Abstract
The responsible implementation of reproductive genetic carrier screening (RGCS) involves understanding the long-term psychosocial and reproductive impacts of results. This mixed-methods study examined these impacts within ‘Mackenzie’s Mission’, an Australia-wide study that offered couple-based RGCS for >1280 genes to 10,000 reproductive couples. Data from participant surveys completed at enrolment and 12 months post-result were analysed. Participants with an increased chance result were interviewed. Reflexive thematic analysis, guided by Interpretive Description was used. 4948 participants (27% response) completed the 12 month post-result survey. Most had minimal decision regret (median ≤5, 0 = no regret, 100 = high regret) and high reproductive confidence. Participants found to have an increased chance result had elevated anxiety (n = 116, median = 39 out of 80, clinically meaningful is ≥40). Interviewees (N = 19, from 16 couples) felt their increased chance result “change[d] everything” about their reproductive plans. Although revising their reproductive plan was an emotionally complex “journey”, participants were “grateful” for the information. The concept of the ‘Reproductive Story’, was used to interpret the results. A reproductive story refers to a person’s expected narrative about parenthood that, if altered, can cause psychosocial distress. Receiving an increased chance result disrupts the reproductive story. By 12 months post-result, most people with an increased chance result felt empowered to revise their reproductive story, but anxiety was elevated. Findings suggest a need for longitudinal models of post-RGCS psychosocial support.
Similar content being viewed by others
Introduction
Reproductive genetic carrier screening (RGCS) provides people with information about their chance of having children with autosomal recessive or X-linked genetic conditions. Approximately 2% of reproductive couples (i.e. the two genetic parents, of opposite chromosomal sex, to a current or planned pregnancy) will have an increased chance of having children with a serious inherited condition, resulting in a 25% chance of the genetic condition in any pregnancy conceived (referred to hereafter as ‘increased chance result’) [1]. Many professional organisations now recommend that RGCS be offered to all people pre-conception or in early pregnancy, regardless of family history [2,3,4,5]. Two important aspects of population-wide implementation of RGCS are supporting reproductive autonomy and supporting people who receive increased chance results [6]. Thus, it is critical to understand the psychosocial and reproductive impacts of RGCS.
Most people expect to receive a low chance RGCS result, with results typically associated with peace-of-mind and increased reproductive confidence [7, 8]. In contrast, people are often under-prepared to receive an increased chance result. Common reactions to result disclosure include shock, anxiety, and fear [8,9,10,11]. The subsequent reproductive decision-making process is also known to be complex and psychosocially impactful [12, 13].
Couples with an increased chance result have access to several reproductive options, although options vary based on geographical location [14]. Nevertheless, for those with access to all available options, most still describe choosing between in-vitro fertilisation (IVF) with pre-implantation genetic testing for the monogenic condition (PGT-M) and prenatal diagnosis (PND) with the view to end an affected pregnancy [12, 13, 15,16,17]. Across three studies from Australia and the United States, more than 60% of people chose to use one of these reproductive interventions to avoid the genetic condition in their children [15,16,17]. Research has typically captured reproductive choices, or intended choices, for people’s first pregnancy at or soon after RGCS. Little research has explored how increased chance results impact reproductive plans throughout the reproductive stage-of-life.
There is some evidence to indicate that with time, people report feeling empowered by the information [8, 10, 18, 19]. However, heterogeneity in data collection methods, varied lengths of follow-up, and small sample sizes make it difficult to adequately assess the long-term psychosocial and reproductive impacts of RGCS [20].
Study aim
The aim of this study was to explore experiences of RGCS within the first 12 months post-result, including:
-
1.
Psychosocial outcomes before and 12 months after receiving RGCS results.
-
2.
How an increased chance result impacts reproductive plans.
Methods
Study setting
This study was part of The Australian Reproductive Genetic Carrier Screening Project (‘Mackenzie’s Mission’), which offered RGCS free-of-charge, before or in early pregnancy, for 1281 autosomal recessive and X-linked genes associated with ~750 serious childhood-onset conditions [1, 21]. Both reproductive partners were screened together and received a combined result [1]. The socio-demographics of the cohort generally reflected that of Australians of reproductive age [1]. Of 9107 reproductive couples screened, almost 2% (n = 175) of couples were newly identified through participation in Mackenzie's Mission to have an increased chance of having children with a condition screened (‘new’ increased chance, including four who already knew they had an increased chance for a different condition. See Kirk et al. [1] for a list of conditions.). A further 176 couples knew, prior to Mackenzie’s Mission, that they had an increased chance for one of the conditions screened and received a low chance for all other conditions (‘known’ increased chance) [1]. New increased chance results were disclosed by a study genetic counsellor and offered genetic counselling to discuss their reproductive options. In Australia, prenatal diagnosis and termination of pregnancy are available through the public health system. IVF with PGT-M is primarily available on a user-pay basis; to assess uptake in the absence of cost, couples screened pre-conception were offered one funded cycle of IVF with PGT-M [21]. Research was conducted alongside the RGCS program; this study draws on data collected at enrolment and 12 months post-result [21].
Study design
This study used an explanatory sequential mixed-methods approach, enabling qualitative data to explain, and provide richness to, a quantitative dataset [22]. The qualitative enquiry was guided by Interpretive Description, a flexible methodological framework that draws upon the constructivist paradigm commonly used in qualitative research to develop findings applicable to clinical practice [23].
Data collection
Survey
Demographics and baseline psychosocial data were collected from all participants at enrolment. The 12 month post-result survey was optional. State anxiety was measured at both timepoints using the short form of the State Trait Anxiety Inventory (STAI-6) [24]. Scores range from 20 to 80 with scores ≥40 considered clinically meaningful [25]. The 12 month post-result survey also included the Decision Regret Scale (DRS, scores ranging from 0 = no regret to 100 = high regret [26]) and purpose-designed questions to capture reproductive confidence and reproductive choices.
Interviews
Participants with a new increased chance result were offered an interview, regardless of 12 month post-result survey completion. Participants were purposively sampled [27] to ensure the experiences of a variety of reproductive choices were captured. Reproductive intentions and outcomes data, which couples had already provided to Mackenzie’s Mission [1], were used to aid sampling. At the time of sampling, couples were either undecided or had chosen one of the following pathways: IVF with PGT-M, PND with the view to end an affected pregnancy, using their increased chance result to plan/prepare to potentially have a child with the genetic condition or not having (more) children [1].
Both members of a couple were invited to take part and if both accepted, separate interviews were organised. This approach allowed for in-depth engagement with each participant, and they could discuss potentially sensitive or emotionally complex topics, such as relationship dynamics, without the influence of the other partner. Semi-structured interviews were conducted over telephone and audio-recorded, with participants providing verbal consent to participate. Audio-recordings were transcribed verbatim and de-identified. Participants were assigned pseudonyms; if both partners participated, pseudonyms beginning with the same letter were selected.
Data analysis
Survey
Demographic data were described using frequencies. To assess possible response bias at 12 months post-result, the demographics of responders and non-responders were examined using X2 tests. STAI, DRS and reproductive confidence scores were summarised per-individual, then grouped by the RGCS result received. Reproductive choices and psychosocial impacts for participants with a new increased chance result were summarised based on their reproductive status (e.g., currently pregnant).
Interviews
Interviews were analysed using reflexive thematic analysis, a form of qualitative analysis that involves distilling data into shared patterns of meaning [28]. Analysis began with data familiarisation followed by inductive coding. If both members of a couple participated, transcripts were compared to examine participants’ unique experience of the same reproductive journey, with similarities and differences noted. As analysis progressed, the study team met to discuss codes, and the development and refinement of themes. This iterative, team-based approach to reflexive thematic analysis meant findings were developed from multiple viewpoints, increasing interpretive rigour.
Results
Survey
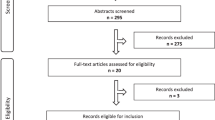
Responses to the 12 month post-result survey from 4984 participants, including 116 with a new increased chance result, were analysed (see Fig. 1). Characteristics are described in Table 1. Of note, 71% of participants were female. Further, at enrolment in MM, 83% of couples were not pregnant and 60% of participants were planning a pregnancy in the next year.
RGCS = reproductive genetic carrier screening | ‘New’ increased chance = People newly identified through Mackenzie’s Mission as having an increased chance of having children with a condition screened | ‘Known’ increased chance = people who already knew they had an increased chance of children with an inherited condition prior to taking part in Mackenzie’s Mission and received a low chance for all other conditions screened in the study. aParticipants were not asked any further survey questions as the combined low chance result was no longer relevant for reproductive planning bFor low chance results, 27.4% individual response rate with 45.7% of couples represented. cFor new increased chance results, 33.1% individual response rate with 54.9% of couples represented c For known increased chance results, 20.3% individual response rate with 35.8% of couples represented.
Psychosocial outcomes are described in Table 2. Median state anxiety was at, or close to, clinically meaningful levels for participants with an increased chance (both new and known) at 12 months post-result. For participants with a new increased chance, the highest levels of anxiety were seen amongst those who were currently trying to become pregnant, were planning a future pregnancy and/or had experienced a pregnancy loss in the last 12 months (see Supplementary Table 2 for reproductive choices made by couples with a new increased chance result). Median decision regret was zero for participants with a low chance result and a known increased chance result (IQR = 0–10) and five (IQR = 0–15) for participants with a new increased chance result. Reproductive confidence was highest for those with a low chance result, although 41% of participants with a new increased chance result also felt the result provided “a lot of confidence” when planning pregnancies.
Interviews
Nineteen participants with a new increased chance result (12 females and 7 males), including both partners from three couples, took part. The reproductive histories and reproductive choices of the 16 couples are presented in Table 3. Four themes were developed, describing the evolving psychosocial impacts of an increased chance result experienced within the first 12 months post-result. Illustrative quotes are provided in-text and in Table 4.
Theme 1 – Receiving an increased chance result alters the expected reproductive path
Most interviewees expected to receive a low chance result. Most who were offered RGCS pre-conception were hoping to achieve peace of mind before becoming pregnant (Table 4, quote 1). Other participants considered receiving an increased chance result to be unlikely and were unconcerned about trying to conceive whilst waiting for results (quote 2). As the increased chance result was unexpected, result disclosure appeared to have a profound emotional effect. Twelve months on, recollections remained vivid and descriptive.
“It was very difficult to process…it certainly wasn’t far off…hearing of the death of a relative. It was that sort of level of emotion.” – Adrian, increased chance, planning to conceive via IVF with PGT-M
Most participants described feeling that an increased chance result had profoundly altered their reproductive story. As Felicity stated, “I just remember thinking… this is going to change everything.” Participant narratives also indicated a sense of disempowerment in their reproductive futures and for some, the result challenged core beliefs about their lives.
“…We just thought ‘oh, everything will be fine’ [with the result]. We were very fortunate, we’ve had pretty easy lives, so we just assumed everything would be fine. Now I think back and think we were idiots.” – Paige, increased chance, currently trying to conceive via IVF with PGT-M
“I felt that the world was ending. All I ever wanted to be in life was to be a Mum. My husband, all he ever wants to be is a Dad, and we both grew up with wonderful families and we wanted to create our own.” – Marnie, increased chance, planning to use PND after becoming pregnant
Given this profound impact, participants appreciated prompt access to genetic counselling to learn more about the condition and discuss their reproductive options. For many, genetic counselling appeared to be the first step towards regaining a sense of confidence in their reproductive futures. Compared to Adrian’s initial reaction to the result, his quote below demonstrates a turning point in his emotions as he started considering reproductive options with his partner.
“…after that [genetic counselling] appointment was when it [the result] started feeling overall like a positive…it still wasn’t like ‘everything’s fantastic’, [but] at least we know where we’re going now.” – Adrian, increased chance, planning to conceive via IVF with PGT-M
Theme 2 – Constructing a new reproductive path is an evolving process
Making a reproductive decision appeared to be a key step in participants’ adaptation to their increased chance result. Several participants used the word “journey” to describe the reproductive decision-making process. The first decision participants described making was whether the condition they received an increased chance result for is one they want to avoid in their future children.
Most participants made the choice to try to avoid the condition in their children. Participants who were pregnant at result disclosure made a choice about PND quickly (quote 3), understandable given the limited time in which to do so. In comparison, those who were pre-conception generally described a more evolving decision-making process. Participants like Andrew and Joel felt that they came to a decision with their partners quickly. Others, such as partners Felicity and Felix, described how their decision was made over a series of conversations. Some also involved significant people in their lives, such as friends, family (quote 4) or religious leaders.
Most reported discussing options such as adoption or donor gametes with their genetic counsellor, however, all participants only considered IVF with PGT-M and PND. Factors involved in the decision are described in Supplementary Table 3. While IVF with PGT-M was the preferred choice for many, several participants acknowledged psychosocial, medical and practical burdens associated with IVF. Some also noted the cognitive dissonance of pursuing IVF without the prior experience of infertility. However, Felicity felt more disappointment at the thought of IVF than her partner, Felix (also interviewed):
“…I remember feeling a bit upset that we would end up going down the IVF route before we’d even started trying [to conceive].” – Felicity, increased chance, planning to conceive via IVF with PGT-M
Two participants (Leah and Samira) became pregnant post-result and chose not to have PND. Some genes screened in Mackenzie’s Mission were associated with conditions for which early treatment can improve prognosis. Leah received an increased chance for one such condition, which she described as “mild” and “manageable”. She explained that the result therefore did not change her plans to conceive and ultimately had a less profound impact on her reproductive plans (quote 5).
At 12 months post-result, all but one participant (Tilly) who had RGCS pre-conception had made a reproductive decision. Tilly explained that she felt ambivalent toward both PND and IVF with PGT-M (quote 6). For this reason, she said: “[we’re] not ‘not trying’ for a child, but we’re also still exploring IVF.”
Participants who had had a pregnancy during the study period also noted that reproductive decisions are not fixed and may change for future pregnancies. For example, some participants who conceived spontaneously and had unaffected pregnancies were considering whether they are willing to attempt this option again in the future knowing that there was 25% chance that the pregnancy would be affected.
“…it’s a tough one because obviously it was easy for us to get pregnant but then you don’t want to, again, risk that one in four chance…You are lucky this time but are you always going to be as lucky?” – Gabby, increased chance, pregnant post-result, had PND and pregnancy was unaffected
Theme 3 – Embarking on a new reproductive path is emotionally complex
By 12 months post-result, participants were at various stages of enacting their reproductive decisions. The following three sub-themes describe the emotional impacts of participants’ chosen reproductive pathway.
“We’d regained our pregnancy” – Experiences of PND
Participants who had PND all described a peak in their anxiety and difficulties connecting with their pregnancy whilst waiting for the diagnostic result (quote 7). Mara used the word “limbo” to describe this experience. Most participants explained that their anxiety quickly resolved after learning their pregnancy was unaffected. However, some participants expressed ongoing psychological impacts after PND (quote 8). To address this, Gabby suggested: “…more support within the pregnancy would have been good.”
“Half enjoying and half worrying” – Experiences of pregnancy without PND
Leah and Samira explained that they would not consider termination of pregnancy and did not have PND after becoming pregnant. Leah, who was pregnant at the time of interview, was confident in the management options should her baby have the condition. Conversely, Samira had experienced infertility and was due to begin IVF with PGT-M when she conceived spontaneously. She described the mixed emotions she experienced during pregnancy (quote 9). She also described the extremely difficult wait for the baby’s test result after birth and how relieved she was to learn her child did not have the genetic condition.
“The uncertainty of IVF” – Experiences of IVF with PGT-M
Experiences of IVF with PGT-M varied greatly. Partners Ruby and Rory (both interviewed), and Carlos and his wife (not interviewed), conceived after their first embryo transfer. All three participants were positive about their experience with IVF and PGT-M, although Rory and Carlos noted that they had not had the embodied experience of IVF and that their role was primarily to support their partners (quote 10).
Ruby acknowledged that while she had a positive experience with IVF and PGT-M, not everyone would have the same experience. This was clear from the experiences of partners Paige and Patrick (both interviewed). Paige explained: “[I] went into the IVF process with an expectation that it was going to work right away…” However, the couple had experienced multiple unsuccessful embryo transfers and ovarian hyper-stimulation and at the time of interview, felt at a crossroad of how to proceed.
“I’m looking for the quickest option [to become pregnant]. I’m like ‘this is all taking too long, this is really hard on my body’… the thought of going through that again [ovarian hyper-stimulation], I don’t want to do that.” – Paige, increased chance, currently trying to conceive via IVF with PGT-M
“We’ve talked about it [stopping IVF], but…if we did do that and got pregnant naturally, we’d still want to test for this condition and…would probably terminate the pregnancy…which would be kind of traumatic… we want to avoid that.” - Patrick, increased chance, currently trying to conceive via IVF with PGT-M
Several participants were soon to commence their first IVF cycle. Whilst some felt excited and hopeful at the prospect, others described anticipatory anxiety and were approaching their first cycle with caution (quote 11).
Theme 4 – An increased chance result has value in the reproductive journey
As participants made and enacted reproductive choices, the meaning ascribed to their increased chance result evolved. At 12 months post-result, many participants felt grateful for the result and did not regret the decision to have RGCS. For example, Andrew explained that it was better to find out pre-conception, rather than after the birth of a child with the condition. As such, when considering the different directions their lives may have taken had they not had RGCS, most concluded that it was better to know than not know.
“It was 100% the right decision [to have RGCS]. I think it still brings a lot of trauma and upset and heartache to make [reproductive] decisions, but it saves a whole lot more than having a potential one in four pregnancy [with the condition].” – Tilly, increased chance, currently deciding on a reproductive option
Nevertheless, the emotional complexities of receiving an increased chance result appear to be long-lasting. Two participants, who were pregnant at result disclosure and had unaffected pregnancies, have chosen not to have more children. Although they had reached the end of their reproductive journey, both described ongoing emotional impacts of their result. Vera, for example, explained how she and her husband feared an unexpected pregnancy (quote 12) as they do not want to experience the stress of PND and possible termination of pregnancy a second time.
Additionally, participants who were trying to conceive, or were planning a future pregnancy, described the result remaining at the forefront of their minds. Further, the steps involved in IVF have meant some participants are considering a future pregnancy sooner than they may have otherwise (quote 13). As Samira said: “It’s hard…I don’t think I could not think about it…”
Discussion
This study describes experiences of RGCS within the first 12 months post-result. Strengths of our study included the large sample size and the longitudinal, mixed-methods design, which enabled us to comprehensively examine psychosocial and reproductive impacts. For most people, decision regret was minimal and reproductive confidence was high, although those with an increased chance result had elevated levels of anxiety compared to baseline. Interviews provided rich explanations for these survey results by highlighting the emotional complexities associated with receiving an increased chance result. The evidence generated in this study can be used to inform how best to deliver RGCS in a way that promotes positive outcomes.
Most people who pursue RGCS will receive a low chance result [1]. Our findings emphasise that this experience has minimal negative psychosocial implications and provides reproductive confidence within the first 12 months post-result. Levels of anxiety were in line with population norms [29] and remained relatively stable from enrolment to 12 months post-result. Similar results have been reported up to six months post-result [25, 30]. The large sample size of this study, along with previously reported smaller studies, indicate that RGCS can be delivered at a population-level without causing harm to most who take part [25, 30].
Thus, whilst the act of being offered RGCS does not appear to adversely impact anxiety, receipt of an increased chance result is psychosocially impactful. Several qualitative studies have described emotional responses such as shock and distress in the days and weeks following result disclosure [8,9,10,11]. By 12 months post-result, we observed levels of anxiety at or almost at clinically meaningful levels for participants with new and known increased chance results. Similar levels of anxiety were observed in Mackenzie’s Mission at three months post-result [1]. Our results therefore show that the emotional impact of an increased chance result can persist. This contrasts with research in the context of predictive genetic testing (e.g., for Huntington disease), in which any increased anxiety typically resolves within the first year post-result [31].
The Reproductive Story can provide a conceptual basis to interpreting these findings. A ‘reproductive story’ refers to a narrative a person creates about what it will be like to be a parent [32]. The development of the reproductive story begins in childhood and is shaped by factors such as life experience, the family system, and social and cultural norms [32]. These factors influence expectations around a person’s future reproductive journey [32]. When these expectations are not met, the reproductive story becomes threatened [33]. The term ‘reproductive trauma’ refers to any reproductive event that negatively impacts the reproductive story, such as infertility and perinatal loss [32]. Evidence of reproductive trauma has also been observed amongst reciprocal translocation carriers and their partners [34].
Our findings show that an increased chance result disrupts the reproductive story and can be a form of reproductive trauma [32]. Participants in several RGCS studies, including ours, have described grieving the loss of the expected reproductive path after receipt of an increased chance result [35]. In our study, grief was most apparent for participants using IVF in the absence of known fertility problems. Given the lengthy PGT-M process, participants also described needing to adjust their expectations around when they would conceive. Grieving lost time and the spontaneity of conception has been reported in similar studies, although the magnitude and duration of grief responses post-RGCS have yet to be explored [18, 35].
An important aspect of the Reproductive Story is that a person’s story can be re-written after a reproductive trauma [32]. Our study demonstrates how people begin to revise their reproductive story in the first 12 months post-result by making reproductive decisions. Our findings regarding the relative advantages and disadvantages of IVF with PGT-M or PND reflect what is already known about the complexities of reproductive decision-making [13]. No participants interviewed had considered the use of donor gametes and further research could explore whether attitudes toward this reproductive option change during the reproductive journey. It is also important to note, however, that in Mackenzie’s Mission, couples were offered one funded cycle of IVF with PGT-M. In Australia, and most parts of the world, IVF and PGT-M incur significant expenses which may prevent people from accessing the reproductive option that they most prefer and/or is most value-consistent [14]. Incorporating funding for IVF and PGT-M into RGCS programs would increase equity of access and may also reduce some of the psychosocial impacts associated reproductive decision-making [14].
Our findings also demonstrate that the process of revising the reproductive story is not always straightforward. Whilst 41% of survey respondents with a new increased chance result reported high reproductive confidence, interview findings indicate that this confidence may fluctuate. As people embark on a new reproductive path, additional reproductive traumas may be experienced [32]. This was most markedly observed in the experiences of Paige and Patrick, who described increasing distress with each unsuccessful round of IVF, with the psychosocial impact in part due to their lack of experience with infertility and therefore higher expectations of pregnancy. Further, most of our survey and interview participants had not completed their families by 12 months post-result, meaning their reproductive stories were still evolving. This highlights the importance of RGCS research and programs continuing to capture reproductive outcomes of people with an increased chance result, to understand if and how results are useful for reproductive planning [36]. Several participants were also undecided about their future reproductive pathway and were actively engaging, or anticipating re-engaging, with the decision-making process. This may explain why elevated levels of anxiety have persisted beyond three months post-result [1], rather than reduced.
Although levels of anxiety were elevated, survey respondents who received an increased chance result reported minimal regret about the decision to pursue RGCS. Interviewees similarly described empowerment arising from the reproductive autonomy afforded by their result. Participants in prior studies also generally agreed that the benefits of knowing about an increased chance result outweighed the potential psychological burdens [8, 10, 18]. These findings suggest that, with time, RGCS results add considerable value to people’s reproductive stories.
Implications for practice
Another important consideration in the ongoing implementation of RGCS is how best to support people who receive an increased chance result throughout their reproductive journey. Whilst elevated anxiety is somewhat expected and suggests participants had understood the implications of the result, our findings do highlight a need for long-term support. The value of genetic counselling is well established [15, 18, 37] and practice resources also emphasise the importance of post-result counselling being available [3]. Participants in our study described moments in the first 12 months post-result in which re-engagement with a genetic counsellor may be most beneficial (e.g., deciding whether to continue with IVF), but longer-term research is needed to comprehensively map when, and what, support needs arise over time. Building this evidence-base will inform how to deliver an effective and feasible model of post-result support.
Limitations
Our sample contained an over-representation of people with a tertiary education. Response bias also means that not all experiences were captured. For example, no participant with an increased chance who had a pregnancy affected by the genetic condition responded to the interview invitation. As such, we cannot describe the impact that continuing the pregnancy or having a pregnancy termination has on the reproductive story. Based on prior research however, it is likely that these experiences have significant, and distinctive, psychosocial impacts [9] that warrant examination.
Conclusion
Our study described psychosocial and reproductive impacts of RGCS within the first 12 months post-result within a large research cohort. Most participants had minimal decision regret and high reproductive confidence. However, receiving an increased chance result disrupts people’s reproductive story and as such, anxiety was elevated. By 12 months post-result, participants were at various stages of revising their reproductive story and described finding value in the information from RGCS, given the reproductive empowerment it provided. Using the concept of the Reproductive Story provided a unique lens through which to examine how people navigate increased chance results over time, and further research is now planned to understand how reproductive stories evolve longer-term.
Data availability
De-identified data that support the findings of this study are available from the corresponding author upon request.
References
Kirk E, Delatycki MB, Archibald AD, Tutty E, Caruana J, Halliday JL, et al. Nationwide, couple-based genetic carrier screening. N Engl J Med. 2024;391:1877–89.
The Royal Australian College of General Practitioners. Genomics in general practice. East Melbourne, Victoria: The Royal Australian College of General Practitioners; 2018. https://www.racgp.org.au/getattachment/63568f23-e288-4a0e-a23a-39fbd046cc21/Genomics-in-general-practice.aspx.
Gregg AR, Aarabi M, Klugman S, Leach NT, Bashford MT, Goldwaser T, et al. Screening for autosomal recessive and X-linked conditions during pregnancy and preconception: a practice resource of the American College of Medical Genetics and Genomics (ACMG). Genet Med. 2021;23:1793–806.
The Royal Australian and New Zealand College of Obstetricians and Gynaecologists. C-Obs 63 Genetic Carrier Screening Clinical Guidance Statement. 2019. https://www.rcpa.edu.au/getattachment/768dc44f-618c-4934-89da-6b22c446c240/Guidelines-for-reproductive-geneticcarrier-screen.aspx.
The Royal College of Pathologists of Australasia, Human Genetics Society of Australasia. Guidelines for reproductive genetic carrier screening for cystic fibrosis, fragile X syndrome and spinal muscular atrophy. 2024. https://doi.org/10.1038/ejhg.2015.271.
Henneman L, Borry P, Chokoshvili D, Cornel MC, van El CG, Forzano F, et al. Responsible implementation of expanded carrier screening. Eur J Hum Genet. 2016;24:e1–e12.
Van Steijvoort E, Cassou M, De Schutter C, Dimitriadou E, Peeters H, Peeraer K, et al. Exploring attitudes and experiences with reproductive genetic carrier screening among couples seeking medically assisted reproduction: a longitudinal survey study. J Assist Reprod Genet. 2024:41:451–64.
Tardif J, Pratte A, Laberge A-M. Experience of carrier couples identified through a population-based carrier screening pilot program for four founder autosomal recessive diseases in Saguenay-Lac-Saint-Jean. Prenat Diagn. 2018;38:67–74.
Ioannou L, Delatycki MB, Massie J, Hodgson J, Lewis S. Suddenly having two positive people who are carriers is a whole new thing” - experiences of couples both identified as carriers of cystic fibrosis through a population-based carrier screening program in Australia. J Genet Couns. 2015;24:987–1000.
Beard CA, Amor DJ, Di Pietro L, Archibald AD. “I’m Healthy, It’s Not Going To Be Me”: exploring experiences of carriers identified through a population reproductive genetic carrier screening panel in Australia. Am J Med Genet. 2016;170:2052–9.
Mathijssen IB, Holtkamp KCA, Ottenheim CPE, van Eeten-Nijman JMC, Lakeman P, Meijers-Heijboer H, et al. Preconception carrier screening for multiple disorders: evaluation of a screening offer in a Dutch founder population. Eur J Hum Genet. 2018;26:166–75.
Cannon J, Van Steijvoort E, Borry P, Chokoshvili D. How does carrier status for recessive disorders influence reproductive decisions? A systematic review of the literature. Expert Rev Mol Diagn. 2019;19:1117–29.
Severijns Y, de Die-Smulders CEM, Gültzow T, de Vries H, van Osch LADM. Hereditary diseases and child wish: exploring motives, considerations, and the (joint) decision-making process of genetically at-risk couples. J Community Genet. 2021;12:325–35.
Delatycki MB, Alkuraya F, Archibald A, Castellani C, Cornel M, Grody WW, et al. International perspectives on the implementation of reproductive carrier screening. Prenat Diagn. 2020;40:301–10.
Archibald AD, Smith MJ, Burgess T, Scarff KL, Elliott J, Hunt CE, et al. Reproductive genetic carrier screening for cystic fibrosis, fragile X syndrome, and spinal muscular atrophy in Australia: outcomes of 12,000 tests. Genet Med. 2018;20:513–23.
Johansen Taber KA, Beauchamp KA, Lazarin GA, Muzzey D, Arjunan A, Goldberg JD. Clinical utility of expanded carrier screening: results-guided actionability and outcomes. Obstet Gynecol Surv. 2019;74:582–4.
Ghiossi CE, Goldberg JD, Haque IS, Lazarin GA, Wong KK. Clinical utility of expanded carrier screening: reproductive behaviors of at-risk couples. J Genet Couns. 2018;27:616–25.
Richardson E, McEwen A, Newton-John T, Crook A, Jacobs C. Outcomes of importance to patients in reproductive genetic carrier screening: a qualitative study to inform a core outcome set. J Pers Med. 2022;12:1310.
Richardson E, McEwen A, Newton-John T, Jacobs C. Defining core outcomes of reproductive genetic carrier screening: a Delphi survey of Australian and New Zealand stakeholders. Prenat Diagn. 2023;43:1150–65.
Richardson E, McEwen A, Newton-John T, Crook A, Jacobs C. Systematic review of outcomes in studies of reproductive genetic carrier screening: towards development of a core outcome set. Genet Med. 2022;24:1–14.
Archibald AD, McClaren BJ, Caruana J, Tutty E, King EA, Halliday JL, et al. The Australian reproductive genetic carrier screening project (Mackenzie’s Mission): design and implementation. J Pers Med. 2022;12:1781.
Creswell JW, Plano Clark VL. Choosing a mixed methods design. Designing Conducting Mixed Methods Res. 2011;2:53–106.
Thorne S. Interpretive description: qualitative research for applied practice. New York: Routledge; 2016.
Marteau TM, Bekker H. The development of a six-item short-form of the state scale of the Spielberger State—Trait Anxiety Inventory (STAI). Br J Clin Psychol. 1992;31:301–6.
Birnie E, Schuurmans J, Plantinga M, Abbott KM, Fenwick A, Lucassen A, et al. Couple-based expanded carrier screening provided by general practitioners to couples in the Dutch general population: psychological outcomes and reproductive intentions. Genet Med. 2021;23:1761–8.
Brehaut JC, O’Connor AM, Wood TJ, Hack TF, Siminoff L, Gordon E, et al. Validation of a decision regret scale. Medical Decis Mak. 2003;23:281–92.
Palinkas LA, Horwitz SM, Green CA, Wisdom JP, Duan N, Hoagwood K. Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Adm Policy Ment Health. 2015;42:533–44.
Braun V, Clarke V, Hayfield N, Davey L, Jenkinson E. Doing reflexive thematic analysis. In: Bager-Charleson S, McBeath A, editors. Supporting research in counselling and psychotherapy: qualitative, quantitative, and mixed methods research. Cham: Springer International Publishing; 2022.
Crawford J, Cayley C, Lovibond PF, Wilson PH, Hartley C. Percentile norms and accompanying interval estimates from an Australian general adult population sample for self-report mood scales (BAI, BDI, CRSD, CES-D, DASS, DASS-21, STAI-X, STAI-Y, SRDS, and SRAS). Aust Psychologist. 2011;46:3–14.
van Dijke I, Lakeman P, Sabiri N, Rusticus H, Ottenheim CPE, Mathijssen IB, et al. Couples’ experiences with expanded carrier screening: evaluation of a university hospital screening offer. Eur J Hum Genet. 2021;29:1252–8.
Broadstock M, Michie S, Marteau T. Psychological consequences of predictive genetic testing: a systematic review. Eur J Hum Genet. 2000;8:731–8.
Jaffe J. Reproductive trauma: psychotherapy with clients experiencing infertility and pregnancy loss. Washington, DC, US: American Psychological Association; 2024.
Jaffe J. The reproductive story: Parents’ possible selves and how things should have been. Reproductive trauma: psychotherapy with clients experiencing infertility and pregnancy loss, 2nd ed. Washington, DC, US: American Psychological Association; 2024.
Cifuentes Ochoa M, Flowers NJ, Pertile MD, Archibald AD. “It becomes your whole life”—exploring experiences of reciprocal translocation carriers and their partners. J Genet Couns. 2023;32:1057–68.
Richardson E, McEwen A, Newton-John T, Crook A, Jacobs C. Incorporating patient perspectives in the development of a core outcome set for reproductive genetic carrier screening: a sequential systematic review. Eur J Hum Genet. 2022;30:756–65.
Henneman L. Genetic carrier screening — call for a global mission. New Engl J Med. 2024;391:1947–8.
Edwards S, Laing N. Genetic counselling needs for reproductive genetic carrier screening: a scoping review. J Pers Med. 2022;12:1699.
Acknowledgements
We would like to thank the participants who generously gave their time to complete the survey and to share their stories with us through interviews. We would also like to acknowledge the members of the Mackenzie’s Mission investigator team who helped make Mackenzie’s Mission possible.
Funding
The Australian Reproductive Genetic Carrier Screening Project (Mackenzie’s Mission) was funded and sponsored through the Australian Government MRFF, Genomic Health Futures Mission (GHFMRCMM000001) and supported by Australian Genomics (NHMRC GNT2000001). Erin Tutty is supported by an Australian Government Research Training Program scholarship and a MCRI PhD Top Up Scholarship. Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and Affiliations
Contributions
Conceptualization: All authors. Data curation: N/A. Formal analysis: ET, BJM, ADA, SL. Funding: ET, EPK, NGL & MD. Investigation: N/A. Methodology: ET, ADA, BJM, SL & MD. Project administration: ET, TB & JC. Software: N/A. Resources: ET, BJM, ADA, SL & MD. Supervision: BJM, ADA, SL & MD. Validation: N/A. Visualization: ET. Writing – original draft: ET. Writing – review and editing: All authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The Royal Children’s Hospital Human Research Ethics Committee (HREC) provided multi-centre ethics approval via the National Mutual Acceptance system (HREC/53433/RCHM-2019). Approval to conduct this study at sites outside of the scheme was also obtained from the relevant HRECs. Informed consent was required and obtained for all participants.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tutty, E., McClaren, B.J., Lewis, S. et al. Revising the reproductive story: psychosocial and reproductive impacts 12 months after reproductive genetic carrier screening. Eur J Hum Genet 33, 1035–1043 (2025). https://doi.org/10.1038/s41431-025-01903-z
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41431-025-01903-z
This article is cited by
-
Genomic medicine in full bloom: a summer farewell issue
European Journal of Human Genetics (2025)