Abstract
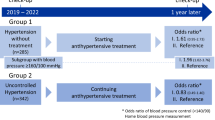
Hypertension is a major risk factor for cardiovascular diseases. This study aimed to clarify blood pressure (BP) management after the health check-up among individuals with grade II or severer hypertension, defined as systolic BP (SBP) ≥ 160 mmHg or diastolic BP (DBP) ≥ 100 mmHg in Japan. This retrospective study used the JMDC Claims Database (2005–2022) in Japan, including 63,785 individuals (median age 50 years; men 75.3%) with BP above grade II hypertension thresholds during the health check-up. We evaluated the BP control and treatment status at 1 year after the first check-up. Poisson regression with robust error variance analyses were performed to assess the association with grade II or severer hypertension at 1 year after the first check-up. Notably, 45.4% continued to have grade II or severer hypertension at 1 year after the first check-up. Among the individuals, 54.5% visited a medical institution within 3 months after undergoing a health check-up, only 23.6% were prescribed antihypertensive medications at 1 year after the first check-up. Factors associated with sustained grade II or severer hypertension included per 5 years lower in age (relative risk [RR]: 1.01, 95% confidence interval [CI]: 1.01–1.02), obesity (RR: 1.04, 95% CI: 1.02–1.06), and skipping breakfast ≥3 times per week (RR: 1.06, 95% CI: 1.04–1.08). Despite strong recommendations for medical consultation, BP control remains inadequate among individuals with grade II or severer hypertension, nearly half of individuals had SBP ≥ 160 mmHg or DBP ≥ 100 mmHg at 1 year after the first check-up in our study. The findings highlight the need for prompt follow-up, particularly among younger adults and those with unhealthy lifestyles.

Similar content being viewed by others
Introduction
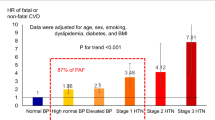
Hypertension is the most prevalent risk factor for cardiovascular disease (CVD) and has a large impact on cardiovascular outcomes [1,2,3]. Managing and controlling hypertension is crucial for preventing subsequent CVD. The global prevalence of hypertension is increasing due to population aging and greater exposure to lifestyle risk factors, such as unhealthy diets and physical inactivity [4]. The proportions of hypertension awareness, treatment, and control that have been reported across many countries vary substantially. Over the past three decades, the proportion of hypertension patients with controlled blood pressure (BP) has risen globally, particularly in high-income Asia-Pacific nations, except Japan [3, 5]. According to a 2016 Japanese survey, the proportion of patients with controlled BP—defined as systolic BP (SBP) < 140 mmHg and diastolic BP (DBP) < 90 mmHg—ranged from 33.3% to 48.0% [6, 7].
The Industrial Safety and Health Act mandates that employers must ensure that their employees undergo annual medical examinations conducted by a physician in Japan. In addition, Specific Health Check-ups and Specific Health Guidance are unique Japanese healthcare initiatives aged from 40 to 74 years aimed at the early detection and prevention of lifestyle-related diseases, focusing on metabolic syndrome through health examinations and guidance to reduce the risk of disease onset, particularly CVD [8, 9]. It is recommended that individuals with SBP ≥ 160 mmHg or DBP ≥ 100 mmHg, as identified during the health check-ups, seek medical consultation promptly [6, 8]. However, there has been no detailed analysis of how individuals with SBP ≥ 160 mmHg or DBP ≥ 100 mmHg during health check-up are treated, and how their BP control evolves. This study aimed to clarify the BP control and treatment status in individuals in whom referral-level BP was observed at the health check-up, using a large-scale Japanese health check-up and claims database.
Methods
Study design and data source
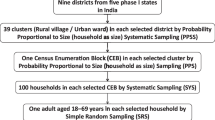
The current study was a retrospective observational analysis using data from the JMDC Claims Database (JMDC, Tokyo, Japan), which is a health claims database in Japan, between 2005 and 2022 [10,11,12]. The JMDC contracts with more than 60 insurers. Most insured individuals in the JMDC database are employees and dependents of relatively large Japanese companies. The JMDC Claims Database includes annual health check-up data, demographics, medical history, medications, and hospital claims with International Classification of Diseases, 10th Revision (ICD-10) coding.
Among the 5,127,304 individuals enrolled in the JMDC Claims Database, the current study focused on individuals aged 20–74 years who had SBP ≥ 160 mmHg or DBP ≥ 100 mmHg at the first health check-up and for more than 1 year after insurance enrollment (one- year look-back period). Exclusion criteria for the current study were as follows: (1) those aged <20 years (n = 5330), (2) those with SBP < 160 mmHg and DBP < 100 mmHg at the first check-up (n = 3,327,918), (3) those with BP data not available at 1 year after the first check-up (n = 1,695,357), (4) those with medication prescriptions for hypertension (n = 21,927), (5) those with a CVD history of myocardial infarction, angina pectoris, stroke, heart failure, dialysis, or renal transplantation (n = 2297), and (6) those with missing data on cigarette smoking (n = 3012), alcohol consumption (n = 4827), physical activity (n = 1929), sleeping quality (n = 709), and breakfast frequency (n = 213). Consequently, the current analysis included 63,785 participants. (Fig. 1).
The Japanese Ministry of Health, Labour and Welfare has provided a recommended protocol for BP measurement. According to the protocol, healthcare professionals were recommended to use either a standard sphygmomanometer or an automated device on the right arm, after the participants had been seated and at rest for 5 min. In principle, BP was recommended to be measured twice, and the average of the two readings was used for assessment, with a single measurement also considered acceptable depending on practical circumstances. When two measurements were performed, the mean of the first and second measurements was to be recorded. We obtained the medication prescriptions for hypertension (WHO-ATC codes starting with C02, C03, C04, C07, C08, or C09), dyslipidemia (WHO-ATC codes starting with C10), and hyperglycemia (WHO-ATC codes starting with A10), from the claims data after the health check-up. In the current study, the visit to a physician within 3 months was defined as any recorded outpatient visit to a medical facility within 3 months following the date of the first health check-up. For medication status, the prescription date listed in the claims data was used to determine the timing of antihypertensive medication use. The medication status at 1 year after the health check-up was determined based on the prescription data recorded on the date closest to the health check-up.
Obesity was defined as body mass index (BMI) ≥ 25 kg/m2. Diabetes was defined as fasting glucose ≥126 mg/dL or use of glucose-lowering medications. Dyslipidemia was defined as low-density lipoprotein cholesterol ≥140 mg/dL, high-density lipoprotein cholesterol <40 mg/dL, triglycerides ≥150 mg/dL, or use of lipid-lowering medications. During the health check-up, employees and dependents are required to complete a standardized self-reported questionnaire concerning their lifestyle habits. Information on cigarette smoking (current or noncurrent/never), alcohol consumption (every day or not every day), healthy sleep as good rest with sleep (yes or no), dietary habit as skipping breakfast ≥3 times per week (yes or no) was collected. We also defined physical inactivity as not performing 30 min of exercise at least twice a week or not walking for more than 1 h per day [13].
Ethics
This study was approved by the University of Tokyo Ethics Committee (approval by the Institutional Review Board of the University of Tokyo: 2018–10862), and was conducted according to the Declaration of Helsinki. Because all data in the JMDC Claims Database were de-identified, the requirement for informed consent was waived in the current study.
Statistical analysis
Descriptive statistics are presented as median (interquartile range (IQR)) and number (percentage). We compared individuals based on their visit to a physician within 3 months after the first health check-up and their antihypertensive treatment status at 1 year. In addition, we evaluated differences among BP categories for isolated grade II or severer systolic hypertension, isolated grade II or severer diastolic hypertension, and grade II or severer systolic and diastolic hypertension. Poisson regression with robust error variance analyses were performed to assess the association with SBP ≥ 160 mmHg or DBP ≥ 100 mmHg at 1 year after the first check-up [14, 15]. The relative risk (RR) was calculated after adjustment for potential confounders, including each of baseline variables. In addition, we performed an analysis adjusted for a variable of the visit to a physician within 3 months after undergoing a health check-up. Moreover, we performed analyses to evaluate independent factors associated with antihypertensive prescription.
Additionally, we compared baseline characteristics between individuals with and without follow-up data at 1 year after the first check-up. The latter group comprised only individuals who had available data on medical visits and antihypertensive medication prescriptions within 3 months after the first check-up. Moreover, these individuals had complete baseline information, including cigarette smoking, alcohol consumption, physical activity, sleeping quality, and breakfast frequency, resulting in 33,175 participants for analysis. Next, we compared individuals based on their visit to a physician within 3 months prior to the one-year follow-up health check-up and their antihypertensive treatment status at 1 year. We classified participants into the following categories based on their follow-up status: a) Follow-up BP ≥ 160/90 mmHg without medical visits, b) Follow-up BP < 160/90 mmHg without medical visits, c) Follow-up BP ≥ 160/90 mmHg with medical visits but without antihypertensive treatment, d) Follow-up BP < 160/90 mmHg with medical visits but without antihypertensive treatment, e) Follow-up BP ≥ 160/90 mmHg with medical visits and antihypertensive treatment, and f) Follow-up BP < 160/90 mmHg with medical visits and antihypertensive treatment. Also, we performed subgroup analyses according to age category, sex, presence or absence of obesity, and individuals aged 40–64 years. P values were calculated by the Mann-Whitney U test or the Kruskal-Wallis test for continuous variables, and chi-square tests for categorical variables. P-values <0.05 were used for statistical significance. All analyses were conducted using Stata version 18 software (StataCorp, College Station, TX, USA).
Results
A total of 63,785 (men 75.3%) individuals were included in our real-world data (RWD) analysis. Among the study participants, 90.0% were insured employees. The median (IQR) age was 50 (44–56) years; median (IQR) SBP was 160 (149–167) mmHg; median (IQR) DBP was 103 (100–108) mmHg; and the median (IQR) BMI was 25.1 (22.6–28.3) kg/m2 at baseline (Table 1). Among those who were recommended to visit a medical institution, 34,789 individuals (54.5%) visited a physician within 3 months after undergoing a health check-up, and only 10,596 individuals (16.6%) were prescribed antihypertensive medications within 3 months after undergoing a health check-up. At 1 year after the first check-up, 28,930 individuals (45.4%) had grade II or severer hypertension and 51,321 individuals (80.5%) still had grade I or greater hypertension. 15,057 individuals (23.6%) were on antihypertensive medication at 1 year after the first check-up. Among the four subgroups, 11,266 (17.7%) visited a physician within 3 months and received antihypertensive treatment at 1 year after the first check-up, while 23,523 (36.9%) visited a physician but remained untreated. 3791 (5.9%) did not visit a physician within 3 months but were prescribed medication at 1 year after the first check-up, whereas 25,205 (39.5%) neither visited a physician nor received treatment. At 1 year after the first check-up, those who visited a physician within 3 months and received treatment had the lowest BP, with SBP at 136 (126–147) mmHg and DBP at 87 (80–94) mmHg. Although fewer in number, individuals who did not visit a physician within 3 months but were on antihypertensive medication at 1 year also had lower BP, with SBP at 137 (128–149) mmHg and DBP at 88 (82–96) mmHg. In contrast, individuals who did not receive treatment at 1 year after the first check-up had the higher BP.
Table 2 presented the baseline characteristics and treatment status of individuals categorized by hypertension subtype at their first health check-up. Those with isolated systolic hypertension were older and had a lower prevalence of obesity, whereas those with isolated diastolic hypertension had higher proportion of men, as well as higher prevalence of cigarette smoking and alcohol consumption. At 1 year after the first check-up, persistent grade II or severer hypertension was most frequent in individuals with grade II or severer systolic and diastolic hypertension (56.9%). The proportion of individuals receiving antihypertensive prescriptions at 1 year was also highest in this group (32.0%) and lowest among those with isolated diastolic hypertension (19.2%).
We compared individuals with (n = 63,785) and without (n = 33,175) follow-up health check-up data at 1 year after their first check-up (Supplementary Table 1). The proportion of men was significantly lower in individuals without follow-up data. The proportion of individuals who visited a physician within 3 months of their health check-up was slightly lower in those without follow-up data (53.1%) compared to those with follow-up data (54.5%, P < 0.001). However, the rate of antihypertensive prescriptions within 3 months was nearly identical between the two groups (16.5% vs. 16.6%, P = 0.60). To further explore the relationship between follow-up BP, medical visits, and antihypertensive treatment status, we categorized participants into six groups based on their follow-up status and provided their characteristics in Supplementary Table 2.
Factors associated with having grade II or severer hypertension at 1 year after the first check-up were identified as per 5 years lower in age (RR: 1.01, 95% CI: 1.01–1.02), obesity (RR: 1.04, 95% CI: 1.02–1.06), per 5 mmHg higher in SBP (RR: 1.05, 95% CI: 1.04–1.05), per 5 mmHg higher in DBP (RR: 1.07, 95% CI: 1.06–1.07), and skipping breakfast ≥3 times per week (RR: 1.06, 95% CI: 1.04–1.08) (Table 3). In the analysis adjusted for the visit to a medical institution within 3 months, the visit to a physician within 3 months after undergoing a health check-up was associated with a reduced risk of SBP ≥ 160 mmHg or DBP ≥ 100 mmHg at 1 year after the first check-up (Table 4).
Factors associated with not receiving antihypertensive medications at 1 year after the first check-up were identified as per 5 years lower in age (RR: 1.02, 95% CI: 1.02–1.02), and skipping breakfast ≥3 times per week (RR: 1.05, 95% CI: 1.04–1.06) (Table 5). Consistent associations were observed across age category and sex (Supplementary Tables 3 and 4). Supplementary Table 5 presented the factors associated with having grade II or severer hypertension at 1 year after the first check-up, stratified by BMI categories at baseline. In the BMI < 25 group, no significant association was observed between age and grade II or severer hypertension, whereas in the BMI ≥ 25 group, lower age was associated with a higher risk (RR: 1.02, 95% CI: 1.02–1.03). Skipping breakfast ≥3 times per week was associated with an increased risk in both BMI groups. Supplementary Table 6 was shown the factors associated with not receiving antihypertensive medications at 1 year after the first check-up, stratified by BMI category. Regardless of BMI, higher BP levels were associated with a lower proportion of individuals remaining untreated. Also, skipping breakfast was associated with a higher proportion of individuals not receiving antihypertensive treatment in both BMI groups. In addition, the analysis was conducted specifically among individuals aged 40–64 years (Supplementary Tables 7–9), the results were generally consistent with those in the overall analysis.
Discussion
In our analysis using a large-scale database in Japan, we found that among individuals in the health check-up with SBP ≥ 160 mmHg or DBP ≥ 100 mmHg, who were strongly recommended for medication consultation, 45.4% individuals had SBP ≥ 160 mmHg or DBP ≥ 100 mmHg at 1 year after the first check-up. 54.5% individuals visited a medical institution within 3 months after undergoing a health check-up, and 23.6% were prescribed antihypertensive medications at 1 year after the first check-up. Factors associated with grade II or severer hypertension (SBP ≥ 160 mmHg or DBP ≥ 100 mmHg) at 1 year after the first check-up included younger age, obesity, and skipping breakfast ≥3 times per week. To the best of our knowledge, this is the first large-scale epidemiological analysis to evaluate BP control after the first check-up among individuals with SBP ≥ 160 mmHg or DBP ≥ 100 mmHg, a level that requires immediate medical consultation according to the health check-ups in Japan.
Hypertension has a high global prevalence and is the leading preventable CVD risk factor worldwide. However, despite the availability of a range of pharmacological treatment options, BP control is often suboptimal [4, 16,17,18,19]. In Japan, a steady decrease in BP levels was observed over a 55-year period. The prevalence of hypertension remains high: over 60% of men aged ≥50 years and women aged ≥60 years display hypertension. However, the control rates of hypertension have shown continuous improvement: they have increased to ~40% over a 36-year period. Nonetheless, the over 50% prevalence of uncontrolled hypertension is a considerable risk for future CVD [7]. Satoh et al. [19] analyzed 27,652 hypertensive patients, showing that 43% had uncontrolled BP (SBP ≥ 140 mmHg or DBP ≥ 90 mmHg) after receiving antihypertensive treatment in Japan. Inadequate treatment, particularly with fewer than three antihypertensive drugs, was a major factor for uncontrolled BP. Consistent with preceding studies, our investigation also highlights the clinical challenges of BP management in real-world clinical settings. Several reviews have emphasized the importance of RWD in understanding and addressing the clinical challenges of hypertension management in Japan. Okada [20] highlighted how RWD can provide valuable insights into treatment patterns and outcomes in hypertension management, facilitating more targeted and effective interventions. Similarly, Tonegawa-Kuji et al. [21] reviewed the utilization of RWD in the cardiovascular field, demonstrating its potential to advance disease prevention and management in Japan. These studies support our findings by underscoring the critical role of RWD in identifying gaps in clinical care and informing strategies to improve BP control in real-world settings.
It is recommended that individuals with SBP ≥ 160 mmHg or DBP ≥ 100 mmHg, as identified during the health check-ups, seek medical consultation promptly. However, within our cohort, only 54.5% of individuals with BP in this range visited a medical institution within 3 months after undergoing a health check-up. It should be noted that the actual proportion of individuals seeking care specifically for BP management may be even lower, as these visits might also include follow-ups for other medical conditions. In the analysis adjusted for the visit to a medical institution within 3 months, visiting a medical institution within 3 months after undergoing a health check-up was associated with a reduced risk of SBP ≥ 160 mmHg or DBP ≥ 100 mmHg at 1 year after the first check-up. Adherence to the recommendations of the health check-up and prompt visit to a medical institution is likely to be crucial for effective BP management. Previous studies emphasized how insights from RWD can guide healthcare policies and improve clinical practice, particularly in managing chronic conditions like hypertension [20, 21]. Incorporating these findings, future initiatives in Japan could focus on enhancing follow-up care and intervention programs tailored to specific populations, using RWD to monitor progress and adjust strategies dynamically.
Factors associated with grade II or severer hypertension (SBP ≥ 160 mmHg or DBP ≥ 100 mmHg) at 1 year after the first check-up included younger age, obesity, and skipping breakfast ≥3 times per week. These findings are extremely implicative. In recent years, the importance of BP management in young adults has been strongly recognized epidemiologically and clinically [22,23,24,25]. Also, epidemiological studies have demonstrated that elevated BP in young adults is associated with an increased risk of future CVD, with the relative risk for young adults being higher than that for older individuals [26,27,28,29]. On the other hand, considering that young adults have a low awareness of health [30], the findings of our study also suggest such a possibility. Therefore, appropriate health education initiatives and social support are urgently needed for this population.
Additionally, obesity itself is a risk factor for hypertension, and the coexistence of obesity and hypertension further increases the risk of future CVD [25, 31, 32]. It should also be emphasized that obesity is associated with a higher prevalence of diabetes and dyslipidemia [33]. For hypertensive cases with obesity detected during health screening, stronger recommendations for medical consultation and appropriate referral to healthcare facilities are needed, as the current study showed that obesity was associated with a higher risk of grade II or severer hypertension. Furthermore, unhealthy lifestyle habits, such as skipping breakfast, are known to be linked to increased risks of hypertension and future CVD in previous studies [34,35,36,37,38]. However, it remains unclear whether skipping breakfast directly contributes to elevated BP or if the underlying irregular lifestyle or work conditions (e.g., shift work) associated with skipping breakfast are related to uncontrolled BP. Also, lifestyle factors, including alcohol consumption, physical activity, and sleep status, differed depending on treatment status in the current study. Further investigation is needed to clarify the relationship between these lifestyle factors and hypertension treatment status.
The strength of this study was to evaluate the outcomes of individuals with referral-level hypertension at 1 year after the first check-up, using claims data in Japan, which highlights significant gaps in strong recommendations for medical consultations and treatment implementation. However, our study has several limitations. First, the study was based on the observational design and data from Japanese health check-up and claims database, which may limit the generalizability of the findings. The challenges of using RWD for research have been discussed in previous studies. Satoh et al. [39] noted that while RWD provides unique insights into hypertension and its association with cardiovascular or renal diseases, issues such as data quality, missing information, and potential biases need careful consideration. These limitations align with those in our study, including the difficulty in strictly differentiating secondary hypertension from the data, as well as unmeasured confounders and selection biases inherent in claims-based databases. Addressing these challenges will be crucial for future research leveraging RWD to produce more robust and generalizable findings. Second, the variables such as socioeconomic status are not included in the database, it is not possible to completely rule out the potential for residual unmeasured confounders. Nevertheless, given that Japan provides universal health coverage to all its citizens, economic factors are less likely to significantly influence the decision-making process for initiating treatment with hypertension drugs. Third, it was possible that selection bias occurred during the process of including and excluding participants. However, when comparing individuals with and without follow-up health check-up data at 1 year, the rate of antihypertensive prescriptions within 3 months was nearly identical between the two groups in the current study. Fourth, the use of antihypertensive medications might have been overreported in the claims database due to the potential misclassification of drugs coded under WHO-ATC categories. While these codes are commonly associated with antihypertensive drugs, they may also include medications prescribed for other conditions, such as heart failure or arrhythmias. To address this issue, we focused on patients with documented BP values indicative of hypertension (grade II or higher) to minimize the impact of non-hypertensive prescriptions. However, it is important to acknowledge that this approach may not completely eliminate the inclusion of non-hypertensive medications, which could lead to minor inaccuracies in our findings. Fifth, a potential limitation of the current study was the influence of regression to the mean. Individuals with extreme first BP values, such as SBP ≥ 160 mmHg or DBP ≥ 100 mmHg, are more likely to show reductions in subsequent measurements, regardless of any treatment received or lifestyle changes. This statistical phenomenon may have contributed to an underestimation of the actual burden of uncontrolled hypertension among the individuals. Sixth, although the standard BP measurement procedures were recommended as described above, it was not unclear whether these methods were accurately or consistently performed in real-world clinical settings. Finally, to evaluate the long-term effects of BP, longer-term follow-up data are warranted.
Perspective of Asia
Hypertension remains a major public health issue across Asia, with considerable variation in awareness, treatment, and control rates among countries [40]. Challenges such as limited access to primary care, poor adherence to therapy, and reliance on monotherapy persist. Our study demonstrates a significant treatment gap in the health check-up, particularly among younger, obese individuals or those with unhealthy lifestyles and grade II or more severe hypertension, despite medical recommendations. These findings reflect broader trends across Asia, where hypertension is often detected through screening but not adequately followed by treatment initiation and sustained management. Regionally tailored follow-up strategies and behaviorally informed interventions may help address this gap.
Conclusion
Our study found that BP control remains inadequate among individuals with grade II or severer hypertension in the health check-up, 45.4% individuals had SBP ≥ 160 mmHg or DBP ≥ 100 mmHg at 1 year after the first check-up despite strong recommendations for medical consultation. It is essential to implement interventions and provide follow-up particularly for younger adults and those with unhealthy lifestyles to enhance BP management.
Data availability
This database is available for anyone who purchases it from JMDC Inc. (https://www.jmdc.co.jp/en/).
References
Lawes CM, Vander Hoorn S, Rodgers A. International Society of H. Global burden of blood-pressure-related disease, 2001. Lancet. 2008;371:1513–8.
Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, et al. Heart Disease and Stroke Statistics-2020 Update: A Report From the American Heart Association. Circulation. 2020;141:e139–596.
Collaborators GBDRF. Global burden and strength of evidence for 88 risk factors in 204 countries and 811 subnational locations, 1990-2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet. 2024;403:2162–203.
Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, et al. Global Disparities of Hypertension Prevalence and Control: A Systematic Analysis of Population-Based Studies From 90 Countries. Circulation. 2016;134:441–50.
Pereira M, Lunet N, Azevedo A, Barros H. Differences in prevalence, awareness, treatment and control of hypertension between developing and developed countries. J Hypertens. 2009;27:963–75.
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens Res. 2019;42:1235–481.
Hisamatsu T, Segawa H, Kadota A, Ohkubo T, Arima H, Miura K. Epidemiology of hypertension in Japan: beyond the new 2019 Japanese guidelines. Hypertens Res. 2020;43:1344–51.
Nakayama T. The fourth phase of specific health checkups and specific health guidance. J Natl Inst Public Health. 2024;73:100–11.
Tsushita K, S Hosler A, Miura K, Ito Y, Fukuda T, Kitamura A, et al. Rationale and Descriptive Analysis of Specific Health Guidance: the Nationwide Lifestyle Intervention Program Targeting Metabolic Syndrome in Japan. J Atheroscler Thromb. 2018;25:308–22.
Ohbe H, Goto T, Miyamoto Y, Yasunaga H. Risk of Cardiovascular Events After Spouse’s ICU Admission. Circulation. 2020;142:1691–3.
Kaneko H, Itoh H, Yotsumoto H, Kiriyama H, Kamon T, Fujiu K, et al. Association of Isolated Diastolic Hypertension Based on the Cutoff Value in the 2017 American College of Cardiology/American Heart Association Blood Pressure Guidelines With Subsequent Cardiovascular Events in the General Population. J Am Heart Assoc. 2020;9:e017963.
Kaneko H, Yano Y, Itoh H, Morita K, Kiriyama H, Kamon T, et al. Association of Blood Pressure Classification Using the 2017 American College of Cardiology/American Heart Association Blood Pressure Guideline With Risk of Heart Failure and Atrial Fibrillation. Circulation. 2021;143:2244–53.
Kaneko H, Itoh H, Yotsumoto H, Kiriyama H, Kamon T, Fujiu K, et al. Association of body weight gain with subsequent cardiovascular event in non-obese general population without overt cardiovascular disease. Atherosclerosis. 2020;308:39–44.
Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–6.
Chen W, Qian L, Shi J, Franklin M. Comparing performance between log-binomial and robust Poisson regression models for estimating risk ratios under model misspecification. BMC Med Res Methodol. 2018;18:63.
Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nat Rev Nephrol. 2020;16:223–37.
Muntner P, Hardy ST, Fine LJ, Jaeger BC, Wozniak G, Levitan EB, et al. Trends in Blood Pressure Control Among US Adults With Hypertension, 1999-2000 to 2017-2018. JAMA. 2020;324:1190–200.
Choudhry NK, Kronish IM, Vongpatanasin W, Ferdinand KC, Pavlik VN, Egan BM, et al. Medication Adherence and Blood Pressure Control: A Scientific Statement From the American Heart Association. Hypertension. 2022;79:e1–14.
Satoh M, Muroya T, Murakami T, Obara T, Asayama K, Ohkubo T, et al. The impact of clinical inertia on uncontrolled blood pressure in treated hypertension: real-world, longitudinal data from Japan. Hypertens Res. 2024;47:598–607.
Okada M. Big data and real-world data-based medicine in the management of hypertension. Hypertens Res. 2021;44:147–53.
Tonegawa-Kuji R, Kanaoka K, Iwanaga Y. Current status of real-world big data research in the cardiovascular field in Japan. J Cardiol. 2023;81:307–15.
Saely CH, Risch L, Frey F, Lupi GA, Leuppi JD, Drexel H, et al. Body mass index, blood pressure, and serum cholesterol in young Swiss men: an analysis on 56784 army conscripts. Swiss Med Wkly. 2009;139:518–24.
Yano Y, Reis JP, Colangelo LA, Shimbo D, Viera AJ, Allen NB, et al. Association of Blood Pressure Classification in Young Adults Using the 2017 American College of Cardiology/American Heart Association Blood Pressure Guideline With Cardiovascular Events Later in Life. JAMA. 2018;320:1774–82.
Andersson C, Vasan RS. Epidemiology of cardiovascular disease in young individuals. Nat Rev Cardiol. 2018;15:230–40.
Suzuki Y, Kaneko H, Yano Y, Okada A, Itoh H, Matsuoka S, et al. Association of Cardiovascular Health Metrics With Risk of Transition to Hypertension in Non-Hypertensive Young Adults. Am J Hypertens. 2022;35:858–66.
Rapsomaniki E, Timmis A, George J, Pujades-Rodriguez M, Shah AD, Denaxas S, et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1.25 million people. Lancet. 2014;383:1899–911.
Suvila K, McCabe EL, Lehtonen A, Ebinger JE, Lima JAC, Cheng S, et al. Early Onset Hypertension Is Associated With Hypertensive End-Organ Damage Already by MidLife. Hypertension. 2019;74:305–12.
Nwabuo CC, Appiah D, Moreira HT, Vasconcellos HD, Yano Y, Reis JP, et al. Long-term cumulative blood pressure in young adults and incident heart failure, coronary heart disease, stroke, and cardiovascular disease: The CARDIA study. Eur. J Prev Cardiol. 2021;28:1445–51.
Kaneko H, Yano Y, Okada A, Itoh H, Suzuki Y, Yokota I, et al. Age-Dependent Association Between Modifiable Risk Factors and Incident Cardiovascular Disease. J Am Heart Assoc. 2023;12:e027684.
Bucholz EM, Gooding HC, de Ferranti SD. Awareness of Cardiovascular Risk Factors in U.S. Young Adults Aged 18-39 Years. Am J Prev Med. 2018;54:e67–77.
Shihab HM, Meoni LA, Chu AY, Wang NY, Ford DE, Liang KY, et al. Body mass index and risk of incident hypertension over the life course: the Johns Hopkins Precursors Study. Circulation. 2012;126:2983–9.
Hall ME, Cohen JB, Ard JD, Egan BM, Hall JE, Lavie CJ, et al. Weight-Loss Strategies for Prevention and Treatment of Hypertension: A Scientific Statement From the American Heart Association. Hypertension. 2021;78:e38–50.
Ueno K, Kaneko H, Okada A, Suzuki Y, Matsuoka S, Fujiu K, et al. Association of four health behaviors in Life’s Essential 8 with the incidence of hypertension and diabetes mellitus. Prev Med. 2023;175:107685.
Song WO, Chun OK, Obayashi S, Cho S, Chung CE. Is consumption of breakfast associated with body mass index in US adults? J Am Diet Assoc. 2005;105:1373–82.
Cahill LE, Chiuve SE, Mekary RA, Jensen MK, Flint AJ, Hu FB, et al. Prospective study of breakfast eating and incident coronary heart disease in a cohort of male US health professionals. Circulation. 2013;128:337–43.
Witbracht M, Keim NL, Forester S, Widaman A, Laugero K. Female breakfast skippers display a disrupted cortisol rhythm and elevated blood pressure. Physiol Behav. 2015;140:215–21.
Rong S, Snetselaar LG, Xu G, Sun Y, Liu B, Wallace RB, et al. Association of Skipping Breakfast With Cardiovascular and All-Cause Mortality. J Am Coll Cardiol. 2019;73:2025–32.
Kaneko H, Itoh H, Kiriyama H, Kamon T, Fujiu K, Morita K, et al. Possible association between eating behaviors and cardiovascular disease in the general population: Analysis of a nationwide epidemiological database. Atherosclerosis. 2021;320:79–85.
Satoh M, Nakayama S, Toyama M, Hashimoto H, Murakami T, Metoki H. Usefulness and caveats of real-world data for research on hypertension and its association with cardiovascular or renal disease in Japan. Hypertens Res. 2024;47:3099–113.
NCD Risk. Factor Collaboration. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021;398:957–80.
Acknowledgements
The authors’ responsibilities were as follows—HK, KK, and YS designed the research; YS analyzed data; KK, HK, and YS wrote the manuscript; AO, AM, KF, NT, HM, TA, KH, KN, YF, KM, HY, and NT interpreted data; KK, HK, and YS revised the manuscript; AO, AM, KF, NT, HM, TA, KH, KN, YF, KM, HY, and NT critically revised the manuscript for important intellectual content; HK had primary responsibility for final content; and all authors: read and approved the final manuscript.
Funding
This work was supported by a grant from the Ministry of Health, Labour and Welfare, Japan (23AA2003). Open Access funding provided by The University of Tokyo.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Research funding and scholarship funds (HK and KF) from Medtronic Japan Co., LTD, Boston Scientific Japan Co., LTD, BIOTRONIK JAPAN INC, and SIMPLEX QUANTUM Inc. HK holds shares in PrevMed Co., Ltd. and Japan Preventive Medical Development Institute Co., Ltd. NT received research funding from Kyowa Kirin Co Ltd; research funding from Bristol Myers Squibb Japan. KN received honoraria from AstraZeneca, Bayer, Boehringer Ingelheim Japan, Daiichi Sankyo, Eli Lilly Japan, Kowa, Mitsubishi Tanabe, MSD, Novartis, Novo Nordisk, and Otsuka; research funding from Astellas, Bayer, Boehringer Ingelheim Japan, Fuji Yakuhin, Mochida, and Novartis; and scholarships from Abbott Medical, Boehringer Ingelheim Japan, Daiichi Sankyo Healthcare, Mitsubishi Tanabe, and Teijin.
Ethics approval and consent to participate
Name of the ethics committee: the Clinical Research Review Board of The University of Tokyo [2018-10862].
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kitaoka, K., Kaneko, H., Suzuki, Y. et al. Blood pressure control and treatment status at 1 year after the first health check-up in individuals with observed referral-level blood pressure. Hypertens Res 48, 2537–2547 (2025). https://doi.org/10.1038/s41440-025-02284-y
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41440-025-02284-y