Abstract
Associations between long-term exposure to nitrogen oxides (NOx) and cause-specific mortality remain insufficiently explored. This study utilizes data from 502,040 participants registered in the UK Biobank. Time-varying Cox regression is used to estimate mortality risks associated with NOx. Cause-specific mortality risks, including non-accidental, accidental and 15 major disease categories across 103 subcategories, are assessed for each 10 μg/m3 increase in NOx. Positive associations are observed between NOx and mortality from all-cause (HR: 1.036; 95% CI: 1.024, 1.049) and non-accidental diseases (HR: 1.032; 95% CI: 1.019, 1.045). We further identify 20 specific diseases related to NOx, notably respiratory diseases, mental and behavioral disorders, and circulatory diseases, with generally linear exposure-response relationships. Sex and residential areas are potential modifiers of the observed associations. Our findings suggest long-term exposure to NOx may increase mortality risks from a range of diseases, emphasizing the urgent need for clean air policies to alleviate the health burden.
Similar content being viewed by others
Introduction
Long-term exposure to nitrogen oxides (NOx) and nitrogen dioxide (NO2) have continued to pose a substantial threat to global public health, even in regions with low air pollution concentrations1. NOx consisting mainly of nitric oxide (NO) and NO2 serves as a critical precursor in photochemical reactions leading to ozone (O3) formation and secondary inorganic aerosols2,3, posing significant threats to human health. High NOx emissions from light-duty diesel vehicles in Europe in 2013 were responsible for up to 10,000 premature deaths4, supporting that reducing NOx emissions could have substantial health implications. The control of NOx emissions might also contribute to the mitigation of population exposure to fine particulate matter (PM2.5) and O35. Nevertheless, research on the health effects of NOx remains limited and the broad disease spectrum that might be affected by NOx has not been fully characterized. An extensive literature review conducted in the preliminary stage of our study indicated that long-term exposure to NOx and NO2 might be associated with mortality from certain diseases, mainly cardiovascular diseases, chronic respiratory conditions, and pulmonary carcinoma6,7 (Supplementary Fig. S1). However, the distinct impacts of NOx on cause-specific mortality, particularly regarding diseases beyond cardiorespiratory conditions, remain inadequately explored. Therefore, there is a critical gap in understanding the full spectrum of health effects associated with NOx exposure, necessitating a comprehensive examination to elucidate their broader implications and explore potential exposure-response relationships.
Here, we analyze a cohort data comprising over 500,000 participants in the UK Biobank (UKB) from 2006 to 2022. Time-varying covariates Cox proportional hazards models are employed to examine the impact of atmospheric NOx exposure on deaths from all-cause, non-accidental cause, accidental cause, 15 main causes and 103 specified subcategories diseases. Furthermore, we explore the potential exposure-response relationships and conduct stratification analyses by age, sex and regional characteristics. We find that long-term exposure to NOx is associated with increased mortality risks of all-cause, non-accidental diseases, and 20 specific diseases. Associations between NOx and cause-specific mortality are generally linear. Sex and residential area seem to be the effect modifiers of NOx-mortality associations. The findings may inform the development of stricter air quality regulations to control atmospheric NOx levels, and provide evidence for developing adaptive strategies to mitigate the social inequalities in public health.
Results
Descriptive data
Baseline characteristics of the participants and air pollutants exposure are shown in Table 1. A total of 502,040 participants with an average age of 56.5 [standard deviation (SD): 8.1] years at the baseline were included in the final analyses, with 54.4% being female. During a median follow-up of 13.7 years, 44,090 individuals died from all-causes, and 1297 participants were lost to follow-up. Compared to the study subjects who survived until the end of follow-up, deceased participants were more likely to be older, male, white, and urban residents, with a higher proportion of them possessing lower household income, having lower educational attainment, and belonging to retired demographics. The prevalence of smoking, obesity, and low physical activity levels was also higher in the deceased group.
Temporal and spatial trends in nitrogen oxides
During 2006–2022, the average concentrations (SD) of NOx and NO2 were 24.5 (11.8) μg/m3 and 16.6 (6.6) μg/m3, respectively. The concentrations of NOx exhibited an overall declining trend but manifested large spatial variations (Supplementary Figs. S2–S4). NOx exhibited the highest yearly average exposure in 2006 (38.9 μg/m3). Supplementary Fig. S5 illustrates the Spearman’s correlation coefficients (rs) among air pollutants. NOx exhibited positive correlations with PM2.5, particulate matter with aerodynamic diameter ≤ 10 μm (PM10) and sulfur dioxide (SO2) (rs = 0.434–0.777).
Effects of nitrogen oxides on mortality from major categories of diseases
Table 2 shows effects of NOx on mortality from 18 broad categories of diseases. Hazard ratios (HRs) for all-cause mortality associated with per 10 μg/m3, SD (11.75 μg/m3) and interquartile range (IQR) (14.16 μg/m3) increases in NOx were 1.036 [95% confidence interval (CI): 1.024, 1.049], 1.043 (95% CI: 1.028, 1.058), and 1.052 (95% CI: 1.034, 1.070), respectively. Regarding non-accidental diseases, the HR was 1.032 (95% CI: 1.019, 1.045) with each 10 μg/m3 increase in NOx. Across the 15 major cause-specific categories, elevated hazards per 10 μg/m3 increase in NOx levels were observed for respiratory diseases (HR: 1.139; 95% CI: 1.090, 1.190), mental and behavioral disorders (HR: 1.096; 95% CI: 1.002, 1.199), and circulatory diseases (HR: 1.043; 95% CI: 1.015, 1.072). Moreover, the notably increased risks associated with NOx were observed for those who died from other symptoms, signs and abnormal findings, as well as external causes. Supplementary Table S1 shows effect estimates of NO2 on mortality from major disease categories. We found significant associations between NO2 and mortality from aforementioned diseases, except for other symptoms, signs and abnormal findings.
Effects of nitrogen oxides on mortality from specific subcategories of diseases
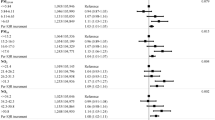
Among 103 subcategories of cause-specific mortality, NOx was linked to mortality risk of 15 types of disease (Fig. 1 and Supplementary Table S2). The NOx-related diseases comprised other peripheral vascular diseases (ICD-10: I73), hypertensive heart disease (I11), phlebitis and thrombophlebitis (I80), accidental poisoning by and exposure to noxious substances (accidental poisoning) (X40-X49), event of undetermined intent (Y10-Y34), fibrosis and cirrhosis of liver (K74), other chronic obstructive pulmonary disease (COPD) (J44), intentional self-harm (suicide) (X60-X84), COVID-19 (U07.1), malignant neoplasm of lip, oral cavity and pharynx (C00-C14), malignant neoplasm of bladder (C67), unspecified dementia (F03), pneumonia (J12-J18), malignant neoplasm of esophagus (C15), and chronic ischemic heart disease (I25), with HRs ranging from 1.075 to 1.342 for each 10 μg/m3 increase in NOx. For NO2, we observed that mortality from 14 types of disease were significantly associated with this pollutant, with HRs ranging from 1.137 to 1.790 (Supplementary Table S2).
Time-varying Cox regression was used to assess the associations between NOx and mortality, with the adjustment of age, sex, ethnicity, body mass index, education, occupation, smoking status, alcohol consumption, physical activity, residential area, and household income. Dots represent the estimated hazards ratios for mortality risk associated with per 10 μg/m3 increase in NOx, and horizontal lines denote corresponding 95% confidence intervals. Two-sided P values less than 0.05 were considered as statistically significant. Asterisk (*) denotes P < 0.05. Source data for Fig. 1 are provided as Source Data 1.
Effects of nitrogen oxides on mortality from common subcategories of diseases
Supplementary Table S3 shows effect estimates for several common causes of death, which are often examined in previous studies on health impact of air pollution. Statistically significant associations were identified for mortality from hypertension (I10-I15), COPD (J40-J44), chronic lower airway disease (J40-J47), and ischemic heart disease (I20-I25). The HRs ranged from 1.041 to 1.250 for each 10 μg/m3 increase in NOx, and from 1.071 to 1.554 for each 10 μg/m3 increase in NO2. We found no association of NOx or NO2 with mortality from lung cancer (C33-C34), cardiac arrest, heart failure (I30-I51), cerebrovascular disease (I60-I69), or asthma (J45-J46).
Exposure-response relationships between nitrogen oxides and mortality
Figure 2 depicts exposure-response curves between NOx and all-cause and cause-specific mortality. A linear and monotonical increase associated with NOx was found for mortality from all-cause, non-accidental, circulatory diseases, respiratory diseases, esophageal cancer, chronic ischemic heart disease, phlebitis and thrombophlebitis, pneumonia, and other COPD, without discernible thresholds (Supplementary Tables S4–S5). Conversely, non-linear associations between NOx and mortality were observed for outcomes of mental and behavioral disorders, hypertensive heart disease, COVID-19, intentional self-harm, and other symptoms, signs, and abnormal findings. Supplementary Fig. S6 indicates similar exposure-response curves between NO2 and cause-specific mortality as NOx.
Associations were assessed utilizing a restricted cubic spline function with 3 knots in time-varying Cox regression, with the adjustment of age, sex, ethnicity, body mass index, education, occupation, smoking status, alcohol consumption, physical activity, residential area, and household income. The minimum concentration of NOx was 0.68 μg/m3, which served as the reference. The lines represent the point estimates, and shaded areas indicate corresponding 95% confidence intervals. The dashed vertical lines are 25th and 75th percentiles of NOx (16.27 μg/m3 and 30.42 μg/m3). Source data for Fig. 2 are provided as Source Data 2.
Subgroup-specific effect estimates of nitrogen oxides on mortality
Figure 3 compares the subgroup-specific risk estimates of all-cause and cause-specific mortality with long-term exposure to NOx, stratified by age, sex, and regional characteristics. A greater effect estimate of NOx on mortality from mental and behavioral disorders was observed in the females, with HR of 1.229 (95% CI: 1.074, 1.407) per 10 μg/m3 increase, compared to the males (P value of 0.037 for the difference test). For residential area, we observed a notably heightened risk of NOx on mortality from fibrosis and cirrhosis of liver in urban areas, but greater risks for pneumonia and accidental poisoning in rural settings. Additionally, we observed that the impact of NO2 on mortality from accidental poisoning was more pronounced in the youth (≤ 65 years) compared to those aged > 65 years (Supplementary Tables S6–S8).
a Models (time-varying Cox regression) adjusted for sex, ethnicity, body mass index, education, occupation, smoking status, alcohol consumption, physical activity, residential area, and household income. b Models adjusted for age, ethnicity, body mass index, education, occupation, smoking status, alcohol consumption, physical activity, residential area, and household income. c Models adjusted for age, sex, ethnicity, body mass index, education, occupation, smoking status, alcohol consumption, physical activity, and household income. Dots represent the estimated hazards ratios for mortality risk associated with per 10 μg/m3 increase in NOx, and vertical lines denote corresponding 95% confidence intervals. The P values are the difference tests between subgroups by the Z-test. Two-sided P values less than 0.05 were considered as statistically significant. Source data for Fig. 3 are provided as Source Data 3.
Sensitivity analyses
Supplementary Tables S9–S18 show the results of sensitivity analyses. Effect estimates remained generally similar when implementing double-pollutant model, integrating additional covariates related to history of chronic diseases, excluding certain individual-level covariates, excluding participants with follow-up durations of less than two years, applying time-varying exposures on extended scale of 5-year average for NOx, limiting to a maximum of ten year follow-up period, employing multiple imputation, excluding participants who exhibited residential mobility, and excluding outliers of NOx concentrations. After excluding the COVID-19 period, effect estimates of NOx on deaths from mental and behavioural disorders (including unspecified dementia), circulatory diseases (including other peripheral vascular diseases), lip, oral cavity and pharynx cancer, bladder cancer, and fibrosis and cirrhosis of liver became statistically insignificant. After false discovery rate (FDR) correction, positive associations remained between NOx exposure and hypertension, hypertensive heart disease, ischemic heart disease, phlebitis and thrombophlebitis, COPD, chronic lower airway disease, COVID-19, and intentional self-harm (all with q values < 0.1, Supplementary Tables S2–S3).
Discussion
This is a large-scale study to conduct a pioneering and comprehensive assessment of the impact of long-term exposure to ambient NOx on mortality, encompassing both all-cause and a wide range of specific causes, thereby expanding our knowledge on the spectrum of mortality associated with nitrogen oxides and uncovering additional potential disease mortality links. Overall, long-term exposure to NOx exhibited statistically significant associations with increased mortality risk of all-cause, non-accidental diseases, and 20 cause-specific diseases. The exposure-response associations between NOx and mortality were generally linear. Elevated mortality risks were observed for all-cause diseases, mental and behavioural disorders, respiratory diseases, unspecified dementia, hypertensive heart disease, COVID-19, and intentional self-harm, even at low NOx concentrations.
Consistent with previous epidemiological studies, our findings substantiated positive associations between long-term exposure to NOx and mortality risks across several common diseases, including all-cause diseases, non-accidental diseases, circulatory diseases, respiratory diseases, ischemic heart disease, and COPD. For example, a previous study in the UK demonstrated positive associations of long-term exposure to NOx with all-cause mortality, cardiovascular mortality, and respiratory mortality, reporting HRs of 1.05 (95% CI: 1.04, 1.06), 1.06 (95% CI: 1.03, 1.08), and 1.10 (95% CI: 1.06, 1.15) per IQR increase in NOx, respectively6. Furthermore, a cohort of Norwegian men found that each 10 μg/m3 increase in NOx was linked to an elevated risk of ischemic heart disease mortality (HR: 1.08; 95% CI: 1.03, 1.12), but not for cerebrovascular diseases8. Another study from China found NOx to be an independent risk factor for mortality from respiratory diseases and COPD9. Regarding associations between NOx and cancer, current evidence was inconsistent. For instance, in line with results of other cohort studies conducted in Israel and China10,11, we found null effect estimates of NOx on overall cancer or lung cancer. However, positive associations were reported in another UK study6. The discrepancies observed in these studies may be due to differences in the characteristics of the study populations, exposure assessment, methodologies, and adjustment for covariates.
Meanwhile, we found significant positive associations of NOx and NO2 with mortality from psychiatric disorders, unspecific dementia, pneumonia, COVID-19, and intentional self-harm, which were consistent with previous studies. For instance, a Danish nationwide study showed that per 10 µg/m3 increase in NO2 was associated with higher mortality from dementia (HR: 1.05; 95% CI: 1.03, 1.07), and psychiatric disorders (HR: 1.23; 95% CI: 1.19, 1.28)12. And compared to our findings, a nationwide cohort study in the UK reported a lower estimated effect (HR: 1.09; 95% CI: 1.03, 1.16) for pneumonia mortality for each IQR increase in NO213. A sub-regional study in England estimated that each 1 µg/m3 increment in NOx was associated with a 1.5% increase in COVID-19 deaths (odds ratio: 1.015; 95% CI: 1.011, 1.019)14. An IQR increase in NO2 was associated with an HR of 1.18 (95% CI: 1.03, 1.34) for COVID-19 death in Denmark15, while an HR of 1.33 (95% CI: 1.09, 1.64) was observed for intentional self-harm mortality in South Korea16.
In a more granular exploration of diseases, we uncovered several underexplored conditions intricately associated with long-term exposure to NOx and NO2, such as lip, oral cavity and pharynx cancer, esophageal cancer, bladder cancer, hypertensive heart disease, other peripheral vascular diseases, phlebitis and thrombophlebitis, hepatic fibrosis and cirrhosis, and accidental poisoning. Although these common but underexplored conditions represent only a small fraction of total mortality, our study offers early evidence supporting their potential role in disease progression. Previous studies have demonstrated that long-term exposure to NOx and NO2 elevated mortality risks of hypertension, ischemic heart disease and heart failure17,18,19. Notably, hypertensive heart disease is intrinsically linked to hypertension and frequently co-occurs with ischemic heart disease or progresses to heart failure20,21. For phlebitis and thrombophlebitis, its subcategory superficial venous thrombosis may increase the risk of deep vein thrombosis, which can potentially lead to life-threatening pulmonary embolism22. Likewise, deep vein thrombosis is associated with adverse outcomes, including stroke, acute coronary syndrome, and increased mortality23. A retrospective case-control study found that long-term exposure to PM2.5, PM10, and O3 may increase the risk of lower extremity deep vein thrombosis23. Another national cohort study conducted in China observed that 62% of the mortality attributable to air pollution occurred within three months following ischemic stroke, elucidating the potential association with acute complications of stroke (e.g., respiratory infection and venous thromboembolism), which may contribute to decreased early survival rate24. As for the liver cirrhosis, a cohort study conducted in UK found that NOx and NO2 increased the risk of non-alcoholic fatty liver disease25, which typically manifests as an early precursor to liver fibrosis and cirrhosis. Overall, further investigation is needed to verify these associations and to understand the underlying mechanisms.
We revealed diverse features in the shapes of exposure-response curves across diseases, suggesting that NOx and NO2 may affect people with various diseases differently. The large European cohorts within the ELAPSE project similarly reported a non-linear association between NO2 exposure and all-cause mortality26. In a previous study conducted in Canada, a supra-linear exposure-response relationship was found for non-accidental mortality27. Eum et al. documented a linear association between NO2 and non-accidental mortality, but non-linear relationships for cardiovascular and respiratory mortality28. Nevertheless, our study provides compelling evidence that there is no safe level of low-dose NOx exposure for mortality from all-cause, mental and behavioural disorders, respiratory diseases, unspecified dementia, hypertensive heart disease, COVID-19, and intentional self-harm. Elevated risks of mortality from these diseases were observed despite concentrations falling below the 25th percentiles of NOx (16.27 μg/m3). Consequently, it is imperative to implement more stringent air pollution control standards or regulations, as mitigating exposure has the potential to reduce death burden.
Stratified analyses revealed that age, sex, and residential area may modify the association between exposure and cause-specific diseases mortality. In age-stratified analyses, we observed that the association between NO2 and accidental poisoning was more pronounced in the younger group (≤ 65 years). An analysis on accidental injury mortality in the US indicated that, compared to those aged 15–24 years, the relative risk of accidental poisoning was strongest among individuals aged 35–54, followed by those aged 25–34 and 55–7429. Age and NO2 may act synergistically on the risk of dying from accidental poisoning.
Our sex-stratified findings indicated a heightened susceptibility among females to the effects of NOx and NO2 concerning mental and behavioral disorders. A study conducted in South Korea found that adverse effects of NO2 on cognitive function were significantly higher among females residing in urban areas compared to males30. Song et al. observed a positive correlation between NO2 and the levels of biomarkers indicating neurological damage, with the estimated impact being notably elevated in females relative to males31. The underlying explanation may be related to estrogen fluctuation among females and difference in hypothalamic-pituitary-adrenal (HPA) axis functioning between males and females, genetic susceptibility, and socio-psychological factors between males and females32.
The area-stratified analysis revealed regional variations in the mortality risks of NOx and NO2, particularly for patients with pneumonia, fibrosis and cirrhosis of liver, and accidental poisoning. We observed a stronger risk of air pollutants for those with fibrosis and cirrhosis of liver among urban dwellers, possibly due to differing lifestyles between urban and rural areas. Previous studies reported that particulate matters could increase the risk of advanced fibrosis in patients with metabolic dysfunction-associated fatty liver disease, which is closely linked to urban lifestyles (e.g., sedentary behavior, urbanization, and Westernized dietary patterns)33,34. We speculated that NOx and NO2 may act similarly to particulate matter by worsening the outcome of patients with pre-existing liver conditions. For pneumonia and accidental poisoning, previous studies identified an elevated risk of Klebsiella pneumoniae oropharyngeal carriage in rural areas35. A study investigating urban-rural disparities in accidental injuries found that the hospitalization rates resulting from accidental poisoning were significantly higher among rural populations36. This may be related to disparities in access to healthcare service. However, these studies did not assess the potential associations between NOx and NO2 and mortality due to pneumonia, fibrosis and cirrhosis of liver, and accidental poisoning. To date, research on pollutant exposure and mortality remains notably limited in examining population characteristics and is marked by considerable heterogeneity. Considering the paucity of epidemiological evidence on susceptible populations and the yet incompletely elucidated etiology, future endeavors necessitate further comprehensive investigations.
It is presently hypothesized that oxidative stress and inflammation are the predominant biological pathways connecting air pollution with health outcomes. The main manifestation involves inducing systemic inflammation and targeting multiple systems or organs, resulting in functional impairment and endocrine disorder, thus contributing to long-term sub-clinical effects and elevating the risks of various disease-related mortality. As there is a lack of evidence on the underlying biological mechanism for NOx, we mainly discussed the potential mechanism of its primary components (NO2 and NO). Animal-model analyses conducted by Poynter et al. revealed that NO2 exposure enhanced and prolonged inflammatory responses and airway hyperresponsiveness, characterized by significantly augmented eosinophilic inflammation and enhanced terminal bronchiolar lesions, which extended markedly into the alveoli37. The COPD mouse model further elucidated that long-term exposure to NO2 may foster the accumulation of inflammatory cells via oxidative stress, signifying a progression from acute to chronic pulmonary injury38. Additionally, exposure to NO2 could disrupt calcium ion equilibrium via apoptotic signaling pathways, actin cytoskeletal reorganization, and negatively impact myocardial contractility and vascular dilation, ultimately resulting in apoptosis of myocardial cells39. Throughout the course of central nervous system (CNS) and psychiatric disorders, the accumulation of abnormal proteins (Aβ42 and α-synuclein), heightened levels of inflammatory cytokines, and elevated concentrations of reactive oxygen species served as mediators for the adverse impacts of air pollution on the CNS, ultimately leading to structural brain impairment and marking the early pathological stages of neurodegenerative diseases40,41. Moreover, systemic inflammation, oxidative stress, and structural damage to the brain caused by air pollution can contribute to the onset of psychological disorders and heighten the risk of accidental injuries16.
In contrast to the harmful effects of NO2 on human health, NO plays an unexpectedly significant role in physiological processes. NO is a critical signaling molecule involved in numerous physiological processes, such as blood pressure regulation, vasodilation, neurotransmission, and immunity42. Despite its role as an atmospheric pollutant, carefully controlled inhaled NO therapy produces selective pulmonary vasodilation, effectively increasing arterial oxygen levels, and providing an effective treatment for pulmonary hypertension in both adults and children43,44. However, dysregulated NO signaling is a key characteristic in the pathogenesis of numerous major diseases, including cardiovascular disease, diabetes, and cancer42. Although NO rapidly reacts with atmospheric oxygen to form NO2, its impact on human health remains significant and should not be overlooked. A multidisciplinary approach will be crucial in the future to comprehensively investigate the role of NOx within both environmental and biological frameworks.
Our study has several strengths, including a large sample size, longitudinal study design, long-term follow-up, and access to high-quality data covering a wide range of diseases and potential covariates. As a result, it provides robust epidemiological evidence on associations of NOx with the full spectrum of diseases, uncovers novel mortality risk linkages, and advances the existing knowledge on NOx-related health effects—an effort that might be challenging in smaller cohorts. Additionally, the atmospheric pollution exposure assessment method used in this study is highly reliable, as it accounts for individuals’ residential mobility throughout the follow-up period and incorporates a long temporal scope, allowing for a more accurate evaluation of individual exposure levels.
This study is subject to certain limitations. Firstly, UKB is based on volunteer participants rather than random selection, which introduces the potential for volunteer bias. Nevertheless, owing to the large sample size advantage of the UKB, the impact of the healthy volunteer effect on the validity of exposure-outcome associations is likely minimal45. Secondly, regarding generalizability and external validity of the results, caution is needed when interpreting our findings beyond the UKB cohort due to differences in populations, geographic regions, demographic characteristics, and exposure levels. Thirdly, we exclusively utilized residential geographical coordinates to evaluate individual exposure to ambient air pollution, without accounting for indoor air pollution, commuting patterns, workplace exposures, and other relevant factors. Further research into exposure to pollutants from various sources is needed, given the continuous evidence of a significant disease burden linked to indoor air pollution46,47. Fourthly, observational study designs inherently struggle to eliminate all potential confounding factors or reverse causality. Nonetheless, this study employed a prospective cohort design and sensitivity analyses that enhanced the ability to effectively assess relationships between nitrogen oxides exposure and cause-specific mortality. Lastly, although we examined the impact of NOx and NO2 on various diseases, an in-depth analysis of disease progression, such as through multi-state modeling, was not conducted. We propose an in-depth examination of disease progression in future endeavors to support earlier intervention strategies and, consequently, reduce the air pollution-related disease burden.
Methods
Study design and participants
This study used data from the UKB, with ethical approval granted by the Northwest Multiple Center Research Ethics Committee, and all participants provided written informed consent. This large-scale national prospective cohort study recruited over 500,000 individuals aged 37–73 encompassing 22 centers across England, Wales, and Scotland during 2006–2010. The UKB dataset provides a rich resource of information on its participants, including demographics from questionnaire surveys, anthropometric measurements, biochemical samples, genomic research data, and longitudinal tracking of participant health outcomes48,49. For this study, we began with 502,356 participants from the UK Biobank. We excluded the participants with missing residential addresses (n = 13) and mortality information (n = 303). A total of 502,040 participants were included in the final analysis (Supplementary Fig. S7).
Air pollution assessment
The annual average concentrations of atmospheric pollutants were obtained from the UK’s Department for Environment Food & Rural Affairs (DEFRA, https://uk-air.defra.gov.uk/data/pcm-data), which functions as a high-resolution data platform for near-surface atmospheric pollution. DEFRA primarily utilizes multi-source estimates of emissions based on the National Atmospheric Emissions Inventory (NAEI), combined with meteorological data and calibrated oxidant distribution modeling processes, to establish an Atmospheric Dispersion Modeling System (ADMS), which evaluates the annual average concentrations of major air pollutants through simulation within a grid with a horizontal resolution of 1 × 1 km50. Subsequently, calibration was performed using data obtained from background monitoring network sites. DEFRA performs comprehensive comparisons between the modelled and measured annual average concentrations of air pollutants to validate the reliability of the models, showing good model performance (R-squared over 0.80)50,51. The National administrative political boundary Shapefile was obtained from the Office for National Statistics licensed under the Open Government Licence v.3.052.
The study employed previously proposed methods to calculate average exposure concentrations of NOx, NO2, PM2.5, PM10 and SO2 during the follow-up period of participants53,54. To simultaneously account for changes in participants’ residential addresses and the long-term exposure status, geospatial information on participants’ residential addresses along with the duration of residence at each address were collected from UKB. Geographic grid cell in the annual concentration map were then aggregated to the residential address history code51. We employed linear interpolation to calculate the time-weighted annual average air pollutant exposure for each participant from enrollment until the occurrence of any outcomes53.
Follow-up and outcome
All participants were followed up prospectively until death, loss to follow-up, or being censored (Nov 30, 2022), whichever occurred first. The all-cause and cause-specific mortality events for this study were sourced from the Office for National Statistics mortality registry55. The specific mortality outcomes were defined according to the International Classification of Diseases Tenth Revision (ICD-10). We conducted a thorough analysis on not only deaths from all causes (A00-Z99), non-accidental (A00-R99), accidental (V01-X59, Y85-Y86), and the 15 major disease causes, but also all subcategories of diseases with mortality rates ≥ 1‰ to ensure statistical precision. The detailed information of outcomes is shown in Supplementary Tables S1–S2.
Covariates
To control for potential confounding biases, we included covariates such as demographic, geographic, and socio-economic status data collected during the baseline assessment period. Specifically, we adjusted for age, sex, ethnicity, body mass index (BMI), education, occupation, smoking status, alcohol consumption, physical activity, residential area, and household income. Details on the covariates are presented in Supplementary Table S19. The proportions of missing values were low for most variables (Supplementary Table S20), except for physical activity, which was dealt with by creating dummy variable56. When analyzing sex-specific mortality outcomes (e.g., malignant tumor of male or female reproductive system), we did not include sex as a covariate in the models.
Statistical analyses
Associations between long-term exposure to NOx and mortality from all-cause, non-accidental, accidental, and cause-specific diseases, namely 15 major disease causes (encompassing 103 subcategories), were investigated using Cox proportional hazards models with time-varying covariates. Considering that NO2 is the major component of NOx, we also assessed the health impact of NO2 as an add-on analysis.
Since all-cause mortality is a competing risk for cause-specific mortality, the models censored participants at death from any cause (or loss to follow-up, or the censoring date of the study) to estimate cause-specific HRs, which compared event rates in participants who were alive and free of the event of interest57. The modeling is detailed as shown below.
The adjustment of time-varying covariates was considered due to the violation of the proportional hazard assumption inherent in traditional Cox proportional hazards models, as well as the consideration that concentrations of air pollutants change over time58,59,60. Therefore, we incorporated ambient pollutants and age as external time-varying variables on a 1-year temporal scale into the Cox proportional hazards model, while adjusting for the aforementioned covariates to control for potential confounding effects. In addition, calendar year was included as a indicatory variable to account for potential temporal trends61. The effect estimates of this study are presented as HRs with 95% CIs for each 10 μg/m3, SD, and IQR increases in the concentrations of NOx and NO2.
A restricted cubic spline (RCS) function was used to smooth exposure-response relationships between long-term air pollutant exposure and all-cause or cause-specific mortality risk. Knots (3–6) were selected based on the Akaike and Bayesian information criteria (AIC/BIC) to optimize model fit by minimizing AIC and BIC values. Likelihood ratio test was further used to test the potential nonlinearity by comparing likelihood values between models with smoothed term of air pollutants and those with linear function62.
We investigated effect modification through stratification by age groups (≤ 65 versus > 65 years), sex (male versus female), and residential-level (rural versus urban) to discern disparities among various subgroups. Significance testing was conducted utilizing two-sample Z-tests63,64, with the specific formula provided below:
E1 and E2 are the natural logarithmically transformed values of HRs, \({SE}\left({E}_{1}\right)\) and \({SE}\left({E}_{2}\right)\) are the corresponding standard errors.
Sensitivity analyses
We conducted a series of sensitivity analyses to examine the robustness of our findings: (1) incorporating PM2.5, PM10 and SO2 to establish double-pollutant models; (2) additionally adjusting for baseline chronic conditions (e.g., cancer, hypertension, and diabetes) to examine whether the observed associations were influenced by pre-existing health status; (3) adjusting for only a portion of individual-level covariates (including age, sex, BMI, ethnicity, household income, and residential area); (4) excluding participants with less than 2 years of follow up to minimize the potential for reverse causality; (5) applying time-varying exposures on extended scales of 5-year averages for NOx; (6) setting the follow-up duration to a maximum of ten years from recruitment; (7) censoring follow-up data by the end of 2019 to eliminate the potential influence of the COVID-19 pandemic; (8) employing the multiple imputation for covariates with missing values; (9) excluding participants whose geographic codes changed during follow-up to account for potential measurement bias induced by residential mobility; (10) excluding the outliers of NOx concentrations (values below the 1st percentile or above the 99th percentile) to test the possible influence of outliers; (11) to control for multiple testing, we employed FDR-adjusted q-values < 0.1 to assess significance. When P < 0.05 but q ≥ 0.1, the relationship between air pollutant and mortality was considered suggestive65.
All statistical analyses were conducted using R 4.2.3 software. The ‘survival’ package and the ‘tmerge’ function were utilized for constructing time-varying covariates Cox proportional hazards models. The ‘rms’ package was employed to construct RCS. This study employed two-sided tests with a significance level of α = 0.05, where P < 0.05 indicated statistical significance.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
This research was conducted using the UK Biobank Resource (http://www.ukbiobank.ac.uk/) under application number 95736. Data from UK Biobank is accessible to eligible researchers via applying to www.ukbiobank.ac.uk. Historical air pollutants data are publicly available at the data set of Department for Environment Food & Rural Affairs (DEFRA, https://uk-air.defra.gov.uk/data/pcm-data). Data from DEFRA are modelled each year and typically the latest updates are checked and approved by the autumn and made available by mid-October. The Office for National Statistics offers free and open access to authoritative geographic products (https://geoportal.statistics.gov.uk/). Map data is sourced from the Office for National Statistics and licensed under the Open Government Licence v.3.0. It includes OS data © Crown copyright and database rights. The source data underlying Figs. 1, 2, and 3 are provided as Source Data files. Source data are provided with this paper.
Code availability
R codes in this study are available on Zenodo repository https://doi.org/10.5281/zenodo.1470998866.
References
Strak, M. et al. Long term exposure to low level air pollution and mortality in eight European cohorts within the ELAPSE project: pooled analysis. BMJ 374, n1904 (2021).
Fu, X. et al. Modeling analysis of secondary inorganic aerosols over China: pollution characteristics, and meteorological and dust impacts. Sci. Rep. 6, 35992 (2016).
Pye, H. O. T., Appel, K. W., Seltzer, K. M., Ward-Caviness, C. K. & Murphy, B. N. Human-health impacts of controlling secondary air pollution precursors. Environ. Sci. Technol. Lett. 9, 96–101 (2022).
Jonson, J. E. et al. Impact of excess NOx emissions from diesel cars on air quality, public health and eutrophication in Europe. Environ. Res. Lett. 12, 094017 (2017).
Pappin, A. et al. Health benefits of reducing NOx emissions in the presence of epidemiological and atmospheric nonlinearities. Environ. Res. Lett. 11, 064015 (2016).
Zhu, Y. et al. Ambient air pollution, lifestyle, and genetic predisposition on all-cause and cause-specific mortality: A prospective cohort study. Sci. Total Environ. 933, 173120 (2024).
Huang, W. et al. Individual and joint associations of long-term exposure to air pollutants and cardiopulmonary mortality: a 22-year cohort study in Northern China. Lancet Reg. Health West Pac. 36, 100776 (2023).
Nafstad, P. et al. Urban air pollution and mortality in a cohort of Norwegian men. Environ. Health Perspect. 112, 610–615 (2004).
Wang, Q., Liu, Y. & Pan, X. Atmosphere pollutants and mortality rate of respiratory diseases in Beijing. Sci. Total Environ. 391, 143–148 (2008).
Cohen, G. et al. Long-term exposure to traffic-related air pollution and cancer among survivors of myocardial infarction: A 20-year follow-up study. Eur. J. Prev. Cardiol. 24, 92–102 (2017).
Cao, J. et al. Association between long-term exposure to outdoor air pollution and mortality in China: a cohort study. J. Hazard Mater. 186, 1594–1600 (2011).
So, R. et al. Long-term exposure to air pollution and mortality in a Danish nationwide administrative cohort study: Beyond mortality from cardiopulmonary disease and lung cancer. Environ. Int 164, 107241 (2022).
Carey, I. M. et al. Mortality associations with long-term exposure to outdoor air pollution in a national English cohort. Am. J. Respir. Crit. Care Med. 187, 1226–1233 (2013).
Travaglio, M. et al. Links between air pollution and COVID-19 in England. Environ. Pollut. 268, 115859 (2021).
Zhang, J. et al. Long-term exposure to air pollution and risk of SARS-CoV-2 infection and COVID-19 hospitalisation or death: Danish nationwide cohort study. Eur. Respir. J. 62, 2300280 (2023).
Min, J. Y., Kim, H. J. & Min, K. B. Long-term exposure to air pollution and the risk of suicide death: A population-based cohort study. Sci. Total Environ. 628–629, 573–579 (2018).
Yorifuji, T. et al. Long-term exposure to traffic-related air pollution and the risk of death from hemorrhagic stroke and lung cancer in Shizuoka, Japan. Sci. Total Environ. 443, 397–402 (2013).
Lim, C. C. et al. Mediterranean Diet and the Association Between Air Pollution and Cardiovascular Disease Mortality Risk. Circulation 139, 1766–1775 (2019).
Mills, K. T., Stefanescu, A. & He, J. The global epidemiology of hypertension. Nat. Rev. Nephrol. 16, 223–237 (2020).
Diez, J. & Butler, J. Growing Heart Failure Burden of Hypertensive Heart Disease: A Call to Action. Hypertension 80, 13–21 (2023).
Frohlich, E. D. Fibrosis and ischemia: the real risks in hypertensive heart disease. Am. J. Hypertens. 14, 194S–199S (2001).
Nasr, H. & Scriven, J. M. Superficial thrombophlebitis (superficial venous thrombosis). BMJ 350, h2039 (2015).
Xiong, Q. et al. Long-term exposures to ambient particulate matter and ozone pollution with lower extremity deep vein thrombosis after surgical operations: a retrospective case-control study in Beijing, China. BMC Public Health 23, 1956 (2023).
Chen, G. et al. Long-Term Exposure to Air Pollution and Survival After Ischemic Stroke. Stroke 50, 563–570 (2019).
Li, F. R. et al. Long-term exposure to air pollution and incident non-alcoholic fatty liver disease and cirrhosis: A cohort study. Liver Int. 43, 299–307 (2023).
Stafoggia, M. et al. Long-term exposure to low ambient air pollution concentrations and mortality among 28 million people: results from seven large European cohorts within the ELAPSE project. Lancet Planet Health 6, e9–e18 (2022).
Crouse, D. L. et al. Ambient PM2.5, O3, and NO2 Exposures and Associations with Mortality over 16 Years of Follow-Up in the Canadian Census Health and Environment Cohort (CanCHEC). Environ. Health Perspect. 123, 1180–1186 (2015).
Eum, K. D. et al. Long-term nitrogen dioxide exposure and cause-specific mortality in the U.S. Medicare population. Environ. Res. 207, 112154 (2022).
Rockett, I. R. et al. Leading causes of unintentional and intentional injury mortality: United States, 2000-2009. Am. J. Public Health 102, e84–e92 (2012).
Kim, H. et al. Gender Difference in the Effects of Outdoor Air Pollution on Cognitive Function Among Elderly in Korea. Front Public Health 7, 375 (2019).
Song, J. et al. Acute effects of ambient nitrogen dioxide exposure on serum biomarkers of nervous system damage in healthy older adults. Ecotoxicol. Environ. Saf. 249, 114423 (2023).
Pitychoutis, P. M. & Papadopoulou-Daifoti, Z. Of depression and immunity: does sex matter? Int J. Neuropsychopharmacol. 13, 675–689 (2010).
Pati, G. K. & Singh, S. P. Nonalcoholic fatty liver disease in South Asia. Eur. J. Hepatogastro. 6, 154 (2016).
Ji, W. et al. Exposure to ambient air pollution and metabolic dysfunction-associated fatty liver disease: Findings from over 2.7 million adults in Northwestern China. Ecotoxicol. Environ. Saf. 272, 116109 (2024).
Dao, T. T. et al. Klebsiella pneumoniae oropharyngeal carriage in rural and urban Vietnam and the effect of alcohol consumption. PLoS One 9, e91999 (2014).
Eddleston, M. et al. The importance of poisoning vs. road traffic injuries as a cause of death in rural Sri Lanka. PLoS One 2, e599 (2007).
Poynter, M. E. et al. Nitrogen dioxide enhances allergic airway inflammation and hyperresponsiveness in the mouse. Am. J. Physiol. Lung Cell Mol. Physiol. 290, L144–L152 (2006).
Wegmann, M., Renz, H. & Herz, U. Long-term NO2 exposure induces pulmonary inflammation and progressive development of airflow obstruction in C57BL/6 mice: a mouse model for chronic obstructive pulmonary disease? Pathobiology 70, 284–286 (2002).
Ji, S., Guo, Y., Li, G. & Sang, N. NO2 exposure contributes to cardiac hypertrophy in male mice through apoptosis signaling pathways. Chemosphere 309, 136576 (2022).
Jayaraj, R. L., Rodriguez, E. A., Wang, Y. & Block, M. L. Outdoor Ambient Air Pollution and Neurodegenerative Diseases: the Neuroinflammation Hypothesis. Curr. Environ. Health Rep. 4, 166–179 (2017).
Alemany, S. et al. Associations between air pollution and biomarkers of Alzheimer’s disease in cognitively unimpaired individuals. Environ. Int. 157, 106864 (2021).
Lundberg, J. O. & Weitzberg, E. Nitric oxide signaling in health and disease. Cell 185, 2853–2878 (2022).
Abman, S. H. et al. Pediatric Pulmonary Hypertension: Guidelines From the American Heart Association and American Thoracic Society. Circulation 132, 2037–2099 (2015).
Yu, B., Muenster, S., Blaesi, A. H., Bloch, D. B. & Zapol, W. M. Producing nitric oxide by pulsed electrical discharge in air for portable inhalation therapy. Sci. Transl. Med 7, 294ra107–294ra107 (2015).
Batty, G. D., Gale, C. R., Kivimaki, M., Deary, I. J. & Bell, S. Comparison of risk factor associations in UK Biobank against representative, general population based studies with conventional response rates: prospective cohort study and individual participant meta-analysis. BMJ 368, m131 (2020).
Lee, K. K. et al. Adverse health effects associated with household air pollution: a systematic review, meta-analysis, and burden estimation study. Lancet Glob. Health 8, e1427–e1434 (2020).
Mandin, C. et al. Assessment of indoor air quality in office buildings across Europe - The OFFICAIR study. Sci. Total Environ. 579, 169–178 (2017).
Sudlow, C. et al. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 12, e1001779 (2015).
Fry, A. et al. Comparison of sociodemographic and health-related characteristics of UK Biobank participants with those of the general population. Am. J. Epidemiol. 186, 1026–1034 (2017).
Pugsley, K. L., et al. Technical report on UK supplementary modelling assessment under the Air Quality Standards Regulations 2010 for 2020. Report for The Department for Environment, Food and Rural Affairs, the Welsh Government, the Scottish Government and the Department of the Environment for Northern Ireland. Ricardo Energy & Environment/R/3474 https://uk-air.defra.gov.uk/assets/documents/reports/cat09/2203150935_2020_PCM_technical_report.pdf (2022).
Ma, Y. et al. Air pollutants, genetic susceptibility, and abdominal aortic aneurysm risk: a prospective study. Eur. Heart J. 45, 1030–1039 (2024).
Office for National Statistics (ONS): https://geoportal.statistics.gov.uk/. Office for National Statistics licensed under the Open Government Licence v.3.0.
Wu, Y. et al. Ambient air pollution associated with incidence and dynamic progression of type 2 diabetes: a trajectory analysis of a population-based cohort. BMC Med. 20, 375 (2022).
Shi, H. et al. Dynamic association of ambient air pollution with incidence and mortality of pulmonary hypertension: A multistate trajectory analysis. Ecotoxicol. Environ. Saf. 262, 115126 (2023).
UK Biobank. Mortality data: linkage to death registries (Version 3.0). http://biobank.ndph.ox.ac.uk/ukb/ukb/docs/DeathLinkage.pdf (2023).
Feng, J. et al. The effects of long-term exposure to air pollution on incident mental disorders among patients with prediabetes and diabetes: Findings from a large prospective cohort. Sci. Total Environ. 897, 165235 (2023).
Millwood, I. Y. et al. Alcohol intake and cause-specific mortality: conventional and genetic evidence in a prospective cohort study of 512 000 adults in China. Lancet Public Health 8, e956–e967 (2023).
Zhang, Z., Reinikainen, J., Adeleke, K. A., Pieterse, M. E. & Groothuis-Oudshoorn, C. G. M. Time-varying covariates and coefficients in Cox regression models. Ann. Transl. Med .6, 121 (2018).
Bradburn, M. J., Clark, T. G., Love, S. B. & Altman, D. G. Survival analysis Part III: multivariate data analysis - choosing a model and assessing its adequacy and fit. Br. J. Cancer 89, 605–611 (2003).
Bellera, C. A. et al. Variables with time-varying effects and the Cox model: some statistical concepts illustrated with a prognostic factor study in breast cancer. BMC Med. Res. Methodol. 10, 1–12 (2010).
Wu, X., Braun, D., Schwartz, J., Kioumourtzoglou, M. & Dominici, F. Evaluating the impact of long-term exposure to fine particulate matter on mortality among the elderly. Sci. Adv. 6, eaba5692 (2020).
Liu, L. et al. Longitudinal impacts of PM2. 5 constituents on adult mortality in China. Environ. Sci. Technol. 56, 7224–7233 (2022).
Altman, D. G. & Bland, J. M. Interaction revisited: the difference between two estimates. BMJ 326, 219 (2003).
Liu, C. et al. Ambient Particulate Air Pollution and Daily Mortality in 652 Cities. N. Engl. J. Med. 381, 705–715 (2019).
Li, P. et al. Association between gut microbiota and preeclampsia-eclampsia: a two-sample Mendelian randomization study. BMC Med. 20, 443 (2022).
Yang, S. et al. Long-term exposure to nitrogen oxides and cause-specific mortality. https://doi.org/10.5281/zenodo.14709988.
Acknowledgements
This research was conducted using the UK Biobank Resource (http://www.ukbiobank.ac.uk/) under application number 95736. The authors gratefully acknowledge the participants and those involved in building the resource. Jun Yang was supported by the National Natural Science Foundation of China (No. 82003552). Mengmeng Li was supported by the National Natural Science Foundation of China (No. 82204131), Guangzhou Science and Technology Project (No. 2025A04J3327), and Young Talents Program of Sun Yat-sen University Cancer Center (No. YTP-SYSUCC-0048). Kaili Lin was supported by the National Natural Science Foundation of China (No. 82204092) and Guangzhou Science and Technology Project (No. 2024A04J10031).
Author information
Authors and Affiliations
Contributions
J.Y. and M.L. designed the study. J.Y. collected the data. S.Y. performed data cleaning and statistical analysis. S.Y. drafted the manuscript. M.L., C.G., W.J.R., M.J.Z.S., K.L., Q.Z., Z.C., P.C., L.Y., and D.L. reviewed the manuscript. J.Y. was responsible for the decision to submit the manuscript after consultation with all listed authors. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks Hanns Mooshammer and the other anonymous reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yang, S., Li, M., Guo, C. et al. Associations of long-term exposure to nitrogen oxides with all-cause and cause-specific mortality. Nat Commun 16, 1730 (2025). https://doi.org/10.1038/s41467-025-56963-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-025-56963-y
This article is cited by
-
Long-term exposure to PM2.5 components and mortality in 237 Chinese cities: a modelling study
Frontiers of Environmental Science & Engineering (2025)
-
Causal impact of air pollution on head and neck cancer: a Mendelian randomization study
Discover Oncology (2025)