Abstract
Recent evidence from clinical and animal studies with anti-inflammatory agents in depression is conflicting. One possible reason is the heterogeneity of baseline inflammation levels. Since older adults are generally associated with chronic low-grade inflammation and depression is one of the most common mental disorders in this population, this meta-analysis aimed to evaluate the therapeutic and preventative effects of anti-inflammatory interventions for depression among older adults. PubMed, Cochrane Library, Embase, and PsycINFO were searched for randomized controlled trials (RCTs) up to November 18, 2024. The primary outcomes were mean change scores of depression scores and incidences of depression after treatment. Pooled standard mean differences (SMDs) and odds ratios (ORs) including 95% confidence intervals (95% CI) were calculated. Of 3116 screened articles, 31 RCTs met the inclusion criteria, with 25 studies investigating efficacy and 7 studies investigating the incidence following anti-inflammatory treatment. Anti-inflammatory interventions were statistically significantly more effective than placebo in reducing depressive scores for older adults with depression (SMD = −0.57, 95% CI = −0.98 to −0.15, p = 0.008). Sub-group analyses supported the use of omega-3 fatty acids (SMD = −0.14, 95% CI = −0.27 to −0.02, p = 0.03) and botanical drug or dietary intervention (SMD = −0.86, 95% CI = −1.58 to −0.13, p = 0.02) among older participants. While limited by substantial heterogeneity among included studies, these results reveal the moderate beneficial effects of anti-inflammatory interventions for the treatment and prevention of depression among older adults. Future high-quality RCTs are warranted to determine which anti-inflammatory interventions are most preferential for older patients with depression.
Similar content being viewed by others
Introduction
Depression is a common mental disorder that severely affects health-related quality of life and even results in death by suicide in extreme cases. In older adults, the prevalence of depression is estimated to be about 10–20% and rises with age [1,2,3,4]. With the aging of the world’s population, depression in older adults will bring an ever-greater disease burden, making it a leading public health concern [5].
When treating a depressive episode, both antidepressants and psychological therapeutic strategies are recommended for the remission of depressive symptoms [6]. In clinical practice, pharmacotherapy is used more frequently than non-pharmacological therapy due to inadequate resources [7]. However, the current antidepressants are unsatisfactory because of their significant adverse effects, lower response, and moderate efficacy, which take weeks to produce a measurable benefit [8]. Even after several sequential treatments with different conventional antidepressants, about one-third of the patients still fail to respond [9]. For geriatric patients with major depressive disorder (MDD), the benefits of traditional antidepressants can be more limited. A meta-analysis revealed that the response rates of antidepressants were 53.9% in younger adult patients, but significantly decreased to 45.2 and 42.2% in older adult patients aged ≥ 55 years old and ≥ 65 years old, respectively [10]. Given that the response rates of placebo reached up to 39.2% in these older patients [10], the efficacy of antidepressants leaves much to be desired. Similarly, another meta-analysis found that second-generation antidepressants seem effective for older MDD patients but the magnitude of the effect is small, and the response rates are numerically lower than those reported for adult MDD patients [11]. Mechanistically, some pioneer studies have discussed that brain-based structural and functional mechanisms [12], including white matter integrity and hyperintensity [13,14,15], may disturb the treatment of late-life depression.
Despite the pathogenesis mechanism of depression being elusive, recent clinical and pre-clinical evidence converges to inflammation and immune dysfunction [16,17,18,19]. Inhibition of inflammation targets sheds light on the discovery of novel therapies for patients suffering from depression [20,21,22]. However, results from studies with anti-inflammatory drugs in depression are conflicting. Taking TNF-α antagonist infliximab, for instance, Lee et al. found a significant reduction in anhedonia after infliximab treatment compared to placebo [23]; McIntyre et al. claimed that infliximab failed to alleviate depressive symptoms compared to placebo [24]. A possible reason for the failure of trials of anti-inflammatory drugs in depression is the heterogeneity of this disease [25]. With the deepening understanding of the role of inflammatory mechanisms in depression, exploring the subgroups of depression patients who may benefit from anti-inflammatory treatment can maximize the treatment effects of anti-inflammatory agents.
Aging is a complex process affected by environmental, genetic, and epigenetic factors and is commonly associated with chronic low-grade inflammation [26]. The low-grade chronic inflammatory status, also termed as inflammaging, has been identified as one of the hallmarks of aging [27]. Inflammaging is a sterile systemic inflammation with self-reactivity in the absence of overt infection [28]. There is compelling evidence showing a reciprocal link between inflammation and depression in older patients, with a possible inflammatory subtype of depression driven by elevated inflammation [29, 30]. Intriguingly, for those depressed patients with increased baseline inflammation, anti-inflammatory interventions are more likely to improve the response rates [31, 32]. Inhibiting the brain inflammaging appears to be a promising strategy for treating late life depression [33]. Preliminary findings suggest that the anti-inflammatory interventions are associated with a lower risk of depressive symptoms [34]. Therefore, Anti-inflammatory treatments are warranted to be further studied in older adults [29, 35].
A few published systematic reviews and meta-analyses have suggested the anti-depressant role of anti-inflammatory interventions in affective disorders [36,37,38]. However, the meta-analysis from Kappelmann et al. [36] focuses on anti-cytokine treatment, but other excluded anti-inflammatory agents may have superior effects. Another meta-analysis from Husain et al. [38] includes patients with major depressive disorder and bipolar disorder, which introduces heterogeneity for the comparisons without subgroup analysis. Moreover, these meta-analyses only assess the efficacy [36] and safety [37,38,39,40] of the interventions in participants, most of whom were adults. No meta-analysis has yet evaluated the preventive effects of anti-inflammatory regimens for depression, and no meta-analysis has examined the evidence among the elder subjects. Importantly, these meta-analyses summarize the data published before 2017 [36,37,38,39,40], while there have been vital research updates from RCTs in this field in the last several years. Therefore, there is an urgent need for a comprehensive examination of the evidence regarding the potential benefits of anti-inflammatory interventions in older adults.
The primary aims of this meta-analysis were to investigate the anti-depressant effects and preventive effects of anti-inflammatory interventions in older participants with or without depressive symptoms. The findings of this study will provide critical insights into the prevention and management of depression in the elderly population.
Materials and methods
Search strategy
The present systematic review and meta-analysis is conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines from Cochrane Handbook [41]. The study protocol was pre-registered online with PROSPERO (no. CRD42023388262). Comprehensive literature searches were performed independently in four electronic databases, including EMBASE, PubMed, Cochrane, PsycINFO, from the date of database inception until November 18, 2024, with indexing terms and text words. Keywords included (depression or depress*) AND (aged or aging or elder* or geriatri* or geronto* or senior*) AND (anti-inflammatory* or NSAID or COX-2 or “cytokine inhibito*” or glucocorticoid or statin* or minocycline or Omega-3). We tried to retrieve all articles using any agents of proved anti-inflammatory properties, including nonsteroidal anti-inflammatory drugs (NSAIDs), antibiotics, cytokine inhibitors, antibodies, steroids and other anti-inflammatory hormones (melatonin and estrogen), statins, glitazones, polyunsaturated fatty acids, modafinil, and anti-inflammatory botanical and dietary interventions. Details of the search strategies and results are provided in Supplementary Table 1. We also searched the reference lists of relevant systematic reviews and meta-analyses. No language restrictions were applied.
Selection criteria
Two independent investigators (H. Gong and W.-J. Su) selected the studies for inclusion. After removing the duplicates, they screened the title/abstract and identified a waitlist of potentially relevant studies for further full-text review. The divergences were resolved by reaching a consensus. Only prospective RCTs, including cross-over randomized trials, were selected when they met all the following inclusion criteria: (1) included older adults aged 55 years or older; (2) reported the depression-related score or incidence; (3) administered monotherapy or combination therapy with anti-inflammatory intervention; (4) included a placebo or active control group. Exclusion criteria included: (1) studies published only as abstracts or reporting insufficient data; (2) enrolled fewer than 20 participants; (3) included patients with bipolar depressive disorder; (4) for multiple studies with overlapping data, only the one with the most information or the largest sample size was selected.
Data extraction
Two investigators (H. Gong and W.-J. Su) extracted the data independently from included RCTs according to a predefined data extraction form. The following information from each trial was obtained: (1) the first author’s surname and publication date of literature; (2) the country where the trial was conducted; (3) the number, age, and sex of the participants (N, age, % women); (4) diseases and comorbidity conditions; (5) intervention and control conditions; (6) treatment duration; and (7) methods for evaluating depression severity. The extracted data were assessed by another author, and the divergence between the two investigators was resolved by discussion with another author.
Quality assessment
The study risk of bias was assessed using the Risk of Bias Tool of the Cochrane Handbook (version 5.1.0. 2011). Briefly, the quality assessment of included RCTs was performed on seven domains: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other biases. Studies were high quality if five or more domains were assessed as having a low risk of bias, and all other items were evaluated as having a low or unknown risk of bias. Studies were classified as low quality if one or more domains were rated as having a high risk of bias. The remaining studies were considered of unclear quality if they met neither the criteria for high risk nor low risk. Divergence was resolved by discussion with a third investigator (S.-L. Deng).
Outcome measures
The primary outcome of this meta-analysis focused on the efficacy and prevention of depression among older adults. To measure the efficacy of anti-inflammatory agents, we summarized the overall mean change in depressive symptom scores from baseline to the end of the trial for patients diagnosed with depression before enrollment. To clarify the preventive effect, we considered the proportion of participants who met the diagnostic criteria for depression at the endpoint. To determine the severity of depressive symptoms, we extracted the score data from several reported rating scales, including the Geriatric Depression Scale (GDS), Center for Epidemiological Studies Depression (CES-D), Hamilton Depression Rating Scale (HDRS), Beck Depression Inventory (BDI), Self-Rating Depression Scale (SDS), Patient Health Questionnaire (PHQ), and Montgomery-Asberg Depression Rating Scale (MADRS). When more than one standardized rating scale was adopted in a single included trial, we selected the data using a predefined hierarchy based on the utilizing frequency and consistency across all included studies. Besides, secondary outcomes included mental health quality (measured by the Quality-of-Life Short Form, SF), response rate (provided in the original trials), all-cause discontinuation, and adverse effects (not presented due to the limited original data obtained).
Data synthesis and analysis
Where applicable, data from comparable trials were pooled in a statistical analysis using the RevMan software (version 5.4, Cochrane Collaboration, Oxford, United Kingdom). Meta-analyses were conducted when data were available from two or more trials for each comparison. A trial with two or more intervention groups was split into two comparisons with the same number of participants in their control groups. Studies without the necessary data were not included in the corresponding quantitative analysis. All tests were two-tailed, with statistical significance set at p ≤ 0.05, except where otherwise specified.
A standardized mean difference (SMD) is appropriate when studies evaluate the same parameter (e.g., depression severity score) with various measuring tools [36]. Thus, for a continuous variable, SMDs and 95% confidence intervals (CIs) were estimated for each trial using the inverse variance analysis method. When the standard deviation (SD) of the change in depressive symptoms from baseline to endpoint was not provided in the original studies, we calculated it according to the formula recommended by the Cochrane Handbook. A global estimation of 0.6 was adopted to estimate the SD [42]. For dichotomous variables, pooled odds ratios (ORs) with 95% CIs were calculated to assess the incidence of depression, response rate, and all-cause discontinuation. The Z-test was used to evaluate the statistical significance of the summarized ORs. The between-trial heterogeneity was assessed by Cochrane’s χ2 test and I2 statistics. The existence of notable heterogeneity is defined as I2 ≥ 50% or p ≤ 0.1. However, considering the expected heterogeneity due to different anti-inflammatory regimens and evaluation tools, the more conservative random-effects model was used for all meta-analyses.
Meta-regression analyses were conducted to investigate potential heterogeneity utilizing the STATA software (version 18, StataCorp LLC, College Station, TX, USA) based on the following potential factors: (1) publication year; (2) gender (% female); (3) sample size; (4) treatment duration; (5) country; (6) age; (7) risk of bias and (8) comorbidity. In addition, subgroup meta-analyses were conducted based on the type of control group (placebo or active control) and type of anti-inflammatory treatment. Sensitivity analyses were performed by sequentially omitting individual trials in each comparison. The results of sensitivity testing were regarded as credible if the summarized p-value was not substantially different (data not shown). Potential publication bias was identified by visual inspection of the funnel plot in comparisons that contained more than 10 trials. Funnel plots with symmetrical scatter and the p-value more than 0.05 of Begg’s test were regarded as having a low risk of publication bias. Furthermore, the quality of evidence for primary outcome will be assessed by two authors (H. Gong and S.-L. Deng) independently utilizing the Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) framework [43] in the GRADE Pro (McMaster University, Ontario, Canada). Consequently, the quality of evidence will be categorized into four different levels: high, moderate, low, and very low.
Results
Study selection
The literature selection process was carried out as shown in the flow diagram of PRISMA (Fig. 1). The literature search yielded a total of 3116 citations, of which 1980 were from Embase, 700 were from PubMed, 267 were from the Cochran Library, 169 were from PsycINFO, and 81 were from other sources. Following the duplicate removal using EndNote X9 software, 2644 unique records were eligible for screening by title and/or abstract. Full-text identification of 136 studies was further performed, of which 31 RCTs met the criteria and were included in this meta-analysis. One article reported both the score changes of depressive symptoms and the number of patients with severe depressive symptoms after treatment with EPA-DHA [44], which was included in the meta-analyses of the treatment and prevention of depression.
Of the 3116 relevant studies, 472 were excluded due to duplication, 2508 were excluded because their titles and abstracts did not meet the criteria, and 105 studies were excluded following full-text screening. 31 RCTs were finally included. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses. *One article reported both the score changes of depressive symptoms and the numbers of patients with severe depressive symptoms after treatment, thus this study was included in the meta-analyses of the treatment and prevention of depression.
Characteristics of eligible studies
The characteristics of eligible studies are shown in Table 1. Twenty-eight eligible studies were published between 1997 and 2023 from various countries (7 from United States, 5 from Australia, 4 from Netherlands, 4 from Iran, 2 from France, 2 from China, 3 from Japan, 2 from Italy, 1 from United Kingdom, and 1 from Sweden). The total sample consisted of 28,727 participants, and female subjects comprised 51.48% (n = 14,788) of them. Most selected studies enrolled participants aged 60 or over, except one that included patients aged 55 or over [45]. Besides, to enlarge sample size, several studies with a mean age over 60 were also included in this meta-analysis [46,47,48,49,50,51,52]. Participants from 11 studies were diagnosed with depression by DSM-V, DSM-IV, GDS, SDS, HADS, HDRS, or CESD. Twenty-five studies reported depressive score changes, allowing meta-analysis of the efficacy of anti-inflammatory agents. Besides, a meta-analysis was conducted to evaluate the preventive effects of anti-inflammatory management based on 7 included studies. Seven studies looked at nonsteroidal anti-inflammatory drugs (NSAIDs), 15 at omega-3 fatty acids (FA), 5 at botanical drugs or dietary interventions, 3 at statins, and 1 at dexamethasone. Most studies adopted placebos as the control groups. Besides outcomes related to depressive symptoms, some studies also reported the quality of life and adverse effects.
Risk of bias
The assessment of the risk of bias showed that 19 studies (61.2%) had a low risk of bias, and 6 studies (19.4%) had an unclear risk of bias. The remaining 6 studies (19.4%) were classified as having a high risk of bias owing to the presence of both performance bias and attrition bias. Overall, most of the RCTs included in this meta-analysis were rated as high-quality studies, as evidenced by the low risk of bias. Supplementary Fig. 1 shows the detailed risk-of-bias assessment, and Supplementary Fig. 2 shows the summary bias risk of the included studies.
Antidepressant effect of anti-inflammatory treatments in older adults
For studies with older patients with a diagnosis of depression, most of them (9 trials) used a placebo as the control group, except for two studies [46, 53, 54]. Compared with the placebo group, older patients administered anti-inflammatory interventions showed significantly lower depressive symptom scores (SMD = −0.57, 95% CI = −0.98 to −0.15, p = 0.008; Fig. 2A). Heterogeneity among the 9 studies was identified as significant (I2 = 92%, p < 0.00001). While compared with the active group (sertraline, tocopherol or tramadol and acetaminophen), the severity of depression in patients from the anti-inflammation group was similar (SMD = 0.80, 95% CI = −0.30 to 1.89, p = 0.15; Fig. 2B). Heterogeneity among the 3 studies was deemed significant (I2 = 90%, p < 0.0001).
A Meta-analysis of anti-inflammatory interventions vs. placebo in older patients with depression. B Meta-analysis of anti-inflammatory interventions vs. active control in older patients with depression. C Meta-analysis of anti-inflammatory interventions vs. placebo in non-depressed elderly adults. SD standard deviation, CI confidence interval.
In addition, 15 studies enrolled 16,505 participants who were not suffering from depression at baseline. All 15 studies compared the effects of anti-inflammatory interventions with a placebo. As shown in Fig. 2C, significant heterogeneity was detected, as evidenced by I2 = 65% (p = 0.0002). Pooling analysis with a random effects model revealed a lower trend in depressive score in the older subjects treated with anti-inflammatory agents compared with the placebo group (SMD = −0.07, 95% CI = −0.16 to 0.01, p = 0.09). Sensitivity analysis of each study yielded very similar findings to those of the original analysis, except for two RCTs from Ness et al. (SMD = −0.09, 95% CI = −0.18 to −0.00, p = 0.04) [51] and Jean-Pierre et al. (SMD = −0.09, 95% CI = −0.18 to 0.00, p = 0.05) [50].
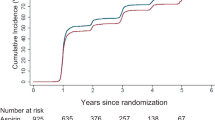
Preventive effect of anti-inflammatory interventions on geriatric depression
Seven of the 31 available trials reported several cases of depression at the end of treatment, allowing us to summarize the preventive effect of anti-inflammatory interventions. From the results of these studies, pooling analysis indicated a moderate but not significant difference in the incidence of depression between anti-inflammatory treatment and placebo, with a pooled OR of 0.73 (95% CI = 0.50 to 1.05, p = 0.09; Fig. 3). This effect estimate was calculated based on a total of 12,961 subjects using a random effects model (I2 = 69%, p = 0.003). Sensitivity analysis of each study yielded very similar findings to those of the original analysis, except for one outlier RCT [52] (SMD = 0.66, 95% CI = 0.43 to 0.99, p = 0.05).
Subgroup analyses
Subgroup analyses were only conducted for the efficacy outcome because of the limited data on prevention. To avoid the disturbance from active control interventions, only studies with placebo control were included in subgroup analyses based on the type of anti-inflammatory treatment. As shown in Fig. 4, four studies with 6 comparisons and 2533 participants investigated the efficacy of NSAIDs, including celecoxib [49, 55], naproxen [49, 55], ibuprofen [49], and aspirin [56, 57]. Subgroup analysis demonstrated that NSAIDs failed to exert antidepressant effects concerning the primary outcome of changes in depressive symptom severity (SMD = −0.09, 95% CI = −0.27 to 0.08, p = 0.28). Significant heterogeneity was detected among studies (I2 = 72%, p = 0.003).
Of the studies included in the meta-analysis, 11 trials with 13,198 participants compared the effects of omega-3 FA with placebo [44, 48, 58,59,60,61,62,63,64,65,66]. Heterogeneity among the 11 comparisons was identified as significant (I2 = 61%, p = 0.005). Subgroup meta-analysis for the primary outcome revealed that omega-3 FA outperformed placebo in terms of antidepressant effects (SMD = −0.14, 95% CI = −0.27 to −0.02, p = 0.03). However, sensitivity analyses showed the results could be affected by omitting one of several studies of omega-3 FA [60, 63,64,65]. A descriptive study [67] was excluded in the meta-analysis. This study demonstrated that the GDS scores were significant improved after treatment with EPA (p = 0.04) and DHA (p = 0.01) [67], suggesting the potential benefits of omega-3 FA intakes in reducing depressive symptoms.
In addition, 6 studies with 915 participants focused on the effects of botanical drugs or dietary interventions, including Xinkeshu tablets [47], nanocurcumin [68], argan oil [69], Soy protein [70], and fish dietary [45, 51]. Subgroup analysis of these studies yielded a moderate but significant improvement in depressive symptom scores, with a pooled SMD of −0.86 (95% CI, −1.58 to −0.13, p = 0.02). A significant heterogeneity was found among these studies (I2 = 95%, p < 0.00001). However, sensitivity analyses performed by excluding each study seriatim in the software could change the results significantly (data not shown) [47, 68]. The remaining study explored the potential anti-depressant effects of lovastatin [71]. No significant effects of this drug were found in this single study (SMD = −0.08, 95% CI = −0.33 to 0.16, p = 0.51).
Mental health quality
Six studies [45, 57, 63, 69, 70, 72] collected the data for the changes in mental health quality as measured by the corresponding component of the SF-12 or SF-36. Meta-analysis showed no difference in score changes of mental health quality between the anti-inflammatory treatment and placebo groups (SMD = 0.04, 95% CI = −0.15 to 0.23, p = 0.69; Fig. 5A). Heterogeneity among these trails was high (I2 = 77%, p = 0.0006).
Response rate
Only two studies [53, 65] provided the number of participants who responded to the anti-inflammatory treatment. Pooling results indicated that the response rate was similar between the two groups (OR = 1.74, 95% CI = 0.79 to 3.81, p = 0.17; Fig. 5B). A random-effects model was used due to the presupposed heterogeneity from the different interventions and treatment durations.
All-cause discontinuation
We further analyzed the all-cause discontinuation, which may help to evaluate the acceptability/safety of these treatments. For these studies missing data about the drop-out participants in each group, they were not synthesized in the meta-analysis. As shown in Fig. 6, the overall all-cause discontinuation was comparable between control group and anti-inflammatory intervention group (OR = 0.99, 95% CI = 0.95 to 1.04, p = 0.75). The similar all-cause discontinuation was also found in each subgroup, including NSAID, omega-3 FA, botanical drug or dietary intervention, statin, modafinil and dexamethasone (Fig. 6).
Meta-regression analyses
Considering the obvious heterogeneity across studies, the meta-regression analyses were performed and the results were presented in the Supplemental Table 2. It showed that most modifiers did not significantly affect the effect of anti-inflammatory interventions in the indices of primary outcome and mental health quality. However, we found that age and risk of bias influenced the antidepressant effect size of anti-inflammatory interventions compared to placebo group in older patients with depression, while country influenced in older patients without depression. The anti-inflammatory interventions seem to be more effective in the younger old patients with depression. More evidence is needed to clarify the impacts of age following anti-inflammatory treatments.
Publication bias and GRADE assessment
Assessment of publication bias was conducted for the effects of anti-inflammatory interventions vs. placebo in older participants without depression at baseline. The inverted funnel plots of these studies presented significant asymmetry (p = 0.035), suggesting the publication bias should not be ignored (Supplementary Fig. 3). The results of GRADE assessment were shown in the Supplementary Table 3. The evidence regarding the comparison of anti-inflammatory interventions with placebo in older adults, both with and without depression, demonstrated low certainty when assessing the antidepressant effect. The low certainty of the evidence is mainly attributed the inadequate allocation concealment, substantial heterogeneity, publication bias, lack of blinding of participants and outcome assessors, etc. Furthermore, the certainty of evidence concerning the antidepressant effect of anti-inflammatory interventions relative to active control in older patients with depression was classified as very low, which is attributed to limitations in study design, significant heterogeneity, and small sample size. Additionally, considering the comorbidities and underlying diseases among the healthy elderly, we upgraded the evidence when evaluating the antidepressant and preventive effects of anti-inflammatory interventions in older adults who did not present with depression at baseline.
Discussion
This meta-analysis represents the most comprehensive summary of currently available data for the treatment and prevention of anti-inflammatory interventions for depression among older adults. Our review of 31 RCTs demonstrated that anti-inflammatory interventions could be more beneficial than placebo control conditions for older adults with or without depressive disorders, and the corresponding SMDs of −0.57 and −0.07 were medium and trivial effect sizes. Compared with active control regimens (sertraline, tocopherol and tramadol), anti-inflammatory treatments were not significantly more effective in reducing depression symptoms for depressed patients, although the limited number of studies available suggests the need for further research. It should be noted that, the evidence of quality in the above outcome of antidepressant effect were low or very low, which may limit the application of this evidence in clinical practice and guideline development. Overall, our results among older adults are consistent with those of previous meta-analyses [37, 39, 40], which also report small to medium effects of anti-inflammatory treatments for patients with depressive symptoms. Intriguingly, we find beneficial effects of omega-3 FA and botanical drug or dietary intervention, but not NSAIDs and statins, among old population. However, young adult MDD patients may benefit from a broader spectrum of anti-inflammatory agents, including NSAIDs, statins, cytokine inhibitors, etc [39, 40]. This distinction might be partially attributed to the severity of depression. The inflammatory activity may be particularly elevated in these severe MDD patients [73], making them benefits more from the classic anti-inflammatory agents.
The preventative effects of anti-inflammatory management for depression have seldom been investigated in previous meta-analyses. Our findings showed that older participants who administered anti-inflammatory interventions might be less likely to suffer from depression than those in the placebo condition. However, the marginal p-value and the upper limit of the credible interval close to the line of no difference suggest concern about whether this estimate is robust enough to guide clinical practice.
Subgroup analyses indicated that omega-3 FA and botanical drug or dietary intervention significantly improved depressive symptoms in older adults, whereas NSAIDs and statins did not. However, the beneficial magnitude of omega-3 FA and botanical drug or dietary intervention is small. Sensitivity analyses also indicate that the anti-depressant effects could be affected by omitting some included studies. Future high-quality RCTs with large sample size are needed to further verify the efficacy of these anti-inflammatory interventions. The current findings suggest that omega-3 FA and botanical drug or dietary intervention may be a superior option than other anti-inflammatory interventions for older adults, even though the benefits of some types, such as statins, have been confirmed among adults [39]. Two meta-analyses of studies reported similar effects of omega-3 FA on reducing depressive symptoms in the elderly population (Hedges’ g = −0.94, 95% CI = −1.37 to 0.50; d = −0.428, 95% CI = −0.822 to −0.035) [74, 75]. However, these previous meta-analyses focused on older adults and only investigated the anti-depressant efficacy of omega-3 FA, without evaluating other types of anti-inflammatory regimens or their preventative effects. Besides, omega-3 FA has been recommended for MDD treatment for the elderly, children, and pregnant women, and prevention in high-risk populations [76]. It should be noted that the negative results of statin and NSAIDs are estimated based on very limited data from studies with significant heterogeneity among them. Surprisingly, several main types of anti-inflammatory agents, such as cytokine inhibitors and corticosteroids for adults with depression were not retrieved in the meta-analysis. One possible interpretation for the lack of these studies is the concern about the safety of these drugs for frail seniors. Moreover, we did not conduct subgroup analyses regarding medical comorbidity condition or the treatment duration due to the insufficient data from included original studies. But certain medical comorbidities may moderate anti-inflammatory treatment impact. For instance, some comorbid conditions of depression, including rheumatoid arthritis [77] and vascular disease [78], are characterized by chronic inflammation. The effectiveness of anti-inflammatory treatment for depression might be partially reduced by overwhelming the comorbidity-evoked inflammation. Besides, comorbidities such as gastrointestinal disorders can affect the drug absorption, and kidney diseases can affect the drug metabolism. These pharmacological alterations may attenuate the benefits of anti-inflammatory treatment for late-life depression. Thus, future studies are need to determine whether increasing the dosage and/or prolonging the treatment duration may enhance the anti-depressant effects of anti-inflammatory interventions in such populations.
Regarding the mental health quality, meta-analysis revealed that anti-inflammatory interventions and control conditions had comparable effects. Several factors may explain this finding. First, participants with chronic comorbidities, such as hypertension and diabetes [45], may benefit less than others. Second, the number of trials in this comparison is few. Physical functioning was not pooled for meta-analysis because some studies only focused on the mental health quality [57, 72]. Moreover, anti-inflammatory interventions have no positive effects on response in older adults with depression, owing to the active control (Sertraline) and small sample size (n = 111). Only two included studies reported the response rates, but did not provide the range and mode of response rate criteria [53, 65]. Future studies are needed to reveal the response rate using accepted definitions. Specifically, for the clinical research community of depression researchers, response is a widely-used psychometric term that is defined as a ≥ 50% decrease from baseline to endpoint in a rating scale [79, 80]. And the 50% limit for response has been validated in multiple depression rating scales, including HAMD, MADRS and BDI [81]. Moreover, it is also helpful to evaluate the efficacy of anti-inflammatory treatment based on the traditional criteria used for endpoint classification: nonresponse ( < 30% improvement), partial response (30–49% improvement), response ( ≥ 50% improvement without reaching remission), and remission (HAMD-17 ≤ 7) [82].
Even though we tried our best to summarize important indicators as much as possible, some of them were not conducted due to insufficient reports, including the detailed safety profile and the comorbidity of inflammatory diseases (such as autoimmune disease [83]). Our meta-analysis showed the similar all-cause discontinuation between two groups, indicating the acceptable safety of anti-inflammatory intervention. These findings are in line with previous evidence of these agents in adult patients with MDD [40]. But whether they are safe and which of them have the highest benefit-risk expectations for older adults remain unanswerable questions. Moreover, most included studies only adopted anti-inflammatory monotherapies as interventions. Given that the add-on therapies based on classic antidepressants also improved depressive symptoms for MDD patients [39, 40], further studies are also needed to investigate the efficacy and safety of adjunctive treatments with antidepressants and anti-inflammatory interventions, especially for these older patients with severe MDD.
To capture these heterogenous processes of inflammaging, various biomarkers related to inflammaging have been proposed to date, however, a broad consensus has not been reached due to this complex biological process. It is possible to identify C-reactive protein (CRP), tumor necrosis factor-alpha (TNF-α) and interleukin-6 (IL-6) and IL-1 as the most relevant systemic markers related to inflammaging [84]. In the context of depression, previous meta-analysis has also identified several inflammatory markers, including CRP and IL-12 [85]. Since CRP is widely used in clinical and research settings, based on the above evidence, CRP could be regarded as one of the potential inflammatory markers in older adults with depression. According to previous work from our and other teams [21, 86], the cut-off of CRP could be set at 3 mg/L. Among the included studies in the present meta-analysis, three studies reported the CRP levels at baseline [48, 65, 69]. One of them reported the change of CRP levels from baseline, which showed no significant change in both control diet group and anti-inflammatory diet group [69]. Future researches are encouraged to report the detailed changes of common inflammatory markers, which would be helpful for preventing the risk of bias and improve the study quality and credibility. Even more importantly, future clinical trials should pay much attention to investigate the pathophysiologic mechanism of the potential anti-inflammatory interventions and avoid to relegate the field to broad spectrum therapeutics [87]. Specifically, future RCTs with anti-inflammatory agents should identify and enrich for inflammatory subgroups of MDD patients using stratified approaches, for instance, circulating CRP > 3 mg/L. Moreover, in addition to the efficacy and safety files, the relevant inflammatory pathways along the chain of pathology should also been verified after anti-inflammatory intervention. All these efforts will contribute to the precise treatment of depression.
This study provides a new perspective on using anti-inflammatory interventions in the elderly population. The anti-inflammatory regimen can be a potential choice for depression amelioration and prevention in older adults. Considering the limited efficacy of current antidepressant agents, it is warranted to further assess the combined effect of antidepressants and omega-3 FA, botanical drug or dietary intervention. Besides, more high-quality RCTs are needed to answer the following important questions. First, which kind of botanical drug or dietary interventions or what ratio of omega-3 FA is most recommended for older adults? Second, how do we adjust the anti-inflammatory regimens for therapeutic or preventative purposes?
This meta-analysis had several limitations. First, to retrieve as much data as possible from available clinical studies of anti-inflammatory interventions in managing of depressive symptoms in elder subjects, we included subjects with an average age older than 60. The results may be underestimated or overestimated due to this confounding factor, while we took this confounding factor into account in the GRADE assessment. Second, although all the included original studies were RCTs, the baseline depressive scores could be different [45]. Meta-analysis based on the changes in depressive symptoms from baseline to endpoint could mitigate but could not fully avoid the potential overestimation of our results. Besides, given that most included studies assessed depressive symptoms by GDS > 5 points, our findings could be more applicable for mild to moderate depression in the elderly. The efficacy of anti-inflammatory treatments on severe depression remains to be verified by further clinical trials. Third, substantial heterogeneity was found in most analyses, which could not be effectively avoided by subgroup analysis or sensitivity analysis. Fourth, insufficient data were available to determine the difference in efficacy of anti-inflammatory interventions on older participants with and without high-level baseline inflammation. Fifth, the classification of anti-inflammatory treatments for older adults remains provisional. For instance, the interventions implemented in the studies of this meta-analysis under the heading “botanical drug or dietary intervention” were somewhat heterogeneous.
In conclusion, our findings of the comprehensive meta-analysis support the notion that anti-inflammatory interventions might help to prevent and reduce depressive symptoms in older participants with or without depression. Omega-3 FA and botanical drugs, or dietary intervention, rather than NSAIDs or statins, show promising anti-depressant effects in older adults. However, the results should be interpreted with caution due to significant heterogeneity in most comparisons. Future RCTs are warranted to further assess the safety and efficacy of anti-inflammatory intervention monotherapy or combined treatment with first-line antidepressants.
Data availability
Data will be made available on request to the author (H. Gong, hgong@tmmu.edu.cn).
References
Chew-Graham C, Baldwin R, Burns A. Treating depression in later life. BMJ. 2004;329:181–2. https://doi.org/10.1136/bmj.329.7459.181
Blazer DG. Depression in late life: review and commentary. J Gerontol A Biol Sci Med Sci. 2003;58:249–65. https://doi.org/10.1093/gerona/58.3.m249
Tang T, Jiang J, Tang X. Prevalence of depressive symptoms among older adults in mainland China: a systematic review and meta-analysis. J Affect Disord. 2021;293:379–90. https://doi.org/10.1016/j.jad.2021.06.050
Kok RM, Reynolds CF 3rd. Management of depression in older adults: a review. JAMA. 2017;317:2114–22. https://doi.org/10.1001/jama.2017.5706
Alexopoulos GS. Depression in the elderly. Lancet. 2005;365:1961–70. https://doi.org/10.1016/s0140-6736(05)66665-2
Croatto G, Vancampfort D, Miola A, Olivola M, Fiedorowicz JG, Firth J, et al. The impact of pharmacological and non-pharmacological interventions on physical health outcomes in people with mood disorders across the lifespan: an umbrella review of the evidence from randomised controlled trials. Mol Psychiatry. 2023;28:369–90. https://doi.org/10.1038/s41380-022-01770-w
Cipriani A, Furukawa TA, Salanti G, Chaimani A, Atkinson LZ, Ogawa Y, et al. Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: a systematic review and network meta-analysis. Lancet. 2018;391:1357–66. https://doi.org/10.1016/s0140-6736(17)32802-7
Malhi GS, Mann JJ. Depression. Lancet. 2018;392:2299–312. https://doi.org/10.1016/s0140-6736(18)31948-2
Cuijpers P. The challenges of improving treatments for depression. JAMA. 2018;320:2529–30. https://doi.org/10.1001/jama.2018.17824
Tedeschini E, Levkovitz Y, Iovieno N, Ameral VE, Nelson JC, Papakostas GI. Efficacy of antidepressants for late-life depression: a meta-analysis and meta-regression of placebo-controlled randomized trials. J Clin Psychiatry. 2011;72:1660–8. https://doi.org/10.4088/JCP.10r06531
Nelson JC, Delucchi K, Schneider LS. Efficacy of second generation antidepressants in late-life depression: a meta-analysis of the evidence. Am J Geriatr Psychiatry. 2008;16:558–67. https://doi.org/10.1097/JGP.0b013e3181693288
Gunning FM, Oberlin LE, Schier M, Victoria LW. Brain-based mechanisms of late-life depression: Implications for novel interventions. Semin Cell Dev Biol. 2021;116:169–79. https://doi.org/10.1016/j.semcdb.2021.05.002
Reppermund S, Zhuang L, Wen W, Slavin MJ, Trollor JN, Brodaty H, et al. White matter integrity and late-life depression in community-dwelling individuals: diffusion tensor imaging study using tract-based spatial statistics. Br J Psychiatry. 2014;205:315–20. https://doi.org/10.1192/bjp.bp.113.142109
Mettenburg JM, Benzinger TL, Shimony JS, Snyder AZ, Sheline YI. Diminished performance on neuropsychological testing in late life depression is correlated with microstructural white matter abnormalities. Neuroimage. 2012;60:2182–90. https://doi.org/10.1016/j.neuroimage.2012.02.044
Sheline YI, Price JL, Vaishnavi SN, Mintun MA, Barch DM, Epstein AA, et al. Regional white matter hyperintensity burden in automated segmentation distinguishes late-life depressed subjects from comparison subjects matched for vascular risk factors. Am J Psychiatry. 2008;165:524–32. https://doi.org/10.1176/appi.ajp.2007.07010175
Bekhbat M, Li Z, Mehta ND, Treadway MT, Lucido MJ, Woolwine BJ, et al. Functional connectivity in reward circuitry and symptoms of anhedonia as therapeutic targets in depression with high inflammation: evidence from a dopamine challenge study. Mol Psychiatry. 2022;27:4113–21. https://doi.org/10.1038/s41380-022-01715-3
Swardfager W, Rosenblat JD, Benlamri M, McIntyre RS. Mapping inflammation onto mood: Inflammatory mediators of anhedonia. Neurosci Biobehav Rev. 2016;64:148–66. https://doi.org/10.1016/j.neubiorev.2016.02.017
Beurel E, Toups M, Nemeroff CB. The Bidirectional Relationship of Depression and Inflammation: Double Trouble. Neuron. 2020;107:234–56. https://doi.org/10.1016/j.neuron.2020.06.002
Xu ZY, Zhang T, Gong H, Zheng H, Liu MS, Guo BH, et al. Beyond the surface: tracing the evolution of inflammatory mechanism in depression through bibliometric analysis. Endocr Metab Immune Disord Drug Targets. 2025. https://doi.org/10.2174/0118715303325541241024060229
Gong H, Su WJ, Cao ZY, Lian YJ, Peng W, Liu YZ, et al. Hippocampal Mrp8/14 signaling plays a critical role in the manifestation of depressive-like behaviors in mice. J Neuroinflammation. 2018;15:252. https://doi.org/10.1186/s12974-018-1296-0
Cao ZY, Liu YZ, Li JM, Ruan YM, Yan WJ, Zhong SY, et al. Glycyrrhizic acid as an adjunctive treatment for depression through anti-inflammation: a randomized placebo-controlled clinical trial. J Affect Disord. 2020;265:247–54. https://doi.org/10.1016/j.jad.2020.01.048
Drevets WC, Wittenberg GM, Bullmore ET, Manji HK. Immune targets for therapeutic development in depression: towards precision medicine. Nat Rev Drug Discov. 2022;21:224–44. https://doi.org/10.1038/s41573-021-00368-1
Lee Y, Mansur RB, Brietzke E, Carmona NE, Subramaniapillai M, Pan Z, et al. Efficacy of adjunctive infliximab vs. placebo in the treatment of anhedonia in bipolar I/II depression. Brain Behav Immun. 2020;88:631–9. https://doi.org/10.1016/j.bbi.2020.04.063
McIntyre RS, Subramaniapillai M, Lee Y, Pan Z, Carmona NE, Shekotikhina M, et al. Efficacy of adjunctive infliximab vs placebo in the treatment of adults with bipolar I/II depression: a randomized clinical trial. JAMA Psychiatry. 2019;76:783–90. https://doi.org/10.1001/jamapsychiatry.2019.0779
Milaneschi Y, Lamers F, Berk M, Penninx B. Depression heterogeneity and its biological underpinnings: toward immunometabolic depression. Biol Psychiatry. 2020;88:369–80. https://doi.org/10.1016/j.biopsych.2020.01.014
Ferrucci L, Corsi A, Lauretani F, Bandinelli S, Bartali B, Taub DD, et al. The origins of age-related proinflammatory state. Blood. 2005;105:2294–9. https://doi.org/10.1182/blood-2004-07-2599
López-Otín C, Blasco MA, Partridge L, Serrano M, Kroemer G. Hallmarks of aging: an expanding universe. Cell. 2023;186:243–78. https://doi.org/10.1016/j.cell.2022.11.001
Baechle JJ, Chen N, Makhijani P, Winer S, Furman D, Winer DA. Chronic inflammation and the hallmarks of aging. Mol Metab. 2023;74:101755. https://doi.org/10.1016/j.molmet.2023.101755
Forbes MP, O’Neil A, Lane M, Agustini B, Myles N, Berk M. Major depressive disorder in older patients as an inflammatory disorder: implications for the pharmacological management of geriatric depression. Drugs Aging. 2021;38:451–67. https://doi.org/10.1007/s40266-021-00858-2
Xia J, Chen M, Shao H, Chen H, Zhu S, Zhao M, et al. Inflammation and late-life depression: unraveling the complex relationship and potential therapeutic strategies. Front Biosci. 2023;28:356. https://doi.org/10.31083/j.fbl2812356
Husain MI, Deakin B, Chaudhry IB, Mulsant BH, Young AH. Trial failures of anti-inflammatory drugs in depression - authors’ reply. Lancet Psychiatry. 2020;7:837–8. https://doi.org/10.1016/s2215-0366(20)30391-6
Berk M, Vieta E, Dean OM. Anti-inflammatory treatment of bipolar depression: promise and disappointment. Lancet Psychiatry. 2020;7:467–8. https://doi.org/10.1016/s2215-0366(20)30155-3
Ishizuka T, Nagata W, Nakagawa K, Takahashi S. Brain inflammaging in the pathogenesis of late-life depression. Hum Cell. 2024;38:7. https://doi.org/10.1007/s13577-024-01132-4
Lv X, Sun S, Wang J, Chen H, Li S, Hu Y, et al. Anti-inflammatory dietary diversity and depressive symptoms among older adults: a nationwide cross-sectional analysis. Nutrients. 2022;14:5062. https://doi.org/10.3390/nu14235062
Milaneschi Y, Corsi AM, Penninx BW, Bandinelli S, Guralnik JM, Ferrucci L. Interleukin-1 receptor antagonist and incident depressive symptoms over 6 years in older persons: the InCHIANTI study. Biol Psychiatry. 2009;65:973–8. https://doi.org/10.1016/j.biopsych.2008.11.011
Kappelmann N, Lewis G, Dantzer R, Jones PB, Khandaker GM. Antidepressant activity of anti-cytokine treatment: a systematic review and meta-analysis of clinical trials of chronic inflammatory conditions. Mol Psychiatry. 2018;23:335–43. https://doi.org/10.1038/mp.2016.167
Köhler O, Benros ME, Nordentoft M, Farkouh ME, Iyengar RL, Mors O, et al. Effect of anti-inflammatory treatment on depression, depressive symptoms, and adverse effects: a systematic review and meta-analysis of randomized clinical trials. JAMA Psychiatry. 2014;71:1381–91. https://doi.org/10.1001/jamapsychiatry.2014.1611
Husain MI, Strawbridge R, Stokes PR, Young AH. Anti-inflammatory treatments for mood disorders: systematic review and meta-analysis. J Psychopharmacol. 2017;31:1137–48. https://doi.org/10.1177/0269881117725711
Köhler-Forsberg O, C NL, Hjorthøj C, Nordentoft M, Mors O, Benros ME. Efficacy of anti-inflammatory treatment on major depressive disorder or depressive symptoms: meta-analysis of clinical trials. Acta Psychiatr Scand. 2019;139:404–19. https://doi.org/10.1111/acps.13016
Bai S, Guo W, Feng Y, Deng H, Li G, Nie H, et al. Efficacy and safety of anti-inflammatory agents for the treatment of major depressive disorder: a systematic review and meta-analysis of randomised controlled trials. J Neurol Neurosurg Psychiatry. 2020;91:21–32. https://doi.org/10.1136/jnnp-2019-320912
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. https://doi.org/10.1136/bmj.b2535
Gong H, Ni C, Shen X, Wu T, Jiang C. Yoga for prenatal depression: a systematic review and meta-analysis. BMC Psychiatry. 2015;15:14. https://doi.org/10.1186/s12888-015-0393-1
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–6. https://doi.org/10.1136/bmj.39489.470347.AD
Giltay EJ, Geleijnse JM, Kromhout D. Effects of n-3 fatty acids on depressive symptoms and dispositional optimism after myocardial infarction. Am J Clin Nutr. 2011;94:1442–50. https://doi.org/10.3945/ajcn.111.018259
Sharifan P, Hosseini MS, Sharifan A. The interventional relationship between frequent fish consumption and depression symptoms in aging adults: a randomized controlled trial. Int J Geriatr Psychiatry. 2017;32:e116–e122. https://doi.org/10.1002/gps.4668
Tetsunaga T, Tetsunaga T, Tanaka M, Ozaki T. Efficacy of tramadol-acetaminophen tablets in low back pain patients with depression. J Orthop Sci. 2015;20:281–6. https://doi.org/10.1007/s00776-014-0674-4
Ma H, Wang Y, Xue Y, Huang D, Kong Y, Zhao X, et al. The effect of Xinkeshu tablets on depression and anxiety symptoms in patients with coronary artery disease: results from a double-blind, randomized, placebo-controlled study. Biomed Pharmacother. 2019;112:108639. https://doi.org/10.1016/j.biopha.2019.108639
Chang JP, Chang SS, Yang HT, Chen HT, Chien YC, Yang B, et al. Omega-3 polyunsaturated fatty acids in cardiovascular diseases comorbid major depressive disorder - results from a randomized controlled trial. Brain Behav Immun. 2020;85:14–20. https://doi.org/10.1016/j.bbi.2019.03.012
Iyengar RL, Gandhi S, Aneja A, Thorpe K, Razzouk L, Greenberg J, et al. NSAIDs are associated with lower depression scores in patients with osteoarthritis. Am J Med. 2013;126:1017.e1011–1018. https://doi.org/10.1016/j.amjmed.2013.02.037
Jean-Pierre P, Morrow GR, Roscoe JA, Heckler C, Mohile S, Janelsins M, et al. A phase 3 randomized, placebo-controlled, double-blind, clinical trial of the effect of modafinil on cancer-related fatigue among 631 patients receiving chemotherapy: a university of Rochester cancer center community clinical oncology program research base study. Cancer. 2010;116:3513–20. https://doi.org/10.1002/cncr.25083
Ness AR, Gallacher JE, Bennett PD, Gunnell DJ, Rogers PJ, Kessler D, et al. Advice to eat fish and mood: a randomised controlled trial in men with angina. Nutr Neurosci. 2003;6:63–65. https://doi.org/10.1080/1028415021000056069
Vyas CM, Mischoulon D, Chang G, Cook NR, Weinberg A, Copeland T, et al. Effects of vitamin D(3) and marine omega-3 fatty acids supplementation on indicated and selective prevention of depression in older adults: results from the clinical center sub-cohort of the VITamin D and omega-3 trial (VITAL). J Clin Psychiatry. 2023;84:22m14629. https://doi.org/10.4088/JCP.22m14629
Ahmadpanah M, Ramezanshams F, Ghaleiha A, Akhondzadeh S, Sadeghi Bahmani D, Brand S. Crocus Sativus L. (saffron) versus sertraline on symptoms of depression among older people with major depressive disorders-a double-blind, randomized intervention study. Psychiatry Res. 2019;282:112613. https://doi.org/10.1016/j.psychres.2019.112613
Carlsson CM, Papcke-Benson K, Carnes M, McBride PE, Stein JH. Health-related quality of life and long-term therapy with pravastatin and tocopherol (vitamin E) in older adults. Drugs Aging. 2002;19:793–805. https://doi.org/10.2165/00002512-200219100-00008
Fields C, Drye L, Vaidya V, Lyketsos C. Celecoxib or naproxen treatment does not benefit depressive symptoms in persons age 70 and older: findings from a randomized controlled trial. Am J Geriatr Psychiatry. 2012;20:505–13. https://doi.org/10.1097/JGP.0b013e318227f4da
Tofler GH, Morel-Kopp MC, Spinaze M, Dent J, Ward C, McKinley S, et al. The effect of metoprolol and aspirin on cardiovascular risk in bereavement: a randomized controlled trial. Am Heart J. 2020;220:264–72. https://doi.org/10.1016/j.ahj.2019.11.003
Berk M, Agustini B, Woods RL, Nelson MR, Shah RC, Reid CM, et al. Effects of aspirin on the long-term management of depression in older people: a double-blind randomised placebo-controlled trial. Mol Psychiatry. 2021;26:5161–70. https://doi.org/10.1038/s41380-021-01020-5
Duffy SL, Lagopoulos J, Cockayne N, Lewis SJ, Hickie IB, Hermens DF, et al. The effect of 12-wk ω-3 fatty acid supplementation on in vivo thalamus glutathione concentration in patients “at risk” for major depression. Nutrition. 2015;31:1247–54. https://doi.org/10.1016/j.nut.2015.04.019
Freund-Levi Y, Basun H, Cederholm T, Faxén-Irving G, Garlind A, Grut M, et al. Omega-3 supplementation in mild to moderate Alzheimer’s disease: effects on neuropsychiatric symptoms. Int J Geriatr Psychiatry. 2008;23:161–9. https://doi.org/10.1002/gps.1857
Hashimoto M, Kato S, Tanabe Y, Katakura M, Mamun AA, Ohno M, et al. Beneficial effects of dietary docosahexaenoic acid intervention on cognitive function and mental health of the oldest elderly in Japanese care facilities and nursing homes. Geriatr. Gerontol. Int. 2017;17:330–7. https://doi.org/10.1111/ggi.12691
Ogawa T, Sawane K, Ookoshi K, Kawashima R. Supplementation with flaxseed oil rich in alpha-linolenic acid improves verbal fluency in healthy older adults. Nutrients. 2023;15:1499. https://doi.org/10.3390/nu15061499
Okereke OI, Vyas CM, Mischoulon D, Chang G, Cook NR, Weinberg A, et al. Effect of long-term supplementation with marine omega-3 fatty acids vs placebo on risk of depression or clinically relevant depressive symptoms and on change in mood scores: a randomized clinical trial. JAMA. 2021;326:2385–94. https://doi.org/10.1001/jama.2021.21187
Rondanelli M, Giacosa A, Opizzi A, Pelucchi C, La Vecchia C, Montorfano G, et al. Effect of omega-3 fatty acids supplementation on depressive symptoms and on health-related quality of life in the treatment of elderly women with depression: a double-blind, placebo-controlled, randomized clinical trial. J Am Coll Nutr. 2010;29:55–64. https://doi.org/10.1080/07315724.2010.10719817
Rondanelli M, Opizzi A, Faliva M, Mozzoni M, Antoniello N, Cazzola R, et al. Effects of a diet integration with an oily emulsion of DHA-phospholipids containing melatonin and tryptophan in elderly patients suffering from mild cognitive impairment. Nutr Neurosci. 2012;15:46–54. https://doi.org/10.1179/1476830511y.0000000032
Tajalizadekhoob Y, Sharifi F, Fakhrzadeh H, Mirarefin M, Ghaderpanahi M, Badamchizade Z, et al. The effect of low-dose omega 3 fatty acids on the treatment of mild to moderate depression in the elderly: a double-blind, randomized, placebo-controlled study. Eur Arch Psychiatry Clin Neurosci. 2011;261:539–49. https://doi.org/10.1007/s00406-011-0191-9
van de Rest O, Geleijnse JM, Kok FJ, van Staveren WA, Hoefnagels WH, Beekman AT, et al. Effect of fish-oil supplementation on mental well-being in older subjects: a randomized, double-blind, placebo-controlled trial. Am J Clin Nutr. 2008;88:706–13. https://doi.org/10.1093/ajcn/88.3.706
Sinn N, Milte CM, Street SJ, Buckley JD, Coates AM, Petkov J, et al. Effects of n-3 fatty acids, EPA v. DHA, on depressive symptoms, quality of life, memory and executive function in older adults with mild cognitive impairment: a 6-month randomised controlled trial. Br J Nutr. 2012;107:1682–93. https://doi.org/10.1017/s0007114511004788
Osali A, Rostami A. Effect of 6 weeks of aerobic training with nanocurcumin consumption on IL1β, nitric oxide, and depression in women with metabolic syndrome. Int J Diabetes Dev Ctries. 2023;43:1007–14. https://doi.org/10.1007/s13410-023-01168-6
Bourdel-Marchasson I, Ostan R, Regueme SC, Pinto A, Pryen F, Charrouf Z, et al. Quality of life: psychological symptoms-effects of a 2-month healthy diet and nutraceutical intervention; a randomized, open-label intervention trial (RISTOMED). Nutrients. 2020;12:800. https://doi.org/10.3390/nu12030800
Kok L, Kreijkamp-Kaspers S, Grobbee DE, Lampe JW, van der Schouw YT. A randomized, placebo-controlled trial on the effects of soy protein containing isoflavones on quality of life in postmenopausal women. Menopause. 2005;12:56–62. https://doi.org/10.1097/00042192-200512010-00011
Santanello NC, Barber BL, Applegate WB, Elam J, Curtis C, Hunninghake DB, et al. Effect of pharmacologic lipid lowering on health-related quality of life in older persons: results from the cholesterol reduction in seniors program (CRISP) pilot study. J Am Geriatr Soc. 1997;45:8–14. https://doi.org/10.1111/j.1532-5415.1997.tb00971.x
Berk M, Woods RL, Nelson MR, Shah RC, Reid CM, Storey E, et al. Effect of aspirin vs placebo on the prevention of depression in older people: a randomized clinical trial. JAMA Psychiatry. 2020;77:1012–20. https://doi.org/10.1001/jamapsychiatry.2020.1214
Strawbridge R, Hodsoll J, Powell TR, Hotopf M, Hatch SL, Breen G, et al. Inflammatory profiles of severe treatment-resistant depression. J Affect Disord. 2019;246:42–51. https://doi.org/10.1016/j.jad.2018.12.037
Bai ZG, Bo A, Wu SJ, Gai QY, Chi I. Omega-3 polyunsaturated fatty acids and reduction of depressive symptoms in older adults: a systematic review and meta-analysis. J Affect Disord. 2018;241:241–8. https://doi.org/10.1016/j.jad.2018.07.057
Bae JH, Kim G. Systematic review and meta-analysis of omega-3-fatty acids in elderly patients with depression. Nutr Res. 2018;50:1–9. https://doi.org/10.1016/j.nutres.2017.10.013
Guu TW, Mischoulon D, Sarris J, Hibbeln J, McNamara RK, Hamazaki K, et al. International society for nutritional psychiatry research practice guidelines for omega-3 fatty acids in the treatment of major depressive disorder. Psychother Psychosom. 2019;88:263–73. https://doi.org/10.1159/000502652
Ren H, Lin F, Wu L, Tan L, Lu L, Xie X, et al. The prevalence and the effect of interferon -γ in the comorbidity of rheumatoid arthritis and depression. Behav Brain Res. 2023;439:114237. https://doi.org/10.1016/j.bbr.2022.114237
Taylor WD, Aizenstein HJ, Alexopoulos GS. The vascular depression hypothesis: mechanisms linking vascular disease with depression. Mol Psychiatry. 2013;18:963–74. https://doi.org/10.1038/mp.2013.20
Deshauer D, Moher D, Fergusson D, Moher E, Sampson M, Grimshaw J. Selective serotonin reuptake inhibitors for unipolar depression: a systematic review of classic long-term randomized controlled trials. CMAJ. 2008;178:1293–301. https://doi.org/10.1503/cmaj.071068
Nierenberg AA, DeCecco LM. Definitions of antidepressant treatment response, remission, nonresponse, partial response, and other relevant outcomes: a focus on treatment-resistant depression. J Clin Psychiatry. 2001;62:5–9. Suppl 16
Riedel M, Möller HJ, Obermeier M, Schennach-Wolff R, Bauer M, Adli M, et al. Response and remission criteria in major depression–a validation of current practice. J Psychiatr Res. 2010;44:1063–8. https://doi.org/10.1016/j.jpsychires.2010.03.006
Kelley ME, Dunlop BW, Nemeroff CB, Lori A, Carrillo-Roa T, Binder EB, et al. Response rate profiles for major depressive disorder: Characterizing early response and longitudinal nonresponse. Depress Anxiety. 2018;35:992–1000. https://doi.org/10.1002/da.22832
Hesselvig JH, Egeberg A, Kofoed K, Gislason G, Dreyer L. Increased risk of depression in patients with cutaneous lupus erythematosus and systemic lupus erythematosus: a Danish nationwide cohort study. Br J Dermatol. 2018;179:1095–101. https://doi.org/10.1111/bjd.16831
Salvioli S, Basile MS, Bencivenga L, Carrino S, Conte M, Damanti S, et al. Biomarkers of aging in frailty and age-associated disorders: state of the art and future perspective. Ageing Res Rev. 2023;91:102044. https://doi.org/10.1016/j.arr.2023.102044
Osimo EF, Pillinger T, Rodriguez IM, Khandaker GM, Pariante CM, Howes OD. Inflammatory markers in depression: a meta-analysis of mean differences and variability in 5166 patients and 5083 controls. Brain Behav Immun. 2020;87:901–9. https://doi.org/10.1016/j.bbi.2020.02.010
Sforzini L, Marizzoni M, Bottanelli C, Kunšteková V, Zonca V, Saleri S, et al. Transcriptomic profiles in major depressive disorder: the role of immunometabolic and cell-cycle-related pathways in depression with different levels of inflammation. Mol Psychiatry. 2024. https://doi.org/10.1038/s41380-024-02736-w
Miller AH, Raison CL. Burning down the house: reinventing drug discovery in psychiatry for the development of targeted therapies. Mol Psychiatry. 2023;28:68–75. https://doi.org/10.1038/s41380-022-01887-y
Maltais M, de Souto Barreto P, Pothier K, Cantet C, Andrieu S, Rolland Y et al. Lifestyle multidomain intervention, omega-3 supplementation, or both for reducing the risk of developing clinically relevant depressive symptoms in older adults with memory complaints? Secondary analysis from the MAPT trial. Exp Gerontol. 2019;28–34. https://doi.org/10.1016/j.exger.2019.02.010.
Kok L, Hillegers MH, Veldhuijzen DS, Cornelisse S, Nierich AP, van der Maaten JM. et al. The Effect of Dexamethasone on Symptoms of Posttraumatic Stress Disorder and Depression After Cardiac Surgery and Intensive Care Admission: Longitudinal Follow-Up of a Randomized Controlled Trial. Crit Care Med. 2016;44:512–20. https://doi.org/10.1097/CCM.0000000000001419.
Acknowledgements
We thank Mr. Zhang Shuai-Long for his assistance in the meta-regression analyses. This work was supported by the National Natural Science Foundation of China (Grant Nos. 82201687, U23A20476, 82071544, and 82101607), and the National Key R&D Program of China (Grant No. 2021YFA1101203).
Author information
Authors and Affiliations
Contributions
HG, DMZ, and XTF jointly conceptualized the study and wrote the draft of the manuscript. HG, WJS, and SLD conducted the statistical analyses and verified the data. YL and KYL visualized the data in tables and figures. JL and ZLD provided administrative and technical supports. HG, WJS, and XTF obtained funding. All authors revised and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Gong, H., Su, WJ., Deng, SL. et al. Anti-inflammatory interventions for the treatment and prevention of depression among older adults: a systematic review and meta-analysis. Transl Psychiatry 15, 114 (2025). https://doi.org/10.1038/s41398-025-03317-3
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41398-025-03317-3