Abstract
Digital therapeutics (DTx) intervention is an emerging therapy for the treatment and long-term management of hypertension. We aim to systematically evaluate the overall effect of DTx intervention on improving hypertension management. The systematic review and meta-analysis of RCTs was conducted and the PubMed, EMBASE, Web of Science, and Cochrane Library were searched to identify eligible RCTs published between Jan 1, 1982 and Sep 10, 2023. Random-effect models were utilized to pool estimates of net changes in systolic blood pressure (BP), diastolic BP, BP control rate, body mass index, weight, waist circumference, and physical activity between the DTx group and control group. 15 RCTs were included with a total of 3789 participants. Compared with the control group, DTx intervention was associated with significant changes in systolic BP, diastolic BP, and BP control rate of –3.75 mmHg(95% CI –5.74 to 1.77), –1.79 mmHg (95% CI –2.81 to –0.77) and 1.47% (95% CI 1.10 to 1.95), respectively. In addition, DTx intervention was statistically significant for improving other risk factors such as lower BMI (−0.5 kg/m2, 95% CI –0.86 to −0.15), increased physical activity (66.73 min/week, 95%CI 49.64 to 83.81), and reduced waist circumference (−2.91 cm, 95% CI −5.15 to −0.66). No difference between groups was demonstrated in weight (P = 0.30). Subgroup analyses revealed consistent effects of the change in SBP and DBP across study duration, age, sample size, patient baseline status, and intervention scenario settings(P > 0.05). DTx intervention may be useful for lowering BP and long-term management of hypertension. More large-size trials providing evidence on the same product are needed.

Similar content being viewed by others
Introduction
Hypertension is the most common preventable risk factor for cardiovascular disease (including coronary heart disease, heart failure, stroke, myocardial infarction, atrial fibrillation and peripheral artery disease), chronic kidney disease (CKD), and cognitive impairment, and is the leading single contributor to all-cause death and disability worldwide [1, 2]. Hypertension is estimated to affect 33% of adults aged 30–79 worldwide and the number of adults with hypertension doubled from 650 million in 1990 to 1.3 billion in 2019 [3, 4]. Globally, high systolic blood pressure (SBP) leads to 108 million deaths and 235 million disability-adjusted life years [1]. Nevertheless, among adults aged 30–79 years with hypertension, 21% are considered to have their hypertension controlled globally and only 16% in China [5]. Suboptimal adherence, which includes failure to initiate pharmacotherapy, to take medications as often as prescribed, and to persist in therapy long-term, is a well-recognized factor contributing to the poor control of blood pressure in hypertension [6]. In some instances, strategies to promote home blood pressure monitoring(HBPM) and long-term management of hypertension have been shown to reduce blood pressure(BP) and improve hypertension control rates [7, 8], particularly when coupled with interventions that lead to treatment intensification [9].
Mobile health and telemedicine technologies have great potential for development in chronic disease management in recent years [10, 11]. Several review articles evaluated the effectiveness of mHealth or smartphone apps for promoting blood pressure management, medication adherence, and lifestyle improvement [12, 13]. Nevertheless, despite the widespread availability of mobile health interventions and software as a medical device(SaMD) claiming to promote hypertension control or medication adherence, not many products have been developed with the involvement of health professionals, have an independent core program, and have been rigorously validated for BP-lowering efficacy [14, 15]. In 2019, the International Digital Therapeutics Alliance defined digital therapeutics (DTx) as, delivering evidence-based therapeutic interventions that are driven by high-quality software programs to prevent, manage, or treat a medical disorder or disease [16]. Digital therapeutics emphasizes evidence-based interventions and high-quality devices to optimize patient care and health outcomes, further rigorously specifying the techniques and categories of digital interventions used for disease treatment and management. Some randomized controlled trials (RCTs), such as HERB-DH1, demonstrated the efficacy of digital therapeutics systems in reducing BP and improving home self-measurement without medications compared with conventional lifestyle interventions [17, 18]. A 2023 narrative review reported potential BP-lowering mechanisms of DTx in hypertension and the process of treating hypertension with DTx [11]. However, due to the ambiguity of the necessary attributes of DTx and the lack of consistency of diverse interventions of DTx products, the analysis only reported a review of the mhealth app interventions. The evidence on the digital therapeutic approach has not yet been synthesized and appraised and the pooled quantitative effect of DTx in hypertension management remained unclear.
Therefore, the current systematic review and meta-analysis centers on the ability of DTx products to generate and deliver validated and measurable medical effects directly to hypertension patients from RCTs, including lower BP and other relevant characteristics. It also further explores where the effects varied by trial duration, and setting, as well as to identify individuals who might benefit most from digital therapeutics products.
Methods
This systematic review of RCTs was conducted in accordance with the Cochrane Handbook for Systematic Reviews of Interventions (Version 6.4). The results were reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Statement (2020). The protocol is registered with PROSPERO (CDR 42024501858).
Search strategy
The search focused on the identification of studies relating to digital therapeutic for hypertension management conducted worldwide. Medline (via Ovid), Embase, Web of Science, the Cochrane Central Registry of Controlled Trials (CENTRAL), and the Cochrane database of systematic reviews for the period up to September 10, 2023 were searched to identify relevant studies. A combination of search terms was used, including Hypertension; Hypertension or Blood Pressure, High or Blood Pressures, High or High Blood Pressure or High Blood Pressures (for the disease type); Smartphone App, Smartphone Apps, Smartphone application, APP Mobile; Telemedicine, Computer-Assisted Drug therapy, Medical Informatics Application, eHealth, Telecommunication, Mobile health, mhealth, Digital health, Telemonitoring (for digital therapeutic). The full search strategy was included in the Appendix p2. Reference lists from related original articles and reviews were also investigated. No language limitation was applied. To ensure the comprehensiveness of the search, we also scanned clinical research database (https://clinicaltrials.gov/), the product library of the digital therapeutics alliance (https://dtxalliance.org/understanding-dtx/product-library/) and the catalog of cleared and approved medical device information from U.S. Food and Drug Administration (https://www.accessdata.fda.gov/scripts/cdrh/devicesatfda/index.cfm) to obtain current clinical trials and products related to antihypertensive digital therapeutics to look back upon the potentially additional studies.
Study selection
To determine the studies to be assessed further, two review authors independently scanned the abstract, title, or both sections of every record retrieved. All potentially relevant articles were investigated as full text. Two investigators (JXT and GJY) independently screened all titles and abstracts to determine eligibility for inclusion in the meta-analysis. In cases of discordance of opinion, a third author (LL) was consulted to achieve consensus. We identified studies among adults and only randomized controlled trials by manually reviewing titles, abstracts, and texts from eligible articles.
Eligibility criteria
Eligible RCTs included the following characteristics:
-
(1)
adult patients (≥18 years) with hypertension who were defined: as patients with inadequately controlled blood pressure (BP ≥ 140/90 mmHg or home BP ≥ 135/95 mmHg whether or not they are receiving hypertension medication) and stage 1 hypertension (BP is 130–139 or 80–89 mmHg).
-
(2)
software was included if it was used for more than one disease (e.g., diabetes and hypertension) and patients with hypertension or comorbid diseases were included as study participants.
-
(3)
the intervention in the experimental group fit into the following intervention criteria for DTx.
-
(4)
changes in SBP or diastolic blood pressure (DBP), blood pressure control, and and health related outcomes were reported, excluding articles that reported only outcomes not related to improvements of health management.
-
(5)
had a comparison group receiving usual clinical care, health education, advice only, or standard follow-up.
Both peer-reviewed publications and conference abstracts were included, but conference abstracts need to report RCT findings as a complement to the RCT’s research design and rationale articles.
According to the definition and core principles of the DTx Alliance, the criteria for digital therapeutics were explicated in this study as (1) Software driving: the interventions of products need to be computer-based software, platforms, and smartphone applications(apps). Through other channels that are not specifically designed for hypertension management algorithms or programs are not eligible, such as telephone, WeChat, SMS, and e-mail, etc (2) Algorithm and model supporting: independent algorithms or models for digital therapeutic products need to be designed for or developed with the collaboration of medical professionals (3) Intervention: software or apps that respond to user input and aim to generate tailored content to blood pressure control or other multiple hypertension care behaviors improvement domains through feedback, customized antihypertensive plans (including dynamically adjusted medication, lifestyle, and disease care prescriptions and advice), reinforcement and rewards, risk scoring and alerts, patient decision support, goal setting, or reminders. Any program, website, or app that is used only for hypertension monitoring or self-reporting, without a feedback interactive system, only for communication or general health education between patients and professionals, and only targeted exclusively at health professionals is not eligible.
Data extraction
For studies that fulfilled inclusion criteria, three review authors (LL, GJY, JXT) independently extracted relevant population and intervention characteristics using standard data extraction templates and completed an intervention description and information extraction form. This included (1) Author(year); country; (2) Sample size; (3) Age (year); (4) Setting; (5) Study population; (6) BP Change as Primary Outcome; (7) SBP/DBP at Baseline; (8) Information related to primary and secondary outcomes; (9) Intervention duration(month), and (10) Adherence and participation measures. Any disagreements were resolved through discussion. Post-intervention blood pressure change means and standard deviations were recorded whenever possible.
Outcomes and quality assessment of included studies
The revised Cochrane risk-of-bias version 2 tool was used to assess the quality of the studies on aspects of selection (random-sequence generation and allocation concealment); performance and detection (masking of participants, personnel, and assessors; deviations from intended interventions; missing outcome data; and measurement of the outcome); appropriateness of analysis (selection of the reported outcome); and bias arising from period and carryover effects (for crossover studies). For quality assessment, 2 coders independently assessed the quality of included studies (LL and GJY).
Integrating all the factors contributing to hypertension management into a unified model to describe how they might affect outcomes is challenging. As many of the health outcomes take many years to develop, it is not practical to use them as primary outcome measures for this review as followed-up in the studies would not be long enough to demonstrate differences in these. However, more proximal variables such as changes in SBP and DBP, and blood pressure control rate, may change over suitable scales. The prespecified primary outcomes of interest were average changes in SBP, DBP, and BP control rate, and secondary outcomes included BMI, weight, waist circumference, and physical activity.
Statistical analysis
The Synthesis Manager used a random-effects model and computed mean difference (MD) to generate pooled estimates of outcomes between the intervention group and the control group. Heterogeneity was assessed by the Q and I2 statistics. If data were available from two or more studies, the outcomes were included in the meta-analysis.
For each research included, the net effect size was defined as the difference in BP change between the intervention and control groups, and was calculated by subtracting the baseline (a) to follow-up (b) change in the control group from the corresponding change in the intervention arm: (Ia−Ib) − (Ca−Cb). If SE or 95% CI were reported instead of SD or SE, then these were calculated as described in Chapter 7.7.3.2 of Cochrane’s handbook [19]. If none of SD, SE, or 95% CI could be obtained from published data or following communication with the authors, then SDs were imputed according to the recommendations in Chapter 16.1.3.1 of Cochrane’s handbook [19].
Priori-defined subgroup analyses were performed to further evaluate the effect of DTx on BP control according to hypertensive status at baseline (whether inclusion criteria included inadequate BP control), antihypertensive use, intervention duration (<6 months or 6 ~ 12 months or ≥12 months), age (<60 years or ≥ 60 years) and intervention setting (hospitals or primary care clinics), sample size (<200 or ≥200 participants). Inadequate BP control was defined as an in-office BP ≥140/90 mmHg or a HBPM ≥135/85 mmHg, per the JNC-8 guideline (Paul A. James et al.) [20] and 2017 ACC/AHA BP Guideline (Whelton et al.) [21]. The associated p-value of <0.1 suggests that heterogeneity is unlikely to be caused by chance alone.
The robustness of summary effect size was assessed via sensitivity analyses that included sequentially removing each study and reanalyzing the remaining datasets to identify if a single study was responsible for the direction of associations. Potential publication bias between studies was assessed by visually inspecting a funnel plot of the mean change in SBP and DBP plotted against their corresponding SE. The Egger test was used to quantify any asymmetry among the funnel plots, with p < 0.05 indicating potential bias and p > 0.05 indicating no significant publication bias. Statistical analyses were performed using Review Manager 5.4 (The Cochrane Collaboration, 2020, Copenhagen, Denmark) and Stata 17.
Results
Study selection and characteristics
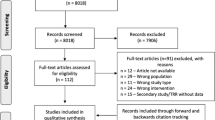
A total of 7732 records were imported into Endnote and 1789 duplicates were removed. After title and abstract screening, of these 5943 articles, 5449 were removed because they did not meet the inclusion criteria. 494 were used for full-text screening. A total of three authors first worked independently in the screening and selection process and then compared their results. Disagreements were resolved through a round of discussion.15 studies with a total of 3789 participants fulfilled the inclusion criteria and were included in the current meta-analysis. (Fig. 1)
Characteristics of the included studies are shown in Table 1. 12 studies were conducted in the past 5 years (2019 and after) and 3 between 2011 and 2018. 7 studies were undertaken in the United States [12, 22,23,24,25,26,27], 2 in China [28, 29], 1 in Japan [17], 1 in Spain [30], 1 in England [18], 1 in German [31], 1 in Iran [32], 1 in Korea [33]. 13 RCTs employed a parallel group design and 2 a cluster design [23, 31]. 13 studies used smartphone APP as the primary mode of delivery of the digital health intervention, 1 used website [26], and 1 used software accessed via wireless tablet computers [27]. All studies had a mean of 253 participants and 66.7% retention over a mean duration of 6 months. At baseline, participants had a mean age of 56.4 years, a mean SBP of 146.2 mmHg, and a mean DBP of 88.4 mmHg.
We included studies of people with hypertension, but the condition of the participants varied from study to study. For instance, five studies involved patients with hypertension who also had diabetes mellitus [12, 17, 24, 28, 30]. Seven studies included patients with various other diseases, such as coronary heart disease, stroke, heart failure, asthma, etc. One study did not report on any other conditions in the participants [26], and seven studies focused exclusively on patients with primary hypertension who did not have any other diseases [18, 22, 25, 29, 31, 32, 34]. The participants were already taking antihypertensive medications at baseline in nine studies. Only one study included non-medicated participants [17], and in 6 studies most participants were not receiving antihypertensives. 8 RCTs only included participants with uncontrolled hypertension, whereas 7 RCTs also included participants with controlled hypertension, with 1 RCT included participants with Stage 1 hypertension [32]. 9 studies were conducted with patients recruited from primary care clinics or the community, and 6 were conducted in hospitals. The follow-up period ranged from 8 weeks to 12 months.
Intervention types varied considerably. The intervention categories in the eleven studies involved hypertension monitoring, recording, reminders, and abnormal blood pressure alerts [12, 17, 18, 22, 24, 26, 29,30,31,32,33]. The carriers of 24 h ambulatory BP monitoring (ABPM) are HPCP APP [24], HERB APP [17], PIA APP [31], Medisafe APP [22] automatic oscilloscope equipment [12], Bluetooth monitor [30, 33]. Patients can also manually record their BP [12, 23, 29], and the APP can give feedback on blood pressure level on the graphic icon [32], and display weekly or monthly blood pressure change charts [30]. Some interventions offered telemonitoring via online data recording forms and had the ability to notify general practitioners about atypical readings. Automatic prescription generation without the need to see a general practitioner was also used. The app alerts users if there is a problem with their blood pressure, users can check information about high blood pressure through the app [29, 34].
Four studies included medication reminder [22, 24, 29, 32], providing alerts to remind patients when they need to take their medications and generate medication adherence reports based on BP or a list of medications and their preferred dosing times from patients. One included medication adherence measurement [30], automatically selecting from the information base to tailor the feedback to the user based on the medication adherence (MA) grading. One included medication change reminder [18], prescribers were asked via email to implement pre-planned medication changes when the average home BP was above target. Three included tailored medication strategies, and embedded algorithms that analyze the input medication data and generate recommendations for the user [27, 31, 33].
Apps were also used for self-care like generating self-care plans, and health reports to help hypertensive patients improve and maintain self-care behaviors [17, 28]. Interventionists managed weekly shared board posts to solicit discussions on self-efficacy, self-regulation, social support, and barriers/facilitators to healthy lifestyles [23]. Due to the smartphones’ capabilities, apps included features reinforcing support, providing advice by “virtual nurses” based on biological, psychological, social data [17], and saving user-recorded information in a web portal for physicians and researchers [32]. Additional functionality included emergency care: Users can call the emergency number with one click to get timely medical treatment [29].
Nine studies assessed the effect of the intervention on promoting a healthy diet and reducing salt intake [17, 26, 32], reducing alcohol and cigarette consumption [17], weight control [12, 17, 24, 26, 28, 32], physical activities [26], improving sleep conditions [17, 24], coping with stress [17, 25], and providing cessation incentives [32]. DTx delivered evidence-based health information to patients about hypertension management or online education sessions, ranging in frequency from once a day to once a week. Some interventions allowed participants to interact with health professionals via face-to-face communication. Two studies assessed the feasibility of apps [23, 26].
Most studies were designed to control groups with usual care or enhanced usual care, (eg, laboratory tests and ancillary clinical services tailored to the condition). In most studies, the control group received education only at baseline; however, some studies provided ongoing health education [18, 27]. One study allowed control participants to delay access to the DTx intervention [23]. Three studies required patients to conduct self-monitoring of BP (SMBP) [29, 34], and one provided a BP tracking app with home monitoring [24].
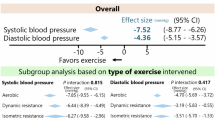
Relative effects of the intervention
Pooled outcomes of SBP (Fig. 2) and DBP (Fig. 3) were similar. SBP (MD –3.75, 95% CI –5.74 to −1.77; 13 studies) with high heterogeneity (I2 = 83%) and DBP (MD –1.79, 95%CI –2.81 to –0.77; 10 studies) with moderate heterogeneity (I2 = 63%) both showed a significant effect in favor of the intervention (P < 0.0001). Five studies reported the BP control rates, and pooled analysis showed a statistically significant effect of the intervention (MD 1.47, 95% CI 1.10–1.95, I2 = 86%). (Fig. 4)
Five studies reported BMI and pooled analysis showed a statistically significant effect of the intervention (MD −0.50 kg/m2, 95% CI −0.86 to −0.15, P = 0.005) (Fig. S1). Two studies reported weight and pooled analysis showed no effect of the intervention (MD −0.90 kg, 95%CI −2.62 to −0.81, P = 0.30) (Fig. S2). Two studies reported waist circumference and pooled analysis showed a moderate effect of the intervention (MD −2.91 cm, 95% CI −5.15 to −0.66, P = 0.01) (Fig. S3). Physical activity is measured in minutes of physical activity per week. Three studies reported physical activity and pooled analysis showed moderate effect of the intervention (MD 66.73 min/week, 95% CI 49.64 to 83.81, P < 0.001) (Fig. S4). Details were available in Appendix p3.
Subgroup analysis
Subgroup analysis showed that whether the blood pressure of the included population was under control or not, the length of the intervention, the number of follow-ups, the place of the intervention, the age, and whether the test population was taking antihypertensive medication were analyzed as subgroup factors, and none of the differences between subgroups were statistically significant. According to our main findings, the effects of digital therapy on SBP and DBP were all significant (P < 0.05), however, after subgrouping, we found that some subgroups did not have satisfactory antihypertensive effects. Also, we hypothesized factors that had an impact on heterogeneity from the subgroup analysis. As shown in the table, when DBP was used as the outcome, after grouping the trial population by whether their blood pressure was controlled or not, the within-group heterogeneity of both subgroups was not significant (P > 0.05, I2 < 50%), which proved that whether the blood pressure of the trial population was controlled or not was one of the factors influencing the heterogeneity. (Table 2)
Sensitivity analysis and bias results
The funnel plot of BP change estimates was roughly symmetrical (Figs. S5 and S6), indicating no significant publication bias (the Egger test: p = 0.599 for SBP and p = 0.737 for DBP). Six and three terms exceeded the confidence interval respectively, suggesting heterogeneity between studies. Due to the considerable heterogeneity of included studies on the effects of digital therapeutic interventions on SBP and DBP, sensitivity analyses were needed to assess the stability and confidence of the results. The results showed that excluding either study, the combined point estimates of the MDs of the remaining studies were within the 95% confidence interval of the effect size, and the results were not highly variable, with good robustness. (Figs. S7 and S8)
Details of the risk of bias in the included studies have been summarized in Figs. S9 and S10. All of the included studies were randomized controlled trials but none were blinded. Three studies did not implement blinding in outcome assessment [26, 27, 32], and three studies did not implement allocation concealment [25, 26, 30]. Studies mostly generated a low risk of bias, though, in a small number of studies, a comprehensive bias assessment revealed several unclear risk components.
Discussion
Principal results
To our knowledge, this study presents the first synthesis of the pooled effectiveness of different DTx interventions in reducing BP and improving other risk factors. Strengths of our study include the use of rigorous standard methodology as documented in the PRISMA and Cochrane guidelines; the comprehensive series of sensitivity analyses performed to ensure the robustness of the calculated summary effect size; and the inclusion of implementation metrics, by limiting inclusion to only randomized controlled trials, thereby restricting potential confounders.
Of the 5943 records identified, 15 RCTs (n = 3789 participants) were included in the meta-analysis, that digital therapeutic interventions were more effective in reducing BP (both SBP and DBP) and improving BP control than usual care. These effects were generally consistent across the different trial settings, sample sizes, intervention durations, and among various population subgroups, which suggested a wide target of hypertensive patients of DTx intervention. In addition, DTx was clinically and statistically significant for improving lifestyle-related metrics such as lower BMI, weight loss, increased physical activity, and reduced waist circumference, compared to traditional interventions. Smartphone APPs are the primary mode of delivering digital health therapy interventions (13 studies, 87%), and therefore smartphone-based DTx interventions are becoming increasingly common ways to support medication adherence and management of hypertension [35]. Our findings provided evidence that DTx intervention could be an important strategy for promoting BP control and improving hypertension health management. From the standpoint of the control group, the mode was not only the usual care and clinical treatment, but also included other modes such as self-monitoring of blood pressure (SMBP) [24, 29, 33], health coaching [18, 27], and so on. Thus, there provided even stronger evidence of the superiority of the digital therapeutic intervention versus the conventional intervention in terms of lowering BP and improvement in the effects of risk factors.
The reductions in BP and improving hypertension-related risk factors were clinically important. Considered overall, digital therapeutic intervention had an incremental BP-lowering effect of −3.75 mm Hg (95% CI −5.74 to −1.77) in SBP, and −1.79 mm Hg (95% CI −2.81 to −0.77) in DBP, and 1.47% in BP control rate (95% CI 1.10–1.95%) compared with control groups. Although the overall net effect was modest from an individual perspective, it is important to note that even relatively small reductions in BP can dramatically reduce the incidence of cardiovascular disease and mortality [36]. There were also statistically significant reductions for BMI (−0.50, 95% CI −0.86 to-0.15), weight (−0.90, 95%CI −2.62 to −0.81), and waist circumference (−2.91, 95% CI −5.15 to −0.66) and increasing for minutes of physical activity per week (66.73, 95% CI 49.64 to 83.81). Many meta-analysis found that weight loss and exercise could benefit blood pressure [37, 38], and therefore DTx may be a potentially effective tool to improve outcomes by these intermediary factors among hypertensive patients broadly.
Combining the results of subgroup analyses, it is indicated that DTx interventions were associated with statistically significant BP reductions, regardless of the mode of delivery of the intervention and patient characteristics at baseline. However, this conclusion is tempered by the considerable heterogeneity of included studies and the high risk of bias in most. For age, most study populations (14 studies) had a mean age of 50 years or above, and only one study had a mean age of 46.5 years [25]. The BP-lowering effect caused by DTx may not be meaningful in more segmented age layers for older adults. It may not be meaningful to explore the antihypertensive effects caused by DTx in more segmented age layers for older adults. For the trial sizes, there was no significant difference in BP change between the follow-up population of ≥200 and the population of <200. Possibly, the study with the largest number of hypertensive patients included 553, which is not large enough compared to other hypertensive RCT trials, so the difference is not revealed.
Notably, this study only explored the effect of DTx interventions on hypertension management and did not refine the effect on patients with hypertension only and also with other diseases. The baseline status of the populations included in the study was not quite the same, though studies were all conducted among the general hypertensive population. Most of studies excluded people with grade III hypertension and above or those with other serious conditions, so DTx interventions may be more appropriate for the general uncontrolled hypertension patients. At the same time, only the HERB trial, excluded the intervention of taking medication, and the other studies included populations that were required to take at least one antihypertensive medication or did not include taking medication in the inclusion criteria, so DTx interventions may be used in the future more as an adjunctive therapy in conjunction with pharmacologic interventions in the treatment and management of hypertension.
Evidence from a large individual trial that meets the optimal sample size would be superior to the results from a systematic review of a similar total sample size to detect the effects of treatment [39]. More large-size trials are needed to validate the role of DTx as a comprehensive intervention strategy in the management of hypertension. Our study found that intervention modes varied widely across DTx products, and it is difficult to carry out combined analyses of different delivery modes. Additional RCT studies providing evidence on the same product are needed, only one effectiveness evidence for one DTx product is much inadequate. In the meanwhile, there was a high heterogeneity of these studies. We ran a series of heterogeneity analyses to explore potential sources, such as subgrouping the studies, but could not fully elucidate the reasons. An inherent source of heterogeneity in our study was the inclusion of DTx interventions because these interventions themselves are heterogeneous. Therefore, additional studies need to describe the mediators and moderators of the effectiveness and implementation of these DTx interventions in detail, and focus on the development of universally applicable and consistent strategies, to both further improve their effectiveness as well as increase their availability and feasibility.
Limitations
This review has some limitations in the evidence. First, all of the included studies were randomized controlled trials but none were blinded, the level of evidence was of moderate quality only. Second, we identified studies from high-income and upper-middle-income countries, primarily, meaning that the findings cannot be generalized. Although lower-middle-income and low-income-countries had higher incidences and debt of hypertension, it is important for future research to collect evidence in these settings too due to the known healthcare equity disparities. Furthermore, considering the availability of mobile phones and the Internet, it is particularly important for patients in rural and remote areas. The effectiveness of these interventions in additional lower-income countries as well as in remote regions warrants examination. Third, 15 RCTs analyzed include those with varying types of blood pressure measurements as primary endpoints, HBPM was the main measurement in the most studies. We used a pooled estimate of the difference in blood pressure before and after the DTx intervention to decrease bias, and tested through sensitivity analysis that removing 24-h ambulatory BP or in-office BP from a single study did not significantly affect the results of the study.
Conclusions
DTx intervention may be useful for lowering BP and long-term management of general hypertensive adults. More large-size trials and studies providing evidence on the same product are needed to validate the role of DTx as a comprehensive intervention strategy in the management of hypertension.
References
Zhou B, Carrillo-Larco RM, Danaei G, Riley LM, Paciorek CJ, Stevens GA, et al. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021;398:957–80.
GBD 2015 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1659–724.
World Population Prospects 2022. Methodoology of the United Nations population estimates and projections. New York: UN; 2022.
World Health Organization. Global report on hypertension: the race against a silent killer. 2023.
Leong DP, Teo KK, Rangarajan S, Lopez-Jaramillo P, Avezum Jr A, Orlandini A. World Population Prospects 2019. Department of Economic and Social Affairs Population Dynamics. New York (NY): United Nations; 2019 (https://population.un.org/wpp/Download/, accessed 20 September 2020). The decade of healthy ageing. Geneva: World Health Organization. World, 2018;73:362k2469.
Burnier M, Egan BM. Adherence in hypertension: a review of prevalence, risk factors, impact, and management. Circ Res. 2019;124:1124–40.
Glynn LG, Murphy AW, Smith SM, Schroeder K, Fahey T. Interventions used to improve control of blood pressure in patients with hypertension. Cochrane Db Syst Rev. 2010;3:CD005182.
Fletcher BR, Hartmann-Boyce J, Hinton L, McManus RJ. The effect of self-monitoring of blood pressure on medication adherence and lifestyle factors: a systematic review and meta-analysis. Am J Hypertens. 2015;28:1209–21.
Tucker KL, Sheppard JP, Stevens R, Bosworth HB, Bove A, Bray EP, et al. Self-monitoring of blood pressure in hypertension: a systematic review and individual patient data meta-analysis. PLoS Med. 2017;14:e1002389.
International Organization for Standardization. Health informatics—Personalized digital health—Digital therapeutics health software systems. Available at: https://www.iso.org/standard/83767.html. Accessed October 10th, 2023.
Kario K, Harada N, Okura A. Digital therapeutics in hypertension: evidence and perspectives. Hypertension. 2022;79:2148–58.
David CN, Iochpe C, Harzheim E, Sesin GP, Gonçalves MR, Moreira LB, et al. Effect of mobile health interventions on lifestyle and anthropometric characteristics of uncontrolled hypertensive participants: secondary analyses of a randomized controlled trial. Healthcare. 2023;11:1069.
Lu X, Yang H, Xia X, Lu X, Lin J, Liu F, et al. Interactive mobile health intervention and blood pressure management in adults: a meta-analysis of randomized controlled trials. Hypertension. 2019;74:697–704.
Alessa T, Hawley MS, Hock ES, de Witte L. Smartphone apps to support self-management of hypertension: review and content analysis. JMIR Mhealth Uhealth. 2019;7:e13645 https://doi.org/10.2196/13645
Xu H, Long H. The effect of smartphone app-based interventions for patients with hypertension: systematic review and meta-analysis. JMIR Mhealth Uhealth. 2020;8:e21759.
Digital therapeutics Alliance. Digital Therapeutics Definition and Core Principles. Available at https://dtxalliance.org/wp-content/uploads/2019/11/DTA_DTx-Definition-and-Core-Principles.pdf. Accessed October 10th, 2023.
Kario K, Nomura A, Harada N, Okura A, Nakagawa K, Tanigawa T, et al. Efficacy of a digital therapeutics system in the management of essential hypertension: the HERB-DH1 pivotal trial. Eur Heart J. 2021;42:4111–22.
Band R, Morton K, Stuart B, Raftery J, Bradbury K, Yao GL, et al. Home and Online Management and Evaluation of Blood Pressure (HOME BP) digital intervention for self-management of uncontrolled, essential hypertension: a protocol for the randomised controlled HOME BP trial. BMJ Open. 2016;6:e12684.
Higgins JPT, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions version 5.1.0. https://training.cochrane.org/handbook/archive/v5.1/ (accessed Jan 16, 2024).
James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the eighth joint national committee (JNC 8). JAMA. 2014;311:507–20.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task force on clinical practice guidelines. J Am Coll Cardiol. 2018;71:e127–248.
Morawski K, Ghazinouri R, Krumme A, Lauffenburger JC, Lu Z, Durfee E, et al. Association of a smartphone application with medication adherence and blood pressure control: the MedISAFE-BP randomized clinical trial. JAMA Intern Med. 2018;178:802–9.
Brewer LC, Jenkins S, Hayes SN, Kumbamu A, Jones C, Burke LE, et al. Community-based, cluster-randomized pilot trial of a cardiovascular mobile health intervention: preliminary findings of the FAITH! trial. Circulation. 2022;146:175–90.
Persell SD, Peprah YA, Lipiszko D, Lee JY, Li JJ, Ciolino JD, et al. Effect of home blood pressure monitoring via a smartphone hypertension coaching application or tracking application on adults with uncontrolled hypertension. JAMA Netw Open. 2020;3:e200255.
Chandler J, Sox L, Diaz V, Kellam K, Neely A, Nemeth L, et al. Impact of 12-month smartphone breathing meditation program upon systolic blood pressure among non-medicated stage 1 hypertensive adults. Int J Environ Res Public Health. 2020;17:1955.
Skolarus LE, Cowdery J, Dome M, Bailey S, Baek J, Byrd JB, et al. Reach out churches: a community-based participatory research pilot trial to assess the feasibility of a mobile health technology intervention to reduce blood pressure among African Americans. Health Promot Pr. 2018;19:495–505.
Neafsey PJ, M Lan CE, Ge M, Walsh SJ, Lin CA, Anderson E. Reducing adverse self-medication behaviors in older adults with hypertension: results of an e-health clinical efficacy trial. Ageing Int. 2011;36:159–91.
Ma Y, Cheng HY, Sit JWH, Chien WT. The effects of a smartphone-enhanced nurse-facilitated self-care intervention for Chinese hypertensive patients: a randomised controlled trial. Int J Nurs Stud. 2022;134:104313.
Gong K, Yan YL, Li Y, Du J, Wang J, Han Y, et al. Mobile health applications for the management of primary hypertension: a multicenter, randomized, controlled trial. Medicine. 2020;99:e19715.
Chandler J, Sox L, Kellam K, Feder L, Nemeth L, Treiber F. Impact of a culturally tailored mHealth medication regimen self-management program upon blood pressure among hypertensive Hispanic adults. Int J Environ Res Public Health. 2019;16:1226.
Leupold F, Karimzadeh A, Breitkreuz T, Draht F, Klidis K, Grobe T, et al. Digital redesign of hypertension management with practice and patient apps for blood pressure control (PIA study): a cluster-randomised controlled trial in general practices. Eclinicalmedicine. 2023;55:101712.
Bozorgi A, Hosseini H, Eftekhar H, Majdzadeh R, Yoonessi A, Ramezankhani A, et al. The effect of the mobile “blood pressure management application” on hypertension self-management enhancement: a randomized controlled trial. Trials. 2021;22:413.
Choi DJ, Park JJ, Yoon M, Park SJ, Jo SH, Kim EJ, et al. Self-Monitoring of blood pressure and Feed-back using APP In TReatment of UnconTrolled Hypertension (SMART-BP): a randomized clinical trial. Korean Circ J. 2022;52:785–94.
Choi D, Park S, Yoon M, Jo S, Kim E, Kim S. Self-monitoring of blood pressure and feedback using app in treatment of uncontrolled hypertension: smart app study. J Hypertens. 2023;41:e317.
Morrissey EC, Casey M, Glynn LG, Walsh JC, Molloy GJ. Smartphone apps for improving medication adherence in hypertension: patients’ perspectives. Patient Prefer Adher. 2018;12:813–22.
Cook NR, Cohen J, Hebert PR, Taylor JO, Hennekens CH. Implications of small reductions in diastolic blood pressure for primary prevention. Arch Intern Med. 1995;155:701–9.
Whelton SP, Chin A, Xin X, He J. Effect of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trials. Ann Intern Med. 2002;136:493–503.
Aucott L, Rothnie H, McIntyre L, Thapa M, Waweru C, Gray D. Long-term weight loss from lifestyle intervention benefits blood pressure?: A systematic review. Hypertension. 2009;54:756–62.
Luo Y, Chang Y, Zhao Z, Xia J, Xu C, Bee YM, et al. Device-supported automated basal insulin titration in adults with type 2 diabetes: a systematic review and meta-analysis of randomized controlled trials. Lancet Regional Health. 2023;35:100746.
Fuchs SC, Harzheim E, Iochpe C, David CN, Gonçalves MR, Sesin GP, et al. Technologies for Innovative Monitoring to Reduce Blood Pressure and Change Lifestyle Using Mobile Phones in Adult and Elderly Populations (TIM Study): Protocol for a Randomized Controlled Trial. JMIR Res Protoc. 2018;7:e169.
Kario K, Nomura A, Harada N, Tanigawa T, So R, Nakagawa K, et al. A multicenter clinical trial to assess the efficacy of the digital therapeutics for essential hypertension: Rationale and design of the HERB-DH1 trial. J Clin Hypertens (Greenwich). 2020;22:1713–22.
Sieverdes JC, Gregoski M, Patel S, Williamson D, Brunner-Jacson B, Rundbaken J, et al. mHealth medication and blood pressure self-management program in Hispanic hypertensives: a proof of concept trial. Smart Homecare Techn, 2013;1:1.
Brewer LC, Jenkins S, Hayes SN, Kumbamu A, Jones C, Burke LE, et al. Community-based, cluster-randomized pilot trial of a cardiovascular mHealth intervention: Rationale, design, and baseline findings of the FAITH! Trial. Am Heart J, 2022;247:1–14.
Acknowledgements
Lu Liu and Lili You designed the study. Lu Liu, Jiayue Guo, and Xitong Jiao reviewed the literature, performed the analyses, and wrote the draft of the manuscript. The manuscript was reviewed and revised by Lili You. All authors contributed to the interpretation of data and the final approved version. This study received no funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liu, L., Guo, J., Jiao, X. et al. The effect of digital therapeutics intervention on improving hypertension management in adults: a meta-analysis of randomized controlled trial. Hypertens Res 48, 456–469 (2025). https://doi.org/10.1038/s41440-024-01892-4
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41440-024-01892-4