Abstract
Impulsivity, increasingly perceived as a transdiagnostic characteristic, significantly influences diverse psychiatric conditions and emanates beyond the boundaries defined by traditional classification systems. Transdiagnostic research has shed light on the complex clinical manifestations of impulsivity, and the underpinning neural circuitry. The pressing challenge now is to translate this enhanced understanding into precise and potent interventions tailored to these different aspects of impulsivity. Recent advancements in neuromodulation, specifically targeting brain circuits, have provided encouraging evidence for improvements in clinical symptoms, and neural circuitry across various psychiatric conditions, signposting a transformative phase in crafting interventions that tackle impulsivity from a transdiagnostic perspective. However, the field continues to ascertain a universally embraced framework that effectively amalgamates these discoveries into a unified clinical methodology. The Research Domain Criteria (RDoC) delivers a neuroscientifically informed framework that aims to reconcile the neurobiological underpinnings with clinical symptoms, thereby facilitating targeted neuromodulation strategies. In this context, we propose a pioneering RDoC-compliant framework that strategically targets the neural circuits implicated in clinical impulsivity symptoms, applicable across diagnostic categories. Furthermore, we introduce a set of meticulously selected tools for each stage within this framework, thus reinforcing its applicability and aiding future investigative pursuits in this area.
Similar content being viewed by others
Introduction
Impulsivity, historically conceptualised as a predisposition toward immediate, undeliberated responses to stimuli without regard for consequences, has evolved beyond traditional unidimensional models through the transdiagnostic lens of modern psychiatry [1,2,3]. This multidimensional construct, encompassing trait-level neurocognitive vulnerabilities and state-dependent behavioural disinhibition, operates across conventional diagnostic boundaries delineated in DSM-5 and ICD-11. Its role as a transdiagnostic nexus spans neurodevelopmental disorders (e.g., attention-deficit/hyperactivity disorder [ADHD] [4]), addictive behaviours (e.g., substance use [5,6,7], gambling [8]), and self-regulatory pathologies (e.g., non-suicidal self-injury [9], eating disorders [10]). Epidemiological data (e.g., the National Impulsivity Survey, N = 34,653 U.S. adults) indicate a population prevalence of 17.2% for clinically significant impulsivity [11]. Moreover, impulsivity severity demonstrates dose-dependent associations with psychopathological complexity, including its role in mediating the transition from suicidal ideation to attempt [12]. These findings collectively position impulsivity not as an epiphenomenal symptom, but as a pathogenic nexus interfacing neurocognitive circuits (ventral striatal reward processing, prefrontal inhibitory control) and maladaptive behavioral repertoires. Hence, there is a growing proposition for assessments and interventions targeting impulsivity across transdiagnostic dimensions of psychopathology [3, 13,14,15,16].
The endeavour of transdiagnostic research into impulsivity is galvanised by the recognition that a multitude of psychiatric maladies manifest a constellation of consistent symptoms [17] and share neurocognitive underpinnings [18, 19]. Advocacy for a reconceptualisation in the diagnostic, therapeutic, and preventative paradigms of mental disorders has surged, predicated upon the identification of shared undercurrents and determinants [20, 21]. A focus on the transdiagnostic attributes of impulsivity promises the inception of more integrated and comprehensive treatment modalities, portending substantive clinical advancements and profound insights into the psychiatric domain. However, as will be elaborated subsequently, the prevailing research milieu of impulsivity is characterised by an assemblage of discrete models centred on specific facets of assessment and intervention, presenting considerable challenges in the clinical application of transdiagnostic interventions [22].
This review evaluates the present state of transdiagnostic interventions that target impulsivity, canvassing a spectrum of methodologies from clinical symptom assessment and neural circuitry analysis to nascent neuromodulation techniques. We scrutinise the challenges of heterogeneity within impulsivity, the collaborative potential of the Research Domain Criteria (RDoC) framework, and the imperative for cohesive transdiagnostic treatment models. Moreover, the exploration of propitious directions points towards the evolution from transdiagnostic assessments to interventions, predicated on neuromodulation therapies that reconcile psychopathological manifestations with their neurological correlates. Herein, we aspire to forge a research trajectory that reconciles the diverse splinters of impulsivity, shaping a unified investigative approach.
Current status of transdiagnostic impulsivity research
The imperative for a systematic framework to guide transdiagnostic research is underscored by the inherently interdisciplinary nature of this field, which demands integration of empirical evidence and theoretical insights across psychiatry, neuroscience, and psychology [22]. Frameworks aligned with the Research Domain Criteria (RDoC) illustrate this integrative approach: Rezapour et al.’s [20] categorised preventative interventions for substance use disorders using RDoC dimensions, while Yücel Oldenhof et al.‘s [23] established a neuropsychological assessment protocol for addiction phenotypes. Concurrently, Deng et al. [24] advanced device-based neuromodulation strategies targeting clinical symptoms-specific neurocircuitry, reflecting a broader pursuit of mechanistic unification. Despite these efforts, the literature remains fragmented, with no consensus on a cohesive framework for impulsivity interventions across diagnostic boundaries.
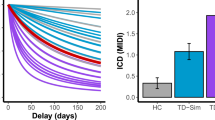
Comparative studies reveal heterogeneity in impulsivity manifestations across disorders, across disorders. While psychoneurobiological mechanisms (e.g., prefrontal-striatal dysregulation) are well-characterised, proposed assessments and interventions remain siloed within narrow diagnostic contexts. Current methodologies predominantly rely on subjective self-report tools measuring trait-level constructs (e.g., impulsiveness, risk-taking) and behavioural tendencies (e.g., delay-discounting), which exhibit transdiagnostic relevance in substance use, personality, and neurodevelopmental disorders [3, 14]. Objective behavioural tasks, such as Go/No-Go paradigms indexing adolescent addiction susceptibility, are increasingly validated as transdiagnostic markers [25]. Notably, discrepancies emerge when combining subjective reports with objective measures: self-assessed impulsivity often diverges from performance on inhibitory control tasks (e.g., stop-signal reaction times) [1]. However, emerging evidence indicates that a combination of complementary objective measures, such as behavioral assays, heart rate variability analysis, and fMRI - derived brain connectivity metrics, might jointly elucidate the dispersed pattern characteristic of multidimensional impulsivity [26]. This paves the way for forthcoming research endeavors to construct reliable impulsivity assessment tools applicable to diverse populations. Emerging interventions show context-dependent efficacy. Acceptance commitment therapy and mindfulness-based dialectical behaviour therapy reduce impulsivity in addictive disorders [27], whereas pharmacological agents like topiramate demonstrate inconsistent therapeutic profiles across diagnostic groups [16]. Despite progress in transdiagnostic evaluation [2, 13, 28, 29], the field lacks a unifying framework synthesising clinical phenotypes, neurocircuitry dysfunction, and therapeutic mechanisms. Existing research presents a fragmented evidence base, hampering clinical translation. To address this gap, a holistic approach - interlinking behavioural, neural, and intervention data - is essential for developing transcranial impulsivity management strategies grounded in mechanistic coherence.
A systematic synthesis of extant evidence across three pivotal domains - transdiagnostic dimensionality of psychological impulsivity (trait-state manifestations), neurobiological pathways (cortico-striatal-thalamic circuitry dysregulation), and intervention strategies (neuromodulation-behavioural synergies) - will facilitate the development of an integrative transdiagnostic framework. This framework aims to unify phenotypic heterogeneity, neural circuitopathies, and therapeutic mechanisms, thereby advancing precision psychiatry for impulsivity-related psychopathology.
Transdiagnostic dimensionality of psychological impulsivity
Impulsivity manifests in myriad forms, ranging from stable impulsive traits to transient responses and reward-driven choices observable across species. Accumulating evidence highlights the transdiagnostic co-morbidity of impulsivity across various mental disorders (see details in refs. [17, 19]). Briefly stated, impulsivity characterises attention-deficit/hyperactivity disorder through impaired behavioural inhibition and compromised delayed gratification [4], while within eating disorders, heightened food-related impulsivity propels binge-eating behaviours [10]. Functioning as both predisposing and maintenance element in addiction, impulsivity perpetuates substance-seeking behaviours along with consumption [5,6,7], extending to behavioural addictions including gambling and internet-related dependencies [8, 30]. This construct also correlates with non-suicidal self-injury, demonstrating parallels to the impulsivity observed in addictions, frequently originating from antecedents like childhood trauma [9, 31].
The construct of impulsivity exhibits both extensive and heterogeneous manifestations [19, 32,33,34]. Systematic deconstruction of its multi-dimensional components offers potential to reveal underlying psychopathological heterogeneity across diagnostic boundaries. Current empirical evidence supports dimensions that bifurcate psychological impulsivity into two primary domains: trait impulsivity and state impulsivity.
Trait impulsivity, conceptualised as a stable personality dimension, demonstrates transdiagnostic prevalence across mental disorders and has garnered substantial clinical relevance [2, 35, 36]. Functioning as a susceptibility marker for external stimuli, it maintains significant associations with severe psychological disorders [3, 28, 37]; emerging network methodologies further identify potential impulsivity subtypes within personality constructs [38]. The emotional impulsivity construct, representing affect-driven responses, is typically quantified through the urgency metrics in the UPPS-P model [39], underscoring its pathogenic role in conditions like substance dependence and binge eating [37, 39]. While critical, conventional trait impulsivity assessments primarily relying on self-report questionnaires demonstrate limited capacity to capture the dynamic nature and complexity of this construct [2, 14].
Conversely, state impulsivity, modulated by environmental contexts, interacts dynamically with disease progression and remission trajectories, serving as a severity marker [36, 40]. Clinical manifestations include premature actions and suboptimal decision-making [41], differentiated into impulsive choices versus motor impulsivity - the former assessed through delay discounting paradigms [42], and the latter measured via motor inhibition tasks evaluating response inhibition [43].
Current, theoretical deconstruction of impulsivity’s multifaceted nature has significantly enhanced conceptual understanding, yet clinical translation frequently results in oversimplification of this complexity. Scholarly consensus remains elusive regarding the separation or integration of impulsivity dimensions [2, 13, 36, 39, 44, 45], with some scholars advocating against impulsivity as a unified psychological construct due to its heterogeneous clinical manifestations and intricate interactions with psychological and cognitive dimensions [46]. This conceptual ambiguity persists due to the absence of unified clinical assessment protocols.
Although impulsivity is increasingly recognised as a multi-faceted construct, the field lacks consensus on operational definition and dimensional independence. The influential three-domain model proposed by MacKillop et al.‘s [44] – encompassing action/response/motor impulsivity, delay discounting-based choice impulsivity, and trait impulsivity - has gained empirical validation across psychiatric populations [37, 47, 48]. However, this categorisation faces methodological challenges, particularly the neurofunctional overlap between impulsive action and choice metrics [19]. Furthermore, the observed discordance between task-based state impulsivity measures and self-reported trait impulsivity [49, 50] may reflect underlying neural heterogeneity [51, 52], necessitating refinement of assessment paradigms such as sequential gambling tasks [53] and reconceptualisation of neural correlates for impulsivity sub-dimensions to establish reliable psychoneurophenotypes [19, 51].
Integrating these perspectives, we propose MacKillop’s model [44] as theoretical foundation for transdiagnostic assessment strategies (Fig. 1). This integrative model, incorporating both trait-state distinctions and cognitive-motor differentiations, provides a promising dimensional assessment approach, particularly for investigating neurobiological substrates of distinct impulsivity dimensions. Recent empirical advances demonstrate the feasibility of cross-diagnostic models integrating psychological and neural measures. For instance, emerging research identifies three neurobehaviourally distinct structural domains - stimulus-driven behavior, executive function, and negative affect - through phenotypic analysis of healthy and addicted populations, subsequently delineating subtypes with unique neurobehavioral profiles that may underlie addiction persistence [54].
Transdiagnostic neurobiological pathways of impulsivity
Ongoing animal and human neuroimaging studies endeavour to elucidate the complex neurobiology of impulsivity, with the ultimate goal of crafting nuanced therapeutic strategies. Key discoveries have pinpointed how impulsive conduct is governed by an intricate network encompassing the prefrontal cortex and its downstream effectors within the basal ganglia [19, 55]. Experimental inactivation of these neural components yields significant behavioural alterations, substantiating their role in impulsivity control [56, 57]. Within the prefrontal cortex, circuits within areas such as the infralimbic cortex [58], orbitofrontal cortex [59], and anterior cingulate cortex [60] have emerged as pivotal in driving and modulating impulsive actions, supported by gene expression profiles. The manipulation of excitatory or inhibitory pathways in these regions produces significant modulations in impulsive behaviours [56, 61], with targeted inhibition of prefrontal projections to the subthalamic nucleus attenuating impulsivity [56].
The basal ganglia’s role in impulsivity is underscored by its composition of interlinked nuclei that mediate behavioural inhibition [62]. Here, the direct and indirect pathways modulate activity within the substantia nigra pars reticulata and the globus pallidus externus, which in turn influences the subthalamic nucleus [63]. Moreover, the hyperdirect pathway facilitates rapid response inhibition within the basal ganglia, crucial for impulsivity regulation [64].
The NAc, a basal ganglia integral, orchestrates impulsive behaviours, integrating projections from regions such as the prefrontal cortex, insula, ventral hippocampus, and amygdala [65]. Dopaminergic signalling coupled with inhibitory mechanisms within the NAc is central to impulsivity modulation [66,67,68]. Within the ventral tegmental area, dopaminergic inputs to the NAc play a pivotal role, especially in mechanisms related to delay discounting—a process finely tuned in the ventral striatum [69]. Distinct regions within the NAc are shown to mediate disparate facets of impulsivity such as premature responses and delay discounting, but not inhibition of initiated responses [19].
Additional structures coordinating motor control, like the ventromedial thalamus [65], anterior lateral motor cortex [70], and the cerebellum [71], may also be implicated in impulsive behaviours. The ventromedial thalamus’s interconnection with the anterior lateral motor cortex, for instance, forms part of the thalamocortical pathway and may influence impulsivity through dendritic integration in motor cortex pyramidal neurons, as recent studies suggest [72,73,74].
The insula’s role, often underestimated, is critical in informed decision-making under uncertainty, integrating internal bodily states to influence conscious decisions. Its pertinence in addiction-related impulsivity is significant, where it contributes to craving and relapse decisions [75].
Comprehensive discourse is emerging about the meso-and macro-scale of human neural circuitry, especially regarding insights into patients’ self-reported impulsivity and behavioural presentations, which herald future groundbreaking intervention strategies [76]. The observation that disruptions to the network properties of the human brain are a common denominator across brain disorders suggests the presence of shared network mechanisms, pivotal for developing neuromodulation strategies [77]. Interventions aimed at these dysregulated networks offer a formidable approach to modulating behavioural and cognitive functions affected by impulsivity [24, 78,79,80]. This not only necessitates aligning neurological findings with clinical interventions [45] but is also crucial for the ongoing endeavour to pinpoint biomarkers indicative of intervention responses [76]. Using neurophysiological correlates of impulsivity, the RDoC framework may foster biomarkers predictive of intervention efficacy, enhancing diagnostic acuity, and personalised therapeutic paths [19, 20, 81]. Despite the potential variation in manifest impulsivity and the diverse brain circuits linked with impulsivity factors [2, 82], the interrelations to impulsive-related mental disorders predominantly revolve around these implicated brain circuits [17, 83]. Therefore, this comprehensive understanding not only sets the stage for identifying potential biomarkers but also propels the development of precision medicine strategies that can transcend diagnostic boundaries, thereby advancing clinical practice.
Transdiagnostic intervention strategies for impulsivity
The array of interventions targeting impulsivity encompasses pharmacotherapies [84, 85] and behavioural therapies [86], with cognitive-behavioural therapy occupying a prominent role [87]. Whereas pharmacotherapy modulates neurotransmitter dynamics, behavioural therapies focus on enhancing self-regulation capacities and decision-making competence. Nevertheless, their efficacy remains constrained to specific populations [86], attributable to inadequate targeting of neurobiological mechanisms underlying impulsivity, thereby limiting transdiagnostic applicability.
Significant progress in transdiagnostic psychiatric interventions has emerged from neuromodulation techniques. Non-invasive brain stimulation (NIBS) methods [24, 76, 78, 88] particularly transcranial magnetic stimulation (TMS) [89], represent an innovative frontier for addressing core neural substrates of transdiagnostic symptoms, including anhedonia, impulsivity, and cognitive deficits [90]. Notably, NIBS-mediated modulation of reward-related endophenotypes has demonstrated promising efficacy in alleviating anhedonia across psychiatric disorders [91], suggesting potential for unifying heterogeneous psychiatric conditions under cohesive therapeutic frameworks. Emerging evidence indicates low-frequency TMS effectively reduces state impulsivity [92], highlighting its target-specific and sustained therapeutic benefits.
Advanced neuromodulation therapies such as TMS, transcranial electrical stimulation, deep brain stimulation (DBS), and focused ultrasound are increasingly designed to modulate discrete neural circuits [78, 80, 93,94,95], offering transdiagnostic therapeutic potential through alignment between individual impulsivity profiles and intervention strategies [96]. Although current research has not yet achieved transformative paradigm shifts in transdiagnostic care, preliminary findings from novel interventions provide cautiously optimistic prospects. The future trajectory of these interventions depends on integrative incorporation of neuroimaging insights, patient-centred adaptations, and synergy with established therapies. While neuromodulation offers new avenues for addressing neurobiological aspects of impulsivity, the challenge of identifying universal neural targets persists, stemming from impulsivity’s phenotypic heterogeneity and inter-individual neuroanatomical variability [97].
Moving forward, systematic methodological frameworks are required to translate these innovative concepts into clinically viable interventions capable of transdiagnostically managing impulsivity. This paradigm shift may enable neuromodulation to complement conventional therapies, ultimately yielding personalised treatment modalities that harmonise neurobiological precision with clinical pragmatism.
Aligning transdiagnostic neuromodulation of impulsivity with the RDoC framework
The need for coherent transdiagnostic intervention models
Traditionally, categorising mental disorders has struggled to capture the complexity of conditions like impulsivity [22, 98]. For example, a data-driven study identified two subtypes of patients with high anxiety but distinct impulsivity levels [99], highlighting the need for transdiagnostic intervention targets over disorder-specific approaches. Evidence suggests that targeting specific neural circuits implicated in impulsivity could enable such interventions. For instance, Parkes et al. linked transdiagnostic variations in impulsivity to the effective connectivity of the cortico-striato-thalamo-cortical loop [100], while Lantrip et al. demonstrated that TMS enhances prefrontal and subcortical/limbic network functionality, likely promoting neuroplasticity and alleviating symptoms of PTSD and anxiety, including cognitive dysfunctions [101]. The RDoC framework, pioneered by the National Institute of Mental Health (NIMH), redefines mental disorders by focusing on observable behaviours and neurobiological attributes [20, 21]. It bypasses traditional diagnostic categories, emphasising fundamental dimensions or ‘constructs’ spanning multiple disorders. Impulsivity research aligns with RDoC’s transdiagnostic mechanistic constructs [18, 19, 23], mapping impulsivity onto these constructs across genetic, molecular, behavioural, and self-reported levels.
There’s a burgeoning agreement on the need for a framework that vaults over the confines of traditional diagnoses [93, 96]. Advocates of a transdiagnostic intervention approach in psychiatry propose a system transcending current categorical diagnoses, enhancing treatment effectiveness. Anchored in the RDoC framework, this approach harmonises symptomatology with neurobiological underpinnings and intervention strategies, encapsulating a nuanced perspective on mental disorders through biobehavioural lenses. Such an ethos equips researchers and clinicians to parse impulsivity’s multifarious aspects across different conditions, stimulating the genesis of precision-oriented, transdiagnostic therapeutic strategies. Thus, the RDoC framework’s promise of spawning robust diagnoses and evidence-driven interventions for impulsivity is intertwined with the trait’s symptomatic and neurobiological variances. It streamlines the discovery of pivotal neural circuits and physiological processes integral to impulsive behaviours, charting a course for standardised neuromodulation interventions.
Impulsivity’s heterogeneous portrayals across psychopathologies, its intricate intertwining with other symptoms, and variable treatment responses present considerable barriers to a unified treatment approach. Transdiagnostic assessments for impulsivity have seen refinements, with self-reports and behavioural measures offering insights into this variegated construct, fundamental to curating bespoke interventions. For instance, the work of Pearlstein et al. [13] serves as a conduit between transdiagnostic evaluations and ensuing interventions. Their focus on the interplay of emotion and impulsivity forges a pathway for tailor-made interventions targeting emotional inciters of impulsive conduct. These developments signal a shift from a blanket approach towards meticulous strategies marrying detailed psychological assessments with corresponding therapies, thus augmenting intervention efficacy for impulsivity-related disorders. Despite its recognised pertinence, interventions for impulsivity lack consensus, stalling transdiagnostic research ventures.
Navigating the journey from comprehension to effective transdiagnostic intervention in impulsivity is laden with obstacles. The alignment of assessment tools with intervention tactics is pivotal, as highlighted by Hook et al. [28]. The metamorphosis from theoretical research to actionable clinical remedies necessitates the continuous refinement of both diagnostic instruments and therapeutic methods, enabling a more profound grasp of impulsivity’s myriad expressions and paving the way for treatments that cater to individual needs across the mental health spectrum.
Synthesising brain circuitry of impulsivity with clinical symptoms and transdiagnostic neuromodulation
Exploring impulsivity within transdiagnostic psychiatry demands integrating neural circuitry insights with clinical manifestations [29, 45, 92, 102], a shift poised to redefine therapeutic paradigms. Central to this approach is the use of neuromodulation technologies to develop precise, patient-centric interventions [76, 78, 96].
Impulsive behaviour is primarily governed by interactions within the cortical-striatal-thalamic-cortical circuitry, particularly the frontostriatal circuits [19, 34]. Neuroimaging techniques, such as MRI, have been instrumental in identifying neuromodulation targets by mapping structural and functional abnormalities associated with impulsivity. These circuits are implicated in various conditions, including ADHD [103], heroin dependence [104], and cocaine addiction [105], where structural and functional disruptions correlate with heightened impulsivity. Aligning with the RDoC framework [19, 34, 55], these findings highlight the potential for transdiagnostic interventions. However, neuroimaging correlations alone do not guarantee clinical efficacy, necessitating further exploration of intervention strategies across mental disorders [106].
Lesion network mapping provides a powerful approach to identifying intervention targets by revealing consistent neural signatures linked to impulsive behaviours. Integrating techniques such as TMS with lesion studies further validates these targets across brain circuits [107]. The complementary use of these modalities allows for fine-tuned circuit modulation [108]. Notably, disruptions induced by neuromodulation can yield significant behavioural changes, underscoring its role in impulsivity regulation [56, 57]. For instance, weight gain following subthalamic nucleus DBS has been associated with increased reward sensitivity and impulsivity [109]. Neuromodulation’s capacity to induce neuroplastic changes within these circuits highlights its potential to bridge clinical symptoms with modifiable neural pathways [78, 88]. However, establishing the feasibility of such approaches across disorders requires robust clinical evidence [78].
Mapping individual brain circuit topographies remains a complex endeavour. Efforts are underway to optimise brain mapping techniques for precise target identification, with a growing emphasis on enhancing predictive value for clinical outcomes [110]. Pre-intervention MRI, which assesses connectivity correlations with symptom changes, stands at the forefront of evaluating neuromodulation efficacy [111]. Additionally, functional MRI (fMRI) and diffusion tensor imaging (DTI) offer detailed insights into relevant brain regions and circuits, informing tailored neuromodulation strategies.
Looking ahead, integrating neuroimaging with neuromodulation holds promise for developing targeted treatments across various mental health conditions [78, 88]. By delineating and modulating the neural underpinnings of impulsivity, emerging interventions stand to benefit from the latest advancements in neuroimaging and neuromodulatory technologies.
Refining neuromodulation for transdiagnostic impulsivity through the RDoC framework
The integration of the RDoC framework into transdiagnostic neuromodulation marks a transformative shift in psychiatric interventions [24]. This paradigm prioritises neurobiological foundations over traditional symptom-based classifications, focusing on the neural substrates underlying various mental health conditions. The RDoC’s intricate and multidimensional structure provides a robust foundation for this approach, fostering deeper biological insights into mental disorders. Future research is expected to expand the RDoC framework by incorporating broader neurological and behavioural phenomena, thereby enhancing its utility for regulating impulsivity across diagnostic categories.
To address impulsivity transdiagnostically, there is a pressing need to synthesise dispersed evidence and establish a comprehensive intervention framework. Building such a framework, informed by the RDoC’s multidimensional matrix, presents unique challenges, particularly in developing a dimensional assessment model that captures the diverse manifestations of impulsivity (Fig. 1). Advancing our understanding of impulsivity’s clinical presentations and neural mechanisms is crucial for improving transdiagnostic assessments. However, integrating these insights with state-of-the-art neuromodulation strategies poses both challenges and opportunities. The continued evolution of RDoC-aligned approaches for impulsivity interventions invites ongoing debate and potential breakthroughs. Moreover, translating this knowledge into clinical practice requires concerted efforts to synthesise the full spectrum of impulsivity manifestations and to distinguish variations within the same pathology. A framework that combines clinical, behavioural, cognitive, and connectivity-based assessments of impulsivity is fundamental for achieving this goal.
Here, we propose a transdiagnostic intervention framework, termed the “Transdiagnostic Neuromodulation for Impulsivity” (TNMI) framework, to address impulsivity in mental health disorders (Fig. 2). Aligned with RDoC principles, this framework integrates clinical symptom evaluation with neuromodulation therapies, aiming to revolutionise mental health interventions on a transdiagnostic scale. The TNMI framework acknowledges the complexity of impulsivity within mental disorders and their associated neural patterns. By tailoring strategies to modulate specific brain circuits, it aspires to provide an alternative to disorder-specific therapies. This framework anticipates the development of novel, effective, and precisely targeted neuromodulatory treatments, supported by existing evidence on the multidimensional nature and neural correlates of impulsivity.
The figure provides examples, including addiction, attention-deficit/hyperactivity disorder (ADHD), and eating disorders (ED), to illustrate the performance of impulsivity, the structure of impulsivity, and the identification of brain circuits. The framework aims to advance precision medicine in the neuromodulation for mental disorders by recognising the multidimensional nature of impulsivity. This includes impulsive choice, impulsive action, and impulsive traits and their neural correlates. The framework incorporates findings from brain circuit research and uses techniques such as magnetic resonance imaging (MRI) and electroencephalography (EEG) to study impulsive brain circuits. The diagram illustrates transcranial magnetic stimulation (TMS) as a neuromodulation technique, with potential applications in modulating impulsive brain circuits. Please note that the figure has been adapted from the ref. [24], with permission from Annual Reviews, Inc. (License ID: 1446321-2).
Evidence-based implementation strategies of the TNMI framework
The TNMI framework introduces a structured approach for transdiagnostic neuromodulation targeting impulsivity-related symptoms and neural circuits (Fig. 2). While the framework’s components are still being refined and lack a unified protocol, we can illustrate its application with a practical example. As previously discussed, the frontostriatal circuitry is a promising neuromodulation target. Using the TNMI framework, TMS could be applied to focal prefrontal targets in disorders characterised by high impulsivity, such as eating disorders, substance use disorders, and gambling disorder. By modulating prefrontal regions, the intervention could influence the entire frontostriatal circuitry through functional or structural connectivity, potentially reducing impulsivity across these conditions.
Notably, to achieve effective transdiagnostic neuromodulation of impulsivity, the framework conceptually encompasses several key steps: delineating a transdiagnostic assessment of clinical impulsivity, targeting brain nodes implicated across diagnostic spectra, and modulating these nodes via neuromodulation. In future implementations, the choice of specific methods remains flexible. We will provide evidence-based options for each component as candidate methods.
Assessing clinical impulsivity symptoms of transdiagnostic neuromodulation
As a compound trait manifesting innately or environmentally, measuring impulsivity necessitates a blend of subjective and objective methodologies due to their modest intercorrelation [98]. Trait impulsivity is often gauged through self-reports like the Barratt Impulsiveness Scale (BIS-11) [28], the UPPS-P Impulsivity Scale [112], and the Eysenck Impulsiveness Questionnaire [113]. These instruments provide insights into the multifarious nature of impulsivity but are hampered by their subjectivity and inadequate correlation with empirical assessments.
In measuring impulsive choices, one must account for temporal discounting, ambiguity in judgement, and decision velocity. Temporal discounting pinpoints the preference for prompt, smaller rewards over significant but delayed gratification. When evaluating risk-based impulsivity, smaller certain rewards are often favoured over larger yet uncertain outcomes. Quickfire decision-making, the third component, signifies a propensity for hurried, often ill-considered choices. Clinically, tasks such as the Kirby Delay-Discounting Task [114], the Experiential Discounting Task [115], the Iowa Gambling Task [116], the Cambridge Gambling Task (CANTAB battery) [117, 118] and the Balloon Analogue Risk Test [119] are employed for diagnostic purposes in mental health conditions.
Motor impulsivity’s evaluation includes tasks assessing SSRT and premature responses. It is important to recognise that these measures disparate facets of impulsivity, each underpinned by distinct neural circuits. The SSRT task is a notable instrument to quantify motor impulsivity, gauging response inhibition through variable stop signals [120]. Additionally, the Go/NoGo paradigm assesses impulsive action/inhibition, demanding participants discriminate between rewarding stimuli and those meriting restraint [43]. Tasks such as these, probing anticipatory responses, provide a window into the waiting dimension of impulsive actions [121]. The inclusion of the Go/NoGo, SSRT, and waiting tasks allows researchers to capture different facets of the impulsive state and examine the diversity in the participants’ decision-making processes. While these tasks provide valuable insights into motor impulsivity and enhance the overall understanding of impulsive behaviour, it’s important to note their limitations. The concept of impulsivity is far from homogeneous, and these different measures may not correlate well with each other or with questionnaire methods [46]. This lack of correlation has led us to fractionate the construct of impulsivity, allowing for a more nuanced exploration of its distinctive elements.
Identifying brain targets of transdiagnostic neuromodulation
Harnessing neuroimaging techniques, researchers have mapped specific neural pathways linked to impulsivity [2, 45]. Trait impulsivity is orchestrated via an intricate web of brain circuits, with discernible correlations between grey and white matter volumes and assessment scores. Specific regions within the dorsolateral prefrontal cortex, like the left anterior cingulate gyrus, left medial frontal gyrus, and left middle frontal gyrus, correlate positively with overall impulsivity scores [122]. However, findings conflict concerning the association between cortical thickness in particular brain regions and impulsivity scores [123]. Cocaine-dependence research has evidenced reduced grey matter volume in certain frontal gyri [124], and high impulsivity scores have been linked with diminished resting-state connectivity in specific brain areas among those individuals [125].
State impulsivity, typified by immediate impulse-driven responses, is modulated by structures such as the PFC, orbitofrontal cortex, anterior insula, ACC, striatum, and frontal gyri [126]. Research in both human and rodent models has demarcated the brain circuits underlying state impulsivity, with motor and choice subtypes inscribed in unique limbic cortico-basal-ganglia pathways [19], embracing structures pivotal in choice impulsivity like the NAc, basolateral amygdala, hippocampus, insula, and orbitofrontal cortex [127,128,129,130].
Given these nuances, advancing transdiagnostic strategies require targeting the nodes within the impulsive brain circuit, integrating insights from neurocircuitry into clinical practices, and thereby innovating the landscape of mental health interventions.
Targeting transdiagnostic impulsivity by neuromodulation techniques
In the TNMI framework, the selection of an appropriate neuromodulation technique is guided by the intervention nodes identified in the previous step. For detailed descriptions of the principles, operational methods, applicable scope, advantages, and limitations of various neuromodulation techniques, we refer readers to dedicated review articles, as numerous comprehensive reviews on this topic are available [78, 131, 132]. In brief, key factors for optimal targeting include spatial localisation, temporal frequency, and nuanced energy modulation. These principles apply to both invasive and non-invasive neuromodulation techniques, such as TMS and DBS, ensuring precise and effective modulation of impulsivity-related neural circuits.
Spatial accuracy is ensured by calibrating stimulation devices to directly interact with the intended neural regions, utilising devices specific to each neuromodulation technique. Intracranial electrodes are found in DBS, stimulation coils in TMS, probes for fUS, and scalp electrodes for tES. Localisation methods such as those outlined by Fitzgerald et. al. [133] offer heightened precision to reach the prefrontal cortex or basal ganglia. Given individual anatomical diversity, tailor-made neuroimaging-guided placement is essential for specificity [132]. Temporal considerations involve the frequency with which stimulation is administered. Brain circuitry rhythms are intrinsic to cognitive processes, and altering these rhythms can significantly impact network dynamics. Adjusting the stimulation frequency can modulate neural activity, consequently altering behavioural and cognitive patterns. Energetic considerations balance intensity to ensure sufficient stimulus without inducing adverse effects. Analogous to a pharmacological dose-response relationship, neuromodulation necessitates intensity titration tailored to individual patients. Energy modulation focuses on calibrating the stimulus intensity. Balancing intensity avoids adverse effects while ensuring the stimulus is potent enough to modulate neural activity effectively. Personalising the stimulus intensity, akin to dose-response paradigms in pharmacology, is pivotal for individual treatment adequacy [132, 134].
The evolution of neuromodulation provides a spectrum of intervention modalities (Fig. 3). Non-targeted and minimally invasive techniques, such as modified electroconvulsive therapy or magnetic seizure therapy, can be foundational in the treatment spectrum. However, alternative and potentially preferable methods, such as deep TMS or high-intensity transcranial alternating current stimulation (tACS), offer reduced side effects and allow for awake treatment delivery with indicators of efficacy in mental disorders [135]. Further to the advent of less invasive methods, technologies such as focused ultrasound and high-frequency differential/temporal interference stimulation present non-invasive possibilities for modulating deep neural activity [136, 137]. These techniques provide the advantage of testability and optimisation of targets before the contemplation of more invasive procedures. Ultimately, invasive modalities like DBS, renowned for their precision and lasting effects, may be reserved for particularly severe cases [138].
The prefrontal cortex (PFC) and basal ganglia are outlined as the basic neurological circuits underlying impulsivity. Within the PFC, specific regions have been identified for their critical role in impulsivity. These regions include the infralimbic cortex, the orbitofrontal cortex (OFC), and the anterior cingulate cortex (ACC). At the same time, the nucleus accumbens (NAc), located in the basal ganglia, makes a significant contribution to impulsivity by acting as a central hub. A number of neuromodulation techniques can be used to modulate neural activity in specific regions associated with impulsivity. Magnetic electroconvulsive therapy (MECT), magnetic convulsive therapy (MCT), deep transcranial magnetic stimulation (dTMS), and high-intensity transcranial alternating current stimulation (Hi-tACS) can target the whole brain. Transcranial magnetic stimulation (TMS) and transcranial electrical stimulation (tES) can target superficial cortical regions such as the prefrontal cortex and orbitofrontal cortex (OFC). Temporal interference (TI), focused ultrasound (FUS), and deep brain stimulation (DBS) can be used to modulate deep nuclei such as the anterior cingulate cortex (ACC) and nucleus accumbens (NAc) in the basal ganglia. These different neuromodulation techniques offer potential therapeutic interventions for impulsivity by selectively modulating neural activity in specific regions associated with impulsive behaviour. Please note that subfigures (a-b) are reprinted with permission from ref. [139] (corresponding to original Fig. 3). Copyright 2017 by the American Association for the Advancement of Science (AAAS). Permission conveyed through Copyright Clearance Center (License ID: 1446338-1). The human architecture of the NAc was obtained from the Brainnetome Atlas [140].
Future research directions
The TNMI framework aligns with the RDoC’s transdiagnostic principles and holds the potential to address impulsivity across diverse disorders. It could also extend beyond impulsivity to explore its interactions with other symptoms, such as hallucinations and delusions. According to the RDoC framework, transdiagnostic approaches could simultaneously target impulsivity and its interplay with other symptom domains. However, these hypotheses currently rely on theoretical and preliminary evidence, necessitating empirical studies to validate the effectiveness of this unified neuromodulation approach.
First, the framework advocates for assessing clinical impulsivity symptoms through validated subjective or objective methods. It is crucial to recognise that impulsivity assessments may vary across different disorders and individuals. According to RDoC principles, a transdiagnostic approach can target impulsivity in various diseases and individuals. However, individual and disorder-specific impulsivity increases the complexity of determining intervention protocols, such as choosing excitatory versus inhibitory stimulation frequencies or doses. Therefore, research into personalised transdiagnostic impulsivity modulation methods is essential.
The era of personalised neuropsychiatric care is ushering in treatments that transcend symptom mitigation, aiming instead to rehabilitate and strengthen neurocognitive structures. This vision aligns with the emergence of personalised medicine, where interventions are intricately tailored to the unique behavioral impulsivity of each patient [110]. Drawing upon genetics, neuroimaging, and behavioral studies, these customised treatment strategies are poised to dramatically enhance efficacy and redefine therapeutic outcomes in impulsivity-related psychiatric conditions [78]. Technological advances, such as brain-computer interfaces (BCIs), refined neuroimaging, and analytics, promise to transform the neuromodulation landscape. These developments are set to enable adaptable, on-demand neuromodulation therapies responsive to fluctuating neural activity, charting the course for customised neuropsychiatric care.
To provide a structured roadmap for future research, we propose a three-tier research question matrix encompassing mechanistic, methodological, and translational levels. At the mechanistic level, future research should focus on identifying the key neural circuits and mechanisms underlying impulsivity across disorders. For example, one hypothesis could be that the strength of prefrontal-striatal functional connectivity is a critical circuit for transdiagnostic impulsivity interventions and can serve as a stimulation target for neuromodulation. This aligns with the RDoC framework’s emphasis on neural circuits and aims to identify shared mechanisms that can be targeted across disorders. At the methodological level, studies should evaluate the effectiveness of transdiagnostic intervention paradigms compared to traditional disorder-specific approaches. A potential hypothesis is that transdiagnostic neuromodulation paradigms targeting impulsivity-specific neural circuits will improve response rates by ≥15% compared to traditional methods in heterogeneous patient populations. Such research would emphasise the importance of developing and testing targeted intervention paradigms that account for impulsivity’s dimensional and transdiagnostic nature. At the translational level, the focus should shift to the clinical applicability and scalability of transdiagnostic interventions, particularly in overcoming the high heterogeneity in clinical response observed in current treatments. For instance, one hypothesis could be that a transdiagnostic neuromodulation approach will reduce response variability by at least 20% in patients with impulsivity-related disorders compared to existing disorder-specific treatments. These translational efforts are critical to demonstrating the practical benefits of transdiagnostic approaches in real-world settings.
Conclusion
This academic review has canvassed the multifaceted nature of neuromodulating impulsivity and its transdiagnostic presence across psychiatric disorders. We have traversed the landscape from the rudimentary conceptualisation of impulsivity to the sophisticated techniques being developed to modulate its underpinnings. The journey has uncovered the intricate web of neural circuitry associated with impulsivity and highlighted the pivotal role that neuromodulation techniques could play in future interventions. The heterogeneity of impulsivity poses significant challenges, which we have addressed by considering advancements in neuromodulation technologies and the unification of research efforts facilitated through the RDoC framework. By moving towards a model that regards impulsivity as a transdiagnostic trait, we can begin to tailor interventions that are as complex and nuanced as the disorders they aim to ameliorate. As research paradigms evolve and new technologies emerge, we are moving toward an age where interventions for impulsivity will be far more dynamic and precisely aimed at modulating the brain’s complex circuitry. The hope is that this progress will catalyze more profound insights and effective interventions, markedly enhancing the quality of life for those affected by impulsivity and related psychopathologies.
References
Crisp ZC, Grant JE. Impulsivity across psychiatric disorders in young adults. Compr Psychiatry. 2024;130:152449.
Schaub A-C, Vogel M, Lang UE, Kaiser S, Walter M, Herdener M, et al. Transdiagnostic brain correlates of self-reported trait impulsivity: a dimensional structure-symptom investigation. Neuroimage Clin. 2023;38:103423.
Koudys JW, Cane C, Nikolova Y, Ruocco A. Transdiagnostic impulsivity-relevant phenotypes and the comorbidity of personality disorders with substance and alcohol use disorders. Curr Addict Rep. 2023;10:122–30.
Patros CH, Alderson RM, Kasper LJ, Tarle SJ, Lea SE, Hudec KL. Choice-impulsivity in children and adolescents with attention-deficit/hyperactivity disorder (ADHD): a meta-analytic review. Clin Psychol Rev. 2016;43:162–74.
Paasche C, Weibel S, Wittmann M, Lalanne L. Time perception and impulsivity: A proposed relationship in addictive disorders. Neurosci Biobehav Rev. 2019;106:182–201.
Herman AM, Duka T. Facets of impulsivity and alcohol use: what role do emotions play? Neurosci Biobehav Rev. 2019;106:202–16.
Verdejo-Garcia A, Albein-Urios N. Impulsivity traits and neurocognitive mechanisms conferring vulnerability to substance use disorders. Neuropharmacology. 2021;183:108402.
Ioannidis K, Hook R, Wickham K, Grant JE, Chamberlain SR. Impulsivity in gambling disorder and problem gambling: a meta-analysis. Neuropsychopharmacology. 2019;44:1354–61.
Chen XC, Xu JJ, Yin XT, Qiu YF, Yang R, Wang ZY, et al. Mediating role of anxiety and impulsivity in the association between child maltreatment and lifetime non-suicidal self-injury with and without suicidal self-injury. J Affect Disord. 2023;347:57–65.
Bevione F, Martini M, Toppino F, Longo P, Abbate-Daga G, Brustolin A, et al. Cognitive impulsivity in anorexia nervosa in correlation with eating and obsessive symptoms: a comparison with healthy controls. Nutrients. 2024;16:1156.
Chamorro J, Bernardi S, Potenza MN, Grant JE, Marsh R, Wang S, et al. Impulsivity in the general population: a national study. J Psychiatr Res. 2012;46:994–1001.
Moore F, Doughty H, Neumann T, Mcclelland H, Allott C, O’Connor R. Impulsivity, aggression, and suicidality relationship in adults: a systematic review and meta-analysis. eClinicalMedicine. 2022;45:101307.
Pearlstein JG, Johnson SL, Timpano K, Stamatis CA, Robison M, Carver C. Emotion-related impulsivity across transdiagnostic dimensions of psychopathology. J Pers. 2023;92:342–60.
Sonmez A, Garcia JQ, Thitiseranee L, Blacker C, Lewis CP. Scoping review: transdiagnostic measurement of impulsivity domains in youth using the UPPS impulsive behavior scales. J Am Acad Child Adolesc Psychiatry. 2024;63:789–812.
Mackillop J, Levitt E, Oshri A, Amlung M, Ray L, Sanchez-Roige S, et al. Evaluation of delay discounting as a transdiagnostic research domain criteria indicator in 1388 general community adults. Psychol Med. 2022;53:1649–57.
Chapron S-A, Nourredine M, Dondé C, Haesebaert F, Micoulaud-Franchi J, Geoffroy P, et al. Efficacy and safety of topiramate for reducing impulsivity: a transdiagnostic systematic review and meta-analysis of a common clinical use. Fundam Clin Pharmacol. 2021;36:15–4.
Moeller FG, Barratt ES, Dougherty DM, Schmitz JM, Swann AC. Psychiatric aspects of impulsivity. Am J Psychiatry. 2001;158:1783–93.
Robbins TW, Gillan CM, Smith DG, de Wit S, Ersche KD. Neurocognitive endophenotypes of impulsivity and compulsivity: towards dimensional psychiatry. Trends Cogn Sci. 2012;16:81–91.
Dalley JW, Robbins TW. Fractionating impulsivity: neuropsychiatric implications. Nat Rev Neurosci. 2017;18:158–71.
Rezapour T, Rafei P, Baldacchino A, Conrod PJ, Dom G, Fishbein DH, et al. Neuroscience-informed classification of prevention interventions in substance use disorders: an RDoC-based approach. Neurosci Biobehav Rev. 2024;159:105578.
Stoyanov D, Telles-Correia D, Cuthbert BN. The research domain criteria (RDoC) and the historical roots of psychopathology: a viewpoint. Eur Psychiatry. 2019;57:58–60.
Fusar-Poli P, Solmi M, Brondino N, Davies C, Chae C, Politi P, et al. Transdiagnostic psychiatry: a systematic review. World Psychiatry. 2019;18:192–207.
Yücel M, Oldenhof E, Ahmed SH, Belin D, Billieux J, Bowden-Jones H, et al. A transdiagnostic dimensional approach towards a neuropsychological assessment for addiction: an international Delphi consensus study. Addiction. 2019;114:1095–109.
Deng ZD, Luber B, Balderston NL, Velez Afanador M, Noh MM, Thomas J, et al. Device-based modulation of neurocircuits as a therapeutic for psychiatric disorders. Annu Rev Pharmacol Toxicol. 2020;60:591–614.
Van Malderen E, Goossens L, Claes L, Wilderjans TF, Kemps E, Verbeken S. Self-regulation profiles in addictive behaviors among adolescents: a transdiagnostic approach. Appetite. 2024;192:107128.
Lamichhane B, Moukaddam N, Salas R, Goodman W, Sabharwal A. Multimodal objective assessment of impulsivity in healthy and mood disorder participants. NPP—Digital Psychiatry and Neuroscience 2025; 3. https://doi.org/10.1038/s44277-025-00026-z.
Moniz-Lewis DIK, Carlon HA, Hebden H, Tuchman FR, Votaw VR, Stein ER, et al. Third-wave treatments for impulsivity in addictive disorders: a narrative review of the active ingredients and overall efficacy. Curr Addict Rep. 2023;10:131–9.
Hook R, Grant J, Ioannidis K, Tiego J, Yücel M, Wilkinson P, et al. Trans-diagnostic measurement of impulsivity and compulsivity: A review of self-report tools. Neurosci Biobehav Rev. 2020;120:455–69.
Kozak K, Lucatch AM, Lowe DJE, Balodis IM, MacKillop J, George TP. The neurobiology of impulsivity and substance use disorders: implications for treatment. Ann N Y Acad Sci. 2019;1451:71–91.
Zhu L, Zhu Y, Li S, Jiang Y, Mei X, Wang Y, et al. Association of internet gaming disorder with impulsivity: role of risk preferences. BMC Psychiatry. 2023;23:754.
McHugh CM, Chun Lee RS, Hermens DF, Corderoy A, Large M, Hickie IB. Impulsivity in the self-harm and suicidal behavior of young people: a systematic review and meta-analysis. J Psychiatr Res. 2019;116:51–60.
Caswell AJ, Bond R, Duka T, Morgan MJ. Further evidence of the heterogeneous nature of impulsivity. Pers Individ Dif. 2015;76:68–74.
Evenden JL. Varieties of impulsivity. Psychopharmacology. 1999;146:348–61.
Dalley JW, Everitt BJ, Robbins TW. Impulsivity, compulsivity, and top-down cognitive control. Neuron. 2011;69:680–94.
Um M, Hershberger AR, Whitt ZT, Cyders MA. Recommendations for applying a multi-dimensional model of impulsive personality to diagnosis and treatment. Borderline Personal Disord Emot Dysregul. 2018;5:6.
Woods-Gonzalez R, Waddell JT, King SE, Corbin WR. Differentiating action from inaction: longitudinal relations among impulsive personality traits, internalizing symptoms, and drinking behavior. Addict Behav. 2024;154:108019.
Minhas M, Murphy CM, Balodis IM, Acuff SF, Buscemi J, Murphy JG, et al. Multidimensional elements of impulsivity as shared and unique risk factors for food addiction and alcohol misuse. Appetite. 2021;159:105052.
Guo L, Chen T, Zheng H, Zhong N, Wu Q, Su H, et al. The structure and individual patterns of trait impulsivity across addiction disorders: a network analysis. Int J Ment Health Ad. 2023. https://doi.org/10.1007/s11469-023-01022-0.
Elliott MV, Johnson SL, Pearlstein JG, Muñoz Lopez DE, Keren H. Emotion-related impulsivity and risky decision-making: a systematic review and meta-regression. Clin Psychol Rev. 2023;100:102232.
Grevet EH, Bandeira CE, Vitola ES, de Araujo Tavares ME, Breda V, Zeni G, et al. The course of attention-deficit/hyperactivity disorder through midlife. Eur Arch Psychiatry Clin Neurosci. 2022.
van Baal ST, Moskovsky N, Hohwy J, Verdejo-García A. State impulsivity amplifies urges without diminishing self-control. Addict Behav. 2022;133:107381.
Hamilton KR, Mitchell MR, Wing VC, Balodis IM, Bickel WK, Fillmore M, et al. Choice impulsivity: definitions, measurement issues, and clinical implications. Personal Disord. 2015;6:182–98.
Helton WS. Impulsive responding and the sustained attention to response task. J Clin Exp Neuropsychol. 2009;31:39–47.
MacKillop J, Weafer J, Gray JC, Oshri A, Palmer A, de Wit H. The latent structure of impulsivity: impulsive choice, impulsive action, and impulsive personality traits. Psychopharmacology. 2016;233:3361–70.
Skandali N, Baek K, Sallie S, Sonkusare S, Mandali A, Ritou V, et al. Neural circuit mapping of waiting impulsivity and proactive inhibition with convergent evidence from fMRI and TMS. Eur Psychiatr. 2023;66:S982–S982.
Strickland JC, Johnson MW. Rejecting impulsivity as a psychological construct: a theoretical, empirical, and sociocultural argument. Psychol Rev. 2021;128:336–61.
Grant JE, Chamberlain SR. Impulsive action and impulsive choice across substance and behavioral addictions: cause or consequence? Addict Behav. 2014;39:1632–9.
Mestre-Bach G, Steward T, Granero R, Fernández-Aranda F, Mena-Moreno T, Vintró-Alcaraz C, et al. Dimensions of impulsivity in gambling disorder. Sci Rep. 2020;10:397.
Cyders MA, Coskunpinar A. Measurement of constructs using self-report and behavioral lab tasks: is there overlap in nomothetic span and construct representation for impulsivity? Clin Psychol Rev. 2011;31:965–82.
Reynolds B, Patak M, Shroff P, Penfold RB, Melanko S, Duhig AM. Laboratory and self-report assessments of impulsive behavior in adolescent daily smokers and nonsmokers. Exp Clin Psychopharmacol. 2007;15:264–71.
Dang J, King KM, Inzlicht M. Why are self-report and behavioral measures weakly correlated? Trends Cogn Sci. 2020;24:267–9.
Enkavi AZ, Poldrack RA. Implications of the lacking relationship between cognitive task and self-report measures for psychiatry. Biol Psychiatry Cogn Neurosci Neuroimaging. 2021;6:670–2.
Meder D, Haagensen BN, Hulme O, Morville T, Gelskov S, Herz DM, et al. Tuning the brake while raising the stake: network dynamics during sequential decision-making. J Neurosci. 2016;36:5417–26.
Drossel G, Brucar L, Rawls E, Hendrickson T, Zilverstand A. Subtypes in addiction and their neurobehavioral profiles across three functional domains. Transl Psychiatry. 2023;13:127.
Friedman NP, Robbins TW. The role of prefrontal cortex in cognitive control and executive function. Neuropsychopharmacology. 2021;47:72–89.
Li B, Nguyen TP, Ma C, Dan Y. Inhibition of impulsive action by projection-defined prefrontal pyramidal neurons. Proc Natl Acad Sci USA. 2020;117:17278–87.
Piszczek L, Constantinescu A, Kargl D, Lazovic J, Pekcec A, Nicholson JR, et al. Dissociation of impulsive traits by subthalamic metabotropic glutamate receptor 4. eLife. 2022;11:e62123.
Murphy ER, Dalley JW, Robbins TW. Local glutamate receptor antagonism in the rat prefrontal cortex disrupts response inhibition in a visuospatial attentional task. Psychopharmacology. 2005;179:99–107.
Xiao X, Deng H, Wei L, Huang Y, Wang Z. Neural activity of orbitofrontal cortex contributes to control of waiting. Eur J Neurosci. 2016;44:2300–13.
Kim J-H, Ma D-H, Jung E, Choi I, Lee S-H. Gated feedforward inhibition in the frontal cortex releases goal-directed action. Nat Neurosci. 2021;24:1452–64.
Hatter JA, Scott MM. Selective ablation of VIP interneurons in the rodent prefrontal cortex results in increased impulsivity. PLoS ONE. 2023;18:e0286209.
Foster NN, Barry J, Korobkova L, Garcia L, Gao L, Becerra M, et al. The mouse cortico–basal ganglia–thalamic network. Nature. 2021;598:188–94.
Lanciego JL, Luquin N, Obeso JA. Functional neuroanatomy of the basal ganglia. Cold Spring Harb Perspect Med. 2012;2:a009621–621.
Aron AR. From reactive to proactive and selective control: developing a richer model for stopping inappropriate responses. Biol Psychiatry. 2011;69:e55–68.
Guzulaitis R, Palmer LM. A thalamocortical pathway controlling impulsive behavior. Trends Neurosci. 2023;46:1018–24.
Sesia T, Temel Y, Lim LW, Blokland A, Steinbusch HWM, Visser-Vandewalle V. Deep brain stimulation of the nucleus accumbens core and shell: Opposite effects on impulsive action. Exp Neurol. 2008;214:135–9.
Besson M, Belin D, McNamara R, Theobald DE, Castel A, Beckett VL, et al. Dissociable control of impulsivity in rats by dopamine D2/3 receptors in the core and shell subregions of the nucleus accumbens. Neuropsychopharmacology. 2009;35:560–9.
Moreno M, Economidou D, Mar AC, López-Granero C, Caprioli D, Theobald DE, et al. Divergent effects of D2/3 receptor activation in the nucleus accumbens core and shell on impulsivity and locomotor activity in high and low impulsive rats. Psychopharmacology. 2013;228:19–30.
Haber SN, Fudge JL, McFarland NR. Striatonigrostriatal pathways in primates form an ascending spiral from the shell to the dorsolateral striatum. J Neurosci. 2000;20:2369–82.
Guo K, Yamawaki N, Svoboda K, Shepherd GMG. Anterolateral motor cortex connects with a medial subdivision of ventromedial thalamus through cell type-specific circuits, forming an excitatory thalamo-cortico-thalamic loop via layer 1 apical tuft dendrites of layer 5B pyramidal tract type neurons. J Neurosci. 2018;38:8787–97.
Miquel M, Nicola SM, Gil-Miravet I, Guarque-Chabrera J, Sanchez-Hernandez A. A working hypothesis for the role of the cerebellum in impulsivity and compulsivity. Front Behav Neurosci. 2019;13:99.
Catanese J, Jaeger D. Premotor ramping of thalamic neuronal activity is modulated by nigral inputs and contributes to control the timing of action release. J Neurosci. 2021;41:1878–91.
Guzulaitis R, Godenzini L, Palmer LM. Neural basis of anticipation and premature impulsive action in the frontal cortex. Nat Neurosci. 2022;25:1683–92.
Takahashi N, Moberg S, Zolnik TA, Catanese J, Sachdev RNS, Larkum ME, et al. Thalamic input to motor cortex facilitates goal-directed action initiation. Curr Biol. 2021;31:4148–55.e4144.
Belin-Rauscent A, Daniel M-L, Puaud M, Jupp B, Sawiak S, Howett D, et al. From impulses to maladaptive actions: the insula is a neurobiological gate for the development of compulsive behavior. Mol Psychiatry. 2015;21:491–9.
Scangos KW, State MW, Miller AH, Baker JT, Williams LM. New and emerging approaches to treat psychiatric disorders. Nat Med. 2023;29:317–33.
van den Heuvel MP, Sporns O. A cross-disorder connectome landscape of brain dysconnectivity. Nat Rev Neurosci. 2019;20:435–46.
Siddiqi SH, Khosravani S, Rolston JD, Fox MD. The future of brain circuit-targeted therapeutics. Neuropsychopharmacology. 2024;49:179–88.
Chen T, Su H, Li R, Jiang H, Li X, Wu Q, et al. The exploration of optimized protocol for repetitive transcranial magnetic stimulation in the treatment of methamphetamine use disorder: a randomized sham-controlled study. EBioMedicine. 2020;60:103027.
Grover S, Nguyen JA, Viswanathan V, Reinhart RMG. High-frequency neuromodulation improves obsessive-compulsive behavior. Nat Med. 2021;27:232–8.
Brooks SJ, Lochner C, Shoptaw S, Stein DJ. Using the research domain criteria (RDoC) to conceptualize impulsivity and compulsivity in relation to addiction. Prog Brain Res 2017;235:177–218.
Chamberlain SR, Sahakian BJ. The neuropsychiatry of impulsivity. Curr Opin Psychiatry. 2007;20:255–61.
Elliott MV, Esmail SAS, Weiner KS, Johnson SL. Neuroanatomical correlates of emotion-related impulsivity. Biol Psychiatry. 2023;93:566–74.
Hjell G, Rokicki J, Szabo A, Holst R, Tesli N, Bell C, et al. Impulsivity across severe mental disorders: a cross-sectional study of immune markers and psychopharmacotherapy. BMC Psychiatry. 2023;23:659.
İnce B, Schlatter J, Max S, Plewnia C, Zipfel S, Giel KE, et al. Can we change binge eating behaviour by interventions addressing food-related impulsivity? a systematic review. J Eat Disord. 2021;9:38.
Anderson AC, Youssef GJ, Robinson AH, Lubman DI, Verdejo-Garcia A. Cognitive boosting interventions for impulsivity in addiction: a systematic review and meta-analysis of cognitive training, remediation and pharmacological enhancement. Addiction. 2021;116:3304–19.
Loya JM, Benitez B, Kiluk BD. The effect of cognitive behavioral therapy on impulsivity in addictive disorders: a narrative review. Curr Addict Rep. 2023;10:485–93.
Paul SM, Potter WZ. Finding new and better treatments for psychiatric disorders. Neuropsychopharmacology. 2023;49:3–9.
Neacsiu AD, Beynel L, Powers JP, Szabo S, Appelbaum L, Lisanby S, et al. Enhancing cognitive restructuring with concurrent repetitive transcranial magnetic stimulation: a transdiagnostic randomized controlled trial. Psychother Psychosom. 2021;91:94–106.
Ferrarelli F, Phillips ML. Examining and modulating neural circuits in psychiatric disorders with transcranial magnetic stimulation and electroencephalography: present practices and future developments. Am J Psychiatry. 2021;178:400–13.
Spano MC, Lorusso M, Pettorruso M, Zoratto F, Di Giuda D, Martinotti G, et al. Anhedonia across borders: transdiagnostic relevance of reward dysfunction for noninvasive brain stimulation endophenotypes. CNS Neurosci Ther. 2019;25:1229–36.
Lohse A, Løkkegaard A, Siebner HR, Meder D. Linking impulsivity to activity levels in pre-supplementary motor area during sequential gambling. J Neurosci. 2023;43:1414–21.
Yücel M, Fontenelle LF, Chamberlain S. Introduction to the special issue on the utility of transdiagnostic approaches for developing novel interventions for substance and behavioural addictions. Neuropsychol Rev. 2019;29:1–3.
Wessel MJ, Beanato E, Popa T, Windel F, Vassiliadis P, Menoud P, et al. Noninvasive theta-burst stimulation of the human striatum enhances striatal activity and motor skill learning. Nat Neurosci. 2023;26:2005–16.
Violante IR, Alania K, Cassarà AM, Neufeld E, Acerbo E, Carron R, et al. Non-invasive temporal interference electrical stimulation of the human hippocampus. Nat Neurosci. 2023;26:1994–2004.
Fani N, Treadway MT. Potential applications of temporal interference deep brain stimulation for the treatment of transdiagnostic conditions in psychiatry. Neuropsychopharmacology. 2023;49:305–6.
Dellu-Hagedorn F, Rivalan M, Fitoussi A, De Deurwaerdère P. Inter-individual differences in the impulsive/compulsive dimension: deciphering related dopaminergic and serotonergic metabolisms at rest. Philos Trans R Soc Lond B Biol Sci. 2018;373:20170154.
Verdejo-Garcia A, Tiego J, Kakoschke N, Moskovsky N, Voigt K, Anderson A, et al. A unified online test battery for cognitive impulsivity reveals relationships with real-world impulsive behaviours. Nat Hum Behav. 2021;5:1562–77.
Fan H, Liu Z, Wu X, Yu G, Gu X, Kuang N, et al. Decoding anxiety-impulsivity subtypes in preadolescent internalising disorders: findings from the adolescent brain cognitive development study. Br J Psychiatry. 2023;223:542–54.
Parkes L, Tiego J, Aquino K, Braganza L, Chamberlain SR, Fontenelle LF, et al. Transdiagnostic variations in impulsivity and compulsivity in obsessive-compulsive disorder and gambling disorder correlate with effective connectivity in cortical-striatal-thalamic-cortical circuits. Neuroimage. 2019;202:116070.
Lantrip C, Szabo YZ, Kozel FA, Holtzheimer P. Neuromodulation as an augmenting strategy for behavioral therapies for anxiety and PTSD: a narrative review. Curr Treat Options Psychiatry. 2022;9:406–18.
Chan CC, Alter S, Hazlett E, Shafritz KM, Yehuda R, Goodman M, et al. Neural correlates of impulsivity in bipolar disorder: a systematic review and clinical implications. Neurosc Biobehav Rev. 2023;147:105109.
Winstanley C, Eagle D, Robbins T. Behavioral models of impulsivity in relation to ADHD: translation between clinical and preclinical studies. Clin Psychol Rev. 2006;26:379–95.
Wang S, Zhang M, Liu S, Xu Y, Shao Z, Chen L, et al. Impulsivity in heroin-dependent individuals: structural and functional abnormalities within frontostriatal circuits. Brain Imaging Behav. 2021;15:2454–63.
Hu Y, Salmeron BJ, Gu H, Stein EA, Yang Y. Impaired functional connectivity within and between frontostriatal circuits and its association with compulsive drug use and trait impulsivity in cocaine addiction. JAMA Psychiatry. 2015;72:584–92.
Isserles M, Tendler A, Roth Y, Bystritsky A, Blumberger DM, Ward H, et al. Deep transcranial magnetic stimulation combined with brief exposure for posttraumatic stress disorder: a prospective multisite randomized trial. Biol Psychiatry. 2021;90:721–8.
Joutsa J, Moussawi K, Siddiqi SH, Abdolahi A, Drew W, Cohen AL, et al. Brain lesions disrupting addiction map to a common human brain circuit. Nat Med. 2022;28:1249–55.
Siddiqi SH, Schaper FLWVJ, Horn A, Hsu J, Padmanabhan JL, Brodtmann A, et al. Brain stimulation and brain lesions converge on common causal circuits in neuropsychiatric disease. Nat Hum Behav. 2021;5:1707–16.
Aiello M, Eleopra R, Foroni F, Rinaldo S, Rumiati RI. Weight gain after STN-DBS: the role of reward sensitivity and impulsivity. Cortex. 2017;92:150–61.
Lynch CJ, Elbau IG, Ng TH, Wolk D, Zhu S, Ayaz A, et al. Automated optimization of TMS coil placement for personalized functional network engagement. Neuron. 2022;110:3263–77.e3264.
Cash RFH, Weigand A, Zalesky A, Siddiqi SH, Downar J, Fitzgerald PB, et al. Using brain imaging to improve spatial targeting of transcranial magnetic stimulation for depression. Biol Psychiatry. 2021;90:689–700.
Whiteside SP, Lynam DR. The five factor model and impulsivity: using a structural model of personality to understand impulsivity. Pers Individ Dif. 2001;30:669–89.
Eysenck SBG, Eysenck HJ. Impulsiveness and venturesomeness: their position in a dimensional system of personality description. Psychol Rep. 1978;43:1247–55.
Kirby KN, Petry NM. Heroin and cocaine abusers have higher discount rates for delayed rewards than alcoholics or non-drug-using controls. Addiction. 2004;99:461–71.
Reynolds B, Schiffbauer R. Measuring state changes in human delay discounting: an experiential discounting task. Behav Processes. 2004;67:343–56.
Bechara A, Damasio AR, Damasio H, Anderson SW. Insensitivity to future consequences following damage to human prefrontal cortex. Cognition. 1994;50:7–15.
Rogers R. Dissociable deficits in the decision-making cognition of chronic amphetamine abusers, opiate abusers, patients with focal damage to prefrontal cortex, and tryptophan-depleted normal volunteers evidence for monoaminergic mechanisms. Neuropsychopharmacology. 1999;20:322–39.
Clark L, Bechara A, Damasio H, Aitken MR, Sahakian BJ, Robbins TW. Differential effects of insular and ventromedial prefrontal cortex lesions on risky decision-making. Brain. 2008;131:1311–22.
Lejuez CW, Read JP, Kahler CW, Richards JB, Ramsey SE, Stuart GL, et al. Evaluation of a behavioral measure of risk taking: the balloon analogue risk task (BART). J Exp Psychol Appl. 2002;8:75–84.
Logan GD, Van Zandt T, Verbruggen F, Wagenmakers E-J. On the ability to inhibit thought and action: general and special theories of an act of control. Psychol Rev. 2014;121:66–95.
Dalley JW, Ersche KD. Neural circuitry and mechanisms of waiting impulsivity: relevance to addiction. Philos Trans R Soc Lond B Biol Sci. 2019;374:20180145.
Cho SS, Pellecchia G, Aminian K, Ray N, Segura B, Obeso I, et al. Morphometric correlation of impulsivity in medial prefrontal cortex. Brain Topogr. 2013;26:479–87.
Schilling C, Kühn S, Romanowski A, Schubert F, Kathmann N, Gallinat J. Cortical thickness correlates with impulsiveness in healthy adults. Neuroimage. 2012;59:824–30.
Moreno-López L, Catena A, Fernández-Serrano MJ, Delgado-Rico E, Stamatakis EA, Pérez-García M, et al. Trait impulsivity and prefrontal gray matter reductions in cocaine dependent individuals. Drug Alcohol Depend. 2012;125:208–14.
McHugh MJ, Demers CH, Braud J, Briggs R, Adinoff B, Stein EA. Striatal-insula circuits in cocaine addiction: implications for impulsivity and relapse risk. Am J Drug Alcohol Abuse. 2013;39:424–32.
Fineberg NA, Chamberlain SR, Goudriaan AE, Stein DJ, Vanderschuren LJMJ, Gillan CM, et al. New developments in human neurocognition: clinical, genetic, and brain imaging correlates of impulsivity and compulsivity. CNS Spectr. 2014;19:69–89.
Cardinal RN, Pennicott DR, Lakmali C, Sugathapala, Robbins TW, Everitt BJ. Impulsive choice induced in rats by lesions of the nucleus accumbens core. Science. 2001;292:2499–501.
Winstanley CA, Theobald DEH, Cardinal RN, Robbins TW. Contrasting roles of basolateral amygdala and orbitofrontal cortex in impulsive choice. J Neurosci. 2004;24:4718–22.
Kable JW, Glimcher PW. The neural correlates of subjective value during intertemporal choice. Nat Neurosci. 2007;10:1625–33.
McClure SM, Laibson DI, Loewenstein G, Cohen JD. Separate neural systems value immediate and delayed monetary rewards. Science. 2004;306:503–7.
Polanía R, Nitsche MA, Ruff CC. Studying and modifying brain function with non-invasive brain stimulation. Nat Neurosci. 2018;21:174–87.
Zhong G, Yang Z, Jiang T. Precise modulation strategies for transcranial magnetic stimulation: advances and future directions. Neurosci Bull. 2021;37:1718–34.
Fitzgerald PB. Targeting repetitive transcranial magnetic stimulation in depression: do we really know what we are stimulating and how best to do it? Brain Stimul. 2021;14:730–6.
Poo M-M. Transcriptome, connectome and neuromodulation of the primate brain. Cell. 2022;185:2636–9.
Wang H, Wang K, Xue Q, Peng M, Yin L, Gu X, et al. Transcranial alternating current stimulation for treating depression: a randomized controlled trial. Brain. 2022;145:83–91.
Toccaceli G, Barbagallo G, Peschillo S. Low-intensity focused ultrasound for the treatment of brain diseases: safety and feasibility. Theranostics. 2019;9:537–9.
Grossman N, Bono D, Dedic N, Kodandaramaiah SB, Rudenko A, Suk HJ, et al. Noninvasive deep brain stimulation via temporally interfering electric fields. Cell. 2017;169:1029–41.e1016.
Frey J, Cagle J, Johnson KA, Wong JK, Hilliard JD, Butson CR, et al. Past, present, and future of deep brain stimulation: hardware, software, imaging, physiology and novel approaches. Front Neurol. 2022;13:825178.
Carlén M. What constitutes the prefrontal cortex? Science. 2017;358:478–82.
Fan L, Li H, Zhuo J, Zhang Y, Wang J, Chen L, et al. The human brainnetome atlas: a new brain atlas based on connectional architecture. Cereb Cortex. 2016;26:3508–26.
Acknowledgements
We express our deepest gratitude to all the contributors who made this article possible. Special thanks to Professor Mu-ming Poo for his invaluable insights and suggestions.
Funding
Funding for this study was supported by National Key R&D Program of China (2023YFC3304204, 2019HY320001); National Nature Science Foundation (82130041, 82171484, 81871045, 82201650, 82171485); Brain Science and Brain-Like Intelligence Technology (2021ZD0202105, 2022ZD0211100); Shanghai Jiao Tong University Medical Engineering Cross Research (YG2023ZD25).
Author information
Authors and Affiliations
Contributions
MZ, JD and TWR conceived the study and outlined the research protocol. GZ and TC performed thorough literature reviews, assembling comprehensive summaries of key prior research studies. NZ, TR, AH and HJ played a pivotal role in dissecting the complexities of impulsivity and profiling its diverse expressions across mental disorders and neuromodulations. HS and TY led the project and supervised the experiments. All authors contributed to the writing of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhong, G., Chen, T., Zhong, N. et al. Transdiagnostic neuromodulation of impulsivity: current status and future trajectories. Transl Psychiatry 15, 209 (2025). https://doi.org/10.1038/s41398-025-03415-2
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41398-025-03415-2
This article is cited by
-
Examining Transdiagnostic Patterns of Motor Differences: Preliminary Findings From the Consortium for Motor Behavior in Neurodivergence (COMBINE)
Journal of Autism and Developmental Disorders (2025)
-
Medial prefrontal cortex circuit dynamics involved in stage-specific addiction
Brain Structure and Function (2025)