Abstract
Oestrogen and progesterone fluctuate cyclically in women throughout their adult lives. Although these hormones cross the blood-retinal barrier and bind to intraocular receptors, their effects remain unclear. We present the first review to date on associations between posterior pole structures—specifically the macula, choroid, and optic disc—and both the menstrual cycle and post-menopausal period, utilising multimodal imaging techniques in healthy adult non-pregnant women. We excluded studies on contraception and hormonal replacement therapy, focusing solely on physiological associations. Despite the comprehensive scope of our review, limited data and inconsistent reporting among studies prevented the establishment of meaningful trends. Across menstrual cycle phases, choroidal thickness (CHT) was the most consistently reported parameter, with thinning during the luteal phase compared to the follicular phase. Conversely, no significant differences were observed in macular or disc morphology across the cycle, likely reflecting a preserved structure despite potential fluctuations in blood flow and perfusion. Studies comparing pre- and post-menopausal associations, after adjusting for age or body mass index (BMI), failed to reveal meaningful trends, highlighting the difficulty in separating the effect of age from hormonal declines in older women. Understanding how hormonal cycles impact the posterior pole in women is crucial for addressing sex differences in various ocular pathologies. Research on female-specific factors is still sparse, and interestingly, the majority of affiliations in the reviewed articles did not originate from regions with the highest biomedical research funding and publication rates. We encourage further studies focusing on female-specific variables and provide recommendations for future designs.
Similar content being viewed by others
Introduction
Female sex steroid hormones, including oestrogen and progesterone, undergo cyclic changes in women from 13 [1] to 48–50 years of age [2], and are influenced by factors such as hormonal contraception, pregnancy, disease, medication, or extreme conditions. In the years preceding menopause, menstrual fluctuations become more irregular [3,4,5], until a permanent hormonal decline is established. Both oestrogen and progesterone cross the blood-retinal barrier [6] and have receptors in various parts of the eye, including the cornea, lens, iris, ciliary body, and retina, demonstrated in both rodents and humans [7, 8]. Oestrogen receptor alpha (ORα) was first identified in the neurosensory retina and retinal pigment epithelium (RPE) in post-mortem eyes of young women in 1999 [9]. Later, mRNA for ORα, oestrogen receptor beta (ORβ), and progesterone were discovered in the retina of both female and male subjects aged between 52 and 84 years, with variable expression levels [10, 11].
Sex-related variation in macular structure is apparent, yet still poorly understood. Women exhibit thinner retinas in both adults [12,13,14,15] and children [16], with differences in individual sublayers, particularly in the inner retina [15, 17,18,19]. Morphologically, they consistently present a broader and shallower foveal pit across different ethnicities compared to male counterparts [20,21,22,23,24,25,26]. While ovarian hormones predominate in women and are known to influence neuronal plasticity and growth [27,28,29], it remains unclear whether these retinal sex differences arise from true physiological variation or potential bias in retinal image scale estimation [25, 30] due to unaccounted sex disparities in cornea topography [31] and shorter axial length [32].
On the other hand, women also exhibit higher susceptibility or greater protection to some retinal diseases across different hormonal phases. Postmenopausal women are reported to have a higher incidence and faster progression of posterior vitreous detachment than men of the same age [33, 34] and idiopathic macular holes are more frequent in women, across different ethnicities [35,36,37,38]. Progestogenic hormones were shown to modulate pro-survival pathways in the retina in experimental acute brain injury and retinitis pigmentosa models [39,40,41]. Furthermore, in age-related macular degeneration (AMD), research suggested a beneficial role of oestrogen due to its antioxidant effects, with longer exposure to oestrogen or hormone replacement therapy (HRT) in post-menopause associated with a lower risk of developing late AMD [42,43,44,45]. Finally, female sex steroid hormones also seem to have a protective effect on the optic disc. In primary open-angle glaucoma, a longer reproductive period, with early menarche and/or late menopause, was associated with a reduced risk of disease [46,47,48] and conversely, early menopause was linked to a higher prevalence of glaucoma [49]. The prevailing hypothesis is that oestrogen may modulate aqueous humour dynamics and vascular tone through nitric oxide synthase, with relatively consistent associations between oestrogen-only HRT use and lower intraocular pressure [48].
In general, studies investigating ocular sex differences often demonstrate variability in study designs and reporting methods, with considerable risk of bias [48]. Understanding the physiological hormonal impact of fluctuating sex steroid hormones across women’s lifespans is a crucial first step in comprehending sex differences and standardising study methodologies. Menstrual cycle phases and menopausal status can be used as proxies for hormonal action [50, 51] and are frequently neglected. This is the first review to date to provide a comprehensive overview of associations between posterior pole structures—specifically the macula, choroid, and optic disc—and the menstrual cycle and post-menopausal period, utilising multimodal imaging techniques in healthy adult women.
Methods
We conducted this scoping review to offer an overview and identify gaps in knowledge within the field of associations between menstrual and menopausal statuses and macular and disc parameters in healthy adult women. We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews (PRISMA-ScR) statement [52] and their checklist adapted to this work is included in Supplementary Material 1. The protocol of this scoping review was registered in the Open Science Framework (OSF) platform on the 18th of February 2024 and is available at osf.io/bfwn3.
Search methods for identifying studies
We developed a comprehensive electronic Boolean search string and applied it to two peer-reviewed biomedical databases: PubMed (www.ncbi.nlm.gov/pubmed) and Embase (https://ovidsp.dc1.ovid.com/). We constructed our search string by combining three concepts: first, macular and disc morphology; second, imaging modalities and related structural changes; and third, cycles influenced by female hormones. The complete search string for PubMed is provided in Supplementary Material 2, and a comparable search was applied in Embase. To maximise the scope, a forward citation search was conducted to identify further relevant papers, and keywords were extracted from grey literature repositories. The last search across all electronic databases was conducted on the 18th of February 2024.
Eligibility criteria for considering studies for this review
We included studies that focused on healthy adult women, exploring differences and associations with retina and disc morphology across the menstrual cycle and menopausal-related factors. These studies assessed macular and/or disc morphology using current clinical multi-imaging modalities and could date back to the beginnings of the databases used. We excluded studies involving pregnancy, breastfeeding, hormonal contraception, HRT, treatments or supplementation of any kind. Additionally, we excluded studies that investigated cycle and menopause changes related to systemic or ocular disease or focused on differences between sexes rather than differences within women’s stages. However, if a study addressed any of these exclusions but also included a segment on healthy women, we included the study, considering only the relevant section. Experimental approaches, as well as functional or haemodynamic studies, were excluded.
Study selection
All identified citations were downloaded from PubMed as.nbib, from Embase as.ris and a merged spreadsheet was then collated using Paperpile (© Paperpile LLC 2023). After eliminating duplicates, title and abstract screening underwent validation by two reviewers (A.P.R.R. and E.I.), with any discrepancies resolved through arbitration by a third reviewer (P.J.P). Initially, we excluded non-human or basic science studies, non-retrievable abstracts, and non-English publications. Subsequently, we thoroughly reviewed the remaining abstracts and, when needed, the full-text versions against our inclusion and exclusion criteria. Articles facing exclusion were categorised as off-topic and further divided into 9 subcategories: (1) contraception, (2) pregnancy, (3) other hormonal factors (such as studies on the menstrual cycle and menopause involving other organs or utilising haemodynamic or experimental modalities), (4) disease-related studies, (5) prematurity, (6) other paediatrics, (7) sex differences, (8) hormonal treatment (encompassing HRT and other hormonal treatments such as androgens or oestrogen receptor modulators like tamoxifen), and (9) other treatment-related studies. The studies to be included were divided into two groups: (1) studies focusing on the menstrual cycle and (2) studies comparing pre- and post-menopause in healthy adult women. In cases where articles could belong to more than one category, only the predominant category was selected.
Data collection and risk of bias assessment
To offer a comprehensive overview of all incorporated sources, participant details, test characteristics, and key outcomes from the included studies were summarised in a standardised data collection template. We extracted general aspects such as title, authors, publication year, study design, journal and the country of affiliation of the main authors. Regarding the population, we collected data on sample size, ethnicity, age, and other specific characteristics. We registered imaging modalities, topographical region studied, methods of measurement extraction from the images, time of the day of the examination and laterality. Regarding the hormonal factors, we identified the main phase within the menstrual or post-menopausal stages as well as subphases, methods of phase measurement and confirmation, parity and other variables. We documented the main statistical tests used and whether adjustments were made. The Newcastle-Ottawa Score (NOS) was employed to evaluate the risk of bias in the included studies, assessing selection, comparability and exposure/outcome criteria [53]. The NOS scale for Case-Control Studies was adapted for cross-sectional studies, while the scale for Cohort Studies was adapted for longitudinal studies. Each article was assigned a specific score ranging from zero to nine stars, with a higher number of stars indicating a higher-quality study. The scoring scale can be found in Supplementary Material 3. Finally, if more than three studies provided quantitative measures of the same region and hormonal stage, a meta-analysis was conducted and visually presented as a forest plot. Standardised mean differences in the thickness of specific retinal areas between groups and 95% confidence intervals were obtained using a random-effects model. The heterogeneity of effect size estimates across studies was assessed using the I2 index. We utilised R version 4.3.0, released on the 21st of April 2023. Data were extracted from published articles accessible through online libraries affiliated with the authors’ organisations.
Results
Search and selection of data
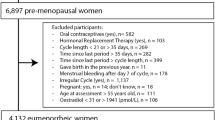
The full study selection process is presented as a PRISMA-ScR flow diagram (Fig. 1). We identified 612 references for analysis: 407 from Embase, 204 from PubMed, and 1 manually selected from grey literature. After removing duplicates, 485 underwent a first screening phase conducted in parallel by two reviewers (A.P.R.R. and E.I.) using a spreadsheet with metadata and abstracts. Disagreements were resolved through re-arbitration. The spreadsheet containing the 485 references and their subcategorisation as well as an accompanying README file are available online in our OSF project folder titled ‘Article selection’ (osf.io/bfwn3). A total of 391 items were retrieved in full and assessed for their compatibility with our inclusion/ exclusion criteria and a total of 14 studies met the criteria [54,55,56,57,58,59,60,61,62,63,64,65,66,67]. Among these, 13 [54,55,56,57,58,59,60,61,62,63,64,65,66] were original research articles published in peer-reviewed journals and 1 was an original research abstract from an international conference [67]. A total of 8 original studies [54,55,56,57,58, 64, 65, 67] examined menstrual cycle factors. Among them, a cross-sectional study explored relationships with cycle length and age of menarche [64] and 7 longitudinal studies investigated morphological changes across menstrual cycle phases [54,55,56,57,58, 65, 67]. The final 6 studies compared pre-menopausal and spontaneous post-menopausal women, in a cross-sectional design [59,60,61,62,63, 66]. A comprehensive overview of the key features of the incorporated studies can be found in Supplementary Material 4 and online in our OSF project folder titled ‘Included studies’ (osf.io/bfwn3).
Study groups and ethnicity
In studies on menstrual cycle phases, Turkey led with the highest number of reports (4 articles) [54,55,56, 67], followed by Australia [64], the United States (US) [57], Japan [65], and China [58], each contributing one study. Only two studies provided information on participant ethnicity. The Australian study referenced ‘predominantly white ethnicity’ [64] while the US study provided demographic data on ethnicity. However, the small sample size (28 menstruating women) limited meaningful comparisons across ethnic groups [57]. Regarding studies on menopausal status, three studies were conducted in Turkey [59,60,61], two in Egypt [62, 63] and one in Nigeria [66]. None of the studies comparing pre- and post-menopause mentioned the ethnicity of the participants.
Associations with the menstrual cycle
Table 1 provides a comprehensive overview of the main findings for the cited papers associating the menstrual cycle with macular, choroidal and disc structures.
Macula
Ulaş et al. conducted a study involving 23 healthy nulliparous females undergoing menstrual cycles, with a mean age of 26 ( ± 3 SD) years, using optical coherence tomography (OCT) at the follicular, ovulatory, and mid-luteal phases within one menstrual cycle. They found no statistical differences in total retinal thickness (TRT) or macular retinal nerve fibre layer (RNFL) [55]. Fortepiani et al. followed 28 women with a mean age of 26 years (±5 SD), of whom 16 were observed during both the first and second halves of a menstrual cycle, while the remaining 12 women were monitored over two or three cycles. They found no statistical differences in foveal thickness between the follicular and luteal phases on OCT [57]. In OCT angiography (OCTA) studies, Asri S.N. et al. observed no statistically significant differences in vessel density of the superficial capillary plexus (SCP), deep capillary plexus (DCP), and foveal avascular zone (FAZ) area between the follicular, ovulatory and mid-luteal phases [68]. On the other hand, Guo et al. conducted a study involving 62 women aged 27 (±2 SD) years, where they investigated the early-follicular, ovulatory and luteal phases controlling for ovulation through urinary luteinising hormone (LH) home-monitoring and adjusting the analysis to age, mean arterial pressure, spherical equivalent, axial length, and intraocular pressure. This study found no significant difference in vessel density of SCP or FAZ. However, they did observe that vascular density in the DCP within the nasal and inferior subfields was significantly lower during ovulation compared to the follicular or luteal phases (p < 0.001) [58].
Optic disc
In the aforementioned study, Ulaş et al. observed no statistically significant differences in peripapillary RNFL thickness on OCT within cycle phases among healthy young women [55]. Additionally, Akar et al. conducted a study involving 38 nulliparous, eumenorrheic women with a mean age of 26 (±4 SD) years, using serological hormonal confirmation of the cycle phase during follicular, ovulatory and late-luteal phases. They also found no significant difference in peripapillary RNFL thickness on OCT [54]. Concerning disc cupping, the latter group found an increased cup-to-disc ratio (CDR) and correspondingly decreased neuroretinal rim area during the late-luteal phase compared to the follicular and ovulatory phases (p < 0.001), with no significant differences observed between the follicular and ovulatory phases [54]. Finally, in a cross-sectional study, 10 females who had given birth at least once had smaller CDR (p < 0.001) and larger neuroretinal rim (p = 0.010) than nulliparous women, suggesting a protective effect of past pregnancies on CDR. However, no relation to the age of menarche or cycle length was found [64].
Choroid
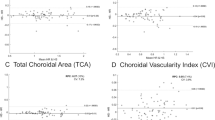
Three studies consistently found a significantly thinner subfoveal CHT during the luteal phase compared to follicular and ovulatory phases using OCT with enhanced depth imaging (EDI). A spreadsheet with the extracted quantitative data is available at our OSF page (osf.io/bfwn3) in the folder ‘Meta-Analysis’. A forest plot of the meta-analysis of these results can be found in Fig. 2. The random-effects model, based on the 3 studies [55, 56, 65], estimated a pooled effect size of −0.43 (95% CI: −0.79 to −0.08; p = 0.02), indicating a significant difference in subfoveal CHT between the two phases. The heterogeneity analysis showed low total heterogeneity (I2 = 12.53%), suggesting that ~12.53% of the total variability in effect sizes was due to true differences between studies rather than chance (p = 0.35). The study with the highest impact on the meta-analysis was Aşikgarip et al. which accounted for almost half of the participants, with a sample size of 36 [56] out of a total of 74 individuals. Additionally to the subfoveal region, they also measured a reduction in mid-luteal CHT in both the mean nasal and mean temporal quadrants [56]. In all three studies, healthy women were followed within a cycle and the time of examination was reported and remained consistent for each study. One study conducted examinations between 12 a.m. and 1 p.m. [55], another between 9 a.m. to 12 a.m. [56], and the last between 12 a.m. and 3 p.m., covering different times of the day.
Associations with the menopausal status
Table 2 provides a comprehensive overview of the main findings of the cited papers associating menopausal status with macular, choroidal and disc structure.
Macula
Four studies investigated macular TRT in both pre and post-menopausal women and did not find any statistically significant differences between the two groups [59,60,61, 63]. In the study by Ataş et al., which involved 72 pre-menopausal and 72 post-menopausal women with mean ages of 40 ( ± 8 SD) and 57 ( ± 5 SD) years respectively, a thinner TRT in all quadrants was observed in the post-menopausal group. However, this difference lost significance after age adjustments [60]. Similarly, Alpogan and Tekcan analysed 94 women, finding no statistically significant difference in macular ganglion cell complex (GCC) relating to menopausal status adjusting for age and BMI [59]. Finally, another study investigated macular ganglion cell layer and RNFL thickness in swept-source OCT in 45 pre-menopausal women and 40 post-menopausal women. The mean age of the two groups was very similar, with pre-menopausal women averaging 46 years and post-menopausal women 49 years. They found no statistically significant difference relating to menopause [61]. In the same study, OCTA revealed no statistically significant difference in vessel density (VD) for both SCP and DCP. However, it noted a significant increase in FAZ area in post-menopausal women (p = 0.013) in both SCP and DCP, as well as a reduction in choriocapillaris VD (p = 0.045) [61].
Optic disc
Peripapillary RNFL thickness between pre- and post-menopausal women was investigated in three studies and did not show significant differences in an unadjusted analysis [63], with or without age adjustment in another study [60] of after accounting for BMI [59]. Fathy et al. investigated 50 pre-menopausal and 50 post-menopausal women with peripapillary OCTA and found that peripapillary VD was significantly thinner in post-menopause (p < 0.001) with oestrogen level being an independent predictor for whole image, peripapillary, superior and temporal VD [62]. This study consistently investigated pre-menopausal women in the mid-follicular phase and measured oestrogen levels, in addition to questionnaire information.
Choroid
Four studies compared the CHT of pre- and post-menopausal women [61, 63, 66, 69], as depicted in the meta-analysis shown in Fig. 3. Three of them reported a statistically significant reduction in the post-menopausal group, with significance persisting after age adjustment in one study (p = 0.005) [60]. On another hand, Cetinkaya & Pota found no difference in CHT between the two groups, even without age adjustment [61]. Neither of these studies referred to the time of the CHT measurement, not considering diurnal variation within individuals but all of them used an EDI system.
Risk of bias analysis and general considerations
Menstrual cycle
Different methods were used to estimate menstrual cycle phases and the specific phases analysed also varied throughout the literature. While some studies compared women across two phases (follicular and luteal) [57, 65], others considered three phases by incorporating ovulation [54,55,56, 58, 67], with some specifying early, mid, or late subphases. We used the NOS criteria to assert the quality of nonrandomised studies and perform a risk of bias analysis of our included articles. The results are presented in Supplementary Material 5. According to the NOS, a high-quality study typically requires three or four stars in the selection domain, one star in the comparability domain, and two or three stars in the outcome domain. Among the six longitudinal studies assessing the menstrual cycle, only one study by Guo et al. [58] achieved a good quality score of 8 out of 9 stars. Its strength lay in the fact that it not only excluded contraception, HRT, and pregnancy but also utilised both self-report and hormonal confirmation of the cycle with at-home LH urinary tests. Furthermore, they accounted for confounding factors such as mean arterial pressure, spherical equivalent, axial length, and intraocular pressure in their analysis. Fortepiani et al. [57] and Akar et al. [54] were the next highest-scoring studies, each receiving 6 out of 9 stars. However, Fortepiani’s study relied solely on self-reported cycle phases, while Akar’s study did not make adjustments for confounders in their analysis. In general, all studies utilised self-report to calculate the cycle phase with only two studies confirming it with hormonal tests: one with temperature measurements and serum oestradiol, progesterone and luteinising hormone levels [54], and another measuring peak LH concentration in urine at home [58]. All studies considered only eumenorrheic women but exclusion criteria also varied. Two of them included only nulliparous individuals [54, 55], while five did not provide information on the number of previous pregnancies. Only two studies explicitly excluded lactating women [54, 56], four studies explicitly excluded participants using hormonal therapy and contraception [54,55,56, 58], while two studies permitted contraception and adjusted for it in their analyses [57, 64]. Included women were mostly in their twenties, with an average age ranging from 20 to 27 years old. All studies analysed ocular coherence-based metrics, and results for macular and optic disc parameters were automatically extracted using in-built software devices, except for CHT, which was manually measured. One study calculated the choroidal vascular index (CVI) by binarising EDI-OCT images with Image-J software [56].
Menopause
In the six menopausal studies, three used self-reporting to categorise participants [59, 61, 63], defining post-menopausal women as those who had experienced their last period spontaneously at least 12 months ago. Two studies employed serological tests, with one considering follicle-stimulating hormone (FSH) serum levels (>40 IU/L) [60] and the other serum oestradiol levels [62], while one study simply established an age cut-off at 45 years old [66]. Within the pre-menopausal participant groups, only one study explicitly identified the phase of the menstrual cycle, choosing the mid-follicular phase [62]. Five studies uniformly excluded HRT in their analyses [59,60,61,62,63], while only one study accounted for the influence of hormonal contraception [62]. The average age of post-menopausal women ranged from 48 to 60 years old. For the premenopausal group, the mean age ranged from 40 to 46 years old, nearing perimenopausal age, except for one study that included younger participants with a mean age of 30 (±3 SD) years old [63]. Similarly to menstrual cycle studies, OCT and OCTA results for macular and disc parameters were automatically extracted using the manufacturer’s built-in software, while choroidal thickness was manually measured in all studies. Two of these cross-sectional studies on menopause achieved good quality scores on the NOS scale [62, 69] and further results can be found in Supplementary Material 6. Both studies adjusted their analysis for age, but neither could achieve any significant results after this adjustment.
Discussion
This review explores structural changes in the posterior pole during healthy women’s hormonal cycles using multimodal imaging. The posterior pole comprises multiple structures, and although our review did not restrict imaging modalities or regions, encompassing the macula, optic disc, and choroid, limited data and inconsistent reporting presented challenges in establishing meaningful associations from the included studies. Interestingly, studies in this review were mainly conducted by groups from Turkey and Egypt, with limited articles from countries where biomedical research funding and publications most commonly originate [70,71,72]. Understanding how hormonal cycles impact the posterior pole is crucial for addressing sex differences in pathology, such as those reported in vitreomacular disease or glaucoma, as previously highlighted. Globally, two out of three blind individuals are women [73]. While influenced to some extent by socioeconomic factors like healthcare accessibility and longer life expectancy, the lack of research on female-specific factors should not be ignored.
Throughout the menstrual cycle, the most consistently reported morphological change in the studies was observed in CHT. Subfoveal CHT was consistently thinner in the luteal phase compared to the follicular phase in all three studies. The authors hypothesised that this phenomenon might be attributed to vasoconstriction caused by increased sympathetic activity during the luteal phase when both oestradiol and progesterone are elevated. However, hemodynamic studies present conflicting evidence compared to these morphological findings. One of the most consistently observed effects of oestrogens and progesterone is an increase in vasodilator tone [74, 75], dependent on endothelial nitric oxide (NO) [76]. Oestradiol appears to enhance beta-adrenergic receptor-mediated vasodilation, counteracting alpha-adrenergic vasoconstriction [77]. This increase in sympathetic outflow was suggested to compensate for a greater NO release, maintaining balanced vascular resistance [78]. Karadeniz et al. conducted a study on 23 healthy women, examining retrobulbar circulation with serial colour Doppler ultrasonography during a normal menstrual cycle, and found that hemodynamic parameters remained stable throughout the menstrual cycle [79]. Another study by Haneda et al. proposed a decrease in choroidal blood flow velocity during the late follicular phase, indicating a potential vessel calibre increase in this phase [80]. The combined sample size from the three studies examined in our review, focusing on CHT totalled only 74 women. Although the time of measurement was standardised within each study, since there is no consensus, it does not always overlap between studies, introducing the potential confounding of diurnal CHT variation into this analysis. To enhance the generalisability of findings, more studies are necessary, with larger sample sizes and more robust research methodologies in future investigations.
Regarding macular and disc morphology, there were no significant changes across the menstrual cycle in any of the OCT layers analysed (TRT, GCC, and macular or peripapillary RNFL). This suggests a conserved structure despite potential fluctuations in blood flow and perfusion. There was not enough evidence to draw any trends on CDR, VD and FAZ on OCTA due to the limited number of studies and conflicting evidence. OCTA studies would be particularly promising in adding information to the circulation and autonomic regulation across the cycle.
Studies on pre- vs. post-menopausal changes were only cross-sectional, and as a group, they did not reveal any meaningful trends when adjusting their analysis for the effect of age or BMI. Since post-menopause is a later life stage, separating the effect of age from the hormonal decline is challenging. Their standardisation was poorer, without reference to the cycle phase of pre-menopausal women and without accounting for diurnal variations of choroidal thickness.
There are multiple limitations to this review. The small number of publications and the inconsistent methods used in the different studies to measure the cycle and menopause made it challenging to draw meaningful relationships. The inconsistent exclusion criteria made populations and research questions slightly different, even within the same topic. Most studies relied solely on questionnaire information to estimate hormonal levels, and the phases of the cycle analysed also differed. Many analyses were not adjusted for important confounders, such as age in menopausal studies, and there were no longitudinal studies on pre- and post-menopause or accounting for the hormonal irregularities typical of perimenopause. Longitudinal studies on the cycle never followed more than one cycle and did not consider intra-individual variability.
Recommendations for future studies
To explore the effects of ovarian hormones, researchers routinely take advantage of life’s natural fluctuations in oestradiol and progesterone. To ensure the homogeneity of the study population when studying physiological variations within the menstrual cycle or menopause, it is important to exclude or account for women in different hormonal environments, such as those experiencing pregnancy, lactation, perimenopause, hormonal treatments, HRT, or contraception.
Determining menstrual cycle phase
Various methods exist for reporting menstrual cycle phases, each with its strengths and weaknesses. These include relying solely on self-reported information, utilising published ranges for ovarian hormone levels (with direct assays available in saliva, blood serum, blood plasma, and urine), combining self-report with hormonal levels or basal body temperature, and examining within-person changes in ovarian hormone levels collected multiple times over the cycle [50, 51, 81]. While self-reporting alone is very common, it is the weakest method in isolation. However, if the calculation of the menstrual cycle phase is transparent and standardised, using it as a proxy for hormonal action could be acceptable since it is the most cost-effective and minimally burdensome for participants [50, 51, 81]. Since it lacks the precision to identify specific cycle subphases, such as early, mid, or late phases, when used in isolation, the identification of ovulation exhibits the lowest accuracy and should not be considered [81]. Finally, it is recommended that cycle tracking by the participants be initiated a couple of months before answering self-report questionnaires and that ovarian hormonal levels are used in conjunction with self-reporting [50, 51, 81].
Determining menopausal status
Spontaneous menopause is defined as the permanent cessation of menstrual periods, established retrospectively after a woman has undergone 12 consecutive months of amenorrhoea without any apparent alternative cause [82]. Determining menopausal status is a more straightforward process, often defined by questionnaire. Longitudinal studies would be particularly valuable for understanding the impact of perimenopause through menopause within individuals, extending beyond chronological age. Caution is advised when including participants in perimenopause as controls since this period has irregular cycle lengths and anovulatory cycles. In the case of potential perimenopausal participants, the staging system ‘Stages of Reproductive Aging Workshop (STRAW + 10)’ for participants aged 40 and above helps in calculating their menopausal status [83]. Finally, in studies exploring pre- and post-menopausal changes, maintaining consistency in the menstrual cycle phase of the pre-menopausal group is crucial for obtaining reliable and comparable results.
Contraception
In the investigation of the natural menstrual cycle or menopause, it is recommended that cycling participants have experienced a minimum of two natural cycles after discontinuing hormonal contraceptives [81]. This approach allows for a more accurate representation of the physiological changes associated with the cycle. Furthermore, consistent exclusion of all types of hormonal contraception and not only oral contraceptives, including hormonal intra-uterine devices, implants, or injections, is essential to minimise confounding variables and enhance the internal validity of the research findings.
Other considerations
In CHT studies, it is crucial to account for the time of day, as diurnal changes can influence measurements and contribute to variations in outcomes [84]. Additionally, ethnicity should always be reported and accounted for due to normal variations within individuals from different groups [85]. Lastly, we encourage equally publishing negative results since this will contribute to a more comprehensive understanding of the field, avoiding publication bias and providing a well-rounded perspective that benefits all.
In summary, additional well-conducted, longitudinal cohort studies better describing female-specific variables are needed to evaluate the association between changes in posterior pole structures during the menstrual cycle and menopause. This could help in improving our understanding of the pathophysiology of posterior pole disorders in women.
References
Rivas Paz M, Torres Mendoza BM, Torres Castillo N. Age of the onset of menarche and its complications: a literature review. Int J Gynaecol Obstet. 2023;162:244–55.
Kojima G, Taniguchi Y, Ogawa K, Aoyama R, Urano T. Age at menopause is negatively associated with frailty: a systematic review and meta-analysis. Maturitas 2022;165:94–99.
Mitake S, Wada-Hiraike O, Kashiwabara K, Nakamura A, Nasu R, Hine M, et al. Distribution of the follicular and luteal phase lengths and their age-dependent changes in Japanese women: a large population study. Reprod Med Biol. 2023;22:e12516.
Li H, Gibson EA, Jukic AMZ, Baird DD, Wilcox AJ, Curry CL, et al. Menstrual cycle length variation by demographic characteristics from the Apple Women’s Health Study. NPJ Digit Med. 2023;6:100.
Bull JR, Rowland SP, Scherwitzl EB, Scherwitzl R, Danielsson KG, Harper J. Real-world menstrual cycle characteristics of more than 600,000 menstrual cycles. NPJ Digit Med. 2019;2:83.
Toda R, Kawazu K, Oyabu M, Miyazaki T, Kiuchi Y. Comparison of drug permeabilities across the blood-retinal barrier, blood-aqueous humor barrier, and blood-brain barrier. J Pharm Sci. 2011;100:3904–11.
Gupta PD, Johar K Sr, Nagpal K, Vasavada AR. Sex hormone receptors in the human eye. Surv Ophthalmol. 2005;50:274–84.
Wickham LA, Gao J, Toda I, Rocha EM, Ono M, Sullivan DA. Identification of androgen, estrogen and progesterone receptor mRNAs in the eye. Acta Ophthalmol Scand. 2000;78:146–53.
Ogueta SB, Schwartz SD, Yamashita CK, Farber DB. Estrogen receptor in the human eye: influence of gender and age on gene expression. Investig Ophthalmol Vis Sci. 1999;40:1906–11.
Munaut C, Lambert V, Noël A, Frankenne F, Deprez M, Foidart J-M, et al. Presence of oestrogen receptor type β in human retina. Br J Ophthalmol. 2001;85:877–82.
Marin-Castaño ME, Elliot SJ, Potier M, Karl M, Striker LJ, Striker GE, et al. Regulation of estrogen receptors and MMP-2 expression by estrogens in human retinal pigment epithelium. Investig Ophthalmol Vis Sci. 2003;44:50–59.
Kashani AH, Zimmer-Galler IE, Shah SM, Dustin L, Do DV, Eliott D, et al. Retinal thickness analysis by race, gender, and age using Stratus OCT. Am. J Ophthalmol. 2010;149:496–502.e1.
Song WK, Lee SC, Lee ES, Kim CY, Kim SS. Macular thickness variations with sex, age, and axial length in healthy subjects: a spectral domain–optical coherence tomography study. Investig Ophthalmol Vis Sci. 2010;51:3913–8.
Patel PJ, Foster PJ, Grossi CM, Keane PA, Ko F, Lotery A, et al. Spectral-domain optical coherence tomography imaging in 67 321 adults: associations with macular thickness in the UK biobank study. Ophthalmology. 2016;123:829–40.
Hashmani N, Hashmani S, Murad A, Mahmood Shah SM, Hashmani M. Assessing reproducibility and the effects of demographic variables on the normal macular layers using the Spectralis SD-OCT. Clin Ophthalmol. 2018;12:1433–40.
Barrio-Barrio J, Noval S, Galdós M, Ruiz-Canela M, Bonet E, Capote M, et al. Multicenter Spanish study of spectral-domain optical coherence tomography in normal children. Acta Ophthalmol. 2013;91:e56–e63.
Chua J, Tham YC, Tan B, Devarajan K, Schwarzhans F, Gan A, et al. Age-related changes of individual macular retinal layers among Asians. Sci Rep. 2019;9:20352.
Nieves-Moreno M, Martínez-de-la-Casa JM, Morales-Fernández L, Sánchez-Jean R, Sáenz-Francés F, García-Feijoó J. Impacts of age and sex on retinal layer thicknesses measured by spectral domain optical coherence tomography with Spectralis. PLoS ONE. 2018;13:e0194169.
Palazon-Cabanes A, Palazon-Cabanes B, Rubio-Velazquez E, Lopez-Bernal MD, Garcia-Medina JJ, Villegas-Perez MP. Normative database for all retinal layer thicknesses using SD-OCT posterior pole algorithm and the effects of age, gender and axial length. J Clin Med Res 2020;9:3317. https://doi.org/10.3390/jcm9103317.
Wagner-Schuman M, Dubis AM, Nordgren RN, Lei Y, Odell D, Chiao H, et al. Race- and sex-related differences in retinal thickness and foveal pit morphology. Investig Ophthalmol Vis Sci. 2011;52:625–34.
Scheibe P, Zocher MT, Francke M, Rauscher FG. Analysis of foveal characteristics and their asymmetries in the normal population. Exp Eye Res. 2016;148:1–11.
Zouache MA, Silvestri G, Amoaku WM, Silvestri V, Hubbard WC, Pappas C, et al. Comparison of the morphology of the foveal pit between African and caucasian populations. Transl Vis Sci Technol. 2020;9:24.
Olvera-Barrios A, Kihara Y, Wu Y, Warwick AN, Müller PL, Williams KM, et al. Foveal curvature and its associations in UK biobank participants. Investig Ophthalmol Vis Sci. 2022;63:26.
Romero-Bascones D, Ayala U, Alberdi A, Erramuzpe A, Galdós M, Gómez-Esteban JC, et al. Spatial characterization of the effect of age and sex on macular layer thicknesses and foveal pit morphology. PLoS ONE. 2022;17:e0278925.
Dubis AM, Hansen BR, Cooper RF, Beringer J, Dubra A, Carroll J. Relationship between the foveal avascular zone and foveal pit morphology. Investig Ophthalmol Vis Sci. 2012;53:1628–36.
Liu Y-T, Ma I-H, Hsieh Y-T. Gender- and age-related differences in foveal pit morphology. Indian J Ophthalmol. 2024;72:S37–41.
Catenaccio E, Mu W, Lipton ML. Estrogen- and progesterone-mediated structural neuroplasticity in women: evidence from neuroimaging. Brain Struct Funct. 2016;221:3845–67.
Beltz AM, Moser JS. Ovarian hormones: a long overlooked but critical contributor to cognitive brain structures and function. Ann N Y Acad Sci. 2020;1464:156–80.
Wan L, Huang R-J, Luo Z-H, Gong J-E, Pan A, Manavis J, et al. Reproduction-associated hormones and adult hippocampal neurogenesis. Neural Plast. 2021;2021:3651735.
Ctori I, Gruppetta S, Huntjens B. The effects of ocular magnification on Spectralis spectral domain optical coherence tomography scan length. Graefes Arch Clin Exp Ophthalmol. 2015;253:733–8.
Hoffer KJ, Savini G. Effect of gender and race on ocular biometry. Int Ophthalmol Clin. 2017;57:137–42.
Pope JM, Verkicharla PK, Sepehrband F, Suheimat M, Schmid KL, Atchison DA. Three-dimensional MRI study of the relationship between eye dimensions, retinal shape and myopia. Biomed Opt Express. 2017;8:2386–95.
Chuo JY, Lee TYY, Hollands H, Morris AH, Reyes RC, Rossiter JD, et al. Risk factors for posterior vitreous detachment: a case-control study. Am J Ophthalmol. 2006;142:931–7.
Hayashi K, Sato T, Manabe S-I, Hirata A. Sex-related differences in the progression of posterior vitreous detachment with age. Ophthalmol Retin. 2019;3:237–43.
McCannel CA, Ensminger JL, Diehl NN, Hodge DN. Population-based incidence of macular holes. Ophthalmology. 2009;116:1366–9.
Darian-Smith E, Howie AR, Allen PL, Vote BJ. Tasmanian macular hole study: whole population-based incidence of full thickness macular hole. Clin Exp Ophthalmol. 2016;44:812–6.
Sen P, Bhargava A, Vijaya L, George R. Prevalence of idiopathic macular hole in adult rural and urban south Indian population. Clin Exp Ophthalmol. 2008;36:257–60.
Wang S, Xu L, Jonas JB. Prevalence of full-thickness macular holes in urban and rural adult Chinese: the Beijing Eye Study. Am J Ophthalmol. 2006;141:589–91.
Doonan F, Cotter TG. Norgestrel may be a potential therapy for retinal degenerations. Expert Opin Investig Drugs. 2012;21:579–81.
Sánchez-Vallejo V, Benlloch-Navarro S, López-Pedrajas R, Romero FJ, Miranda M. Neuroprotective actions of progesterone in an in vivo model of retinitis pigmentosa. Pharmacol Res. 2015;99:276–88.
Singh M, Su C. Progesterone and neuroprotection. Horm Behav. 2013;63:284–90.
Smith W, Mitchell P, Wang JJ. Gender, oestrogen, hormone replacement and age-related macular degeneration: results from the Blue Mountains Eye Study. Aust N Z J Ophthalmol. 1997;25:S13–5.
Snow KK, Cote J, Yang W, Davis NJ, Seddon JM. Association between reproductive and hormonal factors and age-related maculopathy in postmenopausal women. Am J Ophthalmol. 2002;134:842–8.
Blasiak J, Petrovski G, Veréb Z, Facskó A, Kaarniranta K. Oxidative stress, hypoxia, and autophagy in the neovascular processes of age-related macular degeneration. Biomed Res Int. 2014;2014:768026.
Kaarniranta K, Machalińska A, Veréb Z, Salminen A, Petrovski G, Kauppinen A. Estrogen signalling in the pathogenesis of age-related macular degeneration. Curr Eye Res. 2015;40:226–33.
Lee AJ, Mitchell P, Rochtchina E, Healey PR, Blue Mountains Eye Study. Female reproductive factors and open angle glaucoma: the Blue Mountains Eye Study. Br J Ophthalmol. 2003;87:1324–8.
Pasquale LR, Rosner BA, Hankinson SE, Kang JH. Attributes of female reproductive aging and their relation to primary open-angle glaucoma: a prospective study. J Glaucoma. 2007;16:598–605.
Madjedi KM, Stuart KV, Chua SYL, Foster PJ, Strouthidis NG, Luben RN, et al. The association of female reproductive factors with glaucoma and related traits: a systematic review. Ophthalmol Glaucoma. 2022;5:628–47.
Hulsman CA, Westendorp IC, Ramrattan RS, Wolfs RC, Witteman JC, Vingerling JR, et al. Is open-angle glaucoma associated with early menopause? The Rotterdam Study. Am J Epidemiol. 2001;154:138–44.
Gloe LM, Russman Block S, Klump KL, Beltz AM, Moser JS. Determining menstrual cycle phase: an empirical examination of methodologies and recommendations for improvement in behavioral and brain sciences. Horm Behav. 2023;155:105421.
Schmalenberger KM, Tauseef HA, Barone JC, Owens SA, Lieberman L, Jarczok MN, et al. How to study the menstrual cycle: practical tools and recommendations. Psychoneuroendocrinology. 2021;123:104895.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169:467–73.
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2000. https://scholar.archive.org/work/zuw33wskgzf4bceqgi7opslsre/access/wayback/http://www3.med.unipmn.it/dispense_ebm/2009-2010/Corso%20Perfezionamento%20EBM_Faggiano/NOS_oxford.pdf.
Akar ME, Taskin O, Yucel I, Akar Y. The effect of the menstrual cycle on optic nerve head analysis in healthy women. Acta Ophthalmol Scand. 2004;82:741–5.
Ulaş F, Doğan U, Duran B, Keleş A, Ağca S, Celebi S. Choroidal thickness changes during the menstrual cycle. Curr Eye Res. 2013;38:1172–81.
Aşikgarip N, Temel E, Örnek K. Assessment of choroidal vascularity index during the menstrual cycle. Eur J Ophthalmol. 2022;32:2740–6.
Fortepiani L, Foutch BK, Wilson MR. The effects of sex, oral contraception, and menstrual cycle phase on intraocular pressure, central corneal thickness, and foveal thickness: a descriptive analysis. Vision. 2021;5:48. https://doi.org/10.3390/vision5040048.
Guo L, Zhu C, Wang Z, Gao Z, Zhang Z, Pan Q. Retinal vascular changes during the menstrual cycle detected with optical coherence tomography angiography. J Ophthalmol. 2021;2021:5514575.
Alpogan O, Tekcan H. Effects of menopause on the retinal nerve fiber layer and ganglion cell complex and on intraocular pressure. Menopause. 2022;29:460–4.
Ataş M, Açmaz G, Aksoy H, Demircan S, Göktaş A, Arifoğlu HB, et al. Evaluation of the macula, retinal nerve fiber layer and choroid thickness in postmenopausal women and reproductive-age women using spectral-domain optical coherence tomography. Prz Menopauzalny. 2014;13:36–41.
Çetinkaya Yaprak A, Erkan Pota Ç. Comparison of retinochoroidal microvascular circulation in menstrual and postmenopausal periods using swept-source optical coherence tomography angiography. Graefes Arch Clin Exp Ophthalmol. 2023;261:367–73.
Fathy M, Noureldine A, Elmofty HM, Tolba DA. The effect of postmenopausal hormonal drop on optic nerve head and peripapillary perfusion using optical coherence tomography angiography (OCTA). Sci Rep. 2022;12:18185.
Elghonemy K, Zaky M, Shaheen NM, Khairat N. Evaluation of retinal thickness in women using spectral-domain optical coherence tomography. Menoufia Med J. 2022;35:1487.
Lee SSY, Yazar S, Pasquale LR, Sanfilippo PG, Hewitt AW, Hickey M, et al. The relationship between optic disc parameters and female reproductive factors in young women. Asia Pac J Ophthalmol. 2019;8:224–8.
Kurahashi K, Hashimoto Y, Shiraishi K, Kubota N, Yoshitomi T. Choroidal morphology and systemic circulation changes during the menstrual cycle in healthy Japanese women. Cureus.2023;15:e48124.
Okonkwo ON, Hassan AO, Oyekunle I, Akanbi T, Chinedu UB. Choroidal thickness and effect of sex and age in Africans. Ann Afr Med. 2023;22:489–96.
Ozcaliskan S, Asri SN, Ozbek M, Artunay O. Changes in the retinal and choroidal microvasculature during menstrual cycle. J Ophthalmol. 2021;244:5514575. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emed22&NEWS=N&AN=637273298.
Asri SN, Ozbek M, Artunay O. Changes in the retinal and choroidal microvasculature during menstrual cycle. J Ophthalmol. 2021;244:5514575. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emed22&NEWS=N&AN=637273298.
Atas M, Acmaz G, Aksoy H, Demircan S, Goktas A, Arifoglu HB, et al. Evaluation of the macula, retinal nerve fiber layer and choroid thickness in postmenopausal women and reproductive-age women using spectral-domain optical coherence tomography. Prz Menopauzalny. 2014;18:36–41.
Research data. Nature Index. 2023. https://www.nature.com/nature-index/ (2023). Accessed 13 Jan 2024.
Anon. Number of clinical trials by year, country, WHO region and income group (1999–2022). https://www.who.int/observatories/global-observatory-on-health-research-and-development/monitoring/number-of-clinical-trials-by-year-country-who-region-and-income-group (2024). Accessed 13 Jan 2024.
Soteriades ES, Falagas ME. Comparison of amount of biomedical research originating from the European Union and the United States. BMJ 2005;331:192–4.
Abou-Gareeb I, Lewallen S, Bassett K, Courtright P. Gender and blindness: a meta-analysis of population-based prevalence surveys. Ophthalmic Epidemiol. 2001;8:39–56.
Miller VM, Duckles SP. Vascular actions of estrogens: functional implications. Pharmacol Rev. 2008;60:210–41.
Thomas P, Pang Y. Protective actions of progesterone in the cardiovascular system: potential role of membrane progesterone receptors (mPRs) in mediating rapid effects. Steroids. 2013;78:583–8.
Duckles SP, Miller VM. Hormonal modulation of endothelial NO production. Pflug Arch. 2010;459:841–51.
Charkoudian N, Hart ECJ, Barnes JN, Joyner MJ. Autonomic control of body temperature and blood pressure: influences of female sex hormones. Clin Auton Res. 2017;27:149–55.
Minson CT, Halliwill JR, Young TM, Joyner MJ. Influence of the menstrual cycle on sympathetic activity, baroreflex sensitivity, and vascular transduction in young women. Circulation. 2000;101:862–8.
Karadeniz MY, Yucel A, Altan Kara S, Noyan V, Altinok D, Ergin A, et al. Change in retrobulbar circulation during menstrual cycle assessed by Doppler ultrasound. Ultrasound Med Biol. 2002;28:33–37.
Haneda M, Hashimoto Y, Mishima A, Saito D, Yoshitomi T. Changes in choroidal circulation hemodynamics during the menstrual cycle in young, healthy women. PLoS ONE. 2022;17:e0270501.
Allen AM, McRae-Clark AL, Carlson S, Saladin ME, Gray KM, Wetherington CL, et al. Determining menstrual phase in human biobehavioral research: a review with recommendations. Exp Clin Psychopharmacol. 2016;24:1–11.
Chalouhi S. Menopause: a complex and controversial journey. Post Reprod Health. 2017;23:128–31.
Harlow SD, Gass M, Hall JE, Lobo R, Maki P, Rebar RW, et al. Executive summary of the Stages of Reproductive Aging Workshop +10: addressing the unfinished agenda of staging reproductive aging. J Clin Endocrinol Metab. 2012;97:1159–68.
Tan CS, Ouyang Y, Ruiz H, Sadda SR. Diurnal variation of choroidal thickness in normal, healthy subjects measured by spectral domain optical coherence tomography. Investig Ophthalmol Vis Sci. 2012;53:261–6.
Asefzadeh B, Cavallerano AA, Fisch BM. Racial differences in macular thickness in healthy eyes. Optom Vis Sci. 2007;84:941–5.
Author information
Authors and Affiliations
Contributions
Ana Paula Ribeiro Reis; Estelle Ioannidou; Kelsey V Stuart; Siegfried K Wagner; Paul Foster; Anthony P Khawaja; Axel Petzold; Sobha Sivaprasad; Nikolas Pontikos; Pearse A Keane; Konstantinos Balaskas; Praveen J Patel. APRR: Drafting/revision of the manuscript for content, including medical writing for content; major role in the acquisition of data; study concept or design; analysis or interpretation of data. Corresponding author. EI: Drafting/revision of the manuscript for content, including medical writing for content; major role in the acquisition of data; study concept or design; analysis or interpretation of data. KVS: Drafting/revision of the manuscript for content, including medical writing for content; major role in the acquisition of data; study concept or design; analysis or interpretation of data. SKW: Drafting/revision of the manuscript for content, including medical writing for content; major role in the acquisition of data; study concept or design; analysis or interpretation of data. PF: Drafting/revision of the manuscript for content, including medical writing for content; analysis or interpretation of data. APK: Drafting/revision of the manuscript for content, including medical writing for content; major role in the acquisition of data; study concept or design; analysis or interpretation of data. AP: Drafting/revision of the manuscript for content, including medical writing for content; major role in the acquisition of data; study concept or design; analysis or interpretation of data. SS: Drafting/revision of the manuscript for content, including medical writing for content; analysis or interpretation of data. NP: Drafting/revision of the manuscript for content, including medical writing for content; analysis or interpretation of data. PAK: Drafting/revision of the manuscript for content, including medical writing for content; analysis or interpretation of data. KB: Drafting/revision of the manuscript for content, including medical writing for content; analysis or interpretation of data. PJP: Drafting/revision of the manuscript for content, including medical writing for content; major role in the acquisition of data; study concept or design; analysis or interpretation of data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflicts of interest related to the content of this manuscript. Specifically, S. Sivaprasad and A. P. Khawaja, who are members of the Eye editorial board. Their editorial roles have not influenced the peer review or decision-making process for this article.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ribeiro Reis, A.P., Ioannidou, E., Stuart, K.V. et al. Macular, choroidal and disc associations across women’s reproductive life stages: a scoping review from menarche to post-menopause. Eye 39, 402–411 (2025). https://doi.org/10.1038/s41433-025-03592-w
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-025-03592-w