Abstract
Amyotrophic lateral sclerosis-frontotemporal spectrum disorder (ALS-FTSD) is a fatal neurodegenerative condition, and identifying its modifiable risk factors is a critical public health issue. This large-scale prospective cohort study investigated the role of sleep-related factors in ALS-FTSD risk using data from 396,918 UK Biobank participants. Eight sleep-related exposures were assessed, and Cox proportional hazards regression was employed to evaluate their associations with ALS-FTSD incidence. Subgroup and sensitivity analyses were conducted to validate the robustness of our findings. At baseline, participants had a mean age of 56.31 ± 8.12 years, with 47.5% being male. In the fully adjusted Cox model, organic sleep disorders (G47) (HR: 1.81, 95% CI: 1.21, 2.72, P = 0.004), hypersomnia (G47.1) (HR: 36.53, 95% CI: 9.04, 147.55, P < 0.001), and extreme short sleep (<5 h per day) (HR: 2.09, 95% CI: 1.09, 3.99, P = 0.046) were significantly associated with increased ALS-FTSD risk. In conclusions, these findings revealed the relationship between sleep and the risk of ALS-FTSD, identifying new modifiable risk factors and potential preventive possibilities for ALS-FTSD. Further research is warranted to elucidate the mechanistic links between sleep disturbances and ALS-FTSD pathogenesis.
Similar content being viewed by others
Introduction
Amyotrophic lateral sclerosis (ALS) and frontotemporal dementia (FTD) represent two poles of a clinical spectrum characterized by progressive neurodegeneration [1, 2]. ALS primarily affects motor function due to the degeneration of motor neurons, while FTD impacts cognition, behavior, and language through deterioration in the frontal and temporal lobes. Emerging evidence suggests that ALS patients and FTD patients exhibit overlapping clinical manifestations, genetic, molecular, and pathological underpinnings, leading to the gradual recognition of these conditions as a continuum disorder known as the amyotrophic lateral sclerosis-frontotemporal spectrum disorder (ALS-FTSD) [1, 2].
Lifestyle-related risk factors play a crucial role in the etiology and progression of neurodegenerative diseases [3, 4]. Increasing research supports a complex bidirectional relationship between sleep disorders and neurodegeneration, potentially serving as both cause and consequence [5]. Sleep disorders positively impact various neurodegenerative diseases: for instance, insomnia markedly increases the susceptibility of developing Alzheimer’s disease (AD) and Parkinson’s disease (PD), while a strong association exists between rapid eye movement sleep behavior disorder and the risk of synucleinopathies, such as PD and Lewy body dementia (LBD) [5]. Regarding ALS-FTSD, limited-sample cross-sectional studies based on self-reported sleep questionnaires have described the characteristics of sleep disturbances in patients with ALS or FTD [6,7,8]. However, the relationship between sleep factors and the incidence of ALS-FTSD remains unclear.
Therefore, we aim to comprehensively assess the association between sleep-related factors and the risk of patients with ALS-FTSD. This investigation bases on sleep-related exposures obtained from the International Classification of Diseases 10th Revision (ICD-10) diagnosis codes, self-reported questionnaires, and wrist-worn accelerometer data obtained from the UK Biobank.
Methods
Study design and participants
In a large-scale population-based prospective cohort study, the UK Biobank recruited over 500,000 participants aged 40–69 from 22 centers across the United Kingdom between 2006 and 2010. This pioneering initiative has curated a comprehensive repository of health-related data, including detailed demographic profiles, phenotypic records, and lifestyle factors, providing researchers with unprecedented insights into multifaceted aspects of human health and disease. In addition to baseline assessment data, during the period from 2013–2015, over 100,000 UK Biobank participants consented to wear an AX3 wrist-worn triaxial accelerometer (Axivity, Newcastle upon Tyne, UK) for 7 days, generating objective device-monitored physical activity records (referred to as accelerometer data) [9]. Data are accessible through application to the UK Biobank (https://www.ukbiobank.ac.uk/), subject to data availability restrictions. Further detailed descriptions of the UK Biobank have been reported [10].
After controlling for data quality, the analysis included a total of 396,918 UK Biobank participants, along with 83,227 participants who had eligible accelerometer data. Figure 1 summarized the the study design and data source. Individuals reporting an ALS or FTD diagnosis at baseline, as well as those with missing data or unknown values for one or more covariates or exposures, were excluded. Ethical approval for the UK Biobank study was obtained from the North West Multi-centre Research Ethics Committee (11/NW/03820), with all participants providing written informed consent. Our study was conducted under UK Biobank Application Number 98992 and followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline for cohort studies (Supplementary Table 1).
Assessment of sleep exposure
The first reported date of an ICD10 sleep code (G47 or F51) was used as an exposure to sleep disorders. G47 refers to “organic sleep disorders,” classified under diseases of the nervous system, encompassing a wide range of conditions affecting sleep rhythms, including insomnia, hypersomnia disorders, sleep-wake rhythm disorders, and sleep apnea, among others. F51 refers to “nonorganic sleep disorders,” which are sleep disorders not due to a substance or known physiological condition. It is classified under mental and behavioral disorders, including sleepwalking, night terrors, nightmares, and other related conditions.
Complete sleep factor data [Category 100057 (ox.ac.uk)] were collected via the touchscreen questionnaire during the initial assessment visit when participants were recruited. This included information on sleep duration (Field ID: 1160), getting up in morning (Field ID: 1170), chronotype (Field ID: 1180), daytime napping (Field ID: 1190), snoring (Field ID: 1210), and daytime dozing (Field ID: 1220). In line with previous research, sleep duration was categorized as “normal sleep” (7–8 h per day), “mild short sleep” (6 h per day), “moderate short sleep” (5 h per day), “extreme short sleep” (<5 h per day), and “excessive sleep” (>8 h per day) [11]. Getting up in morning was categorized as “not at all easy,” “not very easy,” “fairly easy,” and “very easy.” Chronotype preference was grouped as “definitely a morning person,” “more a morning than evening person,” “more an evening than a morning person,” and “definitely an evening person.” Daytime napping and daytime dozing were both categorized as “never/rarely,” “sometimes,” and “usually.” Snoring was grouped as “Yes” and “No.” Full descriptions for each field can be found on the UK Biobank website.
For accelerometer data, preprocessing was conducted by the UK Biobank accelerometer expert working group [9]. Details of accelerometer data collection and preprocessing can be found at Resource 131600 (ox.ac.uk). Sleep and wake times were obtained based on the average proportion of time spent sleeping per hour over the day (Field ID: 40030), and nighttime sleep duration was calculated accordingly.
Outcomes
The incidence of ALS-FTSD was defined as the earliest occurrence of either ALS or FTD event, with a censored date of June 1, 2023. Specifically, the diagnosis of ALS was based on the ICD-10 code G12.2. ALS incidence data comprised the date of ALS report and the source of ALS report, primarily from hospital admission and self-report. Similarly, FTD diagnosis was established using the ICD-10 code G31.0.
Covariates
To reduce potential confounding and according to previous summary [2], a broad range of covariates including sociodemographic, anthropometric, and lifestyle factors were considered. These included age (continuous), sex (male/female), ethnicity (white/non-white), smoking status (never/previous/current), alcohol drinking status (never/previous/current), coffee drinking (quartiles), body mass index (BMI) (<25/ ≥ 25), physical activity (quartiles), and townsend deprivation index (quartiles). The townsend deprivation index was utilized to categorize socioeconomic status based on national census data corresponding to each postal code area.
Statistical analysis
Participant baseline characteristics were presented as means ± SD or medians (interquartile range) for continuous variables and as percentages for categorical variables. Basic characteristics were compared across groups using ANOVA for normally distributed continuous variables, rank-sum tests for skewed variables, and χ² tests for categorical variables. A two-sided p value of less than 0.05 was considered to indicate statistical significance.
Two Cox proportional hazards models were employed to assess the association between sleep factors and the risk of ALS-FTSD incidence, quantified by hazard ratios (HRs) and 95% confidence intervals (CIs). Model 1 was adjusted for age, sex, and ethnicity. Model 2, built upon Model 1, further adjusted for smoking status, alcohol drinking status, coffee drinking, body mass index, physical activity, townsend deprivation index, anxiety and depression. Furthermore, in the analysis of sleep duration subgroups, considering the low number of outcome events, we applied Firth’s penalized partial likelihood correction to the Cox regression models [12]. The proportional hazards assumption was evaluated for each covariate by examining the correlation between the corresponding set of scaled Schoenfeld residuals and time, and testing for the independence between residuals and time. A global test was conducted for the entire model, and no variables analyzed violated the assumption of independence.
To ensure the robustness of the results and provide more targeted insights for medical decision-making in specific populations, a series of subgroup and sensitivity analyses were performed. Subgroup analyses were stratified by age (<60 or ≥60 years) and sex (male or female). Sensitivity analyses included: (1) limiting the analysis to those who developed ALS or FTD after a 3-year follow-up from baseline; (2) restricting participants to those with device-measured accelerometer data; and (3) defining exposure factors according to specific subcategories within the G47 diagnosis, including insomnia (G47.0), hypersomnia (G47.1), circadian rhythm sleep disorders (G47.2), sleep apnea (G47.3), narcolepsy and cataplexy (G47.4). All subgroup and sensitivity analyses were fully adjusted for confounding factors using the Model 2 as in the main analysis.
Results
Baseline characteristics
During a total follow-up period of 5398,084 person-years (median follow-up of 13.6 years), 633 incident ALS-FTSD events were recorded, comprising 458 cases of ALS, 194 cases of FTD, and 19 cases diagnosed with both ALS and FTD. Over 95% of ALS-FTSD diagnoses were derived from hospital records, a method supported by high diagnostic accuracy in previous studies [13]. Table 1 presents the baseline characteristics of the study participants. The mean age of the 396,918 participants was 56.31 ± 8.12 years, with 47.5% being men. Individuals who developed ALS-FTSD tended to be older, had a higher proportion of males, and experienced greater exposure to sleep disorders.
Sleep and incident ALS-FTSD
After adjusting for multiple covariates in Models 1 and 2, the association between sleep-related exposures and the risk of ALS, FTD, and ALS-FTSD were depicted in Table 2. In both models, G47 (organic sleep disorders) was consistently and significantly associated with an increased risk of ALS (Model 2: HR: 2.11, 95% CI: 1.34, 3.32, P = 0.001) and ALS-FTSD (Model 2: HR: 1.81, 95% CI: 1.21, 2.72, P = 0.004). Conversely, no association was observed between F51 (nonorganic sleep disorders) and the incidence of ALS, FTD, or ALS-FTSD. The combined results of G47 and F51 further underscored the adverse effect of organic sleep disorders on ALS-FTSD.
In the analysis of sleep duration, extreme short sleep (<5 h per day) was associated with an approximately twofold higher risk of ALS (Model 2: HR: 2.59, 95% CI: 1.30, 5.16, P = 0.018) and ALS-FTSD (Model 2: HR: 2.09, 95% CI: 1.09, 3.99, P = 0.046). There was a trend toward an increased risk for FTD, although it did not reach statistical significance. Meanwhile, excessive sleep (>8 h per day) was associated with an increased risk of FTD (Model 1: HR: 1.66, 95% CI: 1.02, 2.68, P = 0.041), but no significant association was observed with the incidence of ALS or ALS-FTSD. When sleep duration was analyzed as a continuous variable, an increase in sleep duration was associated with a higher risk of FTD (Model 2: HR, 1.15; 95% CI, 1.01–1.32; P = 0.045). No significant association was found between mild short sleep (6 h per day) or moderate short sleep (5 h per day) and the incidence of ALS-FTSD.
Additionally, waking up fairly easy or very easy in the morning was found to be a protective factor against ALS and ALS-FTSD, with the most significant protective effect observed in individuals with ALS-FTSD, the largest sample size group. Generally, waking up easily in the morning suggests good and adequate sleep, which aligns with the analysis results of sleep duration to some extent. In the main analyses, no statistically significant associations were observed between chronotype, daytime napping, daytime dozing, or snoring, and the risk of ALS, FTD, or ALS-FTSD.
Subgroup analyses across different age and sex
Subgroup analysis results revealed variations in the effects of sleep exposure across specific age or sex groups (Fig. 2), highlighting disparities within these demographic categories. Analysis by age showed a significant association between G47 diagnosis and ALS or ALS-FTSD in both individuals <60 and ≥60 years old, with a stronger risk effect seen in the <60 years group (Fig. 2A). Remarkably, extreme short sleep was significantly associated with an increased risk of ALS, FTD, and ALS-FTSD in individuals <60 years old, but not in those ≥60 years old. Sex-specific subgroup analyses revealed that a G47 diagnosis was significantly associated with an increased risk of ALS or ALS-FTSD in males, whereas this association did not reach statistical significance in females (Fig. 2B).
Sensitivity analyses
The association between G47 diagnoses and sleep duration with ALS-FTSD remained robust across several sensitivity analyses. In the analysis of individuals who developed ALS-FTSD after 3 years of baseline follow-up, G47 diagnoses were consistently associated with a increased risk of ALS (HR: 2.23, 95% CI: 1.38, 3.60, P = 0.001) and ALS-FTSD (HR: 1.80, 95% CI: 1.17, 2.77, P = 0.007) (Supplementary Table 2). The results indicated that G47 diagnoses might have a stably adverse effect on ALS-FTSD, approximately doubling the risk of developing ALS-FTSD.
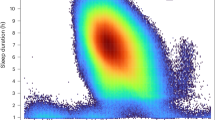
Analysis of accelerometer data from wrist-worn devices recording sleep duration revealed that extreme short sleep was significantly associated with an increased risk of FTD (HR: 46.35, 95% CI: 5.93, 362.52, P = 0.005), and ALS-FTSD (HR: 9.71, 95% CI: 1.79, 52.63, P = 0.045). This finding supported and complemented the primary analysis, emphasizing that extreme short sleep of less than 5 h per day was a strong risk factor for ALS-FTSD (Fig. 3).
A Main analysis, sleep duration derived from questionnaires. B Sensitivity analyses, sleep duration derived from device-measured accelerometer data. The Firth’s penalized partial likelihood method was applied for correction. The bubble area represents the value of hazard ratio (HR). Sleep duration was categorized as “normal sleep” (7–8 h per day), “mild short sleep” (6 h per day), “moderate short sleep” (5 h per day), “extreme short sleep” (<5 h per day), and “excessive sleep” (>8 h per day). ALS amyotrophic lateral sclerosis, ALS-FTSD amyotrophic lateral sclerosis-frontotemporal spectrum disorder, FTD frontotemporal dementia.
Further analysis of specific subcategories of G47 diagnoses indicated that hypersomnia (G47.1) was significantly associated with an increased risk of ALS (HR: 26.54, 95% CI: 3.70, 190.39, P = 0.001), FTD (HR: 51.24, 95% CI: 7.17, 366.15, P < 0.001), and ALS-FTSD (HR: 36.53, 95% CI: 9.04, 147.55, P < 0.001). No significant associations were identified between insomnia (G47.0), circadian rhythm sleep disorders (G47.2), sleep apnea (G47.3), or narcolepsy and cataplexy (G47.4) and ALS-FTSD (Supplementary Table 3). Notably, no cases were diagnosed with G47.0, G47.2, or G47.4 before the onset of ALS-FTSD. This observation may be attributed to the fact that diagnosis of these sleep disorders requires assessment by sleep specialists, whereas many clinicians tend to diagnose a broader spectrum of organic sleep disorders, categorized as G47. Moreover, while insomnia and reduced sleep duration are closely related, insomnia should not be equated with extreme short sleep. Overall, the sensitivity analysis of G47 subcategories indicates that a diagnosis of hypersomnia is significantly associated with an increased risk of ALS, FTD, and ALS-FTSD.
Discussion
Based on a prospective cohort design involving 396,918 individuals from the UK Biobank, we investigated the relationship between sleep-related factors and the risk of incident ALS-FTSD for the first time. After thoroughly adjusting for confounding factors, our findings showed that organic sleep disorders (G47), particularly hypersomnia (G47.1), significantly elevated the risk of ALS-FTSD. Analyses of both self-reported and device-measured sleep data indicated that sleep duration substantially impacts ALS-FTSD risk. Extreme short sleep approximately doubled the risk of ALS-FTSD, excessive sleep also tended to be associated with an increased risk. Overall, we identified a U-shaped relationship between sleep duration and the onset risk of ALS-FTSD, where both insufficient and excessive sleep were associated with higher risk. This U-shaped association has been previously noted in studies examining sleep duration and various health outcomes, including all-cause mortality, cardiovascular disease, aging, and cognitive impairment [14,15,16].
Although poor sleep is increasingly recognized as a non-motor symptom of ALS [17], the association between sleep and ALS-FTSD has not been widely examined. Several cross-sectional studies have evaluated the profiles of sleep abnormalities in patients with ALS-FTSD [6,7,8]. Evidence suggested that the prevalence of sleep-wake disturbances was higher in both sporadic and familial ALS patients compared to healthy controls, manifesting as excessive daytime sleepiness and reduced sleep quality [6, 7]. Polysomnographic studies have also supported the presence of significant sleep abnormalities in ALS patients, as well as in asymptomatic carriers of the C9ORF72 and SOD1 mutations. [18, 19]. Furthermore, ALS patients with sleep disorders often experienced more severe physical, cognitive, and frontal behavior impairments, as well as more rapid deterioration of respiratory function [6, 20]. Similarly, Filardi et al. investigated disruptions in sleep and circadian rhythms among patients with behavioral variant FTD (bvFTD), noting longer sleep duration, lower sleep quality, and alterations in rest-activity rhythms [8]. They discovered that prolonged sleep duration in bvFTD was associated with reduced cortical thickness in frontal regions, indicating that sleep and circadian rhythm disturbances could serve as early markers of neurodegeneration [8]. Although Mendelian randomization studies have pointed a causal link between excessive daytime sleepiness and increased ALS risk [21, 22], the predictive role of sleep disorders in the onset of ALS-FTSD remained unexplored in real-world studies. Therefore, our analysis on a large longitudinal cohort provided higher-level and comprehensive evidence for the correlation between sleep and ALS-FTSD. Sleep-related factors such as organic sleep disorders (G47), hypersomnia (G47.1), and extreme short sleep were identified as shared risk factors for ALS and FTD, supporting the concept of ALS-FTSD as a spectrum of disorders. Moreover, sleep disorders might have a more pronounced effect on the risk of ALS-FTSD in males, aligning with the epidemiological characteristics of ALS, where males were more susceptible than females [2]. Our findings might offer new perspectives on the etiology and treatment of ALS-FTSD.
The pathophysiological mechanisms linking sleep disturbances with neurodegenerative diseases are multifaceted. These mechanisms have been extensively explored in AD and PD, but research on ALS-FTSD remains relatively limited [5]. Sleep disturbances might increase the risk of ALS-FTSD by accelerating the biological aging process [15], as aging is a primary risk factor for most neurodegenerative diseases [23]. Additionally, neuroinflammation has emerged as a critical mediator in the link between sleep disruptions and neurodegeneration [24]. Sleep deprivation or poor-quality sleep has been shown to exacerbate systemic and central nervous system inflammation, leading to the upregulation of multiple pro-inflammatory cytokines and the accumulation of circulating neutrophils [25, 26]. This inflammatory state promotes microglial activation [25], which may trigger neuroinflammatory responses that contribute to motor neuron degeneration in ALS [27].
Sleep plays a crucial role in the brain’s clearance of metabolic waste [28]. In ALS, research had shown that sleep disturbances in early-stage ALS patients were significantly correlated with glymphatic dysfunction [29], which was central to the relationship between sleep, protein clearance, and neurodegenerative diseases [30, 31]. Evidence from both population and animal studies supported that sleep deprivation disrupted brain clearance mechanisms, impeding the removal of pathological proteins such as amyloid-β and tau, thereby exacerbating the pathological burden of neurodegenerative diseases [32, 33]. However, the impact of sleep on the metabolic dynamics and mechanisms of TAR DNA-binding protein 43 (TDP-43)—the primary pathological protein in ALS-FTSD—remains to be elucidated in future research. Notably, although ALS and FTD are classified within the same disease spectrum, the prevalence of TDP-43 pathology differs significantly: approximately 97% of ALS cases exhibit TDP-43 pathology, compared with only 45% of FTD cases [34]. This overlap and divergence in pathology may partly explain why the effects of sleep disturbances on ALS and FTD were not identical in this study. Specifically, in the main analysis, insufficient sleep was associated with an increased risk of ALS and ALS-FTSD but not FTD, while excessive sleep was linked to a higher risk of FTD, with no significant impact on ALS or ALS-FTSD. A similar U-shaped relationship between sleep duration and dementia incidence has been reported previously [35]. As a subtype of dementia, FTD exhibits tau pathology in approximately 45% of cases [34]. Thus, insufficient or excessive sleep duration may have distinct effects on different pathological proteins. Overall, when investigating the influence of sleep on ALS-FTSD, specific pathological inclusions should not be overlooked.
In fact, the relationship between sleep and neurodegenerative diseases is sophisticated and bidirectional [5]. In addition to sleep disturbances promoting the development and progression of neurodegenerative diseases, central nervous system changes associated with neurodegeneration may form the physiological basis of sleep disorders. The hypothalamus, a critical brain region for regulating the sleep-wake cycle, exhibited distinct involvement in ALS-FTSD patients, as indicated by converging neuropathological and neuroimaging findings [36,37,38,39,40,41]. This involvement is primarily characterized by widespread volume atrophy, particularly in the paraventricular nucleus [37], fornix [37], superior tuberal region [38], and anterior and posterior areas [39, 40]. Similar patterns of hypothalamic atrophy have been observed even in presymptomatic ALS mutation carriers [40]. Additionally, hypothalamic involvement is also marked by reduced white matter integrity [41], and widespread presence of TDP-43 inclusions [37]. Furthermore, Dedeene et al. performed histological examinations of hypothalamic neurons associated with the circadian sleep/wake cycle in C9orf72-related ALS-FTSD cases and observed abundant dipeptide repeat protein pathology [42]. Interestingly, animal studies have revealed varying degrees of sleep dysregulation in TDP-43 Drosophila [43,44,45], C9orf72 Drosophila [46], TDP-43 deficient mice [47], and FUS gene mutation knock-in rats [48]. Especially, TDP-43 showed robust circadian rhythmicity and was identified as a clock protein involved in circadian regulation [45, 47]. Both overexpression and knockdown of TDP-43 impaired circadian rhythms [45, 47]. Collectively, sleep disturbances may be the consequence of hypothalamic dysfunction and TDP-43 pathology in ALS-FTSD patients. Our findings that sleep disorders were associated with an increased risk of ALS-FTSD implied that sleep disturbances may serve as an early marker of neurodegeneration in the preclinical phase of ALS-FTSD.
The current study has several limitations. Firstly, neither sleep exposure nor ALS-FTSD outcome misclassification can be excluded from our analysis. Although diagnoses based on hospitalization records are considered highly reliable, they may likely capture only the most severe and typical cases of sleep disorders. Secondly, for the analysis of sleep duration, the primary data were derived from questionnaires, which might be subject to recall bias. While accelerometer data provided more objective and precise sleep measurements, the sample size with such data is limited. Thirdly, in the epidemiological studies, the time of first symptom onset is most relevant; however, we only collected diagnosis time for ALS-FTSD and lack detailed onset information. Thus, future studies are warranted to elucidate the relevance of sleep-related factors for disease onset, which would provide more appropriate insights. Finally, due to limitations in the available data, we were unable to analyze the specific relationship between sleep and early cognitive impairment in ALS-FTD. Exploring this relationship between sleep, cognition, and ALS-FTD remains an important direction for future research.
In conclusion, we conducted the largest population-based prospective cohort study and found that organic sleep disorders (G47), especially hypersomnia (G47.1), were significantly associated with an increased risk of ALS-FTSD. Additionally, sleep duration of less than 5 h per day was linked with a higher risk of ALS-FTSD. These findings support the notion that sleep interventions may represent important modifiable risk factors for ALS-FTSD and provide valuable insights into the potential pathogenesis of the disease.
Data availability
The data supporting the findings of this study are available on the UK Biobank project site and are subject to successful registration and application processes. Further details are available at https://www.ukbiobank.ac.
References
Strong MJ, Abrahams S, Goldstein LH, Woolley S, McLaughlin P, Snowden J, et al. Amyotrophic lateral sclerosis - frontotemporal spectrum disorder (ALS-FTSD): revised diagnostic criteria. Amyotroph Lateral Scler Frontotemporal Degener. 2017;18:153–74.
Feldman EL, Goutman SA, Petri S, Mazzini L, Savelieff MG, Shaw PJ, et al. Amyotrophic lateral sclerosis. Lancet. 2022;400:1363–80.
Huang LY, Ou YN, Yang YX, Wang ZT, Tan L, Yu JT. Associations of cardiovascular risk factors and lifestyle behaviors with neurodegenerative disease: a Mendelian randomization study. Transl Psychiatry. 2023;13:267.
Yang T, Xiao Y, Cheng Y, Huang J, Wei Q, Li C, et al. Epigenetic clocks in neurodegenerative diseases: a systematic review. J Neurol Neurosurg Psychiatry. 2023;94:1064–70.
Shen Y, Lv QK, Xie WY, Gong SY, Zhuang S, Liu JY, et al. Circadian disruption and sleep disorders in neurodegeneration. Transl Neurodegener. 2023;12:8.
Liu S, Huang Y, Tai H, Zhang K, Wang Z, Shen D, et al. Excessive daytime sleepiness in Chinese patients with sporadic amyotrophic lateral sclerosis and its association with cognitive and behavioural impairments. J Neurol Neurosurg Psychiatry. 2018;89:1038–43.
Sun X, Zhao X, Liu Q, Liu S, Zhang K, Wang ZL, et al. Study on sleep-wake disorders in patients with genetic and non-genetic amyotrophic lateral sclerosis. J Neurol Neurosurg Psychiatry. 2021;92:96–102.
Filardi M, Gnoni V, Tamburrino L, Nigro S, Urso D, Vilella D, et al. Sleep and circadian rhythm disruptions in behavioral variant frontotemporal dementia. Alzheimers Dement. 2024;20:1966–77.
Doherty A, Jackson D, Hammerla N, Plotz T, Olivier P, Granat MH, et al. Large scale population assessment of physical activity using wrist worn accelerometers: the UK biobank study. PLoS ONE. 2017;12:e0169649.
Sudlow C, Gallacher J, Allen N, Beral V, Burton P, Danesh J, et al. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 2015;12:e1001779.
Nôga DA, Meth E, Pacheco AP, Tan X, Cedernaes J, van Egmond LT, et al. Habitual short sleep duration, diet, and development of type 2 diabetes in adults. JAMA Netw Open. 2024;7:e241147.
Firth D. Bias reduction of maximum likelihood estimates. Biometrika. 1993;80:27–38.
Horrocks S, Wilkinson T, Schnier C, Ly A, Woodfield R, Rannikmae K, et al. Accuracy of routinely-collected healthcare data for identifying motor neurone disease cases: a systematic review. PLoS ONE. 2017;12:e0172639.
Svensson T, Saito E, Svensson AK, Melander O, Orho-Melander M, Mimura M, et al. Association of sleep duration with all- and major-cause mortality among adults in Japan, China, Singapore, and Korea. JAMA Netw Open. 2021;4:e2122837.
Wang X, Yan X, Li M, Cheng L, Qi X, Zhang J, et al. U-shaped association between sleep duration and biological aging: evidence from the UK biobank study. Aging Cell. 2024;23:e14159.
Ma Y, Liang L, Zheng F, Shi L, Zhong B, Xie W. Association between sleep duration and cognitive decline. JAMA Netw Open. 2020;3:e2013573.
Beswick E, Forbes D, Johnson M, Newton J, Dakin R, Glasmcher S, et al. Non-motor symptoms in motor neuron disease: prevalence, assessment and impact. Brain Commun. 2024;6:fcad336.
Guillot SJ, Lang C, Simonot M, Beckett D, Lul‚ D, Balz LT, et al. Early-onset sleep alterations found in patients with amyotrophic lateral sclerosis are ameliorated by orexin antagonist in mouse models. Sci Transl Med. 2025;17:eadm7580.
Zhang Y, Ren R, Yang L, Nie Y, Zhang H, Shi Y, et al. Sleep in amyotrophic lateral sclerosis: a systematic review and meta-analysis of polysomnographic findings. Sleep Med. 2023;107:116–25.
Li X, Liu Q, Niu T, Jia H, Liu T, Xin Z, et al. Sleep disturbances as a potential risk factor for deterioration of respiratory function in patients with amyotrophic lateral sclerosis. Ann Indian Acad Neurol. 2023;26:754–60.
Zhang G, Zhang L, Xia K, Zhuang Z, Huang T, Fan D. Daytime sleepiness might increase the risk of ALS: a 2-sample Mendelian randomization study. J Neurol. 2021;268:4332–9.
Di H, Zhu Y, Xia W, Meng X, Zhang M, Xu M, et al. Bidirectional Mendelian randomization to explore the causal relationships between sleep traits, Parkinson’s disease and Amyotrophic lateral sclerosis. Sleep Med. 2022;96:42–9.
Hou Y, Dan X, Babbar M, Wei Y, Hasselbalch SG, Croteau DL, et al. Ageing as a risk factor for neurodegenerative disease. Nat Rev Neurol. 2019;15:565–81.
Gudkov SV, Burmistrov DE, Kondakova EV, Sarimov RM, Yarkov RS, Franceschi C, et al. An emerging role of astrocytes in aging/neuroinflammation and gut-brain axis with consequences on sleep and sleep disorders. Ageing Res Rev. 2023;83:101775.
Irwin MR. Sleep and inflammation: partners in sickness and in health. Nat Rev Immunol. 2019;19:702–15.
Sang D, Lin K, Yang Y, Ran G, Li B, Chen C, et al. Prolonged sleep deprivation induces a cytokine-storm-like syndrome in mammals. Cell. 2023;186:5500–16 e5521.
Mifflin L, Hu Z, Dufort C, Hession CC, Walker AJ, Niu K, et al. A RIPK1-regulated inflammatory microglial state in amyotrophic lateral sclerosis. Proc Natl Acad Sci USA. 2021;118:e2025102118.
Jiang-Xie LF, Drieu A, Bhasiin K, Quintero D, Smirnov I, Kipnis J. Neuronal dynamics direct cerebrospinal fluid perfusion and brain clearance. Nature. 2024;627:157–64.
Liu S, Sun X, Ren Q, Chen Y, Dai T, Yang Y, et al. Glymphatic dysfunction in patients with early-stage amyotrophic lateral sclerosis. Brain. 2024;147:100–8.
Eisen A, Nedergaard M, Gray E, Kiernan MC. The glymphatic system and amyotrophic lateral sclerosis. Prog Neurobiol. 2024;234:102571.
Nedergaard M, Goldman SA. Glymphatic failure as a final common pathway to dementia. Science. 2020;370:50–6.
Liu H, Barthelemy NR, Ovod V, Bollinger JG, He Y, Chahin SL, et al. Acute sleep loss decreases CSF-to-blood clearance of Alzheimer’s disease biomarkers. Alzheimers Dement. 2023;19:3055–64.
Parhizkar S, Gent G, Chen Y, Rensing N, Gratuze M, Strout G, et al. Sleep deprivation exacerbates microglial reactivity and abeta deposition in a TREM2-dependent manner in mice. Sci Transl Med. 2023;15:eade6285.
Ling SC, Polymenidou M, Cleveland DW. Converging mechanisms in ALS and FTD: disrupted RNA and protein homeostasis. Neuron. 2013;79:416–38.
Liang Y, Qu LB, Liu H. Non-linear associations between sleep duration and the risks of mild cognitive impairment/dementia and cognitive decline: a dose-response meta-analysis of observational studies. Aging Clin Exp Res. 2019;31:309–20.
Gnoni V, Zoccolella S, Giugno A, Urso D, Tamburrino L, Filardi M, et al. Hypothalamus and amyotrophic lateral sclerosis: potential implications in sleep disorders. Front Aging Neurosci. 2023;15:1193483.
Gabery S, Ahmed RM, Caga J, Kiernan MC, Halliday GM, Petersén Å. Loss of the metabolism and sleep regulating neuronal populations expressing orexin and oxytocin in the hypothalamus in amyotrophic lateral sclerosis. Neuropathol Appl Neurobiol. 2021;47:979–89.
Tse NY, Bocchetta M, Todd EG, Devenney EM, Tu S, Caga J, et al. Distinct hypothalamic involvement in the amyotrophic lateral sclerosis-frontotemporal dementia spectrum. Neuroimage Clin. 2023;37:103281.
Shapiro NL, Todd EG, Billot B, Cash DM, Iglesias JE, Warren JD, et al. In vivo hypothalamic regional volumetry across the frontotemporal dementia spectrum. Neuroimage Clin. 2022;35:103084.
Gorges M, Vercruysse P, Müller HP, Huppertz HJ, Rosenbohm A, Nagel G, et al. Hypothalamic atrophy is related to body mass index and age at onset in amyotrophic lateral sclerosis. J Neurol Neurosurg Psychiatry. 2017;88:1033–41.
Li X, Liu Q, Niu T, Liu T, Xin Z, Zhou X, et al. Sleep disorders and white matter integrity in patients with sporadic amyotrophic lateral sclerosis. Sleep Med. 2023;109:170–80.
Dedeene L, Van Schoor E, Vandenberghe R, Van Damme P, Poesen K, Thal DR. Circadian sleep/wake-associated cells show dipeptide repeat protein aggregates in C9orf72-related ALS and FTLD cases. Acta Neuropathol Commun. 2019;7:189.
Maccioni R, Setzu MD, Talani G, Solari P, Kasture A, Sucic S, et al. Standardized phytotherapic extracts rescue anomalous locomotion and electrophysiological responses of TDP-43 Drosophila melanogaster model of ALS. Sci Rep. 2018;8:16002.
Godfrey RK, Alsop E, Bjork RT, Chauhan BS, Ruvalcaba HC, Antone J, et al. Modelling TDP-43 proteinopathy in Drosophila uncovers shared and neuron-specific targets across ALS and FTD relevant circuits. Acta Neuropathol Commun. 2023;11:168.
Perlegos AE, Durkin J, Belfer SJ, Rodriguez A, Shcherbakova O, Park K, et al. TDP-43 impairs sleep in Drosophila through Ataxin-2-dependent metabolic disturbance. Sci Adv. 2024;10:eadj4457.
Uy G, Farrell LN, Faheem SF, Kinne LE, Adore MG, Im SH, et al. The effects of poly-GA and poly-PR C9orf72 dipeptide repeats on sleep patterns in Drosophila melanogaster. MicroPubl Biol. 2024; https://doi.org/10.17912/micropub.biology.000973.
Zhang H, Chen C, Zhang EE, Huang X. TDP-43 deficiency in suprachiasmatic nucleus perturbs rhythmicity of neuroactivity in prefrontal cortex. iScience. 2024;27:109522.
Zhang T, Jiang X, Xu M, Wang H, Sang X, Qin M, et al. Sleep and circadian abnormalities precede cognitive deficits in R521C FUS knockin rats. Neurobiol Aging. 2018;72:159–70.
Acknowledgements
This research was conducted using the UK Biobank Resource under Application 98992. This work uses data provided by patients and collected by the NHS as part of their care and support. We would like to express our sincere gratitude to the participants of the UK Biobank and the members of the survey, development, and management teams involved in this project.
Funding
This study was supported by the National Natural Science Foundation of China (Grant No. 82371430), the Sichuan Science and Technology Program (Grant No. 2022ZDZX0023), and National Clinical Research Center for Geriatrics, West China Hospital, Sichuan University (Z2024JC004).
Author information
Authors and Affiliations
Contributions
TMY, DJP, JXH, YX and HFS contributed to the conception and design of the study. TMY, DJP, JXH, YX, CYL, and QQW organized the datasets. TMY, DJP, JXH, YX, and CYL performed the statistical analysis. TMY, DJP, and HFS wrote the manuscript. All authors contributed to manuscript revision and read and approved the submitted version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
Ethical approval for the UK Biobank study was obtained from the North West Multi-centre Research Ethics Committee (11/NW/03820).
Consent to participate
All participants provided written informed consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yang, T., Pang, D., Huang, J. et al. Association between sleep and ALS-FTSD: A Prospective Cohort Study based on 396,918 UK biobank participants. Transl Psychiatry 15, 123 (2025). https://doi.org/10.1038/s41398-025-03328-0
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41398-025-03328-0