Abstract
Different forms of phosphorylated tau (p-tau) have shown strong potential as Alzheimer’s disease (AD) biomarkers in both cerebrospinal fluid (CSF) and plasma. We hypothesized that p-tau proteoforms simultaneously phosphorylated at two different sites may have an increased diagnostic value compared with tau phosphorylated at a single site. Here, we developed two immunoassays detecting CSF and plasma tau simultaneously phosphorylated at both T181 and T231 (p-tau181&231) and at T217 and T231 (p-tau217&231). Subsequently, we measured CSF and plasma p-tau181&231, p-tau217&231, p-tau181, p-tau217, and p-tau231 levels in two cohorts across the AD continuum and in frontotemporal dementia (FTD) patients (discovery n = 55, validation n = 118). CSF and plasma p-tau217&231, p-tau181, p-tau217, and p-tau231 and CSF, but not plasma, p-tau181&231 were significantly elevated in all AD continuum groups vs. Neurological Disease Control group. Notably, plasma p-tau217&231 consistently showed an improved diagnostic performance compared with single-site phosphorylation assays – p-tau217 or p-tau231. The differences observed between CSF and plasma measurements suggest matrix-specific protein processing, underscoring the need for further research on the dynamics of tau phosphorylation pattern along the AD continuum.
Similar content being viewed by others
Introduction
Alzheimer’s disease (AD) is the most common neurodegenerative disease, with an escalating global impact on public health1,2. With first disease-modifying therapies becoming available, early diagnosis of AD, prior to clinical manifestation, is of utmost importance3,4,5. Cerebrospinal fluid (CSF) measurement of amyloid-beta (Aβ) peptides and of different forms of tau phosphorylated (p-tau) at single sites (predominantly – threonine (T) 181 (p-tau181), T205 (p-tau205), T212 (p-tau212), T217 (p-tau217), and T231 (p-tau231)), allows for the identification of AD with high accuracy, effectively discriminating AD cases from control subjects and from other neurodegenerative diseases6,7,8,9,10,11. Thanks to development of ultrasensitive technologies that extend the range of measurable protein concentrations in body fluids, last decade has seen a substantial increase of studies exploring the diagnostic potential of AD biomarkers in blood-derived matrices. Compared with CSF collection, blood sampling is a less invasive procedure that can be conducted by a broad range of healthcare professionals, without specific expertise or equipment needed. Importantly, blood allows for repeated sampling, which is essential for longitudinal studies and for monitoring the effects of disease-modifying therapies. Similarly to the findings in CSF, several phosphorylated forms of tau (p-tau181, p-tau205, p-tau212, p-tau217, p-tau231) measured in plasma have demonstrated a high diagnostic value across different stages of the AD continuum7,11,12,13,14,15,16,17,18,19,20,21,22,23. However, diverse tau post-translational modifications (PTMs), including more than 50 phosphorylation sites, have been identified24,25,26, with their importance in physiology and pathology not being fully understood yet. Noteworthy, recent studies raised the question whether tau hyperphosphorylation might be a physiological process which intensifies along the course of AD progression24,26,27,28. Moreover, a pattern of tau staging has been proposed for AD, with site-specific phosphorylation changes occurring along disease progression and following distinct trajectories over time29. Further, the diagnostic and prognostic value of measuring tau simultaneously phosphorylated at different sites is unexplored, as well as its added value compared with single-site phosphorylated tau forms.
To investigate the potential of multiphosphorylated tau as AD biomarker in human body fluids, we developed two sandwich immunoassays detecting tau simultaneously phosphorylated at T181 and T231 (p-tau181&231; assay C231D181) and at T217 and T231 (p-tau217&231; assay C231D217). Subsequently, we measured p-tau181&231 and p-tau217&231 in matched CSF and plasma samples originating from well-characterized cohorts of patients with AD at different clinical stages, frontotemporal dementia (FTD), and Neurological Disease Control group (NDC).
Results
Technical validation
8-point standard curve of C231D181 assay included peptide standard dilutions (1:2) ranging from 80 pg/mL to 1.25 pg/mL and a blank, void of peptide standard (Supplementary Table 2). LLOQ and ULOQ for C231D181 assay were determined as 1.25 pg/mL and 80 pg/mL, respectively (Supplementary Table 3). The CV% for the intra- and inter-assay variability were, respectively, 10% and 3% (Supplementary Tables 4, 5). Good dilution linearity results were obtained as assessed on two different instruments (CV% on instrument 1: 11%, instrument 2: 6%; 1x, 2x, 4x, 8x, 16x, 32x dilutions of a spiked sample tested) (Supplementary Table 6). Spike-recovery assessment for C231D181 assay showed moderate recovery: 69% (low spike) and 87% (high spike) (Supplementary Table 7). Run with a mix of single-site phosphorylated peptides resulted in a blank level signal, showing that double-phosphorylation is required to form immunocomplex and produce the signal (Supplementary Table 8). The 8-point standard curve C231D217 assay included peptide standard dilutions (1:3) ranging from 40 pg/mL to 0.05 pg/mL and a blank, void of peptide standard (Supplementary Table 9). LLOQ and ULOQ for C231D217 assay were determined as 0.05 pg/mL and 40 pg/mL, respectively (Supplementary Table 10). The CV% for the inter- and intra-assay variability were, respectively, 7% and 4% (Supplementary Tables 11, 12). Good dilution linearity results were obtained as assessed on two different instruments (CV% on instrument 1: 2%, instrument 2: 3%; 2x, 4x, 8x, 16x, 32x dilutions of a spiked sample tested) (Supplementary Table 13). Spike-recovery assessment performed for C231D217 assay resulted in recovery of 72% (low spike) and 84% (high spike) (Supplementary Table 14).
Demographic and clinical profile of the cohort
Demographics and clinical parameters of the two cohorts are reported in Table 1. Apart from the expected differences in MMSE and CDR, statistically significant age differences among clinical groups were observed in both discovery and validation cohort (discovery: NDC vs. MCI-AD p ≤ 0.01, NDC vs. AD-dem p ≤ 0.001, validation: NDC vs. pre-AD, p ≤ 0.05, NDC vs. AD-dem p ≤ 0.01, AD-dem vs. FTD p ≤ 0.05). There were no significant differences in sex across the clinical groups in any of the cohorts.
Correlations between CSF and plasma biomarkers
As assessed in the discovery cohort, plasma p-tau181&231 did not correlate with CSF and plasma p-tau181, p-tau231 nor with its CSF equivalent (CSF p-tau181&231) (Fig. 1a). Per contra, both CSF and plasma p-tau217&231 exhibited a strong positive correlation with CSF and plasma levels of p-tau217 and p-tau231 (Spearman correlation analysis) (Fig. 1a, b).
Heatmap presenting results of Spearman’s correlation analysis for CSF and plasma biomarkers across the (a) discovery cohort (n = 55) and (b) validation cohort (n = 118). The color gradient indicates the strength and direction of the correlation according to Spearman’s correlation coefficient (ρ). Source data are provided as a Source Data file.
Diagnostic performance in the discovery cohort
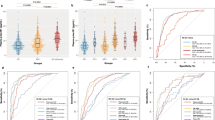
P-tau181, p-tau231, and p-tau181&231: in the discovery cohort, both CSF and plasma p-tau181 and p-tau231 as well as CSF p-tau181&231 levels were consistently increased in MCI-AD and AD-dem groups when compared with NDC (Fig. 2a). Plasma p-tau181&231 levels did not significantly differ between NDC and any of the AD continuum groups (Fig. 2b, Supplementary Fig. 2).
a CSF, (b) plasma measurements. Horizontal line refers to median and error bars indicate interquartile range. Data plotted in log10 scale. Kruskal-Wallis test was applied for multiple group comparisons, followed by Dunn’s post-hoc test. Reported p values are adjusted for multiple comparisons (two-sided). Legend. * = p ≤ 0.05, ** = p ≤ 0.01, *** = p ≤ 0.001, **** = p ≤ 0.0001, comparison vs. NDC. Cohen’s d: standardized effect size, AD: Alzheimer’s disease, pre-AD: preclinical AD, MCI-AD (n = 21): mild cognitive impairment due to AD, AD-dem: AD at dementia stage (n = 19), NDC: Neurological Disease Control group (n = 15). Source data are provided as a Source Data file.
CSF p-tau181, p-tau231, and p-tau181&231 measured in the discovery cohort, showed high accuracy in discriminating NDC from AD (area under the ROC curve (AUC) range 0.986–1.000; Supplementary Table 15). In plasma, p-tau231 exhibited the best ability to differentiate between NDC and both MCI-AD and AD-dem (plasma p-tau231 NDC vs. MCI-AD AUC = 0.925, 95% CI 0.840–1.000; NDC vs. AD-dem AUC = 0.947, 95% CI 0.872–1.000), followed by p-tau181 (plasma p-tau181 NDC vs. MCI-AD AUC = 0.877, 95% CI 0.761–0.993; NDC vs. AD-dem AUC = 0.943, 95% CI 0.857–1.000) (Supplementary Table 15, 16). ROC analysis performed for plasma p-tau181&231 showed low performance in discriminating NDC vs. MCI-AD (AUC = 0.514, 95% CI 0.320–0.709) and NDC vs. AD-dem (AUC = 0.579, 95% CI 0.383–0.775) (Supplementary Table 15, 16).
The analysis of the median concentration fold change performed for clinical groups comparison (median concentration in AD continuum group divided by median concentration in the control group) in the discovery cohort, showed CSF and plasma p-tau231 to result in the highest fold change (Supplementary Table 17). Large (d > 0.8) standardized effect size (Cohen’s d) was observed for all comparisons in CSF (Fig. 2a). In plasma, a large effect size was observed for p-tau231 and a medium effect size for p-tau181 (d > 0.5), while a negligible effect size was noted for p-tau181&231 (d < 0.2) (Fig. 2b).
P-tau217, p-tau231, and p-tau217&231: in the discovery cohort, p-tau217, p-tau231, and p-tau217&231 levels were consistently increased in MCI-AD and AD-dem groups when compared with controls in both CSF and plasma (Fig. 2, Supplementary Fig. 2).
ROC analysis performed for CSF p-tau217, p-tau231, and p-tau217&231 measured in the discovery cohort, showed high accuracy in discriminating between NDC and AD continuum stages (AUC range 0.986–1.000; Supplementary Table 15). In plasma, p-tau217&231 exhibited the best ability to differentiate between NDC vs. MCI-AD (AUC = 0.993, 95% CI 0.974–1.000) and NDC vs. AD-dem (AUC = 0.964, 95% CI 0.898–1.000) (Supplementary Table 15, 16).In the ROC analysis for NDC vs. all combined AD continuum groups (MCI-AD and AD-dem), plasma p-tau217&231 resulted in the highest nominal AUC (AUC = 0.979, 95% CI 0.945–1.000) among the compared plasma markers but no statistically significant difference was observed in comparison with AUC values obtained for plasma p-tau217 or p-tau231 (Fig. 3a).
Superimposed plasma p-tau217, p-tau231, and p-tau217&231 ROC curves for discrimination of NDC vs. all AD continuum groups in the (a) discovery cohort (MCI-AD, AD-dem; n = 40; NDC n = 15) and (b) validation cohort (pre-AD, MCI-AD, AD-dem; n = 55; NDC n = 24). AUC: Area Under Curve. Values in brackets represent CI 95 % (Wilson/Brown method). Source data are provided as a Source Data file.
Also in the ROC analysis performed according to patients’ CSF AT profile, plasma p-tau217&231 showed the highest nominal AUC values among the compared assays (A+ vs. A- AUC = 0.979, 95% CI 0.945–1.000; A + T+ vs. other AUC = 0.973, 95% CI 0.934–1.000) and yielded the highest standardized effect size (Supplementary Fig. 1).
In the discovery cohort, p-tau217&231 (C231D217 assay) showed the highest fold change of median concentration (AD continuum groups vs. NDC) when compared with all the other markers in both CSF and plasma (Supplementary Table 17). Large standardized effect size was observed for all clinical groups comparisons in CSF and plasma (Fig. 2).
Diagnostic performance in the validation cohort
P-tau181, p-tau231, and p-tau181&231: in the validation cohort, CSF p-tau181, p-tau231, and p-tau181&231 levels were consistently elevated in pre-AD, MCI-AD, and AD-dem groups while compared with controls (p ≤ 0.0001) (Fig. 4, Supplementary Fig. 2). CSF p-tau181, p-tau231, and p-tau181&231 levels did not significantly differ between NDC and FTD (Fig. 4, Supplementary Fig. 2).
a CSF, (b) plasma measurements. The horizontal line refers to the median, and error bars indicate the interquartile range. Data plotted in log10 scale. Kruskal-Wallis test was applied for multiple group comparisons, followed by Dunn’s post-hoc test. Reported p values are adjusted for multiple comparisons (two-sided). Legend: * = p ≤ 0.05, ** = p ≤ 0.01, *** = p ≤ 0.001, **** = p ≤ 0.0001, comparison vs. NDC. Cohen's d: standardized effect size, AD: Alzheimer’s disease, pre-AD: preclinical AD (n = 19), MCI-AD: mild cognitive impairment due to AD (n = 21), AD-dem: AD at dementia stage (n = 16), FTD: frontotemporal dementia (n = 39), NDC: Neurological Disease Control group (n = 24). Source data are provided as a Source Data file.
ROC analysis performed for CSF p-tau181, p-tau231, and p-tau181&231 measured in the validation cohort confirmed high accuracy of all three assays in discriminating NDC vs. MCI-AD and NDC vs. AD-dem (AUC range = 0.991–1.000; Supplementary Table 15, 16). Also, ROC analysis of NDC vs. pre-AD resulted in high AUC values for each of the assays (CSF p-tau181 NDC vs. pre-AD AUC = 0.970, 95% CI 0.929–1.000; CSF p-tau231 AUC = 0.991, 95% CI 0.972–1.000; CSF p-tau181&231 AUC = 0.982, 95% CI 0.951–1.000). CSF measurement of p-tau181, p-tau231, and p-tau181&231 allowed for an effective discrimination between AD-dem and FTD (AUC range = 0.968–0.978) (Supplementary Table 15).
In the validation cohort, the analysis of the median concentration fold change for AD continuum groups vs. NDC confirmed a trend observed in the discovery cohort, i.e., CSF and plasma p-tau231 showing the highest median concentration fold change (CSF p-tau231: discovery cohort AD-dem/NDC = 5.39; validation cohort AD-dem/NDC = 5.72; plasma p-tau231: discovery cohort AD-dem/NDC = 6.02; validation cohort AD-dem/NDC = 2.56; Supplementary Table 17). Large standardized effect size was observed for CSF p-tau181, p-tau231, and p-tau181&231 as well as plasma p-tau231 (Fig. 4). Plasma p-tau181 resulted in medium effect size for all clinical groups comparisons (pre-AD/NDC = 0.40, MCI-AD /NDC = 0.26, AD-dem/NDC = 0.29) (Fig. 4).
P-tau217, p-tau231, and p-tau217&231: in the validation cohort, both CSF and plasma p-tau217, p-tau231, and p-tau217&231 levels were consistently elevated in pre-AD, MCI-AD, and AD-dem groups while compared with controls (Fig. 4, Supplementary Fig. 2). Nor CSF neither plasma p-tau217, p-tau231, and p-tau217&231 levels differed significantly between NDC and FTD (Fig. 4).
ROC analysis performed for CSF p-tau217, p-tau231, and p-tau217&231 measured in the validation cohort confirmed the high accuracy of all three assays in discriminating between NDC and AD continuum stages (AUC range = 0.927–1.000), with CSF p-tau217 showing the highest AUC values for all comparisons (Supplementary Table 15). ROC analysis showed CSF p-tau217, p-tau231, and p-tau217&231 to effectively discriminate between AD-dem vs. FTD (AUC range = 0.934–0.978) (Supplementary Table 15). In plasma, the ROC analysis for discrimination between NDC and each of AD continuum stages, showed plasma p-tau217&231 to yield higher nominal AUC values than plasma p-tau217 and p-tau231 (Supplementary Table 15). A significant difference was observed in comparison with AUC of plasma p-tau217 NDC vs. MCI-AD and NDC vs. AD-dem but not in comparison with p-tau231 (Supplementary Table 16). Measurement of plasma p-tau217, p-tau231, and p-tau217&231 allowed for an effective discrimination between AD-dem and FTD (AUC range = 0.803–0.904) (Supplementary Table 15).
In the ROC analysis for NDC vs. all combined AD continuum groups (pre-AD, MCI-AD, and AD-dem), plasma p-tau217&231 provided the highest accuracy, yielding AUC of 0.968 95% CI 0.929–1.000, which was significantly different from AUCs obtained for plasma p-tau217 and p-tau231 (Fig. 3).
Plasma p-tau217&231 also resulted in the highest nominal AUC value among plasma p-tau measurements in discrimination of A+ vs. A- groups (AUC = 0.914, 95% CI 0.855–0.973) and A + T+ vs. other groups (AUC = 0.894 95% CI 0.831–0.957) as defined by CSF AT profile (Supplementary Fig. 1) and yielded the highest standardized effect size.
In the validation cohort, the analysis of median concentration fold change (AD continuum groups vs. NDC) in plasma, confirmed the trend observed in the discovery cohort, showing p-tau217&231 to exhibit higher fold change values than other markers (plasma p-tau217&231 fold change: discovery cohort AD-dem/NDC = 13.63; validation cohort AD-dem/NDC = 20.6; Supplementary Table 17). In CSF, the biggest median concentration fold change was reported for p-tau217&231 in the discovery cohort (CSF p-tau217&231 discovery cohort AD-dem/NDC = 18.13) and p-tau217 (CSF p-tau217 validation cohort AD-dem/NDC = 8.51) (Supplementary Table 17). For both CSF and plasma p-tau217, p-tau231, and p-tau217&231, large standardized effect size was determined for all clinical groups comparisons (Fig. 4).
Discussion
Tau phosphorylation regulates microtubules binding, hence impacts axon outgrowth and axonal transport – processes known to be impaired in AD30. Both CSF and plasma p-tau181, p-tau217, and p-tau231 have shown a very good diagnostic potential as AD biomarkers, with p-tau217 and p-tau231 possibly outperforming p-tau181 as markers of early AD pathology7,10,12,13,14,15,16,17,18,19,20,31,32. In this study, we developed two assays targeting CSF and plasma tau simultaneously phosphorylated at two distinct sites - T181 and T231 (p-tau181&231) and T217 and T231 (p-tau217&231). In both the discovery and validation cohorts, CSF p-tau181&231 and p-tau217&231 measurements consistently enabled discrimination of patients with AD at each clinical stage from the control group. Interestingly, plasma measurement of p-tau181&231 could not differentiate among clinical groups (assessed in the discovery cohort), while plasma p-tau217&231 effectively discriminated control subjects from AD continuum groups in both discovery and validation cohort. From the technical point of view, each of the developed assays enables sensitive and specific detection of tau forms carrying concurrent phosphorylation at two different sites.
The complexity of tau phosphorylation pattern across the AD spectrum, and its relationship between brain and different body fluids, are not fully explored. There is an ongoing debate whether an increasing degree of tau phosphorylation reflects AD progression, as well as what are the characteristics, distribution, and dynamics of tau phosphorylation along the disease continuum24,26,27,28,33. Post-mortem brain mass spectrometry studies comprehensively assessing tau PTMs across AD, showed significantly elevated levels of doubly- and triply-phosphorylated peptides in both soluble and insoluble fraction of AD brain tissue34. Further, multiple tau PTMs have been associated with disease progression26, with distinct tau PTMs proposed to play a different role in tau aggregation process33. Tau PTMs pattern has been also studied in body fluids. In a study investigating patients with dominantly inherited as well as a sporadic AD, Barthélemy et al. proposed a pattern of CSF tau staging with site-specific tau phosphorylation changes occurring along disease progression and following distinct trajectories over time29. Specifically, the authors found that in CSF, increase of p-tau217 preceeded that of p-tau181, and both phosphorylations were temporally associated with the development of amyloid pathology (assessed by amyloid PET). On the other hand, while an increase of CSF t-tau and p-tau205 was associated with development of tau pathology (assessed by tau-PET), for CSF p-tau217 and p-tau181 levels a trend of negative correlation with tau-PET has been observed29.
Current literature suggests that the majority of CSF tau is truncated and present as mainly N-terminal fragments with different cleavage sites (predominantly within positions 221–226)27,35,36. A similar fragmentation pattern has also been found in plasma since a significant decrease of tau peptides spanning the 221–226 positions has been observed16. The existence of these truncations in body fluids may result in a low abundance of tau fragments spanning from 181 to 231 and from 217 to 231 residues. At the same time, in the brain, peptides carrying multiple phosphorylations within the sequence 181–231 have been frequently identified24,37,38. Here, we show that using highly sensitive single molecule immunoassays, we could detect tau species spanning these residues and carrying phosphorylations at two different sites also in body fluids. The evidence for the presence of tau fragments covering residues 181 and 231 and bearing phosphorylation at these two sites in CSF was also shown by Ashton and colleagues18. The authors coupled immunoprecipitation and targeted mass spectrometry to verify the specificity of p-tau181 and p-tau231 antibodies for plasma immunoassay development. They observed that after CSF immunoprecipitation with antibodies against p-tau181, it was possible to detect peptides phosphorylated at T231; the same was true for immunoprecipitation using antibodies against p-tau231, thus confirming, through indirect detection, the presence of doubly phosphorylated species18.
Although both CSF and plasma levels of p-tau217&231 are elevated along the AD continuum, the diagnostic performance of p-tau181&231 significantly differs between the two matrices. The lack of agreement between CSF and plasma might arise due to differences in each matrix environment, driving altered tau processing39. Additionally, peripheral tau production and comorbidities such chronic kidney disease may differently influence plasma concentration of distinct tau fragments40,41.
While CSF and plasma increase of p-tau181, p-tau217, and p-tau231 across AD continuum is already widely reported in the literature10,13,15,18,42, in this work we used immunoassays to assess not only quantitative but also qualitative change of biofluid tau phosphorylation across distinct clinical stages of AD. As previous studies have suggested that the degree of tau hyperphosphorylation reflects disease progression, the detection of tau forms carrying multiple parallel phosphorylations may serve as an enhanced proxy for AD pathology24,27,28,33. At the same time, it should be considered that tau phosphorylation at specific sites may not simply reflect general hyperphosphorylation but rather exhibit a specific pattern24,26. The mosaic of tau phosphorylation (as well as other PTMs) simultaneously present at multiple sites might be thus dynamic and subject to changes, even at the individual level, depending on disease stage or presence of co-pathologies. The presented assay design offers high flexibility, as incorporation of different antibodies, targeting other PTMs with reported AD relevance, is possible. Development of such assays and assessment of their diagnostic performance would provide an important insight into tau metabolism across the AD continuum.
Our study has limitations. One of the limitations is the lack of absolute quantification of the synthetic peptides used as assay calibrators. The presented concentrations of tau simultaneously phosphorylated at T181 and T231 or T231 and T217 should be considered preliminary and not definitive. The use of absolutely quantified peptides as a standard would allow to obtain more precise values. Furthermore, potential risk of antibody cross-reactivity toward non-targeted tau phosphorylation sites should be considered. Additionally, further studies are warranted to define potential differences in protein processing in various matrices, here CSF and plasma. The assay for p-tau217&231 measurement should be re-developed with the use of available p-tau217 antibodies. Another limitation of the study is the relatively low sample size, especially of the pre-AD group, which could lead to overestimation of the diagnostic performance. Thus, we want to emphasize that these findings should be interpreted with caution and investigated on a larger cohort. However, the inclusion of a group of functionally independent patients with no objective evidence of cognitive deficits but with positive core CSF AD biomarkers is fundamental to fully understand the early dynamics of biomarker changes in body fluids across the AD continuum. Additionally, monitoring of a longitudinal cohort, subjected to repetitive plasma sampling and testing of multiphosphorylated tau species would enable further insight into changes of tau phosphorylation pattern along the disease continuum.
In conclusion, we propose the approach to target tau simultaneously phosphorylated at two distinct sites – T181 and T231 (p-tau181&231; assay C231D181) or T231 and T217 (p-tau217&231; assay C231D217). Our results suggest a good AD biomarker potential of CSF but not plasma p-tau181&231. On the other hand, we propose p-tau217&231 as a highly promising CSF and plasma biomarker, which performance in plasma might be potentially even superior to plasma p-tau217 or p-tau231. The differences observed between CSF and plasma suggest the matrix-specific protein processing and warrant further investigation, including assessment of tau simultaneously phosphorylated at sites different than those already analyzed, and extension of clinical validation to larger cohorts.
Methods
All the procedures were performed in accordance with Declaration of Helsinki and International Conference on Harmonization guidelines for Good Clinical Practice. All the patients and/or their legal representatives gave informed written consent for the lumbar puncture and the inclusion in the study that was approved by the local Ethics Committee (Comitato Etico Aziende Sanitarie Regione Umbria 19369/AV and 20942/21/OV).
Assay development and biomarker measurement
Single molecule array (Simoa®) sandwich immunoassay for CSF and plasma detection of tau simultaneously phosphorylated at T181 and T231 (assay C231D181) was developed with a 2-step protocol while a 3-step protocol was employed to develop the assay for detection of tau simultaneously phosphorylated at T217 and T231 (assay C231D217) (Fig. 5). All the measurements were run on the HD-XTM instruments (Quanterix Corp., USA) at the Assay Development laboratory of Quanterix Corp. (Billerica, MA, USA)43,44.
a C231D181, b C231D217 assay. T181: tau phosphorylation at threonine 181, T231: tau phosphorylation at threonine 231, T217 tau phosphorylation at threonine 217, SBG: streptavidin β-galactosidase, RGP: β-D-galactopyranoside. 2-step protocol workflow (C231D181 assay): 1) Sample incubation with a mixture of bead-conjugated capture antibody and biotinylated detector antibody, 2) Incubation with SBG; 3-step protocol workflow (C231D217 assay): 1) Sample incubation with bead-conjugated capture antibody, 2) Incubation with biotinylated detector antibody, 3) Incubation with SBG. Subsequently, immunocomplexes are resuspended in RGP (SBG substrate), resulting in generation of the fluorescent signal.
In both C231D181 and C231D217 assays, paramagnetic, fluorescent dye-encoded beads (647 nm, antibody-bound assay beads, concentration 7.2 × 106/mL) were conjugated with a mouse monoclonal antibody against human p-tau231 (ADx253, ADx NeuroSciences, Belgium18) and mixed with unconjugated helper beads (488 nm, concentration 12.8 × 106/mL). Biotinylated mouse monoclonal antibody against human p-tau181 (AT270; 90007, Fujirebio, Japan45,46); was labelled with SBG enzyme (SBG concentration 150 pM, detector concentration 1 µg/mL) and used as a detector antibody in C231D181 assay. In C231D217 assay, SBG-labelled detector (SBG concentration 150 pM, detector concentration 1 µg/mL) consisted of biotinylated mouse monoclonal antibody fragment against human p-tau217 (confidential, Quanterix Corp., USA). Capture (p-tau231) antibody used in both C231D181 and C231D217 assays was the same as the capture antibody in p-tau231 Advantage Kit (item 102292 Quanterix Corp., USA)18. C231D181 detector (p-tau181) antibody corresponded to the capture antibody in p-tau181 Advantage V2 Kit (item 103714 Quanterix, USA)46. C231D217 detector corresponded to the capture antibody in a prototype, non-commercialized assay for CSF and plasma detection of p-tau217 (Quanterix Corp., USA). 4-fold dilution in N4PE CSF Sample Diluent (Quanterix Corp., USA) was established as the default CSF and plasma sample dilution for both C231D181 and C231D217 assays. A custom synthetic peptide, specifically phosphorylated at T181 and T231 (N-term→C-term sequence: IPAKTPPAPKT (PO3H2) PPSSGEPPKREPKKVAVVRT (PO3H2) PPKSPSSAK; Anaspec, USA) was used as the assay calibrator for C231D181. Another custom synthetic peptide, specifically phosphorylated at T217 and T231 was used to calibrate C231D217 assay (N-term→C-term sequence: SRSRTPSLPT (PO3H2) PPTREPKKVAVVRT (PO3H2) PPKSPSSAK; Anaspec, USA). All peptide standard dilutions were prepared with N4PE CSF Sample Diluent (Quanterix Corp., USA). Before each run, RGP was incubated on the shaker at 35°C for 30 min (800 rpm). In both C231D181 and C231D217 assay protocols, RGP volume was 50 µl.
Both assays underwent analytical validation that consisted in the estimation of the intermediate precision (inter-assay reproducibility within the laboratory), repeatability (intra-assay), dilution linearity, sensitivity (Lower Limit of Quantification, LLOQ; Upper Limit of Quantification, ULOQ), and spike-recovery. Range of the standard curve was established, and the intra- and inter-assay variabilities were assessed based on coefficient of variation (CV) of the replicates. Dilution linearity, assessed on two independent instruments, was assessed for the sample spiked with the peptide standard. Four parameter logistic (4PL) curve model with 1/y (C231D181) and 1/y2 (C231D217) weighting was used for the curve fitting.
As a reference, CSF and plasma levels of p-tau181, p-tau231, and p-tau217 were measured with in-house manufactured Simoa® assays, utilizing the same antibodies, standards, and buffers as the commercially available kits offered by Quanterix i.e., p-tau181 Advantage V2 Kit (item 103714), p-tau231 Advantage Kit (item 102292; at the time of experiments, commercially launched for use with CSF), and a prototype, non-commercialized p-tau217 assay (capture antibody in the p-tau217 corresponding to capture antibody in the C231D217 assay). The p-tau181, p-tau231, and p-tau217 assays were standard format assays, thus employing phosphorylation site-specific capture antibody (T181/T231/T217) and detector antibody targeting unphosphorylated tau46.
Study participants
CSF and plasma samples were selected from a retrospective cohort of 173 patients enrolled at the Section of Neurology of the University of Perugia. The study cohort was then split into a discovery cohort (n = 55) and a validation cohort (n = 118).
All patients underwent a standardized assessment including medical history, physical and neurological examination, laboratory tests, and neuropsychological evaluation including, among screening tests, Mini-Mental State Examination (MMSE). Brain imaging (computed tomography or MRI) or 18F-fluoro-deoxyglucose positron emission tomography (18F-FDG-PET), were also performed in selected cases, according to clinical suspicion. In all cases, the diagnostic process was supported by the analysis of core CSF AD biomarkers (Aβ42, Aβ40, Aβ42/Aβ40, p-tau181, t-tau) measured with the Lumipulse® G600II (Fujirebio, Japan). Following principles of A/T/N system47, the patients were therefore classified as A+/A-, T+/T-, N+/N- according to the following cut-off values: Aβ42/Aβ40 = 0.072, 95% CI 0.07–0.074; p-tau181 = 50, 95% CI 46.2–52.3; t-tau=393, 95% CI 359–39648. Patients within the AD continuum were defined by A+/T+ CSF profile, according to NIA-AA criteria47.
The discovery cohort included patients with AD at dementia stage (AD-dem, n = 19) and patients with mild cognitive impairment due to AD (MCI-AD, n = 21). The AD continuum group in the validation cohort included AD-dem (n = 16), MCI-AD (n = 20), and subjects with preclinical AD (pre-AD, n = 19). The pre-AD patients were subjects with subjective cognitive complaints not confirmed by neuropsychological assessment but with the A+/T+ CSF profile. The clinical stage was defined according to the neuropsychological assessment and Clinical Dementia Rating (CDR) scale. In the validation cohort we also included a subgroup of FTD patients (n = 39). The diagnosis of FTD was supported by 18F-FDG-PET49,50. Each cohort included a control group (NDC, discovery cohort n = 15, validation cohort n = 24), composed of cognitively normal patients diagnosed with minor neurological disorders (e.g., headache, psychiatric disorders, mononeuropathies), other than inflammatory or degenerative disease of the CNS or of the peripheral nervous system, and patients with MCI attributed to cerebrovascular diseases. All subjects categorized as NDC were negative for classical AD CSF biomarkers (A-/T-/N- profile).
Age, sex, years of education, and MMSE scores for each clinical group are reported in Table 1. A/T/N profile data are reported in Supplementary Table 1.
Collection of human samples
CSF and plasma samples were collected between 2012 and 2021, following international guidelines and the same standard operating procedures throughout the study51,52. LP and blood sampling were performed between 8:00 and 10:00 a.m. after overnight fasting. CSF was collected into sterile polypropylene tubes and centrifuged for 10 min at 2000 × g at room temperature (RT). Whole blood was collected into sterile polypropylene tubes containing EDTA as the anticoagulant and centrifuged for 10 min at 2000 × g (RT) to obtain plasma. Once processed, CSF and plasma samples were stored in 0.5 mL tubes (72.730.007, Sarstedt, Germany) and immediately frozen at −80 °C pending analysis.
Statistics & Reproducibility
Continuous variables are represented as the median ± 1st−3rd quartile (Q1-Q3). Statistical analysis was performed with the use of GraphPad Prism software version 9.5.0 (USA) and R software version 4.2.253. The power analysis showed that a minimum sample size of 4–8 participants per group is required to achieve β = 0.2 and α = 0.05 for detection of true differences between AD-dem and NDC groups (estimates of plasma p-tau181, p-tau217, and p-tau231 levels derived from18,22). In-house Quanterix Corp. software was used for curve fitting and for extrapolation of concentrations from raw AEB signal (AEB: Average Enzyme per Bead, Simoa® units). For technical validation experiments, standard curve was included in each run. For clinical samples, raw AEB values were initially analyzed and the calibrator-based concentrations were assigned to the measurements post hoc, based on average standard curve obtained from technical validation runs. Samples were anonymized and the researcher completing measurements was blinded to patients’ clinical profile. Two-tailed p value ≤ 0.05 was considered statistically significant. D’Agostino-Pearson omnibus K2 test was applied to assess data normality. Kruskal-Wallis test was applied for multiple group comparisons, followed by Dunn’s post-hoc test. The statistical significance of differences in prevalence of categorical variables was assessed by means of the chi-squared test. Correlations were assessed by means of Spearman’s correlation coefficient. Receiver operating characteristic curve (ROC) analysis was applied to calculate the accuracy of each assay to discriminate between the control group and each of disease groups. To determine the 95% confidence interval (CI) of areas under the ROC curves, the Wilson/Brown method was applied. DeLong test was employed for comparison of Area Under Curve (AUC) values between the assays (pROC R package). For each of the analyzed biomarkers, median concentration fold change was calculated by dividing median concentration of AD continuum group (i.e., pre-AD, MCI-AD or AD-dem) by median concentration in the control group (NDC). Standardized effect size (Cohen’s d) was calculated with effsize R package (large: d > 0.8, medium d > 0.5, small d > 0.2, < 0.2 negligible)54.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
Source Data are provided with this paper. The raw data are provided in the Source Data file and Supplementary Information file. Any other blinded anonymized data is available on request from the corresponding authors. Request will be reviewed by the investigators and respective institutions to verify if the data transfer is in agreement with EU legislation on general data protection or is subject to any intellectual property or confidentiality obligations. Source data are provided with this paper.
References
2023 Alzheimer’s disease facts and figures. Alzheimers Dement 19, 1598–1695 (2023).
2020 Alzheimer’s disease facts and figures. Alzheimers Dement https://doi.org/10.1002/alz.12068 (2020).
van Dyck, C. H. et al. Lecanemab in early Alzheimer’s disease. N. Engl. J. Med 388, 9–21 (2023).
Söderberg, L. et al. Lecanemab, aducanumab, and gantenerumab - binding profiles to different forms of amyloid-beta might explain efficacy and side effects in clinical trials for Alzheimer’s Disease. Neurotherapeutics 20, 195–206 (2023).
Jönsson, L. et al. Viewpoint The affordability of lecanemab, an amyloid-targeting therapy for Alzheimer’ s disease: an EADC-EC viewpoint. 29, 1–7 (2023).
Blennow, K. & Zetterberg, H. The past and the future of Alzheimer’s disease fluid biomarkers. J. Alzheimer’s. Dis. 62, 1125–1140 (2018).
Gobom, J. et al. Antibody-free measurement of cerebrospinal fluid tau phosphorylation across the Alzheimer’s disease continuum. Mol. Neurodegener. 17, 81 (2022).
Ashton, N. J. et al. Cerebrospinal fluid p-tau231 as an early indicator of emerging pathology in Alzheimer’s disease. eBioMedicine 76, 103836 (2022).
Barthélemy, N. R. et al. CSF tau phosphorylation occupancies at T217 and T205 represent improved biomarkers of amyloid and tau pathology in Alzheimer’s disease. Nat. Aging 3, 391–401 (2023).
Janelidze, S. et al. Cerebrospinal fluid p-tau217 performs better than p-tau181 as a biomarker of Alzheimer’s disease. Nat. Commun. 11, 1–12 (2020).
Kac, P. R. et al. Plasma p-tau212 antemortem diagnostic performance and prediction of autopsy verification of Alzheimer’s disease neuropathology. Nat. Commun. 15, 2615 (2024).
Thijssen, E. H. et al. Diagnostic value of plasma phosphorylated tau181 in Alzheimer’s disease and frontotemporal lobar degeneration. Nat. Med. 26, 387–397 (2020).
Milà-Alomà, M. et al. Plasma p-tau231 and p-tau217 as state markers of amyloid-β pathology in preclinical Alzheimer’s disease. Nat. Med. 28, 1797–1801 (2022).
Janelidze, S. et al. Plasma P-tau181 in Alzheimer’s disease: relationship to other biomarkers, differential diagnosis, neuropathology and longitudinal progression to Alzheimer’s dementia. Nat. Med. 26, 379–386 (2020).
Palmqvist, S. et al. Discriminative accuracy of plasma phospho-tau217 for Alzheimer's disease vs other neurodegenerative disorders. JAMA 324, 772 (2020).
Barthélemy, N. R., Horie, K., Sato, C. & Bateman, R. J. Blood plasma phosphorylated-tau isoforms track CNS change in Alzheimer’s disease. J. Exp. Med. 217, 1–12 (2020).
Wilson, E. N. et al. Performance of a fully—automated Lumipulse plasma phospho ‑ tau181 assay for Alzheimer’ s disease. Alzheimer’s Res. Ther. 14, 172 (2022).
Ashton, N. J. et al. Plasma p-tau231: a new biomarker for incipient Alzheimer’s disease pathology. Acta Neuropathologica 141, 709–724 (2021).
Brickman, A. M. et al. Plasma p-tau181, p-tau217, and other blood-based Alzheimer’s disease biomarkers in a multi-ethnic, community study. 1353–1364 https://doi.org/10.1002/alz.12301 (2021).
Montoliu-Gaya, L. et al. Mass spectrometric simultaneous quantification of tau species in plasma shows differential associations with amyloid and tau pathologies. Nat. Aging 3, 661–669 (2023).
Lantero Rodriguez, J. et al. Plasma p-tau181 accurately predicts Alzheimer’s disease pathology at least 8 years prior to post-mortem and improves the clinical characterisation of cognitive decline. Acta Neuropathol. 140, 267–278 (2020).
Thijssen, E. H. et al. Plasma phosphorylated tau 217 and phosphorylated tau 181 as biomarkers in Alzheimer’s disease and frontotemporal lobar degeneration: a retrospective diagnostic performance study. Lancet Neurol. 20, 739–752 (2021).
Gonzalez-Ortiz, F. et al. A novel ultrasensitive assay for plasma p-tau217: Performance in individuals with subjective cognitive decline and early Alzheimer’s disease. Alzheimer’s & Dementia 20, 1239–1249 (2024).
Wegmann, S., Biernat, J. & Mandelkow, E. A current view on Tau protein phosphorylation in Alzheimer’s disease. Curr. Opin. Neurobiol. 69, 131–138 (2021).
Kimura, T., Sharma, G., Ishiguro, K. & Hisanaga, S. Phospho-Tau bar code: analysis of phosphoisotypes of Tau and its application to tauopathy. Front Neurosci. 12, 44 (2018).
Wesseling, H. et al. Tau PTM profiles identify patient heterogeneity and stages of Alzheimer’s disease. Cell 183, 1699–1713.e13 (2020).
Barthélemy, N. R., Mallipeddi, N., Moiseyev, P., Sato, C. & Bateman, R. J. Tau phosphorylation rates measured by mass spectrometry differ in the intracellular brain vs. Extracellular cerebrospinal fluid compartments and are differentially affected by Alzheimer’s disease. Front. Aging Neurosci. 11, 1–18 (2019).
Drepper, F., Biernat, J., Kaniyappan, S. & Meyer, H. E. ARTICLE A combinatorial native MS and LC-MS / MS approach reveals high intrinsic phosphorylation of human Tau but minimal levels of other key modifications. J. Biol. Chem. 295, 18213–18225 (2020).
Barthélemy, N. R. et al. A soluble phosphorylated tau signature links tau, amyloid and the evolution of stages of dominantly inherited Alzheimer’s disease. 26, 398–407 (2020).
Wang, Z., Tan, L. & Yu, J. Axonal transport defects in Alzheimer’ s disease. 1309–1321 https://doi.org/10.1007/s12035-014-8810-x (2015).
Yu, L. et al. Plasma p-tau181 and p-tau217 in discriminating PART, AD and other key neuropathologies in older adults. Acta Neuropathol. https://doi.org/10.1007/s00401-023-02570-4 (2023).
Leuzy, A. et al. Comparing the clinical utility and diagnostic performance of CSF P-Tau181, P-Tau217, and P-Tau231 Assays. Neurology 97, e1681–e1694 (2021).
Kyalu Ngoie Zola, N. et al. Specific post-translational modifications of soluble tau protein distinguishes Alzheimer’s disease and primary tauopathies. Nat. Commun. 14, 3706 (2023).
Lantero-Rodriguez, J. et al. Tau protein profiling in tauopathies: a human brain study. Mol. Neurodegener. 19, 54 (2024).
Cicognola, C. et al. Novel tau fragments in cerebrospinal fluid: relation to tangle pathology and cognitive decline in Alzheimer’s disease. Acta Neuropathologica vol. 137, 279–296 (2019).
Sato, C. et al. Tau kinetics in neurons and the human central nervous system. Neuron 97, 1284–1298.e7 (2018).
Brinkmalm, G. et al. Phosphorylations Correlate With Disease Specific Isoforms In Sarkosyl Insoluble Tau From Brain. in (Gothenburg, Sweden, 2023).
Horie, K. et al. Regional correlation of biochemical measures of amyloid and tau phosphorylation in the brain. Acta Neuropathologica Commun. 8, 149 (2020).
Cicognola, C. et al. Novel tau fragments in cerebrospinal fluid: relation to tangle pathology and cognitive decline in Alzheimer’ s disease. Acta Neuropathologica 137, 279–296 (2019).
Dugger, B. N. et al. The presence of select tau species in human peripheral tissues and their relation to Alzheimer’s disease. J. Alzheimer’s. Dis. 51, 345–356 (2016).
Janelidze, S., Barthélemy, N. R., He, Y., Bateman, R. J. & Hansson, O. Mitigating the associations of kidney dysfunction with blood biomarkers of Alzheimer disease by using phosphorylated tau to total Tau ratios. JAMA Neurol. 80, 516–522 (2023).
Karikari, T. K. et al. Blood phosphorylated tau 181 as a biomarker for Alzheimer’s disease: a diagnostic performance and prediction modelling study using data from four prospective cohorts. Lancet Neurol. 19, 422–433 (2020).
Rissin, D. M. et al. Single-molecule enzyme-linked immunosorbent assay detects serum proteins at subfemtomolar concentrations. Nat. Biotechnol. 28, 595–599 (2010).
Teunissen, C. E. et al. Methods to discover and validate biofluid-based biomarkers in neurodegenerative dementias. Mol. Cell. Proteom. 22, 100629 (2023).
Vanmechelen, E. & Vanderstichele, H. Diagnosis Of Tauopathies Determining Tau/phospho-tau Ratio. (2002).
Ashton, N. J. et al. Plasma and CSF biomarkers in a memory clinic: head-to-head comparison of phosphorylated tau immunoassays. Alzheimers Dement 19, 1913–1924 (2023).
Jack, C. R. et al. NIA-AA research framework: toward a biological definition of Alzheimer’s disease. Alzheimer’s. Dement. 14, 535–562 (2018).
Bellomo, G. et al. Machine learning driven profiling of cerebrospinal fluid core biomarkers in Alzheimer’s disease and other neurological disorders. Front. Neurosci. 15, 1–9 (2021).
Rascovsky, K. et al. Sensitivity of revised diagnostic criteria for the behavioural variant of frontotemporal dementia. Brain 134, 2456–2477 (2011).
Gorno-Tempini, M. L. et al. Classification of primary progressive aphasia and its variants. Neurology 76, 1006–1014 (2011).
Teunissen, C. E. et al. A consensus protocol for the standardization of cerebrospinal fluid collection and biobanking. Neurology 73, 1914–1922 (2009).
Rózga, M., Bittner, T., Batrla, R. & Karl, J. Preanalytical sample handling recommendations for Alzheimer’s disease plasma biomarkers. Alzheimer’s. Dement.: Diagnosis, Assess. Dis. Monit. 11, 291–300 (2019).
R Core Team (2019). R: A Language And Environment For Statistical Computing. (R Foundation for Statistical Computing, Vienna, Austria, 2019).
Cohen, J. et al. Statistical Power Analysis for the Behavioral Sciences. (Routledge, New York, 1988).
Acknowledgements
We thank Quanterix Corp. for providing technical support, instrumentation, and reagents necessary to perform the experiments. We thank Dr. Dandan Shan for sharing extensive expertise on the Simoa® technology and assay development. We extend our acknowledgements to Dr. Silvia Paciotti, Dr. Alfredo Megaro, and Andrea Toja, MD, for their help in samples selection. We also thank all the Members of the MIRIADE consortium for collaboration and scientific discussion. This project has received funding from the European Union’s Horizon 2020 research and innovation program under grant agreement no. 860197 (ALW, LP, CET). GB is supported by the Postdoctoral Fellowship for Basic Scientists grant of the Parkinson’s Foundation (Award ID: PF-PRF-934916).
Author information
Authors and Affiliations
Contributions
All authors read and approved the final manuscript. A.L.W.: design of the work, data acquisition, analysis, and interpretation, visualization, manuscript writing; G.B.: data analysis and interpretation, visualization, critical revision of the manuscript; L.G.: patients’ diagnosis (neurological assessment) and cohort enrollment, critical revision of the manuscript; C.E.T.: project administration, funding acquisition, critical revision of the manuscript; L.P.: patients’ diagnosis (neurological assessment) and cohort enrollment, project administration, funding acquisition, critical revision of the manuscript; D.C.: design of the work, data analysis and interpretation, visualization, manuscript writing, project supervision.
Corresponding authors
Ethics declarations
Competing interests
ALW completed the experiments during the internship at Quanterix Corp. that was an integral part of MIRIADE project (European Union’s Horizon 2020 research and innovation program under grant agreement no. 860197). GB received honoraria from Fujirebio and completed paid consultancies for Parkinson’s Foundation. He received travel/educational grants from Fujirebio and Alzheimer’s Association. LG has participated in advisory boards for, and received writing or speaker honoraria and travel grants from, Almirall, Biogen, Eisai, Euroimmun, Fujirebio, Lilly, Merck, Mylan, Novartis, Roche, Sanofi, Siemens Healthineers, and Teva. LP served as Member of Advisory Boards for Fujirebio, IBL, Roche, and Merck. CET is employed by Amsterdam UMC. She has grants or contracts for Research of the European Commission (Marie Curie International Training Network, grant agreement No. 860197 (MIRIADE), Innovative Medicines Initiatives 3TR (Horizon 2020, grant no 831434) EPND (IMI 2 Joint Undertaking (JU), grant no. 101034344) and JPND (bPRIDE), National MS Society (Progressive MS alliance), Alzheimer Drug Discovery Foundation, Alzheimer Association, Health Holland, the Dutch Research Council (ZonMW), including TAP-dementia, a ZonMw funded project (#10510032120003) in the context of the Dutch National Dementia Strategy, Alzheimer Drug Discovery Foundation, The Selfridges Group Foundation, Alzheimer Netherlands. She is recipient of ABOARD, which is a public-private partnership receiving funding from ZonMW (#73305095007) and Health~Holland, Topsector Life Sciences & Health (PPP-allowance; #LSHM20106). She is also a contract researcher for ADx Neurosciences, AC-Immune, Aribio, Axon Neurosciences, Beckman-Coulter, BioConnect, Bioorchestra, Brainstorm Therapeutics, Celgene, Cognition Therapeutics, EIP Pharma, Eisai, Eli Lilly Fujirebio, Grifols, Instant Nano Biosensors, Merck, Novo Nordisk, Olink, PeopleBio, Quanterix, Roche, Siemens, Toyama, Vivoryon, and the European Commission. She has received payment or honoraria from Roche, Novo Nordisk, and Grifols, where all payments were made to her institution. She also serves on editorial boards of Medidact Neurologie/Springer; and in Neurology: Neuroimmunology & Neuroinflammation. She is editor of Alzheimer Research and Therapy. DC received travel/educational grant from Fujirebio.
Peer review
Peer review information
Nature Communications thanks Fernando Gonzalez-Ortiz, Marc Suárez-Calvet and the other, anonymous, reviewers for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wojdała, A.L., Bellomo, G., Gaetani, L. et al. Immunoassay detection of multiphosphorylated tau proteoforms as cerebrospinal fluid and plasma Alzheimer’s disease biomarkers. Nat Commun 16, 214 (2025). https://doi.org/10.1038/s41467-024-54878-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-024-54878-8