Abstract
We analyzed the neutrophil-to-lymphocyte ratio (NLR) in 1508 patients with PV and found that those with an NLR ≥ 5 were generally older, had a longer disease history, and had higher cardiovascular risk factors, more arterial thrombosis, and more aggressive blood counts, indicating a more proliferative disease. NLR was an accurate predictor of mortality, with patients with NLR ≥ 5 having significantly worse overall survival and more than twice the mortality rate compared to those with NLR < 5. Multivariable models confirmed that increasing age, previous venous thrombosis and NLR ≥ 5 were strong predictors of death, further influenced by cardiovascular risk factors. We examined the interaction between NLR and the number of cardiovascular risk factors and found a progressive trend of increased mortality risk for NLR values ≥ 5 in addition to the presence of more than one risk factor. In conclusion, patients with NLR ≥ 5 require careful monitoring and management of cardiovascular risk factors because they increase mortality when associated with progressive levels of NLR.
Similar content being viewed by others
Introduction
In polycythemia vera (PV), essential thrombocythemia (ET), and primary myelofibrosis (PMF), systemic chronic inflammation plays a central role in disease development and progression [1, 2]. These myeloproliferative neoplasms (MPNs) are driven by somatic gene mutations (JAK2V617F, MPL and CALR) that give rise to mutated cells, leading to elevated levels of inflammatory cytokines, such as interleukin-1 (IL-1), interleukin-6 (IL-6), and tumor necrosis factor-alpha (TNF-α), along with dysregulation of the adaptive immune system [1, 3].
Non-mutated inflammatory cells also contribute to this inflammatory response, exacerbating cytokine overproduction and impairing the immune system’s ability to regulate these cytokine levels [3]. The result is a state of chronic systemic inflammation that fuels the expansion of neoplastic clones [1].
This process may be further influenced by external factors related to the patient and environment. Identified risk factors include aging, chemotherapy, radiation treatments, inflammatory conditions, germline variants, and lifestyle factors such as smoking, body mass index, diet, and diabetes. Smoking, in particular, significantly contributes to the chronic inflammatory state in MPNs and is recognized as a precursor to several chronic diseases, including cardiovascular disease, chronic obstructive pulmonary disease, and various cancers, including MPN [4, 5].
Inflammatory biomarkers such as C-reactive protein and pentraxin-3 have been correlated with the risk of thrombosis [6] and disease progression in MPN and have been correlated with JAK2V617F allele burden [7]. Recently, the neutrophil-to-lymphocyte ratio (NLR) has emerged as a prognostic biomarker in several chronic inflammatory diseases and cancer [8, 9] has been correlated with the incidence of venous thrombosis in MPN [10]. In MPN, neutrophils circulate in an activated state and participate in the inflammatory processes not only by producing cytokines associated with clonal hematopoiesis and the formation of neutrophil extracellular traps, but also by directly interacting with tissue macrophages and dendritic cells. The key role of lymphocyte subsets in this neutrophil-induced inflammation is to modulate their functions [11, 12].
Neutrophilia, often associated with relative lymphocytopenia, reflects a significant decrease in the cell-mediated adaptive immune response, and the NLR effectively captures the balance between the potentially deleterious effects of neutrophilia and the beneficial effects of lymphocyte-mediated adaptive immunity [11, 12].
Although a large body of literature supports the prognostic potential of NLR in the general population and in cancer, its translation into clinical practice remains challenging, as the strength of the association between NLR and overall survival varies significantly between studies, possibly due to differences in patient subgroup analyses. In particular, the predictive value of high NLR levels for mortality in polycythemia vera remains unclear. However, recent evidence suggests that higher NLR levels may be associated with increased mortality in MPN patients, especially when associated with comorbid conditions [13]. This intriguing observation warrants further validation in different MPN subgroups to establish clinically meaningful thresholds for risk stratification and correlation with relevant outcomes. In addition, it remains to be determined whether NLR can serve as a predictive biomarker for response to therapy beyond its role as a prognostic indicator.
In this study, we analyzed the neutrophil-to-lymphocyte ratio (NLR) in a large cohort of PV patients from the ECLAP trial with a median follow-up of 2.8 years (IQR 1.9-3.8). Our objectives were (1) to describe the disease burden associated with different NLR levels, (2) to assess the independent prognostic value of NLR for mortality, and (3) to evaluate whether the predictive power of NLR for mortality is influenced by conventional risk factors for thrombosis, which remains the leading cause of mortality in PV patients.
Patients and Methods
Patients
The European Collaboration on Low-Dose Aspirin in Polycythemia Vera (ECLAP) trial included PV patients with new and old diagnoses made according to World Health Organization (WHO) 2008 diagnostic criteria with no exclusion criteria with respect to age, therapy, or duration of disease. Treatment strategies had to comply with the recommendation of maintaining the hematocrit value at less than 0.45 and the platelet count at less than 400 × 109/L. Clinical outcomes during the prospective follow-up were recorded at follow-up visits at 12, 24, 36, 48, and 60 months. Out of the 1638 patients of the whole cohort [14] included in the ECLAP study, 1508 were selected for this analysis as they had details on blood count and differential at enrollment. Events were diagnosed as previously described [15].
Statistical analysis
Descriptive statistics were used to summarize patients’ characteristics at baseline. Continuous variables were summarized by median and interquartile range, and categorical variables were presented as frequencies and percentages. Characteristics of study population were stratified for NLR levels at baseline and differences between groups were tested with the chi-squared test (or Fisher’s exact test, where appropriate) or the rank-sum test for categorical or continuous variables, respectively.
Generalized additive models (GAMs) were used to investigate the association between blood counts and risk of death. This approach allows for capturing potential non-linear relationships between neutrophils, lymphocytes, NLR and mortality risk. Hazard ratio (HR) estimates and their 95% confidence intervals were plotted on a logarithmic scale.
Overall survival was estimated using the Kaplan-Meier method: the log-rank test was used to compare group-specific curves.
Two multivariable Cox proportional hazards models were fitted to identify predictors of death: (i) a first model with the inclusion of known predictors and (ii) a second model with the additional inclusion of NLR and the conventional cardiovascular risk factors. The HRs and the corresponding 95% Confidence Intervals (CIs) were reported. The discriminatory power of the models was tested using Harrell’s C-statistic.
Moreover, the effect of a possible interaction between NLR levels and the number of CV risk factors was tested by a multivariable Cox model adjusting for known predictors.
To assess the robustness of our findings, a sensitivity analysis was performed to assess whether the effect of NLR on mortality was independent of disease duration.
A significance level of p < 0.05 was used. Statistical analysis was performed using STATA software, release 16.1 (StataCorp LP, College Station, TX, USA).
Results
Baseline features and follow-up events
Table 1 shows patient characteristics at baseline and stratified by NLR < or ≥ 5. Patients with higher NLR tended to be older, had a longer duration since PV diagnosis, had a higher prevalence of arterial thrombosis, and had higher CV risk factors. Regarding blood counts at enrollment, they were influenced by previous phlebotomies, which explains that a proportion of them had HCT and hemoglobin on target. At the time of recruitment, 28.4% of patients were managed by phlebotomy alone, 26.5%, by chemotherapeutic agents; and 35.1%, by phlebotomy plus chemotherapeutic agents. A significant difference in various blood counts, with higher WBC, neutrophils, and platelets but lower hemoglobin and lymphocytes, was documented in the group with NLR > 5 compared to patients with NLR < 5. In addition, patients with a higher NLR were more likely to have more phlebotomies during follow-up, a higher incidence of total and venous thrombosis, and a higher rate of progression to myelofibrosis. Based on these data, patients with an NLR ≥ 5 had characteristics indicative of more proliferative disease.
NLR and mortality
-
(i)
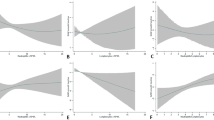
A total of 151 deaths (10%) were recorded for an overall mortality rate of 3.7 deaths per 100 persons per year. The incidence rates of CV and non-CV mortality were 1.7 and 1.8 deaths per 100 persons per year, respectively. CV mortality accounted for 45% of all deaths, while hematologic transformation and solid tumors were the cause of death in 13% and 19.5% of fatal cases, respectively. To evaluate how the NLR and individual neutrophil and lymphocyte counts impacted the risk of death, we used generalized additive proportional hazards models (GAMs) (Fig. 1). In Panel A the curve shows that higher neutrophil counts were associated with an increased risk of death, as the hazard ratio rises with increasing neutrophil counts. Panel B shows an inverse relationship between lymphocyte counts and the risk of death; higher lymphocyte count was associated with a lower hazard ratio, indicating a lower risk of death. Panel C shows that an increasing NLR was associated with a higher hazard ratio, indicating that a higher NLR correlated with an increased risk of death.
Fig. 1: Generalized additive models (GAMs) for the prediction of death. The figure reports GAMs by absolute neutrophils (A), lymphocytes (B) and their ratio NLR (C). The effect of neutrophils, lymphocytes and their ratio on the risk of death was analyzed on a continuous scale using a Generalized Additive Model (GAM) with a smooth function fitted by cubic splines. Hazard ratio estimates (solid line) along with their 95% confidence intervals (gray area) are plotted on a logarithmic scale.
-
(ii)
We also examined whether NLR values compared with absolute numbers of individual neutrophil and lymphocyte counts had greater discriminatory power in predicting death, but found no significant difference. However, the NLR appeared a more robust and precise predictor of mortality risk, particularly at higher values, compared to absolute neutrophil or lymphocyte counts. This is evidenced by the narrower confidence intervals at higher NLR values (Fig. 1), indicating greater precision and reliability in predicting death.
-
(iii)
Kaplan-Meier curve (Fig. 2) illustrates the overall survival of patients stratified by their NLR values. Patients with a higher NLR ( ≥ 5) had a significantly lower overall survival compared to those with a lower NLR ( < 5) (p < 0.001); the rate of deaths was more than double in patients with higher NLR levels (rate % patient-years: 5.93, 95% CI 4.73-7.44 versus 2.76, 95% CI 2.20-3.45, respectively).
Fig. 2: Kaplan-Meier survival curve by baseline NLR values. Kaplan-Meier curve illustrates the overall survival of patients stratified by their Neutrophil-to-Lymphocyte Ratio (NLR) values. Patients with a higher NLR had a significantly lower overall survival compared to those with a lower NLR (p < 0.001); the rate of deaths was more than double in patients with higher NLR levels.
Death prediction factors
-
(i)
Table 2 presents two multivariable models for death prediction, with different combinations of variables and updates across models. Model A represents the confirmation of prior risk score by Tefferi et al. [16]: (i) increasing age was strongly associated with a higher risk of death. Individuals aged 67 years and older have a significantly higher hazard ratio (HR = 4.03) compared to those younger than 57 years; (ii) elevated WBC was associated with a higher risk of death (HR = 1.65); (iii) previous venous thrombosis also increases the risk (HR = 1.57). In Model B, NLR ≥ 5 was added together with the conventional CV risk factors; NLR was independently associated with a higher risk of death (HR = 1.84), the association with age and previous venous thrombosis remained strong and the negative effect of diabetes (HR = 2.26), heart failure (HR = 2.75) and smoking emerged (HR = 2.47). The discriminatory power of this model was higher than the previous one as documented by the significant improvement in Harrell’s C-statistic (0.75 vs 0.69, p < 0.001).
Table 2 Multivariable models for death prediction. Sensitivity analysis showed that the effect of NLR on mortality was independent of disease duration (Table 1S).
-
(ii)
Figure 3 displays the predicted hazard rates for different combinations of NLR and the number of CV risk factors adjusted for age and previous venous thrombosis. Patients with higher NLR exhibited a steep increase in predicted hazard rates as the number of CV risk factors increases. The hazard rate remained relatively stable when moving from 0 to 1 CV risk factor, but there was a sharp increase when moving from 1 to 2 or more CV risk factors. The increase is much less pronounced in low NLR group compared to the high NLR group.
Fig. 3: Predicted Hazard Rate by NLR levels and number of CV risk factors. The graph shows the predicted hazard rates for different combinations of the Neutrophil-to-Lymphocyte Ratio (NLR) and the number of cardiovascular (CV) risk factors adjusted for age and previous venous thrombosis. Patients with higher NLR ( ≥ 5) and more CV risk factors exhibit significantly higher predicted hazard rates, particularly as the number of CV risk factors increases.
Discussion
Consistent with several reports on NLR as a prognostic factor for outcome in inflammatory and cancer diseases, our findings highlight the value of NLR for mortality and provide important insights into this inflammatory biomarker and patient mortality in PV patients.
We showed that patients with a higher NLR ( ≥ 5) presented characteristics of a more advanced disease and a higher burden of cardiovascular risk factors. These patients were older, had a longer duration since PV diagnosis, and were more likely to have a history of arterial thrombosis. The differences in blood counts, including higher white blood cell, neutrophils, and platelet counts but lower lymphocyte counts, suggest that a higher NLR is indicative of a more proliferative and inflammatory disease state associated with an impairment of innate immunity [11, 12]. The fact that patients with higher NLR also required more phlebotomies during follow-up and had a higher incidence of venous thrombosis and progression to myelofibrosis further supports that a high NLR reflects a more aggressive disease. Although no direct data are available on the relationship between NLR levels and JAK2V617F VAF in this series, a recent study in polycythemia vera (PV) patients with low thrombotic risk has demonstrated a linear association between these two variables [17]. This finding suggests that NLR, a biomarker of inflammation, may be correlated with the JAK2V617F driver mutation.
The use of GAMs allowed for a nuanced analysis of how neutrophil and lymphocyte counts and their ratio (NLR) affected the risk of death. The relationships between NLR and survival (Fig. 1) showed that higher neutrophil counts were associated with an increased risk of death, consistent with the understanding that elevated neutrophils are associated with worse outcomes in PV [13] and that, conversely, higher lymphocyte counts were associated with a reduced risk of death [13, 18]. This inverse relationship highlights the protective role that lymphocytes may play, possibly through their involvement in the regulation of immune responses. Absolute neutrophil and lymphocyte counts showed agreement with NLR; however, the latter correlated with a higher hazard ratio for death, and the model’s confidence intervals were narrower at higher NLR values, indicating robust and reliable predictions.
The Kaplan-Meier survival analysis further confirms the importance of NLR in predicting patient outcomes. Patients with an NLR ≥ 5 had a significantly lower overall survival compared to those with an NLR < 5. The fact that the mortality rate was more than doubled in the high NLR group highlights the critical role of NLR in this setting.
In line with the findings of Tefferi et al. [16], our analysis of the ECLAP series also identified age, white blood cell count, and prior thrombosis as significant and independent predictors of mortality. Notably, the inclusion of the NLR, alongside conventional cardiovascular risk factors, enhanced the model’s ability to discriminate survival probability, as evidenced by the significant improvement in Harrell’s C-statistic (Harrell’s C = 0.75 vs. 0.69; p < 0.001).
Furthermore, the interaction between NLR and factors such as diabetes, heart failure, and smoking shows that patients with an NLR ≥ 5 experience a synergistic effect between NLR and these CV risk factors. This underscores the importance of considering both NLR levels and the number of CV risk factors in assessing patient prognosis. It also highlights the crucial role of appropriate interventions to reduce the detrimental effects of these modifiable risk factors particularly when associated with other inflammatory factors as revealed by high NLR values.
Overall, the results of our prospective observational study of PV are consistent with the recent paper by Larsen et al. [13]. These investigators analyzed the association of NLR with all-cause mortality and mortality by comorbidity burden in the general population and in individuals with MPN. They included 835,430 individuals from the Danish General Suburban Population Study and showed that in the general population, increasing NLR was associated with a stepwise increase in all-cause mortality in individuals with NLR ≥ 6 compared with those with NLR 1–1.9 (HR 2.07 vs. NLR 1–1.9, respectively). In addition, individuals with prevalent ET, PV, or MF had a higher HR for all-cause mortality compared with no MPN (HRs for ET, PV, or MF were 2.15, 2.20, 2.32, and 1.48, respectively). Of great interest was the demonstration of the interaction between increasing NLR and Charlson comorbidity Index (CCI) in both the general population and in MPN. They showed that increasing NLR and comorbidity burden were associated with lower survival in individuals without MPN, but were even worse in prevalent and incident MPN, ET, PV, and MF diseases.
The International Working Group (IWG) on MPN, led by Tefferi, has recently revised the risk model for PV survival, proposing a score based on four key variables: age, absolute neutrophil count, monocytes, and the presence of arterial thrombosis at baseline [19]. This analysis provides new insights into the risk of death associated with leukocyte levels and types and suggests to investigate whether these individual variables may be more effectively used in clinical practice than the NLR ratio that is a broader marker involving at the same time innate and adaptive immunity of disease severity.
Our study has some limitations: the first is the mixed patient population of the ECLAP prospective observational cohort, which also includes a randomized controlled trial of low-dose aspirin [15, 20]; the second is the fact that ECLAP was conducted before the inclusion of the JAK2V617F mutation in the diagnostic criteria, which may raise doubts about the unintended inclusion of non-PV patients. However, the strengths of the study, such as its prospective design, regular follow-up, strict compliance monitoring and independent event validation by an expert panel, ensure high data quality and reliability. These robust methods help to mitigate the limitations and add considerable strength to the study’s conclusions.
In conclusion, the data suggest that NLR is a marker of inflammation that selects a PV subgroup with a more aggressive, pro-inflammatory disease phenotype. This is particularly relevant in this phenotype, where inflammation and thrombosis are major contributors to disease morbidity and mortality.
The multivariable models underscored the importance of NLR, especially in combination with conventional CV risk factors, and the overall results suggest that NLR should be considered in routine clinical risk assessment alongside traditional factors such as age and prior thrombosis. However, it is crucial to validate these findings in modern cohorts diagnosed after the discovery of the JAK2 V617F mutation, as this could lead to more homogeneous patient populations and potentially further refine the prognostic value of NLR in relation to JAK2 V617F VAF.
Ongoing clinical trials trials or recently completed [21,22,23] or observational studies [24, 25] could consider longitudinal monitoring of NLR to observe how changes in NLR over time correlate with long-term survival and disease progression, as this may help determine whether NLR could be a dynamic marker reflecting real-time responses to therapy.
Data availability
Aggregated data available by request. Patient-level data will not be shared.
References
Hasselbalch HC. Perspectives on chronic inflammation in essential thrombocythemia, polycythemia vera, and myelofibrosis: is chronic inflammation a trigger and driver of clonal evolution and development of accelerated atherosclerosis and second cancer? Blood. 2012;119:3219–25.
Tefferi A, Barbui T. Polycythemia vera: 2024 update on diagnosis, risk-stratification, and management. Am J Hematol. 2023;98:1465–87.
Hermouet S, Bigot-Corbel E, Gardie B. Pathogenesis of myeloproliferative neoplasms: role and mechanisms of chronic inflammation. Mediators Inflamm. 2015;2015:145293.
Ramanathan G, Hoover BM, Fleischman AG. Impact of Host, Lifestyle and Environmental Factors in the Pathogenesis of MPN. Cancers (Basel). 2020;12:2038.
Pedersen KM, Bak M, Sørensen AL, Zwisler A-D, Ellervik C, Larsen MK, et al. Smoking is associated with increased risk of myeloproliferative neoplasms: A general population-based cohort study. Cancer Med. 2018;7:5796–802.
Barbui T, Carobbio A, Finazzi G, Vannucchi AM, Barosi G, Antonioli E, et al. Inflammation and thrombosis in essential thrombocythemia and polycythemia vera: different role of C-reactive protein and pentraxin 3. Haematologica. 2011;96:315–8.
Lussana F, Carobbio A, Salmoiraghi S, Guglielmelli P, Vannucchi AM, Bottazzi B, et al. Driver mutations (JAK2V617F, MPLW515L/K or CALR), pentraxin-3 and C-reactive protein in essential thrombocythemia and polycythemia vera. J Hematol Oncol. 2017;10:54.
Hibino S, Kawazoe T, Kasahara H, Itoh S, Ishimoto T, Sakata-Yanagimoto M, et al. Inflammation-induced tumorigenesis and metastasis. Int J Mol Sci. 2021;22:5421.
Templeton AJ, McNamara MG, Šeruga B, Vera-Badillo FE, Aneja P, Ocaña A, et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J Natl Cancer Inst. 2014;106:dju124.
Carobbio A, Vannucchi AM, De Stefano V, Masciulli A, Guglielmelli P, Loscocco GG, et al. Neutrophil-to-lymphocyte ratio is a novel predictor of venous thrombosis in polycythemia vera. Blood Cancer J. 2022;12:28.
Mantovani A, Cassatella MA, Costantini C, Jaillon S. Neutrophils in the activation and regulation of innate and adaptive immunity. Nat Rev Immunol. 2011;11:519–31.
Jaillon S, Galdiero MR, Del Prete D, Cassatella MA, Garlanda C, Mantovani A. Neutrophils in innate and adaptive immunity. Semin Immunopathol. 2013;35:377–94.
Larsen MK, Skov V, Kjær L, Eickhardt-Dalbøge CS, Knudsen TA, Kristiansen MH, et al. Neutrophil-to-lymphocyte ratio and all-cause mortality with and without myeloproliferative neoplasms-a Danish longitudinal study. Blood Cancer J. 2024;14:28.
Marchioli R, Finazzi G, Landolfi R, Kutti J, Gisslinger H, Patrono C, et al. Vascular and neoplastic risk in a large cohort of patients with polycythemia vera. J Clin Oncol. 2005;23:2224–32.
Marchioli R, Finazzi G, Specchia G, Cacciola R, Cavazzina R, Cilloni D, et al. Cardiovascular events and intensity of treatment in polycythemia vera. N. Engl J Med. 2013;368:22–33.
Tefferi A, Rumi E, Finazzi G, Gisslinger H, Vannucchi AM, Rodeghiero F, et al. Survival and prognosis among 1545 patients with contemporary polycythemia vera: an international study. Leukemia. 2013;27:1874–81.
Barbui T, Carobbio A, Guglielmelli P, Ghirardi A, Fenili F, Loscocco GG, et al. Neutrophil/lymphocyte ratio identifies low-risk polycythemia vera patients for early ropeginterferon Alpha-2b Therapy. Br J Haematol. 2024.
Warny M, Helby J, Nordestgaard BG, Birgens H, Bojesen SE. Incidental lymphopenia and mortality: a prospective cohort study. CMAJ. 2020;192:E25–E33.
Tefferi A, Loscocco GG, Iftikhar M, Rana MS, Jadoon Y, Atanasio, A, et al. Revised International Working Group Risk Model for Survival in Polycythemia Vera. Submitted to the ASH Congress (2024).
Landolfi R, Marchioli R, Kutti J, Gisslinger H, Tognoni G, Patrono C, et al. Efficacy and safety of low-dose aspirin in polycythemia vera. N. Engl J Med. 2004;350:114–24.
Harrison CN, Nangalia J, Boucher R, Jackson A, Yap C, O’Sullivan J, et al. Ruxolitinib Versus Best Available Therapy for Polycythemia Vera Intolerant or Resistant to Hydroxycarbamide in a Randomized Trial. J Clin Oncol. 2023;41:3534–44.
Kremyanskaya M, Kuykendall AT, Pemmaraju N, Ritchie EK, Gotlib J, Gerds A, et al. Rusfertide, a Hepcidin Mimetic, for Control of Erythrocytosis in Polycythemia Vera. N. Engl J Med. 2024;390:723–35.
Gisslinger H, Klade C, Georgiev P, Krochmalczyk D, Gercheva-Kyuchukova L, Egyed M, et al. Ropeginterferon alfa-2b versus standard therapy for polycythaemia vera (PROUD-PV and CONTINUATION-PV): a randomised, non-inferiority, phase 3 trial and its extension study. Lancet Haematol. 2020;7:e196–e208.
Bewersdorf JP, How J, Masarova L, Bose P, Pemmaraju N, Mascarenhas J, et al. Moving toward disease modification in polycythemia vera. Blood. 2023;142:1859–70.
Abu-Zeinah K, Saadeh K, Silver RT, Scandura JM, Abu-Zeinah G. Excess mortality in younger patients with myeloproliferative neoplasms. Leuk Lymphoma. 2023;64:725–9.
Acknowledgements
This work is part of the RICO project (Ricerca Istituzionale Collaborativa-Ospedale Papa Giovanni XXIII di Bergamo), BCC, Milano, Italy; it is sponsored by FROM-Fondazione per la Ricerca Ospedale di Bergamo-ETS and endorsed by the AIRC - Gruppo Italiano Malattie Mieloproliferative (AGIMM) with the program number 1005 and MYNERVA project, program number 21267, website at https://progettomynerva.it.
Author information
Authors and Affiliations
Contributions
TB conceived and designed the study, supervised the analysis, and wrote the paper. AC and AG performed statistical analyses and contributed to paper writing. FF directed the project and collected the data. AMV, PG, AR, NG and AT revised the study and contributed to paper writing. MCF and MC collected the data. The manuscript was approved by all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no conflict of interest.
Ethics approval and consent to participate
Results of this trials were derived from ECLAP randomized clinical trial (NEJM 350;2, 2004). In this study the following information was provided “The study protocol conformed to good clinical practice for trials and to the 2000 revision of the Declaration of Helsinki regarding medical research in humans. We obtained the approval of each local ethics committee before the start of the trial. All patients provided written informed consent. The study was conceived, conducted, and analyzed by the independent investigators under the aegis of the steering committee”.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Barbui, T., Carobbio, A., Ghirardi, A. et al. Neutrophil-to-lymphocyte ratio as a prognostic indicator of mortality in Polycythemia Vera: insights from a prospective cohort analysis. Blood Cancer J. 14, 195 (2024). https://doi.org/10.1038/s41408-024-01176-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41408-024-01176-7