Abstract
Ferroptosis is a promising strategy for cancer therapy, with numerous inhibitors of its braking axes under investigation as potential drugs. However, few studies have explored the potential of activating the driving axes to induce ferroptosis. Herein, phosphatidylcholine peroxide decorating liposomes (LIPPCPO) are synthesized to induce ferroptosis by targeting divalent metal transporter 1 (DMT1). LIPPCPO is found to boost lysosomal Fe2+ efflux by inducing cysteinylation of lysosomal DMT1, resulting in glutathione peroxidase 4 (GPX4) suppression, glutathione depletion and ferroptosis in breast cancer cells and xenografts. Importantly, LIPPCPO induced ferroptotic cell death is independent of acquired resistance to radiation, chemotherapy, or targeted agents in 11 cancer cell lines. Furthermore, a strong synergistic ferroptosis effect is observed between LIPPCPO and an FDA-approved drug, artesunate, as well as X rays. The formula of LIPPCPO encapsulating artesunate significantly inhibits tumor growth and metastasis and improves the survival rate of breast cancer-bearing female mice. These findings provide a distinct strategy for inducing ferroptosis and highlight the potential of LIPPCPO as a vector to synergize the therapeutic effects of conventional ferroptosis inducers.
Similar content being viewed by others
Introduction
Ferroptosis is a recently discovered type of cell death that is closely associated with the metabolism of iron, lipids, and amino acids1. It is characterized by unique morphology, biochemical, and genetic changes that distinguish it from other forms of cell death2,3. Ferroptosis has attracted substantial research interest due to its potential role in tumor biology, particularly in refractory cancers4. The harsh tumor microenvironments often pose a dilemma in conventional cancer therapies5, as treatments (e.g., chemo-agents, ionizing radiations) may help establish local control and palliation, but can also lead to cancer cells evolving to become more refractory6. Ferroptosis offers new therapeutic opportunities to synergize with oncological treatments for the conquest of refractory cancers7. For example, IFNγ released from activated CD8+ T cells in immunotherapy downregulates cystine uptake, enhances lipid peroxidation, and increases ferroptosis, thereby contributing to the antitumor efficacy of immunotherapy8. Drug-tolerant persister cancer cells are found to be highly sensitive to ferroptosis9.
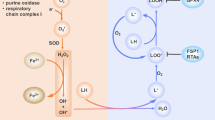
Since the definition of ferroptosis by Stockwell’s group in 201210, various regulatory molecules have been identified. These include system xc−, glutathione peroxidase 4 (GPX4), 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA), coenzyme Q10 (CoQ10), ferroptosis suppressor protein 1 (FSP1), lipoxygenase (LOXs), six-transmembrane epithelial antigen of prostate 3 (STEAP3), divalent metal transporter 1 (DMT1), labile iron pool and lipid peroxides (LOOH). These ferroptosis indices can be integrated into a comprehensive signaling network11, which consists of two braking axes including system xc−/GSH/GPX4 and vitamin B5/acetyl-CoA/HMG-CoA/CoQ10/FSP1 for degradation of lipid peroxides, and two driving axes involving lipid peroxide production (PUFA/LOXs/LOOH) and iron metabolism (STEAP3/DMT1/Fe2+/LOOH)12. Among them, GPX413, FSP114, and system xc−15 in braking axes are found to play critical roles in controlling ferroptosis. Chemical inhibitors targeting these proteins have been extensively studied as candidate ferroptosis inducers. For instance, erastin and sulfasalazine were identified as the inhibitors of system xc−16; RSL3, FINO2, FIN56, and altretamine could directly inhibit GPX4 activity17; Statins (e.g., atorvastatin) could indirectly reduce the activity of GPX4 by suppressing HMG-CoA reductase18. However, few of them have been successful in clinical translation19,20,21, which necessitates a rethinking of the ferroptosis induction manners. Activation of driving axes represents a promising strategy, but synthetic activators are lacking. Among the regulatory proteins in the driving axes of ferroptosis, DMT1 is the critical transmembrane protein as a switch to control the efflux of ferrous iron across lysosomal compartments22. Given that the lysosome is the destination of most nanosized objects23, we speculated that the DMT1 activator could be identified from increasingly produced nanomaterials.
In this study, we aimed to identify the most promising candidates from a group of 70 synthetic materials, including functionalized liposomes, and metallic and carbonaceous nanomaterials, by conducting fluorescent screening of lipid peroxide accumulation in cells. As a result, peroxide-decorating liposomes (LIPPO) were discovered as a potential activator. A lipoxygenase V-catalyzed peroxidation reaction was developed to construct LIPPO formulas with different hydrophobic tails or hydrophilic heads. We evaluated the stability and targeting capability of LIPPO in different biological fluids and cancer cell spheroids, respectively. Our results indicated that the LIPPCPO consisting of 1,2-dilinoleoyl-sn-glycero-3-phosphocholine (PC, 18:2) had the best performance. Dynamic simulations (DMs) revealed a strong interaction between LIPPCPO and lysosomal DMT1, which was further validated in DMT1 knockdown (KD) cells. We examined the cascaded events in LIPPCPO-induced ferroptosis by imaging of subcellular Fe2+, lipid peroxidation, GSH depletion assay, and GPX4 immunoblots. The potential of LIPPCPO-induced ferroptosis was tested in 11 resistant cell lines, including breast cancer, hepatic carcinoma, lung cancer, and melanoma. Moreover, we loaded an FDA-approved drug, artesunate (AS), into LIPPCPO to synergize ferroptosis in breast cancer cells. To evaluate the antitumor effect of AS@LIPPCPO, we used bioluminescence imaging, animal survival rate evaluation, and metastasis assessment in an orthotopic breast tumor model. Our findings indicate that LIPPCPO-induced ferroptosis has potential as a strategy for cancer therapy, and the combination with artesunate further enhances its efficacy.
Results
Discovery of ferroptosis inducers from synthetic nanomaterials
Given that liposomes have been successfully utilized as nanosized vectors in clinical applications, we prepared various liposomes using pristine phospholipids (PL) or functionalized PL with hydroxyl (PL-OH), carboxyl (PL-COOH), and peroxide (PL-OOH) groups at the hydrophobic tails. As PL-OOH is not commercially available, we developed a lipoxygenase-catalyzed reaction to prepare it. Specifically, we evaporated a solution of 1,2-dilinoleoyl-sn-glycero-3-phosphocholine (PC, 18:2) to form a PL layer that allowed peroxidation reactions to occur in the presence of lipoxygenase V (5-LOX). As shown in Fig. 1A, 5-LOX catalyzed oxidation at the bis-allylic position of polyunsaturated phospholipids to form peroxide groups in a stereospecific manner. The functionalized lipid layers were further subjected to sonication and extrusion to prepare phospholipid peroxide-decorating liposomes (LIPPO). The resulting LIPPO was analyzed by liquid chromatography coupled with mass spectrometry (LC-MS). PL and PL-OOH could be differentiated by their LC retention times as well as molecular ion peaks on MS. PC and PCOOH were detected at 13.5 min and 10.1 min with molecular ion peaks at m/z 782.5 and m/z 814.5, respectively (Table 1). The morphology and size of LIPPCPO were further visualized by cryo-electron microscopy (cryo-EM). As shown in Fig. 1B and Supplementary Fig. S1, a spherical unilamellar vesicle structure with a diameter of approximately 87 nm was detected. In addition, we collected other synthetic materials, including metallic and carbonaceous nanomaterials, and subjected them to a comprehensive characterization of primary size, hydrodynamic size, surface charge, and lipid peroxidation (Supplementary Table S1). Although most inorganic nanomaterials formed agglomerates in water, all liposome samples showed hydrodynamic sizes of 90–150 nm in solution.
A Schematic image showing the synthesis of LIPPO. LIPPO was prepared by LOX-mediated oxidation of phospholipids (DG, PC, PS), evaporation, sonication, and extrusion. B Representative images of liposome and LIPPCPO were acquired by cryo-electron microscopy (n = 3). C Heatmap displaying the accumulation of lipid peroxides in cells induced by 15 representative nanomaterials. D Confocal images of FITC-liposomes retained in 4T1 cell organoids (n = 3). 4T1 cell organoids were cultured in normal culture media or tumor microenvironment simulating conditions (acidic & hypoxia). After incubation with FITC-LIPPO for 72 h, the organoids were stained with Hoechst 33342 for confocal imaging. The dashed circles indicate the cell organoids. Source data are provided as a Source Data file.
As lipid peroxidation plays a crucial role in ferroptosis, we utilized a fluorescent substrate (C11-BODIPY) for lipid peroxides to investigate the impact of 70 nanomaterials. Following incubation with the nanomaterials, the treated doxorubicin-resistant MCF-7 (MCF-7R) cells were stained with C11-BODIPY, which emits green fluorescence upon reacting with cellular lipid peroxides24. A high-content imaging system was used to analyze the fluorescence intensity ratio of green v.s. red. Although most nanomaterials had no significant effect (Supplementary Table S1), LIPPCPO-induced dose-dependent accumulation of lipid peroxides in cells, as shown by a heatmap displaying the fluorescence intensity of lipid peroxides induced by representative nanomaterials (Fig. 1C). Liposomes (LIP) prepared in the absence of LOX was used as a control. Additionally, we prepared three phospholipid peroxide-decorating liposomes (LIPPO) with different hydrophilic heads using PC, 1,2-dilinoleoyl-sn-glycero-3-phospho-L-serine (PS, 18:2), and 1,3-dilinoelaidoyl glycerol (DG, 18:2). Since intravenous injection is the most common administration route for liposomal formulations in clinics, LIPPO must cross different biological media to reach their destination, i.e., lysosomes of tumor cells. Therefore, we evaluated the stability of LIPPO samples in three representative bio-contexts, including serum, tumor microenvironment simulated fluid (TMSF), and phagolysosomal simulated fluid (PSF). After 24 h of incubation, the activity of the three LIPPO samples remained relatively stable in serum, suggesting that these functionalized liposomes could maintain their activity during blood circulation (Supplementary Fig. S2). Interestingly, these functionalized liposomes exhibited high activity in TMSF and PSF, with 8.67–41.52% decline in relative fluorescence intensity (RFI). Furthermore, we compared the retention of the three liposomes in 4T1 cell organoids cultured under hypoxic and normal conditions. The liposomes were labeled with fluorescein isothiocyanate (FITC), and their retention in the organoids was visualized by confocal microscopy after 72 h of incubation. As depicted in Fig. 1D, the retention of all three functionalized liposomes in organoids at hypoxic and acidic conditions was higher than that under normal culture conditions. The ratios of retained liposomes were calculated based on the fluorescence intensities in organoids (Supplementary Fig. S3). Notably, among the three liposomes tested, LIPPCPO exhibited the highest retention in 4T1 cell organoids, indicating that it may enable a prolonged interaction with cancer cells.
Impacts of LIPPO on drug-resistant cells
To investigate the effects of LIPPO on drug-resistant cells, we first examined the killing effects of LIPPO. As shown in Supplementary Table S2, the cancer cells developed robust resistances after long-term exposure to antitumor agents, resulting in at least a 10-fold higher IC50 value compared to their parent cells. We evaluated the effects of LIPPO on doxorubicin-resistant MCF-7 (MCF-7R) cell organoids using an MTS assay and included liposomes constructed by pristine DG, PC, or PS for comparison. As shown in Fig. 2A, all of the pristine liposomes had no impact on cell viability, while three LIPPO significantly inhibited the proliferation of MCF-7R cells. Among them, LIPPCPO had the strongest killing effect (80.33%) in MCF-7R cells and was selected for further examination. Compared to DG and PS, PC-based LIPPO exhibited higher stability in PSF, enhanced penetration capability into tumor organoids, and potent killing effects against cancer cells (Fig. 2A). We attribute the superior performance of LIPPCPO to the choline head group of PC, which renders it zwitterionic at physiological pH and facilitates strong binding affinities with other biomolecules.
A Cell viability test in MCF-7R cells. MCF-7R cells were treated with liposomes or LIPPO containing 100 μM lipid peroxides (LIPDGPO, LIPPCPO, LIPPSPO) for 24 h. Cell viability was detected by MTS assays (n = 4 independently treated cell cultures). Data are presented as mean ± SD. **p < 0.01 and ***p < 0.001 compared to the control by two-tailed Student’s t-test. B Resistance-dependent indexes (RDIs) of LIPPCPO and antitumor agents in nine pairs of resistant and sensitive cancer cells. RDIs represent the IC50 ratios of antitumor agents in resistant v.s. sensitive cells. A375-R1 defined as A375 cell resistance to dacarbazine; B16-R1 defined as B16 cell resistance to dacarbazine; A549-R1 defined as A549 cell resistance to cisplatin; LLC-R1 defined as LLC cell resistance to cisplatin; B16-R2 defined as B16 cell resistance to vemurafenib; HepG2-R1 defined as HepG2 cell resistance to sorafenib; LLC-R2 defined as LLC cell resistance to gefitinib; B16-R3 and 4T1-R1 defined as B16 and 4T1 cell resistance to X-rays, respectively. C Resistance acquisition under exposure to DTX and LIPPCPO. An acquired drug-resistance evolution assay was performed by exposing 4T1-R to dose escalation of DTX and LIPPCPO at 24 h intervals from 0.25 × IC50 for 60 days. Source data are provided as a Source Data file.
We then examined the proportion of peroxide in LIPPCPO to acquire an optimized formula for effective cell killing. As shown in Supplementary Fig. S4a, the killing effects of LIPPCPO increased along with the proportion of peroxides and reached a plateau (>80% cell deaths) in MCF-7R and 4T1-R cells at 40% PC peroxides (Supplementary Fig. S4b), which was selected as the ideal formula for further examinations. At this optimal formula, LIPPCPO-treated MCF-7R cells exhibited a significant time-dependent decrease in cell viability from 0 to 24 h, with the proportion of alive cells reaching a minimum level of 17.3% after 48 h (Supplementary Fig. S5). The saturation levels of PC tails significantly impacted the cytotoxicity of LIPPCPO. Among phospholipids with varying saturation levels (18:0, 18:1, and 18:2), only LIPPCPO derived from polyunsaturated PC (18:2) was capable of effectively killing cancer cells (Supplementary Fig. S6). Additionally, we assessed the killing effect of LIPPCPO in more chemo-, radio-, or targeted therapy-resistant cells by calculating the resistance-dependent index (RDI), which is the ratio of IC50 values of antitumor agents in resistant cells relative to parent cells (Supplementary Table S3). Although LIPPCPO demonstrated relatively lower efficacy compared to clinical drugs in sensitive cancer cells, its killing effect remained consistent regardless of the acquired tolerances in resistant cells, displaying the RDIs of LIPPCPO at one in all resistant cells (Fig. 2B). This result indicates that the killing effects of LIPPCPO are independent of acquired resistances. More importantly, its hollow structure enables efficient loading of clinical drugs, allowing for synergistic killing of cancer cells.
In clinics, cancer patients who initially respond to antitumor agents may rapidly acquire secondary resistance to these agents after a few treatments25. To examine whether the administration of LIPPCPO in resistant cells results in the generation of secondary resistance, we treated 4T1-R cells with LIPPCPO by dose escalation for two months. We also included a sensitive chemo-agent, docetaxel (DTX), for comparison (Supplementary Fig. S7). Surprisingly, LIPPCPO showed persistent antitumor effects without triggering detectable resistance in 4T1-R cells during long-term treatment (Fig. 2C). In contrast, 4T1-R cells rapidly developed robust resistance to DTX treatment, displaying a 15-fold increment of IC50 value in the acquired cells.
Cascaded signaling events in LIPPCPO-induced ferroptosis
We compared the effects of apoptosis inhibitor (Z-VAD-FMK), necrosis inhibitor (necrostatin-1, Nec-1), and ferroptosis inhibitor (ferrostatin-1, Fer-1) on LIPPCPO-induced cell deaths. As highlighted in Supplementary Fig. S8, the effects of Fer-1 pretreatment on LIPPCPO-induced cell death were striking. Notably, this intervention led to a substantial increase in cell viability, with improvements ranging from 62% to 72% observed in both MCF-7R and 4T1-R cell lines. These findings underscore the pivotal role of ferroptosis in the observed cell death phenomenon. To unravel the sequential events driving ferroptosis, we further examined the intracellular distribution of LIPPCPO specifically in MCF-7R cells. Confocal microscopy imaging revealed that FITC-labeled liposomes were internalized into cells after 12 h incubation (Supplementary Fig. S9) and overlapped significantly (89.6%) with lysosomes stained with lysosomal-associated membrane protein 1 (LAMP-1) antibodies (Supplementary Fig. S10). The internalized LIPPCPO had a strong association with DMT1, as demonstrated by their colocalization under confocal microscopy (Fig. 3A) as well as the high binding affinity (−5.7 kcal/mol) in molecular dynamics (MD) simulations. We then isolated lysosomes from LIPPCPO-treated cells to extract lysosomal proteins for separation by gel electrophoresis. The gel band containing DMT1 was subjected to digestion by trypsin. The acquired peptides were detected by mass spectrometry for proteomics analysis. Significant molecular weight changes were detected at two topological domains facing the lysosomal compartment. As shown in Fig. 3B, mass peaks at m/z of 752.23 and 1165.90 indicate the formation of disulfide bonds in two peptides from LIPPCPO treatment. Specifically, cysteines at 245, 248, 334, and 365 form two cystines after reaction with LIPPCPO, indicating a cysteinylation of DMT1. The sequences of the two peptides were determined by analyzing the corresponding fragment ions in the mass spectra (Supplementary Fig. S11). In contrast, the control group exhibited a prominent peak of GMFVPSCSGCR at m/z 754.23, indicating a minimal level of cysteinylation (Supplementary Fig. S12). The occurrence of cysteinylation reactions is further supported by MD simulations. Specifically, the MD results demonstrated a rapid association of PC peroxides with DMT1 within 50 ns, during which the PC peroxides interact with amino acids within transmembrane domains (TMD) 5 and 8 (Supplementary Fig. S13). Notably, TMD 5 and 8 contain cysteines at positions 245, 248, 334, and 365, suggesting a high interaction probability of lipid peroxides with these cysteines.
A Confocal microscopy images of colocalization of FITC-liposomes and DMT1 in MCF-7R cells (n = 3). The treated MCF-7R cells were stained with anti-DMT1 antibodies (red). Hoechst 33342 was used to stain cell nuclei (blue). B LIPPCPO-induced cysteinylation at the topological domain of DMT1 facing lysosomal compartment. Lysosomes in LIPPCPO-treated cells or untreated cells were isolated for separation of DMT1 by gel electrophoresis. The DMT1 bands were digested by trypsin for mass spectrometry analysis (Thermo, Easy nLC1200/Q Exactive plus). Peaks at m/z of 752.23 and 1165.90 indicate the formation of disulfide bonds in two peptides. C Confocal microscopy images of Fe2+ distribution in MCF-7R cells (n = 3). The treated MCF-7R cells were stained with FeRhoNox-1 (red). Hoechst 33342 was used to stain cell nuclei (blue). Fe(NH4)2(SO4)2 (FAS, 100 μM) was used as a positive control. D Cell viability in wild-type and DMT1-KD MCF-7R cells exposed to 100 μM LIPPCPO for 24 h (n = 5 independently treated cell cultures). E Effects of iron chelators on LIPPCPO-induced cell death. MCF-7R cells were pretreated with 100 μM deferoxamine (DFO) or deferiprone (DFP) for 2 h and then treated with 100 μM LIPPCPO for 24 h. Cell viability was assessed by MTS assay (n = 6 independently treated cell cultures). F Confocal images of lipid peroxides in MCF-7R cells (n = 3). G Western blotting of GPX4 and H GSH levels in MCF-7R and 4T1-R cells. The treated MCF-7R and 4T1-R cells were stained with the Image-iT lipid peroxidation staining kit to observe the accumulation of lipid peroxides in cells. RSL3 (25 μM) was used as a positive control. Cell lysates were subjected to a Western blotting assay to assess GPX4 expression, and GSH levels were detected by a GSH/GSSG Assay kit (n = 3 independently treated cell cultures). Data are presented as the mean ± SD for (D), (E), and (H). **p < 0.01 and ***p < 0.001 compared to the control by two-tailed Student’s t-test for (D), (E), and (H). Source data are provided as a Source Data file.
Since lysosomes are a reservoir of ferrous ions and DMT1 controls the iron transport, cysteinylation of DMT1 by LIPPCPO may promote the efflux of Fe2+ into the cytoplasm. To confirm this, nonluminous FeRhoNox-1 was used to detect labile Fe2+ in cells, and diffuse red fluorescence of FeRhoNox-1 was observed in LIPPCPO-treated cells (Fig. 3C), indicating that lysosomal internalized LIPPCPO could drive the spatial distribution of lysosomal Fe2+ in the cytoplasm. However, the total iron content in cells had limited changes (Supplementary Fig. S14). To further confirm the role of DMT1, a DMT1 knockdown (DMT1-KD) cell line was established to examine the effect of LIPPCPO. Knockdown of DMT1 in MCF-7R cells dramatically diminished the effects of LIPPCPO on ferrous ion release and the killing effect of LIPPCPO had a 29.76% decline in DMT1-KD cells (Fig. 3D, Supplementary Fig. S15). Iron chelates of deferiprone (DFP) and deferoxamine (DFO) efficiently rescued 60.6% and 62.34% of LIPPCPO-induced cell death, respectively (Fig. 3E). All these results indicate that LIPPCPO could target the DMT1 in lysosomes, facilitate the efflux of Fe2+, and induce iron-dependent cell death, i.e., ferroptosis.
To further validate this cell death type, we examined other cascaded events in the ferroptosis pathways. Since the redox-active ferrous ions in the labile iron pool could drive non-enzymatic peroxidation of lipids24, we first examined lipid peroxidation in MCF-7R cells by C11-BODIPY staining. RSL3 that prevents the degradation of lipid peroxides was included as a positive control. As shown in Fig. 3F, LIPPCPO-induced accumulations of lipid peroxides in MCF-7R cells are similar to the effect of RSL3, as demonstrated by the intensive green fluorescence of oxidized C11-BODIPY. To eliminate this hazard signal, living organisms developed a core selenoenzyme, GPX4 that utilizes glutathione (GSH) to catalyze the degradation of lipid peroxides26. We therefore detected the quantities of GSH and GPX4 in cell lysates. Western blots showed that the LIPPCPO treatment suppressed the expression of GPX4 in cells with a 0.23-fold decrease (Fig. 3G, Supplementary Fig. S16), and induced more than 70% GSH depletion (Fig. 3H). Overall, these results suggest that LIPPCPO can induce ferroptotic cell death in resistant cancer cells by lysosomal internalization, interaction with DMT1, liberation of lysosomal Fe2+, lipid peroxidation, GPX4 suppression, and GSH depletion.
To validate the ferroptotic effect of LIPPCPO in vivo, a syngeneic breast cancer model was established in BALB/c mice by orthotopically transplanting firefly luciferase-transfected 4T1-R (fLuc-4T1-R) cells. The distribution of LIPPCPO was visualized by iodine-125 (125I) labeling under single photon emission computed tomography with computed tomography (SPECT/CT). As shown in Supplementary Fig. S17a, the radioactivity was first detected in tumors 6 h after injection, gradually increased to a peak at 24 h, and declined to the background at 48 h. During treatment, there was no significant body weight loss in any treated mice (Supplementary Fig. S17b). Interestingly, LIPPCPO showed significant accumulation in tumors. Given that the surface corona is increasingly regarded as a key parameter responsible for the biological distribution of nanosized objects, we speculated that LIPPCPO might form a unique surface corona in breast cancer-bearing mice. To investigate this, LIPPCPO was incubated with plasma samples from both healthy and cancer-bearing mice. The surface corona constituents on LIPPCPO were analyzed by proteomics. A comparison of corona constituents revealed 105 proteins with more than 2-fold higher expression in the corona of LIPPCPO formed in the plasma of cancer-bearing mice (Supplementary Table S4). Among these, thirteen highly abundant proteins including endoplasmic reticulum chaperone BiP (HSPA5), β-arrestin-1 (ARRβ1), proliferation-associated protein 2G4 (PA2G4), fatty acid synthase (FASN), neutrophil gelatinase-associated lipocalin (NGAL), von Willebrand factor type A (VWFA), annexin, protein tyrosine kinase (PTK), Ras GTPase-activating-like protein (IQGAP1), protein disulfide-isomerase (PDI), inter-alpha-trypsin inhibitor (IαI), mammalian disintegrin-metalloprotease (ADAMs), and hypoxia up-regulated protein 1 (HYOU1), are closely associated with tumor growth, proliferation, metastasis or microenvironment (Supplementary Fig. S18). These constituents in the corona of LIPPCPO may contribute to its accumulation in tumors.
Tumor-bearing mice were intravenously injected with either DTX or LIPPCPO. After approximately 8 days of orthotopic transplantation, qualified mice were randomly assigned into three groups and given different agents including saline, DTX (36 mg/kg), and LIPPCPO (100 mg/kg) on the 1st, 4th, and 7th day. Tumor samples were collected on the 2nd and 10th day and subjected to IVIS system imaging, immunostaining, and Western blot analysis. The extracted tumor cells were used to validate the ferroptotic cell death. Although the total iron content was similar across all treatments (Supplementary Fig. S14), a significant fluorescent signal of FeRhoNox-1 was observed in the cytoplasm of LIPPCPO-treated tumor cells, indicating an elevation of the labile iron pool (Fig. 4A). Additionally, the tumors were stained with C11-BODIPY to image lipid peroxides using the IVIS system. LIPPCPO-treated tumors showed a strong fluorescent signal emitted by the oxidized C11-BODIPY upon reaction with lipid peroxides (Fig. 4B), displaying a 3.6-fold increase of lipid peroxidation accumulation in tumors (Supplementary Fig. S19). Moreover, we have elaborated on the analysis of cell death markers, including 4-HNE (indicative of ferroptosis), cleaved caspase-3 (associated with apoptosis), and RIP3 (related to necrosis), in tumor sections treated with LIPPCPO. As depicted in Fig. 4C, we observed abundant expression of 4-HNE in LIPPCPO-treated tumor sections. This finding is significant as 4-HNE is a reactive lipid peroxidation product and serves as an indicator of ferroptosis. The pronounced expression of 4-HNE indicates lipid peroxide accumulation in LIPPCPO-treated tumors, consistent with our in vitro findings. In contrast, we noted a significant increase in cleaved caspase-3 expression in tumors treated with DTX, suggesting that apoptosis contributes to the antitumor effect of DTX. Notably, necrotic cell death was not observed in either LIPPCPO- or DTX-treated tumors, as indicated by the lack of significant changes in RIP3 expression in both treatments. Furthermore, the treated tumor tissues were homogenized into lysates to examine GPX4 expression, revealing a dramatic decline (0.37-fold) of GPX4 in tumor lysates treated with LIPPCPO compared to vehicle control (Fig. 4D, Supplementary Fig. S20). These data well validate the induction of LIPPCPO-induced ferroptosis in vivo. Both the in vitro and in vivo results suggest that lysosomal internalized LIPPCPO could induce DMT1 cysteinylation (Fig. 5). This post-modification boosts the efflux function of DMT1 to elevate the level of Fe2+ in the cytoplasm, inducing GPX4 suppression, GSH depletion, lipid peroxide accumulation and ferroptotic cell deaths.
A Representative images of Fe2+ distribution in tumor cells (n = 3). Tumor cells were extracted from LIPPCPO-treated tumor tissue and stained with FeRhoNox-1 for confocal imaging. B Representative images of lipid peroxide accumulation in tumors. Tumors were resected from LIPPCPO-treated tumor-bearing mice and stained with C11-BODIPY for IVIS system imaging. C Representative images of immunostaining (4-HNE, cleaved caspase-3, and RIP3) in tumor sections (n = 3). DTX: docetaxel. D Assessment of GPX4 expression in tumor tissue lysates (n = 3). Source data are provided as a Source Data file.
Lysosomal internalized LIPPCPO reacts with the cysteines at 245 and 248, 334 and 365 sites of DMT1 to form two cystines. This post-modification boosts the efflux function of DMT1 and exports more Fe2+ in cytoplasm, resulting in GSH depletion, GPX4 suppression and lipid peroxide accumulation. These events cumulate into ferroptosis.
Antitumor activity of LIPPCPO formulations
Before conducting in vivo applications, we extensively evaluated the biocompatibility of LIPPCPO. First, we tested the effect of LIPPCPO on red blood cells using a hemolysis assay. The results showed that LIPPCPO at concentrations of 40–200 μM did not cause visible hemoglobin release (Supplementary Fig. S21). We also assessed the biosafety of LIPPCPO by measuring 15 biochemical indexes in blood. The results, shown in Supplementary Table S5, demonstrated no significant changes in immune cell counts, white blood cell counts, platelet levels, mean platelet volume, etc. Furthermore, we found that while LIPPCPO induced significant ferroptotic death in cancer cells, normal tissue cells were less sensitive (Supplementary Fig. S22, Table S6).
Compared to conventional ferroptosis inducers, LIPPCPO displayed a distinct ferroptosis pathway by activating the driving axis. Given the hollow structure of LIPPCPO, we hypothesized that loading hydrophobic ferroptosis inducers could synergize the ferroptosis effect in cancer cells. To test this, we loaded several reported ferroptosis inducers11, including sulfasalazine (SSZ), atorvastatin (AT), artesunate (AS), and altretamine (HMM), into LIPPCPO. Interestingly, AS, an FDA-approved drug, showed strong synergistic killing effects with LIPPCPO, with a correlation factor of 0.1 (Supplementary Table S7). Therefore, we selected AS@LIPPCPO to treat resistant breast tumors at a late stage (with a large tumor size of ∼150 mm3, ∼14 days).
The breast cancer-bearing mice were randomly divided into four groups and treated with intravenous injections of saline, AS (11.7 mg/kg), LIPPCPO (100 mg/kg), or AS@LIPPCPO (111.7 mg/kg) on the 1st, 4th, and 7th day (Fig. 6A). Of the four treatments, AS exhibited limited effects on the growth of resistant breast cancer. In contrast, LIPPCPO and AS@LIPPCPO significantly inhibited tumor growth, as observed in Fig. 6B and Supplementary Fig. S23. The combined treatment led to tumor sizes that were 2.5-fold smaller than those of the vehicle control, demonstrating a potent antitumor effect. These results were further validated using bioluminescence imaging (BLI), a non-invasive optical imaging modality that allowed us to visualize the bioluminescent signals catalyzed by the fLuc-4T1-R cells in vivo. As shown in Fig. 6C, untreated and AS-treated mice displayed intense luminescence with 20.8- and 18.5-fold higher than AS@LIPPCPO treatments, respectively (Supplementary Fig. S24a), indicating rapid duplication of fLuc-4T1-R cells. The fast proliferation of fLuc-4T1-R cells led to nutrient deficiency and cell necrosis, which were evidenced by diminishing luminescence signals in tumor cores on the 21st day. Interestingly, both LIPPCPO and AS@LIPPCPO treatments showed no detectable lung metastases, whereas animals injected with vehicle and AS solution displayed 12–25 metastatic foci per lung with 9.2- and 6.9-fold increment of luminescence intensity, respectively (Fig. 6D, Supplementary Fig. S24b). As a result, all untreated and AS-treated tumor-bearing animals either died or reached a moribund state within 45 days. However, in the AS@LIPPCPO group, three out of five mice survived for more than 60 days, indicating a significant extension in survival time in breast cancer-bearing mice at late stages (Fig. 6E). These data demonstrate that AS@LIPPCPO treatment can effectively extend the survival time of breast cancer-bearing mice at late stages.
A Schematic illustration of LIPPCPO formula treatment in tumor-bearing mice. After 14 days post-implantation of fLuc-4T1-R cells, each mouse received saline (n = 5 mice), Artesunate (AS) (11.7 mg/kg, n = 5 mice), LIPPCPO (100 mg/kg, n = 5 mice), or AS@LIPPCPO (111.7 mg/kg, n = 5 mice) thrice a week. B Tumor growth curves of each mouse. After receiving the indicated treatments, the tumor volumes of each mouse were recorded every 3 days and displayed as tumor growth kinetics. C Bioluminescence images of tumor-bearing mice. Animals receiving different treatments were subjected to bioluminescence imaging (BLI) using an IVIS imaging spectrum system at 0, 7, 14, 21, and 28 days. D Ex vivo imaging of pulmonary metastases. Tumor-bearing mice receiving different treatments were sacrificed on the 28th day for visualization of metastatic foci in the lungs. BF: bright field, BLI: bioluminescence imaging. E Kaplan–Meier curves displaying the survival rates of treated tumor-bearing mice over 60 days. Source data are provided as a Source Data file.
Moreover, we examined the effects of LIPPCPO on radiotherapy. Breast cancer-bearing mice were randomly divided into four groups and treated with saline, LIPPCPO (100 mg/kg), X-rays (6 Grays), or a combination of LIPPCPO and X-rays (Supplementary Fig. S25a). As shown in Supplementary Fig. S25b, c, the combination of LIPPCPO and X-rays exhibited the most potent inhibitory effect on tumor growth, with an average tumor volume of 197.8 mm³ on day 21. In contrast, animals receiving the vehicle solution, X-rays therapy alone, and LIPPCPO alone showed tumor volumes of 614.1 mm³, 419.4 mm³, and 313.6 mm³, respectively. These results indicate that LIPPCPO could potentially serve as a synergistic agent in both chemo- and radiotherapies.
Discussion
Acquired and intrinsic resistance to conventional cancer therapies remains a major obstacle in cancer treatment27. Despite numerous preclinical and clinical studies aimed at overcoming drug resistance, progress has been limited. Dysregulation of apoptosis is the primary mechanism responsible for refractory cancer, and activating non-apoptotic cell death pathways, such as ferroptosis, may provide a distinct therapeutic avenue28,29. Recent efforts have focused on exploring chemical inhibitors of ferroptosis brake axes, such as system xc−/GSH/GPX4 and vitamin B5/acetyl-CoA/HMG-CoA/CoQ10/FSP1, for cancer therapy12,30. However, conventional ferroptosis inducers, such as erastin, often lead to severe systemic toxicity19. Elevated iron deposition in cancer cells due to their rapid metabolism and proliferation makes the elevation of the labile iron pool a promising strategy for inducing ferroptosis for cancer therapy31. In this study, we designed a peroxide-functionalized liposome (LIPPCPO) to induce ferroptosis via the DMT1/Fe2+/LOOH axis for refractory cancer therapy. Our LIPPCPO targets DMT1 in lysosomes, facilitates the efflux of Fe2+ into the cytoplasm, and induces iron-dependent ferroptotic cell death. The ferroptosis induction mechanism of LIPPCPO differs from that of conventional ferroptosis inducers such as erastin and RSL3, which primarily target the core regulatory protein GPX4 within the braking axis of ferroptosis. In our study, LIPPCPO-treated cells showed a significant elevation in the labile iron pool and lipid peroxide accumulation due to direct interactions with DMT1. However, LIPPCPO induced a less pronounced decrease in GPX4 protein levels, suggesting that LIPPCPO may have a strong synergistic effect with ferroptosis inducers targeting the braking axis. Importantly, the unique ferroptosis mechanism of LIPPCPO allowed it to exhibit a higher killing effect on cancer cells than normal cells. Administering the LIPPCPO in vivo did not alter biochemical indexes in the blood, nor did it elicit any pathological changes in main organs, indicating a lower cytotoxicity in normal cells.
Iron metabolism is a tightly controlled process at both the cellular and systemic levels by a comprehensive signaling network32. In mammals, DMT1 is primarily responsible for dietary iron uptake on the plasma membranes of enterocytes in the gastrointestinal tract. After entering the bloodstream via ferroportin (FPN) and binding to transferrin receptors (TfRs), iron is taken into endosomes33. After reduction by six-transmembrane epithelial antigen of prostate (STEAP) families, the ferrous iron could be pumped out by lysosomal DMT1 to elevate the labile iron pool34. Although various inhibitors of TfRs or DMT1 have been discovered to prevent excess iron uptake for treating iron overload-related hereditary hemochromatosis35, there are currently no available activators of DMT1 or TfRs to enhance iron uptake. Interestingly, elevated iron deposition has been reported in Parkinson’s disease36, and a recent study demonstrated that NO-induced cysteinylation of DMT1 could enhance Fe2+ uptake in cells37. Inspired by this phenomenon, we designed peroxide-functionalized phospholipids to replace NO for DMT1 cysteinylation, which efficiently internalized into lysosomes. Lysosomal internalization facilitates the interactions between DMT1 and LIPPCPO. As expected, the LIPPCPO activates the efflux function of DMT1, elevates the labile iron pool, and induces ferroptosis. Taken together, our study discovered a synthetic material to boost the function of DMT1.
The chemical structure of phospholipids, including chain length, polar head group, and saturation status, significantly impacts the ferroptosis induced by LIPPO. It is noteworthy that the peroxide reaction on phospholipids often occurs at the 1,4-pentadiene units of the phospholipid chains. Therefore, the saturation status is particularly critical, as it determines the number of peroxide groups that can interact with DMT1. Our study demonstrates that only LIPPCPO derived from polyunsaturated phospholipids can induce ferroptotic cell death. This finding is consistent with a report by Stockwell’s group, which showed that phospholipids containing polyunsaturated fatty acyl tails, especially those with two such tails, significantly induce ferroptosis in cancer cells38. Furthermore, our data indicate that the type of polar head group in phospholipids is another crucial parameter. It affects interactions with cells and target molecules, modulating their efficacy in inducing ferroptosis. Among the three tested phospholipids: PC, DG, and PS, LIPPCPO exhibits the highest retention in cancer cell organoids and the strongest killing efficiency. However, the impacts of chain lengths on ferroptosis remain poorly understood. This is primarily due to the limited availability of commercially available phospholipids with the same polar heads and saturation status but different chain lengths, making comprehensive comparisons challenging. Therefore, future studies should explore the relationships between phospholipid structures and ferroptosis to identify potent ferroptosis inducers.
In summary, this study has demonstrated the potential of LIPPCPO to induce ferroptosis in cancer cells by elevating labile iron pool via DMT1 and inducing cellular events including accumulation of LOOH, GPX4 suppression, and GSH depletion. The activation of DMT1 could be attributed to LIPPCPO-induced cysteinylation at 245, 248, 334, and 365 sites of DMT1. The LIPPCPO was effective in inducing ferroptotic cell deaths in cancer cells, which resistant to conventional therapies such as chemo-, radio-, and targeted therapy. Furthermore, the AS@LIPPCPO formula displayed a strong synergistic ferroptosis effect, resulting in improved survival rates of breast cancer-bearing mice by inhibiting tumor growth and metastasis. Our study highlights a distinct approach to induce ferroptosis and provides a promising synthetic vector to enhance the therapeutic effects of conventional ferroptosis inducers.
Methods
Ethics statement
All animal experiments were performed in accordance with the guidelines approved by the Animal Care Committee of the Laboratory Animals at Soochow University (No. 202109A0130). The maximum tumor size permitted by the ethics committee/institutional review board is 2000 mm3. The tumor sizes in all experiments have never exceeded this threshold.
Material and reagents
Mini-extruder, 1,2-dilinoleoyl-sn-glycero-3-phosphocholine (PC, 18:2), and 1,2-dilinoleoyl-sn-glycero-3-phospho-L-serine (PS, 18:2) were purchased from Avanti Polar Lipids (Alabaster, Alabama, USA). Lipid peroxidation kit, C11-BODIPY (581/591), Fluorescein isothiocyanate (FITC), Hoechst 33342, RIPA lysate, Alexa Fluor 594-labeled wheat germ agglutinin (WGA) and DMT1 antibody (PA5-35136) were obtained from Thermo Fisher Scientific (Grand Island, NY, USA). Cisplatin, Dacarbazine, Vemurafenib, Sorafenib, and Genfitinib were obtained from MedChemExpress (Monmouth Junction, New Jersey, USA). Doxorubicin hydrochloride was purchased from Aladdin (Shanghai, China). Ferrostatin-1, Polybrene, and Puromycin were purchased from Sigma-Aldrich (St. Louis, Mo, USA). TNF-α was obtained from BD biosciences (San Jose, CA, USA). Deferiprone (DFP), Deferoxamine (DFO), and 1,3-dilinoelaidoyl glycerol (DG, 18:2) were purchased from Cayman Chemical (Ann Arbor, MI, USA). CHX, Z-VAD-FMK, Nec-1, GPX4 (ab125066), LAMP-1 (ab278043), RIP3 (ab62344) and β-actin (ab8227) antibody were obtained from Abcam (Cambridge, MA, USA). 4-HNE (MA5-27570) antibody was purchased from Invitrogen (CA, USA). A cleaved Caspase-3 (bs-2593R) antibody was purchased from Bioss Inc. (Boston, USA). Lentiviral vectors were obtained from GenePharma Co., Ltd. (Shanghai, China). Fetal bovine serum (FBS) was obtained from Gibco (Gemini, Woodland, USA). RPMI 1640 medium and Dulbecco’s modified Eagle’s medium (DMEM) were purchased from Corning (NY, USA). Penicillin, Streptomycin, and Trypsin-EDTA were purchased from HyClone Laboratory (South Logan, Utah, USA).
Molecular dynamics simulation
Molecular dynamics simulation was used to explore the interactions between DMT1 protein and PC derivatives including pristine PC, carboxylic PC, hydroxyl PC, and peroxide PC. Specifically, we used Autodock Vina 1.1.2 to dock PC derivatives and DMT1 protein at an exhaustiveness value of 100. After a 50 ns simulation, we calculated the relative binding free energy of PC derivatives and DMT1 protein using MM-PBSA/GBSA methods.
Preparation, separation, and characterization of lipid peroxides
To create a phospholipid monolayer, PC, PS, or DG dissolved in chloroform at 600 μM were added to a 5 mL round-bottom flask. The solvents were removed by a rotary evaporator for 10 min at 25 °C, 80 rpm, and 400 mbar. The resulting phospholipid monolayers were reacted with O2 in 1 mL PBS or RPMI 1640 media containing 105 units of lipoxygenase type-V (5-LOX) for 4 h at 37 °C. After sonication for 30 s, the supernatants containing lipid peroxides were centrifuged (Allegra 64R, Beckman) at 20,000 × g for 10 min to collect the supernatants. The organic layers were extracted three times with 4 mL CHCl3, concentrated by a vacuum centrifugal concentrator (CentriVap 7810040, Labconco), and stored at −80 °C for further analysis.
The phospholipid peroxide extracts were analyzed using an LC system (Agilent 1100 Series, Santa Clara, CA, USA) coupled with an LTQXL mass spectrometer (Thermo Fisher Scientific, Waltham, MA, USA) with an electrospray ionization (ESI) source. Injection samples of 3 μL were separated by an Xqua C8 column (55 °C) at a flow rate of 0.25 mL/min with a gradient of 5–95% mobile phase B in 20 min. The eluent was scanned by an MS in positive ionization mode with the capillary temperature at 350 °C, source current at 4 μA, source voltage at 3.5 kV, sheath gas flow rate at 25 arb, aux gas flow rate at 8 arb, voltage of tube lens at 120 V, and m/z of isolation width at 1.5. The scan ranges were 100–1000 m/z. The MS data were collected and analyzed by Xcalibur software (Thermo Xcalibur 2.2). To obtain pure phospholipid peroxides, the extracts were separated by high-performance liquid chromatography (HPLC). The mobile phase A was 60% acetonitrile in water, and the mobile phase B was acetonitrile/isopropanol (10/90, v/v), containing 10 mM ammonium formate. Injection sample volumes of 5 μL were separated by an Xqua C8 column (2.1 mm × 100 mm, 3.5 μm, 100 Å) at a flow rate of 0.25 mL/min with a gradient of 5–95% mobile phase B in 30 min. The eluent at 13–21 min was collected per min and concentrated by a vacuum centrifugal concentrator for 2 h. The concentrated samples were further characterized by LC-MS analysis, as reported previously34.
Construction and characterization of LIPPO
To construct the LIPPO samples, we used a thin-film hydration method followed by extrusion. We mixed PC, PS or DG with their peroxides in different mass ratios (100%, 90%, 80%, 60%, 40%, 20%, and 0%) and dissolved 200 μM of the resulting phospholipid mixtures in chloroform. A single lipid molecular thin film was formed in a round-bottom flask using rotary evaporation (25 °C) and hydrated it with 1 mL of DI water or RPMI 1640 media. After sonication (40 W) for 30 s in a water bath, we obtained heterogeneous LIPPO. The uniform liposomes were acquired by extruding the heterogeneous LIPPO with an Avanti extruder equipped with 0.1 μm polycarbonate membranes. The acquired LIPPO was characterized using dynamic light scattering (Zetasizer Nano ZS90, Malvern) and cryo-electron microscopy (Talos F200C 200 kV, FEI).
Encapsulation of drug molecules into LIPPCPO
To encapsulate drug molecules into the LIPPCPO, we dissolved sulfasalazine, atorvastatin, artesunate, or altretamine in DMSO at 200 μM and added them into 500 μL of chloroform containing 120 μM of PC and 80 μM of PC peroxides. We evaporated the solvents using a rotary evaporator (120 rpm) at room temperature to obtain a film in a round-bottom flask, which we then hydrated with 1 mL of DI water. After sonication (40 W) for 30 s in a water bath and extrusion by an Avanti extruder equipped with 0.1 μm polycarbonate membranes, we removed the free hydrophobic drugs by centrifugation at 20,000 × g for 10 min to obtain liposome formulas encapsulating the drugs. The liposome formulas encapsulating drugs were then lyophilized using a vacuum centrifugal concentrator and dissolved in DMSO or methanol for UV-Vis spectroscopy detection. The encapsulation efficiency (EE) was calculated using the following equation:
where CL and CT are the concentrations of hydrophobic drugs loaded in liposome formulas and the total concentrations of drugs used for liposome formula encapsulation, respectively35.
Preparation of FITC-LIPPCPO and 125I-LIPPCPO
FITC-labeled PC was synthesized by covalent conjugation of FITC to PC. Briefly, 10 mg of 1,2-dioleoyl-sn-glycerol and 0.238 mg of 4-Dimethylaminopyridine (DMAP) were dissolved in 2 mL anhydrous toluene and placed in a 25 mL three-neck round-bottom flask with magnetic stirring under N2. The flask was placed in an ice bath and 200 μL of 2-chloro-1,3,dioxaphospholane-2-oxide toluene (41.5 mg/mL) was added via a 1 mL syringe. Then, 100 μL of triethylamine (TEA) toluene (37 mg/mL) was added dropwise, and the reaction mixture was stirred for 4 h at room temperature. After that, 200 μL of N-Boc-N,N′-dimethyl ethylenediamine acetonitrile at 3.68 mg/mL was added to the flask, and the mixture was reacted for 4 h at 65 °C. The pellet products were collected by rotary evaporation (100 rpm) at room temperature to remove the solvents, and washed thrice with 0.5 mL hexyl hydride to remove TEA. The BOC deprotection of the products was achieved by adding 1 mL CF3COOH and 1 mL CH2Cl2 and reacted at room temperature for 3 h. The deprotected products were acquired by rotary evaporation to remove solvents and washed thrice with 1 mL CH2Cl2. The products were reacted with 2 mL FITC methanol (3.75 mg/mL, pH 8∼9) for 6 h at room temperature. The crude FITC-PC products were obtained by rotary evaporation to remove solvents, washed thrice with 1 mL DI water and 1 mL CH2Cl2, and finally dissolved in 1 mL tetrahydrofuran. The crude FITC-PC tetrahydrofuran samples were purified by a C8 SPE column that was pretreated with 1 mL methanol and 1 mL DI water and eluted with 30 mL DI water, 30 mL methanol, and 15 mL isopropanol. The purified FITC-PC isopropanol eluents were concentrated using a vacuum centrifugal concentrator.
125I-labeled 4-tetradecylphenol was synthesized by electrophilic substitution reaction between the adjacent hydrogen of phenol moiety on 4-tetradecylphenol and iodine cation. Specifically, 1 mg of 1,3,4,6-tetrachloro-3α,6α-diphenylglycouril dissolved in 1 mL of trichloromethane was added to a 5 mL flask. The solvents were evaporated by a rotary evaporator (120 rpm) at room temperature to obtain a film in the round-bottom flask. Then, 200 μL of 4-tetradecylphenol acetonitrile solution (5 mg/mL) was added to the flask, and the solvents were removed to form a film in the flask with a rotary evaporator (120 rpm) at room temperature. A total of 500 μCi Na125I dispersed in 100 μL of KOH-H3PO4 buffer (0.1 M, pH 7) was added to the flask at a flow rate of 10 μL per 3 min for 30 min. After that, 25 μL acetonitrile was thoroughly mixed with the reaction solution. The supernatant samples were collected by centrifugation at 15,000 × g for 10 min, and purified by a SPE column pretreated with 3 mL anhydrous methanol and 3 mL DI water. The 125I-labeled 4-tetradecylphenol was collected after 3 mL acetonitrile washing and dried at 60 °C. The FITC-PC and 125I-labeled 4-tetradecylphenol were added in the construction process of LIPPCPO with a mass ratio of 1:9 to acquire FITC-LIPPCPO and 125I-LIPPCPO.
Cell culture
Breast cancer cell lines MCF-7 (Cat: CBP61090) and 4T1 (Cat: CBP60352), lung cancer cell line A549 (Cat: CBP60084), melanoma cell lines A375 (Cat: CBP60329) and B16 (Cat: CBP60334), hepatoma cell line HepG2 (Cat: CBP60199) were purchased from Cell Bank Type Culture Collection (CAS, Shanghai, China). LLC cells were kindly donated by Dr. Sijin Liu (Shandong First Medical University). Liver, lung and skin normal cells were extracted from mouse tissues. All cells were cultured in RPMI 1640 or DMEM medium supplemented with 10% FBS and 1% penicillin/streptomycin at 37 °C with a humidified atmosphere of 5% CO2. Drug-resistant cell lines were established according to a reported method with a few modifications39. Dacarbazine (0–1500 µM), doxorubicin (0–2 μg/mL) and cisplatin (0–10 μg/mL), vemurafenib (0–100 µM), sorafenib (0–20 µM) and genfitinib (0–40 µM) were used to treat cancer cells at stepwise changed concentrations. After 2–4 months treatment, eight resistant cell lines were acquired, including A375-R1 (dacarbazine, DTIC), B16-R1 (dacarbazine, DTIC), 4T1-R (doxorubicin, DOX), A549-R1 (cisplatin, DDP), LLC-R1 (cisplatin, DDP), B16-R2 (vemurafenib, Vem), HepG2-R1 (sorafenib, SOR) and LLC-R2 (genfitinib, Gef). Radiation-resistant cells (B16-R3, 4T1-R1) were established by exposure of the parent cells to 5–10 Grays of X-rays per week for 10–20 weeks. Doxorubicin-resistant MCF-7 cells (MCF-7R) were kindly donated by Dr. Xiangshen Liu (Institute of Cancer and Basic Medicine, Chinese Academy of Sciences). Supplementary Table S8 justified the specific treatments for each cell.
Accumulation of lipid peroxidation induced by LIPPCPO in cells
Aliquots of 100 μL MCF-7R (5 × 103 cells/well) suspensions were added to each well of 96-well plates and cultured at 37 °C overnight. The supernatants were then replaced with 100 μL RPMI 1640 media containing 0–100 μM of LIPPCPO for 12 h. Meanwhile, the same amounts of LIPPCPO were added into 1.5 wt% sodium alginate solutions to prepare calcium alginate microspheres using an electrostatic droplet generator5. Aliquots of 100 μL microsphere suspensions were also added to each well of 96-well plates (5 × 103/well) and cultured at 37 °C. To detect the accumulation of lipid peroxides in cells, the treated cells and microspheres were washed with PBS and stained with 10 μM C11-BODIPY (581/591) reagent for 1 h. After washing thrice with PBS, the stained cells and microspheres were analyzed using a high-content imaging system. The lipid peroxide accumulation in cells was assessed using the following formula:
Where FTG and FTR represent the fluorescence of BODIPY C11 at green and red channels, respectively, emitted from cells exposed to LIPPCPO; FBG and FBR are the fluorescence of BODIPY C11 at the green and red channels, respectively, emitted from the gel spheres containing LIPPCPO.
Cell transfection
MCF-7R cells were seeded in 24-well plates at a density of 2 × 105 cells per well and cultured overnight. Lentiviral vector transfection reagent complexes were prepared in RPMI 1640 media containing DMT1-small hairpin RNA (shRNA) lentivirus or non-targeting vector-control shRNA lentivirus, and polybrene (5 μg/mL) transfecting agent. The complexes were then added to the cells and incubated for 48 h. Subsequently, the cells were replaced with fresh RPMI 1640 media containing puromycin (20 µg/mL) to select a population of resistant cells. The stably transfected cells were isolated by sorting GFP and were denoted as DMT1-KD MCF-7R. The sequence of DMT1 shRNA was 5′-GCTTTCTCATCACTATTATGG-3′, and the control shRNA coding sequence was 5′-TTCTCCGAACGTGTCACGT-3′.
Construction of cancer cell spheroids
4T1-R cells (1 × 106 cells) were mixed with 1 mL of 1.5% (w/v) sodium alginate dissolved in 0.9% sodium chloride solution. The microspheres encapsulating 4T1-R cells were prepared by injecting the mixture into a gelling bath of 100 μM calcium chloride solution at a flow velocity of 8.2 mL/h through a 0.5 mm needle, under the assistance of an electrostatic field produced by a Tissue/Cell Microsphere Fabrication System (Bio-leader Incorporation, Ganzhou, Jiangxi, China), with a voltage of 4.5 kV37. After gelling for 30 min, the microspheres were collected by natural sedimentation and cultured in RPMI 1640 media. Mature cancer cell spheroids were obtained after 5–7 days of culture once the size of cell agglomerates in each microsphere was >50 μm.
Cell viability test
MCF-7R (5 × 103 cells/well), 4T1-R (4 × 103 cells/well), other resistant cancer cells (5 × 103 cells/well), or mature cell spheroids (500/well) were incubated in 96-well plates overnight at 37 °C. Subsequently, the cell media were replaced with 100 μL fresh media containing 0–5 mM dacarbazine, 0–100 μM doxorubicin, 0–200 μg/mL cisplatin, 0–500 µM vemurafenib, 0–100 µM sorafenib, and 0–100 µM genfitinib, 0–200 µM liposomes (DG, PC, or PS), LIPPCPO, LIPDGPO, or LIPPSPO. After 24–72 h of incubation at 37 °C, the supernatants in each well were removed and replaced with 120 μL of 5 mg/mL MTS working solution in phenol red-free media. After incubating for 2 h at 37 °C, 100 μL of the cultured supernatants were transferred into a new plate to read absorbance at 490 nm using a microplate reader. Cell viability was calculated using Eq. 3:
where At, Ac, and Ab were the absorbance of MTS substrate at 490 nm in treated, untreated, and blank samples, respectively.
Acquired resistance evolution test
Evolution tests were performed to determine the effects of DTX and LIPPCPO on 4T1-R cells by sequential exposure of cells to 0.25 × IC50 for 60 days7. Briefly, aliquots of 4T1-R cell suspensions (1 × 105) were added to each well of 6-well plates (2 mL/well) or 24-well plates (0.5 mL/well) and incubated at 37 °C for 24 h. The cells were then exposed to 0.25 × IC50 of DTX and LIPPCPO. After 24 h, the cell density was assessed using an inverted microscope (Olympus, CKX53, Tokyo, Japan). When the cells adapted to the tested concentrations and showed >80% cell confluence, the exposure dose of DTX or LIPPCPO was increased. Otherwise, the exposure concentration was sustained for another 24 h. After 60-day exposure, the evolved cells were obtained Details for culture conditions, the container, culture media, cell density, and LIPPCPO/DTX doses used each day are listed in Supplementary Table S9.
Perl’s staining
Aliquots of MCF-7R suspensions (5 × 105 cells/well) were added to each well of six-well plates and cultured at 37 °C for 24 h. Then, the supernatants were replaced with fresh RPMI 1640 media (2 mL) or RPMI 1640 media containing 100 μM of LIPPCPO. After 12 h of culture, the cells were washed with PBS and fixed with 4% paraformaldehyde (2 mL) for 20 min. Then, the cells were washed with DI water (2 mL) and stained with Perl’s staining solution following the specific protocol. The stained cells were imaged by a microscope (Olympus, CX41, Tokyo, Japan).
ICP-OES detection
To quantify iron contents, aliquots of 2 mL MCF-7R suspensions were added to six-well plates at 5 × 105 cells/well and incubated overnight at 37 °C. The supernatants were then replaced with 2 mL fresh RPMI 1640 media or 2 mL RPMI 1640 media containing 100 μM of LIPPCPO for MCF-7R cells. After culturing for 12 h, the cells were washed with 2 mL PBS. The fresh tumor samples (∼50 mg) were weighed and washed with ice-cold PBS to remove any residual blood or debris and cut into small pieces with a sterile scissor. Both the cell and tumor samples were homogenized in 1 mL ice-cold RIPA buffer for freezing and thawing. The lysates were centrifuged at 20,000 × g for 10 min at 4 °C to remove the insoluble debris and collect supernatants. The protein concentrations in supernatants were detected by a BCA protein assay kit according to the manufacturer’s instructions. After that, the lysates were placed in a 25 mL flask and incubated with a 5 mL digested solution consisting of 10 M H2O2 and 14.4 M HNO3 for 12 h at room temperature. The samples were then digested at 300 °C for 4 h using a heater (Lichen, Shanghai, China) with continuous addition of DI H2O. The supernatants of digested solutions were collected by centrifugation at 10,000 × g for 10 min and subjected to ICP-OES (Thermo Fisher, ICAP 7200) analysis. Fe standard solutions were also detected to acquire a standard curve.
Confocal microscopy imaging
Confocal microscopy imaging was used to visualize the distribution of Fe2+, lipid oxide, and FITC-labeled liposomes in cells or cell spheroids. Aliquots of 200 μL MCF-7R (2 × 105 cells/well), DMT1-KD MCF-7R (2 × 105 cells/well), 4T1-R (1.5 × 105 cells/well), or mature 4T1-R cell spheroid (1 × 103 spheroids/well) suspensions were added to each well of eight-well chambers (155411, Lab-Tek, USA) and cultured at 37 °C overnight. The supernatants were then replaced with 200 μL RPMI 1640 media containing either 100 μM of FITC-LIPPO for MCF-7R cells and 4T1-R cell spheroids, 100 μM of LIPPCPO for MCF-7R cells, or 150 μM of LIPPCPO for 4T1-R cells.
To assess the distribution of Fe2+ in cells, LIPPCPO-treated MCF-7R cells were incubated for 12 h, washed with PBS, and stained with 10 μg/mL Hoechst 33342 for 20 min and FeRhoNox-1 (10 μg/mL) for 1 h. After washing thrice with PBS, the stained cells were imaged using confocal microscopy (FV1200, Olympus, Japan) with a 60× oil immersion objective lens at 405 nm or 559 nm excitation. Positive controls were cells treated with 100 μM Fe(NH4)2(SO4)2.
To assess the accumulation of lipid peroxides in cells, LIPPCPO-treated MCF-7R or 4T1-R cells were incubated for 12 h, washed with PBS, and stained with 10 μg/mL Hoechst 33342 for 20 min and C11-BODIPY (581/591) (10 μM) reagent for 1 h. After washing thrice with PBS, the stained cells were imaged using confocal microscopy with a 20× objective lens at 405 nm, 488 nm, or 559 nm excitation. Positive controls were cells treated with 25 μM RSL3.
To detect the localization of FITC-liposomes inside cells or cell spheroids, we incubated MCF-7R cells or 4T1-R cell spheroids treated with FITC-LIPPCPO for 2-12 or 72 h. The cells were then washed with PBS and stained with Hoechst 33342 (10 μg/mL) for 20 min and Alexa Fluor 594-labeled wheat germ agglutinin (WGA) (20 μg/mL) for 1 h, or anti-LAMP-1 antibody (1:100, Abcam, ab278043) for 12 h, following the manufacturer’s protocol. After washing thrice with PBS, we imaged the stained cells using a confocal microscope with a 4× or 60× oil immersion objective lens, with excitation at 405 nm, 488 nm, or 559 nm.
To visualize the interaction of FITC-liposomes with DMT1 protein in cells, we incubated MCF-7R cells treated with FITC-LIPPCPO for 12 h. Then the cells were washed with PBS and fixed in 4% paraformaldehyde, followed by 15 min treatment in 0.05% Triton X-100 for membrane permeabilization. The fixed cells were incubated with anti-DMT1 antibody (1:100, Abcam, ab62562) for 12 h, following the manufacturer’s protocol. After washing thrice with PBS, we stained the cells with Hoechst 33342 (10 μg/mL) for 20 min and a second fluorescence antibody Alexa Fluor 594 (20 μg/mL). After five-time washing by PBS, the stained cells were visualized with a 60× oil immersion objective lens, with excitation at 405 nm, 488 nm, or 559 nm.
GSH assay
MCF-7R and 4T1-R cells (5 × 105 cells/well) were inoculated in 6-well plates and incubated overnight at 37 °C. The cell media in each well was replaced with 2 mL fresh RPMI 1640 media containing 25 μM RSL3 or 100–150 μM LIPPCPO. After 12 h of incubation, the GSH contents in the cells were detected using a GSH/GSSG Assay kit following the manufacturer’s protocol.
Western blotting assay
MCF-7R and 4T1-R cells (5 × 105 cells/well) were inoculated in 6-well plates and incubated overnight at 37 °C. The cells were then treated with 2 mL aliquots of fresh RPMI 1640 media containing 25 μM RSL3 or 100–150 μM LIPPCPO for 12 h. Breast cancer samples that had received different treatments were collected on the 10th day post-injection and ground in liquid nitrogen. The treated cells and tumor samples were lysed in RIPA buffer containing 5% protease (Cat: P5147, Sigma) and 2% cocktail phosphatase (Cat: P5726, Sigma) inhibitors. The supernatants from the protein lysates were centrifuged at 14,000 × g for 10 min to remove cell debris. The protein concentrations in the supernatants were measured and adjusted using the Bradford assay. The protein samples were separated by loading onto a 12% SDS-PAGE gel (Beyotime, Shanghai, China) using a Mini-PROTEAN Tetra System (Bio-Rad, CA, USA) at 100 V in tris-glycine-SDS buffer. The separated proteins were then transferred to a nitrocellulose membrane at 300 mA. The membranes were washed three times with 0.1% Tween 20/TBS (v/v, TBST), blocked with 5% (w/v) milk (Biofrox, Einhausen, Germany) in TBST solution at room temperature for 2 h, and then incubated with β-actin (1:1000) and GPX4 (1:500) antibodies in the blocking buffer for 16 h at 4 °C. After washing the membranes with TBST solution three times, they were incubated with an HRP-conjugated secondary antibody (1:1000) at room temperature for 2 h, followed by sufficient washing with TBST. The membranes were stained using an ECL hypersensitive chemiluminescence solution, and detected under a fluorescence chemiluminescence imaging system (FluorChem M, Alpha, USA).
Animal treatment
Female Balb/c mice (6–8 weeks old) were obtained from Cavens Biological Technology (Changzhou, Jiangsu, China) and housed in an animal facility under controlled conditions of 60% relative humidity, filtered air, 12-h light/12-h dark cycle, acidified water, autoclaved food, and wood shaving for bedding. The mice were anesthetized using intraperitoneal injection of sodium pentobarbital (40 mg/kg) before 4T1-R cells suspended in 80 μL PBS at 5 × 105 cells were injected into the 4th mammary fat pads of each mouse. Tumor volumes were measured using a digital caliper and calculated using the formula 4:
When the tumor size reached ∼50 mm3, the qualified mice were randomly divided into three groups by throwing dice for subsequent treatments, including intravenous injection of 100 μL saline (n = 8), DTX (36 mg/kg, n = 3), X-rays (6 Grays, n = 5), LIPPCPO (100 mg/kg, n = 8), or LIPPCPO + X-rays (100 mg/kg + 6 Gray, n = 5) thrice a week. The mice were sacrificed on the 10th day to collect tumor samples in Ctrl, DTX, and LIPPCPO for ferroptosis biomarker examination. The tumor sections were stained with antibodies against 4-HNE (1:50), cleaved caspase-3 (1:200), and RPI3 (1:200) and imaged using a microscope (Olympus, CX41, Tokyo, Japan). The tumor size, body weight, and survival rate of animals in Ctrl (n = 5), X-rays (n = 5), LIPPCPO (n = 5), and LIPPCPO + X-rays were recorded.
When the tumor size reached ∼150 mm3, the qualified mice were randomly divided into four groups by throwing dice for the following treatments, including intravenous injection of 100 μL saline (Control, n = 5), artesunate (11.7 mg/kg, n = 5), LIPPCPO (100 mg/kg, n = 5), or artesunate@LIPPCPO (111.7 mg/kg, n = 5) thrice a week. The tumor sizes were recorded every 3 days. Humane endpoints were applied to the tumor-bearing mice once they met one of the following criteria: (i) tumor volume ∼2000 mm3 or (ii) severe effects on eating, drinking, or movement. The mice and ex vivo lung tissues were imaged using a Canon camera (Japan) and an IVIS imaging spectrum system (PerkinElmer, ME, USA).
In vivo biosafety assessment
Healthy female BALB/c mice aged 6–8 weeks were randomly assigned to two groups. The mice were intravenously injected with either 100 μL of saline or LIPPCPO (20 mg/mL) via the tail vein. After administration, the mice’s appearance and behavior were monitored periodically for 3 days. Blood and organs (heart, liver, lung, kidney, brain, and spleen) were collected from the treated mice for biosafety testing. Blood samples (∼600 μL) from each mouse were analyzed to measure routine blood indicators using a Mindray BC-2800Vet hematology analyzer (Mindray Global, China).
Mass spectrometry analysis
A total of 12 protein samples were analyzed using mass spectrometry, including 3 LIPPCPO-treated DMT1 gel band samples, 3 DMT1 control samples, and 6 serum samples from tumor-bearing and healthy mice. The serum samples were initially centrifuged at 40,000 × g for 1 h to remove subcellular organelles such as exosomes and microsomes. LIPPCPO was then dispersed in 400 μL of mouse serum samples at a concentration of 1 mg/mL. After incubating for 1 h at 37 °C and 200 rpm, the LIPPCPO were retrieved by ultracentrifugation at 40,000 × g for 1 h, followed by a gentle rinse in PBS. The collected LIPPCPO were then subjected to protein extraction, digestion, and analysis of protein constituents in surface coronas, based on an established proteomics method40. The DMT1 gel samples were cut into 1 mm³ pieces and incubated with 300 µL acetonitrile (ACN) for 5 min with shaking. After lyophilization, the samples were incubated with NaHCO₃ solution (80 µL, 50 mM) containing 2 µg trypsin at 37 °C for 12 h. The digested peptide samples were dissolved in 100 µL of 10% ACN containing 0.1% formic acid (FA) and analyzed using an Easy nLC1200/Q Exactive+ mass spectrometer (Thermo Fisher Scientific, USA). Separation was performed on a C18 column (0.15 mm × 150 mm, Column Technology Inc.) with 0.1% FA in H₂O as mobile phase A and 0.1% FA in ACN-H₂O (v/v, 84/16) as mobile phase B. The mobile phase flow rate was set at 300 nL/min, with a gradient of 4% B to 50% B over 50 min, followed by 50% B to 100% B over 4 min, and holding at 100% B for 6 min. Mass spectrometry detection settings were as follows: spray voltage at 2.1 kV, capillary temperature at 275 °C, mass range of 300–2000 m/z for MS, and 200–2000 m/z for MS/MS. The raw mass spectrometry data were processed using Proteome Discoverer version 2.4 (Thermo Fisher Scientific, USA) and searched against the UniProt human protein database (uniprotkb_Mus_musculus_55086_2023_12_19) using Mascot version 1.5.5.1 (Matrix Science, London, UK). The database search parameters were: Enzyme: Trypsin, with a maximum of 2 missed cleavages; Precursor Mass Tolerance: ±20 ppm; Fragment Mass Tolerance: ±0.1 Da; False Discovery Rate (FDR) <1%.
Statistical analysis
All animals were randomly assigned to each group using a randomization method by throwing dice. Each experiment was repeated at least three times, and no data were excluded. The results are presented as the mean ± standard deviation (SD) of at least three replicates. The two-tailed Student’s t-test was used to analyze the data, and differences among groups were considered significant if p < 0.05.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
Data supporting this manuscript is available in Harvard Dataverse (https://doi.org/10.7910/DVN/Q7RHE7). Source data are provided with this paper.
References
Stockwell, B. R. et al. Ferroptosis: a regulated cell death nexus linking metabolism, redox biology, and disease. Cell 171, 273–285 (2017).
Yang, W. S. & Stockwell, B. R. Ferroptosis: death by lipid peroxidation. Trends Cell Biol. 26, 165–176 (2016).
Zheng, H. Z. et al. Nanoparticle-induced ferroptosis: detection methods, mechanisms and applications. Nanoscale 13, 2266–2285 (2021).
Lei, G., Zhuang, L. & Gan, B. Targeting ferroptosis as a vulnerability in cancer. Nat. Rev. Cancer 22, 381–396 (2022).
Wang, W. et al. Engineering micro oxygen factories to slow tumour progression via hyperoxic microenvironments. Nat. Commun. 13, 4495 (2022).
Shiao, S. L. et al. Commensal bacteria and fungi differentially regulate tumor responses to radiation therapy. Cancer Cell. 39, 1202–1213 (2021).
Viswanathan, V. S. et al. Dependency of a therapy-resistant state of cancer cells on a lipid peroxidase pathway. Nature 547, 453–457 (2017).
Wang, W. et al. CD8(+) T cells regulate tumour ferroptosis during cancer immunotherapy. Nature 569, 270–274 (2019).
Hangauer, M. J. et al. Drug-tolerant persister cancer cells are vulnerable to GPX4 inhibition. Nature 551, 247–250 (2017).
Dixon, S. J. et al. Ferroptosis: an iron-dependent form of nonapoptotic cell death. Cell 149, 1060–1072 (2012).
Welsh, J. et al. Pembrolizumab with or without radiation therapy for metastatic non-small cell: a randomized phase I/II trial. J. Immunother. Cancer 8, e001001 (2020).
Yang, L. L., Cai, X. M. & Li, R. B. Ferroptosis induced by pollutants: an emerging mechanism in environmental toxicology. Environ. Sci. Technol. 58, 2166–2184 (2024).
Ingold, I. et al. Selenium utilization by GPX4 is required to prevent hydroperoxide-induced ferroptosis. Cell 172, 409–422 (2018).
Doll, S. et al. FSP1 is a glutathione-independent ferroptosis suppressor. Nature 575, 693–698 (2019).
Koppula, P. et al. A targetable CoQ-FSP1 axis drives ferroptosis- and radiation-resistance in KEAP1. Nat. Commun. 13, 2206 (2022).
Twyman-Saint Victor, C. et al. Radiation and dual checkpoint blockade activate non-redundant immune mechanisms in cancer. Nature 520, 373–377 (2015).
El-Khoueiry, A. B. et al. Nivolumab in patients with advanced hepatocellular carcinoma (CheckMate 040): an open-label, non-comparative, phase 1/2 dose escalation and expansion trial. Lancet 389, 2492–2502 (2017).
Tang, W. et al. The mechanisms of sorafenib resistance in hepatocellular carcinoma: theoretical: theoretical basis and therapeutic aspects. Signal Transduct. Target. Ther. 5, 87 (2020).
Zhao, J., Xu, B., Xiong, Q., Feng, Y. & Du, H. Erastin-induced ferroptosis causes physiological and pathological changes in healthy tissues of mice. Mol. Med. Rep. 24, 713 (2021).
Brackett, C. M. et al. Toll-like receptor-5 agonist, entolimod, suppresses metastasis and induces immunity by stimulating an NK-dendritic-CD8+ T-cell axis. Proc. Natl Acad. Sci. USA 113, E874–E883 (2016).
Apisarnthanarax, S. et al. External beam radiation therapy for primary liver cancers: an ASTRO clinical practice guideline. Pract. Radiat. Oncol. 12, 28–51 (2022).
Halcrow, P. W. et al. HIV-1 gp120-induced endolysosome de-acidification leads to efflux of endolysosome iron, and increases in mitochondrial iron and reactive oxygen species. J. Neuroimmune Pharmacol. 17, 181–194 (2022).
Hara, K. et al. Radiotherapy for hepatocellular carcinoma results in comparable survival to radiofrequency ablation: a propensity score analysis. Hepatology 69, 2533–2545 (2019).
Xu, S. et al. Vacancies on 2D transition metal dichalcogenides elicit ferroptotic cell death. Nat. Commun. 11, 3484 (2020).
Garcia-Martinez, L., Zhang, Y., Nakata, Y., Chan, H. L. & Morey, L. Epigenetic mechanisms in breast cancer therapy and resistance. Nat. Commun. 12, 1786 (2021).
Parikh, A. R. et al. Radiation therapy enhances immunotherapy response in microsatellite stable colorectal and pancreatic adenocarcinoma in a phase II trial. Nat. Cancer 2, 1124–1135 (2021).
Jarosz-Biej, M. et al. Brachytherapy in a single dose of 10Gy as an “in situ” vaccination. Int J. Mol. Sci. 21, 4585 (2020).
Chen, B. et al. Application of radiotherapy before or during immunotherapy to enhance its efficacy in metastatic and recurrent liver cancer: a pilot study from the real-world data. J. Clin. Oncol. 39, e16195–e16195 (2021).
Jiang, J. et al. Nano-enabled photosynthesis in tumours to activate lipid peroxidation for overcoming cancer resistances. Biomaterials 285, 121561 (2022).
Jiang, X. J. et al. Ferroptosis: mechanisms, biology and role in disease. Nat. Rev. Mol. Cell Biol. 22, 266–282 (2021).
Yin, M. M., Liu, Y. P. & Chen, Y. Iron metabolism: an emerging therapeutic target underlying the anti-cancer effect. Free Radic. Res. 55, 296–303 (2021).
Zhang, Z. F., Liu, X., Chen, D. W. & Yu, J. M. Radiotherapy combined with immunotherapy: the dawn of cancer treatment. Signal Transduct. Target. Ther. 7, 258 (2022).
Wang, X. Y. et al. Oral administration of ginger-derived lipid nanoparticles and Dmt1 siRNA potentiates the effect of dietary iron restriction and mitigates pre-existing iron overload in Hamp KO mice. Nutrients 13, 1686 (2021).
Meng, F. J. et al. Lysosomal iron recycling in mouse macrophages is dependent upon both LcytB and Steap3 reductases. Blood Adv. 6, 1692–1707 (2022).
Crielaard, B. J., Lammers, T. & Rivella, S. Targeting iron metabolism in drug discovery and delivery. Nat. Rev. Drug Discov. 16, 400–423 (2017).
Thomas, G. E. C. et al. Regional brain iron and gene expression provide insights into neurodegeneration in Parkinson’s disease. Brain 144, 1787–1798 (2021).
Cui, W. Q. et al. Discovering anti-cancer drugs via computational methods. Front. Pharmacol. 11, 733 (2020).
Qiu, B. Y. et al. Phospholipids with two polyunsaturated fatty acyl tails promote ferroptosis. Cell 187, 1177–1190 (2024).
Gu, L., Zhang, G. & Zhang, Y. L. A novel method to establish glucocorticoid resistant acute lymphoblastic leukemia cell lines. J. Exp. Clin. Cancer Res. 38, 269 (2019).
Cai, X. M. et al. Multi-hierarchical profiling the structure-activity relationships of engineered nanomaterials at nano-bio interfaces. Nat. Commun. 9, 4416 (2018).
Acknowledgements
This work was supported by the National Key R&D Program of China (X.C. 2022YFE0124000, R.L. 2020YFA0710700), the National Natural Science of Foundation of China (R.L. No.21976126), and the Natural Science Foundation of Jiangsu Province (R.L. BK20211545).
Author information
Authors and Affiliations
Contributions
R.L. and S.L. conceptualized the project and designed the experiments. Jun Jiang and L.Y. designed and performed most experiments. Q.X. constructed the liposomes. X.L. constructed the 125I-labeled liposomes and detected the distribution of 125I-labeled liposomes in vivo. J.Z. and S.Z. contributed to the iron detection. Jie Jiang conducted the GSH detection experiments. H.Z. constructed the cell organoids. W.L. extracted the cells from tissues. X.C. performed the LC-MS experiments. The writing of the manuscript was led by R.L. with the participation from Jun Jiang.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks Morteza Mahmoudi and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Jiang, J., Yang, L., Xie, Q. et al. Synthetic vectors for activating the driving axis of ferroptosis. Nat Commun 15, 7923 (2024). https://doi.org/10.1038/s41467-024-52312-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-024-52312-7