Abstract
The incidence of low serum testosterone has been increasing in men of all ages across a period which also corresponds to an increasing prevalence of kidney stones. Currently, the relationship between testosterone and kidney stones is unclear. Using the TriNetX Research Network, we performed a retrospective cohort study to evaluate the risk of developing an initial kidney stone in men based on their total testosterone level. Men aged ≥18 were divided into a low testosterone (<300 ng/dL) and normal testosterone (≥ 300 ng/dL) cohort. Men were excluded if they had a history of a kidney stone encounter diagnosis before testosterone measurement and a history of testosterone therapy prescription at any point. Propensity score matching was employed with an absolute standardized mean difference of less than 0.1 used as an indicator of successful matching. Our main outcome of interest was risk of developing an initial kidney stone in men aged ≥18 and within age-based subgroups. In men 18 and older, low testosterone was associated with a higher risk of one or more kidney stone encounter diagnoses (HR 1.12, 95% CI [1.09–1.15]). When stratified by age, no significant association between low testosterone and kidney stone encounter diagnoses was seen in men aged 18–24 (HR 1.09, 95% CI [0.85–1.39]). The highest risk was observed in men with low testosterone aged 34-44 (HR 1.29, 95% CI [1.17–1.38]). In this study, low serum testosterone was associated with an increased risk of initial kidney stone diagnosis in adult men without testosterone therapy prescriptions at any point in their life. Stratifying by age, the increased risk appears to begin in men aged 25, with the highest observed risk in men aged 33-44.
Similar content being viewed by others
Introduction
Testosterone is the hormone vital for the maintenance of secondary sex characteristics in men [1]. The maximum testosterone level a man experiences during their lifetime typically occurs between 20–25 years of age [2]. Serum testosterone levels are known to decline as men age [3, 4]. The proportion of men with low testosterone increases from 20% for men over 60, to 50% for men over 80 [3]. Recently, it has also been shown that serum testosterone levels have been declining on a population level since 1999 in adolescent and young adult males [5]. Symptoms of low testosterone levels include reduced sex drive, erectile dysfunction, sarcopenia, fatigue, depression, and difficulty with memory [6].
Known risk factors for kidney stones include obesity, diabetes, hypertension, metabolic syndrome, hot arid climate, urine electrolyte and pH imbalance [7]. Some of these risk factors are also associated with low testosterone. Medications including loop diuretics, acetazolamide, and topiramate have also been associated with kidney stone formation [8]. Recently, an association between testosterone replacement therapy and increased urinary stone disease was demonstrated [9].
The prevalence of kidney stones has increased worldwide since the 1990s [10]. Once an initial stone develops, kidney stone disease is highly recurrent with varying recurrence rates cited throughout the literature [11, 12]. Men are two times more likely than women to form kidney stones [13]. It is suspected that testosterone may contribute to the disparate rates of kidney stone formation between males and females. However, the role of testosterone in the development of kidney stones remains controversial.
In the present study, we utilize the multi-institutional TriNetX platform to investigate the association between testosterone levels and kidney stones in men aged 18 and older.
Materials and methods
Study design and database identification codes
We conducted a retrospective cohort analysis utilizing de-identified clinical information identified by querying the TriNetX Research Network (Cambridge, MA, USA). The STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines were followed to the best of our ability within the confines of the TriNetX system when writing this manuscript [14]. We used the International Classification of Disease (ICD-10) and RxNorm codes to identify men for inclusion in this study (Supplemental Table 1). The main outcome of this study was one or more encounter diagnoses of kidney stones (calculus of the kidney), ICD-10 N20.0.
Data source and patient selection
We used the TriNetX Research Network, a globally federated health research network to collect de-identified electronic health record (EHR) information compiled from 81 healthcare organizations (HCOs) across 4 countries. Because this study uses only de-identified EHR data, the MetroHealth System Institutional Review Board has deemed using TriNeX in this way exempt from IRB review. Clinical information for men included in this study was curated from 2007–2023. Statistical analyses were performed using the TriNetX platform on 1/7/2024. We selected males (aged ≥18) with a known testosterone level. Men with a kidney stone encounter diagnosis before testosterone measurement ((ICD-10 N20.0 (Calculus of kidney), Z87.442 (Personal history of urinary calculi)) and a history of a testosterone therapy (TTh) prescription ((RxNorm 10379 (testosterone), 37855 (testosterone 17-phenylpropionate)) at any point in their life were excluded. Body mass index (TriNetX Curated 9083, LOINC 39156-5) in this study represents a calculated value curated by the TriNetX research platform. Body mass index (BMI) categories representing underweight ( < 18.5 kg/m2), normal (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2), obesity class I (30.0–34.9 kg/m2), obesity class II (35.0–39.9 kg/m2), and obesity class III ( > 40 kg/m2) were used at the time of propensity score matching. Age in this study represents the age at which men meet the index event, i.e., no kidney stone encounter diagnosis prior to their first laboratory-confirmed level of testosterone in addition to no history of a testosterone therapy prescription at any point in their life. Following American Urologic Association guidelines [15] we used a serum testosterone level of 300 ng/dL to divide the men into a low testosterone (< 300 ng/dL) and normal testosterone (300–1000 ng/dL) group. The collection time of testosterone levels is unknown in the TriNetX database. Demographic and clinical characteristics, including comorbidities and medications, were compared using descriptive statistics for all patients.
To delineate the association between low testosterone and kidney stones in men of different ages, we stratified men by age cohorts. Age strata included men aged 18–24, 25–33, 34–44, 45–54, 55–64, and ≥65. Men in these strata were matched to their eugonadal counterparts.
Statistical analyses and data handling
To address potential confounders, we used propensity score matching based on patient demographic and clinical characteristics within 180 days prior to the index event (Table 1). We used 1:1 greedy nearest-neighbor matching with a caliper of 0.1 pooled standard deviations of the propensity score. An absolute standardized mean difference (SMD) of less than 0.1 for each variable included in the propensity score model indicated successful matching. Our outcome of interest was the risk of developing an initial kidney stone in men aged ≥18 following the first available laboratory-confirmed testosterone value. While testosterone deficiency guidelines [15] recommend using two testosterone values prior to initiating therapy, the purpose of our study was not related to therapy. This study excluded men with testosterone therapy receipt to investigate the association between low testosterone and kidney stones, and therefore a single testosterone value was used for inclusion in this study. Patients were followed until their last record in the TriNetX Research Network. Missing or partial data is not imputed or estimated by the TriNetX platform. Exceptions that may influence this study include discordance with HCO-supplied encounter dates and HCO encounter list. If an encounter is missing a start date, the earliest start data associated with the observations from the same encounter will be used. If an encounter is missing an end date, the latest end date from the observations associated with the encounter will be used. (https://trinetx.com/) Therefore, all patients included in this analysis should not have any missing data for our outcome of interest.
Subgroup analyses were performed on age cohorts. Survival analysis was performed using a log-rank test and Cox proportional hazards regression. Unadjusted (before matching) and adjusted (after matching) hazard ratios (HR) and 95% confidence intervals are reported for each cohort. All analyses were performed on the TriNetX platform without any natural language processing.
Results
Patient characteristics before propensity score matching
The characteristics of all men aged ≥18 included in this study are seen in Table 1. 265,816 men with low testosterone and 530,406 men with normal testosterone were included. The mean ( ± standard deviation) age of men with low testosterone was 53.4 ± 15.7 years and 50.3 ± 15.2 years for men with normal testosterone (SMD 0.201). The age subgroup that differed significantly were men aged ≥65 (SMD 0.182). Comorbidities that differed significantly between the men with low testosterone compared to men with normal testosterone included BMI, encounter diagnoses for essential hypertension, and encounter diagnoses for diabetes mellitus. Furosemide use was the only medication prescription that differed significantly between the groups before propensity score matching.
When subgrouped by age, men aged 18–33 differed significantly in BMI (Supplemental Table 2, 3). Men aged 34–54 differed significantly in BMI, essential hypertension, and diabetes mellitus (Supplemental Table 4, 5). Men aged 34–54 differed significantly in BMI, essential hypertension, and diabetes mellitus, and furosemide use (Supplemental Table 6). Men aged ≥65 differed significantly in age at index, the number of African American men, BMI, diabetes mellitus, chronic kidney disease, heart failure, and furosemide use (Supplemental Table 7).
Patient characteristics after propensity score matching
Propensity score matching established a cohort of 527,114 men aged ≥18 with a measured total serum testosterone level. 263,557 men with low testosterone were matched 1:1 to their eugonadal counterparts. The mean age of men with low testosterone was 53.3 ± 15.7 years whereas the mean age of men with normal testosterone was 52.9 ± 15.3 years. Once matched by propensity score matching, there were no large differences in covariates used for matching indicated by all absolute SMDs <0.1 (Table 1). Age strata for men with low testosterone included men aged 18–24 (n = 11,637), 25–33 (n = 23,582), 34-44 (n = 44,241), 45–54 (n = 56,748), 55–64 (n = 65,642), and ≥65 (n = 73,865). Men in these strata were matched 1:1 to their eugondal counterparts (Table 2).
Kidney stone incidence increases with age regardless of serum testosterone levels
The number of men with low testosterone or normal testosterone with one or more kidney stone encounter diagnoses at any time following a laboratory-confirmed testosterone level in our matched cohorts is shown in Table 2. The proportion of men with one or more kidney stone encounter diagnosis increased with age in both the low testosterone and normal testosterone cohorts. In men aged 18 and older with low testosterone, 9684 (4.10%) men had a kidney stone encounter diagnosis compared to 8879 (3.78%) men with normal testosterone levels (p < 0.0001). Men 18–24 had the lowest proportion of kidney stones encounter diagnoses (1.13% low testosterone; 1.08% normal testosterone, p = 0.515), while men greater than 65 had the highest proportion of kidney stones encounter diagnoses (5.53% low testosterone; 5.46% normal testosterone, p < 0.004).
Association of kidney stones with low testosterone in all men (aged 18 and older)
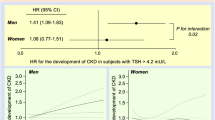
For men 18 and older, low testosterone was associated with an increased risk of incident kidney stone encounter diagnosis compared to men with normal testosterone (adjusted HR: 1.12, 95% CI [1.09–1.15]) (Fig. 1).
The total number of patients in each age subgroup is seen in Table 2.
Association of kidney stones with low testosterone by age stratification
When stratified by age, men with low testosterone aged 25 and older had a statistically significant difference in the risk of initial kidney stone encounter diagnosis compared to men with normal testosterone (Table 2). Men 18–24 with low testosterone did not have a statistically significant difference in kidney stone encounter diagnoses (p = 0.515) (Table 2). Men aged 25-33 have an increased risk of encounter diagnoses of kidney stone compared to their eugonadal counterparts (adjusted HR: 1.15, 95% CI [1.01–1.32]) (Fig. 1). Men aged 34–44 with low testosterone had the highest risk of kidney stone encounter diagnosis when compared to their eugonadal counterparts (adjusted HR: 1.29, 95% CI [1.17–1.38]) (Fig. 1). Men aged 45–54 (adjusted HR: 1.13, 95% CI [1.07–1.20]), 55–64 (adjusted HR: 1.13, 95% CI [1.08–1.19]), and ≥65 (adjusted HR: 1.07, 95% CI [1.02–1.11]) have an increased risk of an encounter diagnosis of kidney stone compared to their eugonadal counterparts (Fig. 1).
Discussion
In this study we used the American Urological Association’s testosterone cutoff of 300 ng/dL to investigate the association between low testosterone and incident diagnosis of kidney stones in 263,557 men with low testosterone [15]. To reduce the risk of confounding, men with low testosterone and normal testosterone were matched by age and BMI, along with comorbidities and medications associated with an increased risk of kidney stones. Our results show that an increased incidence of encounter diagnoses of kidney stones begins in men aged 25 with low testosterone and peaks in men aged 34–44 with low testosterone when compared to their eugonadal counterparts.
The prevalence of reported kidney stones in the National Health and Nutrition Examination Survey has increased dramatically since 1994 [16]. The prevalence of kidney stones increases with age, ranging from 5.1% to 19.7% for men aged 20–39 and greater than 80 years old, respectively [17]. Here, we showed that incident encounter diagnoses of kidney stones increased with age regardless of total testosterone status, but men with low testosterone were diagnosed more often than men with normal testosterone. To the best of our knowledge, no studies exist that investigate whether men with low testosterone experience more complications secondary to kidney stone presence or treatment compared to men with normal testosterone levels.
The excess risk of kidney stone development in men compared to women is not fully explained by differences in lifestyle risk factors [18]. Men are two times more likely than women to develop a kidney stone [13]. Predominant stone composition also differs between males and females. Men are more likely to develop calcium oxalate monohydrate stones whereas women are more likely to develop carbonate apatite and struvite stones [19]. Accordingly, men have been shown to excrete more calcium and oxalate per day than women [20]. To date, the role of testosterone in kidney stone formation is unclear.
Data supporting the role of testosterone in kidney stone development exists in animal models and human studies. Two studies posit that high testosterone levels are associated with kidney stones in men [21, 22]. However, these studies are limited by small sample sizes of 26 [21] and 40 [22] men. The physiologic basis underlying testosterone promotion of stone formation is unknown, but testosterone-induced hepatic glycolate oxidase activity and increased urinary excretion of oxalate have been shown in rats [23]. If transferrable to humans, a similar mechanism may underly the recent association of testosterone replacement therapy with an increased 2-year risk of stone events in hypogonadal men aged 40–64 [9].
Two studies have reported no significant association between testosterone levels and kidney stones [24, 25]. With a median follow-up length of 12.8 years, Knoedler et al. [24] reported no association between testosterone levels and all-time risk of kidney stones in men aged 40–79 living in Minnesota. A total of 102 men developed a kidney stone with 41 men developing an incident kidney stone following hormone measurement. No association between testosterone levels and incident kidney stones was seen in this study. Nackeeran et al. [25] also found no association between testosterone levels and a history of kidney stones in men aged 20 and older when analyzing the National Health and Nutrition Examination Survey (NHANES) [25]. Huang et al. [26] also showed no association between low testosterone and kidney stones in men aged 20–40 when analyzing NHANES [26].
In our study, we demonstrate that low testosterone is associated with an increased risk of incident kidney stone encounter diagnosis. Previously, two studies have shown an association between low testosterone levels and kidney stones [27, 28]. In men aged 41–60, testosterone levels were inversely associated with kidney stone incidence [26]. Importantly, we also showed an association between low testosterone and kidney stones in men aged 25–40. In studies showing an association between low testosterone and kidney stones, patients were either older than 35 [27] or no association was observed in men younger than 40 [26]. While more research is needed to confirm the association between low testosterone and kidney stones, it is important to consider increasing rates of hypogonadism in young adult males that may contribute to an increase in the prevalence of kidney stones in younger men.
Strengths of our study include a large sample size obtained from healthcare organizations from multiple geographic regions. We also employed an extensive list of comorbidities associated with kidney stone formation or low testosterone when matching. To the best of our knowledge, this is also the first study to directly include medications as an exclusion criterion or covariate for propensity score matching.
Limitations inherent to the use of curated EHR data containing de-identified data impact our study. First, we used ICD-10 and RxNorm codes to identify patients, which may contain errors. Second, in attempting to exclude patients with a history of kidney stones, it is possible that patients presented to healthcare organizations not included in the TriNetX platform and therefore have a history of kidney stones unknown to our data. This limitation is also transferrable to our attempt to exclude patients with testosterone therapy prescription at any point in their lives or identifying patients diagnosed with a kidney stone following inclusion in our study. Third, our study is likely not representative of men as a whole, given men were only included if they had a recorded testosterone level. Particularly, younger men may also be underrepresented in our study. Fourth, when splitting our cohort by testosterone values, we potentially discarded useful information inadvertently as a function of dichotomizing a continuous variable. Fourth, we could not control for urologist visits, which may introduce bias regarding the diagnosis frequency of kidney stones. Finally, our study strictly reports the association between low testosterone and renal calculi and thus limits the generalizability of these results to first-time renal stones. Future studies are needed to investigate the association between low testosterone and first-time urolithiasis, including ureteral stones.
The testosterone levels used in our study are also limited as TriNetX does not report the assay used or the time of collection. Given the increasing prevalence of hypogonadism and kidney stones, future studies using morning testosterone levels are needed as the association is currently unclear. Moreover, the dose-response relationship between total testosterone levels and incident kidney stones could also be investigated. Simultaneously, the association between testosterone therapy and kidney stones requires additional research as only one retrospective study has investigated this question. Future studies addressing these questions could inform future treatment of hypogonadal men to minimize the occurrence of kidney stones.
Conclusion
In a cohort of 263,557 men aged 18 and older with low testosterone, we demonstrate that low testosterone ( < 300 ng/dL) is associated with an increased risk of first-time kidney stone encounter diagnoses in men without a history of kidney stones or testosterone therapy prescription when compared to men with normal testosterone. The increased risk appears to begin in men aged 25, with the highest risk of first-time kidney stones observed in men aged 34–44.
Data availability
All data generated or analyzed during this study is included in this published article.
References
Nassar GN, Leslie SW. Physiology, Testosterone. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 [cited 2023 Aug 28]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK526128/.
Zornitzki T, Tshori S, Shefer G, Mingelgrin S, Levy C, Knobler H. Seasonal Variation of Testosterone Levels in a Large Cohort of Men. Int J Endocrinol. 2022;2022:6093092.
Harman SM, Metter EJ, Tobin JD, Pearson J, Blackman MR. Baltimore Longitudinal Study of Aging. Longitudinal effects of aging on serum total and free testosterone levels in healthy men. Baltimore Longitudinal Study of Aging. J Clin Endocrinol Metab. 2001;86:724–31.
Feldman HA, Longcope C, Derby CA, Johannes CB, Araujo AB, Coviello AD, et al. Age trends in the level of serum testosterone and other hormones in middle-aged men: longitudinal results from the Massachusetts male aging study. J Clin Endocrinol Metab. 2002;87:589–98.
Lokeshwar SD, Patel P, Fantus RJ, Halpern J, Chang C, Kargi AY, et al. Decline in Serum Testosterone Levels Among Adolescent and Young Adult Men in the USA. Eur Urol Focus. 2021;7:886–9.
Low Testosterone: Symptoms, Diagnosis & Treatment - Urology Care Foundation [Internet]. [cited 2022 Dec 20]. Available from: https://www.urologyhealth.org/urology-a-z/l/low-testosterone.
Khan SR, Pearle MS, Robertson WG, Gambaro G, Canales BK, Doizi S, et al. Kidney stones. Nat Rev Dis Primer. 2016;2:16008.
Matlaga BR, Shah OD, Assimos DG. Drug-Induced Urinary Calculi. Rev Urol. 2003;5:227–31.
McClintock TR, Valovska MTI, Kwon NK, Cole AP, Jiang W, Kathrins MN, et al. Testosterone replacement therapy is associated with an increased risk of urolithiasis. World J Urol. 2019;37:2737–46.
Stamatelou K, Goldfarb DS. Epidemiology of Kidney Stones. Healthcare. 2023;11:424.
Wang K, Ge J, Han W, Wang D, Zhao Y, Shen Y, et al. Risk factors for kidney stone disease recurrence: a comprehensive meta-analysis. BMC Urol. 2022;22:62.
Moe OW. Kidney stones: pathophysiology and medical management. The Lancet. 2006;367:333–44.
Gillams K, Juliebø-Jones P, Juliebø SØ, Somani BK. Gender Differences in Kidney Stone Disease (KSD): Findings from a Systematic Review. Curr Urol Rep. 2021;22:50.
Elm EV, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61:344–9.
Mulhall JP, Trost LW, Brannigan RE, Kurtz EG, Redmon JB, Chiles KA, et al. Evaluation and Management of Testosterone Deficiency: AUA Guideline. J Urol. 2018;200:423–32.
Scales CD, Smith AC, Hanley JM, Saigal CS. Urologic Diseases in America Project. Prevalence of kidney stones in the United States. Eur Urol. 2012;62:160–5.
Chewcharat A, Curhan G. Trends in the prevalence of kidney stones in the United States from 2007 to 2016. Urolithiasis. 2021;49:27–39.
Ferraro PM, Taylor EN, Curhan GC. Factors associated with sex differences in the risk of kidney stones. Nephrol Dial Transplant. 2022;38:177–83.
Kravdal G, Helgø D, Moe MK. Kidney stone compositions and frequencies in a Norwegian population. Scand J Urol. 2019;53:139–44.
Wood K, Boyd C, Whitaker D, Ashorobi O, Poore W, Gower B, et al. Impact of Demographic Factors and Systemic Disease on Urinary Stone Risk Parameters Amongst Stone Formers. Rev Urol. 2019;21:158–65.
Kuczera M, Kiersztejn M, Kokot F, Klin M. [Behavior of sex hormone and gonadotropin secretion in men with active nephrolithiasis]. Endokrynol Pol. 1993;44:539–47.
Naghii MR, Babaei M, Hedayati M. Androgens Involvement in the Pathogenesis of Renal Stones Formation. PLoS ONE. 2014;9:e93790.
Yoshihara H, Yamaguchi S, Yachiku S. Effect of sex hormones on oxalate-synthesizing enzymes in male and female rat livers. J Urol. 1999;161:668–73.
Knoedler JJ, Krambeck AE, Astorne W, Bergstralh E, Lieske J. Sex Steroid Hormone Levels May Not Explain Gender Differences in Development of Nephrolithiasis. J Endourol. 2015;29:1341–5.
Nackeeran S, Katz J, Ramasamy R, Marcovich R. Association between sex hormones and kidney stones: analysis of the National Health and Nutrition Examination Survey. World J Urol. 2021;39:1269–75.
Huang F, Li Y, Cui Y, Zhu Z, Chen J, Zeng F, et al. Relationship Between Serum Testosterone Levels and Kidney Stones Prevalence in Men. Front Endocrinol. 2022;13:863675.
Polat EC, Ozcan L, Otunctemur A, Ozbek E. Relation of urinary stone disease with androgenetic alopecia and serum testosterone levels. Urolithiasis. 2016;44:409–13.
Otunctemur A, Ozbek E, Cakir SS, Dursun M, Polat EC, Ozcan L, et al. Urolithiasis is associated with low serum testosterone levels in men. Arch Ital Urol Androl Organo Uff Soc Ital Ecogr Urol E Nefrol. 2015;87:83–6.
Acknowledgements
This project was supported in part by the Clinical and Translational Science Collaborative of Northern Ohio which is funded by the National Institutes of Health, National Center for Advancing Translational Sciences, Clinical and Translational Science Award grant, UM1TR004528. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Contributions
AT and DOL conceptualized the study. AT, DOL, NT, and SR conceptualized the methodology. AT performed the formal analysis. AT and BJ were involved in visualization. AT, DOL, SR, BJ, DO, DK, NT were involved in writing and revising the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This study was exempt from Institutional Review Board because only de-identified patient records were utilized from the TriNetX Research Network. This study did not obtain or use protected health information or personally identifying data.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Thompson, A., Omil-Lima, D., Rhodes, S. et al. Low serum testosterone is associated with an increased risk of first-time renal calculi in men without testosterone replacement therapy. Int J Impot Res 37, 623–628 (2025). https://doi.org/10.1038/s41443-024-00963-x
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41443-024-00963-x
This article is cited by
-
Response to comment on: Low serum testosterone is associated with an increased risk of first-time renal calculi in men without testosterone replacement therapy
International Journal of Impotence Research (2025)
-
Comment on: Low serum testosterone is associated with an increased risk of first-time renal calculi in men without testosterone replacement therapy
International Journal of Impotence Research (2025)