Abstract
Background/Objectives
The main aim of this study was to describe the stage at which posterior capsular rupture (PCR) occurred during cataract surgery and the association with anterior capsular (AC) tears.
Subjects/Methods
This was a retrospective, observational cross-sectional study of all cataract surgeries conducted in Moorfields Eye Hospital complicated by PCR, between January 2014 and December 2018. The primary outcome measure was the stage of cataract surgery in which PCR occurred. The secondary outcome measures were the incidence of AC tears, intraoperative complications and location of intraocular lens (IOL) implantation.
Results
1042 eyes were included in the study and PCR occurred at the following stages: hydrodissection in 40 (3%) eyes, phacoemsulsification in 621 (60%) eyes, irrigation-aspiration (IA) in 248 (24%) eyes, lens implantation in 87(8%) eyes, viscoelastic removal in 44(4%) eyes and wound hydration in 2 (1%) eyes. 624/1042(60%) patients had a sulcus lens, 117/1042(11%) lens in the bag, 190/1042(19%) sulcus optic capture, 24/1042(2%) AC lens and 87/1042(8%) aphakic. 15% of PCR cases were associated with an AC tear. There was a significant difference in the timing of PCR and location of IOL implantation between the eyes with an intact anterior capsulorhexis and those with an AC tear (p < 0.01).
Conclusion
PCR is most likely to occur during the phacoemulsification stage of cataract surgery. However, surgeons should be aware that the presence of AC tears may alter this and possibly influence the location of IOL implantation.
Similar content being viewed by others
Introduction
Cataract surgery is the most commonly performed intraocular surgery in the world [1]. Advancements in technology, surgical techniques and anaesthesia have led to the establishment of modern small-incision phacoemulsification surgery [2, 3]. Although a very safe procedure yielding significant improvements in patients’ vision, complications may still occur [4].
Posterior capsular rupture (PCR) is the most common serious intraocular complication that can occur during cataract surgery, which is associated with an increased risk of visual loss [5]. This is because it increases the risk of the following post-operative complications: cystoid macular oedema by 2.6 times, endophthalmitis by 21 times and retinal detachment by up to 40 times [6, 7]. As the presence of such intraoperative and postoperative complications can have an adverse impact on visual outcomes following surgery, risk factors for PCR have been carefully studied and identified. It is estimated that PCR occurs in 0.9% of cataract surgeries done in the National Health Service [8]. Ocular risk factors that can increase the risk of a PCR include dense/mature/brunescent cataract, phacodenesis and pseudoexfoliation [9,10,11]. Extraocular factors associated with a higher risk of PCR include advanced age, inability to lie flat and trainee surgeons [12,13,14].
Although the ocular and systemic risk factors for PCR during cataract surgery have been established, there is limited literature on the timing of PCR during cataract surgery [15,16,17]. The main objective of this study was to identify the stage of cataract surgery during which PCR occurred. We also report on patient characteristics, incidence of other intraoperative complications, choice of IOL and location of IOL implantation.
Materials and Methods
A retrospective cohort study of all cataract surgeries complicated by PCR performed at Moorfields Eye Hospital NHS Foundation Trust over a period of five years between January 2014 and December 2018, was carried out. Moorfields Eye Hospital is one of the largest providers of ophthalmic services in Europe. Through ten regional clinical commissioning groups, it caters to a population of approximately 3.7 million people within London, United Kingdom. Given that this was classified as a retrospective audit and involved analysis of data that was routinely collected by the Trust, it was exempted from institutional review board approval by the institution’s Research and Development Department.
Data was exported from the electronic medical records system employed by Moorfields Eye Hospital NHS Foundation Trust, OpenEyes™ (Apperta Foundation, England). Specific search terms were used to screen all patient letters and patient diagnoses. The search terms used were “PCR”, “posterior capsule rupture” and “posterior capsular rupture” and the medical records of patients identified through these search terms were reviewed. Recording of intraoperative complications is a mandatory field in the electronic medical records system. The operation notes and text box comments were also reviewed to identify details of intraoperative complications. We included all consecutive eyes with a PCR that occurred during routine cataract surgery in the study period. Phacoemulsification was performed using the Alcon Infiniti or Centurion Vision Systems in all cases. Subsequently, irrigation/aspiration (IA) was performed bimanually with metallic IA tips in the majority of cases. The bimanual aspiration cannula that was utilized was a curved 23-gauge cannula with a 0.4 mm top aspiration port. The bimanual irrigation cannula that was used was a curved 21-gauge cannula with 0.51 mm open-end irrigation port. Eyes that had PCR during combined corneal, glaucoma surgery or phacovitrectomy were excluded. Eyes in which there was lack of clear documentation regarding which stage of cataract surgery the PCR occurred in were also excluded. Baseline demographics, pre-operative risk factors (lack of fundal view and presence of posterior plaque), choice of IOL, location of IOL implantation, stage of PCR and presence of other intra-operative complications (anterior capsular tear, vitreous loss, zonular dialysis, dropped lens fragment) were collected for all patients.
Cataract surgery was broadly classified into six stages: hydrodissection, phacoemulsification, IA, IOL implantation, removal of viscoelastic and hydration of wounds. Patient demographics were described using descriptive statistics. Categorical variables were reported using numbers and percentages and continuous variables were reported using mean and standard deviation. Pearson’s χ2 test was used to analyse associations between categorical variables. A p-value of less than 0.05 was considered to be statistically significant. Statistical analyses were performed using R version 4.1.0 (R Foundation for Statistical Computing).
Results
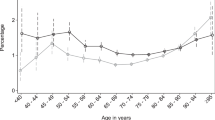
Over the five-year period between January 2014 and December 2018, a total of 1042 eyes with PCR during cataract surgery were included. The average age at the time of surgery was 70.3 years and 522 (50.1%) eyes were female (Table 1). There was an even spread of PCR across the five-year period and the year with the highest incidence was 2016 with 235 (23%) eyes reported. The IOL that was most frequently implanted during cataract surgery was the MA60AC lens with it being implanted in 814 (79%) eyes. The next most frequently implanted lens was the SN60WF lens in 111 (10%) eyes. 87 (8%) eyes were left aphakic following surgery with no lens being implanted. In 24 (2%) eyes, the IOL implanted was the MTA4U0 lens. The SA60AT lens was only used in 13 (1%) eyes.
Anterior capsular (AC) tear was reported alongside PCR in 155 (15%) eyes (Table 2). Vitreous loss occurred in 835 (80%) eyes and no vitreous loss was observed in 207 (20%) eyes. Zonular dialysis was only observed in 47 (5%) eyes with PCR. The main location of implantation of the IOL, MA60AC, was in the sulcus and was performed in 624 (60%) eyes. In 24 (2%) eyes, the MTA4U0 lens was implanted in the anterior chamber.
The stage during which the highest proportion of eyes experienced PCR was phacoemulsification with 621 (59.6%) eyes (Table 3). After phacoemulsification, PCR was most likely to occur during the IA stage, with 248 (23.8%) eyes having it then. During the hydrodissection and lens implantation stage, 40 (3.8%) and 87 (8.3%) eyes experienced PCR, respectively. Following IOL implantation, PCR was noted in 44 (4.2%) eyes during removal of the viscoelastic. 2 (0.3%) eyes had a PCR during the final stage of cataract surgery, wound hydration.
Of the 1042 eyes, 155 eyes had both an AC tear and PCR. When comparing those with and without an AC tear, there was no significant difference in the age at the time of event or sex (Table 4). There was significant difference in the stage of cataract surgery during which PCR occurred between the two groups (p < 0.01). There was also a statistically significant difference in the location of implantation in those with AC tear compared to those without AC tear (p < 0.01).
Discussion
In this consecutive series of 1042 eyes, PCR was most likely to occur during the phacoemulsification stage, followed by IA. Alongside PCR, vitreous loss was the most frequently observed intraoperative complication in these eyes. The IOL was most likely to be implanted in the ciliary sulcus in cataract surgery complicated with PCR. The presence of an AC tear influences the timing of PCR and the location of IOL implantation. In eyes with an AC tear, PCR was more likely to occur during the earlier stages of cataract surgery, such as hydrodissection and phacoemulsification. The IOL was also less likely to be implanted to the bag and placed in alternative location,s such as the anterior chamber in these eyes compared to those with an intact anterior capsulotomy.
There is very limited published data on the stage at which PCR occurs, and our finding that PCR occurred most frequently during the phacoemulsification stage of cataract surgery (60%) is consistent with that previously published, whereby PCR during phacoemulsification occurred in 41% to 57% of cases [18,19,20]. There are several mechanisms that increase the risk of PCR during phacoemulsification. An AC tear caused by iatrogenic trauma to the rhexis edge by the phacoemulsification probe may extend posteriorly [21]. There may also be mechanical trauma to the posterior capsule if the groove is deeper than intended [22]. Towards the end of phacoemulsification, removal of the last nuclear fragment is also another risky stage of cataract surgery for posterior capsular rupture [18].
Several studies demonstrated that PCR was most likely to occur during the IA stage of cataract surgery. Gimbel reported that PCR occurred in 53% of cases during the removal of cortical material [15]. Zheng and Lin identified that PCR occurred most frequently during the same stage in 39% of eyes in their series [16]. In our study, PCR occurred during removal of cortical material in 24% of cases, making it the stage with the second highest frequency of PCR after phacoemulsification. There are several mechanisms that could contribute to a PCR during the IA stage. Firstly, it could be attributed to the use of excessive aspiration [23]. Secondly, placement of the aspiration port close to the posterior capsule may also precipitate rupture. Finally, overzealous polishing of the thin posterior capsule may also lead to its rupture [23].
Furthermore, improvements in cataract surgery technology and instrumentation may also account for this change in the timing of PCR. In Gimbel and Zheng’s case series, IA was performed co-axially. In our study, a bimanual approach was performed for aspiration of the cortex in the majority of cases. Bimanual IA has several advantages compared to the co-axial approach. Firstly, there is greater anterior chamber stability as the instruments are inserted via the smaller paracentesis instead of the larger main incision [24]. Secondly, the surgeon has superior access to the cortex, especially the sub-incisional cortex, when IA is performed bimanually instead of co-axially. Both of these help to reduce the risk of PCR during IA. In more recent years, the adoption of silicone tips has helped to further decrease the risk of PCR during this stage. Thorough assessment and examination of the inner bore, lumen and opening aperture of metallic aspiration tips revealed that hidden, sharp irregularities are present within these tips [25]. Contact between these tips and the posterior capsule, even if minimal, could easily result in a PCR. Silicone tips help to overcome this by increasing the distance between the posterior capsule and bare metal.
As a result of a PCR, another important consideration facing the surgeon is the location of IOL implantation. Our results show that the IOL was most frequently implanted within the ciliary sulcus with the IOL placed within the sulcus in 60% of eyes. Comparatively, the IOL was implanted within the bag in only 11% of eyes. When deciding between placing the IOL in the ciliary or sulcus or in the bag, the main characteristics to consider are the size and nature of the posterior capsular tears. If the tear measures less than 6 mm and has well-defined borders not indicative of vitreous loss, the IOL may be implanted within the bag [26]. If the posterior capsular tears are larger and borders are less defined, the ciliary sulcus may be a more appropriate place to implant the IOL. Although the size and nature of the tears were not described in all the cases included in our study, Osher and Cionni found that only 10% of posterior capsular tears had well-defined margins [16]. As most posterior capsular tears may have margins that are not visible, implantation of the IOL in the ciliary sulcus may be preferable to the bag when a PCR occurs. In addition to placing the IOL within the sulcus, some surgeons may opt for sulcus placement with optic capture, and this was performed in 19% of cases in our study. This is achieved by placing the haptics of the IOL within the ciliary sulcus and the optic pushed posteriorly and secured behind a well-centred anterior capsulotomy. The main advantages of this technique compared to just placement within the sulcus is better stability and no IOL power adjustment [27]. 8% of eyes in our study were left aphakic and without any IOL following a posterior capsular rupture during cataract surgery. There are several reasons why surgical aphakia may occur. Firstly, if there is a dropped lens fragment into the vitreous, the surgeon may opt to leave the patient aphakic. This makes subsequent retrieval of the lens fragment from the vitreous easier, as there is no IOL obstructing it. Secondly, a patient may also be left aphakic if there is not sufficient capsular support to make implantation of the IOL within the ciliary sulcus or bag safe. This might occur as a result of lack of anterior capsular support, zonular dialysis, or widespread zonular dehiscence [28]. In such cases with inadequate capsular support, scleral-fixated, iris-fixated or anterior chamber lenses (AC-IOL) may be more appropriate. In our study, 2% of eyes had an AC-IOL implanted. In the absence of stable capsular support, placing an AC-IOL remains a viable option. However, as AC-IOLs increase the risk of glaucoma, uveitis, corneal endothelial cells loss and pseudophakic macular oedema, careful patient selection based on age, corneal clarity and presence of glaucoma is required [29,30,31,32].
PCR is an intraoperative complication that may occur with or without vitreous loss. In our study, PCR with vitreous loss was reported in 80% of eyes. This rate of vitreous loss is similar to the rate reported in the National Ophthalmology Database. Vitreous loss was identified in 79% of cataract surgeries that were complicated by a PCR [33]. When a PCR occurs, there is a breach in the barrier between the anterior and posterior segments. Disruption of the anterior hyaloid face causes the vitreous to advance forward into the capsular bag and leads to vitreous loss. The incidence of other intraoperative complications alongside PCR was reported in our study. AC tear and dropped lens fragments into the vitreous cavity occurred in 15% and 12% of eyes, respectively. Zonular dialysis was the least frequently reported intraoperative complication and only noted in 5% of eyes. Various studies comparing the incidence of intraoperative complications during cataract surgery have previously reported a similarly low incidence of zonular dialysis, ranging between 0.7% and 13% [5, 21, 33].
PCR occurred during hydrodissection or phacoemulsification in 80% of eyes with AC tears and in 61% of eyes without an AC tear. In this group, 14% of eyes had a PCR during IOL implantation, removal of viscoelastic or wound hydration. In the AC tear group, only 4.5% of eyes had a PCR during the same stages. These results seem to indicate an association between the presence of an AC tear and a PCR in the earlier stages of surgery. During hydrodissection, there is an increase in the hydrostatic pressure within the capsule [13]. There is also vigorous endocapsular manipulations during phacoemulsification. Both of these factors can lead to the peripheral extension of an AC tear and lead to a PCR. Although the presence of such AC tears may be associated with PCR during the earlier stages of cataract surgery, they may be associated with a lower incidence of PCR during the later stages of cataract surgery. Initially, it may be challenging to identify AC tears during the hydrodissection and phacoemulsification stages due to the presence of a significant amount of lens material within the bag. Once the nuclear fragments and cortical material have been removed, any AC tears may become more visible. As surgeons are likely to identify such AC tears during the later stages of cataract surgery and there is widespread understanding that AC tears increase the risk of PCR, they may exhibit greater caution when performing IOL insertion, viscoelastic removal, and wound hydration. It is estimated that PCR occurs in up to 24% of eyes with an anterior capsular tear during cataract surgery [34]. As a result of this higher level of caution and more delicate movements, the risk of PCR may be lower during the latter stages if there is an AC tear.
In our study, we also found that there was a significant difference in the location of IOL implantation between the AC tear and non-AC tear groups. In both groups, although the IOL was most frequently implanted in the ciliary sulcus, only 4.5% eyes with AC tear had IOL implanted within the bag, compared to that in 12.4% of eyes without AC tear. In the presence of a PCR, the IOL is only likely to be placed within the bag if the break in the posterior capsule tear is small and has well-defined boundaries. Since the morphology of AC tears extending to the posterior capsule is likely to be radial with poorly defined margins, fewer surgeons may have opted to implant the lens within the capsular bag if there was an AC tear. 23.2% of eyes in the AC tear groups had the IOL implanted within the anterior chamber or left aphakic. Comparatively, only 8.5% of eyes in the non-AC tear groups had the IOL implanted within the anterior chamber or left aphakic. If there is evidence of capsular support, it is preferable to implant an IOL within the bag or ciliary sulcus. In the absence of robust capsular support, it may be more prudent to look for alternative locations such as the anterior chamber or utilise scleral-fixated or iris-fixated lenses. Since the presence of both anterior and posterior tears highlights that there may be inadequate capsular support to support a lens within the bag or sulcus, more surgeons in the AC tear group elected to leave the patient aphakic or implant an AC-IOL.
Our study does have several limitations. Firstly, the classification of cataract surgery into stages is broad. For instance, phacoemulsification includes grooving, cracking and removal of nuclear segments. Further stratification of phacoemulsification into the steps in detail could have yielded more specific results and precise identification of the high-risk stages of cataract surgery but this is not always possible through freetext search from our EPR. Secondly, our cohort consists of a mixture of bimanual, automated and simcoe IA. Although IA was performed bimanually in most cases, it is challenging to standardise instrument choice during cataract surgery. A small proportion of surgeons utilised simcoe or automated IA instead of a bimanual approach. Thirdly, the main aim of our study was to describe the stage of cataract surgery during which PCR occurred. Further research assessing how pre-operative risk factors, such as grade of surgeon, cataract grade and zonular pathology, correlate with the incidence of intraoperative risk factors are required in the future.
In summary, this study found that PCR was most likely to occur during the phacoemulsification stage of cataract surgery. When there is a PCR, the most likely location of intraocular lens implantation was the ciliary sulcus. PCR occurred with vitreous loss in 4 of every 5 cases. Our study also highlights that the presence of an AC tear in these cases may be associated with a higher risk of PCR during the earlier stages such as hydrodissection and phacoemulsification. Surgeons must also be aware that such deficiencies in the anterior capsulotomy are likely to have an impact on the location of intraocular lens implantation.
Summary
What was known before:
-
1.
There is a lack of recent studies conducted into the timing of PCR during cataract surgery.
-
2.
PCR has been shown to occur most frequently during the phacoemulsification or irrigation-aspiration stage of cataract surgery in case series reported in the 1980s and 1990s.
-
3.
PCR may occur secondary to an extension of an anterior capsular tear in about 1 in 4 cases with an anterior capsular tear.
What this study adds:
-
1.
This is the largest case series of cataract surgeries complicated with PCR that has been reported and the first one in the 21st century specifically looking at the timing of PCR during cataract surgery.
-
2.
PCR was most frequently reported during the phacoemulsification stage and the proportion of cases with PCR during IA has decreased, compared to previous studies published in the 1980s and 1990s. This is likely due to widespread improvements in cataract surgery technology and instrumentation.
-
3.
The first report, to the authors’ knowledge, to report that the presence of AC-tear alongside PCR may influence the timing of PCR during cataract surgery.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
GBD 2019 Blindness and Vision Impairment Collaborators; Vision Loss Expert Group of the Global Burden of Disease Study. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: the Right to Sight: an analysis for the Global Burden of Disease Study. Lancet Glob Health.;9:e144-e160. Epub 2020 Dec 1. Erratum in: Lancet Glob Health. 2021;9:e408.
Pesudovs K, Lansingh VC, Kempen JH, Tapply I, Fernandes AG, Cicinelli MV et al; Vision Loss Expert Group of the Global Burden of Disease Study; GBD 2019 Blindness and Vision Impairment Collaborators. Global estimates on the number of people blind or visually impaired by cataract: a meta-analysis from 2000 to 2020. Eye. 2024. Epub ahead of print.
Erie JC, Baratz KH, Hodge DO, Schleck CD, Burke JP. Incidence of cataract surgery from 1980 through 2004: 25-year population-based study. J Cataract Refract Surg. 2007;33:1273–7.
Davis G. The Evolution of Cataract Surgery. Mo Med. 2016;113:58–62.
Day AC, Norridge CFE, Donachie PHJ, Barnes B, Sparrow JM. Royal College of Ophthalmologists’ National Ophthalmology Database study of cataract surgery: report 8, cohort analysis of the relationship between intraoperative complications of cataract surgery and axial length. BMJ Open. 2022;12:e053560.
Chu CJ, Johnston RL, Buscombe C, Sallam AB, Mohamed Q, Yang YC. Risk Factors and Incidence of Macular Edema after Cataract Surgery: A Database Study of 81984 Eyes. Ophthalmology. 2016;123:316–23.
Wong TY, Chee SP. Risk factors of acute endophthalmitis after cataract extraction: a case-control study in Asian eyes. Br J Ophthalmol. 2004;88:29–31.
Clark A, Morlet N, Ng JQ, Preen DB, Semmens JB. Risk for retinal detachment after phacoemulsification: a whole-population study of cataract surgery outcomes. Arch Ophthalmol. 2012;130:882–8.
Artzén D, Lundström M, Behndig A, Stenevi U, Lydahl E, Montan P. Capsule complication during cataract surgery: Case-control study of preoperative and intraoperative risk factors: Swedish Capsule Rupture Study Group report 2. J Cataract Refract Surg. 2009;35:1688–93.
Rutar T, Porco TC, Naseri A. Risk factors for intraoperative complications in resident-performed phacoemulsification surgery. Ophthalmology. 2009;116:431–6.
Blomquist PH, Morales ME, Tong L, Ahn C. Risk factors for vitreous complications in resident-performed phacoemulsification surgery. J Cataract Refract Surg. 2012;38:208–14.
Zare M, Javadi MA, Einollahi B, Baradaran-Rafii AR, Feizi S, Kiavash V. Risk factors for posterior capsule rupture and vitreous loss during phacoemulsification. J Ophthalmic Vis Res. 2009;4:208–12.
Chakrabarti A, Nazm N. Posterior capsular rent: Prevention and management. Indian J Ophthalmol. 2017;65:1359–69.
Ergun ŞB, Kocamış Sİ, Çakmak HB, Çağıl N. The evaluation of the risk factors for capsular complications in phacoemulsification.Int Ophthalmol.2018;38:1851–61.
Gimbel HV Posterior capsular tears during phacoemulsification – causes, prevention and management. Eur J Refract Surg. 1990:63-69
Zheng D, Lin Z. Reason and management of posterior capsular breaks during cataract extraction and lens implantation. Yan Ke Xue Bao. 1995;11:95–7.
Ng DT, Rowe NA, Francis IC, Kappagoda MB, Haylen MJ, Schumacher RS, et al. Intraoperative complications of 1000 phacoemulsification procedures: a prospective study. J Cataract Refract Surg. 1998;24:1390–5.
Mulhern M, Kelly G, Barry P. Effects of posterior capsular disruption on the outcome of phacoemulsification surgery. Br J Ophthalmol. 1995;79:1133–7.
Osher RH, Cionni RJ. The torn posterior capsule: its intraoperative behavior, surgical management, and long-term consequences. J Cataract Refract Surg. 1990;16:490–4.
Leang LJ, Liechty JJ, Powell A, Schwartz C, DiSclafani M, Drucker MD, et al. Rate of posterior capsule rupture in phacoemulsification cataract surgery by residents with Institution of a Wet Laboratory Course. J Acad Ophthalmol. 2022;14:e70–e73.
Koch PS. Managing the torn posterior capsule and vitreous loss. Int Ophthalmol Clin. 1994;34:113–30.
Lambrou FH Jr, Stewart MW. Management of dislocated lens fragments during phacoemulsification. Ophthalmology. 1992;99:1260–2.
Vajpayee RB, Sharma N, Dada T, Gupta V, Kumar A, Dada VK. Management of posterior capsule tears. Surv Ophthalmol. 2001;45:473–88.
Colvard DM. Bimanual technique to manage subincisional cortical material. J Cataract Refract Surg. 1997;23:707–9.
Lockington D, Macente A, Marrocco T, Sillars F. Novel internal analysis of metal irrigation/aspiration tips could explain mechanisms of posterior capsule rupture. Eye (Lond). 2021;35:1915–21.
Natchiar G, Robin AL, Nalgirkar AR, Krishnadas R. Posterior capsule tears during extracapsular cataract surgery in India. Arch Ophthalmol. 1993;111:706–8.
Mehta R, Aref AA. Intraocular lens implantation in the ciliary sulcus: challenges and risks. Clin Ophthalmol. 2019;13:2317–23.
Tribus C, Alge CS, Haritoglou C, Lackerbauer C, Kampik A, Mueller A, et al. Indications and clinical outcome of capsular tension ring (CTR) implantation: A review of 9528 cataract surgeries. Clin Ophthalmol. 2007;1:65–9.
Smith PW, Wong SK, Stark WJ, Gottsch JD, Terry AC, Bonham RD. Complications of semiflexible, closed-loop anterior chamber intraocular lenses. Arch Ophthalmol. 1987;105:52–7.
Biro Z. Results and complications of secondary intraocular lens implantation. J Cataract Refract Surg. 1993;19:64–7.
Drolsum L. Long-term follow-up of secondary flexible, open-loop, anterior chamber intraocular lenses. J Cataract Refract Surg. 2003;29:498–503.
Hennig A, Johnson GJ, Evans JR, Lagnado R, Poulson A, Pradhan D, et al. Long term clinical outcome of a randomised controlled trial of anterior chamber lenses after high volume intracapsular cataract surgery. Br J Ophthalmol. 2001;85:11–7.
Magyar M, Sándor GL, Ujváry L, Nagy ZZ, Tóth G. Intraoperative complication rates in cataract surgery performed by resident trainees and staff surgeons in a tertiary eyecare center in Hungary. Int J Ophthalmol. 2022;15:586–90.
Carifi G, Miller MH, Pitsas C, Zygoura V, Deshmukh RR, Kopsachilis N, et al. Complications and outcomes of phacoemulsification cataract surgery complicated by anterior capsule tear. Am J Ophthalmol. 2015;159:463–9.
Funding
No financial support was received for the work submitted.
Author information
Authors and Affiliations
Contributions
AN - Conceptualisation, data analysis, manuscript writing (lead). YNN – Conceptualisation, methodology, data collection, analysis, visualisation, review and editing. DL – Supervision, review and editing. ACD - Conceptualisation Supervision, review and editing. All authors approved the final manuscript and agreed to be accountable for all aspects of the work
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Narayan, A., Neo, Y.N., Lockington, D. et al. Timing of posterior capsular rupture during cataract surgery. Eye 39, 2708–2712 (2025). https://doi.org/10.1038/s41433-025-03942-8
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-025-03942-8