Abstract
Background/Objectives
Ophthalmic care for patients who are incarcerated or in immigration detention presents complex challenges for patients and providers. There remains a paucity of literature investigating ophthalmic care for these marginalised populations. We investigated the delivery of ophthalmic care in an academic health system to patients who were incarcerated or in immigration detention.
Subjects/Methods
We conducted a retrospective observational study and secondary analysis of electronic health record data for inpatient, outpatient, and surgical visits between 1 November 2018 and 30 September 2023 in an ophthalmology department at an academic medical centre in the United States for patients who were incarcerated or in immigration detention. Attendance at outpatient clinic visits and follow-up based on ophthalmic subspecialty, loss to follow-up, delays in follow-up, and rates of ancillary testing were analysed.
Results
1628 scheduled visits were extracted for 401 patients, of which 1084 were attended (2.7 ± 3.6 per patient) and 544 were cancelled or no-showed (1.4 ± 1.8 per patient). Patients attended 100 (68.5%) of cornea, 116 (64.4%) of glaucoma, 2 (28.6%) of neuro-ophthalmology, 139 (58.2%) oculoplastics, 9 (36.0%) of paediatrics/strabismus, and 109 (54.5%) of retina visits. Using a 2-week grace period for follow-up, 72 patients (40.9% with complete follow-up data) completed follow-up within 2 weeks. 229 patients (57.1%) were lost to follow-up at the end of the study period, which is consistent with data from previous reports on ophthalmic care at other centres for patients who were incarcerated.
Conclusions
Delays in care and visit attrition were substantial for patients who were incarcerated or in immigration detention. More work is needed to quantify outcomes and address disparities in care for these marginalised communities.
Similar content being viewed by others
Introduction
In the United States (US), approximately 2 million people are incarcerated before or after trial in 100 federal prisons, 1600 state prisons, 3000 local jails, 140 immigration detention centres, and other facilities [1]. Of these, approximately 18,000 are held criminally and civilly for immigration-related reasons by the U.S. Marshals Service [1]. Separately, 38,000 people in the US are civilly detained by US Immigration and Customs Enforcement in federal or privately run immigration detention facilities because they are asylum seekers and/or facing deportation, rather than for any suspected crime [1].
While correctional facilities and detention centres in the US are required to provide healthcare to people who are incarcerated or detained [2], studies have reported substantial disparities in health outcomes and health care access for these marginalised populations [3,4,5]. Many facilities are remote and unable to provide onsite primary and subspecialty care, and thus partner with external health care systems to deliver care to patients [6]. In these cases, coordination of transportation, security, and initial and follow-up appointments for patients is required for patients to receive necessary care. A recent systematic review of studies from 16 distinct cohorts found that surgical complications, delayed hospital presentations, and complex cases were more prevalent in incarcerated versus non-incarcerated individuals [7].
Ophthalmic care for patients who are incarcerated or in immigration detention also presents complex challenges to patients and providers. Ocular and orbital trauma [8, 9], as well as chronic ophthalmic conditions that may be manifestations of or affected by systemic conditions (e.g., diabetic retinopathy and glaucoma) [10, 11] require regular follow-up and may require surgical management. A study of follow-up care in an outpatient ophthalmology setting at a single academic medical centre for patients who were incarcerated found that over 60% of patients were lost to follow-up; of those who were not lost to follow-up, over 40% experienced delays in care [12]. There remains a paucity of literature investigating health care delivery across ophthalmic subspecialties for these marginalised populations. Data on ophthalmic care provision for patients who are in immigration detention are especially sparse. To address this gap in knowledge, we investigated the delivery of inpatient, outpatient, and surgical ophthalmic care to these populations in an academic health system.
Methods
The UCSD Institutional Review Board approved this study (IRB #120516) and the described research adheres to the tenets of the Declaration of Helsinki and Health Insurance Portability and Accountability Act (HIPAA) of 1996. The study’s participant selection, methodology, results, and discussion adhere to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines. Informed consent was waived by the UCSD IRB in this retrospective study.
Data source and collection
We conducted a retrospective observational study using data from the electronic health record system (Epic, Verona, WI, USA) at a single academic medical centre. The study population included: (1) patients who were incarcerated at local jails or state or federal prisons, or detained at immigration detention facilities at the time of the study, and (2) patients had one or more in-office visits with the ophthalmology service at University of California San Diego (UCSD) from 1 November 2018 to 30 September 2023, inclusive. We employed the Epic SlicerDicer tool (Epic Systems, Verona, WI, USA) to query this population. Between 19 October 2023 and 25 May 2024, we extracted data for study participants’ visits within the study period.
Patients who were incarcerated presented to UCSD either via the ED or referral to a comprehensive or subspecialty clinic. If ancillary imaging, such as OCT or HVF, was required, patients were scheduled to present at a separate imaging appointment at a different location before their clinical visit as imaging equipment was not available at the office for where the patient's visit occurred. A flowchart of hospital, clinic, imaging, and surgery visits for patients who are incarcerated and present to care at UCSD is shown in Fig. 1.
Each block represents a distinct setting/location where a visit occurs. At our institution, ancillary testing (i.e., Humphrey visual fields [HVF], lens calculations, and optical coherence tomography [OCT], among other tests) occurs at a different location than the comprehensive and subspecialty clinics.
We manually extracted data from ophthalmology encounters in the emergency department (ED), hospitalisation follow-ups, outpatient clinic visits, and surgeries for patients who were incarcerated. Demographic and visit data were extracted for each patient’s visit. Demographic data included: date of birth, gender, ethnicity, race, and insurance provider (e.g., County Medical Services, State of California/State Prison, Immigration Health Services, US Marshal Services, etc.). Visit data included: type of visit; subspecialty of provider, visit attendance, the first three 3 ophthalmic diagnoses that were addressed in the visit, interventions planned and performed, ancillary testing received and planned, recommended time to follow-up, and recommended time to planned interventions. Planned interventions included laser procedures (capsulotomy, laser peripheral iridotomy, selective laser trabeculoplasty) and surgical procedures (cataract surgery, vitrectomy, orbital wall fracture repair, etc). Intravitreal injections were excluded as the decision for injection for the majority of patients in this cohort was contingent on their visit imaging (i.e., diabetic macular oedema).
Statistical analysis
All data analysis was performed using R version 4.3.2 (Vienna, Austria) [13]. The total number of patients who met the inclusion criteria was enumerated. Mean and standard deviations were calculated for counts of each category of demographic data. The most common ophthalmic diagnoses were tabulated. Visits were categorised into the following: emergency department, hospitalisation follow-up (i.e., seen by ophthalmology during inpatient admission), outpatient in-person (i.e., clinic visit), outpatient telemedicine, or surgical. Visit attendance, categorised as attended vs. cancelled or no-show, was enumerated for each visit category. Cancelled and no-show visits were grouped together because ancillary staff often opened visit encounters before the patient arrived, and cancellations or no-shows were often marked after the visit was over. Visit attendance by sum and percentage was calculated for each visit type, on a per-patient basis, and also by subspecialty. Ancillary tests were tabulated by the test performed. Due to the non-normal distribution of visit attendance, the Mann-Whitney U test was used to assess statistical differences between visit attendances by subspecialty, with p ≤ 0.05 thresholded for statistical significance. Follow-up intervals were calculated between each visit. Delays in follow-up were calculated as the difference between the recommended time interval for follow-up and the actual follow-up interval, with a 2-week grace period. We also ascertained loss to follow-up, which was defined as a lack of follow-up visits with ophthalmologists in this health system as scheduled, after incarceration or the end of the study period.
Results
Patient characteristics
401 patients were included in this study. The mean age at presentation was 44.2 ± 14.2 years. The majority of patients were male (n = 363 [90.5%]) and reported an ethnicity of Non-Hispanic or Latino (n = 189 [47.1%]). The majority of patients did not report their race (n = 209 [52.1%]), although the most common reported races were White (n = 117 [29.2%]) and Black (n = 62 [15.4%]). The most common insurance coverage for these patients were county medical services (n = 191 [47.6%]) and California state prison (n = 134 [33.4%]). The average distance from facility to clinic was 44.8 ± 55.2 miles. Complete demographic data are shown in Table 1.
Overall visit statistics
1628 scheduled visits were extracted for the 401 included patients, of which 1084 visits were attended (2.7 ± 3.6 per patient) and 544 visits were cancelled or no-showed (1.4 ± 1.8 per patient). Of the 1413 outpatient visits, 1409 were in-person and 4 were telemedicine. Patients attended 874 outpatient in-person visits (2.2 ± 2.9 per patient), representing 53.1% of all visits or 62.1% of outpatient in-person visits. Patients also no-showed or cancelled 535 outpatient in-person visits (1.3 ± 1.8 per patient), or 32.5% of all visits or 37.9% of outpatient in-person visits. There were 93 ED visits (0.2 ± 0.5 per patient) and 64 hospitalisation follow-up visits (0.2 ± 1.0 per patient). Patients attended 2 telemedicine visits (0.0 ± 0.1 per patient) and cancelled or no-showed 2 telemedicine visits (0.0 ± 0.1 per patient). Visit attendance data are summarised in Table 2.
Visit statistics by subspecialty
Of the 874 attended outpatient visits and 535 cancelled/no-showed outpatient visits, 401 (65.0%) were attended and 216 (35.0%) were cancelled/no-showed in the comprehensive clinic. Patients attended 100 (68.5%) of cornea, 116 (64.4%) of glaucoma, 2 (28.6%) of neuro-ophthalmology, 139 (58.2%) of oculoplastics, and 9 (36.0%) of paediatrics/strabismus, and 109 (54.5%) of retina visits. Patients generally cancelled or no-showed neuro-ophthalmology, oculoplastics, paediatrics/strabismus, and retina visits more often compared to the comprehensive clinic (p < 0.05). These data are shown in Table 3.
Surgeries and ancillary testing
Patients were scheduled for a total of 58 surgeries, of which patients attended 51 (0.1 ± 0.4 per patient) and cancelled or no-showed 7 (0.0 ± 0.1 per patient). The most common procedures performed were vitrectomies (n = 19), cataract surgery (n = 12), and glaucoma drainage devices (n = 5) (Supplementary Table 1). Ancillary tests (i.e., OCTs, HVFs) were requested in follow-up for 131 attended outpatient visits (14.9% of attended visits), although those tests were only performed in follow-up for 22 attended outpatient visits (16.8% of visits for which ancillary tests were requested).
Delays in and loss to follow-up
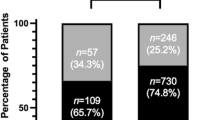
Complete follow-up data with attended follow-ups and return to clinic requests from the prior visit were available for 473 attended visits from 176 patients. Overall, the mean delay in follow-up, was 9.1 ± 19.4 weeks. Using a 2-week grace period for follow-up, 72 patients (40.9% with complete follow-up data) completed follow-up within 2 weeks. The distribution of delays in follow-ups is shown in Fig. 2.
Of the 401 patients included in the study, 229 patients (57.1%) were lost to follow-up at the end of the study period. We were not able to accurately calculate delays in follow-up ophthalmic care for patients seen for ophthalmology consult services in the emergency department, as some of these data were incomplete or missing.
Discussion
This study used EHR data to quantify visit attendance and adherence as well as delays in follow-up care and loss to follow-up (LTFU) experienced by patients in an academic health system who were incarcerated or in immigration detention. Our study has two key findings: (1) visit adherence and attrition are substantial issues for patients who are incarcerated, and when follow-up occurs, it tends to occur at longer than recommended intervals; and (2) utilisation and attendance of ancillary testing were also low for this population.
Visit adherence and attrition
First, visit adherence and attrition were found to be substantial issues for patients who are incarcerated or in immigration detention. LTFU and follow-up delay rates (using a 2-week grace period for follow-up) were 57.1% and 40.9% (Fig. 2), respectively. LTFU for comprehensive ophthalmology visits in the present study was consistent with data from previous reports on ophthalmic care delivery for patients who were incarcerated [12, 14]. On subgroup analyses within the present study, paediatric ophthalmology had a relatively high incidence of visit non-adherence, consistent with reports of low visit adherence among the general population [15, 16]. By contrast, the present study population had a substantially higher rate of visit cancellation or no-show for oculoplastics clinic appointments than the general population in the literature [17]. Previous studies have shown that delays in follow-up care for patients with chronic conditions that require long-term follow-up and management (e.g., glaucoma) can substantially worsen outcomes [18]. In diseases in which vision is not usually immediately threatened (i.e., orbital wall fractures without entrapment and glaucoma), patients may not be aware of the need for routine follow-up to prevent complications of their diseases or vision loss. Prior work has demonstrated low rates of health literacy among patients who are incarcerated, and suggested that interventions to increase health literacy may improve follow-up rates [19].
Factors cited from previous studies for non-adherence and attrition in health care for the general population include socioeconomic disparities, long waiting times, and transportation to health care facilities [14, 20,21,22]. Logistical and communication difficulties in scheduling and transporting patients to appointments pose substantial barriers in access to care for patients who are incarcerated or in immigration detention. Many jails, prisons, and detention facilities have policies that do not allow for disclosing specific follow-up details of inmates for security reasons [10]. Also, nearly half of the patients had coverage through County Medical Services, reflective of their incarceration in city jails. This subpopulation may experience higher rates of turnover given that jails hold individuals prior to trials and/or relocation to prisons or release to the community. Administrative staff of jails, prisons, and detention facilities must therefore coordinate future appointments directly with staff at health care facilities, which can delay and complicate timely health care delivery [10]. Individuals who are incarcerated have high levels of distrust in the health care system, which could also contribute to attrition and LTFU [23]. Other marginalised populations (e.g., uninsured, undocumented, and previously incarcerated people) have also been shown to have low rates of follow-up [3, 24]. Randomised trials within the general population have reported improvements in follow-up by implementing text message and telephone reminders for appointments [25] and employing patient navigators and social workers to engage with patients to provide appropriate health care and social resources [26].
Further work is needed to understand how we can improve access to ophthalmic care and follow-up for patients who are incarcerated or detained.
Ancillary testing
Second, there were particularly low rates of attendance and utilisation of ancillary testing. Ancillary testing, including imaging (e.g., OCT and ultra-widefield fundus imaging) and visual fields, provides essential information on the management of various ophthalmic conditions. For example, RNFL OCTs and HVF are ideally used to assess management of primary open-angle glaucoma, and macula OCTs are essential in the management of diabetic retinopathy and retinal detachments. Ancillary tests were requested in follow-up for 15% of attended outpatient visits; however, these tests were only completed in follow-up for 17% of those respective visits (data not shown). The health system in which this study took place requires ancillary testing to be completed at separate appointments following the visits at which tests are requested, which may logistically limit visit adherence, as two separate instances of transportation would be required for a given visit. Low rates of requesting ancillary testing could reflect biases by providers: providers may be under-ordering tests for patients who are incarcerated or detained. This disparity may be due to expectations of barriers to adherence and attendance, as well as stigma and bias against this marginalised population [27].
To improve the utilisation of ancillary testing, interdisciplinary teams could combine the provision of ancillary testing and outpatient clinic visits, such that patients could see their ophthalmologist and complete ancillary testing on the same date. Future research could integrate greater sample sizes of patients who are incarcerated and who are able to complete ancillary testing. These measures are necessary as our study found no statistical differences between measurements of VA and IOP at patients’ first vs. last visits. It is likely that VA and IOP broadly are inadequate measures of patient outcomes alone. The lack of statistically significant differences persisted even within the sub-analysis of patients with retinal detachments, cataracts, and orbital wall fractures; however, these data were limited by small sample sizes. Future work should focus on analysing objective metrics for ophthalmic disease severity to better understand outcomes of patients who are incarcerated with ophthalmic disease.
Limitations
This study has multiple limitations. First, our study was limited in sample size. This may limit the generalisability of our findings to other incarcerated populations domestically and internationally. Second, we did not compare follow-up rates and patient outcome metrics to the general population at UCSD. Although this broader analysis was out of the scope of our study, future work may focus on comparing visit adherence and patient outcomes between these populations. Third, our definition of loss to follow-up was limited, given the study design as a retrospective chart review of visits at a single centre over a five-year study period. We defined loss to follow-up as not having a follow-up visit as scheduled, after incarceration or the end of the study period. This would also include cases in which patients themselves cancelled a visit and had no further visits, were transferred to a facility served by another medical system, or passed away during the study period. Fourth, we did not analyse medication adherence as we found medication documentation and review were often incomplete, consistent with prior literature [28]. Future studies and interventions should focus on analysing how patients who are incarcerated use medications and how to improve medication adherence.
Conclusion
The present study is among the first to investigate the delivery of ophthalmic care to patients who are incarcerated or detained. We demonstrate that visit attrition is particularly high in this marginalised population, which in turn limits our ability to objectively study the outcomes of these patients. Multidisciplinary collaborations between clinicians, ancillary staff, hospital administrators, jail/detention staff, and social workers will be necessary to improve healthcare delivery, including improved visit adherence and outcomes, for these patients.
Summary
What was known before:
-
Previous studies in the US and UK have shown that visit adherence and attrition are substantial issues for patients who are incarcerated.
What this study adds:
-
Our study of data from an academic medical centre in the US found that patients who were incarcerated or in immigration detention found that patients experienced substantial delays in ophthalmic care as well as loss to follow-up.
-
Although visual acuity and intraocular pressure were unchanged on average, the determination of outcomes was limited by low rates of ancillary testing utilisation in this patient population.
Data availability
The datasets analysed during the current study are not publicly available as they include individual-level health data from a marginalised study population. Summary statistics are available from the corresponding author on reasonable request.
References
Sawyer W, Wagner P. Mass Incarceration: The Whole Pie 2024. Accessed 26 May 2024. https://www.prisonpolicy.org/reports/pie2024.html.
US Immigration and Customs Enforcement. National Detention Standards for Non‑Dedicated Facilities. 2019. Accessed 26 May 2024. https://www.ice.gov/doclib/detention-standards/2019/nds2019.pdf.
Zhao J, Star J, Han X, Williams A, Patel S, Nguyen T, et al. Incarceration History and Access to and Receipt of Health Care in the US. JAMA Health Forum. 2024;5:e235318. https://doi.org/10.1001/jamahealthforum.2023.5318.
Zhao J, Han X, Zheng Z, Kim L, Lopez M, Carter R, et al. Incarceration history and health insurance and coverage changes in the U.S. Am J Prev Med. 2023;64:334–342. https://doi.org/10.1016/j.amepre.2022.09.023.
Winkelman T, Kieffer E, Goold S, Morenoff J, Cross K, Ayanian J Health Insurance Trends and Access to Behavioral Healthcare Among Justice‑Involved Individuals — United States, 2008‑2014. J Gen Intern Med. 2016;31. https://doi.org/10.1007/s11606-016-3845-5.
Binswanger I. Opioid use disorder and incarceration — hope for ensuring the continuity of treatment. N Engl J Med. 2019;380:1193–1195. https://doi.org/10.1056/NEJMp1900069.
Dhimal T, Cupertino P, Ghaffar A, Singh R, Patel A, O’Connor K, et al. Systematic review of surgical care in the incarcerated population: identifying knowledge gaps for future research. Ann Surg Open. 2024;5:e434. https://doi.org/10.1097/AS9.0000000000000434.
Jordan DR, Allen LH, White J, Harvey J, Pashby R, Esmaeli B. Intervention within days for some orbital floor fractures: the white‑eyed blowout. Ophthal Plast Reconstr Surg. 1998;14:379.
Jeng F, Bonnell AC, O’Neil EC, Smith R, Lee D, Green T, et al. Vision‑related malpractice involving prisoners: Analysis of the Westlaw Database. Retina. 2022;42:816. https://doi.org/10.1097/IAE.0000000000003382.
Kanu LN, Jang I, Oh DJ, Martinez A, Singh R, Chen L, et al. Glaucoma care of prison inmates at an academic hospital. JAMA Ophthalmol. 2020;138:358–364. https://doi.org/10.1001/jamaophthalmol.2020.0001.
Aoki N, Dunn K, Fukui T, Beck JR, Schull WJ, Li HK. Cost‑effectiveness analysis of telemedicine to evaluate diabetic Retinopathy in a prison population. Diab Care. 2004;27:1095–1101. https://doi.org/10.2337/diacare.27.5.1095.
Abou‑Jaoude MM, Crawford J, Kryscio RJ, Moore DB. Accuracy of Ophthalmology clinic follow‑up in the incarcerated patient population. J Acad Ophthalmol. 2022;14:e258–e262. https://doi.org/10.1055/s-0042-1758562.
R Foundation for Statistical Computing. R: A Language and Environment for Statistical Computing. Published online 2023. https://www.R-project.org/.
Zou D, Lakhani B, Reynolds R, Umer M, King AJ, Stead R. Quantification of missed hospital appointments and related harm for prisoners attending ophthalmology services. Eye. 2022;36:1713–1714. https://doi.org/10.1038/s41433-021-01823-4.
Hekmatjah N, Turner CH, Mesfin Y, Ramirez L, Patel S, Gomez A, et al. Factors associated with pediatric ophthalmology follow‑up adherence before and during the COVID‑19 pandemic. JAAPOS. 2024;28. https://doi.org/10.1016/j.jaapos.2024.103963.
Chen J, Goldstein IH, Lin WC, Chiang MF, Hribar MR. Application of machine learning to predict patient no‑shows in an academic pediatric ophthalmology clinic. AMIA Annu Symp Proc. 2021;2020:293.
Sinha S, Nudelman N, Feustal PJ, Caton‑Darby M, Rothschild MI, Wladis EJ. Factors associated with appointment “no‑shows” at two tertiary level outpatient oculoplastic clinics. Orbit. 2023;42:523–528. https://doi.org/10.1080/01676830.2022.2148259.
Foot B, MacEwen C. Surveillance of sight loss due to delay in ophthalmic treatment or review: frequency, cause and outcome. Eye. 2017;31:771–775. https://doi.org/10.1038/eye.2017.1.
Hadden KB, Puglisi L, Prince L, Edwards M, Clark R, Johnson T, et al. Health literacy among a formerly incarcerated population using data from the transitions clinic network. J Urban Health. 2018;95:547–555. https://doi.org/10.1007/s11524-018-0276-0.
Scanzera AC, Sherrod RM, Potharazu AV, Davis L, Singh P, White M, et al. Barriers and Facilitators to Ophthalmology Visit Adherence in an Urban Hospital Setting. Transl Vis Sci Technol. 2023;12:11. https://doi.org/10.1167/tvst.12.10.11.
Fuge TG, Tsourtos G, Miller ER. A systematic review and meta‑analyses on initiation, adherence and outcomes of antiretroviral therapy in incarcerated people. PLoS One. 2020;15:e0233355. https://doi.org/10.1371/journal.pone.0233355.
Jennings L, Branson CF, Maxwell AM, Winkelman TNA, Shlafer RJ. Physicians’ perspectives on continuity of care for patients involved in the criminal justice system: A qualitative study. PLoS One. 2021;16:e0254578. https://doi.org/10.1371/journal.pone.0254578.
Vandergrift LA, Christopher PP. Do prisoners trust the healthcare system?. Health Justice. 2021;9:15. https://doi.org/10.1186/s40352-021-00141-x.
Nandi A, Galea S, Lopez G, Nandi V, Strongarone S, Ompad DC. Access to and use of health services among undocumented mexican immigrants in a US Urban area. Am J Public Health. 2008;98:2011–2020. https://doi.org/10.2105/AJPH.2006.096222.
Lin H, Wu X. Intervention strategies for improving patient adherence to follow‑up in the era of mobile information technology: a systematic review and meta‑analysis. PLoS One. 2014;9:e104266. https://doi.org/10.1371/journal.pone.0104266.
Leiby BE, Hegarty SE, Zhan T, Kim S, Patel R, Lewis J, et al. A randomized trial to improve adherence to follow‑up eye examinations among people with glaucoma. Prev Chronic Dis. 2021;18:E52. https://doi.org/10.5888/pcd18.200567.
Moore K, Stuewig J, Tangney J. Jail inmates’ perceived and anticipated stigma: implications for post‑release functioning. Self Identity. 2012;12:527–540. https://doi.org/10.1080/15298868.2012.702425.
Lin WC, Chen JS, Kaluzny J, Chen A, Chiang MF, Hribar MR. Extraction of active medications and adherence using natural language processing for glaucoma patients. AMIA Annu Symp Proc. 2021;2022:773–782.
Funding
L.E.W. (T32GM007198-48S1) and L.H.S. (T32GM007198-49) are supported by the NIH Medical Scientist Training Programme. J.S.C. is supported by a research award from the VitreoRetinal Surgery Foundation. J.M.Y. is supported by the Programme in Medical Education - Health Equity (PRIME-HEq) at UCSD.
Author information
Authors and Affiliations
Contributions
LEW, JSC, and NLS contributed to the conception and design of study; LEW, JSC, TS, LHS, JMY, SL, FGPK, and KVM contributed to the acquisition of data; J.S.C. contributed to analysis of data; LEW, JSC, JEL, and NLS contributed to the interpretation of data; LEW, JSC, and NLS contributed to drafting the work. All authors reviewed and revised the work, granted final approval for publication, and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wedekind, L.E., Chen, J.S., Sestak, T. et al. Ophthalmic care at an academic medical centre for patients who were incarcerated or in immigration detention. Eye 39, 3015–3020 (2025). https://doi.org/10.1038/s41433-025-04005-8
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-025-04005-8