as the rate-limiting precursor for GSH synthesis, and GSH is a critical intracellular antioxidant. In cancer cells overexpressing SLC7A11 under glucose-deprived (NADPH-reduced) conditions, abnormal accumulation of cystine or other disulfide molecules can occur, triggering disulfide stress and leading to cell death. This novel form of cell death is termed disulfidoptosis.201 I/R injury can enhance protein glutathionylation, thereby triggering intracellular disulfide stress.202 Glutathionylation is the formation of a disulfide bond between a protein and GSH, serving as a critical redox regulatory mechanism. Under normal physiological conditions, glutathionylation protects protein cysteine residues from hyperoxidation, thereby preserving their structural integrity and functional capacity. However, under pathological conditions, excessive glutathionylation can reduce the activity of antioxidant enzymes, weaken cellular antioxidant defenses, and promote intracellular disulfide stress.203 Following myocardial I/R injury, persistent glutathionylation triggers disulfide stress, exacerbating cardiomyocyte damage and ultimately leading to cell death. This novel form of cell death offers new therapeutic insights for treating I/R injury.
Additionally, sulfur-containing biomolecules are also involved in the regulation of I/R injury. Research204 has shown that Hcy can activate ERK1/2 pathway (Fig. 3) and oxidative stress in rats subjected to I/R injury, leading to mitochondrial dysfunction and subsequent cardiac dysfunction. Furthermore, a methionine-restricted diet can alleviate myocardial injury induced by I/R; this dietary intervention increases H2S concentrations in myocardial tissue and peripheral blood of I/R mice, thereby reducing cardiomyocyte apoptosis.205 GYY4137 is a H2S donor.206 Under physiological pH and temperature, GYY4137 has the ability to gradually release small amounts of H2S in water for an extended period, replicating the release pattern of H2S in the human body. GYY4137 can protect heart function and reduce the infarct area after myocardial I/R. GYY4137 can protect heart function and reduce the infarct area after myocardial I/R,207 while I/R rats with CSE knockout experience exacerbated oxidative stress damage.208 This suggests that exogenous H2S supplementation or promotion of endogenous H2S production can exert cardioprotective effects. Mechanistically, H2S supplementation reduces serum malondialdehyde and myeloperoxidase levels after I/R, diminishes superoxide anion levels, inhibits myocardial mitogen-activated protein kinases (MAPK) signaling pathways, and alleviates systemic oxidative stress. Moreover, it can lower Bax expression, caspase-3 activity, and apoptosis209 (Fig. 3). H2S reduced infarction after I/R by stimulating adenosine monophosphate (AMP)-activated protein kinase and restoring autophagic flux, which in turn providing protection against myocardial I/R injury210 (Fig. 4).
Atherosclerosis involves endothelial dysfunction and vascular inflammation, leading to lipid accumulation and plaque formation on arterial walls, ultimately causing rupture and thrombotic events.211,212,213 A methionine-deficient diet leads to hepatic lipid accumulation, a well-known risk factor for atherosclerosis.214 Decreased SAM levels or increased SAH levels can both promote the progression of atherosclerosis. SAM supplementation can inhibit the proliferation and migration of vascular smooth muscle cells (VSMCs) by reducing inflammatory processes and endoplasmic reticulum oxidative stress. It also reduces carotid intima thickness and prevents endothelial dysfunction by inducing heme oxygenase-1 expression. In contrast, elevated plasma SAH levels promote VSMC proliferation and migration via activation of the oxidative stress-mediated ERK signaling pathway and activate endothelial cell inflammation through the NF-κB signaling pathway.215 SAM/SAH regulate processes related to atherosclerosis through multiple signaling pathways; however, these pathways may involve complex cross-talk and feedback mechanisms. Current studies tend to focus on individual signaling pathways, often overlooking the interactive effects between these pathways. High concentrations of Hcy can exacerbate the onset and progression of atherosclerosis in patients with systemic lupus erythematosus.216 Supplementation of H2S has shown improvement in atherosclerosis, while inhibiting CSE activity or having CSE gene defects can lower endogenous H2S levels and accelerate the progression of atherosclerosis.217 Liu218 designed and synthesized H2S donors modified with either niacin or clofibrate. All three H2S donors reduced the expression of apoptosis-related proteins Bax and caspase-3, exhibited antioxidant effects (significantly decreased ROS and MDA levels, while increasing SOD expression), and inhibited inflammatory responses (suppressing foam cell inflammation, reducing pro-inflammatory cytokine TNF-α, and increasing anti-inflammatory cytokine IL-10). Further studies revealed that these H2S donors inhibit the PI3K/Akt/NF-κB signaling pathway, thereby improving vascular function and suppressing atherosclerosis (Fig. 3). Similarly, NaHS, as an H2S donor, can improve vascular dysfunction, reduce the area of aortic atherosclerotic lesions and inhibit their progression by inhibiting the production of vascular superoxide.219 During the development of atherosclerosis, not only do plaques change, but the media and external elastic lamina of arteries continuously expand or contract, leading to changes in vascular lumen and causing vascular remodeling. Endogenous H2S protects vascular remodeling by maintaining the peroxisome proliferator activated receptor delta/suppressor of cytokine signaling 3 (PPARδ/SOCS3) anti-inflammatory signaling pathway. The lack of endogenous H2S results in vascular remodeling, thickening of the aortic wall, collagen deposition, increased phosphorylation of signal transducer and activator of transcription 3 (STAT3), reduced generation of aortic PPARδ and SOCS3. Therefore, the lack of endogenous H2S may be a risk factor for atherosclerosis and vascular remodeling220 (Fig. 4). Most current studies focus on the short-term effects of H2S donors, without thoroughly exploring their long-term impact on atherosclerosis progression, vascular remodeling, and clinical outcomes. Long-term effects may involve complex adaptive changes that have not been fully addressed. Additionally, the influence of different doses and administration methods on H2S donor efficacy remains underexplored. Varying doses may elicit distinct biological effects, and either excessive or insufficient doses could alter therapeutic outcomes or cause side effects.
The initial hypertrophy of the heart is a compensatory response to a failing heart, increasing contractility and reducing ventricular wall pressure in response to hemodynamic overload, but sustained hypertrophy can lead to cardiac dilation, loss of contractile function, and decreased ejection fraction, ultimately leading to heart failure.221,222,223 Elevated levels of Hcy can promote cardiac hypertrophy in patients with hypertension, with the calcium/calmodulin-dependent protein kinase-NFAT signaling pathway potentially involved in Hcy-induced hypertrophy.224 H2S is a product generated from Hcy via the transsulfuration pathway, and its donors can mitigate Hcy-induced cardiomyocyte hypertrophy.225 The protective role of H2S in pathological myocardial hypertrophy is increasingly being confirmed. In a myocardial hypertrophy model established by isoproterenol (ISO) injection, H2S decreased the expression of cleaved caspase-3 and NADPH oxidase 4 (NOX4), inhibited cardiac cell apoptosis, and improved cardiac structure. Furthermore, H2S can maintain mitochondrial membrane potential, and decrease the production of ROS within the mitochondria.226 However, this model differs from human pathology, particularly in long-term pathological conditions or clinical contexts, where the translational relevance of animal models is limited. The hypertrophic signaling pathway activated by myocardial infarction is defective in CSE knockout mice. However, 2 h after the onset of myocardial infarction, the treatment of both CSE knockout mice and wild-type mice with the exogenous H2S donor GYY4137 reduce infarct size, myocardial hypertrophy, adverse remodeling, and preserve cardiac function.227 An age-dependent association between 3-MST and cardiac hypertrophy has been found in mice. Knockout of 3-MST has a cardiac protective effect in young adult animals (2–3 months old); however, in older mice (>18 months), 3-MST knockout leads to reduced antioxidant signaling and subsequent hypertension and cardiac hypertrophy.228 In addition, H2S can increase glucose uptake and the expression of the glucose transporter glucose transporters type 4 (GLUT4) in hypertrophic cardiomyocytes, while inhibition of GLUT4 in mice can worsen myocardial hypertrophy.229 Notably, the accumulation of SAH in the heart reflects the concentration of free cytosolic adenosine and serves as a sensitive indicator of localized myocardial ischemia.230 In adult mice, knockout of mitochondrial Rieske iron-sulfur protein (RISP) leads to an increase in SAM, which is necessary for methyltransferase activity, resulting in proliferative remodeling of the heart with a doubling of cardiomyocyte numbers, although cellular hypertrophy does not occur231 (Fig. 4).
Liver disease
NAFLD is widely assumed as the most common chronic liver disease, and the interaction between lipid metabolism disorders and the resulting inflammatory response can jointly promote the occurrence and development of NAFLD.232,233,234 It has been found that,235 in the livers of NAFLD patients, especially in fibrosis areas, the expression of CSE protein was significantly downregulated. The CSE/H2S pathway was also downregulated in high-fat diet (HFD)-induced NAFLD mice or oleic acid-induced liver cell models. Feeding CSE knockout mice with HFD increased liver lipid deposition, fatty acid de novo synthesis pathway activity, liver insulin resistance, and enhanced hepatic gluconeogenesis, while treatment with an H2S donor attenuated these phenotypes. The protective effect of H2S was blocked when farnesoid X receptor (FXR) was knocked down. Furthermore, CSE/H2S promoted the persulfidation of FXR at Cys138/141 locations, consequently boosting its effectiveness in regulating the expression of target genes associated with lipid-glucose metabolism, inflammation, and fibrosis, thus alleviating NAFLD. In an HFD-fed SD rat model, the H2S donor AP39 reduced weight gain, improved HFD-induced liver pathology, and reduced serum lipid accumulation. AP39 also exhibited antioxidant effects by reducing ROS and MDA levels, increasing GSH levels, and superoxide dismutase (SOD) activity. In addition, AP39 reduced both mRNA and protein levels of HIF-1α, decreased mitochondrial swelling, and restored changes in mitochondrial membrane potential.236 In addition to the commonly used HFD models, there are also animal models of methionine-choline deficient (MCD) diet.237,238,239 Methionine and choline play critical roles in hepatic lipid metabolism. When these nutrients are deficient, they can cause dysregulation of lipid metabolism, oxidative stress, and inflammatory responses, ultimately leading to hepatic fat accumulation and hepatocyte injury. Deficiencies in methionine and cystine can induce non-alcoholic steatohepatitis (NASH), which is characterized primarily by steatosis, oxidative injury, and inflammation.240 Prolonged deficiencies in methionine and cystine lead to reduced protein synthesis and increased oxidative stress. The heightened oxidative stress in the liver results in mitochondrial damage, which is considered a trigger for the pathogenesis of NASH. SAM is most abundant in the liver, and its biosynthesis requires methionine adenosyltransferase (MAT), with MAT1A expressed in normal mature liver and MAT2A expressed in extrahepatic tissues, induced during liver growth and dedifferentiation.241 In fatty liver disease, alterations in the methionine cycle leads to reduced expression of MAT1A and increased expression of MAT2A, resulting in decreased SAM levels and contributing to the development of NAFLD.242 Plasma methionine levels are significantly elevated in MAT1A knockout mice, while hepatic SAM and glutathione levels are notably decreased, with no change in SAH levels. These mice are more susceptible to liver damage and more vulnerable to fat accumulation induced by a choline-deficient diet243 (Fig. 4). Although the HFD and MCD models are widely used in NAFLD research, these animal models differ from the pathological processes observed in human NAFLD. For instance, the HFD model primarily induces fat accumulation and insulin resistance, while the MCD model results in more pronounced hepatic fibrosis. Therefore, these animal models may not fully recapitulate the complexity of human NAFLD, limiting the translational relevance of the findings.
Liver fibrosis is a wound healing response following liver damage (like NAFLD and hepatitis). Liver fibrosis is linked to oxidative stress, inflammation, and excessive deposition of extracellular matrix (ECM), and can eventually develop into cirrhosis.244,245,246 Serum Hcy levels are positively correlated with the progression of liver fibrosis, potentially exerting their effects through the homocysteinylation of the autophagosome/lysosome fusion protein Syntaxin 17 (Stx17).247 Folic acid can protect the liver from cholestasis and liver fibrosis by reducing serum Hcy levels and exerting its antioxidant properties.248 In patients with liver fibrosis, the expression and activity of H2S-generating enzymes and plasma H2S levels are significantly lower than in the healthy group.249 In a mouse model, H2S can improve liver damage, lower serum alanine transaminase (ALT) and aspartate transaminase (AST) levels, reduce lipid deposition, and decrease liver cell death. Moreover, H2S induces sulfhydrylation of Kelch-like ECH-associated protein 1 (Keap1) at Cys151, promotes its association with (NF-E2)-related factor 2 (Nrf2), and increases the expression of Nrf2-associated antioxidant genes in vivo and in vitro, thereby improving liver function and reducing liver fibrosis.250 S-allyl-cysteine (SAC) is an endogenous donor of H2S, which can alleviate carbon tetrachloride (CCL4)-induced liver fibrosis in rats, reduce the mRNA expression of inflammatory and fibrotic cytokines, and increase antioxidant enzyme activity. SAC lowered the phosphorylation levels of Smad family member 3 (Smad3) and STAT3, inhibited their binding ability to the transcription promoter, thereby restraining the transcription of fibrosis-related genes and causing the expression of antioxidant-related genes251 (Figs. 3, 4). The mechanisms of H2S in liver fibrosis remain incomplete. While it inhibits fibrosis by activating the Keap1-Nrf2 pathway and downregulating the phosphorylation of Smad3 and STAT3, the interactions among involved signaling pathways (such as PI3K/Akt, MAPK, TGF-β, Wnt/β-catenin) and their roles at different pathological stages have not been systematically studied. The complexity of these mechanisms limits the clinical application of H2S in liver fibrosis treatment and warrants further investigation.
Brain-related diseases
The pathophysiological process of hypoxic-ischemic (HI) brain injury involves multiple mechanisms, including synaptic injury,252 inflammation,253 and oxidative stress.254 SAM can exacerbate hypoxic-ischemic injury in cortical cells of rats.255 Hcy can increase damage in the hippocampus of ischemic-hypoxic models in rats, which is consistent with the heightened susceptibility of patients with hyperhomocysteinemia to ischemic events.256 Increased cystine uptake and elevated extracellular glutamate levels can enhance hypoxic neuronal injury in cortical cultures from mice.257 Latest studies have shown that the expression of CBS and H2S levels in samples from HI patients and animals were significantly decreased.258 L-Cys, through its ability to generate H2S, can reduce early brain injury in HI, improve behavioral deficits, and synaptic injury. Treatment with L-Cys reduced the accumulation of CD11b+/CD45high cells, the activation of microglia and astrocytes, and the increase in ROS and MDA within the injured cortex. It is hypothesized that H2S may be effective in attenuating HI injury by inhibiting reactive glial responses, synaptic modifications, and the triggering of autophagic fluxes259 (Fig. 4). Although L-Cys can inhibit the excessive activation of microglial cells and astrocytes, the effects of H2S on immune cell function are complex. Microglial cells not only play a role in inflammation but also contribute to neural repair and regeneration. In certain contexts, H2S may interfere with the normal functioning of microglial cells, potentially impairing their reparative functions.
As a result of cerebral ischemia, cerebral ischemia-reperfusion injury (CIRI) is a pathological condition characterized by an aggravation of damage once blood flow is restored. It plays an important part in the development and progression of ischemic brain diseases.260,261,262 The occurrence of CIRI is mainly related to neuroinflammation, oxygen free radical damage, autophagy, and calcium overload, ultimately leading to mitochondrial dysfunction, disruption of the blood-brain barrier (BBB), and neuronal death. SAM can inhibit blood-brain barrier disruption and promote neuronal survival following transient cerebral ischemia in gerbils.263 Elevated levels of Hcy are associated with neurotoxicity after CIRI. Hcy can enhance autophagy mediated by oxidative damage, thereby promoting cell death following cerebral ischemia.264,265 In contrast, SAM can reduce oxidative damage in rat models of cerebral ischemia-reperfusion.266 Notably, low concentrations of H2S can exert protective effects in the central nervous system through multiple mechanisms.25,267 Studies have reported that NaHS improves neurofunction in rats after transient middle cerebral artery occlusion (MCAO) and reperfusion, reduces the infarct area, and inhibits autophagy activity in the brains of MCAO rats, suggesting that H2S can alleviate CIRI in rats by suppressing excessive autophagy activation.268 In addition, H2S preconditioning prevents neurological dysfunction, inflammation, oxidative damage, and cognitive impairment in mice caused by CIRI, and its protective effect may be achieved through the induction of heat shock protein 70 (HSP70) expression via the PI3K/Akt/Nrf2 signaling pathway.269 It has been found that Ras Homolog Family Member A (RhoA) and Rho-associated coiled-coil-containing protein kinase 2 (ROCK2) expression is upregulated in the hippocampal tissue of CIRI mice. ROCK has a significant inhibitory effect on cell survival and axon growth, and the upregulation of ROCK2 is considered a marker of activation of the RhoA/ROCK pathway in the brain. This regulation can be blocked by treatment with the exogenous H2S donor NaHS. Subsequent studies confirmed that H2S derived from CSE can promote the recovery of neurological function in CIRI mice by inhibiting the RhoA/ROCK2 signaling pathway and suppressing reactive proliferation of astrocytes270 (Figs. 3, 4). Although H2S can alleviate CIRI by inhibiting excessive autophagy, autophagy plays a dual role within the cell. It is a protective mechanism that, under certain conditions, promotes cell survival by clearing damaged cellular components. However, excessive inhibition of autophagy may lead to the accumulation of cellular debris, which could be detrimental to neuroprotection. Therefore, the modulation of autophagy by H2S requires precise regulation in terms of cell type, injury severity, and dosage to avoid potential adverse effects.
H2S, as a neuromodulator, plays an important role in regulating neuron health and synaptic structure integrity.271 In the adult mouse brain, CBS is ubiquitously expressed, and inhibition or knockout of CBS affects the proliferation and differentiation of neural stem cells, which can be blocked by supplementation with H2S donor.272 Dysregulation of H2S levels is commonly observed in neurodegenerative diseases, indicating the potential therapeutic value of H2S in conditions, for instance, Alzheimer’s disease (AD), Parkinson’s disease (PD), Huntington’s Disease (HD) and amyotrophic lateral sclerosis (ALS) (Fig. 4).
AD is characterized by the aggregation of microtubule-associated protein Tau and Aβ peptide, forming neurofibrillary tangles and amyloid plaques, respectively.273,274,275 Hyperphosphorylation of Tau protein, a hallmark of AD, reduces its affinity for microtubules and causes it to aggregate.276,277 In AD mouse models, H2S donors can alleviate disease symptoms, improve spatial and cognitive deficits in mice. Furthermore, H2S prevents the pathological phosphorylation of Tau by inhibiting the catalytic activity of glycogen synthase kinase 3β (GSK3β), one of the main kinases responsible for Tau protein phosphorylation, ultimately exerting neuroprotective effects against AD.278 Notably, cerebrospinal fluid levels of SAM and the SAM/SAH ratio, as well as SAM levels in specific brain regions (cerebral cortical subdivisions, hippocampus, and putamen), are significantly decreased in patients with AD compared to controls, likely due to excessive utilization in polyamine biosynthesis.279 The reduction in SAM levels may impair metabolic processes and brain function in AD patients.280 A randomized controlled trial demonstrated that folic acid supplementation can increase plasma levels of SAM and the SAM/SAH ratio in patients with AD, reduce inflammation, and thereby alleviate AD symptoms.281 SAM and superoxide dismutase 1 (SOD1) can synergistically counteract the exacerbation of AD-like features caused by B-vitamin deficiency, suggesting that the combination of SAM and SOD1 may serve as a potential adjunctive therapy for AD. However, current studies may be limited by small sample sizes and insufficiently accurate dosage stratification. Further research is needed to explore and validate these findings in greater depth.
PD is caused by progressive degeneration of dopaminergic cells in the substantia nigra, which is the second most common neurodegenerative disease after AD.282,283,284 Abnormal protein handling, excitotoxicity, neuroinflammation, and apoptosis can all contribute to the development of PD. In a mouse model of PD caused by the neurotoxin 1-Methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP),285 inhalation of H2S can prevent MPTP-induced motor impairments and the degeneration and apoptosis of tyrosine hydroxylase (TH)-containing neurons. Additionally, H2S can increase the expression of detoxifying enzymes and antioxidant proteins in the brain’s substantia nigra, suggesting that H2S can mitigate PD pathology by upregulating antioxidant defense mechanisms and suppressing inflammation and cell apoptosis in the brain.286
HD is a progressive neurodegenerative disorder characterized by motor, cognitive, and psychiatric symptoms. The Huntingtin gene encodes a protein known as “huntingtin”, but this gene contains an expanded CAG repeat sequence, leading to the production of an abnormal protein.287 The aggregation of mutant huntingtin protein disrupts numerous cellular processes, including transcription and translation regulation,288,289 amino acid homeostasis,290 antioxidant and stress responses,291,292 DNA repair, and autophagy.293,294,295 Among these processes, oxidative stress plays a crucial role, with H2S exerting antioxidant effects in HD by activating antioxidant enzymes to limit free radical reactions.296 In HD tissues, there is a deficiency in CSE mRNA levels, and cysteine supplementation has been shown to alleviate abnormalities in HD mouse models, suggesting its therapeutic potential.297 Additionally, Hcy levels are significantly elevated in HD patients, indicating that Hcy may contribute to neurodegeneration in HD.298
Notably, Hcy levels are also elevated in ALS patients, suggesting that higher Hcy levels may be associated with the progression of ALS.299 ALS is caused by the degeneration of motor neurons, leading to muscle atrophy, paralysis, and ultimately death.300 Similar to HD, oxidative stress also plays a significant role in ALS. SOD1 is located in the mitochondrial outer membrane, intermembrane space, and inner membrane. Mutations in SOD1 are considered oxidative stress-inducing factors in ALS pathogenesis. H2S has shown therapeutic potential for ALS by inhibiting SOD1 aggregation and countering oxidative modifications.301 Dietary supplementation with SAM also impacts SOD1. SAM supplementation can delay ALS onset in mouse models by 2–3 weeks and mitigate neurodegenerative characteristics, including preventing motor neuron loss, reducing gliosis, and inhibiting SOD1 aggregation.302 SOD1 mutations are considered an oxidative stress-inducing factor in the pathogenesis of ALS. However, not all ALS patients harbor SOD1 mutations, and these mutations account for only a small fraction of ALS cases. Therefore, the findings from studies on SOD1 mutations may not be generalizable to all ALS patients.
Multiple sclerosis (MS) is an inflammatory disease of the central nervous system, affecting motor, sensory, visual, and autonomic systems.303,304,305 Studies have shown that methionine and glutathione levels are decreased in MS patients, both of which may serve as potential biomarkers for disease prognosis.306 However, Hcy is more commonly considered a potential indicator of MS progression.307,308 Those abovementioned findings suggest that sulfur-containing compounds are broadly involved in the pathogenesis of MS. NaHS, as an H2S donor, has shown potential therapeutic effects in the progression of MS. Studies indicate that309 NaHS reduces the expression of IRAK-1, NF-κB, and brain levels of IL-17 and IL-1β, thereby improving motor dysfunction in MS mice, reducing axonal demyelination, oxidative stress, and neuroinflammation. The role of H2S has also been validated in MS patients, as evidenced by the downregulation of 3-MST expression in peripheral blood mononuclear cells, with 3-MST expression inversely correlated with several pro-inflammatory cytokines.310 Additional evidence suggests that H2S can inhibit the production of inflammatory mediators by immune cells such as T cells and macrophages, highlighting its therapeutic potential in MS treatment311 (Figs. 3, 4).
Notably, in the cerebellum, the D-Cys pathway predominates and produces more H2S and protects cerebellar neurons from oxidative stress more effectively than the L-Cys pathway.129 It has been shown,312 that D-Cys promotes dendritic development in Purkinje cells. However, the promotion of D-Cys was inhibited by the administration of a DAO inhibitor, and its effects could be subsequently restored by treatment with donors of 3-MP and H2S. These results indicate that D-Cys promotes dendritic development of primary cultured Purkinje cells through the production of H2S, which also suggests that this pathway could be a novel therapeutic direction for cerebellar diseases.
Metabolic disease
H2S-generating enzymes are also present in endocrine glands and organs.313,314,315 Studies indicate that CBS mRNA and protein expression levels are highest in the pancreas, particularly within acinar cells.316 Similarly, 3-MST is highly expressed in tissues such as the thyroid, parathyroid, adrenal glands, and pancreas.317 Consequently, H2S plays a significant role in lowering blood glucose. Plasma H2S levels are notably decreased in patients with type 2 diabetes, paralleling poor glycemic control318 (Fig. 4). In diabetic rat models, fasting blood glucose levels are inversely correlated with plasma H2S levels and H2S synthesis activity. Additionally, both plasma H2S levels and H2S synthesis activity are significantly reduced in diabetic rats.319 Notably, H2S can also improve left ventricular function, preventing myocardial hypertrophy and fibrosis in diabetic rats. Its protective mechanism may involve the activation of the Nrf2/ARE and PI3K/Akt pathways, thereby reducing inflammation, oxidative stress, and apoptosis, which helps mitigate the progression of diabetic cardiomyopathy.320 Additionally, elevated levels of Hcy are considered a potent contributor to chronic complications in diabetes.321 Hyperhomocysteinemia is an independent risk factor for the development and progression of diabetic retinopathy, whereas Hcy levels below a specific serum threshold serve as a protective factor for diabetic retinopathy.322 However, it is worth noting that lower Hcy levels are not necessarily better, as excessively low Hcy can indicate deficiencies in other substances, such as vitamins. In the future, it is also essential to monitor changes in other biomarkers reflected behind low Hcy levels.323 The measurement of Hcy levels may be influenced by various factors, including renal function, medications, gender, and age. These factors can lead to fluctuations in Hcy levels, potentially affecting its accuracy as a predictive marker for diabetic complications.
Diabetic kidney disease (DKD) is a form of chronic kidney disease caused by diabetes mellitus and is one of the leading causes of end-stage renal disease.324,325,326 Studies indicate that, as the disease progresses, SAH levels in red blood cell increase, but SAM levels and SAM/SAH ratio decrease. SAM deficiency may lead to methyl deficiency, which is associated with the high incidence and mortality of DKD patients.327 Glycine N-methyltransferase (GNMT), a SAM-dependent enzyme, plays a critical role in methyl transfer reactions by regulating the cellular SAM/SAH ratio. Research shows that GNMT expression is significantly downregulated in the serum of patients with type 1 diabetes and in the kidney tissues of DKD mice. GNMT overexpression alleviates renal inflammation and fibrosis, presenting a new therapeutic target for DKD.328 Although GNMT is considered a novel therapeutic target for DKD, treatment strategies targeting GNMT may need to account for individual differences, such as genetic polymorphisms, disease stage, and comorbidities, all of which could influence treatment outcomes. Moreover, H2S plays a significant role in diabetic nephropathy. Increasing H2S levels has been shown to mitigate renal dysfunction and pathological changes in diabetic rats. The protective effect of H2S against diabetic nephropathy may be associated with a reduction in oxidative stress through enhanced antioxidant activity.329 SIRT1 is considered an anti-aging molecule that utilizes the coenzyme NAD+ to deacetylate target proteins, thereby exerting protective effects in the kidneys by inhibiting renal cell apoptosis,330 inflammation331 and fibrosis,332 ultimately slowing the progression of DKD. H2S can upregulate SIRT1 expression, reduce ROS, and inhibit apoptosis, thus protecting renal cells from further DKD-related damage.333 Moreover, H2S can lower blood pressure in spontaneously hypertensive diabetic rats, alleviate renal dysfunction, and inhibit the progression of early DKD.334 Thus, sulfides exhibit a mitigating effect on diabetes and its complications, offering new insights for the prevention and treatment of these conditions (Fig. 4).
Obesity is closely associated with type 2 diabetes, and both conditions represent major global health burdens. The prevalence of obesity has shown a sharp increase over the past few years.335,336,337 Research has shown that plasma total cysteine levels are positively correlated with obesity, particularly with adipose tissue mass.338 In several rodent models, increased dietary cysteine levels have been associated with increased obesity.339 However, there is also evidence suggesting that cysteine can reduce appetite in both humans and rodents,340 which contradicts its role in promoting adiposity. Therefore, a deeper understanding of the additional mechanisms by which cysteine influences metabolic control is warranted. In addition to focusing on cysteine itself, its metabolic product, H2S, is also critical in the context of obesity. H2S levels are lower in obese individuals. Plasma H2S shows a negative correlation with obesity, such as waist circumference and waist-to-hip ratio.341 However, it is important to note that H2S has a complex role in both lipogenesis and lipolysis. H2S promotes the differentiation of preadipocytes into adipocytes by activating a series of transcription factors, including peroxisome proliferator-activated receptor gamma (PPAR-γ), CCAAT/enhancer-binding protein alpha (C/EBPα), sterol regulatory element-binding protein 1 (SREBP1), and carbohydrate response element-binding protein (ChREBP), thereby increasing triglyceride accumulation..342 In comparison to wild-type mice, the knockout mice for CBS and CSE exhibit significantly reduced adipose tissue mass and decreased body weight.343,344 The role of H2S in regulating lipolysis in adipose tissue is contentious. The CSE/H2S pathway inhibits lipolysis via the protein kinase A-perilipin/hormone-sensitive lipase pathway while simultaneously reducing high-fat diet-induced insulin resistance.345 However, other studies indicate that H2S can stimulate lipolysis in adipose tissue in a cAMP-PKA-dependent manner. Upregulation of the CSE/H2S pathway in adipose tissue may facilitate lipolysis in animals fed high-fat diets.346 Therefore, the controversial role of H2S necessitates further exploration to provide stronger evidence for the perspective that H2S donors or enhancers of H2S signaling may improve adipose tissue dysfunction in common metabolic disorders (Fig. 4).
Tumor
Sulfur-containing biomolecules347 are involved in a variety of processes associated with tumor progression, including angiogenesis, tumor growth, cell migration, invasion and metastasis, epithelial-mesenchymal transition, energy metabolism in mitochondria, and chemoresistance.348,349,350,351 Sulfur-containing biomolecules have recently been well studied in the pathogenesis of hepatocellular carcinoma (HCC), breast cancer, colon cancer, lung cancer, pancreatic cancer, ovarian cancer and prostate cancer (Fig. 4).
HCC is the most common type of liver cancer and is associated with changes in cell proliferation, oxidative stress, and inflammatory responses.352,353,354 The effects of H2S on HCC are complex and can promote or inhibit the development of HCC by modulating different cell signaling pathways. It has been found that,355 low concentrations of H2S stimulate the growth of cancer cells. Treatment with low concentrations of NaHS (10-100 µM) increases the protein levels of phosphorylated-epidermal growth factor receptor (p-EGFR), phosphorylated-extracellular signal-regulated protein kinases (p-ERK), matrix metalloproteinase 2 (MMP-2), and p-Akt, which could activate the EGFR and its downstream signaling pathways to promote HCC proliferation and invasion (Fig. 3). On the other hand, high concentrations of H2S have anti-tumor effects on cancer cells. Treatment with high concentrations of NaHS (600-1,000 µM) inhibits the (phosphatase and tensin homolog) PTEN/Akt signaling pathway, thereby inhibiting angiogenesis and tumor growth without causing significant systemic toxicity. However, some studies have shown that356 extremely low concentrations of NaHS (1–10 µM) can also inhibit HCC cell migration, proliferation, and division. H2S can upregulate the expression of LC3-II and autophagy-related protein Atg5, two autophagy-related proteins, in HepG2 cells, while significantly inhibiting the expression of p-PI3K, p-Akt, and mammalian target of rapamycin (mTOR) proteins in liver cancer cells. This indicates that extremely low concentrations of H2S can inhibit HCC by promoting autophagy and suppressing apoptosis. High concentrations of H2S also exhibit dual effects.357 Treatment with 500 µM NaHS for 24 h enhances cell viability and migration ability, while reducing the number of apoptotic cells. The levels of p-STAT3 and STAT3 significantly increase, leading to overexpression of cyclooxygenase-2 (COX-2) and COX-2 mRNA, indicating that H2S can decrease cell apoptosis through the STAT3/COX-2 signaling pathway and promote the progression of HCC. These findings demonstrate the complexity and environment-dependent role of the H2S signaling pathway in the occurrence and development of HCC, and further studies are needed to fully understand the molecular mechanisms underlying the dual effects of H2S and develop targeted and efficient anti-cancer therapies. Moreover, studies have shown that SAM is significantly reduced in HCC, consequently impacting critical metabolic pathways, including transmethylation reactions, the methionine cycle, and trans-sulfuration pathways.358 The gluconeogenic enzyme phosphoenolpyruvate carboxykinase 1 (PCK1) can promote SAM production. PCK1 deficiency exacerbates HCC, potentially exerting its tumor-promoting effects by upregulating the PI3K/AKT signaling pathway. Furthermore, both in vivo and in vitro supplementation of SAM has been shown to inhibit the progression of HCC caused by PCK1 deficiency. This suggests that SAM may act as a bridge linking PCK1 and PI3K, playing a beneficial role in the progression of HCC.359 Importantly, disulfidptosis, as a novel form of cell death, has significant implications for clinical prognosis in HCC. Researchers have analyzed patient samples to develop a disulfidptosis risk score, with higher scores correlating with increased mortality risk. This finding suggests that novel biomarkers associated with disulfidptosis could serve as valuable tools in the clinical diagnosis, prognostic prediction, and therapeutic targeting of HCC.360 The development of a disulfidptosis risk score, while promising, may oversimplify the complex, multifactorial nature of HCC. Tumor progression and patient prognosis depend on various genetic, epigenetic, and microenvironmental factors, many of which may not be fully captured by a single risk score based solely on disulfidptosis. Therefore, relying too heavily on this score could lead to an incomplete understanding of a patient’s prognosis, potentially overlooking other important factors.
SAM has also demonstrated similar effects in breast cancer. A preclinical study indicated that the combination of SAM and decitabine shows significant potential in the anticancer treatment of breast cancer.361 SAM enhances the levels of autophagy markers beclin-1 and LC3B-II in MCF-7 breast cancer cells and significantly increases the Bax/Bcl-2 ratio, indicating that SAM can inhibit breast cancer by inducing autophagy and apoptosis in MCF-7 cells.362 In contrast to SAM, elevated levels of Hcy are considered a risk factor for cancer and a potential novel tumor marker.363 Women with high levels of Hcy and cysteine who also have low folate levels are at an increased risk of developing breast cancer.364 However, factors such as gender, ethnicity, and individual genetic background may influence the expression and function of these biomarkers. For example, folate absorption and metabolism can vary across different populations, which suggests that relying solely on these biomarkers to assess breast cancer risk may have limitations and may not be universally applicable to all populations. H2S plays a dual role in breast cancer. Wu365 found that inhibiting endogenous H2S can reduce the vitality, proliferation, migration, and invasion rate of human breast cancer cells, induce apoptosis in human breast cancer cells, and decrease the phosphorylation levels of PI3K, Akt, and mTOR. In an animal model of human breast cancer xenografts, it was found that inhibiting H2S can reduce the generation and growth of tumor blood vessels. This indicates that H2S acts on the PI3K/Akt/mTOR pathway in human breast cancer cells, and inhibiting the production of endogenous H2S can reduce cell proliferation and tumor growth through this signaling pathway. Triple-negative breast cancer (TNBC) is the most aggressive subtype of breast cancer, currently lacking targeted therapy.366,367,368 Chemotherapy is the only systemic treatment strategy available for TNBC patients and has a poor prognosis. TNBC cells are also inhibited from growing, proliferating, migrating, and invading when treated with H2S inhibitors. Moreover, it also reduces the protein levels of PI3K, Akt, mTOR, and Ras, Raf, and p-ERK, indicating that H2S may regulate human TNBC cells through dual targeting of the PI3K/Akt/mTOR and Ras/Raf/ERK signaling pathways369 (Fig. 3). Nevertheless, some studies have also shown that H2S donor can inhibit tumor invasion and metastasis. During the metastatic process, matrix metalloproteinases (MMP-2 and MMP-9) play a crucial role by degrading type IV collagen. Lu370 investigated the effects of H2S donor on MMPs and found that H2S donor can inhibit the viability of TNBC cells, increase apoptosis, and significantly suppress the mRNA levels, protein expression, and enzymatic activity of MMP-2/9 during invasion, tumorigenesis, and metastasis by blocking the NF-κB and ERK/MAPK signaling pathways. Additionally, other studies have shown that H₂S donors and their derivatives can exert strong antitumor effects by inhibiting the aberrant activation of the β-catenin pathway, thereby reducing the expression of MMP-9371 (Fig. 3). The contradictory roles of H₂S suggest that further in-depth research is needed to explore the potential mechanisms and specific contexts in which H₂S exerts its effects, thereby providing new therapeutic targets for the treatment of breast cancer patients.
In patients with colon cancer, Hcy levels are similarly elevated, and Hcy levels correlate with the patients’ IL-6, TNF-α, and folate levels. This suggests that Hcy may be associated with inflammation related to colon cancer, potentially involving TNF-α-mediated pathways.372 5-MTHF is a key metabolic product in the folate and homocysteine metabolism pathways. In colon cancer cells treated with Hcy, both folate and 5-MTHF can reverse the growth enhancement induced by Hcy and inhibit the excessive proliferation of colon cancer cells, thus providing a protective effect.373 Epithelial-mesenchymal transition (EMT) is a major pathological change in colon cancer, representing the process of transition from a normal (epithelial) state to a transformed (mesenchymal) state.374,375,376 EMT represents a series of complex cellular events, typically controlled by the Wnt/β-catenin signaling pathway.377 Epithelial cells thus lose their intercellular adhesion capacity and acquire mesenchymal properties. This process can also occur in the opposite direction, known as mesenchymal-epithelial transition (MET).378,379 Research has found that,380 H2S promoted EMT in human colon cancer HCT116 cells, and inhibiting H2S could significantly downregulate Wnt3 mRNA levels and β-catenin protein expression, as well as reduce ATP-citrate lyase (ACLY) mRNA and protein levels. Reports indicate that ACLY is associated with the Wnt signaling pathway and is involved in EMT in colon cancer cell lines.381 The ACLY promoter is regulated by Sp1 and Sp3. It has been found that under the action of H2S inhibitors, the mRNA levels of Sp1 and Sp3 both decrease, with the effect on Sp3 being more pronounced. This suggests that the mechanism by which H2S maintains EMT is related to the regulation of the Sp3-ACLY-Wnt-β-catenin pathway. Comparing the gene expression levels between normal and tumor tissues in colon cancer patients revealed an upregulation of the TRIP6 gene associated with disulfide death. The TTPAL gene can prevent TRIP6 from being degraded by the proteasome and enhance its interaction with β-catenin. This suggests that the TTPAL-TRIP6-β-catenin axis present in disulfidptosis can activate the Wnt/β-catenin pathway, thereby promoting the progression of colon cancer.382 One study reported that,383 treating HCT116 cells with a low concentration (0.3 mM) of GYY4137 (a slow-release H2S donor) increased the proliferation rate of HCT116 cells, while enhancing mitochondrial function and glycolysis, thereby promoting tumor growth. It is worth noting that overexpression of CBS and supplementation of exogenous H2S can inhibit the proliferation, colony formation, migration, and hepatic metastasis of colon cancer cells. CD44 and SP-1 may be involved in the inhibitory effect of the CBS/H2S on colon cancer cells.384 The above findings indicate that the role of H2S is biphasic, concentration- and time-dependent. Szabo385 evaluated the impact of different concentrations of H2S donors on HCT116 proliferation and found that moderate H2S stimulation can enhance the proliferation of colon cancer cells, while high concentrations of sustained H2S treatment can reduce the proliferation activity of tumor cells. Different H2S donors vary in their rates of H2S release, stability, and metabolism, which can influence their biological effects in vivo. Additionally, the selectivity of H2S donors, individual differences among patients, interactions with other therapeutic modalities, and potential side effects need to be further investigated in future research. Studies on the clinical application of H2S should focus more on finding appropriate treatment doses and safe, effective, and specific small molecule agonists and inhibitors.
Non-small cell lung cancer (NSCLC) accounts for 85% to 90% of all lung cancers,386 and is a common type of lung cancer, with lung adenocarcinoma being the most prevalent subtype within NSCLC.387,388 Studies have shown that disulfide death is closely related to the occurrence and progression of lung adenocarcinoma. Researchers constructed a prognostic risk score based on disulfidptosis-related genes in lung adenocarcinoma. The high-risk score group exhibited a higher mortality rate, poorer survival outcomes, and a less favorable immune microenvironment compared to the low-risk score group. This suggests that the genetic features associated with disulfidptosis have various impacts on the occurrence, proliferation, and metastasis of lung cancer, and may provide insights for identifying patient prognosis.389 Furthermore, the levels of SAM are elevated in patients with NSCLC, suggesting its potential as a biomarker for early-stage NSCLC.390 Moreover, compared to normal pulmonary epithelial cells, NSCLC cells express higher levels of CBS, CSE and 3-MST, leading to increased production of H2S. H2S can induce migration and invasion of NSCLC cells, as well as the EMT process. Additionally, H2S plays a significant role in the growth and angiogenesis of NSCLC by activating HIF-1α, which may provide new avenues for targeting H2S in therapeutic strategies.391 An important aspect to consider is that H2S may exert its effects through multiple signaling pathways, which could differ depending on the tumor type or cellular context. The interactions between H2S and other factors, such as ROS and NF-κB, and their collective impact on the tumor microenvironment, as well as on tumor cell proliferation, migration, and invasion, still require further in-depth exploration.
Pancreatic cancer encompasses various types, with pancreatic adenocarcinoma being the most common, typically associated with a poor prognosis and a five-year survival rate of only 5%.392,393,394 Recent findings suggest that H2S donor hold potential in the treatment of pancreatic cancer. Erucin (ERU) can penetrate the cell membrane of pancreatic adenocarcinoma cells and release H2S intracellularly. High concentrations of ERU (30-100 μmol/L) induce apoptosis by reducing the levels of phosphorylated ERK1/2 and upregulating the expression of caspase-3 and caspase-7, thereby inhibiting cancer cell proliferation. This mechanism may be related to the hyperactivation of the oncogene KRAS, leading to the excessive phosphorylation of the downstream kinase ERK1/2.395 Sulforaphane (SFN) also gradually releases H2S in the biological environment. SFN induces the production of excessive ROS, which activates the AMPK signaling pathway, promoting the translocation of Nrf2 and resulting in the inhibition of pancreatic cancer cell viability. This suggests that H2S plays a crucial role in suppressing the growth of pancreatic cancer cells, promoting apoptosis, and modulating the migration and invasion of pancreatic cancer cells.396 Moreover, demethylation treatment can disrupt protein methylation, leading to the accumulation of SAH while depleting cellular SAM, resulting in the inhibition of autophagy and apoptosis induced by endoplasmic reticulum stress in pancreatic cancer cells. Additionally, demethylation may cause an imbalance in KRAS signaling, resulting in partial inactivation of ERK and excessive activation of the PI3K/AKT-mTORC1 pathway397 (Fig. 3). This demethylation treatment offers a novel therapeutic strategy for patients with pancreatic adenocarcinoma. It is important to highlight that MAT, a key enzyme in the generation of SAM, also plays a significant role in pancreatic cancer. Altered expression of MAT in pancreatic cancer makes it a potential biomarker for early diagnosis and prognostic prediction. Dysregulation of MAT is associated with pathways involved in carcinogenesis, chemotherapy resistance, and the activation of tumor-associated macrophages. This suggests that direct and indirect targeting of MAT may represent a promising therapeutic strategy.398 Although demethylation and MAT-targeted strategies offer new perspectives for the treatment of pancreatic cancer, their clinical translation faces numerous challenges. Demethylation therapy may lead to cytotoxicity and various side effects, while optimizing the dosage and treatment duration for MAT-targeted therapy, improving drug delivery methods, and addressing potential drug resistance issues require further investigation. Currently, there is a substantial amount of preclinical research on demethylation and MAT-targeted therapies, but translating these findings into effective clinical treatment protocols requires additional clinical validation.
Ovarian cancer (OC) is a common tumor in women, often associated with poor prognosis.399,400,401 Comparative analyses between OC tissues and normal tissues led to the identification of 14 differentially expressed genes related to disulfidptosis, which were used to create a risk signature. Patients in the high-risk group exhibited lower overall survival rates. The risk assessment tool established in this study can effectively stratify risk in OC patients, facilitating personalized treatment and follow-up management for individuals affected by this disease.402 Sulfides play an important role in OC.403 CBS is a sulfur-containing amino acid metabolic enzyme highly expressed in various OC cell lines and plays a significant role in the occurrence and development of OC. Studies have shown that silencing CBS notably inhibits OC cell proliferation and metastasis, and increases sensitivity to cisplatin. Mechanistically, silencing CBS impairs H2S production, significantly reduces cellular GSH levels, increases ROS production, activates the tumor suppressor p53 and inhibits NF-κB activation. This indicates that downregulation of CBS can alter antioxidant levels, trigger apoptotic cascades, and enhance drug sensitivity. In cancer cells, CBS colocalizes with mitochondrial markers. And silencing CBS was found to reduce mitochondrial respiration and inhibit ATP synthesis. OC growth and drug resistance phenotype can be maintained by CBS by controlling the cellular redox response and mitochondrial bioenergetics.404 Furthermore, CBS drives lipid metabolism dysregulation in OC.405 Cells were transiently transfected with CBS siRNA to probe the transcriptional regulation of sterol regulatory element binding protein (SREBP) (lipid transcription factor). It was found that all cells showed downregulation of gene expression of SREBP1a, SREBP1c, and SREBP2, as well as their target genes such as ACC1 and FASN, which are key enzymes in lipid synthesis. Further research revealed that silencing CBS hinders Sp1 nuclear translocation, thereby affecting Sp1 binding to the SREBP-1a promoter site. The stability of the Sp1 protein is maintained through the peroxidation function in the presence of CBS. Therefore, selectively targeting CBS and modulating abnormal lipid metabolism could offer new thoughts for the therapy of ovarian cancer. However, the potential impact of CBS-targeted therapy on normal cells remains unclear. CBS is involved not only in cancer cells but also in crucial physiological processes such as sulfur metabolism and antioxidant responses. Targeting CBS may interfere with these normal functions, potentially leading to unforeseen side effects. The long-term safety, dose optimization, and management of side effects associated with CBS inhibition still require further investigation.
Prostate cancer (PC) is one of the most common cancers in men and is especially prevalent in older men.406,407,408 It was shown that CSE was upregulated in bone metastatic PC cells and in patients with advanced PC, and the high expression of CSE in patients was associated with poor survival. Further investigation revealed that CSE could promote PC cell migration and invasion, and knockdown of CSE could inhibit cell invasion by suppressing IL-1β/NF-κB-mediated signaling.409 SAM exhibits antitumor effects in PC cells by inducing cell cycle arrest in the S phase and inhibiting cell proliferation. Additionally, SAM increases the ratio of pro-apoptotic factor Bax to anti-apoptotic factor Bcl-2, as well as the activity of caspase-3, thereby promoting apoptosis in PC cells. The therapeutic effects of SAM are associated with the downregulation of the ERK1/2 and STAT3 signaling pathways, both of which are involved in the survival, proliferation, migration, and invasion of cancer cells.410 EZH2, as an oncogene, is overexpressed in PC and is associated with poor clinical outcomes in PC patients.411,412 Treatment of PC cells with an AHCY inhibitor leads to the accumulation of SAH and a reduction in levels of Hcy and histone H3K27 methylation, subsequently decreasing PC cell proliferation. To some extent, miR-26a induced by AHCY inhibitors can regulate the expression of EZH2,413 which may represent a significant mechanism of action for AHCY inhibitor therapy in prostate cancer. Although AHCY inhibitors show potential in the treatment of prostate cancer, the safety and side effects of their long-term use remain unclear. Inhibition of AHCY may interfere with normal sulfur metabolism, leading to systemic metabolic disturbances or adverse effects on other physiological processes. Furthermore, whether AHCY inhibitors could induce resistance or alter tumor cell responses to other therapies requires further investigation.
Sulfide-based therapeutics
H2S donor
The importance of maintaining endogenous H₂S homeostasis in various diseases has sparked interest in exploring pharmacological approaches to either increase or decrease its levels. Direct inhalation of H₂S gas could offer targeted therapy for pulmonary diseases; however, this approach carries risks of toxicity and flammability.414 Intraperitoneal or intravenous administration of inorganic H₂S donors, such as sodium sulfide and sodium hydrosulfide,415,416,417 allows for site-specific delivery. However, these compounds have a short half-life, undergo rapid oxidation, and their H₂S release is uncontrolled. Lawesson’s reagent, widely used as a sulfurizing agent in organic synthesis, can also function as an H₂S donor.418,419,420 Upon spontaneous hydrolysis in aqueous solution, it releases H₂S. However, similar to other donors, it presents the challenge of uncontrolled H₂S release.421 The rapid and excessive release of H₂S may exert toxic effects on the body. Therefore, the development of compounds capable of stable and controlled H₂S release has become a key focus of research.
GYY4137 is an organic H2S donor, chemically referred to as N-(4-hydroxyphenyl)thiourea dioxide.182 It is a relatively stable compound capable of releasing H2S in a slow and sustained manner. Compared to traditional H2S salts, GYY4137 has a longer half-life, allowing for a more controlled release of H2S over time.422 A ADT-OH (5-(4-hydroxyphenyl)-3H-1,2-dithiocyclopentene-3-thione) is also capable of stabilizing H2S levels through slow release.423 Studies have demonstrated that ADT-OH, as a hydrogen sulfide donor, exerts therapeutic effects in malignant melanoma424 and breast cancer.425 Phenol thiosemicarbazone (AP39) is a mitochondria-targeted H2S donor. AP39 maintains intracellular H2S homeostasis while enhancing mitochondrial antioxidant capacity, reducing inflammatory responses, and protecting cells from apoptosis.191 Similar to AP39, hydroxythiobenzamide (AP123) slowly releases H2S within the mitochondrial region of cells, thereby reducing mitochondrial oxidative stress and improving the function of the mitochondrial electron transport chain.426,427 ATB-346 is a compound formed by conjugating an H2S donor group with the non-steroidal anti-inflammatory drug (NSAID) naproxen. Unlike previous H2S donors, ATB-346 can only release H2S through metabolic processes within the body, and it is incapable of releasing H2S in non-biological environments. ATB-346 retains the anti-inflammatory and analgesic properties of naproxen by inhibiting cyclooxygenase (COX) enzyme activity, thereby reducing prostaglandin production and exerting its anti-inflammatory and analgesic effect.428 Additionally, the release of H2S contributes to the protection of the gastrointestinal mucosa, reducing inflammatory responses and oxidative stres.429 Similar to ATB-346, ATB-337 combines an H2S-releasing moiety with an NSAID molecule to reduce gastrointestinal side effects.430 In addition, garlic extracts contain H2S-releasing compounds, with the most characteristic being diallyl thiosulfinate. This compound rapidly decomposes in aqueous solution into various compounds, among which diallyl trisulfide (DATS) generates the highest amount of H2S.431,432,433 However, its limitations include a structure unsuitable for chemical modification, poor water solubility, and the potential reduction of its original physiological effects when these compounds are isolated from garlic.432 SG-1002 is a prodrug of H2S that acts solely through H2S signaling pathways.434 Its unique advantage is its oral administration, which enhances patient compliance.435 Multiple clinical studies have already demonstrated its potential value,436,437 indicating that SG-1002 warrants further investigation in the treatment of H2S-related diseases in the future. Notably, the strong reducing agent dithiothreitol (DTT) can react with disulfide bonds in proteins, reducing them to thiol groups.438 This reaction produces sulfides, which can further react to generate H2S. However, DTT is primarily used in biochemical experiments, particularly in the field of protein research.
Current H₂S donors show great potential, but they have limitations. Inorganic donors like sodium sulfide have rapid oxidation and uncontrolled release, while organic donors such as GYY4137 offer more stability but still face issues with dose control and toxicity. Mitochondria-targeted donors like AP39 show localized effects but lack precise control over H₂S release. Prodrugs like SG-1002 improve oral bioavailability but need further clinical validation. Compounds like ATB-346 combine H₂S release with anti-inflammatory properties but face challenges in structural optimization and solubility. Future research should focus on the development of H₂S donors that allow for more precise, controlled, and sustained release, minimizing the risks of toxicity and side effects. Efforts should also be directed toward improving the pharmacokinetic properties, such as stability and bioavailability, and investigating targeted delivery mechanisms to enhance therapeutic efficacy while reducing off-target effects.
Studies have found that several marketed drugs can upregulate intracellular H2S levels (Table 2). Zofenopril is an angiotensin-converting enzyme inhibitor (ACEI) that has been marketed in Europe and is widely used for the treatment of primary hypertension and acute myocardial infarction. Zofenopril alleviates vascular constriction pressure by inhibiting the generation of angiotensin II, which indirectly induces endothelial cells to release NO and H2S.439,440,441 N-acetylcysteine (NAC) is a widely used medication that has been FDA-approved for the treatment of acetaminophen overdose and is utilized as a mucolytic agent for respiratory conditions such as chronic obstructive pulmonary disease (COPD). The thiol structure of NAC enables it to replenish glutathione (GSH), which is crucial in antioxidant and detoxification processes. Although NAC is not a direct precursor for H2S generation, it indirectly upregulates H2S levels by modulating redox status, thereby providing protective effects against oxidative stress.442,443,444 Metformin is a biguanide antidiabetic medication that was initially approved by the FDA in 1995 for the treatment of type 2 diabetes. It primarily reduces hepatic glucose production and increases peripheral tissue sensitivity to insulin by activating the adenosine 5‘-monophosphate (AMP)-activated protein kinase (AMPK) pathway. Recent studies have demonstrated that metformin can also promote the production of H2S by upregulating the expression of CSE. H2S plays a critical role in metabolic regulation and exerts significant protective effects on the cardiovascular system and in inflammation. This mechanism may partially explain metformin’s role in preventing cardiovascular complications in diabetic patients, as well as its multiple pharmacological effects beyond metabolic improvement.445,446,447 Atorvastatin is one of the most commonly used statins, approved by the FDA in 1996 for the treatment of hypercholesterolemia and the prevention of cardiovascular events. It lowers serum low-density lipoprotein (LDL) levels not only by inhibiting HMG-CoA reductase but also by enhancing the production of H2S in endothelial cells, thereby exerting cardiovascular protective effects.448,449,450 Anetholedithiolethione is a sulfur-containing compound that has been shown in preclinical studies to exert protective effects on the liver and cardiovascular system by activating endogenous H2S production pathways. Although this drug has not been widely approved for clinical use, it is utilized in some countries as an adjunct treatment for liver diseases. It exerts antioxidant and anti-inflammatory effects through the release of H2S. Despite its limited clinical application, the mechanism of H2S release has been demonstrated in several studies.451,452,453 These medications demonstrate significant clinical efficacy within their respective therapeutic areas, and in some cases, promote the generation of H2S, providing a novel pharmacological mechanism for the protection of the cardiovascular system and other organs. The diversity of these drugs is reflected not only in their therapeutic uses and mechanisms of action but also in their routes of administration and widespread global production, underscoring the biological importance of H2S as a gaseous signaling molecule and its broad potential in pharmacological interventions. Current research focuses on the development of H2S donors, H2S prodrugs, and molecular entities capable of targeting and regulating endogenous H2S synthesis or metabolism. In the future, scientists will need to further investigate the safety, dose-dependence, and specific molecular mechanisms of H2S-related therapies to facilitate their application in clinical treatment.
While several marketed drugs, including Zofenopril, NAC, Metformin, Atorvastatin, and Anetholedithiolethione, have shown the ability to upregulate endogenous H₂S production, their limitations remain. These drugs may not directly target H₂S synthesis, but rather modulate its levels indirectly, which could lead to unpredictable or suboptimal effects. The mechanisms of H2S release from these drugs merit study. Additionally, the specific molecular mechanisms underlying their H₂S-related actions are not fully understood, and the safety and efficacy of long-term use in relation to H₂S modulation require further investigation.
Future research should focus on developing more precise H₂S-targeted therapies, optimizing the dose-response relationship, and exploring the safety profiles of H₂S-based treatments. This includes better understanding the molecular pathways that regulate endogenous H₂S synthesis and the potential risks of chronic modulation. The development of H₂S donors, prodrugs, and molecules that can specifically target H₂S production pathways in a controlled and tissue-specific manner will be crucial for advancing clinical applications.
Therapy targeting H2S-producing enzymes
Many natural and synthetic H2S donors also have drawbacks such as short in vivo metabolic half-life, potential toxicity, and poor pharmacokinetics.454,455,456 Similarly, commonly used H2S inhibitors also lack safety and selectivity, especially in their inability to specifically inhibit CBS or CSE, causing significant challenges in the advancement of disease research.14 Hence, an increasing number of scientists are beginning to focus on discovering specific agonists or inhibitors of H2S-generating enzymes (CBS, CSE, 3-MST) based on drug screening technologies (Table 3 and Fig. 5).
Summary of agonists and inhibitors targeting CBS, CSE and 3-MST. CBS activity can be enhanced by the agonist S-adenosylmethionine (AdoMet), while its inhibition is mediated by compounds such as Podocarpusflavone A, Sikokianin C, 2”,4”-Di-O-(Z-p-coumaroyl)afzelin, Agathisflavone, Cupressuflavone, 3’-Hydroxy-Volkensiflavon and Benserazide. CSE activity is stimulated by Norswertianolin (NW) and inhibited by I157172 and NSC4056. For 3-MST, inhibition is achieved by Rutin and Compounds 1, 2, 3, and 5
Drug screening457 first requires identification and confirmation of disease targets. Disease targets can be discovered through disease genomics and proteomics, followed by target confirmation through reverse docking, protein structure prediction, and other methods. The small molecule library used for screening can be obtained from active components of natural products, endogenous bioactive substances, existing drugs, or through tissue chemistry and high-throughput screening. Once these two parts are prepared, structure-based drug design can be carried out, which is currently the most common screening method and is often divided into receptor-based direct methods and ligand-based indirect methods.458,459 The direct method involves molecular docking to predict the binding conformation of ligands and score the rationality and binding affinity of the receptor-ligand binding mode. Subsequently, visual analysis and structural inspection are conducted on the highly scored small molecules to obtain lead compounds. Indirect methods are used to obtain lead compounds by analyzing the three-dimensional structure and conformation of the active small molecule to create a pharmacophore model and subsequently searching a small molecule library for compounds that match the pharmacophore model. Lead compounds can be optimized through principles such as bioisosterism, prodrugs, quantitative structure-activity relationships (QSAR), and 3D-QSAR, followed by in silico ADMET (Absorption, Distribution, Metabolism, Excretion, Toxicity) prediction and physiologically-based pharmacokinetic simulations for preclinical testing.460,461,462 Finally, new drugs are obtained through clinical trials (Fig. 6).
Rational drug design approaches. Drug screening begins with the identification and validation of disease targets, including proteins, nucleic acids, and other biomacromolecules. The small molecule library can be sourced from natural products, endogenous bioactive substances, existing drugs, or high-throughput screening. Structure-based drug design involves receptor-based molecular docking or ligand-based pharmacophore modeling to identify lead compounds. These leads are optimized using bioisosterism, prodrug strategies, and QSAR/3D-QSAR, followed by in silico ADMET (absorption, distribution, metabolism, excretion, toxicity) predictions and PBPK simulations for preclinical evaluation. Promising candidates are then advanced to clinical. Created with BioRender.com
CBS agonists
CBS is a tetrameric enzyme, with each polypeptide chain containing three domains, each of which contains different cofactors required for CBS enzyme activity.463 The N-terminal region binds heme, potentially playing a role in proper enzyme folding and assembly464; next is the central catalytic core that contains a PLP molecule forming a Schiff base with Lys119; and finally, the C-terminal regulatory domain contains a tandem of CBS domains, which bind the CBS allosteric activator SAM most likely.463,465 In order to study the effect of SAM on the stability and activity of wild-type CBS and mutant CBS, Krau463 applied a combination of calorimetric methods, functional assays, and kinetic modeling. Research has identified two distinct binding sites with different binding conformations and properties for SAM at the CBS regulatory domain. The high-affinity site binds two SAM molecules per CBS tetramer, possibly contributing to the kinetic stabilization of the regulatory domain. While the low-affinity site can accommodate up to four SAM molecules and is associated with enzyme activation. CBS half-life is nearly three times shorter under extremely low SAM concentrations, such as during methionine restriction. Under natural circumstances, SAM first stabilizes the basic conformation of CBS. With increasing concentrations of SAM, the CBS regulatory domain undergoes conformational rearrangement, leading to enzyme activation. Meanwhile, SAM maintains the activated conformation, which is essential to enzyme functio.466 The CBS regulatory domain can serve as a novel curative target, while SAM and its structural analogs can serve as original scaffolds for new drugs.
CBS inhibitors
To obtain more efficient and selective CBS inhibitors, an enzyme activity assay method compatible with high-throughput screening is needed. Szabo120 used a commercial AzMc probe to detect H2S generated by CBS and to monitor CBS activity. Researchers screened 8871 clinically used drugs and well-annotated pharmacological compounds. AOAA (a small molecule inhibitor of CBS) was used as a positive control at a compound concentration of 30 μM to assess its ability to inhibit H2S production. The authors identified 30 compounds for further study, among which hexachlorophene (IC50: 60 μM), tannic acid (IC50: 40 μM), and benserazide (IC50: 30 μM) showed concentration-dependent inhibitory effects on CBS. Additionally, benserazide could inhibit the proliferation of colon cancer cell line HT29 with high CBS expression, as well as the growth of tumors in nude mice carrying human colon cancer cell xenografts. Silico docking (Schrodinger Inc., Small-Molecule Drug Discovery Suite, 2016-1) revealed that benserazide binds to the active site of CBS (PDB ID: 1JBQ) and reacts with the PLP cofactor to form a reversible but kinetically stable Schiff base, and its trihydroxybenzyl ring can form hydrogen bonds with polar residues located in the peripheral cavity (such as His203, Tyr223, and Tyr308), resulting in strong inhibition. While benserazide shows potential as an H2S inhibitor, its clinical applicability remains limited by factors such as its pharmacokinetic profile and stability in vivo. The effectiveness of benserazide as a CBS inhibitor in cancer treatment requires further validation through extensive preclinical and clinical studies. Additionally, high specificity and selectivity for CBS inhibition, without off-target effects, must be ensured for therapeutic use.
Similarly, Xu467 also adopted a high-throughput approach to screen for CBS inhibitors. Through their research, the authors explored a new method for measuring enzyme activity that was simple, sensitive, continuous, and not interfered by enzyme assay buffer. CBS could catalyze the production of methanethiol (CH3SH) from methylcysteine.468 The enzymatic activity of CBS was then measured by reacting with the generated CH3SH using a commercial fluorescent thiol probe (CPM), which increased the fluorescence intensity with increasing incubation time. In order to screen for effective CBS inhibitors, the researchers selected 6491 compounds in a natural product library, including compounds isolated from plants and microorganisms, ensuring a wide range of chemical diversity and biological activity. The screening was initially performed at a concentration of 100 μM, and compounds with >80% CBS inhibition were selected for further study. A secondary screening was then conducted at a concentration of 50 μM, and 25 compounds displayed inhibition rates exceeding 50%. Half-maximal inhibitory concentration (IC50) values of the compounds against CBS showed that 11 compounds had IC50 values below 20 μM. H2S generation experiments were used to study the selectivity of these 11 compounds, and the results showed that two compounds exhibited similar inhibitory activities against CSE and CBS; The three compounds exhibited high selectivity for CBS, which were >10 times higher than CSE; The remaining six compounds did not inhibit the activity of CSE, even at high concentrations (IC50 > 400 μM). It is worth noting that these six compounds are all flavonoids, with five of them being biflavonoids. Further validation of these six compounds showed that four of them were able to inhibit the proliferation of HT29 human colon cancer cells, but the anti-proliferation mechanisms of these inhibitors still need to be further elucidated in future studies.
CSE agonists
Geng23 attempted to search for CSE activator in natural small molecules to stimulate the production and release of endogenous H2S. The main strategy was to use molecular docking techniques to screen natural small molecules with high affinity to CSE in the Chinese Natural Product Database (CNPD). The results showed that norswertianolin (NW) had good affinity with CSE, and microscale thermophoresis (MST)750 was used to verify the interaction between NW and CSE (KD = 1.6 ± 0.33 μM). Meanwhile, the binding mode of the interaction between NW and CSE indicated that Leu68 and Asp164 might be important binding sites for their interaction. To verify the binding site, Niu et al. repeated the binding assay using the CSE-GFP mutant protein, and the direct binding between Leu68 mutant protein and NW was weakened, proving that Leu68 was a critical binding site for NW and CSE interaction. By detecting the effect of NW on H2S production in different tissue homogenates, it was found that NW increased H2S production in the heart, aorta, and kidney. This finding was validated in in vivo experiments, where the elevation of H2S in heart and kidney tissues was observed. Additionally, the researchers established an acute renal I/R injury model and found that NW significantly increased CSE activity and alleviated renal injury. In spontaneously hypertensive rats, NW up-regulated CSE expression in the aorta, increased H2S production, and alleviated hypertension, vascular remodeling, and inflammation. Therefore, as a newly discovered small molecule activator of CSE, NW can directly bind to CSE, thereby enhancing H2S production, and has potential value in the treatment of renal I/R injury and cardiovascular diseases.
CSE inhibitors
Inspired by the high-throughput screening method for CBS inhibitors, scientists attempted to use this method to screen for CSE inhibitors. In order to monitor the activity of CSE in a high-throughput mode, Wu et al. designed a method based on tandem-well plate to measure the production of H2S.469 The designed 192-tandem-well plate was modified from a traditional 384-well assay plate by connecting the upper channels between adjacent wells for gas exchange. This device traps and accurately measures the gas generated in the enzymatic reaction solution well and the well adjacent to it, thus eliminating interference from the assay reagents on the enzyme and its substrate. Through this high-throughput screening method,470 62 compounds with CSE inhibition rates >50% were initially selected from 11,954 compounds, with 10 compounds having IC50 values <10 μM. The most potent inhibitor was NSC4056, with an IC50 value of 0.6 μM. Subsequently, researchers tested the effect of NSC4056 on CBS activity, and the results displayed that NSC4056 had a higher inhibitory activity on CSE compared to CBS, with a selectivity of 137-fold higher than CBS. Counter screen assays confirmed the inhibitory activity of NSC4056 on CSE enzymes, indicating that it was not simply trapping H2S. It was also discovered that the inhibitory effect of NSC4056 on CSE could be reversed, suggesting that this compound may be a noncovalent inhibitor of CSE. Unlike most current CSE inhibitors, NSC4056 exerts competitive inhibition on the substrate L-cysteine, rather than being a competitive inhibitor of PLP. NSC4056 completely occupies the same binding site as the L-cysteine substrate, with its two carboxyl groups forming six hydrogen bonds with Arg62, Tyr114, and Arg119, collectively ensuring the inhibitory effect. Structure-activity relationship (SAR)470 is an important method for guiding the optimization design of lead compounds and its study results have shown that the carboxyl group and tripod structure of NSC4056 are essential for inhibiting CSE activity. Further investigation into the effects of NSC4056 on cells revealed that it could reduce the endogenous H2S levels in Raw264.7 cells, with an IC50 value of 43.2 μM, effectively alleviating hypotension in hemorrhagic shock rats. The tandem-well analysis method provides a foundation for the development of more effective and selective CSE inhibitors, and the development of new inhibitors offers new insights into the treatment of related diseases.
Wang121 studied CSE inhibitors using virtual screening technology. The Site Finder module was used to identify the binding pocket of the CSE protein (PDB ID: 3COG), and the Wash module was used to prepare the SPECS compound library (200,000 compounds) to investigate the affinity of compounds for the CSE protein. MOE Dock was used for docking simulations of the ligands. Initially, high-throughput rigid docking was used to filter out many inactive small molecules. Subsequently, the selected 20,000 compounds were subjected to flexible docking using force field refinement to obtain 1000 compounds. These compounds were then ranked, and the top 100 compounds were selected. Among them, I157172 (S: -7.9215) exhibited the highest binding affinity to the protein. To confirm the inhibitory activity of I157172 on CSE, the study further examined the effects of I157172 on H2S production and CSE protein expression. Western blot results also demonstrated that I157172 significantly inhibited CSE protein expression in MCF7 cells. Therefore, I157172 efficiently suppressed the proliferation, migration, and invasion of MCF7 cells. It could be a potential candidate drug for the treatment of breast cancer and further exploration needed to understand its anticancer mechanisms in vivo. It is important to note that the virtual screening approach may not fully account for the dynamic nature of protein-ligand interactions under physiological conditions, which could lead to discrepancies between in silico predictions and actual biological activity. Furthermore, although I157172 demonstrated inhibitory effects on CSE expression in vitro, its efficacy and safety in vivo have not been fully validated, necessitating further preclinical and clinical studies.
3-MST inhibitors
Hanaok471 used H2S selective fluorescent probe HSip-1 for high-throughput screening of a large compound library and discovered effective 3-MST inhibitors. 3-MST utilizes 3-MP as a substrate to generate H2S through enzymatic reaction. HSip-1 is then added to the solution as a fluorescent probe to monitor the production of H2S and evaluate the compound’s activity. The researchers screened a library containing 174,118 compounds, testing all compounds at 10 μM concentration. False positives were eliminated by combining inhibitory activity, resulting in 146 compounds. The dose-dependency (0.25, 1, 3, 10 and 30 μM) of 3-MST-inhibitory activity of each compound was examined to determine the IC50. Compounds 1–3, 5 showed >80% inhibition of 3-MST activity at 10 μM, and their IC50 values were 2–7 μM. High-level coupled-cluster calculation (CCSD(T)) combined with a large aug-cc-pVDZ basis set revealed that compounds 1-3 shared a similar structural backbone, characterized by an aromatic ring-carbonyl-S-pyrimidinone structure. Subsequently, the selectivity of these compounds to 3-MST was examined. Gas chromatography was used to determine the selectivity of compounds 1-3 and 5 towards two other enzymes, CSE and CBS, which also catalyze the production of H2S. It was found that compound 3 exhibited almost no activity against CBS and CSE, indicating its highest selectivity to 3-MST. The X-ray crystal structures of the 3-MST complexes with 1 and 3 revealed that their active pockets were located at the active site of 3-MST, specifically at the perthiolated cysteine residue. Persulfur anions of persulfurated cysteine residues and positively charged carbonyl carbons of pyrimidone moiety of inhibitor have a substantial long-range electrostatic interaction, according to theoretical calculations. The pKa value determined for the cysteine persulfide is 4.34, suggesting that the persulfurated cysteine residue is present in a negatively charged deprotonated state, aligning with the robust electrostatic interaction observed in this investigation. Currently, 3-MST knockout mice have been utilized in many disease studies,472 and these mice are also important tools for investigating the physiological functions of 3-MST. In future work, extensive in vitro and in vivo studies can be conducted with the identified selective 3-MST inhibitors, providing a basis for the treatment of cancer, cardiovascular, and neurological diseases.131
In addition to focusing on mammals, 3-MS473 also has an influence in the generation of sulfides in Leishmania. Vijayakumar474 used molecular docking (the Genetic Optimization for Ligand Docking (GOLD) software) and molecular dynamic simulations to screen the binding affinity of natural compounds against L. donovani 3-MST (Ld3MST). Compared to mammalian 3-MST, Leishmania 3-MST contains an additional 70 amino acids in the C-terminal domain. Due to the lack of X-ray and nuclear magnetic resonance structures for Ld3MST, homology model is required. Using homology model, the Ld3MST protein was docked with 5,284 natural compounds, and the active site and affinity of 3-MP binding to Ld3MST were used as positive controls. A total of 275 natural compounds were discovered. Among them, the dock score (55.30) and binding energy score (-10.5 kcal/mol) of quercetin 3-rutinoside (Rutin) were higher than 3-MP, and Rutin forms more hydrogen bonds with the active site than other compounds. Subsequently, molecular dynamics simulations were performed on three systems: Ld3MST, Ld3MST-3-MP, and Ld3MST-Rutin complex. The trajectories of each system were analyzed and compared. It was found that the average RMSD value of the Ld3MST-Rutin complex (~0.35 nm) was lower than that of other systems, indicating better stability of the Ld3MST-Rutin complex. At the same time, the radius of gyration (Rg) of the Ld3MST-Rutin complex converged over time, and the solvent accessible surface area (SASA, ~44 nm2) remained stable, indicating a compactness and a more stable binding of the complex. Considering the high number of hydrogen bonds and strong binding affinity between Ld3MST and Rutin, Rutin can be considered a potential inhibitor of Ld3MST. Furthermore, the activity of Rutin was verified, with IC50 values of 40.95 μM and 90.09 μM for promastigotes and amastigotes, respectively, and no cytotoxicity at a concentration of 819.00 μM. This study suggests that Rutin may be an effective compound that can be used in combination with other anti-leishmanial drugs. This study also highlights the use of molecular docking and molecular dynamics simulations for screening selective inhibitors of human 3-MST.
Unfortunately, current specific small molecule screening targeting DAO is mainly focused on the effect of DAO on the N-methyl-D-aspartate (NMDA) receptor,475,476,477 while neglecting the important role of DAO in generating H2S, which is also a new direction for future exploration of H2S targeted therapy.
Clinical trials of H2S
Research has found that patients with heart failure (HF) have lower circulating levels of H2S, and there is a negative correlation between H2S levels and the severity of HF.478 A novel H2S prodrug, SG1002, can increase plasma H2S levels (Table 4). The prevalence and incidence of heart failure with preserved ejection fraction (HFpEF) have been rising, with nearly half of all heart failure patients globally being classified as this subtype.479 A preclinical study indicated that,480 adjunctive treatment with SG1002 can enhance circulating and tissue levels of H2S, alleviating cardiac dysfunction in HFpEF and significantly reducing cardiac interstitial fibrosis. Additionally, Krum436 found that H2S levels were lower in patients with HF and were negatively correlated with the severity of HF. A novel H2S precursor, SG1002, was shown to increase plasma H2S levels. Therefore, Krum conducted a Phase I clinical trial to evaluate the changes in H2S levels, treatment effectiveness, and safety of oral SG1002 in both healthy individuals and HF patients. The results showed that SG1002 reduced the levels of B-type natriuretic peptide (BNP), a biomarker for cardiac injury, in the patients’ blood and demonstrated a stable drug level throughout the trial. Furthermore, SG1002 was safe and well tolerated in all participants at all doses. These data suggest that SG1002 is a promising new drug for treating heart failure, but further investigation is needed in larger-scale clinical studies to determine its precise role. The Phase I trial of SG1002 primarily focused on safety and H2S levels, without fully addressing long-term efficacy and potential side effects. While the drug showed promise in reducing BNP levels, its impact on overall heart failure progression and survival remains unclear. Additionally, larger, more diverse clinical trials are needed to confirm the drug’s effectiveness across different stages of heart failure and in various patient populations.
Na2S2O3, a clinically approved H2S donor with little side effects, used for the treatment of cyanide poisoning,481,482 calcific uremic arteriolopathy, and chemotherapy-induced nephrotoxicity (Table 4). A study was conducted on 18 patients who underwent coronary angiography due to acute coronary syndrome. The patients were intravenously administered Na2S2O3 in combination with vasodilators and antihypertensive drugs. No severe adverse events were observed, with only two patients experiencing transient hypotension and one patient experiencing mild nausea. This indicates the safety and tolerability of Na2S2O3 in patients with acute coronary syndrome. However, this study has limitations like a small sample size and a short-term following up, and the benefits of Na2S2O3 treatment must be further tested in larger studies.483 The study on Na₂S₂O₃ demonstrated its safety and tolerability in acute coronary syndrome patients, but its small sample size limits the generalizability of the results. The short-term follow-up period also restricts the understanding of long-term efficacy and potential side effects. Larger, more comprehensive studies with extended follow-up are necessary to fully evaluate the therapeutic benefits and risks of Na₂S₂O₃ in coronary artery disease and other cardiovascular conditions.
As previously mentioned, AP39 is a mitochondria-targeted H2S donor (Table 4). A preclinical study has investigated the effects of AP39 on endothelial cells under both baseline and oxidative stress conditions.484 AP39 has been shown to increase H2S levels within the mitochondria of endothelial cells. Furthermore, the effects of AP39 on mitochondrial activity are concentration-dependent; at low concentrations (30-100 nM), it stimulates mitochondrial electron transport and cellular bioenergetics, while at higher concentrations (300 nM), it exerts an inhibitory effect on mitochondria. Under oxidative stress conditions, pre-treatment with AP39 can attenuate its impact on mitochondrial activity and prevent mitochondrial DNA damage. Mitochondrial dysfunction plays a critical role in cardiovascular diseases, inflammatory disorders, and various critical illnesses, often accompanied by a disruption in the body’s H2S balance.485,486,487 Therefore, mitochondria-selective H2S donors may offer potential therapeutic benefits under certain pathophysiological conditions.
The covalent linkage of NSAIDs with H2S releasing moieties has been shown to significantly reduce gastrointestinal damage and bleeding while enhancing anti-inflammatory and analgesic efficacy.488,489 ATB-352 is a novel H2S-releasing anti-inflammatory agent (Table 4). A preclinical study has evaluated the potential of ATB-352 for application in clinical research.490 In a mouse model of nociceptive hypersensitivity, ATB-352 demonstrated greater analgesic efficacy compared to ketorolac. Ketorolac is a highly effective NSAID but is associated with significant gastrointestinal toxicity. The analgesic effect of 30 mg/kg of ketorolac is comparable to that of ATB-352 at one-third of the molar equivalent dose. Although ATB-352 exhibits notable inhibitory effects on COX, it does not induce gastrointestinal damage. Anandamide is an endogenous cannabinoid that exerts analgesic effects by activating CB1 receptors, and it is considered an analgesic mediator.491 Pre-treatment with the CB1 antagonist AM251 can reverse the analgesic effects of ATB-352, but it does not diminish the analgesic effects of ketorolac. This indicates that endogenous cannabinoids play a significant role in the analgesic properties of ATB-352. Additionally, it is noteworthy that ATB-352 does not activate μ-opioid receptors even at concentrations as high as 30 μg/mL. Therefore, this compound may serve as a promising alternative to opioid analgesics in the treatment of severe pain, potentially addressing the opioid crisis. ATB-352 shows promising analgesic effects with less gastrointestinal toxicity compared to ketorolac, but its long-term safety and human applicability require further clinical evaluation. The exact mechanisms, particularly the role of cannabinoid signaling, need more exploration. While it may serve as an opioid alternative, more comprehensive trials are needed to confirm its efficacy and safety.
ATB-346 is an H2S-NSAID derived from naproxen (Table 4). NSAIDs exert their effects primarily by inhibiting COX, but they often lead to gastrointestinal adverse reactions. In a Phase II clinical trial conducted by researchers,492 244 healthy volunteers were divided into two groups and received either ATB-346 or naproxen, with upper gastrointestinal ulcers assessed through endoscopic examination. Both drugs showed similar inhibition efficiency on COX activity, but the naproxen group experienced more ulcers, particularly larger ones, compared to the ATB-346 group. The incidence of dyspepsia, abdominal pain, and gastroesophageal reflux was lower in the ATB-346 group than in the naproxen group. Additionally, the plasma H2S levels in the ATB-346 group were significantly higher than in the naproxen group, suggesting that H2S may play a role in reducing gastrointestinal toxicity. Gilroy493 also conducted a study on ATB-346. They created an acute skin inflammation model in 23 healthy volunteers and measured the accumulation of inflammatory cells and factors within the inflamed skin. ATB-346 was found to have a strong anti-inflammatory effect, suggesting that H2S release is involved in the regulation of inflammation. However, similar to existing clinical studies, this study had a limited number of participants and lacked subsequent investigations. Nevertheless, it has provided initial evidence of the tremendous potential of H2S in clinical therapy, and we look forward to more follow-up clinical research on H2S in the future.
Furthermore, it is important to mention that NO-releasing NSAIDs have been shown to be effective in preclinical models of inflammation with fewer side effects.494,495 Consequently, researchers have developed a novel compound that combines both NO and H2S gas signaling molecules with the aspirin molecule, referred to as NOSH-aspirin (NBS-1120)496 (Table 4). A preclinical study investigated the gastrointestinal safety, anti-inflammatory, analgesic, antipyretic, antiplatelet, and tumor-inhibiting effects of equimolar doses of aspirin and NBS-1120 in rats.497 The findings indicated that NBS-1120 exhibited lower toxicity and superior safety compared to aspirin. Furthermore, NBS-1120 demonstrated a greater efficacy as a chemopreventive agent, with its effects on tumor growth inhibition and tumor size reduction being dose-dependent. At the highest dose of 100 mg/kg (0.21 mmol/kg), the tumor growth reduction rate was 95%, and the tumor mass reduction rate was 97%. Although NBS-1120 demonstrates superior safety and efficacy compared to aspirin, its potential interactions with other drugs or underlying conditions have not been fully explored. The tumor inhibition results, while promising, are based on preclinical models, and their translation to clinical settings remains uncertain. Furthermore, the long-term pharmacokinetics and toxicity of NBS-1120 need more rigorous investigation before widespread clinical use.
In addition to combining with NSAIDs, researchers have identified that conjugating the H₂S-releasing counterion 3-thiocarbamoylbenzoate (3TCB) with trimebutine can enhance its antispasmodic effect in the gastrointestinal tract. At equimolar doses, this novel compound, GIC-1001 (trimebutine 3-thiocarbamoylbenzene-sulphonate), shows rapid onset of action (2 h) and more effectively mitigates nociceptive responses to colorectal distension, providing pain relief during colonoscopy (Table 4). Additionally, GIC-1001 exhibits significant physical stability and exerts an antihyperalgesic effect through H₂S release.498 As a result, GIC-1001 has been selected as a drug development candidate and has progressed to clinical investigation. In 2012, a Phase I randomized, double-blind, placebo-controlled, comprehensive study was conducted in Canada to evaluate the safety, tolerability, and pharmacokinetics of single and multiple escalating oral doses of GIC-1001, as well as the impact of food on the pharmacokinetics of a single oral dose of GIC-1001 in healthy subjects.499 The results showed no adverse events related to vital signs or ECGs with either single or multiple escalating doses. The pharmacokinetics of GIC-1001 were primarily linear and dose-proportional. These findings indicate that GIC-1001 is well-tolerated, with a safety profile comparable to placebo, and that its safety is consistent under both fed and fasted conditions. However, variability in food intake posed challenges for pharmacokinetic analysis, making it difficult to determine whether GIC-1001 should be taken on an empty stomach. Given that GIC-1001 is intended for use in colonoscopy, where patients must fast beforehand, it is recommended that the drug be administered in a fasted state. Subsequently, a Phase IIa study was conducted in 2013 (ClinicalTrials.gov ID: NCT01926444) involving 240 patients. Eligible patients were randomized in a 1:1:1:2 ratio into one of four treatment groups: GIC-1001 at doses of 250 mg, 375 mg, or 500 mg, and a matching placebo group. Patients underwent unsedated colonoscopy within 3 days of taking the assigned medication. Results showed that the moderate dose (375 mg) of GIC-1001 reduced pain by 26.6% compared to placebo. Based on these findings, GIC-1001 demonstrates promise as a novel colonic analgesic, warranting further clinical investigation.
Conclusion and perspective
In recent decades, the presence of sulfur-containing amino acid metabolic pathway in various cells of the human body has been recognized, with their metabolic products serving as endogenous bioactive molecules responsible for maintaining health. These molecules play crucial roles in multiple biological processes, including anti-inflammatory responses, methylation, antioxidant defense, membrane stabilization, ion transport, osmoregulation, protein synthesis, and energy metabolism. Dysregulation of these sulfur-containing biomolecules can lead to numerous pathological consequences across different systems. By exploring the metabolic mechanisms, signaling pathways, and potential impacts of these sulfur-containing biomolecules in various diseases, we lay the groundwork for understanding their complex biological functions and clinical applications. Importantly, Hcy has been widely recognized as an independent risk factor for cardiovascular diseases. This suggests that future interventions targeting Hcy metabolism may help prevent related diseases. Research on SAM has also provided new perspectives for the development of antidepressant and neuroprotective drugs.500,501 SAM plays a crucial role in maintaining brain function and offers significant insights for the treatment of mood regulation, neuroinflammation, and neurodegenerative diseases.502,503 Additionally, cystine, with its antioxidant properties and role in H2S production, positions it as a potential intervention target for combating oxidative stress, inflammation, and metabolic disorders. H2S, as an endogenous gaseous signaling molecule, participates in life activities such as cell survival, proliferation, differentiation, migration, and death by regulating energy metabolism, inflammatory response, and oxidative homeostatic balance, and plays an important biological effect in physiological and pathophysiological regulation of multiple systems in the body. Currently, there is a large controversy in H2S research. H2S is a double-edged sword that tends to have opposite effects on certain biological processes. For example, the pro-inflammatory and anti-inflammatory effects of H2S. H2S activates NF-κB in pancreatic alveolar cells, promoting inflammation, but inhibit NF-κB in HUVECs, suppressing inflammation. H2S also has a dual role in tumors. H2S can inhibit the aberrant activation of the β-catenin pathway, which in turn inhibits TNBC cell viability, as well as enhance mitochondrial function and glycolysis which in turn promotes colon cancer growth. However, this also indicates that H2S possesses significant research potential. Clarifying the mechanisms by which H2S functions in specific diseases and identifying targeted therapeutic agents could lay the foundation for future treatment strategies.
In future research exploration, the following aspects are worth considering: (1) The role of the methionine cycle in disease prevention and personalized treatment is increasingly recognized. By integrating metabolic biomarkers with genomic and metabolomic data, personalized intervention strategies can be developed, particularly for patients with metabolic disorders. However, the interactions among sulfur-containing biomolecules and their relationships with other nutrients or pharmaceuticals remain incompletely understood, limiting research on their potential synergistic effects. Therefore, future studies should further explore these interactions and expand research on the physiological roles of sulfur-containing biomolecules in immune function and other underexplored systems, especially their role in modulating immune responses and the reactivation of HIV latency.504 (2) Current studies on sulfur-containing biomolecules mostly focus on rats and mice, lacking clinical evidence. The effects of H2S could be studied in large animal models, such as pigs and monkeys, which exhibit similar characteristics to human diseases, to provide a research foundation for clinical trials. (3) In clinical practice, the coexistence of multiple chronic diseases often results in suboptimal treatment outcomes. Therefore, research should expand to explore the therapeutic effects of sulfur-containing biomolecules in the context of comorbidities, leveraging their multi-systemic functions to develop more effective integrated treatment strategies. Additionally, since the effects of sulfur-containing biomolecules are highly tissue-specific, clinical studies should focus on designing methods to selectively modulate the levels of these molecules in specific tissues, ensuring targeted local effects while minimizing potential adverse outcomes in other tissues. (4) Strengthen research on DAO, as current studies mainly focus on the three H2S-producing enzymes CBS, CSE, and 3-MST. In fact, DAO plays a major part in the generation of H2S in the cerebellum and kidneys. Exploring new mechanisms of H2S through DAO as a target can provide new insights for the clinical treatment of cerebellum and kidney-related diseases. (5) When studying endogenous sulfur-containing biomolecules, pay attention to their interaction with other endogenous bioactive small molecules, especially as the fourth emerging endogenous gaseous signal molecule SO2. H2S can oxidize to produce SO2, and both are generated from L-Cys. Therefore, it is important to consider the sulfur-containing amino acid metabolic family as a complex network. Reversing the disrupted sulfur-containing amino acid metabolic homeostasis in diseases is an important scientific question for future research.505
References
Gamgee, A. & Dewar, J. Researches on the constitution and physiological relations of cystine (C(3)H(5)NO(2)S). J. Anat. Physiol. 5, 142–149 (1870).
Plimmer, R. H. The separation of cystine and tyrosine. Biochem J. 7, 311–317 (1913).
Go, Y. M. & Jones, D. P. Cysteine/cystine redox signaling in cardiovascular disease. Free Radic. Biol. Med. 50, 495–509 (2011).
Madden, S. C. et al. Ten amino acids essential for plasma protein production effective orally or intravenously. J. Exp. Med. 77, 277–295 (1943).
Madden, S. C., Woods, R. R., Shull, F. W. & Whipple, G. H. Amino acid mixtures effective parenterally for long continued plasma protein production. Casein digests compared. J. Exp. Med. 79, 607–624 (1944).
Bruk, G. et al. Hyperhomocysteinemia as a cause of erectile dysfunction. Georgian Med. News 350, 54–56 (2024).
Du Vigneaud, V., Loring, H. S. & Craft, H. A. The oxidation of the sulfur of homocystine, methionine, and S-METHYLCYSTEINE in the animal body. J. Biol. Chem. 105, 481–488 (1934).
Szabo, C. A timeline of hydrogen sulfide (H(2)S) research: from environmental toxin to biological mediator. Biochem Pharm. 149, 5–19 (2018).
Cantoni, G. L. S-Adenosylmethionine; a new intermediate formed enzymatically from L-methionine and adenosinetriphosphate. J. Biol. Chem. 204, 403–416 (1953).
De La Haba, G. & Cantoni, G. L. The enzymatic synthesis of S-adenosyl-L-homocysteine from adenosine and homocysteine. J. Biol. Chem. 234, 603–608 (1959).
Abe, K. & Kimura, H. The possible role of hydrogen sulfide as an endogenous neuromodulator. J. Neurosci. 16, 1066–1071 (1996).
Hosoki, R., Matsuki, N. & Kimura, H. The possible role of hydrogen sulfide as an endogenous smooth muscle relaxant in synergy with nitric oxide. Biochem Biophys. Res. Commun. 237, 527–531 (1997).
Li, J. et al. Hydrogen sulfide attenuates ferroptosis and stimulates autophagy by blocking mTOR signaling in sepsis-induced acute lung injury. Mol. Immunol. 141, 318–327 (2022).
Shatalin, K. et al. Inhibitors of bacterial H(2)S biogenesis targeting antibiotic resistance and tolerance. Science 372, 1169–1175 (2021).
Saaranen, M. J. & Ruddock, L. W. Applications of catalyzed cytoplasmic disulfide bond formation. Biochem. Soc. Trans. 47, 1223–1231 (2019).
Lu, S. C. Glutathione synthesis. Biochim. Biophys. Acta 1830, 3143–3153 (2013).
Guertin, D. A. & Wellen, K. E. Acetyl-CoA metabolism in cancer. Nat. Rev. Cancer 23, 156–172 (2023).
Jomova, K. & Valko, M. Advances in metal-induced oxidative stress and human disease. Toxicology 283, 65–87 (2011).
Fang, W. et al. Methionine restriction constrains lipoylation and activates mitochondria for nitrogenic synthesis of amino acids. Nat. Commun. 14, 2504 (2023).
Wu, G. et al. Dietary methionine restriction ameliorated fat accumulation, systemic inflammation, and increased energy metabolism by altering gut microbiota in middle-aged mice administered different fat diets. J. Agric. Food Chem. 68, 7745–7756 (2020).
Djuric, D. M. Editorial: sulfur-containing amino acids in cardiovascular and neural physiology, pathophysiology and pharmacology: an overview and update. Curr. Med. Chem. 25, 322–323 (2018).
Zhang, P. et al. Role of hydrogen sulfide in myocardial ischemia-reperfusion injury. J. Cardiovasc. Pharm. 77, 130–141 (2021).
Niu, Y. et al. Norswertianolin promotes cystathionine gamma-lyase activity and attenuates renal ischemia/reperfusion injury and hypertension. Front Pharm. 12, 677212 (2021).
Loiselle, J. J., Yang, G. & Wu, L. Hydrogen sulfide and hepatic lipid metabolism - a critical pairing for liver health. Br. J. Pharm. 177, 757–768 (2020).
Huang, Y. et al. Hydrogen sulfide and its donors for the treatment of cerebral ischaemia-reperfusion injury: a comprehensive review. Biomed. Pharmacother. 161, 114506 (2023).
Sen, S. et al. Role of cystathionine beta-synthase in human breast cancer. Free Radic. Biol. Med. 86, 228–238 (2015).
Phillips, C. M. et al. Upregulation of cystathionine-beta-synthase in colonic epithelia reprograms metabolism and promotes carcinogenesis. Cancer Res. 77, 5741–5754 (2017).
Guo, H. et al. Characterization of hydrogen sulfide and its synthases, cystathionine beta-synthase and cystathionine gamma-lyase, in human prostatic tissue and cells. Urology 79, 483 e481–483.e485 (2012).
Guo, S. et al. The CBS-H(2)S axis promotes liver metastasis of colon cancer by upregulating VEGF through AP-1 activation. Br. J. Cancer 126, 1055–1066 (2022).
Shackelford, R. E. et al. Molecular functions of hydrogen sulfide in cancer. Pathophysiology 28, 437–456 (2021).
You, J. et al. Cystathionine- gamma-lyase promotes process of breast cancer in association with STAT3 signaling pathway. Oncotarget 8, 65677–65686 (2017).
Paulusma, C. C., Lamers, W. H., Broer, S. & van de Graaf, S. F. J. Amino acid metabolism, transport and signalling in the liver revisited. Biochem Pharm. 201, 115074 (2022).
Li, C. et al. Amino acid catabolism regulates hematopoietic stem cell proteostasis via a GCN2-eIF2alpha axis. Cell Stem Cell 29, 1119–1134.e1117 (2022).
Li, Z. & Zhang, H. Reprogramming of glucose, fatty acid and amino acid metabolism for cancer progression. Cell Mol. Life Sci. 73, 377–392 (2016).
Pencharz, P. B. & Ball, R. O. Amino acid needs for early growth and development. J. Nutr. 134, 1566S–1568S (2004).
Terstappen, F. et al. Prenatal amino acid supplementation to improve fetal growth: a systematic review and meta-analysis. Nutrients. 12, 2535 (2020).
Balakrishnan, M. et al. Growth and neurodevelopmental outcomes of early, high-dose parenteral amino acid intake in very low birth weight infants: a randomized controlled trial. JPEN J. Parenter. Enter. Nutr. 42, 597–606 (2018).
Li, P. et al. Amino acids and immune function. Br. J. Nutr. 98, 237–252 (2007).
Han, C., Ge, M., Ho, P. C. & Zhang, L. Fueling T-cell antitumor immunity: amino acid metabolism revisited. Cancer Immunol. Res. 9, 1373–1382 (2021).
McGaha, T. L. et al. Amino acid catabolism: a pivotal regulator of innate and adaptive immunity. Immunol. Rev. 249, 135–157 (2012).
Brosnan, J. T. & Brosnan, M. E. The sulfur-containing amino acids: an overview. J. Nutr. 136, 1636S–1640S (2006).
Willke, T. Methionine production–a critical review. Appl Microbiol. Biotechnol. 98, 9893–9914 (2014).
Sanderson, S. M., Gao, X., Dai, Z. & Locasale, J. W. Methionine metabolism in health and cancer: a nexus of diet and precision medicine. Nat. Rev. Cancer 19, 625–637 (2019).
Ouyang, Y. et al. S-adenosylmethionine: A metabolite critical to the regulation of autophagy. Cell Prolif. 53, e12891 (2020).
Finkelstein, J. D. The metabolism of homocysteine: pathways and regulation. Eur. J. Pediatr. 157, S40–S44 (1998).
Lu, S. C. Regulation of glutathione synthesis. Mol. Asp. Med. 30, 42–59 (2009).
Gibbs, C. A., Fedoretz-Maxwell, B. P. & Warren, J. J. On the roles of methionine and the importance of its microenvironments in redox metalloproteins. Dalton Trans. 51, 4976–4985 (2022).
Schoneich, C. Redox processes of methionine relevant to beta-amyloid oxidation and Alzheimer’s disease. Arch. Biochem Biophys. 397, 370–376 (2002).
Cantoni, G. Methylation of nicotinamide with a soluble enzyme system from rat liver. J. Biol. Chem. 189, 203-1 (1951).
Bentley, R. Role of sulfur chirality in the chemical processes of biology. Chem. Soc. Rev. 34, 609–624 (2005).
Aposhian, H. V. Enzymatic methylation of arsenic species and other new approaches to arsenic toxicity. Annu Rev. Pharm. Toxicol. 37, 397–419 (1997).
Fontecave, M., Atta, M. & Mulliez, E. S-adenosylmethionine: nothing goes to waste. Trends Biochem. Sci. 29, 243–249 (2004).
Satterwhite, E. R. & Mansfield, K. D. RNA methyltransferase METTL16: targets and function. Wiley Interdiscip. Rev. RNA 13, e1681 (2022).
Fujimori, D. G. Radical SAM-mediated methylation reactions. Curr. Opin. Chem. Biol. 17, 597–604 (2013).
Jones, P. A. Functions of DNA methylation: islands, start sites, gene bodies and beyond. Nat. Rev. Genet 13, 484–492 (2012).
Meyer, K. D. & Jaffrey, S. R. The dynamic epitranscriptome: N6-methyladenosine and gene expression control. Nat. Rev. Mol. Cell Biol. 15, 313–326 (2014).
Kouzarides, T. Chromatin modifications and their function. Cell 128, 693–705 (2007).
Soda, K. Polyamine metabolism and gene methylation in conjunction with one-carbon metabolism. Int. J. Mol. Sci. 19, 3106 (2018).
Casero, R. A. Jr., Murray Stewart, T. & Pegg, A. E. Polyamine metabolism and cancer: treatments, challenges and opportunities. Nat. Rev. Cancer 18, 681–695 (2018).
Pegg, A. E. & Williams-Ashman, H. G. Phosphate-stimulated breakdown of 5’-methylthioadenosine by rat ventral prostate. Biochem J. 115, 241–247 (1969).
Madeo, F., Eisenberg, T., Pietrocola, F. & Kroemer, G. Spermidine in health and disease. Science. 359, eaan2788 (2018).
Pegg, A. E. Functions of polyamines in mammals. J. Biol. Chem. 291, 14904–14912 (2016).
Igarashi, K. & Kashiwagi, K. Modulation of cellular function by polyamines. Int J. Biochem Cell Biol. 42, 39–51 (2010).
Mato, J. M., Martinez-Chantar, M. L. & Lu, S. C. S-adenosylmethionine metabolism and liver disease. Ann. Hepatol. 12, 183–189 (2013).
Frostesjo, L. et al. Interference with DNA methyltransferase activity and genome methylation during F9 teratocarcinoma stem cell differentiation induced by polyamine depletion. J. Biol. Chem. 272, 4359–4366 (1997).
Dante, R., Arnaud, M. & Niveleau, A. Effects of 5’deoxy-5’-methylthioadenosine on the metabolism of S-adenosyl methionine. Biochem Biophys. Res. Commun. 114, 214–221 (1983).
Kujubu, D. A. et al. Early responses of PC-12 cells to NGF and EGF: effect of K252a and 5’-methylthioadenosine on gene expression and membrane protein methylation. J. Neurosci. Res. 36, 58–65 (1993).
Broderick, J. B., Broderick, W. E. & Hoffman, B. M. Radical SAM enzymes: Nature’s choice for radical reactions. FEBS Lett. 597, 92–101 (2023).
Broderick, W. E. & Broderick, J. B. Radical SAM enzymes: surprises along the path to understanding mechanism. J. Biol. Inorg. Chem. 24, 769–776 (2019).
Vizan, P., Di Croce, L. & Aranda, S. Functional and pathological roles of AHCY. Front Cell Dev. Biol. 9, 654344 (2021).
Kloor, D. & Osswald, H. S-Adenosylhomocysteine hydrolase as a target for intracellular adenosine action. Trends Pharm. Sci. 25, 294–297 (2004).
Ingrosso, D. et al. Influence of osmotic stress on protein methylation in resealed erythrocytes. Eur. J. Biochem. 244, 918–922 (1997).
Mi, J. et al. S-adenosylhomocysteine induces cellular senescence in rat aorta vascular smooth muscle cells via NF-kappaB-SASP pathway. J. Nutr. Biochem. 107, 109063 (2022).
You, Y. et al. Inhibition of S-adenosylhomocysteine hydrolase induces endothelial senescence via hTERT downregulation. Atherosclerosis 353, 1–10 (2022).
You, Y. et al. Epigenetic modulation of Drp1-mediated mitochondrial fission by inhibition of S-adenosylhomocysteine hydrolase promotes vascular senescence and atherosclerosis. Redox Biol. 65, 102828 (2023).
Wang, Y. et al. Insufficient S-adenosylhomocysteine hydrolase compromises the beneficial effect of diabetic BMSCs on diabetic cardiomyopathy. Stem Cell Res. Ther. 13, 418 (2022).
Hermann, A. & Sitdikova, G. Homocysteine: biochemistry, molecular biology and role in disease. Biomolecules. 11, 737 (2021).
Raghubeer, S. & Matsha, T. E. Methylenetetrahydrofolate (MTHFR), the one-carbon cycle, and cardiovascular risks. Nutrients. 13, 4562 (2021).
Zaric, B. L. et al. Homocysteine and hyperhomocysteinaemia. Curr. Med. Chem. 26, 2948–2961 (2019).
Yang, Z. J. et al. Betaine alleviates cognitive impairment induced by homocysteine through attenuating NLRP3-mediated microglial pyroptosis in an m(6)A-YTHDF2-dependent manner. Redox Biol. 69, 103026 (2024).
Imbard, A. et al. Plasma choline and betaine correlate with serum folate, plasma S-adenosyl-methionine and S-adenosyl-homocysteine in healthy volunteers. Clin. Chem. Lab. Med. 51, 683–692 (2013).
Bhatia, M. et al. Allosteric inhibition of MTHFR prevents futile SAM cycling and maintains nucleotide pools in one-carbon metabolism. J. Biol. Chem. 295, 16037–16057 (2020).
Prudova, A. et al. S-adenosylmethionine stabilizes cystathionine beta-synthase and modulates redox capacity. Proc. Natl Acad. Sci. USA 103, 6489–6494 (2006).
Huang, C. F. et al. Echinocystic acid ameliorates hyperhomocysteinemia-induced vascular endothelial cell injury through regulating NF-kappaB and CYP1A1. Exp. Ther. Med. 14, 4174–4180 (2017).
Ji, C. et al. Propofol alleviates inflammation and apoptosis in HCY‑induced HUVECs by inhibiting endoplasmic reticulum stress. Mol. Med. Rep. 23, 333 (2021).
Wu, Y. et al. The expression of SAH, IL-1beta, Hcy, TNF-alpha and BDNF in coronary heart disease and its relationship with the severity of coronary stenosis. BMC Cardiovasc. Disord. 22, 101 (2022).
Jakubowski, H. Homocysteine modification in protein structure/function and human disease. Physiol. Rev. 99, 555–604 (2019).
Liu, L. et al. Plasma homocysteine and autonomic nervous dysfunction: association and clinical relevance in OSAS. Dis. Markers 2020, 4378505 (2020).
Pi, T., Liu, B. & Shi, J. Abnormal homocysteine metabolism: an insight of alzheimer’s disease from DNA methylation. Behav. Neurol. 2020, 8438602 (2020).
Park, J. H. et al. Effect of B-vitamins on stroke risk among individuals with vascular disease who are not on antiplatelets: A meta-analysis. Int J. Stroke 11, 206–211 (2016).
Marti-Carvajal, A. J., Sola, I., Lathyris, D. & Dayer, M. Homocysteine-lowering interventions for preventing cardiovascular events. Cochrane Database Syst. Rev. 8, CD006612 (2017).
Lu, S. C. Regulation of hepatic glutathione synthesis. Semin. Liver Dis. 18, 331–343 (1998).
Forman, H. J., Zhang, H. & Rinna, A. Glutathione: overview of its protective roles, measurement, and biosynthesis. Mol. Asp. Med. 30, 1–12 (2009).
Dixon, S. J. et al. Ferroptosis: an iron-dependent form of nonapoptotic cell death. Cell 149, 1060–1072 (2012).
Stockwell, B. R. et al. Ferroptosis: a eegulated cell death nexus linking metabolism, redox biology, and disease. Cell 171, 273–285 (2017).
Koppula, P., Zhuang, L. & Gan, B. Cystine transporter SLC7A11/xCT in cancer: ferroptosis, nutrient dependency, and cancer therapy. Protein Cell 12, 599–620 (2021).
Dixon, S. J. et al. Pharmacological inhibition of cystine-glutamate exchange induces endoplasmic reticulum stress and ferroptosis. Elife 3, e02523 (2014).
Huang, C. W. et al. Hydrogen sulfide and its roles in Saccharomyces cerevisiae in a winemaking context. FEMS Yeast Res. 17, 6 (2017).
Simoni, R. D., Hill, R. L. & Vaughan, M. A new sulfur-containing amino-acid isolated from the hydrolytic products of protein(Mueller, J. H. (1923) J. Biol. Chem. 56, 157-169). J. Biol. Chem. 277, 14e (2002).
Barger, G. & Coyne, F. P. The amino-acid methionine; constitution and synthesis. Biochem J. 22, 1417–1425 (1928).
Ericson, L. E., Williams, J. N. Jr. & Elvehjem, C. A. Studies on partially purified betaine-homocysteine transmethylase of liver. J. Biol. Chem. 212, 537–544 (1955).
Gayon, U. J. C. R. A. S. Note de MU. Gayon presentee par M. Pasteur 85, 1074–1076 (1877).
Myers, J. T. The production of hydrogen sulphide by bacteria. J. Bacteriol. 5, 231–252 (1920).
Rodler, M., Vadon, V. & Pekar, K. Ability to form H2S in various bacteria. Zentralbl Bakteriol. Orig. 206, 117–122 (1968).
Massidda, A. Production of H2s in brucella. Nuovi. Ann. Ig. Microbiol 15, 424–431 (1964).
Clarke, P. H. Hydrogen sulphide production by bacteria. J. Gen. Microbiol 8, 397–407 (1953).
Stutzenberger, F. J. & Bennett, E. O. Sensitivity of mixed populations of staphylococcus aureus and escherichia coli to mercurials. Appl. Microbiol. 13, 570–574 (1965).
Kadota, H. & Ishida, Y. Production of volatile sulfur compounds by microorganisms. Annu. Rev. Microbiol. 26, 127–138 (1972).
Hanson, H. & Eisfeld, G. Intermediary sulfur metabolism. III. Formation of hydrogen sulfide from cystine and cysteine by the liver. Z. Gesamt. Inn. Med. 7, 801–810 (1952).
Chatagner, F. & Sauret-Ignazi, G. Role of transamination and pyridoxal phosphate in the enzymatic formation of hydrogen sulfide from cysteine by the rat liver under anaerobiosis. Bull. Soc. Chim. Biol. (Paris) 38, 415–428 (1956).
Hylin, J. W. & Wood, J. L. Enzymatic formation of polysulfides from mercaptopyruvate. J. Biol. Chem. 234, 2141–2144 (1959).
Yao, K. Effects of several unusual sulfur-containing amino acids on rat liver cystathionine-gamma-lyase. Physiol. Chem. Phys. 7, 401–408 (1975).
De Cormis, L. J. C. A. S. Release of hydrogen sulfide into an atmosphere containing sulfur dioxide. 266, 683–685 (1968).
Fenchel, T. & Riedl, R. J. M. B. The sulfide system: a new biotic community underneath the oxidized layer of marine sand bottoms. 7, 255–268 (1970).
Jannasch, H. W. & Wirsen, C. O. Morphological survey of microbial mats near deep-sea thermal vents. Appl Environ. Microbiol 41, 528–538 (1981).
Jannasch, H. W. & Mottl, M. J. Geomicrobiology of deep-sea hydrothermal vents. Science 229, 717–725 (1985).
Gaill, F. Aspects of life development at deep sea hydrothermal vents. FASEB J. 7, 558–565 (1993).
Sylvan, J. B., Toner, B. M. & Edwards, K. J. Life and death of deep-sea vents: bacterial diversity and ecosystem succession on inactive hydrothermal sulfides. mBio 3, e00279–00211 (2012).
Sugiyama, E. et al. Precolumn derivatization LC/MS method for observation of efficient hydrogen sulfide supply to the kidney via d-cysteine degradation pathway. J. Pharm. Biomed. Anal. 222, 115088 (2023).
Druzhyna, N. et al. Screening of a composite library of clinically used drugs and well-characterized pharmacological compounds for cystathionine beta-synthase inhibition identifies benserazide as a drug potentially suitable for repurposing for the experimental therapy of colon cancer. Pharm. Res 113, 18–37 (2016).
Wang, L. et al. I157172, a novel inhibitor of cystathionine gamma-lyase, inhibits growth and migration of breast cancer cells via SIRT1-mediated deacetylation of STAT3. Oncol. Rep. 41, 427–436 (2019).
Liu, Y. H. et al. Hydrogen sulfide in the mammalian cardiovascular system. Antioxid. Redox Signal 17, 141–185 (2012).
Fernandez-Rodriguez, C. et al. Structural basis of the inhibition of cystathionine gamma-lyase from Toxoplasma gondii by propargylglycine and cysteine. Protein Sci. 32, e4619 (2023).
Yang, Q. & He, G. W. Imbalance of homocysteine and H(2)S: significance, mechanisms, and therapeutic promise in vascular injury. Oxid. Med. Cell Longev. 2019, 7629673 (2019).
Giuffre, A. & Vicente, J. B. Hydrogen sulfide biochemistry and interplay with other gaseous mediators in mammalian physiology. Oxid. Med. Cell Longev. 2018, 6290931 (2018).
Ascencao, K. & Szabo, C. Emerging roles of cystathionine beta-synthase in various forms of cancer. Redox Biol. 53, 102331 (2022).
Jia, Y. et al. Rational design of a profluorescent substrate for S-adenosylhomocysteine hydrolase and its applications in bioimaging and inhibitor screening. ACS Appl. Mater. Interfaces 8, 25818–25824 (2016).
Henthorn, H. A. & Pluth, M. D. Mechanistic insights into the H(2)S-mediated reduction of aryl azides commonly used in H(2)S detection. J. Am. Chem. Soc. 137, 15330–15336 (2015).
Shibuya, N. & Kimura, H. Production of hydrogen sulfide from d-cysteine and its therapeutic potential. Front Endocrinol. (Lausanne) 4, 87 (2013).
Mikami, Y. et al. Thioredoxin and dihydrolipoic acid are required for 3-mercaptopyruvate sulfurtransferase to produce hydrogen sulfide. Biochem J. 439, 479–485 (2011).
Rao, S. P., Dobariya, P., Bellamkonda, H. & More, S. S. Role of 3-mercaptopyruvate sulfurtransferase (3-MST) in physiology and disease. Antioxidants (Basel). 12, 603 (2023).
Augsburger, F. & Szabo, C. Potential role of the 3-mercaptopyruvate sulfurtransferase (3-MST)-hydrogen sulfide (H(2)S) pathway in cancer cells. Pharm. Res. 154, 104083 (2020).
Ye, H. et al. Rational design of a dual-reactive probe for imaging the biogenesis of both H(2)S and GSH from l-Cys rather than d-Cys in live cells. RSC Chem. Biol. 3, 848–852 (2022).
Schumann, U. & Subramani, S. Special delivery from mitochondria to peroxisomes. Trends Cell Biol. 18, 253–256 (2008).
Suzuki, Y., Saito, J., Munakata, M. & Shibata, Y. Hydrogen sulfide as a novel biomarker of asthma and chronic obstructive pulmonary disease. Allergol. Int. 70, 181–189 (2021).
Insko, M. A. et al. Detection of exhaled hydrogen sulphide gas in rats exposed to intravenous sodium sulphide. Br. J. Pharm. 157, 944–951 (2009).
Toombs, C. F. et al. Detection of exhaled hydrogen sulphide gas in healthy human volunteers during intravenous administration of sodium sulphide. Br. J. Clin. Pharm. 69, 626–636 (2010).
Suzuki, N. et al. Induction and inhibition of oral malodor. Mol. Oral. Microbiol. 34, 85–96 (2019).
Jia, J. et al. SQR mediates therapeutic effects of H(2)S by targeting mitochondrial electron transport to induce mitochondrial uncoupling. Sci. Adv. 6, eaaz5752 (2020).
Beltowski, J. Synthesis, metabolism, and signaling mechanisms of hydrogen sulfide: an overview. Methods Mol. Biol. 2007, 1–8 (2019).
Landry, A. P., Ballou, D. P. & Banerjee, R. H(2)S oxidation by nanodisc-embedded human sulfide quinone oxidoreductase. J. Biol. Chem. 292, 11641–11649 (2017).
Kamoun, P. H2S, a new neuromodulator. Med. Sci. (Paris) 20, 697–700 (2004).
Weisiger, R. A., Pinkus, L. M. & Jakoby, W. B. Thiol S-methyltransferase: suggested role in detoxication of intestinal hydrogen sulfide. Biochem. Pharm. 29, 2885–2887 (1980).
Weisiger, R. A. & Jakoby, W. B. Thiol S-methyltransferase from rat liver. Arch. Biochem. Biophys. 196, 631–637 (1979).
Hiemke, C. & Ghraf, R. Distribution and properties of thiol S-methyltransferase in rat brain. J. Neurochem. 40, 592–594 (1983).
Jensen, B. & Fago, A. Reactions of ferric hemoglobin and myoglobin with hydrogen sulfide under physiological conditions. J. Inorg. Biochem. 182, 133–140 (2018).
Suzuki, Y. et al. Methemoglobin-albumin clusters for the treatment of hydrogen sulfide intoxication. J. Control Release 349, 304–314 (2022).
Lin, K. et al. Disrupted methionine cycle triggers muscle atrophy in cancer cachexia through epigenetic regulation of REDD1. Cell Metab. 37, 460–476.E8 (2024).
Lu, Y. et al. Lactylation-driven IGF2BP3-mediated serine metabolism reprogramming and RNA m6A-modification promotes lenvatinib resistance in HCC. Adv. Sci. (Weinh.) 11, e2401399 (2024).
Verdejo-Torres, O. et al. Cysteine rich intestinal protein 2 is a copper-responsive regulator of skeletal muscle differentiation and metal homeostasis. PLoS Genet 20, e1011495 (2024).
Yu, Z. J. et al. Gold nanoparticles-based colorimetric immunoassay of carcinoembryonic antigen with metal-organic framework to load quinones for catalytic oxidation of cysteine. Sensors (Basel). 24, 6701 (2024).
Huang, Y. Q. et al. Interaction among hydrogen sulfide and other gasotransmitters in mammalian physiology and pathophysiology. Adv. Exp. Med. Biol. 1315, 205–236 (2021).
Irvine, J. C., Ravi, R. M., Kemp-Harper, B. K. & Widdop, R. E. Nitroxyl donors retain their depressor effects in hypertension. Am. J. Physiol. Heart Circ. Physiol. 305, H939–H945 (2013).
Mancardi, D. et al. HNO protects the myocardium against reperfusion injury, inhibiting the mPTP opening via PKCepsilon activation. Antioxidants (Basel). 11, 382 (2022).
Kimura, H. Hydrogen sulfide (H(2)S)/polysulfides (H(2)S(n)) signalling and TRPA1 channels modification on sulfur metabolism. Biomolecules. 14, 129 (2024).
Peleli, M., Zampas, P. & Papapetropoulos, A. Hydrogen sulfide and the kidney: physiological roles, contribution to pathophysiology, and therapeutic potential. Antioxid. Redox Signal 36, 220–243 (2022).
Zaorska, E. et al. Hydrogen sulfide in pharmacotherapy, beyond the hydrogen sulfide-donors. Biomolecules. 10, 323 (2020).
Webb, G. D. et al. Contractile and vasorelaxant effects of hydrogen sulfide and its biosynthesis in the human internal mammary artery. J. Pharm. Exp. Ther. 324, 876–882 (2008).
Sheibani, L. et al. Augmented H2S production via cystathionine-beta-synthase upregulation plays a role in pregnancy-associated uterine vasodilation. Biol. Reprod. 96, 664–672 (2017).
Song, H. B. et al. Significance of serum NT-proBNP and endogenous H(2)S for predicting coronary artery lesions in pediatric kawasaki disease. J. Coll. Physicians Surg. Pak. 30, 37–40 (2020).
Siegel, L. M. A Direct microdetermination for sulfide. Anal. Biochem. 11, 126–12 (1965).
Brown, M. D., Hall, J. R. & Schoenfisch, M. H. A direct and selective electrochemical hydrogen sulfide sensor. Anal. Chim. Acta. 1045, 67–76 (2019).
Li, X. H., Zhang, C. Y., Wu, J. X. & Zhang, T. Changes in plasma hydrogen sulfide and nitric oxide levels and their clinical significance in children with Kawasaki disease. Chin. Med. J. (Engl.) 124, 3445–3449 (2011).
Yang, G. et al. H2S as a physiologic vasorelaxant: hypertension in mice with deletion of cystathionine gamma-lyase. Science 322, 587–590 (2008).
Zhang, L. et al. Ag(2)S/Ag nanoparticle microelectrodes for in vivo potentiometric measurement of hydrogen sulfide dynamics in the rat brain. Anal. Chem. 93, 7063–7070 (2021).
Zhen, Y. et al. Exogenous hydrogen sulfide exerts proliferation/anti-apoptosis/angiogenesis/migration effects via amplifying the activation of NF-kappaB pathway in PLC/PRF/5 hepatoma cells. Int. J. Oncol. 46, 2194–2204 (2015).
Velazquez-Moyado, J. A. & Navarrete, A. The detection and quantification, in vivo and in real time, of hydrogen sulfide in ethanol-induced lesions in rat stomachs using an ion sensitive electrode. J. Pharm. Toxicol. Methods 89, 54–58 (2018).
Tian, X., Li, Z., Lau, C. & Lu, J. Visualization of in vivo hydrogen sulfide production by a bioluminescence probe in cancer cells and nude mice. Anal. Chem. 87, 11325–11331 (2015).
Olson, K. R., Gao, Y. & Straub, K. D. Oxidation of hydrogen sulfide by quinones: how polyphenols initiate their cytoprotective effects. Int. J. Mol. Sci. 22, 961 (2021).
Wang, L. Y., Chen, X. G. & Cao, D. R. A nitroolefin functionalized DPP fluorescent probe for the selective detection of hydrogen sulfide. N. J. Chem. 41, 3367–3373 (2017).
Liu, C. R. et al. Capture and visualization of hydrogen sulfide by a fluorescent probe. Angew. Chem. Int. Ed. 50, 10327–10329 (2011).
Peng, B. et al. Fluorescent probes based on nucleophilic substitution-cyclization for hydrogen sulfide detection and bioimaging. Chem.-Eur. J. 20, 1010–1016 (2014).
Liu, C. R. et al. Reaction based fluorescent probes for hydrogen sulfide. Org. Lett. 14, 2184–2187 (2012).
Singha, S. et al. Toward a selective, sensitive, fast-responsive, and biocompatible two-photon probe for hydrogen sulfide in live cells. Anal. Chem. 87, 1188–1195 (2015).
Wu, Q., Huo, F. J., Wang, J. P. & Yin, C. X. Fluorescent probe for detecting hydrogen sulfide based on disulfide nucleophilic substitution-addition. Spectrochim. Acta. A. 238, 118437 (2020).
Liu, J. et al. Molecular engineering of aqueous soluble triarylboron-compound-based two-photon fluorescent probe for mitochondria H2S with analyte-induced finite aggregation and excellent membrane permeability. Anal. Chem. 88, 1052–1057 (2016).
Chen, L. L., Huang, P. H., Tan, H. L. & Wang, L. A terbium(III)-based coordination polymer for time-resolved determination of hydrogen sulfide in human serum displacement of copper(II). Anal. Methods-Uk 9, 1004–1010 (2017).
Moretti, M. et al. Fatal poisoning of four workers in a farm: distribution of hydrogen sulfide and thiosulfate in 10 different biological matrices. Forensic Sci. Int. 316, 110525 (2020).
Vitvitsky, V. & Banerjee, R. H2S analysis in biological samples using gas chromatography with sulfur chemiluminescence detection. Methods Enzymol. 554, 111–123 (2015).
Shen, X. et al. Measurement of plasma hydrogen sulfide in vivo and in vitro. Free Radic. Biol. Med. 50, 1021–1031 (2011).
Klingerman, C. M., Trushin, N., Prokopczyk, B. & Haouzi, P. H2S concentrations in the arterial blood during H2S administration in relation to its toxicity and effects on breathing. Am. J. Physiol. Regul. Integr. Comp. Physiol. 305, R630–R638 (2013).
Luo, S. et al. Endothelial HDAC1-ZEB2-NuRD complex drives aortic aneurysm and dissection through regulation of protein S-Sulfhydration. Circulation 147, 1382–1403 (2023).
Weng, L. et al. TGF-beta1/SMAD3 regulates programmed cell death 5 that suppresses cardiac fibrosis post-myocardial infarction by inhibiting HDAC3. Circ. Res. 133, 237–251 (2023).
Yuan, J. et al. Microneedle patch loaded with exosomes containing microRNA-29b prevents cardiac fibrosis after myocardial infarction. Adv. Health. Mater. 12, e2202959 (2023).
Micheletti, R. et al. The long noncoding RNA Wisper controls cardiac fibrosis and remodeling. Sci. Transl. Med. 9, eaai9118 (2017).
Zhao, K. et al. Alamandine alleviated heart failure and fibrosis in myocardial infarction mice. Biol. Direct 17, 25 (2022).
Zhao, Q. et al. Metformin decreased myocardial fibrosis and apoptosis in hyperhomocysteinemia -induced cardiac hypertrophy. Curr. Res Transl. Med. 69, 103270 (2021).
Nam, M., Jung, Y., Ryu, D. H. & Hwang, G. S. A metabolomics-driven approach reveals metabolic responses and mechanisms in the rat heart following myocardial infarction. Int. J. Cardiol. 227, 239–246 (2017).
Li, Y. et al. Exogenous hydrogen sulfide inhibits apoptosis by regulating endoplasmic reticulum stress-autophagy axis and improves myocardial reconstruction after acute myocardial infarction. Acta Biochim Biophys. Sin. (Shanghai) 52, 1325–1336 (2020).
Guo, Z. et al. CSE/H2S system protects mesenchymal stem cells from hypoxia and serum deprivation‑induced apoptosis via mitochondrial injury, endoplasmic reticulum stress and PI3K/Akt activation pathways. Mol. Med. Rep. 12, 2128–2134 (2015).
Yang, T. et al. AP39 inhibits ferroptosis by inhibiting mitochondrial autophagy through the PINK1/parkin pathway to improve myocardial fibrosis with myocardial infarction. Biomed. Pharmacother. 165, 115195 (2023).
Angelovski, M. et al. Myocardial infarction and oxidative damage in animal models: objective and expectations from the application of cysteine derivatives. Toxicol. Mech. Methods 33, 1–17 (2023).
Nishizawa, H. et al. Ferroptosis is controlled by the coordinated transcriptional regulation of glutathione and labile iron metabolism by the transcription factor BACH1. J. Biol. Chem. 295, 69–82 (2020).
Gao, E. et al. A novel and efficient model of coronary artery ligation and myocardial infarction in the mouse. Circ. Res. 107, 1445–1453 (2010).
Chen, C. L. et al. Mitochondrial redox regulation and myocardial ischemia-reperfusion injury. Am. J. Physiol. Cell Physiol. 322, C12–C23 (2022).
Lee, H. L. et al. Biphasic modulation of the mitochondrial electron transport chain in myocardial ischemia and reperfusion. Am. J. Physiol. Heart Circ. Physiol. 302, H1410–H1422 (2012).
Jang, S. et al. Elucidating mitochondrial electron transport chain supercomplexes in the heart during ischemia-reperfusion. Antioxid. Redox Signal 27, 57–69 (2017).
Hashmi, S. & Al-Salam, S. Acute myocardial infarction and myocardial ischemia-reperfusion injury: a comparison. Int. J. Clin. Exp. Pathol. 8, 8786–8796 (2015).
Li, N. et al. Chemotactic NO/H(2)S nanomotors realizing cardiac targeting of G-CSF against myocardial ischemia-reperfusion injury. ACS Nano 17, 12573–12593 (2023).
Xu, S. et al. Macrophage heterogeneity and its impact on myocardial ischemia-reperfusion injury: An Integrative Review. J. Inflamm. Res. 16, 5971–5987 (2023).
Liu, X. et al. Actin cytoskeleton vulnerability to disulfide stress mediates disulfidptosis. Nat. Cell Biol. 25, 404–414 (2023).
Qian, S. et al. Disulfide stress and its role in cardiovascular diseases. Redox Biol. 75, 103297 (2024).
Rashdan, N. A., Shrestha, B. & Pattillo, C. B. S-glutathionylation, friend or foe in cardiovascular health and disease. Redox Biol. 37, 101693 (2020).
Wang, L., Niu, H. & Zhang, J. Homocysteine induces mitochondrial dysfunction and oxidative stress in myocardial ischemia/reperfusion injury through stimulating ROS production and the ERK1/2 signaling pathway. Exp. Ther. Med. 20, 938–944 (2020).
Pan, Y. et al. Dietary methionine restriction attenuates renal ischaemia/reperfusion-induced myocardial injury by activating the CSE/H2S/ERS pathway in diabetic mice. J. Cell Mol. Med. 24, 9890–9897 (2020).
Lazarevic, M. et al. The H(2)S donor GYY4137 stimulates reactive oxygen species generation in BV2 cells while suppressing the secretion of TNF and Nitric Oxide. Molecules. 23, 2966 (2018).
Elrod, J. W. et al. Hydrogen sulfide attenuates myocardial ischemia-reperfusion injury by preservation of mitochondrial function. Proc. Natl Acad. Sci. USA 104, 15560–15565 (2007).
Luo, Y. et al. Activation of the CaR-CSE/H2S pathway confers cardioprotection against ischemia-reperfusion injury. Exp. Cell Res. 398, 112389 (2021).
Meng, G. et al. GYY4137 protects against myocardial ischemia and reperfusion injury by attenuating oxidative stress and apoptosis in rats. J. Biomed. Res. 29, 203–213 (2015).
Xie, H. et al. Hydrogen sulfide protects against myocardial ischemia and reperfusion injury by activating AMP-activated protein kinase to restore autophagic flux. Biochem. Biophys. Res. Commun. 458, 632–638 (2015).
Gimbrone, M. A. Jr. & Garcia-Cardena, G. Endothelial cell dysfunction and the pathobiology of atherosclerosis. Circ. Res. 118, 620–636 (2016).
Xu, S. et al. Endothelial dysfunction in atherosclerotic cardiovascular diseases and beyond: from mechanism to pharmacotherapies. Pharm. Rev. 73, 924–967 (2021).
Back, M. et al. Inflammation and its resolution in atherosclerosis: mediators and therapeutic opportunities. Nat. Rev. Cardiol. 16, 389–406 (2019).
Dhar, I. et al. Plasma methionine and risk of acute myocardial infarction: Effect modification by established risk factors. Atherosclerosis 272, 175–181 (2018).
Dai, X. et al. Betaine supplementation attenuates S-adenosylhomocysteine hydrolase-deficiency-accelerated atherosclerosis in apolipoprotein E-deficient mice. Nutrients. 14, 718 (2022).
Roman, M. J. et al. Rate and determinants of progression of atherosclerosis in systemic lupus erythematosus. Arthritis Rheum. 56, 3412–3419 (2007).
Munteanu, C. Hydrogen sulfide and oxygen homeostasis in atherosclerosis: a systematic review from molecular biology to therapeutic perspectives. Int. J. Mol. Sci. 24, 8376 (2023).
Bai, Z. et al. Anti-atherosclerosis effect of H(2)S donors based on nicotinic acid and chlorfibrate structures. Bioorg. Med. Chem. 27, 3307–3318 (2019).
Ford, A., Al-Magableh, M., Gaspari, T. A. & Hart, J. L. Chronic NaHS treatment is vasoprotective in high-fat-fed ApoE(-/-) mice. Int J. Vasc. Med. 2013, 915983 (2013).
Tian, D. et al. Endogenous hydrogen sulfide improves vascular remodeling through PPARdelta/SOCS3 signaling. J. Adv. Res. 27, 115–125 (2021).
Nakamura, M. & Sadoshima, J. Mechanisms of physiological and pathological cardiac hypertrophy. Nat. Rev. Cardiol. 15, 387–407 (2018).
Tham, Y. K. et al. Pathophysiology of cardiac hypertrophy and heart failure: signaling pathways and novel therapeutic targets. Arch. Toxicol. 89, 1401–1438 (2015).
Nomura, S. et al. Cardiomyocyte gene programs encoding morphological and functional signatures in cardiac hypertrophy and failure. Nat. Commun. 9, 4435 (2018).
Deng, Y. et al. Hyperhomocysteinemia promotes cardiac hypertrophy in hypertension. Oxid. Med Cell Longev. 2022, 1486157 (2022).
Kar, S. et al. Hydrogen sulfide ameliorates homocysteine-induced cardiac remodeling and dysfunction. Front Physiol. 10, 598 (2019).
Lu, F. et al. Exogenous hydrogen sulfide prevents cardiomyocyte apoptosis from cardiac hypertrophy induced by isoproterenol. Mol. Cell Biochem. 381, 41–50 (2013).
Ellmers, L. J. et al. Hydrogen sulfide treatment improves post-infarct remodeling and long-term cardiac function in CSE knockout and wild-type mice. Int. J. Mol. Sci. 21, 4284 (2020).
Peleli, M. et al. Cardiovascular phenotype of mice lacking 3-mercaptopyruvate sulfurtransferase. Biochem. Pharm. 176, 113833 (2020).
Liang, M. et al. Hydrogen sulfide improves glucose metabolism and prevents hypertrophy in cardiomyocytes. Nitric Oxide 46, 114–122 (2015).
Borst, M. M., Deussen, A. & Schrader, J. S-adenosylhomocysteine hydrolase activity in human myocardium. Cardiovasc. Res. 26, 143–147 (1992).
Waypa, G. B. et al. Mitochondria regulate proliferation in adult cardiac myocytes. J. Clin. Invest. 134, e165482 (2024).
Rong, L. et al. Advancements in the treatment of non-alcoholic fatty liver disease (NAFLD). Front Endocrinol. (Lausanne) 13, 1087260 (2022).
Heeren, J. & Scheja, L. Metabolic-associated fatty liver disease and lipoprotein metabolism. Mol. Metab. 50, 101238 (2021).
Gross, B., Pawlak, M., Lefebvre, P. & Staels, B. PPARs in obesity-induced T2DM, dyslipidaemia and NAFLD. Nat. Rev. Endocrinol. 13, 36–49 (2017).
Xu, W. et al. Hepatocellular cystathionine gamma lyase/hydrogen sulfide attenuates nonalcoholic fatty liver disease by activating farnesoid X receptor. Hepatology 76, 1794–1810 (2022).
Yu, Y., Ye, S. M., Liu, D. Y. & Yang, L. Q. AP39 ameliorates high fat diet-induced liver injury in young rats via alleviation of oxidative stress and mitochondrial impairment. Exp. Anim. 70, 553–562 (2021).
Alshawsh, M. A. et al. A comparison of the gene expression profiles of non-alcoholic fatty liver disease between animal models of a high-fat diet and methionine-choline-deficient diet. Molecules. 27, 858 (2022).
Wang, Q. et al. Naringenin attenuates non-alcoholic fatty liver disease by down-regulating the NLRP3/NF-kappaB pathway in mice. Br. J. Pharm. 177, 1806–1821 (2020).
Park, H. S. et al. TXNIP/VDUP1 attenuates steatohepatitis via autophagy and fatty acid oxidation. Autophagy 17, 2549–2564 (2021).
Balkrishna, A. et al. Livogrit prevents methionine-cystine deficiency induced nonalcoholic steatohepatitis by modulation of steatosis and oxidative stress in human hepatocyte-derived spheroid and in primary rat hepatocytes. Bioengineered 13, 10811–10826 (2022).
Lu, S. C. & Mato, J. M. S-adenosylmethionine in liver health, injury, and cancer. Physiol. Rev. 92, 1515–1542 (2012).
Pascale, R. M. et al. S-Adenosylmethionine: from the discovery of its inhibition of tumorigenesis to its use as a therapeutic agent. Cells. 11, 409 (2022).
Lu, S. C. et al. Methionine adenosyltransferase 1A knockout mice are predisposed to liver injury and exhibit increased expression of genes involved in proliferation. Proc. Natl Acad. Sci. USA 98, 5560–5565 (2001).
Asrani, S. K., Devarbhavi, H., Eaton, J. & Kamath, P. S. Burden of liver diseases in the world. J. Hepatol. 70, 151–171 (2019).
Rodriguez, M. J. et al. Maresin-1 prevents liver fibrosis by targeting Nrf2 and NF-kappaB, reducing oxidative stress and inflammation. Cells. 10, 3406 (2021).
Aljobaily, N. et al. Creatine alleviates doxorubicin-induced liver aamage by inhibiting liver fibrosis, inflammation, oxidative stress, and cellular senescence. Nutrients. 13, 41 (2020).
Tripathi, M. et al. Vitamin B(12) and folate decrease inflammation and fibrosis in NASH by preventing syntaxin 17 homocysteinylation. J. Hepatol. 77, 1246–1255 (2022).
Mohammadian, Z. et al. Effects of folic acid on dyslipidemia and serum homocysteine in a rat model of cholestasis and hepatic fibrosis. Pol. J. Pathol. 66, 49–56 (2015).
Fiorucci, S., Distrutti, E., Cirino, G. & Wallace, J. L. The emerging roles of hydrogen sulfide in the gastrointestinal tract and liver. Gastroenterology 131, 259–271 (2006).
Zhao, S. et al. Hydrogen sulfide alleviates liver injury through the S-sulfhydrated-kelch-like ECH-associated protein 1/Nuclear erythroid 2-related factor 2/low-density lipoprotein receptor-related protein 1 pathway. Hepatology 73, 282–302 (2021).
Gong, Z. et al. S-allyl-cysteine attenuates carbon tetrachloride-induced liver fibrosis in rats by targeting STAT3/SMAD3 pathway. Am. J. Transl. Res. 10, 1337–1346 (2018).
Peng, X. et al. Resveratrol improves synaptic plasticity in hypoxic-ischemic brain injury in neonatal mice via alleviating SIRT1/NF-kappaB signaling-mediated neuroinflammation. J. Mol. Neurosci. 72, 113–125 (2022).
Barks, J. D. E., Liu, Y., Dopp, I. A. & Silverstein, F. S. Azithromycin reduces inflammation-amplified hypoxic-ischemic brain injury in neonatal rats. Pediatr. Res. 92, 415–423 (2022).
Xu, X. et al. Irisin prevents hypoxic-ischemic brain damage in rats by inhibiting oxidative stress and protecting the blood-brain barrier. Peptides 161, 170945 (2023).
Liu, Y. et al. Downregulation of nitric oxide by electroacupuncture against hypoxic‑ischemic brain damage in rats via nuclear factor‑kappaB/neuronal nitric oxide synthase. Mol. Med. Rep. 11, 837–842 (2015).
Tagliari, B. et al. Hyperhomocysteinemia increases damage on brain slices exposed to in vitro model of oxygen and glucose deprivation: prevention by folic acid. Int J. Dev. Neurosci. 24, 285–291 (2006).
Fogal, B. et al. System x(c)- activity and astrocytes are necessary for interleukin-1 beta-mediated hypoxic neuronal injury. J. Neurosci. 27, 10094–10105 (2007).
Liu, C. Y. et al. The role of cystathionine-beta-synthase, H(2)S, and miRNA-377 in hypoxic-ischemic encephalopathy: insights from human and animal studies. J. Mol. Neurosci. 73, 921–931 (2023).
Xin, D. et al. l-Cysteine suppresses hypoxia-ischemia injury in neonatal mice by reducing glial activation, promoting autophagic flux and mediating synaptic modification via H(2)S formation. Brain Behav. Immun. 73, 222–234 (2018).
Yuan, Q. et al. Anti-cerebral ischemia reperfusion injury of polysaccharides: A review of the mechanisms. Biomed. Pharmacother. 137, 111303 (2021).
Xu, D. et al. Orexin-A alleviates astrocytic apoptosis and inflammation via inhibiting OX1R-mediated NF-kappaB and MAPK signaling pathways in cerebral ischemia/reperfusion injury. Biochim Biophys. Acta Mol. Basis Dis. 1867, 166230 (2021).
Zhu, K. et al. Inhibition of TLR4 prevents hippocampal hypoxic-ischemic injury by regulating ferroptosis in neonatal rats. Exp. Neurol. 345, 113828 (2021).
Rao, A. M. et al. Beneficial effects of S-adenosyl-L-methionine on blood-brain barrier breakdown and neuronal survival after transient cerebral ischemia in gerbils. Brain Res. Mol. Brain Res. 44, 134–138 (1997).
Zhao, Y. et al. Homocysteine aggravates cortical neural cell injury through neuronal autophagy overactivation following rat cerebral ischemia-reperfusion. Int. J. Mol. Sci. 17, 1196 (2016).
Petras, M. et al. Effect of hyperhomocysteinemia on redox balance and redox defence enzymes in ischemia-reperfusion injury and/or after ischemic preconditioning in rats. Cell Mol. Neurobiol. 37, 1417–1431 (2017).
Villalobos, M. A. et al. Effect of S-adenosyl-L-methionine on rat brain oxidative stress damage in a combined model of permanent focal ischemia and global ischemia-reperfusion. Brain Res. 883, 31–40 (2000).
Deng, G. et al. Protective effect of hydrogen sulfide on cerebral ischemia-reperfusion injury. Cell Mol. Neurobiol. 43, 15–25 (2023).
Jiang, W. W. et al. Sodium hydrosulfide attenuates cerebral ischemia/reperfusion injury by suppressing overactivated autophagy in rats. FEBS Open Bio. 7, 1686–1695 (2017).
Ji, K., Xue, L., Cheng, J. & Bai, Y. Preconditioning of H2S inhalation protects against cerebral ischemia/reperfusion injury by induction of HSP70 through PI3K/Akt/Nrf2 pathway. Brain Res. Bull. 121, 68–74 (2016).
Zhang, Y. et al. CSE-derived H(2)S inhibits reactive astrocytes proliferation and promotes neural functional recovery after cerebral ischemia/reperfusion injury in mice via inhibition of RhoA/ROCK(2) pathway. ACS Chem. Neurosci. 12, 2580–2590 (2021).
Zhang, X. & Bian, J. S. Hydrogen sulfide: a neuromodulator and neuroprotectant in the central nervous system. ACS Chem. Neurosci. 5, 876–883 (2014).
Wang, Z. et al. L-Cysteine promotes the proliferation and differentiation of neural stem cells via the CBS/H(2)S pathway. Neuroscience 237, 106–117 (2013).
Sun, X. Y. et al. Rutin prevents tau pathology and neuroinflammation in a mouse model of Alzheimer’s disease. J. Neuroinflamm. 18, 131 (2021).
Congdon, E. E. & Sigurdsson, E. M. Tau-targeting therapies for Alzheimer disease. Nat. Rev. Neurol. 14, 399–415 (2018).
Muraoka, S. et al. Proteomic and biological profiling of extracellular vesicles from Alzheimer’s disease human brain tissues. Alzheimers Dement. 16, 896–907 (2020).
Zhao, X. et al. A microtubule stabilizer ameliorates protein pathogenesis and neurodegeneration in mouse models of repetitive traumatic brain injury. Sci. Transl. Med. 15, eabo6889 (2023).
Hadar, A. et al. Introducing ADNP and SIRT1 as new partners regulating microtubules and histone methylation. Mol. Psychiatry 26, 6550–6561 (2021).
Giovinazzo, D. et al. Hydrogen sulfide is neuroprotective in Alzheimer’s disease by sulfhydrating GSK3beta and inhibiting Tau hyperphosphorylation. Proc. Natl Acad. Sci. USA. 118, e2017225118 (2021).
Linnebank, M. et al. S-adenosylmethionine is decreased in the cerebrospinal fluid of patients with Alzheimer’s disease. Neurodegener. Dis. 7, 373–378 (2010).
Morrison, L. D., Smith, D. D. & Kish, S. J. Brain S-adenosylmethionine levels are severely decreased in Alzheimer’s disease. J. Neurochem. 67, 1328–1331 (1996).
Chen, H. et al. Folic acid supplementation mitigates alzheimer’s disease by reducing inflammation: a randomized controlled trial. Mediators Inflamm. 2016, 5912146 (2016).
Zhu, B., Yin, D., Zhao, H. & Zhang, L. The immunology of Parkinson’s disease. Semin Immunopathol. 44, 659–672 (2022).
Kikuchi, T. et al. Human iPS cell-derived dopaminergic neurons function in a primate Parkinson’s disease model. Nature 548, 592–596 (2017).
Zheng, X. et al. Human iPSC-derived midbrain organoids functionally integrate into striatum circuits and restore motor function in a mouse model of Parkinson’s disease. Theranostics 13, 2673–2692 (2023).
Liu, Y. et al. Involvement of microRNA-135a-5p in the protective effects of hydrogen sulfide against Parkinson’s Disease. Cell Physiol. Biochem. 40, 18–26 (2016).
Kida, K. et al. Inhaled hydrogen sulfide prevents neurodegeneration and movement disorder in a mouse model of Parkinson’s disease. Antioxid. Redox Signal 15, 343–352 (2011).
A novel gene containing a trinucleotide repeat that is expanded and unstable on Huntington’s disease chromosomes. The huntington’s disease collaborative research group. Cell 72, 971–983 (1993).
Zsindely, N., Siagi, F. & Bodai, L. DNA methylation in huntington’s diseas. Int. J. Mol. Sci. 22, 12736 (2021).
Cha, J. H. Transcriptional signatures in Huntington’s disease. Prog. Neurobiol. 83, 228–248 (2007).
Sbodio, J. I., Snyder, S. H. & Paul, B. D. Transcriptional control of amino acid homeostasis is disrupted in Huntington’s disease. Proc. Natl Acad. Sci. USA 113, 8843–8848 (2016).
Paul, B. D. & Snyder, S. H. Impaired redox signaling in Huntington’s disease: therapeutic implications. Front Mol. Neurosci. 12, 68 (2019).
Perluigi, M. et al. Proteomic analysis of protein expression and oxidative modification in r6/2 transgenic mice: a model of Huntington disease. Mol. Cell Proteom. 4, 1849–1861 (2005).
Maiuri, T. et al. DNA repair in Huntington’s disease and spinocerebellar ataxias: somatic instability and alternative hypotheses. J. Huntingt. Dis. 10, 165–173 (2021).
Oh, Y. M. et al. Age-related Huntington’s disease progression modeled in directly reprogrammed patient-derived striatal neurons highlights impaired autophagy. Nat. Neurosci. 25, 1420–1433 (2022).
Jones, L., Wheeler, V. C. & Pearson, C. E. Special issue: DNA repair and somatic repeat expansion in Huntington’s disease. J. Huntingt. Dis. 10, 3–5 (2021).
Tabassum, R., Jeong, N. Y. & Jung, J. Therapeutic importance of hydrogen sulfide in age-associated neurodegenerative diseases. Neural Regen. Res. 15, 653–662 (2020).
Paul, B. D. et al. Cystathionine gamma-lyase deficiency mediates neurodegeneration in Huntington’s disease. Nature 509, 96–100 (2014).
Andrich, J. et al. Hyperhomocysteinaemia in treated patients with Huntington’s disease homocysteine in HD. Mov. Disord. 19, 226–228 (2004).
Zoccolella, S. et al. Elevated plasma homocysteine levels in patients with amyotrophic lateral sclerosis. Neurology 70, 222–225 (2008).
Hardiman, O. et al. Amyotrophic lateral sclerosis. Nat. Rev. Dis. Prim. 3, 17085 (2017).
Tabassum, R. & Jeong, N. Y. Potential for therapeutic use of hydrogen sulfide in oxidative stress-induced neurodegenerative diseases. Int J. Med. Sci. 16, 1386–1396 (2019).
Suchy, J., Lee, S., Ahmed, A. & Shea, T. B. Dietary supplementation with S-adenosyl methionine delays the onset of motor neuron pathology in a murine model of amyotrophic lateral sclerosis. Neuromol. Med. 12, 86–97 (2010).
Yamout, B. I. & Alroughani, R. Multiple Sclerosis. Semin Neurol. 38, 212–225 (2018).
Tollar, J. et al. Exercise effects on multiple sclerosis quality of life and clinical-motor symptoms. Med Sci. Sports Exerc. 52, 1007–1014 (2020).
Karussis, D. The diagnosis of multiple sclerosis and the various related demyelinating syndromes: a critical review. J. Autoimmun. 48–49, 134–142 (2014).
Bystricka, Z., Laubertova, L., Durfinova, M. & Paduchova, Z. Methionine metabolism and multiple sclerosis. Biomarkers 22, 747–754 (2017).
Russo, C. et al. Hyperhomocysteinemia is associated with cognitive impairment in multiple sclerosis. J. Neurol. 255, 64–69 (2008).
Sahin, S. et al. Increased plasma homocysteine levels in multiple sclerosis. Mult. Scler. 13, 945–946 (2007).
Ghaiad, H. R. et al. Modulating miR-146a expression by hydrogen sulfide ameliorates motor dysfunction and axonal demyelination in cuprizone-induced multiple sclerosis. ACS Chem. Neurosci. 14, 3047–3058 (2023).
Lazarevic, M. et al. Upregulation of tolerogenic pathways by the hydrogen sulfide donor GYY4137 and impaired expression of H(2)S-producing enzymes in multiple sclerosis. Antioxidants (Basel). 9, 608 (2020).
Li, M., Mao, J. C. & Zhu, Y. Z. Hydrogen sulfide: a novel immunoinflammatory regulator in rheumatoid arthritis. Adv. Exp. Med. Biol. 1315, 161–179 (2021).
Seki, T. et al. d-Cysteine promotes dendritic development in primary cultured cerebellar Purkinje cells via hydrogen sulfide production. Mol. Cell Neurosci. 93, 36–47 (2018).
Zhu, X. Y., Gu, H. & Ni, X. Hydrogen sulfide in the endocrine and reproductive systems. Expert Rev. Clin. Pharm. 4, 75–82 (2011).
Hine, C., Zhu, Y., Hollenberg, A. N. & Mitchell, J. R. Dietary and endocrine regulation of endogenous hydrogen sulfide production: implications for longevity. Antioxid. Redox. Signal 28, 1483–1502 (2018).
Wu, L. et al. Pancreatic islet overproduction of H2S and suppressed insulin release in Zucker diabetic rats. Lab. Invest. 89, 59–67 (2009).
Bao, L., Vlcek, C., Paces, V. & Kraus, J. P. Identification and tissue distribution of human cystathionine beta-synthase mRNA isoforms. Arch. Biochem. Biophys. 350, 95–103 (1998).
Nagahara, N. Multiple role of 3-mercaptopyruvate sulfurtransferase: antioxidative function, H(2) S and polysulfide production and possible SO(x) production. Br. J. Pharm. 175, 577–589 (2018).
Suzuki, K. et al. Clinical implication of plasma hydrogen sulfide levels in japanese patients with type 2 diabetes. Intern. Med. 56, 17–21 (2017).
Dutta, M. et al. Evaluation of plasma H2S levels and H2S synthesis in streptozotocin induced Type-2 diabetes-an experimental study based on Swietenia macrophylla seeds. Asian Pac. J. Trop. Biomed. 4, S483–S487 (2014).
Zhou, X., An, G. & Lu, X. Hydrogen sulfide attenuates the development of diabetic cardiomyopathy. Clin. Sci. (Lond.) 128, 325–335 (2015).
Mursleen, M. T. & Riaz, S. Implication of homocysteine in diabetes and impact of folate and vitamin B12 in diabetic population. Diab. Metab. Syndr. 11, S141–S146 (2017).
Fotiou, P. et al. Vitamin status as a determinant of serum homocysteine concentration in type 2 diabetic retinopathy. J. Diab. Res. 2014, 807209 (2014).
Luo, W. M. et al. The association of homocysteine and diabetic retinopathy in homocysteine cycle in chinese patients with type 2 diabetes. Front Endocrinol. (Lausanne) 13, 883845 (2022).
Tuttle, K. R. et al. Molecular mechanisms and therapeutic targets for diabetic kidney disease. Kidney Int. 102, 248–260 (2022).
Barrera-Chimal, J., Lima-Posada, I., Bakris, G. L. & Jaisser, F. Mineralocorticoid receptor antagonists in diabetic kidney disease - mechanistic and therapeutic effects. Nat. Rev. Nephrol. 18, 56–70 (2022).
Pereira, P. R. et al. Metabolomics as a tool for the early diagnosis and prognosis of diabetic kidney disease. Med. Res. Rev. 42, 1518–1544 (2022).
Poirier, L. A. et al. Blood S-adenosylmethionine concentrations and lymphocyte methylenetetrahydrofolate reductase activity in diabetes mellitus and diabetic nephropathy. Metabolism 50, 1014–1018 (2001).
Liu, X. Q. et al. Carnosine alleviates diabetic nephropathy by targeting GNMT, a key enzyme mediating renal inflammation and fibrosis. Clin. Sci. (Lond.) 134, 3175–3193 (2020).
Hussain Lodhi, A., Ahmad, F. U., Furwa, K. & Madni, A. Role of oxidative stress and reduced endogenous hydrogen sulfide in diabetic nephropathy. Drug Des. Devel Ther. 15, 1031–1043 (2021).
Kitada, M. et al. Sirtuins and renal diseases: relationship with aging and diabetic nephropathy. Clin. Sci. (Lond.) 124, 153–164 (2013).
He, W. et al. Sirt1 activation protects the mouse renal medulla from oxidative injury. J. Clin. Invest. 120, 1056–1068 (2010).
Liang, J., Tian, S., Han, J. & Xiong, P. Resveratrol as a therapeutic agent for renal fibrosis induced by unilateral ureteral obstruction. Ren. Fail 36, 285–291 (2014).
Ahmed, H. H. et al. Hydrogen sulfide modulates SIRT1 and suppresses oxidative stress in diabetic nephropathy. Mol. Cell Biochem. 457, 1–9 (2019).
Iseki, K. Parathyroid hormone and the vascular response to norepinephrine. Am. J. Hypertens. 3, 238S–240S (1990).
Caballero, B. Humans against obesity: who will win? Adv. Nutr. 10, S4–S9 (2019).
Pulgaron, E. R. & Delamater, A. M. Obesity and type 2 diabetes in children: epidemiology and treatment. Curr. Diab Rep. 14, 508 (2014).
Malone, J. I. & Hansen, B. C. Does obesity cause type 2 diabetes mellitus (T2DM)? Or is it the opposite? Pediatr. Diab. 20, 5–9 (2019).
Elshorbagy, A. K., Smith, A. D., Kozich, V. & Refsum, H. Cysteine and obesity. Obes. (Silver Spring) 20, 473–481 (2012).
Elshorbagy, A. K. et al. Cysteine supplementation reverses methionine restriction effects on rat adiposity: significance of stearoyl-coenzyme A desaturase. J. Lipid Res. 52, 104–112 (2011).
McGavigan, A. K. et al. L-cysteine suppresses ghrelin and reduces appetite in rodents and humans. Int. J. Obes. (Lond.) 39, 447–455 (2015).
Whiteman, M. et al. Adiposity is a major determinant of plasma levels of the novel vasodilator hydrogen sulphide. Diabetologia 53, 1722–1726 (2010).
Tsai, C. Y. et al. Hydrogen sulfide promotes adipogenesis in 3T3L1 cells. PLoS ONE 10, e0119511 (2015).
Mani, S., Yang, G. & Wang, R. A critical life-supporting role for cystathionine gamma-lyase in the absence of dietary cysteine supply. Free Radic. Biol. Med. 50, 1280–1287 (2011).
Gupta, S. & Kruger, W. D. Cystathionine beta-synthase deficiency causes fat loss in mice. PLoS One 6, e27598 (2011).
Geng, B. et al. Increase or decrease hydrogen sulfide exert opposite lipolysis, but reduce global insulin resistance in high fatty diet induced obese mice. PLoS ONE 8, e73892 (2013).
Beltowski, J. & Jamroz-Wisniewska, A. Hydrogen sulfide in the adipose tissue-physiology, pathology and a target for pharmacotherapy. Molecules. 22, 63 (2016).
Nohara, T. et al. Antitumor allium sulfides. Chem. Pharm. Bull. (Tokyo) 65, 209–217 (2017).
Khattak, S. et al. Hydrogen sulfide biology and its role in cancer. Molecules. 27, 3389 (2022).
Majumder, A. Targeting homocysteine and hydrogen sulfide balance as future therapeutics in cancer treatment. Antioxidants (Basel). 12, (2023).
Santos, S. S. et al. Role of cystathionine beta-synthase and 3-mercaptopyruvate Sulfurtransferase in the regulation of proliferation, migration, and bioenergetics of murine breast cancer cells. Antioxidants (Basel). 12, 1520 (2023).
Fu, M. et al. Hydrogen sulfide (H2S) metabolism in mitochondria and its regulatory role in energy production. Proc. Natl Acad. Sci. USA 109, 2943–2948 (2012).
Blanc, V. et al. Apobec1 complementation factor overexpression promotes hepatic steatosis, fibrosis, and hepatocellular cancer. J. Clin. Invest. 131, e138699 (2021).
Zhou, T. et al. DTYMK promote hepatocellular carcinoma proliferation by regulating cell cycle. Cell Cycle 20, 1681–1691 (2021).
Zhu, H. et al. CCAT1 promotes hepatocellular carcinoma cell proliferation and invasion. Int. J. Clin. Exp. Pathol. 8, 5427–5434 (2015).
Wu, D. et al. Hydrogen sulfide acts as a double-edged sword in human hepatocellular carcinoma cells through EGFR/ERK/MMP-2 and PTEN/AKT signaling pathways. Sci. Rep. 7, 5134 (2017).
Wang, S. S. et al. Hydrogen sulfide promotes autophagy of hepatocellular carcinoma cells through the PI3K/Akt/mTOR signaling pathway. Cell Death Dis. 8, e2688 (2017).
Zhen, Y. et al. Exogenous hydrogen sulfide promotes hepatocellular carcinoma cell growth by activating the STAT3-COX-2 signaling pathway. Oncol. Lett. 15, 6562–6570 (2018).
Lozano-Rosas, M. G. et al. Diminished S-adenosylmethionine biosynthesis and its metabolism in a model of hepatocellular carcinoma is recuperated by an adenosine derivative. Cancer Biol. Ther. 21, 81–94 (2020).
Gou, D. et al. Gluconeogenic enzyme PCK1 supports S-adenosylmethionine biosynthesis and promotes H3K9me3 modification to suppress hepatocellular carcinoma progression. J. Clin. Invest. 133, e161713 (2023).
Wang, T. et al. Disulfidptosis classification of hepatocellular carcinoma reveals correlation with clinical prognosis and immune profile. Int. Immunopharmacol. 120, 110368 (2023).
Mahmood, N. et al. S-adenosylmethionine in combination with decitabine shows enhanced anti-cancer effects in repressing breast cancer growth and metastasis. J. Cell Mol. Med. 24, 10322–10337 (2020).
Cave, D. D. et al. S-Adenosylmethionine-mediated apoptosis is potentiated by autophagy inhibition induced by chloroquine in human breast cancer cells. J. Cell Physiol. 233, 1370–1383 (2018).
Akilzhanova, A. et al. Genetic profile and determinants of homocysteine levels in Kazakhstan patients with breast cancer. Anticancer Res. 33, 4049–4059 (2013).
Lin, J. et al. Plasma homocysteine and cysteine and risk of breast cancer in women. Cancer Res 70, 2397–2405 (2010).
Khan, N. H. et al. pharmacological inhibition of endogenous hydrogen sulfide attenuates breast cancer progression. Molecules. 27, 4049 (2022).
Deepak, K. G. K. et al. Tumor microenvironment: challenges and opportunities in targeting metastasis of triple negative breast cancer. Pharm. Res. 153, 104683 (2020).
Lev, S. Targeted therapy and drug resistance in triple-negative breast cancer: the EGFR axis. Biochem. Soc. Trans. 48, 657–665 (2020).
Leon-Ferre, R. A. & Goetz, M. P. Advances in systemic therapies for triple negative breast cancer. BMJ 381, e071674 (2023).
Liu, Y. et al. A novel cystathionine gamma-lyase inhibitor, I194496, inhibits the growth and metastasis of human TNBC via downregulating multiple signaling pathways. Sci. Rep. 11, 8963 (2021).
Liu, Y. et al. Antimetastatic therapies of the polysulfide diallyl trisulfide against triple-negative breast cancer (TNBC) via suppressing MMP2/9 by blocking NF-kappaB and ERK/MAPK signaling pathways. PLoS ONE 10, e0123781 (2015).
Huang, J. et al. Diallyl disulfide inhibits growth and metastatic potential of human triple-negative breast cancer cells through inactivation of the beta-catenin signaling pathway. Mol. Nutr. Food Res. 59, 1063–1075 (2015).
Ferroni, P. et al. Determinants of homocysteine levels in colorectal and breast cancer patients. Anticancer Res 29, 4131–4138 (2009).
Akoglu, B., Milovic, V., Caspary, W. F. & Faust, D. Hyperproliferation of homocysteine-treated colon cancer cells is reversed by folate and 5-methyltetrahydrofolate. Eur. J. Nutr. 43, 93–99 (2004).
Wang, L. et al. PCSK9 promotes the progression and metastasis of colon cancer cells through regulation of EMT and PI3K/AKT signaling in tumor cells and phenotypic polarization of macrophages. J. Exp. Clin. Cancer Res. 41, 303 (2022).
Stehr, A. M. et al. Neutrophil extracellular traps drive epithelial-mesenchymal transition of human colon cancer. J. Pathol. 256, 455–467 (2022).
Mao, L. et al. Decorin deficiency promotes epithelial-mesenchymal transition and colon cancer metastasis. Matrix Biol. 95, 1–14 (2021).
Sun, L. et al. Wnt/beta-catenin signalling, epithelial-mesenchymal transition and crosslink signalling in colorectal cancer cells. Biomed. Pharmacother. 175, 116685 (2024).
Peng, C. et al. Norcantharidin suppresses colon cancer cell epithelial-mesenchymal transition by inhibiting the alphavbeta6-ERK-Ets1 signaling pathway. Sci. Rep. 6, 20500 (2016).
Pavlic, A. et al. Epithelial-mesenchymal transition in colorectal carcinoma: comparison between primary tumor, lymph node and liver metastases. Front Oncol. 11, 662806 (2021).
Ascencao, K. et al. Pharmacological induction of mesenchymal-epithelial transition via inhibition of H2S biosynthesis and consequent suppression of ACLY activity in colon cancer cells. Pharm. Res. 165, 105393 (2021).
Wen, J. et al. ACLY facilitates colon cancer cell metastasis by CTNNB1. J. Exp. Clin. Cancer Res. 38, 401 (2019).
Hu, G. et al. A bioinformatics approach to identify a disulfidptosis-related gene signature for prognostic implication in colon adenocarcinoma. Sci. Rep. 13, 12403 (2023).
Untereiner, A. A. et al. H(2)S-induced S-sulfhydration of lactate dehydrogenase a (LDHA) stimulates cellular bioenergetics in HCT116 colon cancer cells. Biochem. Pharm. 136, 86–98 (2017).
Zhang, Y. et al. Overexpression of CBS/H(2)S inhibits proliferation and metastasis of colon cancer cells through downregulation of CD44. Cancer Cell Int. 22, 85 (2022).
Hellmich, M. R., Coletta, C., Chao, C. & Szabo, C. The therapeutic potential of cystathionine beta-synthetase/hydrogen sulfide inhibition in cancer. Antioxid. Redox Signal 22, 424–448 (2015).
Zheng, M. Classification and pathology of lung cancer. Surg. Oncol. Clin. N. Am. 25, 447–468 (2016).
Ruiz-Cordero, R. & Devine, W. P. Targeted therapy and checkpoint immunotherapy in lung cancer. Surg. Pathol. Clin. 13, 17–33 (2020).
Vokes, N. I. et al. Concurrent TP53 mutations facilitate resistance evolution in EGFR-mutant lung adenocarcinoma. J. Thorac. Oncol. 17, 779–792 (2022).
Huang, J. et al. Identification of a disulfidptosis-related genes signature for prognostic implication in lung adenocarcinoma. Comput Biol. Med. 165, 107402 (2023).
Greenberg, A. K. et al. S-adenosylmethionine as a biomarker for the early detection of lung cancer. Chest 132, 1247–1252 (2007).
Wang, M. et al. Hydrogen sulfide modulates epithelial-mesenchymal transition and angiogenesis in non-small cell lung cancer via HIF-1alpha activation. Biochem. Pharm. 172, 113775 (2020).
Vincent, A. et al. Pancreatic cancer. Lancet 378, 607–620 (2011).
Ren, B. et al. Tumor microenvironment participates in metastasis of pancreatic cancer. Mol. Cancer 17, 108 (2018).
Wang, S., You, L., Dai, M. & Zhao, Y. Mucins in pancreatic cancer: a well-established but promising family for diagnosis, prognosis and therapy. J. Cell Mol. Med. 24, 10279–10289 (2020).
Citi, V. et al. Anticancer properties of erucin, an H(2) S-releasing isothiocyanate, on human pancreatic adenocarcinoma cells (AsPC-1). Phytother. Res. 33, 845–855 (2019).
Chen, X. et al. Activation of Nrf2 by sulforaphane inhibits high glucose-induced progression of pancreatic cancer via AMPK dependent signaling. Cell Physiol. Biochem. 50, 1201–1215 (2018).
Montenegro, M. F. et al. Targeting protein methylation in pancreatic cancer cells results in KRAS signaling imbalance and inhibition of autophagy. Cell Death Dis. 14, 761 (2023).
Yang, P. W. et al. Keep a watchful eye on methionine adenosyltransferases, novel therapeutic opportunities for hepatobiliary and pancreatic tumours. Biochim. Biophys. Acta Rev. Cancer 1877, 188793 (2022).
Kossai, M., Leary, A., Scoazec, J. Y. & Genestie, C. Ovarian cancer: a heterogeneous disease. Pathobiology 85, 41–49 (2018).
O’Shea, A. S. Clinical staging of ovarian cancer. Methods Mol. Biol. 2424, 3–10 (2022).
Jiang, Y., Wang, C. & Zhou, S. Targeting tumor microenvironment in ovarian cancer: Premise and promise. Biochim Biophys. Acta Rev. Cancer 1873, 188361 (2020).
Jin, M., Ni, D., Cai, J. & Yang, J. Identification and validation of immunity- and disulfidptosis-related genes signature for predicting prognosis in ovarian cancer. Heliyon 10, e32273 (2024).
Zhu, H. et al. Cystathionine beta-synthase in physiology and cancer. Biomed. Res. Int. 2018, 3205125 (2018).
Bhattacharyya, S. et al. Cystathionine beta-synthase (CBS) contributes to advanced ovarian cancer progression and drug resistance. PLoS ONE 8, e79167 (2013).
Chakraborty, P. K. et al. Role of cystathionine beta synthase in lipid metabolism in ovarian cancer. Oncotarget 6, 37367–37384 (2015).
Siegel, R. L., Miller, K. D. & Jemal, A. Cancer statistics, 2015. CA. Cancer J. Clin. 65, 5–29 (2015).
Litwin, M. S. & Tan, H. J. The diagnosis and treatment of prostate cancer: a review. JAMA 317, 2532–2542 (2017).
Preisser, F. et al. Intermediate-risk prostate cancer: stratification and management. Eur. Urol. Oncol. 3, 270–280 (2020).
Wang, Y. H. et al. Dysregulation of cystathionine gamma-lyase promotes prostate cancer progression and metastasis. EMBO Rep. 20, e45986 (2019).
Schmidt, T. S-Adenosylmethionine affects ERK1/2 and STAT3 pathway in androgen-independent prostate cancer cells. Mol. Biol. Rep. 49, 4805–4817 (2022).
Bracken, A. P. et al. EZH2 is downstream of the pRB-E2F pathway, essential for proliferation and amplified in cancer. EMBO J. 22, 5323–5335 (2003).
Varambally, S. et al. The polycomb group protein EZH2 is involved in progression of prostate cancer. Nature 419, 624–629 (2002).
Uchiyama, N., Tanaka, Y. & Kawamoto, T. Aristeromycin and DZNeP cause growth inhibition of prostate cancer via induction of mir-26a. Eur. J. Pharm. 812, 138–146 (2017).
Francis, R. C. et al. Protective and detrimental effects of sodium sulfide and hydrogen sulfide in murine ventilator-induced lung injury. Anesthesiology 115, 1012–1021 (2011).
Li, L. et al. Characterization of a novel, water-soluble hydrogen sulfide-releasing molecule (GYY4137): new insights into the biology of hydrogen sulfide. Circulation 117, 2351–2360 (2008).
Wang, Y. et al. Hydrogen sulfide alleviates particulate matter-induced emphysema and airway inflammation by suppressing ferroptosis. Free Radic. Biol. Med. 186, 1–16 (2022).
Wang, M. et al. Exogenous H(2)S initiating Nrf2/GPx4/GSH pathway through promoting Syvn1-Keap1 interaction in diabetic hearts. Cell Death Discov. 9, 394 (2023).
Kupai, K. et al. H(2)S confers colonoprotection against TNBS-induced colitis by HO-1 upregulation in rats. Inflammopharmacology 26, 479–489 (2018).
Torok, S. et al. Protective effects of H(2)S donor treatment in experimental colitis: a focus on antioxidants. Antioxidants (Basel). 12, 1025 (2023).
Lucetti, L. T. et al. Nitric oxide and hydrogen sulfide interact when modulating gastric physiological functions in rodents. Dig. Dis. Sci. 62, 93–104 (2017).
Nicolau, L. A. et al. The hydrogen sulfide donor, Lawesson’s reagent, prevents alendronate-induced gastric damage in rats. Braz. J. Med Biol. Res. 46, 708–714 (2013).
Star, B. S. et al. GYY4137-derived hydrogen sulfide donates electrons to the mitochondrial electron transport chain via sulfide: quinone oxidoreductase in endothelial cells. Antioxidants (Basel). 12, 587 (2023).
Hasegawa, U. & van der Vlies, A. J. Design and synthesis of polymeric hydrogen sulfide donors. Bioconjug. Chem. 25, 1290–1300 (2014).
Cai, F. F. et al. ADT-OH inhibits malignant melanoma metastasis in mice via suppressing CSE/CBS and FAK/Paxillin signaling pathway. Acta Pharm. Sin. 43, 1829–1842 (2022).
Dong, Q. et al. A novel hydrogen sulfide-releasing donor, HA-ADT, suppresses the growth of human breast cancer cells through inhibiting the PI3K/AKT/mTOR and Ras/Raf/MEK/ERK signaling pathways. Cancer Lett. 455, 60–72 (2019).
Montanaro, R. et al. Hydrogen sulfide donor AP123 restores endothelial nitric oxide-dependent vascular function in hyperglycemia via a CREB-dependent pathway. Redox Biol. 62, 102657 (2023).
Lohakul, J. et al. Mitochondria-targeted hydrogen sulfide delivery molecules protect against UVA-induced photoaging in human dermal fibroblasts, and in mouse skin in vivo. Antioxid. Redox Signal 36, 1268–1288 (2022).
De Cicco, P. et al. ATB-346, a novel hydrogen sulfide-releasing anti-inflammatory drug, induces apoptosis of human melanoma cells and inhibits melanoma development in vivo. Pharm. Res. 114, 67–73 (2016).
Van Dingenen, J., Pieters, L., Vral, A. & Lefebvre, R. A. The H(2)S-releasing naproxen derivative ATB-346 and the slow-release H(2)S donor GYY4137 reduce intestinal inflammation and restore transit in postoperative ileuss. Front Pharm. 10, 116 (2019).
Dzielska-Olczak, M. Cyclooxygenases inhibitors and other compounds with antiinflammatory potential in osteoarthrosis–part II. Pol. Merkur Lekarski 30, 82–86 (2011).
Amagase, H. Clarifying the real bioactive constituents of garlic. J. Nutr. 136, 716S–725S (2006).
Benavides, G. A. et al. Hydrogen sulfide mediates the vasoactivity of garlic. Proc. Natl Acad. Sci. USA 104, 17977–17982 (2007).
Jeremic, J. N. et al. Garlic derived diallyl trisulfide in experimental metabolic syndrome: metabolic effects and cardioprotective Role. Int. J. Mol. Sci. 21, 9100 (2020).
Gojon, G. & Morales, G. A. SG1002 and catenated divalent organic sulfur compounds as promising hydrogen sulfide prodrugs. Antioxid. Redox Signal 33, 1010–1045 (2020).
Islam, R. K. et al. H(2)S prodrug, SG-1002, protects against myocardial oxidative damage and hypertrophy in vitro via induction of cystathionine beta-synthase and antioxidant proteins. Biomedicines. 11, 612 (2023).
Polhemus, D. J. et al. A novel hydrogen sulfide prodrug, SG1002, promotes hydrogen sulfide and nitric oxide bioavailability in heart failure patients. Cardiovasc. Ther. 33, 216–226 (2015).
Kondo, K. et al. H(2)S protects against pressure overload-induced heart failure via upregulation of endothelial nitric oxide synthase. Circulation 127, 1116–1127 (2013).
Sonobe, T. & Haouzi, P. H2S concentrations in the heart after acute H2S administration: methodological and physiological considerations. Am. J. Physiol. Heart Circ. Physiol. 311, H1445–H1458 (2016).
Balan, H., Popescu, E. & Angelescu, G. Comparing different treatment schedules of Zomen (zofenopril). Rom. J. Intern. Med. 49, 75–84 (2011).
Macabrey, D. et al. Hydrogen sulphide release via the angiotensin converting enzyme inhibitor zofenopril prevents intimal hyperplasia in human vein segments and in a mouse model of carotid artery stenosis. Eur. J. Vasc. Endovasc. Surg. 63, 336–346 (2022).
Donnarumma, E. et al. Zofenopril protects against myocardial ischemia-reperfusion injury by increasing nitric oxide and hydrogen sulfide bioavailability. J. Am. Heart Assoc. 5, e003531 (2016).
Pedre, B., Barayeu, U., Ezerina, D. & Dick, T. P. The mechanism of action of N-acetylcysteine (NAC): The emerging role of H(2)S and sulfane sulfur species. Pharm. Ther. 228, 107916 (2021).
Buhimschi, C. S. et al. Antenatal N-acetylcysteine to improve outcomes of premature infants with intra-amniotic infection and inflammation (Triple I): randomized clinical trial. Pediatr. Res. 89, 175–184 (2021).
Tsikas, D. et al. S-Nitroso-N-acetyl-L-cysteine ethyl ester (SNACET) and N-acetyl-L-cysteine ethyl ester (NACET)-Cysteine-based drug candidates with unique pharmacological profiles for oral use as NO, H(2)S and GSH suppliers and as antioxidants: results and overview. J. Pharm. Anal. 8, 1–9 (2018).
Foretz, M. et al. Metformin: from mechanisms of action to therapies. Cell Metab. 20, 953–966 (2014).
Ma, X., Jiang, Z., Wang, Z. & Zhang, Z. Administration of metformin alleviates atherosclerosis by promoting H2S production via regulating CSE expression. J. Cell Physiol. 235, 2102–2112 (2020).
Wilinski, B. et al. Metformin raises hydrogen sulfide tissue concentrations in various mouse organs. Pharm. Rep. 65, 737–742 (2013).
Wierzbicki, A. S. Atorvastatin. Expert Opin. Pharmacother. 2, 819–830 (2001).
Xu, Y. et al. Statins upregulate cystathionine gamma-lyase transcription and H2S generation via activating Akt signaling in macrophage. Pharm. Res. 87, 18–25 (2014).
Yan, L. et al. Atorvastatin protects against contrast-induced acute kidney injury via upregulation of endogenous hydrogen sulfide. Ren. Fail 42, 270–281 (2020).
Dali, M. M., Dansette, P. M., Mansuy, D. & Boucher, J. L. Comparison of various aryl-dithiolethiones and aryl-dithiolones as hydrogen sulfide donors in the presence of rat liver microsomes. Drug Metab. Dispos. 48, 426–431 (2020).
Dulac, M. et al. Mechanism of H(2)S formation from the metabolism of anetholedithiolethione and anetholedithiolone by rat liver microsomes. Drug Metab. Dispos. 47, 1061–1065 (2019).
Zhao, C. et al. Slow-release H(2)S donor anethole dithiolethione protects liver from lipotoxicity by improving fatty acid metabolism. Front Pharm. 11, 549377 (2020).
Beltowski, J. Hydrogen sulfide in pharmacology and medicine–an update. Pharm. Rep. 67, 647–658 (2015).
Liang, W. et al. Conductive hydrogen sulfide-releasing hydrogel encapsulating ADSCs for myocardial infarction treatment. ACS Appl Mater. Interfaces 11, 14619–14629 (2019).
Gero, D. et al. The novel mitochondria-targeted hydrogen sulfide (H(2)S) donors AP123 and AP39 protect against hyperglycemic injury in microvascular endothelial cells in vitro. Pharm. Res. 113, 186–198 (2016).
Sadybekov, A. V. & Katritch, V. Computational approaches streamlining drug discovery. Nature 616, 673–685 (2023).
Macalino, S. J., Gosu, V., Hong, S. & Choi, S. Role of computer-aided drug design in modern drug discovery. Arch. Pharm. Res. 38, 1686–1701 (2015).
Kumar, A. & Zhang, K. Y. Hierarchical virtual screening approaches in small molecule drug discovery. Methods 71, 26–37 (2015).
Ma, X. H. et al. In-silico approaches to multi-target drug discovery : computer aided multi-target drug design, multi-target virtual screening. Pharm. Res. 27, 739–749 (2010).
Wang, J. & Skolnik, S. Recent advances in physicochemical and ADMET profiling in drug discovery. Chem. Biodivers. 6, 1887–1899 (2009).
Vucicevic, J., Nikolic, K. & Mitchell, J. B. O. Rational drug design of antineoplastic agents using 3D-QSAR, cheminformatic, and virtual screening approaches. Curr. Med. Chem. 26, 3874–3889 (2019).
Pey, A. L., Majtan, T., Sanchez-Ruiz, J. M. & Kraus, J. P. Human cystathionine beta-synthase (CBS) contains two classes of binding sites for S-adenosylmethionine (SAM): complex regulation of CBS activity and stability by SAM. Biochem. J. 449, 109–121 (2013).
Majtan, T. et al. Active cystathionine beta-synthase can be expressed in heme-free systems in the presence of metal-substituted porphyrins or a chemical chaperone. J. Biol. Chem. 283, 34588–34595 (2008).
Zuhra, K., Augsburger, F., Majtan, T. & Szabo, C. Cystathionine-beta-synthase: molecular regulation and pharmacological inhibition. Biomolecules. 10, 697 (2020).
Majtan, T., Pey, A. L. & Kraus, J. P. Kinetic stability of cystathionine beta-synthase can be modulated by structural analogs of S-adenosylmethionine: potential approach to pharmacological chaperone therapy for homocystinuria. Biochimie 126, 6–13 (2016).
Niu, W. et al. Discovery of selective cystathionine beta-synthase inhibitors by high-throughput screening with a fluorescent thiol probe. Medchemcomm 8, 198–201 (2017).
Niu, W. N., Yadav, P. K., Adamec, J. & Banerjee, R. S-glutathionylation enhances human cystathionine beta-synthase activity under oxidative stress conditions. Antioxid. Redox Signal 22, 350–361 (2015).
Zhou, Y. et al. High-throughput tandem-microwell assay identifies inhibitors of the hydrogen sulfide signaling pathway. Chem. Commun. (Camb.) 49, 11782–11784 (2013).
Hu, Y. et al. Discovery of a bioactive inhibitor with a new scaffold for cystathionine gamma-lyase. J. Med. Chem. 62, 1677–1683 (2019).
Hanaoka, K. et al. Discovery and mechanistic characterization of selective inhibitors of H(2)S-producing enzyme: 3-mercaptopyruvate sulfurtransferase (3MST) targeting active-site cysteine persulfide. Sci. Rep. 7, 40227 (2017).
Akahoshi, N. et al. Increased urinary 3-mercaptolactate excretion and enhanced passive systemic anaphylaxis in mice lacking mercaptopyruvate sulfurtransferase, a model of mercaptolactate-cysteine disulfiduria. Int. J. Mol. Sci. 21, 818 (2020).
Alphey, M. S. et al. The crystal structure of Leishmania major 3-mercaptopyruvate sulfurtransferase. A three-domain architecture with a serine protease-like triad at the active site. J. Biol. Chem. 278, 48219–48227 (2003).
Kant, V. et al. In silico screening, molecular dynamic simulations, and in vitro activity of selected natural compounds as an inhibitor of Leishmania donovani 3-mercaptopyruvate sulfurtransferase. Parasitol. Res. 121, 2093–2109 (2022).
Katane, M. et al. Identification of novel D-amino acid oxidase inhibitors by in silico screening and their functional characterization in vitro. J. Med. Chem. 56, 1894–1907 (2013).
Katane, M. et al. Identification of novel D-aspartate oxidase inhibitors by in silico screening and their functional and structural characterization in vitro. J. Med. Chem. 58, 7328–7340 (2015).
Terry-Lorenzo, R. T. et al. Novel human D-amino acid oxidase inhibitors stabilize an active-site lid-open conformation. Biosci Rep. 34, e00133 (2014).
Jackson, M. R. et al. Discovery of a first-in-class inhibitor of sulfide:quinone oxidoreductase that protects against adverse cardiac remodelling and heart failure. Cardiovasc Res. 118, 1771–1784 (2022).
Bozkurt, B. et al. Heart failure epidemiology and outcomes statistics: A report of the heart failure society of america. J. Card. Fail 29, 1412–1451 (2023).
Doiron, J. E. et al. Adjunctive therapy with an oral H(2)S donor provides additional therapeutic benefit beyond SGLT2 inhibition in cardiometabolic heart failure with preserved ejection fraction. Br. J. Pharmacol. 181, 4294–4310 (2024).
Datzmann, T. et al. Effects of sodium thiosulfate (Na(2)S(2)O(3)) during resuscitation from hemorrhagic shock in swine with preexisting atherosclerosis. Pharm. Res 151, 104536 (2020).
Merz, T. et al. H(2)S in critical illness-a new horizon for sodium thiosulfate? Biomolecules. 12, 543 (2022).
de Koning, M. L. Y. et al. Safety and tolerability of sodium thiosulfate in patients with an acute coronary syndrome undergoing coronary angiography: a dose-escalation safety pilot study (SAFE-ACS). J. Inter. Cardiol. 2020, 6014915 (2020).
Szczesny, B. et al. AP39, a novel mitochondria-targeted hydrogen sulfide donor, stimulates cellular bioenergetics, exerts cytoprotective effects and protects against the loss of mitochondrial DNA integrity in oxidatively stressed endothelial cells in vitro. Nitric Oxide 41, 120–130 (2014).
Abou-Hamdan, A. et al. Oxidation of H2S in mammalian cells and mitochondria. Methods Enzymol. 554, 201–228 (2015).
Magierowska, K. et al. The mitochondria-targeted sulfide delivery molecule attenuates drugs-induced gastropathy. Involvement of heme oxygenase pathway. Redox Biol. 66, 102847 (2023).
Yan, X. et al. Endogenous H(2)S targets mitochondria to promote continual phagocytosis of erythrocytes by microglia after intracerebral hemorrhage. Redox Biol. 56, 102442 (2022).
Fiorucci, S., Santucci, L. & Distrutti, E. NSAIDs, coxibs, CINOD and H2S-releasing NSAIDs: what lies beyond the horizon. Dig. Liver Dis. 39, 1043–1051 (2007).
Vandiver, M. & Snyder, S. H. Hydrogen sulfide: a gasotransmitter of clinical relevance. J. Mol. Med. (Berl.) 90, 255–263 (2012).
Costa, S. et al. Enhanced analgesic effects and gastrointestinal safety of a novel, hydrogen sulfide-releasing anti-inflammatory drug (ATB-352): a role for endogenous cannabinoids. Antioxid. Redox Signal 33, 1003–1009 (2020).
Sasso, O. et al. Multitarget fatty acid amide hydrolase/cyclooxygenase blockade suppresses intestinal inflammation and protects against nonsteroidal anti-inflammatory drug-dependent gastrointestinal damage. FASEB J. 29, 2616–2627 (2015).
Wallace, J. L. et al. A proof-of-concept, phase 2 clinical trial of the gastrointestinal safety of a hydrogen sulfide-releasing anti-inflammatory drug. Br. J. Pharm. 177, 769–777 (2020).
Glanville, J. R. W. et al. Potent anti-inflammatory effects of an H(2) S-releasing naproxen (ATB-346) in a human model of inflammation. FASEB J. 35, e21913 (2021).
Schnitzer, T. J. et al. Comparison of the COX-inhibiting nitric oxide donator AZD3582 and rofecoxib in treating the signs and symptoms of Osteoarthritis of the knee. Arthritis Rheum. 53, 827–837 (2005).
Fiorucci, S. & Distrutti, E. COXIBs, CINODs and H(2)S-releasing NSAIDs: current perspectives in the development of safer non steroidal anti-inflammatory drugs. Curr. Med. Chem. 18, 3494–3505 (2011).
Fonseca, M. D., Cunha, F. Q., Kashfi, K. & Cunha, T. M. NOSH-aspirin (NBS-1120), a dual nitric oxide and hydrogen sulfide-releasing hybrid, reduces inflammatory pain. Pharm. Res. Perspect. 3, e00133 (2015).
Kodela, R., Chattopadhyay, M., Velazquez-Martinez, C. A. & Kashfi, K. NOSH-aspirin (NBS-1120), a novel nitric oxide- and hydrogen sulfide-releasing hybrid has enhanced chemo-preventive properties compared to aspirin, is gastrointestinal safe with all the classic therapeutic indications. Biochem. Pharm. 98, 564–572 (2015).
Cenac, N. et al. A novel orally administered trimebutine compound (GIC-1001) is anti-nociceptive and features peripheral opioid agonistic activity and Hydrogen Sulphide-releasing capacity in mice. Eur. J. Pain. 20, 723–730 (2016).
Paquette, J. M. et al. Safety, tolerability and pharmacokinetics of trimebutine 3-thiocarbamoylbenzenesulfonate (GIC-1001) in a randomized phase I integrated design study: single and multiple ascending doses and effect of food in healthy volunteers. Clin. Ther. 36, 1650–1664 (2014).
Ullah, H. et al. The efficacy of S-Adenosyl methionine and probiotic supplementation on depression: a synergistic approach. Nutrients. 14, 2751 (2022).
Ullah, H. et al. Efficacy of a food supplement based on S-adenosyl methionine and probiotic strains in subjects with subthreshold depression and mild-to-moderate depression: a monocentric, randomized, cross-over, double-blind, placebo-controlled clinical trial. Biomed. Pharmacother. 156, 113930 (2022).
Xu, F. et al. Integration of ATAC-Seq and RNA-Seq identifies key genes and pathways involved in the neuroprotection of S-adenosylmethionine against perioperative neurocognitive disorder. Comput Struct. Biotechnol. J. 21, 1942–1954 (2023).
Bekdash, R. A. Methyl donors, epigenetic alterations, and brain health: understanding the connection. Int. J. Mol. Sci. 24, 2346 (2023).
Pal, V. K. et al. Hydrogen sulfide blocks HIV rebound by maintaining mitochondrial bioenergetics and redox homeostasis. Elife. 10, e68487 (2021).
Wang, X. B., Cui, H., Liu, X. & Du, J. B. Sulfur dioxide: foe or friend for life? Histol. Histopathol. 32, 1231–1238 (2017).
Acknowledgements
This work was supported by National Natural Science Foundation of China (82170243, 81921001, 82270428), Beijing Natural Science Foundation (7222188), Changjiang Scholars Award Program, National Youth Top-Notch Talent Support Program, and Clinical Medicine Plus X - Young Scholars Project, Peking University, the Fundamental Research Funds for the Central Universities.
Author information
Authors and Affiliations
Contributions
Y.Y.H. sorted out, reviewed, and analyzed the literatures, drew the diagrams, and wrote the manuscript. B.L. sorted out, reviewed, and analyzed the literatures and revised the manuscript. H.J. devised the concept. J.D., M.Y., H.J., Y.Y., and Y.Q.H. supervised the writing and revised the manuscript. All authors have read and approved the article.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hou, Y., Lv, B., Du, J. et al. Sulfide regulation and catabolism in health and disease. Sig Transduct Target Ther 10, 174 (2025). https://doi.org/10.1038/s41392-025-02231-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41392-025-02231-w