Abstract
Next Generation Sequencing-based subtyping and interim- and end of treatment positron emission tomography (i/eot-PET) monitoring have high potential for upfront and on-treatment risk assessment of diffuse large B-cell lymphoma patients. We performed Dana Farber Cancer Institute (DFCI) and LymphGen genetic subtyping for the HOVON84 (n = 208, EudraCT-2006-005174-42) and PETAL (n = 204, EudraCT-2006-001641-33) trials retrospectively combined with DFCI genetic data (n = 304). For all R-CHOP treated patients (n = 592), C5/MCD- and C2/A53-subtypes show significantly worse outcome independent of the international prognostic index. For all subtypes, adverse prognostic value of i/eot-PET-positive status is confirmed. Consistent with frequent primary refractory disease, only 67% C2 patients become eot-PET-negative versus 81-88% for other subtypes. Indicative of high relapse rates, outcome of C5 i/eot-PET-negative patients remains significantly worse in HOVON-84, which trend validates in the PETAL and SAKK38-07 trials (NCT00544219). These results show the added value of integrated genetic subtyping and PET monitoring for prognostic stratification and subtype-specific trial design.
Similar content being viewed by others
Introduction
Diffuse large B-cell lymphoma not otherwise specified (DLBCL-NOS) is the most frequent type of B-cell lymphoma in adults and one of the most heterogeneous in presentation, treatment response and long-term outcome1,2,3. Five-year survival rates after standard immunochemotherapy containing rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) range between 80% and 40% depending on International Prognostic Index (IPI) status. Mortality is largely due to relapse and primary refractory disease as second-line high-dose chemotherapy and stem cell rescue-based approaches are only limitedly successful4,5,6,7. Over the past decades, the biological knowledge provided by RNA expression-based cell-of-origin (COO) dichotomization has served as the basis for targeted approaches in various large, randomized phase 3 clinical trials. However, these trials have not been as successful as anticipated to demonstrate improved outcome when assumed targeted compounds were added to R-CHOP8,9,10,11. Therefore, COO requires further refinement to capture a more complete biological heterogeneity of DLBCL-NOS in a clinically relevant manner. More recently, several large DNA-based next generation sequencing (NGS) subtyping studies have shed light on the complexity of the genetic landscape of DLBCL12,13,14,15. The respectively 5 to 7 genetic DLBCL-NOS subtypes proposed by the Dana Farber Cancer institute (DFCI)12 and the National Cancer Institute (LymphGen)14,16 have significant overlap, based on their subtype-specific genomic drivers and signalling pathways17,18. This overlap underpins their biological significance, particularly given the different approaches that have led to their description19. The clinical predictive potential was recently demonstrated by retrospective analysis of the PHOENIX phase III clinical trial that showed benefit of the addition of ibrutinib to R-CHOP for two of the genetic subtypes for patients under 6020. Further potential was demonstrated in the phase II GUIDANCE-01 trial in which addition of a variety of targeted agents to R-CHOP guided by LymphGen genetic subtyping showed benefit, albeit based on very small numbers of patients21. While this demonstrates the feasibility for upfront treatment stratification, a broader implementation of genetic profiling in clinical management, including risk assessment during and at end of first-line treatment is insufficiently explored.
Thus far, the DFCI and LymphGen genetic subtypes have been recapitulated in few independent patient series15,22. Since treatment in the discovery cohorts as well as in these independent series was rather heterogeneous, even the prognostic impact under standard R-CHOP treatment has not been fully resolved. These arguments have precluded inclusion of genetic subtypes in prognostic models to complement the gold standard of the IPI1,16,21,22,23,24. Lack of consensus on significant genetic drivers defining proposed clusters in a unified concept has further contributed to the decision that implementation of genetic subtyping in the newest Lymphoma Classifications is too early2,3.
For DLBCL-NOS, 18Fluorodeoxyglucose-positron emission tomography (PET)-computed tomography (CT) is well-established as a staging procedure at diagnosis and for end-of-treatment (eot) response evaluation25. Thereby, a negative eot-PET is valued as highly predictive of good outcome (negative predictive value, NPV > 85%) and considered a reliable basis for clinical decision making26. A positive eot-PET is by and large predictive of poor outcome, though positive predictive values (PPVs) reported are highly variable27. The value of interim PET (i-PET) monitoring holds high potential for response monitoring, but is less widely accepted, since the optimal timing of i-PET during treatment is not fully determined26. In view of the knowledge on DLBCL-NOS genetic subtypes underpinning their different biological characteristics, we hypothesize that therewith also PPV and NPV of i/eot-PET may depend on the genetic subtype. Consequently, upfront knowledge of the genetic subtype would impact on clinical decisions of the results of i/eot-PET during and after treatment.
In this manuscript, we perform genetic subtyping of uniformly R-CHOP treated DLBCL-NOS patient samples derived from 3 clinical-trial cohorts, and correlate the respective subtypes with i/eot-PET outcome. Thereby, the present study aims to I) establish the independent value of genetic subtyping for outcome and II) evaluate the predictive value of i/eot-PET in the different genetic subtypes. These results show that knowledge of the genetic subtype of a patient’s lymphoma is clinically relevant to interpret i/eotPET outcome.
Results
Recapitulation of DFCI and LymphGen genetic subtypes
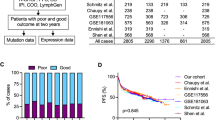
The spectrum of mutations, CNAs and translocations of the 208 HOVON-84 and 204 PETAL uniformly R-CHOP treated trial patients (Fig. 1, Table 1) was calculated (overview of called mutations, CNA, translocations see Supplementary Fig. S1A and S1B and detailed molecular information according to reporting guidelines by Dreval et al. 28 (see Supplementary Data S3 and Supplementary Data S4). Based on these genetic characteristics compared to the genetic characteristics of DFCI and other larger DLBCL studies13,21,22, we conclude that these 2 cohorts form a representative selection (Supplementary Fig. S1C). To allow for optimal robust clustering, we applied DFCI NMF clustering using genetic data of all 208 HOVON-84 and 204 PETAL samples, combined with the genetic data of 304 DFCI samples (input matrix for NMF clustering see Supplementary Data S5). With this large merged cohort, NMF recapitulated the expected five clusters with a distribution across the subtypes commensurate with the original DFCI clustering (Supplementary Data S1) and each driven by the reported alterations12 (Fig. 2). For all 716 samples combined, NMF cluster adherence was calculated, which considered 502 (70%) cases as “core samples”, as they were consistently assigned to the same cluster in the 1000 iterations applied (Supplementary Data S1). This performance is in line with the 70% core- versus 30% non-core samples previously determined using only DFCI cohort samples19. Altogether, we conclude that we successfully recapitulated the NMF stratification and assigned cluster and cluster adherence (core versus non-core) for each of the 716 samples. DFCI-C5-core samples of the three cohorts were subsequently used to build a classifier and assign the 76 SAKK-38/07 samples to either DFCI-C5 or non-C5, which classified 15 patients as DFCI-C5 (20%), and 61 as non-C5 (80%).
acases of follicular lymphoma grade 3B, primary testicular large B-cell lymphoma, primary CNS large B-cell lymphoma and primary mediastinal B-cell lymphoma were excluded. bcases for which FFPE blocks were not available, containing insufficient remaining tissue or not representative material were excluded. call cases failing NGS quality control, including tumor percentage <20% as measured by the algorithm ACE were excluded. dall cases with stage 1 disease and receiving any other treatments than R-CHOP-14, including Burkitt-like treatment were excluded. NGS=next generation sequencing, i/eot-PET=interim/end-of-treatment 18fluoro-deoxyglucose-postron emission tomography, IPI=International Prognostic Index.
Coloured boxes in the heat map and “NMF cluster” bars in the header show the 5 clusters; C1, purple; C2, blue; C3, orange; C4, green; C5, red; and non-annotated samples C0, grey. The header furthermore shows the dendrogram; Top bar “Cohort” colour coded per sample; DFCI, dark red; HOVON-84, blue; PETAL, yellow; “COO” bar, cell-of-origin assignment with GCB, orange; non-GCB, green; unclassifiable, yellow; not assessed, white; “DFCI assignment” bar, DFCI samples with their originally published cluster assignment. “LymphGen” assignment bar, colour coded per sample with colour codes according to their DFCI counterparts18 with BN2, purple; A53, blue; EZB, orange; ST2, green; MCD, red; Other, grey; unclassified, white. “NMF cluster” bar colour coded accordingly. The right y-axis gives the genetic alterations that define the 5 clusters, per cluster ranked by significance, -log10q Fisher exact test values (Benjamini-Hochberg corrected p-values) grey horizontal bars. Type of genomic drivers are colour coded in the heat map: synonymous mutations, light green; non-synonymous mutations, dark green; copy number gains, red; copy number losses, blue; translocations, purple. Source data are provided in Supplementary Data 1 and 5.
The LymphGen classification algorithm could assign 126 HOVON-84 (61%) and 124 PETAL (61%) samples to LymphGen classes, with a similar distribution across the subtypes as previously reported and left 39% of each cohort unclassified, which is in line with reported experience16 (Supplementary Data S1). Samples uniquely assigned to one of the genetic subtypes by the LymphGen classification algorithm (both core and extended) had significant overlap with the DFCI genetic subtypes (core and non-core)17,18 (Fig. 2).
In summary, we reliably recapitulated the 5 reported NMF clusters DFCI-C1 to C5 and the 6 LymphGen subtypes BN2, EZB, A53, ST2, MCD and “unclassified/other” to genetically assign all HOVON-84 and PETAL samples as well as assigned DFCI-C5 versus non-C5 subtypes for SAKK-38/07.
Association of genetic subtypes with survival
COO classification could be determined for the majority of the HOVON-84 and PETAL patient samples and showed a relative overrepresentation of GCB cases in these trial cohorts, which is not an uncommon clinical trial bias (Supplementary Table S1 and Supplementary Data S1). Survival analysis of those patients uniformly treated with R-CHOP (n = 612), showed expected survival advantage of GCB-type (Fig. 3A, B and Supplementary Fig. S2) This supports the representative nature for survival analysis of the present study cohort.
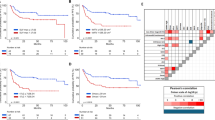
Kaplan-Meier survival analyses for HOVON-84, PETAL and DFCI cohorts combined, N = 607; (A) PFS for Cell-of origin (COO) class. GCB: green; ABC/non-GCB orange. (B) for OS (C) PFS for DFCI clusters. C1, purple; C2, blue; C3, orange; C4, green; C5, red. (D) for OS (E) PFS for LymphGen classes. P-values were calculated using the log-rank test. BN2, purple; A53, blue; EZB, orange; ST2, green; MCD, red; other, grey. (F) for OS. PFS progression-free survival. OS overall survival. Source data are provided as a Source Data file.
Next, for the 612 HOVON-84, PETAL and DFCI patients that received R-CHOP treatment we assessed the prognostic significance of the NMF and LymphGen genetic subtypes. A significant association of the DFCI subtypes and survival was found for this combined cohort (PFS p = 0.002, OS p = 0.015 Fig. 3C, D), implicating that DLBCL genetic subtype impacts survival, with DFCI-C5 showing a significantly adverse outcome (C5 vs. rest PFS; p = 0.001, OS; p = 0.01). Consistent poor outcome for DFCI-C5 substantiated for the individual cohorts separately (Supplementary Fig. S3). Similarly, a significant association of the Lymphgen subtypes and survival was found for this combined cohort (PFS p = 0.017, OS p = 0.003 Fig. 3E and F), with LymphGen-MCD, and -A53 having an adverse outcome for both PFS and OS for the combined cohort (LymphGen-MCD vs. rest, PFS: p = 0.07, OS: p = 0.04; LymphGen-A53 vs.rest, PFS; p = 0.004, OS: p = 0.002, Fig. 3E, F), which observation substantiated for Lymphgen-MCD in the individual cohorts separately (Supplementary Fig. S4).
It should be noted that after the original definition, the LymphGen-EZB subtype was subdivided into two groups based on a positive or negative MYC-related double hit (DHIT) gene expression prolife. EZB/DHIT-positive cases had a poor survival, while EZB/DHIT-negative cases were associated with a relatively good survival16,29. DHIT gene-expression data was not performed for these cohorts and therefore the presented mixed EZB subtype data should be interpreted with caution.
Prognostic value of genetic subtypes in relation to IPI
We first verified the prognostic value of IPI for the HOVON-84, PETAL and DFCI cohorts and observed the expected prognostic separation of low-, low intermediate-, high intermediate- and high-risk groups (Supplementary Fig. S5)1. Next, we analysed the relation of DFCI- or LymphGen genetic subtypes and IPI in the HOVON-84, PETAL and DFCI combined study cohort using the n = 592 patient samples that had IPI and PFS data available (Fig. 1). We found a significant association of IPI with DFCI subtypes (Chi-squared test, p = 0.022) and LymphGen subtypes (Chi-squared test, p = 0.0015). Multivariate Cox regression showed that the molecular subtypes are significant independent variables for PFS (LymphGen; p = 0.004, DFCI; p = 0.001, ANOVA) and OS (LymphGen; p = 0.0001, DFCI; p = 0.007, ANOVA) (Supplemental Fig. S5). DFCI’s C5 and LymphGen’s counterpart MCD had adverse outcome independent of IPI (C5 vs. rest, PFS; p = 0.004, MCD vs. rest, PFS; p = 0.002), whereas for DFCI’s C2 and LymphGen’s counterpart A53 only the latter had adverse outcome independent of IPI, as furthermore supported by separate analyses (DFCI-C2 vs. rest, PFS; p = 0.24, A53 vs rest, PFS; p = 0.004) (Supplemental Fig. S5).
Association of genetic subtypes with i/eot-PET status
The relation of i/eot-PET with genetic subtypes was investigated in the HOVON-84 cohort (i-PET after 4 R-CHOP cycles and eot-PET performed) and PETAL cohort (iPET after 2 R-CHOP cycles performed only). I/eot-PET was not available for the DFCI cohort. Results are presented in Fig. 4. As compared to all other subtypes, a significantly higher percentage of DFCI-C2 patients did not reach negative i-PET after 4 cycles and eot-PET after 6- to 8-cycles of R-CHOP treatment (44% and 14% respectively, p = 0.00004; 33% and 12% respectively, p = 0.003). After only 2-cycles of treatment such association was not observed in the PETAL cohort (p = 0.17). DFCI-C1 patients showed early response. DFCI-C5 patients showed similar high response levels after first-line R-CHOP treatment to DFCI-C1 and C4 patients (81–87% negative eot-PET) in HOVON-84, and therefore does not explain the adverse prognosis of this subtype. Significant associations could not be demonstrated for LymphGen subtypes, most likely caused by low numbers of samples that are assigned per subtype and the high proportion of unclassified samples, which is inherent to this classification (Supplementary Fig. S6)16,17,22.
C1 patients show early, maximal response after 2 cycles, while only 39%–46% of C3, C4 and C5 patients show early response, which further extends after 4 cycles and until conclusion of treatment. C2 patients show initial similar response, but limited further improvement. PET-negative status: green; PET-positive status red. Source data are provided as a Source Data file.
Added value of genetic subtypes to i/eot-PET status for outcome prediction
The impact of genetic subtypes on i/eot-PET as outcome predictor was investigated in a test/validation design with the HOVON-84 cohort for test and the PETAL- and SAKK-38/07 cohorts for validation. As expected, i/eot-PET-positive status was a significant poor prognostic factor for PFS and OS in all three cohorts, though not (yet) significant after 2 cycles of R-CHOP for PFS in the PETAL and SAKK cohorts (Supplementary Figs. S7, S8, S9). The prognostic value of i/eot-PET-positive status in DFCI and LymphGen genetic subtypes could not be further analysed due to low numbers of PET-positive cases.
Eot-PET-negative patients in the HOVON-84 cohort showed a significantly adverse prognosis for DFCI-C5 patients compared to all other subtypes (Fig. 5A, D, PFS: p < 0.001, Supplementary Fig. S10). Also, i-PET negative DFCI-C5 HOVON-84 patients after 4 cycles of treatment showed this significantly worse prognosis compared to all other subtypes (Fig. 5A, D; PFS: p = 0.00011, Supplementary Fig. S10). In line with these observations, PETAL DFCI-C5 i-PET negative patients already after 2 cycles of treatment showed a trend towards an unfavourable prognosis, (Fig. 5B, D; p = 0.073, Supplementary Fig. S10). In the SAKK-38/07 trial, i-PET after 2 and 4 cycles and eot-PET had been performed. Again, despite a low number of events for DFCI-C5 patients, a clear yet not statistically significant trend was observed for worse PFS of the DFCI-C5 i/eot-PET negative patients compared to all other subtypes (Fig. 5C, D). The observation that DFCI-C5 patients have a poor prognosis but respond similarly to first line R-CHOP treatment compared to all other subtypes prompted us to calculate the NPV of eot-PET for clinical purposes. For HOVON-84 DFCI-C5 patients, this NPV was reduced to 81% in contrast to a NPV of 88% for all other genetic subtypes.
Kaplan Meier plots for (A) HOVON-84; (B) PETAL; (C) SAKK-38/07; left column “i-PET2”: i-PET after 2 cycles of R-CHOP, middle column “i-PET4”: i-PET after 4 cycles of R-CHOP, right column “eot-PET”: eot-PET after 6 to 8 cycles of R-CHOP treatment, C5 subtype (red), all other subtypes combined (black), PFS, progression-free survival. The risk table below each plot denotes the number of patients at risk in each group at different timepoints. D Forest plot, per cohort and number of R-CHOP treatment cycles. The groups compared correspond to the groups in (A–C). Hazard ratios, confidence intervals and statistical significance (P-values) were determined using Cox regression. The sample size in each model corresponds to the number of patients at risk at timepoint 0 in the risk tables in (A–C). HR: hazard ratio, black squares with size proportional to weight. (95% CI): confidence interval horizontal lines, and P, unadjusted P-values. Source data are provided as a Source Data file.
Since, only 61% of cases were assigned to specific classes LymphGen subtypes inherent to the algorithm, a detailed analysis for these genetic subtypes was limited. Therefore, we concentrated on MCD as the molecular counterpart of DFCI-C5. In the HOVON-84 cohort, the n = 17 eot-PET-negative MCD patients showed significantly worse PFS compared to the n = 142 non-MCD patients (p = 0.0029), further substantiating our findings (Supplementary Fig. S10). For PETAL, only 7 i-PET negative cases classified as MCD with only 1 event, preclude further meaningful conclusions (Supplementary Fig. S10).
Discussion
We studied i/eot-PET for clinical decision making in the context of the various genetic subtypes, performed as part of the trial protocols of the HOVON-84, PETAL and SAKK-38/07 trials. For all genetic subtypes, a high prognostic value of i/eot-PET positive status could be confirmed. However, the frequency and predictive value of negative i/eot-PET differed between genetic subtypes and thereby its interpretation and potential clinical consequences. Two subtypes in particular were identified that merit discussion.
In our uniformly R-CHOP-treated cohort of DLBCL patients we show that comprehensive genetic subtyping according to DFCI12 or LymphGen14,16 is a significant prognostic factor for outcome independent of IPI. Both DFCI subtype C5 and LymphGen counterpart MCD, as well as DFCI-C2 were identified as poor survival subtypes. We observed that most patients with either DFCI-C5 or Lymphgen-MCD subtype disease are initially responsive to first-line R-CHOP treatment, as reflected by a high fraction of patients that convert to i/eot-PET-negative status. Despite this complete metabolic response (CMR), these patients however have a high relapse rate as shown by PFS and fatal outcome. The disease course of patients with genetic DFCI subtype C2 follows a different pattern; a much higher percentage of these patients remain PET-positive during and after standard R-CHOP treatment. Similar to all other subtypes (except those in subtype C5 or MCD) those DFCI-C2 patients who do respond and reach CMR have long-term remission rates. This indicates that the clinical problem for C2 patients is primary refractory disease, rather than relapse.
The potential of NGS-based genetic profiling in clinical management of DLBCL patients is widely acknowledged. Its optimal position in clinical implementation is still a subject of active debate. Our results indicate that genetic subtyping may be positioned as i) a complement to current IPI-based risk stratification, ii) to direct the interpretation of i/eot-PET for disease monitoring and iii) to serve in the exploration of specific experimental treatment approaches. Obviously, a single and uniform standardized classification of genetic subtypes is thereby critical17,19. CMR as assessed by i/eot-PET predicts a favourable outcome with high NPV justifying standard follow-up protocols and conclusions on potential “cure”. The exception is the C5/MCD subtype that has poor prognosis because of a persistent high risk of relapse despite reaching CMR. This argues for a more personalized approach that may include additional treatment even after reaching CMR on R-CHOP, possibly as some form of maintenance, and/or targeted approaches in first line, such as ibrutinib20. Such alternative treatment options should be explored in a genetic subtype bespoke clinical trial context for which the feasibility has been shown by the GUIDANCE-01 trial21.
High rates of treatment failure on R-CHOP in patients with DFCI-C2 DLBCL may argue for early treatment conversion or immediate experimental programs. For all other patients especially those with low stage/low risk disease, initial treatment with R-CHOP should remain the first treatment choice21. Only those few patients that remain PET-positive may be diverted to genetically-targeted and/or immunologically-directed treatment. For any of the subtypes, response evaluation will play an essential role in timely treatment adaptation for which liquid biopsy monitoring as an alternative or in addition to PET monitoring is likely to find its place in the near future30. Such comprehensive treatment programs will be pivotal to implement new treatments in an efficient, cost-effective, and timely manner.
There are various limitations of this study. First of all, meaningful correlative statistics for the LymphGen classification16 were frequently hindered by the low number of evaluable patients, inherent to the algorithm that classifies only about 50–60% of samples uniquely to one of the subtypes16,17,22. This clearly impacted on the evaluation of LymphGen-A53 patients, the counterpart of DFCI-C2. Another limitation was that for the large PETAL cohort no eot-PET was performed, hindering validation. In clinical practice, eot-PET for response evaluation and outcome prediction is quite widely accepted, whereas the optimal timing and consequences of i-PET are less established31. After 4 cycles of R-CHOP i-PET is more commonly performed, and conceivably after 2 cycles too early as a surrogate marker for response. Nevertheless, despite early i-PET timing in the PETAL trial, and a limited number of SAKK 38/07 study patients, we were able to demonstrate trends towards an adverse clinical outcome for i/eot-PET negative patients with the DFCI-C5 or Lymphgen-MCD genetic subtypes in both these validation cohorts.
We conclude that genetic subtyping confers significant added prognostic value for DLBCL independent of IPI and impacts the predictive value of currently accepted disease monitoring methods, in particular of i/eot PET. Hence, our findings provide a rationale for subtype-directed disease monitoring and personalized subtype-specific clinical trial design for DLBCL patients.
Methods
Patient cohorts and study design
Written informed consent was obtained from all patients, including use of biopsy material for research purposes and the study was approved by the Medical Ethical Committee of Amsterdam UMC, location VUMC (METC2018-556, BUP02015-058) and Medical Ethical Committee of ErasmusMC (METC 2007-055).
This retrospective study was performed for DLBCL-NOS patients treated in the HOVON-84, (Eudra, T-2006-005174-42)32, PETAL33, and SAKK-38/07 (NCT00544219)34 clinical trials, augmented with patients from the DFCI cohort12. The exploratory analyses conducted in this study were not part of the clinical trial’s prospective designs. HOVON-84 and PETAL are randomized phase 3 clinical trials, comparing 6- or 8 cycles of R-CHOP-14 (rituximab, doxorubicin, vincristine, cyclophosphamide, prednisone) with- or without rituximab intensification, for which patient inclusions in this study are summarized in Table 1. After 4 R-CHOP-14 cycles for HOVON-84 and 2 R-CHOP-14 cycles for PETAL i-PET analyses were performed. PET was dichotomized as negative Deauville score DS1-3, or positive DS4-535. IPI was categorized into low (0-1), low-intermediate (2), high-intermediate (3) and high (4-5) risk. Only patients with diagnoses of DLBCL-NOS and cases with DLBCL morphology with a recorded DH/TH genotype (MYC, BCL2 and/or BCL6 double- hit (DH) or (TH) triple-hit rearrangements) were included as per the inclusion criteria of the clinical trial and consistent with the original publications on DFCI12 and LymphGen classifications14,16. Follicular lymphoma grade 3B, primary testicular and central nervous system DLBCL, primary mediastinal B-cell lymphoma and transformed indolent lymphoma were excluded from the present study for consistency with the original publications on DFCI and LymphGen classifications. For clinical correlations, the HOVON-84 and PETAL cohorts were harmonized by exclusion of all patients with stage I disease3,36 and patients receiving any other treatment than R-CHOP-14 (Fig. 1). Patients from the different arms were combined, since significant survival differences were neither observed in the 2 trials32,33, nor in the study selections. We included 304 patients from the DFCI cohort12. For the DFCI patients, IPI but no PET data was available. Only DFCI patients treated with R-CHOP of which outcome data was available (n = 249) were used for survival analysis (Fig. 1).
SAKK-38/07 is a single arm prospective clinical trial, evaluating the prognostic impact of i-PET after 2- and 4 cycles of R-CHOP-14 and 6 cycles eot-PET. Of the 138 SAKK-38/07 patients 76 could be included in this study as an extra validation that fulfilled the inclusion/exclusion criteria listed above.
Genomics data
For 274 of the 574 patients enrolled in the HOVON-84 trial32 pre-treatment formalin-fixed paraffin-embedded (FFPE) tumor biopsy samples could be retrieved and 235 FFPE tumor biopsies of the 609 patients enrolled in the PETAL trial33 for which genomic DNA was extracted using the DNA FFPE Tissue Kit (Qiagen, Hilden, Germany). For 55 of the PETAL patients matched normal blood samples were available for which DNA was extracted using the DNA Mini Blood Kit (Qiagen, Hilden, Germany). For the HOVON-84 DNA samples ultrasound fragmentation was performed (Covaris ME220 Focused-Ultrasonicator, Covaris Inc.,Wob urn, MA) and for the PETAL DNA samples enzymatic fragmentation, both followed by NGS library preparation (KAPA HyperPlus Library Preparation, KAPA Biosystems, Wilmington, MA). Subsequently, shallow whole genome sequencing (sWGS) was performed for genome-wide copy number aberration (CNA) analysis on a HiSeq 2500 (Illumina San Diego, CA)37. Mutations and translocations for HOVON-84 were identified with a targeted NGS protocol of 369 genes and 12 common translocation breakpoint regions using a custom SeqCapEZ target probe panel (Supplementary Data S2) (Roche Nimblegen, Madison, WI)38. The PETAL samples were subjected to whole exome sequencing (WES) using the KAPA HyperExome Prep Kit (KAPA Biosystems, Wilmington, MA) to identify mutations. For 44 of the PETAL samples, the translocation status was complemented using the targeted NGS panel. NGS data was deposited at the European Genome-phenome Archive39 (HOVON-84: EGAS00001003949, PETAL: EGAS00001005828).
Chromosomal breaks were assessed for MYC, BCL6 and BCL2 with standard break-apart fluorescence in situ hybridization (FISH) and MYC::IGH fusion FISH on tissue microarray (Abbott molecular, Vysis, Chicago IL, USA)40. Results were evaluated according to criteria validated for diagnostic purposes in daily pathology practice with a cut-off value of >7.5% of evaluable nuclei with FISH break-apart patterns consistent with breaks to be scored as positive. Immunohistochemistry (IHC) was performed by the HOVON Pathology Facility and Biobank and/or the original pathology laboratories as part of the central pathology review, including at least CD20, CD3, MIB1, BCL2, CD10, BCL6, MUM141. Positive translocation status determined by either NGS or FISH was considered a positive result.
To dichotomize samples in Germinal Center B Cell-like (GCB) and non-GCB, immunohistochemistry for CD10, BCL6 and MUM1 was evaluated using the Hans algorithm42 as part of the pathology review. This was supplemented by digital gene expression with the Lymph2Cx assay (nCounter®, Nanostring, Seattle, WA, USA).
As a quality criterion for sample exclusion, CNA, mutation and translocation data were used as follows; samples with any positive MYC, BCL2 or BCL6 translocation status as determined by FISH or NGS were included. Samples with a tumor purity less than 20% as estimated from CNA data using ACE(v1.17.0)43 were excluded if; (I) a median (mutation) variant allele frequency higher than 0.3 was observed and (II) less than 30 variants were called. Based on these criteria, N = 208 HOVON84 samples and N = 204 remained for downstream analysis (Fig. 1).
Mutation, CNA, and translocation data of all 304 DFCI patients were included for genetic subtyping12. DFCI patients with no detected alterations (C0) and with the N1 Lymphgen subtype were excluded for downstream analysis. For 76 of the 138 patients enrolled in the SAKK-38/07 trial34, NGS amplicon-based mutation status of 68 genes and FISH of MYC and BCL2 translocation status were included44. CNA analysis was not performed for the SAKK-38/07 trial patients.
Bioinformatic procedures for targeted and shallow whole genome sequencing
For HOVON-84 samples a panel-of-normal (PON) from 25 non-tumor DNA samples isolated from FFPE biopsy samples retrieved from the archives of the Department of Pathology, AmsterdamUMC/VUMC, Amsterdam, was used to exclude germline single nucleotide polymorphisms (SNPs) and platform-specific artifacts38. For PETAL samples, a PON consisting of 138 non-tumor FFPE biopsy samples retrieved from the data archives of the Department of Pathology, AmsterdamUMC/VUMC, Amsterdam were used as well as the 55 matched-normal PETAL samples. To ensure conformity between mutation data from HOVON-84 and PETAL, the PETAL WES data was reduced to the 369 genes of the custom SeqCapEZ target panel (Supplementary Data S2). We applied a tumor-only pipeline to identify somatic mutations. Single-nucleotide variants (SNVs) that were detected by both LoFreq (v2.1.3.1)45 and VarScan (v.2.3.7)46 were considered as germline SNPs, when i) present in the dbSNP database (build 142) with a minor allele frequency above 0.001 and/or ii) present in at least 4 out of 1762 cases from the reference whole genome sequencing database of healthy individuals in the Dutch population (Hartwig Medical Foundation, Amsterdam, The Netherlands) and iii) present in at least 2 out of 25 and 3 out of 193 in HOVON-84 and PETAL non-tumor control samples from the PON respectively. Only the SNVs detected by both LoFreq and VarScan that remained after all 3 filters were considered genuine somatic mutations. To filter low allele frequency FFPE artifacts in the PETAL data, the variant allele frequency cut-off was decreased to 2.5% for inclusion into the PON and base changes detected in 6 out of 216 PETAL tumor samples which occurred exclusively with a variant allele frequency below 25% were filtered. Structural variants were detected using the overlap in four different algorithms, including BreaKmer (v0.04), GRIDSS (v1.4.2), wham (v1.7.0) and novoBreak (v1.1.3)47,48,49,50. Structural variants detected by at least 2 of the 4 algorithms were selected51. CNA calling was performed using the shallow whole genome sequencing data and the QDNAseq algorithm (v1.5.1)37.
Clustering, cluster adherence and classification
To (re-)assign each sample to either of the C1- through C5 DFCI clusters, we performed non-negative matrix factorization (NMF)12. Thereto, we first combined the data of the HOVON-84 and PETAL samples, with the data of the DFCI sample series (ntotal=716) in one matrix (Supplementary Data S5). From the 158 genetic alterations that were present in the gene sample matrix of the original DFCI clustering12 130 were available in our dataset; 62 SNVs, 65 CNAs and 3 translocations. Similar weights as described in the original 5-class molecular classification were assigned to each of the genomic alterations and NMF was performed using the identical scripts52(https://github.com/broadinstitute/DLBCL_Nat_Med_April_2018.git). To define NMF cluster stability, cluster adherence was determined per sample by performing 1000 clustering iterations with each time 80% subsampling19,53. Samples were defined as ‘core samples’ if recurrently assigned to the same cluster indicating samples with prototypical genetic features for the specific DFCI subtype19. Thereto for each sample pair, the frequency of occurring in the same cluster (hereafter referred to as cluster adherence) was calculated. A Gaussian mixture model was fitted to the cluster adherence for each of the 5 clusters independently. Two components were fitted to distinguish ‘core’ from ‘non-core’ samples and Gaussian parameters were estimated using Bayesian inference with independent priors implemented in the Bayesmix R package (v0.7.5) (http://CRAN.R-project.org/package=bayesmix).
For the 76 DLBCL patients of the SAKK 38/07 trial, a limited number of genetic determinants was available, and particularly CNA data lacked completely. Therefore, this data was insufficient to reliably assign samples to each of the 5 DFCI clusters by NMF clustering. Instead, we trained a classifier to reliably distinguish C5 DLBCLs from the other 4 DLBCL clusters, referred to as non-C5. Here, a binary classifier was trained by logistic regression (glmnet R package v2.0.18) with 28 of the 130 genetic features available in the SAKK38/07 cohort using only ‘core’ DFCI samples, blinded for IPI, i/eot-PET and survival data. Of note, since only MYD88-L265P mutation information was available in the SAKK38/07 cohort, all other variant MYD88 mutations were omitted for training and validation. We used lasso regularization (alpha=1) with the logistic function as the linkage. To optimize performance, sample weights were assigned to the model by multiplying cluster adherence by 4 for C5 cases and by 1 for non-C5 cases. A 10-fold cross-validation scheme was used to measure the performance of the classifier in an unbiased manner, and the model with the best performance in terms of area under the curve (AUC) was selected as the final model. Performance was validated on the HOVON-84 and PETAL sample data resulting in an AUC of 0.90 and 0.88 respectively. The classifier was then applied to assign C5 vs non-C5 for the 76 SAKK-38/07 samples.
Next to DFCI subtypes, also LymphGen genetic subtypes were determined for all HOVON-84 and PETAL cases using the standard LymphGen algorithm16 (https://zenodo.org/record/3700087#.YxickEdBxaQ). For the DFCI cohort, the LymphGen genetic subtype assignments from the original study were used16.
PET/CT analysis
For all DLBCL patients from the HOVON-84, PETAL and SAKK-38/07 clinical trials that were analysed in this study, 18fluorodeoxyglucose-positron emission tomography (PET) scores were dichotomized based on the 5-point Deauville scoring system. Deauville scores 1-3 were considered as negative, and Deauville scores 4-5 were considered as positive35. For HOVON-84 and SAKK-38/07 patients in our study cohort with unavailable eot-PET scores, values were imputed based on available i-PET scores as follows. In HOVON-84: 12 missing eot-PET scores were imputed based on 5 positive i-PET4 scores and 7 negative i-PET4 scores. In SAKK-38/07: 6 missing eot-PET scores were imputed based on 1 positive i-PET4 scores and 5 negative i-PET4 scores. Also, in SAKK-38/07: 30 missing i-PET4 scores were imputed based on 9 positive i-PET2 scores and 21 negative i-PET2 scores.
Statistics & Reproducibility
Overall Survival (OS) was defined as time from start of treatment until death from any cause. Subjects not confirmed dead were censored at the time last known to be alive. Progression-Free Survival (PFS) was defined as the time from start of treatment until lymphoma progression or death from any cause and censored at time last known to be alive and free of progression. Comparison between groups were performed using the log-rank test. Hazard ratio’s (HRs) and 95% confidence intervals (CIs) were determined for each endpoint. Univariate- and multivariable analyses of time-to-event endpoints were performed using Cox regression. Self-reported sex was taken along as a covariate in this study and did not influence study design. Global significance of categorical variables in multivariate analysis was tested using an Cox regression ANOVA model. Negative predictive value (NPV) was defined as probability of PFS at 2 years for eot-PET negative patients. Fisher’s exact test was used to test for association between categorical variables. The Kruskal-Wallis test was performed to assess a shift in distribution between continuous variables. Reported P-values were 2-sided for all primary analyses with a significance threshold of 0.05. No randomization was performed and no statistical method was used to predetermine sample size. Sample exclusions are presented in Fig. 1. All statistical analyses were performed with R software (v3.3.1) with additional R-packages survival (v2.40-1), survminer (v0.4.3) and powerSurvEpi (v0.1.0).
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
The raw sequencing data generated in this study have been deposited in the EGA database under accession code EGAS00001003949 and EGAS00001005828 and available under restricted access upon written application and signature of a Data Access Agreement (DAA) to the Data Access Committee EGAC0000100018 who evaluate according to the Data Access Policy, EGAP00001000188 whether the proposed work is allowed given patient consent, as well as the scientific purpose. All processed sequencing data is available in the supplementary files of this paper. Publicly available data from the DFCI and SAKK datasets were retrieved from the supplementary files of the articles; for DFCI https://static-content.springer.com/esm/art%3A10.1038%2Fs41591-018-0016-8/MediaObjects/41591_2018_16_MOESM4_ESM.xlsx and https://static-content.springer.com/esm/art%3A10.1038%2Fs41591-018-0016-8/MediaObjects/41591_2018_16_MOESM10_ESM.xlsx)12 and for SAKK https://static-content.springer.com/esm/art%3A10.1186%2Fs13045-017-0438-7/MediaObjects/13045_2017_438_MOESM1_ESM.xlsx44. Source data are provided with this paper.
Code availability
Pipelines used for the preprocessing of NGS data can be found on Github: (I) code used for processing of CNA data can be found at https://github.com/tgac-vumc/QDNAseq.snakemake54, (II) code used for processing of mutation data can be found at https://github.com/tgac-vumc/tumor-only-snakemake55 and (III) code used for processing of translocation data can be found at https://github.com/tgac-vumc/translocation-snake56. The code associated to these repositories are available without restrictions under an MIT license. Original code for NMF clustering presented by Chapuy et al. 12 is freely available through GitHub (https://github.com/broadinstitute/DLBCL_Nat_Med_April_2018) under no licence and is used following the code of conduct of the maintainers.
References
Shipp, M. A. & Harrington, D. P. A predictive model for aggressive non-Hodgkin’s lymphoma. N. Engl. J. Med. 329, 987–994 (1993).
Campo, E. et al. The International Consensus Classification of Mature Lymphoid Neoplasms: a report from the Clinical Advisory Committee. Blood 140, 1229–1253 (2022).
Alaggio, R. et al. The 5th edition of the World Health Organization Classification of Haematolymphoid Tumours: Lymphoid Neoplasms. Leukemia 36, 1720–1748 (2022).
Van Imhoff, G. W. et al. Ofatumumab versus rituximab salvage chemoimmunotherapy in relapsed or refractory diffuse large B-cell lymphoma: The ORCHARRD study. J. Clin. Oncol. 35, 544–551 (2017).
Gisselbrecht, C. & Van Den Neste, E. How I manage patients with relapsed/refractory diffuse large B cell lymphoma. Br. J. Haematol. 182, 633–643 (2018).
Liu, Y. & Barta, S. K. Diffuse large B-cell lymphoma: 2019 update on diagnosis, risk stratification, and treatment. Am. J. Hematol. 94, 604–616 (2019).
Tilly, H. et al. Polatuzumab Vedotin in Previously Untreated Diffuse Large B-Cell Lymphoma. N. Engl. J. Med. 386, 351–363 (2022).
Davies, A. et al. Gene-expression profiling of bortezomib added to standard chemoimmunotherapy for diffuse large B-cell lymphoma (REMoDL-B): an open-label, randomised, phase 3 trial. Lancet Oncol. 20, 649–662 (2019).
Younes, A. et al. Randomized phase III trial of ibrutinib and rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone in non–germinal center B-cell diffuse large B-cell lymphoma. J. Clin. Oncol. 37, 1285–1295 (2019).
Vitolo, U. et al. ROBUST: First report of phase III randomized study of lenalidomide/R-CHOP (R 2 -CHOP) vs placebo/R-CHOP in previously untreated ABC-type diffuse large B-cell lymphoma. Hematol. Oncol. 37, 36–37 (2019).
Davies, A. J. et al. Differential Efficacy From the Addition of Bortezomib to R-CHOP in Diffuse Large B-Cell Lymphoma According to the Molecular Subgroup in the REMoDL-B Study With a 5-Year Follow-Up. J. Clin. Oncol. 41, 2718–2723 (2023).
Chapuy, B. et al. Molecular subtypes of Diffuse Large B-cell Lymphoma are associated with distinct pathogenic mechanisms and outcomes. Nat. Med. 24, 679–690 (2018).
Reddy, A. et al. Genetic and Functional Drivers of Diffuse Large B Cell Lymphoma. Cell 171, 481–494 (2017).
Schmitz, R. et al. Genetics and Pathogenesis of Diffuse Large B-Cell Lymphoma. N. Engl. J. Med. 378, 1396–1407 (2018).
Lacy, S. E. et al. Targeted sequencing in DLBCL, molecular subtypes, and outcomes: a Haematological Malignancy Research Network report. Blood 135, 1759–1771 (2020).
Wright, G. W. et al. A Probabilistic Classification Tool for Genetic Subtypes of Diffuse Large B Cell Lymphoma with Therapeutic Implications. Cancer Cell 37, 551–568.e14 (2020).
Mendeville, M. et al. The path towards consensus genome classification of diffuse large B-cell lymphoma for use in clinical practice. Front. Oncol. 12, 970063 (2022).
Sehn, L. H., Salles, G., LH, S. & G, S. Diffuse Large B-Cell Lymphoma. N. Engl. J. Med. 384, 842–858 (2021).
Mendeville, M. et al. A bioinformatics perspective on molecular classification of diffuse large B-cell lymphoma. Leukemia 36, 2177–2179 (2022).
Wilson, W. H. et al. Effect of ibrutinib with R-CHOP chemotherapy in genetic subtypes of DLBCL. Cancer Cell 39, 1643–1653.e3 (2021).
Nastoupil L. J. & Bartlett N. L. Navigating the Evolving Treatment Landscape of Diffuse Large B-Cell Lymphoma. J. Clin. Oncol. 41, 903–913 (2023).
Runge, H. F. P. et al. Application of the LymphGen classification tool to 928 clinically and genetically-characterised cases of diffuse large B cell lymphoma (DLBCL). Br. J. Haematol. 192, 216–220 (2021).
Bolen, C. R. et al. Prognostic impact of somatic mutations in diffuse large B-cell lymphoma and relationship to cell-of-origin: data from the phase III GOYA study. Haematologica 105, 2298–2307 (2019).
Dubois, S. et al. Refining diffuse large B-cell lymphoma subgroups using integrated analysis of molecular profiles. EBioMedicine 48, 58–69 (2019).
Mikhaeel, N. G. et al. Proposed New Dynamic Prognostic Index for Diffuse Large B-Cell Lymphoma: International Metabolic Prognostic Index. J. Clin. Oncol. 40, 2352–2360 (2022).
Eertink, J. J. et al. Optimal timing and criteria of interim PET in DLBCL: a comparative study of 1692 patients. Blood Adv. 5, 2375–2384 (2021).
Barrington, S. F. & Mikhaeel, N. G. PET Scans for Staging and Restaging in Diffuse Large B-Cell and Follicular Lymphomas. Curr. Hematol. Malig. Rep. 11, 185–195 (2016).
Dreval, K., Boutros, P. C. & Morin, R. D. Minimal information for reporting a genomics experiment. Blood 140, 2549–2555 (2022).
Ennishi, D., Hsi, E. D., Steidl, C. & Scott, D. W. Toward a New Molecular Taxonomy of Diffuse Large B-cell Lymphoma. Cancer Discov. 10, 1267–1281 (2020).
Kurtz, D. M. et al. Noninvasive monitoring of diffuse large B-cell lymphoma by immunoglobulin high-throughput sequencing. Blood 125, 3679–3687 (2015).
Spinner, M. A. & Advani, R. H. Current Frontline Treatment of Diffuse Large B-Cell Lymphoma. Oncology 36, 51–58 (2022).
Lugtenburg, P. J. et al. Rituximab-CHOP With Early Rituximab Intensification for Diffuse Large B-Cell Lymphoma: A Randomized Phase III Trial of the HOVON and the Nordic Lymphoma Group (HOVON-84). J. Clin. Oncol. 38, 3377–3387 (2020).
Dührsen, U. et al. Positron emission tomography-guided therapy of Aggressive Non-Hodgkin Lymphomas (PETAL): A multicenter, randomized phase III trial. J. Clin. Oncol. 36, 2024–2034 (2018).
Tzankov, A. et al. Multiparameter analysis of homogeneously R-CHOP-treated diffuse large B cell lymphomas identifies CD5 and FOXP1 as relevant prognostic biomarkers: report of the prospective SAKK 38/07 study. J. Hematol. Oncol. 8, 70 (2015).
Barrington, S. F. et al. Role of imaging in the staging and response assessment of lymphoma: consensus of the International Conference on Malignant Lymphomas Imaging Working Group. J. Clin. Oncol. 32, 3048–3058 (2014).
Swerdlow S. H., et al. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. WHO Ser. Histol. Genet. typing Hum. tumours (2017).
Scheinin, I. et al. DNA copy number analysis of fresh and formalin-fixed specimens by shallow whole-genome sequencing with identification and exclusion of problematic regions in the genome assembly. Genome Res. 24, 2022–2032 (2014).
Mendeville et al. Aggressive genomic features in clinically indolent primary HHV8-negative effusion-based lymphoma. Blood 133, 377–380 (2019).
Freeberg et al. The European Genome-phenome Archive in 2021. Nucleic Acids Res 50, D980–D987 (2022).
van den Brand, M. et al. A subset of low-grade B cell lymphomas with a follicular growth pattern but without a BCL2 translocation shows features suggestive of nodal marginal zone lymphoma. J. Hematop. 9, 3–8 (2016).
Rayman, N. et al. Prognostic relevance of immunohistochemical subclassification of diffuse large B-cell lymphoma in two prospective phase III clinical trials. Clin. Lymphoma, Myeloma Leuk. 11, 23–32 (2011).
Hans, C. P. et al. Confirmation of the molecular classification of diffuse large B-cell lymphoma by immunohistochemistry using a tissue microarray. Blood 103, 275–282 (2004).
Poell, J. B. et al. ACE: absolute copy number estimation from low-coverage whole-genome sequencing data. Bioinformatics 35, 2847–2849 (2019).
Juskevicius, D. et al. Mutations of CREBBP and SOCS1 are independent prognostic factors in diffuse large B cell lymphoma: mutational analysis of the SAKK 38/07 prospective clinical trial cohort. J. Hematol. Oncol. 10, 70 (2017).
Wilm, A. et al. LoFreq: A sequence-quality aware, ultra-sensitive variant caller for uncovering cell-population heterogeneity from high-throughput sequencing datasets. Nucleic Acids Res. 40, 11189–11201 (2012).
Koboldt, D. C. et al. VarScan 2: Somatic mutation and copy number alteration discovery in cancer by exome sequencing VarScan 2: Somatic mutation and copy number alteration discovery in cancer by exome sequencing. Genome Res. 22, 568–576 (2012).
Abo, R. P. et al. BreaKmer: detection of structural variation in targeted massively parallel sequencing data using kmers. Nucleic Acids Res 43, e19 (2015).
Chong, Z. et al. NovoBreak: Local assembly for breakpoint detection in cancer genomes. Nat. Methods 14, 65–67 (2016).
Cameron, D. L. et al. GRIDSS: Sensitive and specific genomic rearrangement detection using positional de Bruijn graph assembly. Genome Res 27, 2050–2060 (2017).
Kronenberg, Z. N. et al. Wham: Identifying Structural Variants of Biological Consequence. PLoS Comput. Biol. 11, 1–19 (2015).
Allahyar A. et al. Robust detection of translocations in lymphoma sequencing. Nat. Commun. 12, 3361 (2021).
Brunet, J. P., Tamayo, P., Golub, T. R. & Mesirov, J. P. Metagenes and molecular pattern discovery using matrix factorization. Proc. Natl Acad. Sci. Usa. 101, 4164–4169 (2004).
Monti, S., Tamayo, P., Mesirov, J. & Golub, T. Consensus clustering: A resampling-based method for class discovery and visualization of gene expression microarray data. Mach. Learn. 52, 91–118 (2003).
Tumor Genome Analysis Core, Integrating Genetic Subtypes with PET Scan Monitoring to Predict Outcome in Diffuse Large B-Cell Lymphoma, qDNAseq-snakemake. https://doi.org/10.5281/zenodo.13969159 (2024).
Mendeville M. Integrating Genetic Subtypes with PET Scan Monitoring to Predict Outcome in Diffuse Large B-Cell Lymphoma, tumor-only-snakemake. https://doi.org/10.5281/zenodo.13969165 (2024).
Los-de Vries T. Integrating Genetic Subtypes with PET Scan Monitoring to Predict Outcome in Diffuse Large B-Cell Lymphoma, translocation-snakemake. https://doi.org/10.5281/zenodo.13969169 (2024).
Acknowledgements
We thank Paul P. Eijk, H. (Dirk) F. B. van Essen and Daoud Sie, from the Tumor Genomic Analyses Core (www.tgac.nl) of the Amsterdam UMC, location VUmc (Amsterdam, the Netherlands), for their help and advice with the NGS experiments, and Jeroen Maertzdorf (from the same affiliation) and Bjoern Chapuy (Department of Hematology, Oncology and Tumorimmunology, Charité Universität, Berlin, Germany) for critically reviewing the manuscript prior to submission. We thank King H. Lam from the Department of Pathology, Erasmus MC (Rotterdam, the Netherlands) and Philip M. Kluin from the Department of Pathology, UMCG Groningen (Groningen, the Netherlands) for stimulating discussions. We thank the HOVON data center for central data management. We would like to acknowledge the support provided by Dr Staudt’s Laboratory at NCI/NIH Bethesda (Maryland, USA), for online analyses of Lymph2Cx raw data for COO characterization. We thank the Hartwig Medical Foundation (Amsterdam, The Netherlands) for generating, analysing and providing access to reference whole genome sequencing data of the Netherlands population. This work was supported by the Dutch Cancer Society grant KWF 2012-5711, KWF 2013-6269 and KWF 2015-7925 to B.Y. and D.d.J. Funders had no role in the study design, material collection, the analyses or interpretation of the data, the writing of the manuscript, or the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
M.S.M., J.J., G.T.L.d.V., E.v.D., and Y.K. analyzed the data. M.G.M.R, P.S., N.J.H., R.B. and D.A.P., performed experimental work. D.d.J., A.D., A.v.d.B., C.J.E., C.N.B., J.M.Z., P.J.L., U.D., A.H. J.R. and W.K., contributed pathology materials and data, clinical annotations and PET data for the HOVON84 and PETAL clinical trials. A.T. and S.D. contributed NGS and PET data for the SAKK clinical trial. B.Y. and D.d.J. designed the study The manuscript was written by M.S.M., J.J., G.T.L.d.V., M.N., B.Y. and D.d.J., and was critically evaluated and approved by all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks the anonymous, reviewers for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Mendeville, M.S., Janssen, J., Los-de Vries, G.T. et al. Integrating genetic subtypes with PET scan monitoring to predict outcome in diffuse large B-cell lymphoma. Nat Commun 16, 109 (2025). https://doi.org/10.1038/s41467-024-55614-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-024-55614-y