Abstract
Uveal melanoma (UM) is the most common intraocular cancer in adults, with metastatic disease (mUM) occurring in approximately half of the patients. Tebentafusp, an immune-mobilizing monoclonal T cell receptor against cancer (ImmTAC), is a therapeutic shown to improve overall survival (OS) in HLA-A*02:01+ adult patients with mUM. Here we investigate the impact of tumor-associated macrophages (TAM) on ImmTAC activity. In vitro, M2 macrophages inhibit ImmTAC-mediated tumor-killing in a dose-dependent and contact-dependent manner. Accordingly, high baseline intratumoral TAM-to-T cell ratios correlate with shorter OS (HR = 2.09, 95% CI, 1.31–3.33, p = 0.002) in tebentafusp-treated mUM patients from a phase 2 trial. By contrast, IL-2 conditioning of T cells overcomes M2 macrophage-mediated suppression in vitro, while ImmTAC treatment leads to M2-to-M1 macrophage reprogramming both in vitro and in tebentafusp-treated mUM patients. Overall, we show that tebentafusp reshapes the tumor microenvironment to enhance anti-tumor T cell activity, whilst combining tebentafusp with IL-2 may enhance benefit in patients with high levels of TAM.
Similar content being viewed by others
Introduction
T cell engagers are a new class of immunotherapy molecules with notable efficacy in redirecting T cells to recognize and eliminate target tumor cells. Blinatumomab, the first CD19xCD3 bispecific T cell engager (BiTE), gained FDA approval for the treatment of certain hematologic malignancies1,2. Subsequently, immune-mobilizing monoclonal T cell receptor against cancer (ImmTAC) molecules, engineered as high affinity T cell receptor - anti-CD3 (TCR-CD3) bispecific fusion proteins3, have emerged as pioneering T cell engagers for the treatment of solid tumors. ImmTAC molecules bind with picomolar affinity to antigens presented by target cells on human leukocyte antigen (HLA) molecules. The anti-CD3 single-chain variable fragment effector domain binds to polyclonal T cells and forms an immune synapse leading to T cell-mediated elimination of target cells, irrespective of their endogenous TCR specificity. Tebentafusp, a first-in-class TCR-CD3 bispecific therapy, targets a gp100-derived peptide (expressed in melanocytes/melanoma cells) presented on HLA-A*02:01 molecules and has shown efficacy in both cutaneous and uveal melanoma4,5. In a phase 3 trial (NCT03070392)6,7 of HLA-A*02:01+ patients with previously untreated metastatic uveal melanoma (mUM), tebentafusp treatment demonstrated improved therapeutic benefit compared to investigator’s choice of therapy consisting of either pembrolizumab, ipilimumab, or dacarbazine. The one- and three-year survival rates with tebentafusp were 73%6 and 27%7 compared with 59% and 18% with control treatments, respectively.
The tumor immune microenvironment (TME) can influence the anti-tumor activity of immunotherapies8. Tumor-associated macrophages (TAM) are among the most abundant immune cells in the TME, and their infiltration is often associated with T cell suppression and exhaustion8,9. TAM suppress T cells via multiple mechanisms, including secretion of immunomodulatory cytokines and enzymes (e.g., interleukin-10 [IL-10], transforming growth factor-β [TGF-β], indoleamine 2,3-dioxygenase)9,10, expression of checkpoint ligands (e.g., programmed cell death-ligand 1 and 2 [PD-L1 and PD-L2]), and induction of regulatory T cell (Treg) expansion11,12. TAM have additionally been associated with immune exclusion where they impede T cell infiltration into the tumor regions through decreasing T cell motility13 or by inducing T cell apoptosis14. Conversely, TAM have also been linked to favorable clinical outcomes in certain indications, such as gastric and colorectal cancers15. The conflicting role of TAM in tumor progression is largely attributed to their marked plasticity, where their functional polarization is spatially and temporally shaped by cues from their surrounding microenvironment16,17,18. Multiple macrophage subsets exist, and these have been historically grouped into either classically activated pro-inflammatory macrophages (M1 macrophages) or alternatively activated anti-inflammatory macrophages (M2 macrophages)19. While advances in single-cell and spatial proteomics and transcriptomics have revealed that macrophages exist in a spectrum of phenotypic and transcriptional states reflecting their diverse roles in pro- and anti-inflammatory responses to pathogens and tumors, wound healing, and tissue remodeling20,21,22, the utilization of the broad M1/M2 designations remains a useful shorthand. The main type of TAM present within uveal melanoma is reported to be of the pro-tumoral M2 phenotype expressing CD163 within enucleated eye specimens and their presence is associated with poor overall survival (OS)23. TAM were also described within liver metastases from mUM, however, their prognostic role remains conflicted23,24,25.
Here, we evaluate the role of M2 macrophages on ImmTAC-mediated killing of tumor cells in vitro where we find that macrophages suppress cell killing and we investigate the mechanisms by which this is achieved. We confirm these findings in vivo using biopsies collected in a phase 2 clinical trial of tebentafusp in uveal melanoma patients26, where we find that the relative ratios of CD163+ TAM to CD3+ T cells dictate clinical response. We also identify an ImmTAC-mediated M2 to M1 reprogramming of macrophages in vitro which we validate in vivo. Finally, we show that conditioning of T cells with interleukin-2 (IL-2), a promoter of T cell activity, overcomes macrophage-mediated T cell suppression. As IL-2 is an approved treatment for melanoma, this combination could be an important strategy that could enhance outcomes with tebentafusp, and potentially other T cell engagers in patients with solid tumors.
Results
Pro-tumoral macrophages suppress ImmTAC-redirected T cell activation and killing in vitro
To assess the effect of macrophages on the ability of ImmTAC to redirect T cells against tumor cells, we established a co-culture model using target antigen-expressing cancer cell lines, healthy primary human T cells, and autologous monocyte-derived macrophages differentiated into pro-tumoral M2 phenotypes (Fig. 1a, Supplementary Fig. 1, and Supplementary Fig. 2). ImmTAC-redirected T cell-mediated tumor killing was assessed by mimicking a physiologically relevant co-culture with a low effector (E): target (T) ratio (1:2) and tumor killing was assessed at 20 h to better capture early and late apoptotic events prior to partition of tumor cytoplasm and nuclei into apoptotic bodies. ImmTAC was able to promote CD8+ T cell activation (measured by CD69 expression, Fig. 1b) and killing of the melanoma cell line A375 (Fig. 1c), whilst CD69 upregulation and tumor killing were reduced in the presence of M2 macrophages (Fig. 1b, c).
a Schematic diagram of ImmTAC-redirection assays using pan T cells (Effectors, E) co-cultured with cancer cells (targets, T) in the presence or absence of M2 macrophages. b CD69 expression by T cells redirected against the melanoma tumor cell line A375. Median fluorescent intensity (MFI) on CD3+CD8+ T cells was quantified per donor (mean of 2 biological replicates is shown, two independent experiments). c Quantification of early and late apoptotic A375 tumor cells by flow cytometry (mean of 2 biological replicates is shown, two independent experiments). d CD69 expression by T cells redirected against THP-1 tumor cells. MFI on CD3+CD8+ T cells was quantified per donor (n = 7 biological replicates, Wilcoxon matched-pairs single rank test, two-sided p values < 0.05 are shown). e IFN-γ levels in co-culture supernatants measured by ELISA (n = 4 biological replicates, Mann-Whitney test two-sided p values < 0.05 are shown). f Representative tumor killing flow cytometry plots. Early apoptotic (Annexin V+ 7AAD-) and late apoptotic cells (Annexin V+ 7AAD+) percentages were quantified for estimation of total dying THP-1 targets (labeled orange). g Quantification of early and late apoptotic targets following co-culture with ImmTAC-redirected T cells in the presence or absence of M2 macrophages (n = 7 biological replicates, Wilcoxon matched-pairs single rank test, exact two-sided p values are given). h, i Quantification of CD69 expression by ImmTAC-redirected CD3+ CD8+ T cells (h) and early and late apoptotic targets (i) using decreasing E:M2 cell ratio (n = 4 biological replicates). Abbreviations: E = Effectors, T = Targets, M2 = M2 macrophages, MFI = Mean Fluorescence Intensity.
We extended and confirmed these observations in antigen-expressing THP-1 leukemic tumor cells, where ImmTAC was able to promote CD8+ T cell activation (CD69 expression) and interferon (IFN)-γ release against these target cells (Fig. 1d, e). CD69 upregulation and IFN-γ secretion by ImmTAC-redirected T cells was drastically reduced in the presence of M2 macrophages (Fig. 1d, e). ImmTAC-redirected T cells induced tumor lysis in 18.5% (±4.5% standard error of the mean [SEM]) of target cells at 20 h (Fig. 1f, g). Tumor cell elimination by ImmTAC-redirected T cells was significantly reduced in the presence of M2 macrophages (Fig. 1f, g), and macrophage-mediated T cell suppression was substantially more evident in the presence of pro-tumoral M2 macrophages compared with M1 macrophages (Supplementary Fig. 3a). M2 macrophage suppression of T cell activation and tumor killing was dose dependent, with a 1:5 T cell-to-M2 ratio (E:M2) achieving almost complete T cell inhibition (Fig. 1h, i).
To gain further insight on the effect of M2 macrophage suppression, T cells were sorted post ImmTAC redirection, and their transcriptomic profile was assessed by bulk RNA-sequencing. We confirmed the ability of ImmTAC to redirect T cell activation at a transcriptional level using T cell activation pathways previously described by Szabo et al27. Specifically, ImmTAC-stimulated T cells demonstrated upregulation of genes associated with proliferation, IFN-γ response, cytokines, and cytolytic pathways (Fig. 2a, b). The presence of M2 macrophages in co-cultures significantly impacted the transcriptome of ImmTAC-redirected T cells (314 and 541 genes downregulated and upregulated, respectively [absolute log2 fold-change > 0.75; adjusted p < 0.05]) (Fig. 2c), with CD8+ T cell activation and proliferation genes27 notably downregulated (Fig. 2d, Supplementary Data File 1 and 2).
a Validation of ImmTAC-redirected T cell activation using bulk RNA-seq analysis. Ridge plot showing the fold change of T cell activation genes in response to ImmTAC redirection grouped in proliferation (log2 fold-change = 4.44 ± 0.26), IFN-γ response (log2 fold-change = 2.98 ± 0.24) and CD8-related cytotoxic and cytokine genes (log2 fold-change = 1.5 ± 0.36) (n = 6 biological replicates of unstimulated T cells and n = 4 biological replicates for ImmTAC-stimulated T cells). b T cell activation gene expression heatmap plot of untreated T cells (n = 6 biological replicates) and ImmTAC-redirected T cells sorted from E:T + ImmTAC co-cultures (n = 4 biological replicates, the 30 most up- or down-regulated genes with an adjusted (adj) p-value < 0.05 are shown using Wald test, DESeq2). c Bulk-RNA-seq analysis of effector T cells sorted after 20 h of co-cultures. Volcano plot shows differentially upregulated or downregulated genes of T cells in ImmTAC redirected co-cultures in the presence of M2 macrophages (n = 4 biological replicates, adj p < 0.05, absolute log2 fold-change > 0.75, using Wald test, DESeq2). d Fold-change of the top 15 downregulated T cell genes in the presence of M2 macrophages. CD8+ T cell activation (cytotoxic response/cytokine release, IFN-γ mediated- response) (blue), proliferation (orange) genes are shown (n = 4 biological replicates, box plots represent the interquartile range with the line set at median and whiskers show minimum and maximum values, adj p < 0.05, absolute log2 fold-change >0.75, Wald test, DESeq2). Abbreviations: E = Effectors, T = Targets, M2 = M2 macrophages, (UT) = Untreated T cells, TPM = Transcripts Per Million.
Macrophage suppression of ImmTAC-redirected T cells in vitro is contact dependent and does not rely on individual known checkpoint receptor interactions
We investigated the mechanisms by which M2 macrophages suppress ImmTAC-redirected T cells in vitro. Cell culture assays were repeated using transwells to assess whether macrophage suppression occurs via secretion of immunosuppressive factors or through direct cell-to-cell contact. M2 macrophages were either cultured together with T cells and tumor cells or seeded on a transwell insert to prevent direct cell-cell contact (Fig. 3a). M2 macrophages only suppressed T cell activation (Fig. 3b) and tumor-killing (Fig. 3c, d) when in direct contact with T cells.
a Schematic diagram of ImmTAC-redirected E:T + M2 cell-cell contact-dependent or no contact co-cultures using transwell inserts b MFI of CD69 expression by ImmTAC-redirected CD3+ CD8+ T cells (mean ± SEM, n = 4 biological replicates, Tukey’s multiple comparison’s test, exact two-sided p values are given). c, d Representative flow cytometry plots (c) and quantification of early and late apoptotic targets (d) in M2-T cell-cell contact and contact-free co-cultures (Annexin V+, 7AAD+/-), (mean ± SEM, n = 4 biological replicates, Tukey’s multiple comparison’s test, exact two-sided p values are given). T cell checkpoint receptors blocked in ImmTAC-redirected cell-cell contact M2 co-cultures using the indicated neutralizing antibodies. CD69 expression fold-change relative to ImmTAC-redirected E:T co-culture with IgG isotype control (e), IFN-γ release fold-change relative to IgG (E:T) controls (f), quantification of early and late apoptotic targets (g) [n = 3 for anti-TIM-3, anti-TIGIT, and anti-PD1 + anti-LAG-3 + anti-CTLA-4, n = 4 for anti-LILRB1, n = 6 for anti-PD-1 and anti-PD-L1, n = 7 for anti-CTLA-4 and anti-LAG-3, n = 10 for anti-IgG for (e) and (f) and n = 11 for anti-IgG for (g) all replicates are biological replicates and data shown is mean ± SEM]. Dashed lines represent IgG Ctrl mean. Abbreviations: E = Effectors, T = Targets, M2 = M2 macrophages, MFI = Mean Fluorescence Intensity.
We therefore investigated the role of common checkpoint receptors and ligands including PD-1, PD-L1, T cell immunoglobulin and mucin domain-containing protein 3 (TIM-3), T cell immunoreceptor with immunoglobulin and ITIM domain (TIGIT), T lymphocyte-associated antigen 4 (CTLA-4), lymphocyte activation gene-3 (LAG-3), and the macrophage checkpoint leukocyte immunoglobulin like receptor B1 (LILRB1)28,29. M2 macrophage-mediated suppression of ImmTAC-induced T cell activation (Fig. 3e), secretion of IFN-γ (Fig. 3f), and tumor killing (Fig. 3g) was not reversed by individual checkpoint receptor blockade. We focused on neutralizing PD-1, LAG-3, and CTLA-4 checkpoint receptors, which are clinically validated in melanoma, and we assessed their combined role in M2 macrophage-mediated suppression. Simultaneous blockade of PD-1, LAG-3, and CTLA-4 did not restore IFN-γ secretion (Fig. 3f), whilst their blockade resulted in partial restoration of ImmTAC-mediated tumor killing (Fig. 3g). These findings suggest that M2 macrophage suppression of ImmTAC therapy may rely on multiple overlapping pathways and targeting individual or a subset of checkpoint receptors may not be sufficient to fully reverse the suppression.
To assess the role of well-known immunosuppressive factors secreted by M2 macrophages on ImmTAC redirection of T cells, we neutralized TGF-β, IL-10, and inhibited arginase12. Blocking these soluble factors did not reverse macrophage suppression of ImmTAC-redirected T cell activation and tumor killing (Supplementary Fig. 3b). While we cannot exclude the possibility of uncharacterized soluble inhibitory factors, these results are consistent with the hypothesis that macrophage suppression is cell-cell contact-dependent.
Pre-treatment of T cells with IL-2 enhances ImmTAC-redirected tumor killing and overcomes pro-tumoral macrophage suppression
Since targeting known inhibitory checkpoint pathways individually did not reverse M2 macrophage-mediated suppression, we explored whether augmenting T cell responsiveness to ImmTAC could reduce their sensitivity to macrophage suppression. We first evaluated and confirmed that several T cell-activating cytokines, including IL-2, IL-7, and IL-15, were capable of enhancing ImmTAC-mediated tumor killing in a dose-dependent manner in the absence of any M2 macrophages (Supplementary Fig. 4a).
IL-2 is known to reduce the TCR signaling threshold30, enhance T cell activation and proliferation, and is an approved immunotherapy for melanoma31,32. Additionally, IL-2 in combination with tumor-targeting treatments showed potential benefit in reprogramming macrophages in mouse models33. We therefore focused on IL-2 and characterized its effect on T cells and their sensitivity to M2-mediated inhibition. First, we explored simultaneous versus staggered IL-2-ImmTAC combination to assess the most effective combination strategy. Clinically relevant IL-2 doses were derived from a phase 2 trial of adoptive therapy for patients with metastatic melanoma who were administered low dose subcutaneous IL-2 (125,000 IU/kg/day)34. ImmTAC-mediated killing of tumors was enhanced by IL-2 combination where pre-treatment with IL-2 for 4 days was superior to simultaneous ImmTAC IL-2 administration (Supplementary Fig. 4b). Ensuing experiments, unless otherwise stated, used IL-2 pre-treated T cells for 4 days as effector cells to assess the combinatorial benefit of IL-2 therapy with tebentafusp.
ImmTAC-mediated activation of T cells pre-treated with IL-2 resulted in significant induction of pro-inflammatory cytokines but not enhanced CD69 expression (Fig. 4a, b and Supplementary Fig. 4c, d). Tumor killing by ImmTAC-redirected T cells was up to 2-fold higher when T cells were pre-treated with IL-2 (Fig. 4c, d). IL-2 pre-treated T cells were less susceptible to M2 macrophage suppression following ImmTAC-redirection (Fig. 4a–d).
a–d Untreated or IL-2 pre-treated T cells were used in ImmTAC-redirected co-cultures with or without M2 macrophages for 20 h. CD69 MFI quantification of CD3+CD8+ T cells (mean ± SEM, n = 7 biological replicates, Wilcoxon matched-pairs single rank test, exact two-sided p values are given) (a), IFN-γ levels in co-culture supernatants (mean ± SEM, n = 4 biological replicates, Mann Whitney test, two-sided p values < 0.05 are shown) (b), representative tumor killing flow cytometry plots (c), quantification of early and late apoptotic cells in ImmTAC-redirected cultures (mean ± SEM, n = 7 biological replicates, Wilcoxon matched-pairs single rank test, two-sided p values < 0.05 are shown) (d). e Bulk RNA-seq analysis of effector T cells sorted from co-cultures. Venn diagram shows common and uncommon differentially expressed genes in untreated or IL-2 pre-treated T cell co-cultures in the presence of M2 (blue, upregulated; red, downregulated) (n = 4 biological replicates, adj p < 0.05, absolute log2 fold change >0.75, Wald test, DESeq2). f Bulk RNA-seq heatmap plot showing the expression levels of activated CD8+ T cell-associated genes in different conditions (light green, ImmTAC-redirected; dark green, ImmTAC-redirected in the presence of M2; light purple, IL-2 pre-treated T cells in ImmTAC-redirected cultures; purple, IL-2 pre-treated ImmTAC-redirected T cells in the presence of M2 (log2 (TPM + 1), n = 4 biological replicates, genes with a log2 fold change >2 are shown). g Comparison of gene expression of T cell activation markers, cytokines, and chemokines across different donors (n = 4 biological replicates, box plots represent the interquartile range with the line set at median and whiskers show minimum and maximum values, Tukey’s multiple comparisons test, two-sided p values < 0.05 are shown). Abbreviations: E = Effectors, T = Targets, M2 = M2 macrophages, (UT) = Untreated T cells, (IL-2) = IL-2 pre-treated T cells, MFI = Mean Fluorescence Intensity, TPM = Transcripts Per Million, ns = not significant.
We used transcriptomic and flow cytometry analyses to understand the molecular mechanisms induced in T cells by IL-2 that made them less sensitive to M2 inhibition. Pre-treatment of T cells with IL-2 resulted in minimal signs of activation at the cell surface (assessed by lack of CD69 and CD25 expression; Supplementary Fig. 4c) and low levels of IFN-γ and IL-2 secretion (Supplementary Fig. 4d). Transcriptomic analysis showed that IL-2 pre-treatment results in weak upregulation of genes associated with proliferation (mean log2 fold-change = 0.9 ± 0.14 SEM) and CD8+ T cell-associated cytokines (mean log2 fold-change = 1.3 ± 0.13 SEM) (Supplementary Fig. 4e–g).
To further understand the impact of IL-2 pre-treatment on ImmTAC-redirected T cells with or without M2 macrophages, transcriptomic analysis of sorted T cells was performed after 20 h of ImmTAC-redirection. Co-culture with M2 macrophages caused a drastic reprogramming of gene expression in ImmTAC-redirected T cells, significantly upregulating 541 genes and downregulating 314 genes compared to ImmTAC-redirected T cells in the absence of M2 macrophages (Figs. 2c, 4e). In contrast, M2 macrophages had minimal effects on ImmTAC-redirected IL-2 pre-treated T cells as only 30 genes were differentially regulated (14 upregulated, 16 downregulated) in the presence of M2 macrophages (Fig. 4e), with five of these genes related to CD8+ T cell activation27 (Supplementary Table 1, Supplementary Data File 3).
Top-ranked T cell activation genes previously described by Szabo et al.27 were found to be highly induced by ImmTAC-redirection of untreated and IL-2 treated T cells in the absence of M2 macrophages (Fig. 4f). However, upregulation of these genes by ImmTAC-redirected untreated T cells was inhibited in the presence of M2 macrophages (Fig. 4f, Supplementary Table 1). Conversely, M2 macrophages had minimal influence on ImmTAC-redirection of IL-2 pre-treated T cells at the transcriptomic level relative to ImmTAC-redirected untreated T cells (Fig. 4f, Supplementary Table 1).
In addition, common cell surface marker genes of T cell activation (CD69, IL2RA) and cytokine/chemokine gene expression (IFN-γ, TNF, CXCL10, IL-2) were upregulated in response to ImmTAC-redirection of untreated and IL-2-treated T cells (Fig. 4g). M2 macrophages significantly inhibited the upregulation of these genes by ImmTAC-redirected untreated T cells, but not IL-2 pre-treated T cells (Fig. 4g). Although IL-2 pre-treated T cells were thoroughly washed prior to co-culture with macrophages, IL-2 may be captured by CD25 expressing T cells and may act in trans on M2 macrophages. In our study, M2 macrophages expressed minimal levels of IL2RA and IL2RB (Supplementary Fig. 4h), suggesting that this potential trans-signaling might not be the main driver by which IL-2 pre-treated T cells overcome M2 macrophage suppression. However, IL-2 receptor genes were found to be upregulated by M2 macrophages 20 h post co-culture with ImmTAC-redirected T cells, suggesting that they may respond to IL-2 stimulation post activation as previously described35,36 (Supplementary Fig. 4h). The mechanisms by which IL-2 renders T cells less sensitive to M2 macrophage inhibition were found to be independent of PD-1, PD-L1, TIM-3, TIGIT, CTLA-4, and LAG-3 blockade (Supplementary Fig. 5). Of note, inhibition of the PD-1/PD-L1 axis further augmented IL-2-mediated enhancement of ImmTAC-redirection of T cell activation, IFN-γ release, and tumor killing; effects which were independent of macrophage presence (Supplementary Fig. 5).
Combining ImmTAC redirection and IL-2 pre-treatment of T cells induces macrophage reprogramming from a pro- to an anti-tumoral phenotype
We previously established that the TAM-to-T cell ratio is important for T cell suppression (Fig. 1). To ascertain how T cells can overcome macrophage suppression in this scenario, we assessed whether macrophage polarization may be influenced by ImmTAC-redirection at high effector T cell-to-M2 macrophage (E:M2) ratios, given that macrophages are highly plastic and polarize their phenotype in response to their cytokine milieu. By assessing T cell activation and M2 macrophage polarization simultaneously in ImmTAC-redirected co-culture assays, we confirmed the direct correlation between E:M2 ratios and T cell activation (up to 11.5-fold±2.5 standard deviation [SD] reduction in CD69 expression in low E:M2 ratio conditions, Fig. 5a). However, at high E:M2 ratios, M2 polarization (assessed by CD163 expression) was reduced, suggesting a M2 to M1 reprogramming occurring in the presence of ImmTAC-redirected T cells. This reprogramming showed trends to be more pronounced with IL-2-pre-treated T cells (Fig. 5a). High E:M2 ratios also reduced expression of the M2 marker CD206 and increased macrophage expression of the costimulatory molecules CD40, CD80, and CD86 by macrophages (Supplementary Fig. 6).
a T cell activation marker (CD69) and M2 macrophage marker (CD163) expression by T cells and macrophages respectively using untreated or IL-2 pre-treated T cells as effectors in ImmTAC re-direction co-culture assays with different effector T cell to M2 macrophage ratios (E:M2) (n = 4 biological replicates, Tukey’s multiple comparisons test, two-sided p values < 0.05 are shown). b, c Bulk RNA-seq analysis of sorted M2 macrophages from co-cultures. Ridge density plot of PC1 scores from PCA analysis of gene expression data (21.3% variance). M1 and M2 macrophages used as reference (n = 4 biological replicates) (b), heatmap gene expression plot using M1 and M2 associated genes. Top genes plotted based on variance of expression (n = 4 biological replicates) (c). d IFN-γ induced gene expression and pro-inflammatory cytokine expression levels of M2 cells sorted from ImmTAC-redirected co-cultures using untreated or IL-2 pre-treated effector T cells (M1 and M2 cells used as reference, n = 4 biological replicates). Abbreviations: E = Effectors, T = Targets, M1 = M1 macrophages, M2 = M2 macrophages, (UT) = Untreated T cells, (IL-2) = IL-2 pre-treated T cells, MFI = Mean Fluorescence Intensity.
To further assess the extent of M2 macrophage reprogramming by ImmTAC-redirected T cells, sorted macrophages were subjected to bulk RNA-seq analysis 20 h post co-culture with ImmTAC-redirected T cells (1:1 E:M2 ratio) and their transcriptomic profiles were compared with reference M1 and M2 macrophages using dimension reduction (Fig. 5b, Supplementary Table 2) and gene set enrichment analyses (Supplementary Fig. 7) using published gene signatures (Supplementary Table 3)37,38,39. We found that M2 macrophages were reprogrammed towards M1 macrophages at the transcript level in the presence of ImmTAC-redirected T cells. This reprogramming was more prominent when macrophages were exposed to ImmTAC-redirected IL-2-pre-treated T cells (Fig. 5b, Supplementary Table 2).
Based on variance, we highlighted expression of the top 15 M1- and M2-associated genes from published gene signatures (Fig. 5c, Supplementary Table 4), further supporting ImmTAC-mediated M2 to M1 macrophage reprogramming. Since IFN-γ is a master regulator of M1 macrophage polarization40,41, we explored IFN-γ signaling-related genes such as IFITM1, ISG15, IRF138,40, and downstream cytokines/chemokines including CXCL10, IL-1B, TNF40. M2 macrophages exposed to ImmTAC-redirected T cells substantially upregulated IFN-γ-inducible genes to similar levels observed in M1 macrophages that had been polarized with recombinant IFN-γ and lipopolysaccharide (LPS) (Fig. 5d).
To evaluate whether M2 macrophage reprogramming by ImmTAC-redirected T cells was cell contact dependent, we subjected M2 macrophages to supernatants derived from ImmTAC-redirected untreated or IL-2-pre-treated T cells (Supplementary Fig. 8a). M2 macrophages downregulated surface expression of CD206 and upregulated CD86 whilst CD163 levels remained unaltered when cultured with ImmTAC supernatants, suggesting that ImmTAC-mediated M2-M1 reprogramming is partially mediated through soluble factors (Supplementary Fig. 8b). These reprogrammed macrophages lost the ability to suppress ImmTAC-mediated redirection of T cells against tumor cells (Supplementary Fig. 8c).
High ratio of CD163+ TAM-to-T cells in tumor biopsies is associated with short OS on tebentafusp treatment
We described that pro-tumoral macrophages suppress ImmTAC-redirected T cell activation and killing in vitro (Fig. 1). This led to the hypothesis that the relative number of TAM compared to T cells in tumor biopsies may modulate clinical outcomes with ImmTAC therapy. We, therefore, investigated the effect of TAM on clinical outcomes in patients treated with tebentafusp, a TCR-CD3 bispecific that targets gp100 on melanoma cells. Baseline tumor biopsies from metastatic uveal melanoma (mUM) patients treated with tebentafusp in a phase 1/2 study (IMCgp100-10226) were analyzed by immunohistochemistry. CD163 and CD3 markers were used to identify immunosuppressive TAM and T cells respectively. High immunosuppressive TAM (CD163+) counts alone within the TME at baseline were not associated with OS on tebentafusp (hazard ratio [HR] = 1.37; 95% confidence interval [CI], 0.85-2.22; p = 0.193, Fig. 6a). Similarly, high CD3+ T cell levels alone within the TME at baseline were not associated with OS (HR = 0.82; 95% CI, 0.52-1.29; p = 0.393; Fig. 6a). However, patients with high CD163+ TAM-to-CD3+ T cell ratios (ratio of CD163:CD3 > 2) at baseline had shorter OS compared with those with a low CD163+ TAM-to-CD3+ T cell ratio prior to treatment (HR = 2.09; 95% CI, 1.31-3.33; p = 0.002; Fig. 6b, c). Similarly, patients with high CD163+ TAM-to-CD3+ T cell ratio showed less tumor reduction upon tebentafusp treatment (odds ratio [OR] = 3.07; 95% CI, 1.17-8.41; p = 0.02; Supplementary Fig. 9a).
a Kaplan-Meier plot of OS of patients on tebentafusp treatment. Patients stratified by CD163+ TAM, and CD3+ T cells (hazard ratios [HR] and p values using Cox likelihood ratio test are shown). b Kaplan-Meier plot of OS of patients on tebentafusp treatment. Patients stratified by CD163:CD3 high (orange) and low (blue) by lower quantile cutoff (LQ) (n = 117 baseline biopsies from tebentafusp-treated patients, HR and p values using Cox likelihood ratio test are shown). c Representative immunohistochemistry images (from n = 117 individual patients) of tumor infiltrating CD3+ T cells and CD163+ TAM. Low CD163:CD3 ratio (mean) determined as 1:2 (SD±0.3) and high CD163+:CD3+ ratio (mean) is 6:1 (SD±11). d Representative immunofluorescence images (from n = 14 individual patients) of a patient with high CD163: CD3 ratio (DAPI [blue], SOX10 [cyan], CD3 [green], CD163 [red]). Abbreviations: LQ = lower quartile, TAM = Tumor-associated macrophages, HR = Hazard Ratio, CI = Confidence Interval.
We previously established that M2 macrophages exerted their inhibitory function through direct cell-cell contact (Fig. 3a–d). To establish whether direct TAM-T cell interactions occur in tebentafusp-treated mUM patients, we stained a subset of baseline tumor biopsies from patients with high CD163+ TAM-to-CD3+ T cell ratio (n = 14) with a custom multi-immunofluorescence panel of markers including CD3 (T cells), CD163 (TAM), and SOX10 (tumor cells), followed by nearest neighbor spatial image analysis (Fig. 6d, Supplementary Fig. 9b). We defined direct TAM-to-T cell interaction based on distances of no more than 10 µM as previously described42,43. Direct TAM-to-T cell interactions were identified in all tumor biopsies analyzed with a mean of 21% of tumor infiltrating CD3+ T cells being in direct contact with CD163+ TAM (range 10% -36%).
These results are consistent with the hypothesis developed from the in vitro cell culture experiments and highlight the importance of the ratio of macrophages to T cells in macrophage-mediated suppression of ImmTAC activity in vivo.
Tebentafusp treatment induces upregulation of anti-tumoral macrophage gene signatures in patients with mUM
Since ImmTAC can re-polarize pro-tumoral M2 macrophage to anti-tumoral M1 in T cell co-cultures, we assessed whether ImmTAC treatment can influence macrophage polarization in vivo. We performed gene-set enrichment analysis of tumor biopsies of patients with mUM collected at baseline and after 3 doses of tebentafusp treatment (Fig. 7a) to determine M1- and M2-associated gene signatures37,38,39,44 (Fig. 7b, Supplementary Table 3). We found an enrichment of M1 macrophage-associated genes (normalized enrichment score [NES] =0.7, adjusted p = 0.003) but not M2 macrophage-associated genes (NES = 0.37, p = 0.62, Fig. 7b).
a Schematic illustration of tumor sample processing for bulk RNA-seq. b Gene set enrichment analysis using M1- and M2-associated gene list in bulk RNA-seq of patients 16 days on tebentafusp treatment (n = 35 patients, two-sided adjusted p values are shown using ReactomePA package). c Selected M1-associated and M2-associated gene expression pre-treatment and 16 days on-tebentafusp treatment in patients with mUM (n = 35 patients, paired Wilcoxon test, two-sided p values < 0.05 are shown). Abbreviations: M1 = M1 macrophages, M2 = M2 macrophages, FC = Fold-change, TPM = Transcripts Per Million, NES = Normalized Enrichment Score, ns = not significant.
Gene expression of inflammatory markers (IL-1B, IFN-γ-inducible chemokines CXCL10, CXCL11, and IFN-γ-induced IRF1 and IFITM1) was significantly upregulated in tumor biopsies collected after 3 doses of tebentafusp treatment (1.3–2.5-fold-change, Fig. 7c). Conversely, the M2 macrophage-associated genes CA2 and ARG145,46 were significantly downregulated (0.9–1.3 fold-change) in post tebentafusp treatment biopsies (Fig. 7c).
Since the above-mentioned explorations relied on bulk RNA-seq analysis, we could not exclude the potential contribution of other myeloid cells, including dendritic cells, which can also express a number of macrophage-associated genes47,48. We therefore extended our analysis to explore baseline TAM using single-cell RNA-seq analysis of eight tumor biopsies from patients with mUM (Supplementary Figs. 10 and 11). One of these patients was HLA-A*02:01+ and treated with tebentafusp as first-line therapy. Prior to treatment with tebentafusp, this patient had four non-evaluable hepatic lesions and one measurable liver metastatic lesion, which remained stable by RECIST 1.1 criteria on tebentafusp treatment for 18 months, followed by surgical removal (Fig. 8a, Supplementary Fig. 10, Supplementary Table 5). We explored the genomic profile of TAM from this patient’s baseline and on-treatment tumor samples. Tumor and immune cells were clustered using unsupervised clustering approach (Supplementary Fig. 10a, b, Supplementary Data File 4) and myeloid cells (including TAM) were annotated using published gene signatures37,38,39. Prior to tebentafusp treatment, TAM and monocytic precursors made up 55.1% (±16 SD) of all myeloid cells in the tumor biopsy and expressed M2-associated gene signatures (Supplementary Fig. 11d, e). The tumor sample collected after 18 months of tebentafusp treatment showed the emergence of a second TAM cluster which consisted of 55.6% of all identified TAM populations (Fig. 8b, c). Transcriptomic analysis of all myeloid cells using M1- and M2-associated gene lists revealed that 7 out of 9 most expressed genes within the myeloid compartment were M2-associated and were expressed by all TAM populations, whilst 2 out of 9 most expressed genes were M1-associated (NFKBIA and NAMPT) and were found to be expressed within the tebentafusp-induced TAM and monocyte clusters (Fig. 8d). This was confirmed using a multivariate linear model analysis where M2 gene signature was significantly associated with TAM subsets whilst M1 gene signature was confined to monocytes and tebentafusp-induced TAM (Fig. 8e). Transcriptomic profiling of pre-treatment TAM and tebentafusp-induced TAM population using M1- and M2-associated gene lists further revealed that tebentafusp-induced TAMs expressed considerably more M1-associated genes with inflammatory and anti-tumoral functions such as CCL4, IL1B, NFKB1, IRF1 and IRF7 compared with pre-treatment TAM (Fig. 8f, g, Supplementary Table 3, and Supplementary Data File 4). Notably, both baseline and tebentafusp-induced TAM populations expressed similar levels of M2-associated genes apart from genes such as ITGA4, LGALS9, and TGFB1, which were downregulated in tebentafusp-induced TAM populations (Fig. 8f, g). Taken together, these results demonstrate the effect of tebentafusp on macrophage reprogramming from a pro- to an anti-tumoral phenotype as early as day 16, after 3 doses of tebentafusp, and up to 18 months on treatment.
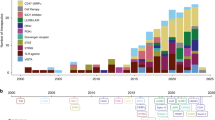
a Schematic illustration of tumor sample processing for single-cell RNA sequencing from a patient prior to, and 18 months on tebentafusp treatment. b UMAP plot showing the monocyte, dendritic cell, and macrophage clusters in tumors prior to, and 18 months on tebentafusp treatment. c Percentages of pre-treatment TAM and tebentafusp (Tebe)-induced TAM among the total identified TAM population (range 0-1). d UMAP plots showing the most expressed M1 and M2 genes. e Multivariate linear model analysis of M1 and M2 signatures across myeloid populations (* shows signatures that are significantly enriched or depleted in the indicated cell type). f Average expression of M1 and M2 associated genes in tebentafusp-induced and pre-treatment TAM subsets (p values are shown using a Wilcoxon rank sum test). g M1- and M2-associated gene expression profiles of pre-treatment TAM and tebentafusp-induced TAM populations (n = 1 patient). Abbreviations: M1 = M1 macrophages, M2 = M2 macrophages, Tebe = tebentafusp, TAM = Tumor-associated macrophages.
Discussion
In this study, we investigated the role of TAM in ImmTAC-mediated tumor killing both in vitro and in patients with mUM treated with tebentafusp. We identified an additive effect of IL-2 pre-treatment combined with ImmTAC-mediated redirection of T cells in counteracting TAM-mediated immunosuppression and TAM reprogramming towards an anti-tumoral phenotype. Both outcomes were strongly dependent on TAM-to-T cell ratios and their cell-cell interactions.
Presence of TAM in cutaneous melanoma has been associated with poor OS in multiple studies49,50,51. Evidence for the prognostic role of TAM in patients with UM remains contradictory. An early study showed that high levels of TAM, defined by either CD68 or CD163 expression, in primary UM correlated with poor OS23. Later studies in mUM showed that above median expression of CD68, but not CD163, expression correlated with longer OS following isolated hepatic perfusion24. More recently, Mariani et al.25 showed that the level of TAM (CD68+ or CD163+) was higher in biopsies of mUM compared with primary UM. Moreover, CD68 positivity at the metastatic site was associated with longer OS25. Our findings may explain some of these discrepancies, as we found that the CD163+ TAM-to-CD3+ T cell ratio is a key determinant of clinical outcome, rather than CD163+ TAM infiltration alone. TAM-mediated immunosuppression appears to be particularly relevant in conditions with high TAM levels and low T cells. While we cannot exclude the possibility that CD163+ TAM-to-CD3+ T cell ratio may be prognostic, the potential association with tumor reduction observed in our study suggests that it may be specific to CD3 T cell engagers. However, it must be noted that RECIST response underestimates the survival benefit from tebentafusp as previously reported26.
ImmTAC-induced T cell activation resulted in immune checkpoint marker upregulation in our in vitro co-culture model, however blockade of individual checkpoint receptors did not alleviate macrophage-mediated suppression, nor did inhibition of well-known soluble factors including TGF-β and arginase, suggesting the existence of additional or overlapping mechanisms by which M2 macrophages exert their suppressive function. One potential mechanism could be spatial constraints restricting T cell access to tumors or depletion of essential T cell nutrients, particularly at high M2 macrophage-to-T cell ratios. However, this is unlikely to be the sole mechanism of suppression given that M1 macrophages were found to be less suppressive at the same macrophage-to-T cell ratios.
We explored an alternative approach to enhance T cell activation through cytokine pre-treatment to decrease the TCR signaling threshold and reduce T cell sensitivity to M2 macrophage inhibition. We utilized IL-2, given its documented pleiotropic effects on T cell activation and proliferation and its role in enhancing immunotherapy efficacy31. Concurrent signaling of IL-2 and TCR has been shown to be necessary for memory CD8+ T cell development and secondary antigen-dependent activation52. In our in vitro models, T cell pre-treatment with IL-2 resulted in a transcriptional shift to an activation goldilocks state where T cells showed minimal signs of phenotypic and functional activity in the absence of ImmTAC, while they were significantly more responsive when redirected by ImmTAC against tumors. Additionally, our macrophage phenotype analysis revealed that ImmTAC redirection induces strong macrophage reprogramming, which synergizes with IL-2 pre-treatment. These results suggest that combining IL-2 with ImmTAC therapy may reduce the impact of suppressive macrophages and offer enhanced therapeutic benefits compared with ImmTAC alone. Taken together, our data lays the foundation for the clinical evaluation of ImmTAC and IL-2 combination therapies. Agents that could be explored include aldesleukin31, which is approved for treatment of metastatic renal cell carcinoma and metastatic melanoma53, and other engineered IL-2 molecules that preferentially activate effector T cells but not Tregs54.
The concept of reprogramming TAM to be anti-tumoral has recently gained significant interest, as increasing evidence indicates that TAM exhibit multiple phenotypes in tumors including mUM55. Our study is the first to demonstrate that tebentafusp can reprogram suppressive TAM towards an anti-tumoral phenotype both in vitro and in the clinic, after just 3 doses. This reprogramming is likely driven by IFN-γ-mediated signaling as indicated by RNA-seq data revealing an increase in IFN-γ signaling-dependent gene expression in response to ImmTAC-mediated T cell redirection. Qin et al.56 have shown that in patients with mUM, IFN-γ-mediated pathways play a crucial role in predicting responses to immune checkpoint blockade, supporting our findings that IFN-γ signaling may play a key role in patients responding to ImmTAC-redirected therapy. However, in vitro reprogramming occurs concurrently with macrophage-mediated T cell suppression, further emphasizing that both aspects depend on the TAM-to-T cell ratio.
Single-cell RNA sequencing of tumors from a patient with mUM confirmed that TAM upregulate anti-tumoral markers on tebentafusp treatment. However, it remains unclear whether these tebentafusp-induced TAM reflect a transcriptional shift from pro-tumoral towards anti-tumoral or the recruitment of de novo macrophages to the TME, or perhaps both. Nonetheless, these findings suggest that ImmTAC therapy can induce a long-lasting effect on the TME and on TAM phenotypes that is favorable to T cell immunotherapy. Interestingly, despite significant genetic reprogramming towards an anti-tumoral phenotype, these cells did not demonstrate reduced expression of M2-associated markers such as MRC1, CD163, or CD209. While these biomarkers are used to identify M2 macrophages, their immunosuppressive role, especially when co-expressed with anti-tumoral M1 markers, remains unclear. Of note, in the in vitro setting, CD163 was found to be downregulated at high M2-to-T cell ratio further highlighting the need to fully characterize whether these reprogrammed macrophages in patient tumors exhibit functional anti-tumoral properties such as killing and phagocytosis of tumor cells, and T and NK cell activation57.
Altogether, our study highlights the importance of the TAM-to-T cell ratio in determining clinical response to ImmTAC immunotherapy. We conclude that at low TAM-to-T cell ratios, T cell engagers such as tebentafusp can reshape the TME towards an anti-tumoral environment, while in patients with high TAM-to-T cell ratios, combining ImmTAC with IL-2 would allow T cells to overcome TAM-mediated inhibition and thus augment anti-tumor activity (Supplementary Fig. 12). Our observations provide strong rationale for testing this combination in the clinic.
Methods
Clinical studies
Tumor biopsies were obtained from patients with mUM enrolled in the phase 2 IMCgp100-102 study (NCT02570308)26. This was a multicenter, single-arm, open-label phase 2 study of tebentafusp in 127 HLA-A*02:01+ patients with treatment-refractory mUM. The primary endpoint was objective response rate based on RECIST v1.1. Samples for single-cell RNA-seq were derived from a patient from the IMCgp100-202 study (NCT03070392)6,7, a phase 3 study of previously untreated HLA-A*02:01+ patients with mUM. Patients were randomized 2:1 to receive tebentafusp or the investigator’s choice of therapy with either pembrolizumab, ipilimumab, or dacarbazine, stratified according to the lactate dehydrogenase level and the primary endpoint was OS.
Patient tumor biopsy for immunohistochemistry
Tumor biopsies were collected prior to tebentafusp infusion. Biopsies were fixed and processed for immunohistochemistry analysis. After blocking with Discovery Inhibitor (Roche Diagnostics), the following primary antibodies were used: CD3 (2GV6, Roche Diagnostics) and CD163 (MRQ-26, Roche Diagnostics). Antibody staining was amplified using horseradish peroxidase-labeled secondary antibodies, detected using purple kits, and counterstained with hematoxylin and bluing reagents on the Ventana autostainer (reagents from Roche Diagnostics). Slides were dehydrated and cover slipped. Stained slides were scanned using either the MIDI II (3DHISTECH) or Pannoramic 250 FLASH III (3DHISTECH) Whole-Slide Scanners. Digital image analysis of the scanned images was carried out using HALO™ software (Indica Labs) to quantify the number of positive CD3 and CD163 cells within the tumor, peri-tumoral stroma, and TME (tumor + peri-tumoral stroma).
A subset of tumor biopsies was stained with a custom multiplex immunofluorescence (mIF) InSituPlex® panel of markers including CD3, CD163, and SOX10, nuclear staining was detected with DAPI (Ultivue). Slides were scanned with the Axioscan Z1 scanner (Zeiss). Image processing was carried out on the STARVUE Image Data Science Platform, images were co-registered by Ultistacker.AI software and UltiAnalyzer.AI was used to quantify cell densities and signal intensities on the mIF images (Ultivue). Nearest neighbor analysis was conducted to assess the spatial relationships between cells. Cell coordinates were mapped and the distance between each cell and its nearest neighbors was calculated using NearestNeighbour function from scikit-learn python package (v1.5.2) and visualized with squidpy package (1.5.0). For each cell, only neighbors located within 10 microns were included to limit the analysis to cells with direct contact.
Patient tumor biopsy for bulk-RNA sequencing
RNA sequencing libraries were generated from tumor biopsy samples, which had been placed in RNAlater or were snap frozen, using the Illumina TruSeq stranded mRNA kit at E.A.Genomics. Paired end fragments of 100 bp length were sequenced (50 million reads per sample) using the Illumina Novaseq system. Following sequencing, raw FASTQ files were trimmed using Trim Galore (v0.6.2)58, and quality was assessed using FastQC and MultiQC (v1.9)59. The resulting reads were aligned using STAR aligner (v2.5)60. Reads were mapped to the GRCh38 primary assembly provided by Ensembl. Gene expression was quantified using RSEM (v 1.2.25)61. Transcript per kilobase per million (TPM) values were log2 transformed in R. A pseudo-count value of 1 was added to each TPM value prior to transformation.
T cell and monocyte isolation from PBMC
Peripheral blood mononuclear cells (PBMC) were derived from blood from healthy individuals who consented to donate at Immunocore as part of a UK Health Research Authority-approved study. PBMC were isolated from fresh blood by using Lymphoprep™ density gradient media. Monocytes were positively selected from PBMC by using CD14+ Microbeads, while pan T cells were negatively selected using the pan T cell Isolation Kit (Miltenyi Biotec). Isolated cells were stored in liquid nitrogen in freezing medium (10% dimethyl sulfoxide (DMSO, Sigma-Aldrich) + 90% fetal bovine serum (FBS)).
Cell lines
A375 cell line was derived from a 54-year-old female with malignant melanoma (CRL-1872TM, ATCC). MP41 cell line was derived from a 49-year-old female with uveal melanoma (CRL-3297TM, ATCC). THP-1 cell line was derived from a 1-year-old male with acute monocytic leukemia (TIB-202TM, ATCC).
Cell culture
Primary T cells, macrophages, and THP-1 cells were cultured in R10 medium (RPMI 1640 media supplemented with 10% fetal bovine serum (FBS), 1% L-Glutamine (Gibco), and 1% Penicillin-Streptomycin (Gibco)). A375 human cutaneous melanoma cells were cultured in 10% DMEM medium supplemented with 4.5 g/L glucose (Gibco). CD14+ monocytes sorted from PBMC were cultured in 50 ng/ml human recombinant macrophage colony-stimulating factor (Peprotech) for six days in six-well plates for macrophage differentiation. Cells were differentiated into M2 macrophages in 20 ng/ml IL-4 (BioLegend) or differentiated into M1 macrophages by using 50 ng/ml IFN-γ (BioLegend) and 10 ng/ml LPS (Sigma-Aldrich) for 24 h. Macrophages were detached from the flask by washing with ice cold PBS buffer with 2% FBS and 2 mM Ethylenediaminetetraacetic acid solution (EDTA, Sigma-Aldrich). Untreated and IL-2 pre-treated T cells were cultured for four days in either R10 medium or R10 medium supplemented with 150 IU/ml aldesleukin (Proleukin®, Novartis) respectively. T cells were then thoroughly washed with PBS and resuspended in fresh R10 medium before use in co-culture assays. For xCELLigence cytotoxicity measurements, PBMC were treated for four days with increasing concentrations of aldesleukin, recombinant IL-7, or IL-15 (Miltenyi Biotec).
Co-culture assays
Tumor cells were washed with PBS and labeled with 1 µM Cell Tracer Violet (CTV) (Thermo Fisher Scientific) for 15 min at 37 °C. 1 × 105 CTV-labeled THP-1 cells were seeded in U-bottom 96-well plates and 5 × 104 M2 macrophages and 5 × 104 untreated or IL-2-treated T cells were added on each well. Cells were incubated for 90 min at 37 °C before addition of 0.1 nM of ImmTAC molecule (Immunocore) on the co-cultures. Supernatants were collected 20 h or 48 h later for cytokine analysis. Cells were analyzed using flow cytometry. For mechanism of action studies, nor-NOHA monoacetate (BioTechne), TGF-β, IL-10 (Thermo Fisher Scientific), Tim-3, CTLA-4 (BioLegend), TIGIT (Tebu-Bio), LAG-3 (Abcam), and LILRB1 (Thermo Fisher Scientific) neutralizing antibodies, and pembrolizumab and atezolizumab (Selleck Chemicals GmBH) were used. For transwell co-culture assays, 96-well transwells (Corning) with 1 µm pore size were used. Macrophages were seeded on top of the transwell; tumor cells and T cells were seeded on the bottom well of the plate. Cells were co-cultured for 24 h.
PBMC-mediated cytotoxicity was measured by xCELLigence. 15 × 103 uveal melanoma MP41 cells were seeded into 96-well E-Plates (PET) and placed in an xCELLigence RTCA MP instrument (ACEA Biosciences, USA). Cell impedance was recorded for 24 h at 37 oC and 5% CO2. Plates were then removed and either untreated or cytokine pre-treated PBMC in 5:1 (E:T) ratio were added in the presence or absence of 100 pM ImmTAC (Immunocore). MP41 tumor cell lysis was then tracked in real-time based on the tumor impedance-derived cell index for three days in accordance with the manufacturer guidelines. Impedance-derived normalized cell indexes from target alone and target effector and ImmTAC cocultures were used to estimate PBMC cytolytic activity over time. Area under the curve (AUC) values over 72 h cytolysis were calculated.
Cytokine multiplex assays
Co-culture supernatants were collected and IFN-γ, CXCL11, IL-2, TNF-α cytokine levels were measured using Meso Scale Discovery (MSD) V-Plex or Milliplex MAP 11-plex custom magnetic bead panel (Millipore) according to manufacturer instructions. Samples were diluted 1:25 and cytokines were measured by electrochemiluminescence detection technology ~620 nm by MSD Quickplex SQ 120 or Luminex Magpix® instrument xPONENT 4.3. Total cytokine levels were quantified by using linear regression curves in MSD Discovery Workbench or xPONENT 4.2 software.
Flow cytometry
Co-cultures were harvested 24 h after ImmTAC treatment and washed with cold PBS supplemented with 2% FBS and 2 mM EDTA. For T cell activation analysis, cells were labeled with anti-human CD3, CD69, CD8, CD25, LAG-3, and PD-1 (BioLegend). For M1 and M2 phenotype analysis, cells were labeled with CD163, CD40 (BioLegend), CD206, CD86, CD80 (BD Bioscience). Viability of cells was assessed by Zombie NIR live/dead staining (BioLegend) or 7AAD Staining solution and APC Annexin V for apoptosis detection kit (BioLegend). Samples were then acquired on a BD LSRFortessaTM X-20 flow cytometer (BD Bioscience) or ID7000 spectral analyzer (Sony). Data analysis was performed using FlowJo V10.7.1 (Tree Star Inc, USA). A full list of antibodies and reagents used in this study is provided in Supplementary Data File 5.
Cell sorting and bulk-RNA sequencing in vitro
T cells and macrophages were sorted from co-cultures 20 h after ImmTAC-redirected killing. Cells were sorted using a Sony MA900 Multi-Application Cell sorter (Supplementary Fig. 2). To sort T cells only, cells were labeled with CTV dye before their addition to co-cultures. For macrophage sorting, THP-1 tumor cells were labeled with CTV, while macrophages were labeled by CD163 (BioLegend), and CTVmid/-CD163high cells were sorted. Sorted T cells and macrophages were lysed by RLT buffer (Qiagen), and samples were processed for RNA extraction. Sample RNA was extracted by RNA Micro-column extraction kit (Qiagen). T cell RNA-seq libraries were prepared by using NEBNext® Ultra II Directional RNA Library Preparation Kit, Strand-specific, PE100 Base Reads (60 M Total Reads). For macrophage RNA-seq analysis, low-input Poly A+ RNA (Takara Bio) used to enrich mRNA transcripts with 50 M paired samples, in total 100 M reads. SMART-Seq HT PLUS mRNA Library Construction (PolyA + Capture) were used (Takara Bio), 250 pg to 10 ng amount of RNA used prior to amplification, sequencing was done on NovaSeq 2X 100 bp PE. Following sequencing, raw FASTQ files were trimmed using Trim Galore (v0.6.2)58, and quality was assessed using FastQC and MultiQC (v1.9)59. The resulting reads were aligned using STAR aligner (v2.5)60. Reads were mapped to the GRCh38 primary assembly provided by Ensembl. Gene expression was quantified using RSEM (v 1.2.25)61. Transcript per kilobase per million (TPM) values were log2 transformed in R. A pseudo-count value of 1 was added to each TPM value prior to transformation. Downstream analysis and plotting of the data were carried out in R. Batch normalization against lot number was carried out using the Limma package62. Differential expression analysis was carried out using DESeq263, controlling for patient as a batch effect. Differentially expressed protein coding genes were filtered using adjusted p-value < 0.05 and absolute log2 fold change > 0.75. BiomaRt64 was used for gene name ID conversion. The package ReactomePA65 was used to carry out functional overrepresentation analysis, with pathways considered significant if the adjusted p-value was <0.05.
Preparation of single cell suspension from biopsies for single-cell RNA-sequencing
After surgery, liver metastasis biopsies from patient 1 to 8 (corresponding IDs: UM2101, PULSE1291, UM0039, UM0015, UM0006, UM0004, UM0041, and UM0019 respectively, Supplementary Table 5) were placed in DMEM culture medium (Gibco) and transported to the CNAG (Centro Nacional de Análisis Genómico) on ice. Upon arrival, samples were transferred in a 10 mm Petri dish on ice, washed twice with cold 1X Hank’s Balanced Salt Solution (HBSS, Thermo Fisher Scientific), and minced using a razor blade. Next, the samples were digested for 20 min at 37 °C with 2 mL of a pre-warmed dissociation mix (200 U/ml Collagenase II and DNAase I [Sigma-Aldrich] in 1X HBSS) with gentle shaking in a thermomixer. Enzymatic digestion was stopped by adding 10% FBS (Thermo Fisher Scientific) and cell suspension filtered with a 70 μm and 40 cell μm strainer (Corning). Cells were washed with 1X HBSS and centrifuged for 5 min at 400 × g at 4 °C. Cells were counted and processed for analysis. The on-treatment sample belonging to patient 8 (ID UM2146) was previously disaggregated and cryopreserved at IDIBELL and successively sent to CNAG for processing. A cryotube containing approximately 2 million cells was thawed and transferred into a pre-warmed media (Hibernate-A [Gibco] supplemented with 10% FBS). Cells were centrifuged at 200 × g for 8 min at 4 °C and counted for analysis.
CD45-positive cells enrichment for single-cell RNA-sequencing
CD45-positive cells from sample IDs UM2101, UM0041, and UM0019 (Supplementary Table 5) were isolated by Magnetic-activated cell sorting (MACS) using the OctoMACS™ Separator and MS columns (Miltenyi Biotec) according to manufacturer instructions. CD45-positive cells from sample IDs PULSE1291 and UM2146 were isolated using the EasySep™ Release Human CD45 Positive Selection Kit (StemCell Technologies) following manufacturer instructions. The pooled eluates were concentrated by centrifugation at 4°C and resuspended in appropriate volume of 1X PBS with 0.05% bovine serum albumin (Thermo Fisher Scientific) and counted.
Cell encapsulation and single-cell RNA-sequencing library preparation
Samples were loaded for a Target Cell Recovery between 3000 and 8000 cells on the Chromium Controller instrument (10X Genomics). More specifically, baseline samples UM0039, UM0015, UM0006, UM0004, UM0041, and pre-treatment sample UM0019, were encapsulated using the Chromium Next GEM Single Cell 3’ Reagent Kit v3, while baseline samples belonging to UM2101, PULSE1291 and on-treatment sample UM2146 were encapsulated using the Chromium Next GEM Single Cell 5’ Reagent Kit v1.1 (sample UM2101) and v2 (samples PULSE1291 and UM2146, Supplementary Table 5). cDNA libraries were prepared following manufacturer instructions of protocol CG000183 for the standard 3’ assay, and protocols CG000207 and CG000331 for 5’ assay. Sequencing was carried out on a NovaSeq6000 system (Illumina) using the following sequencing conditions: 28 bp (Read 1) + 8 bp (i7 index) + 0 bp (i5 index) + 91 bp (Read 2) for single indexed libraries and 28 bp (Read 1) + 10 bp (i7 index) + 10 bp (i5 index) + 90 bp (Read 2) for dual-indexed libraries. Approximately 40,000 read-pairs per cell for the Gene Expression (GEX) library and 10,000 read-pairs per cell for the TCR library were obtained after sequencing.
Single-cell RNA-sequencing data analysis
Raw sequencing data (FASTQ) was processed using Cellranger Multi1 (v6.0.1, 10x Genomics) to align reads to the GRCh38 human genome. Low-quality cells were filtered in a sample-specific manner. Overall, excluded cells with less than 200 and more than 30,000 unique molecule identifiers, less than 100 and more than 6000 detected genes or a mitochondrial expression larger than 25% of the transcriptome (potentially broken cells or empty droplets). To harmonize samples across patients, batches, and libraries, we performed a standard downstream analysis with Seurat3 and integration with Harmony4. All these steps were carried out in R4.2.25 and used Harmony batch correction algorithm, across batches, libraries, and patients. The main clusters were identified after principal component analysis using the Louvain algorithm. Identified clusters were annotated in a marker-gene-based manner using Seurat’s FindAllMarkers function. This process was repeated also for annotated cluster subsets such as immune cells and myeloid compartments. Bad-quality clusters (those only expressing mitochondrial genes) and those with high-doublet scores (computed using Scrublet) were removed. Throughout the analysis of myeloid clusters, Ucell7 package and published gene signature datasets were used37,38,39.
Ethical approvals for use of human material
All uses of human material have been approved for this study. The use of PBMC from healthy donor volunteers for the in vitro investigations was approved by the Oxford A Research Ethics Committee under study protocol reference 13/SC/0226. All participants provided written informed consent.
Ethical approval for the use of tumor biopsies obtained from uveal melanoma patients treated with tebentafusp were obtained through the phase 2 IMCgp100-102 study (NCT02570308)26 which was approved by the relevant ethics bodies at each participating site as published by Carvajal et al.26. This trial was carried out in accordance with the principles of the Declaration of Helsinki and Good Clinical Practice guidelines, and the study protocol was approved by the relevant ethics bodies at each participating site: Princess Margaret Cancer Centre, Toronto, Canada; Charite Universitaetsmedizin Berlin—Campus Benjamin Franklin, Berlin, Germany; Universitaetsklinikum Heidelberg, Heidelberg, Germany; Institut Catala d’Oncologia (ICO) l’Hospitalet, Hospital Duran i Reynals, Barcelona, Spain; Hospital Universitario Virgen Macarena, Seville, Spain; Centro de Investigación Biomédica en Red de Cáncer (CIBERONC), Madrid, Spain/Hospital Universitario La Paz, Madrid, Spain; Hospital General Universitario de Valencia, Valencia, Spain; The Clatterbridge Cancer Centre, Wirral, UK; Mount Vernon Cancer Centre, Northwood, UK; Columbia University Medical Center, New York, USA; Washington University School of Medicine, St Louis, USA; Thomas Jefferson University Hospital, Philadelphia, USA; Vanderbilt University Medical Center, Nashville, USA; Memorial Sloan Kettering Cancer Center, New York, USA; University of Colorado Cancer Center, Aurora, USA; The Angeles Clinic and Research Institute, a Cedars-Sinai Affiliate, Los Angeles, USA; H. Lee Moffitt Cancer Center and Research Institute, Inc., Tampa, USA; University of California San Diego Moores Cancer Center, La Jolla, USA; California Pacific Medical Center, San Francisco, USA; Baylor Scott & White Health, Dallas, USA; Dean A. McGee Eye Institute, University of Oklahoma, Oklahoma City, USA; Georgetown University—Lombardi Comprehensive Cancer Center, Washington, USA; University of Miami Hospital Clinics/Sylvester Comprehensive Cancer Center, USA; The University of Chicago Medical Center, Chicago, USA; Roswell Park Cancer Institute, Buffalo, USA; and Providence Portland Medical Center, Portland, USA. All Patients provided written informed consent before being screened for enrollment.
The use of tumor biopsies from uveal melanoma patients for single-cell RNA-seq analysis was approved by The Hospital de Bellvitge/Catalan Cancer Institute Institutional Review Boards and Ethics Committee at IDIBELL. All recruited patients provided informed consent for this study.
For all analyses using human material in this study, sex and gender of trial participants and healthy volunteers were not considered in the study design.
Statistical analysis
Statistical analyses of in vitro biological assays were calculated using GraphPad Prism 9.0.1. Data is presented as mean ± SEM unless otherwise indicated. Matched pairs were compared by Wilcoxon matched-pairs single-rank test and unmatched groups were compared by Mann-Whitney test and Tukey’s multiple comparisons test. All comparisons were two-sided and p values below 0.05 were considered statistically significant. Survival analysis was carried out using the R package survminer v0.4.9, the Cox likelihood ratio test was used to assess differences between survival curves, whilst Wald test (DESeq2) was used for differential gene expression analysis. Univariate Cox proportional hazards methods (R package survival v3.2-11) were used to model the prognostic importance of potential predictors of survival. Fisher’s exact test was used to compare categorical data between groups (R stats package 4.1).
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
All data are included in the article and its supplementary Information. The raw values for charts and graphs are available in the Source Data File whenever possible. All differentially expressed gene datasets identified in this study have been provided in Supplementary Tables and Data Files within this manuscript. Information on all commercially available and unique reagents used in this study have been provided in the supplementary Information (Supplementary Data File 5).
Bulk RNA sequencing data from the in vitro studies (healthy donor T cells and macrophages) have been deposited in European Genome-phenome Archive (EGA) under EGAD50000001226. Bulk RNA sequencing data from tumor biopsies from mUM patients have been deposited in EGA under the EGAD50000001225. Single cell RNA sequencing from tumor biposies from mUM patients have been deposited in Gene Expression Omnibus (GEO) under GSE287090. To access RNA sequencing data, researchers should submit their request including purpose, hypothesis, and rationale through The EGA repository platform (https://ega-archive.org/). Access will be subject to approval by the relevant committee at Immunocore Ltd to comply with patient consent and to determine the scientific purpose of data reuse. Source data are provided with this paper.
Code availability
No custom-made code was generated for this study and all publicly available r packages are listed in the methods section of this manuscript.
References
Kantarjian, H., Jabbour, E. & Topp, M. S. Blinatumomab for acute lymphoblastic leukemia. N. Engl. J. Med. 376, e49 (2017).
Hagop, K. et al. Blinatumomab versus chemotherapy for advanced acute lymphoblastic leukemia. N. Engl. J. Med. 376, 836–847 (2017).
Berman, D. M. & Bell, J. I. Redirecting polyclonal T cells against cancer with soluble T cell receptors. Clin. Cancer Res. OF1–OF8 (2022) https://doi.org/10.1158/1078-0432.ccr-22-0028.
Middleton, M. R. et al. Tebentafusp, a TCR/Anti-CD3 bispecific fusion protein targeting gp100, potently activated antitumor immune responses in patients with metastatic melanoma. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 26, 5869–5878 (2020).
Liddy, N. et al. Monoclonal TCR-redirected tumor cell killing. Nat. Med. 18, 980–987 (2012).
Nathan, P. et al. Overall survival benefit with tebentafusp in metastatic uveal melanoma. N. Engl. J. Med. 385, 1196–1206 (2021).
Hassel, J. C. et al. Three-year overall survival with tebentafusp in metastatic uveal melanoma. N. Engl. J. Med. (2023) https://doi.org/10.1056/nejmoa2304753.
Binnewies, M. et al. Understanding the tumor immune microenvironment (TIME) for effective therapy. Nat. Med. 24, 541–550 (2018).
Güç, E. & Pollard, J. W. Redefining macrophage and neutrophil biology in the metastatic cascade. Immunity 54, 885–902 (2021).
Mellor, A. L., Keskin, D. B., Johnson, T., Chandler, P. & Munn, D. H. Cells expressing indoleamine 2,3-dioxygenase inhibit T cell responses. J. Immunol. 168, 3771–3776 (2002).
Cassetta, L. & Pollard, J. W. Targeting macrophages: therapeutic approaches in cancer. Nat. Rev. Drug Discov. 17, 887–904 (2018).
Mantovani, A., Allavena, P., Marchesi, F. & Garlanda, C. Macrophages as tools and targets in cancer therapy. Nat Rev Drug Discov 1–22 (2022) https://doi.org/10.1038/s41573-022-00520-5.
Peranzoni, E. et al. Macrophages impede CD8 T cells from reaching tumor cells and limit the efficacy of anti–PD-1 treatment. Proc. Natl Acad. Sci. U. S. Am. 115, E4041–E4050 (2018).
Yu, J. et al. Liver metastasis restrains immunotherapy efficacy via macrophage-mediated T cell elimination. Nat. Med. 27, 152–164 (2021).
Fridman, W. H., Zitvogel, L., Sautès–Fridman, C. & Kroemer, G. The immune contexture in cancer prognosis and treatment. Nat. Rev. Clin. Oncol. 14, 717–734 (2017).
Chávez-Galán, L., Olleros, M. L., Vesin, D. & Garcia, I. Much More than M1 and M2 Macrophages, There are also CD169+ and TCR+ Macrophages. Front. Immunol. 6, 263 (2015).
Guilliams, M. & Scott, C. L. Liver macrophages in health and disease. Immunity 55, 1515–1529 (2022).
Lazarov, T., Juarez-Carreño, S., Cox, N. & Geissmann, F. Physiology and diseases of tissue-resident macrophages. Nature 618, 698–707 (2023).
Mantovani, A. et al. The chemokine system in diverse forms of macrophage activation and polarization. Trends Immunol. 25, 677–686 (2004).
Cassetta, L. & Pollard, J. W. A timeline of tumour-associated macrophage biology. Nat. Rev. Cancer 23, 238–257 (2023).
Gordon, S. & Plüddemann, A. Tissue macrophages: heterogeneity and functions. BMC Biol. 15, 53 (2017).
Ma, R.-Y., Black, A. & Qian, B.-Z. Macrophage diversity in cancer revisited in the era of single-cell omics. Trends Immunol. 43, 546–563 (2022).
Bronkhorst, I. H. G. et al. Detection of M2-Macrophages in Uveal Melanoma and Relation with Survival. Investig. Ophthalmol. Vis. Sci. 52, 643–650 (2011).
Johansson, J. et al. Presence of tumor-infiltrating CD8+ T cells and macrophages correlates to longer overall survival in patients undergoing isolated hepatic perfusion for uveal melanoma liver metastasis. OncoImmunology 9, 1854519 (2020).
Mariani, P. et al. Immunohistochemical characterisation of the immune landscape in primary uveal melanoma and liver metastases. Br. J. Cancer 1–10 (2023) https://doi.org/10.1038/s41416-023-02331-w.
Carvajal, R. D. et al. Clinical and molecular response to tebentafusp in previously treated patients with metastatic uveal melanoma: a phase 2 trial. Nat. Med. 1–10 (2022) https://doi.org/10.1038/s41591-022-02015-7.
Szabo, P. A. et al. Single-cell transcriptomics of human T cells reveals tissue and activation signatures in health and disease. Nat. Commun. 10, 4706 (2019).
Barkal, A. A. et al. Engagement of MHC class I by the inhibitory receptor LILRB1 suppresses macrophages and is a target of cancer immunotherapy. Nat. Immunol. 19, 76–84 (2018).
Zeller, T. et al. Dual checkpoint blockade of CD47 and LILRB1 enhances CD20 antibody-dependent phagocytosis of lymphoma cells by macrophages. Front. Immunol. 13, 929339 (2022).
Au-Yeung, B. B. et al. IL-2 modulates the TCR signaling threshold for CD8 but not CD4 T cell proliferation on a single-cell level. J. Immunol. 198, 2445–2456 (2017).
Rosenberg, S. A. IL-2: The first effective immunotherapy for human cancer. J. Immunol. 192, 5451–5458 (2014).
Raeber, M. E., Sahin, D., Karakus, U. & Boyman, O. A systematic review of interleukin-2-based immunotherapies in clinical trials for cancer and autoimmune diseases. eBioMedicine 90, 104539 (2023).
Wang, C. et al. Reprogramming NK cells and macrophages via combined antibody and cytokine therapy primes tumors for elimination by checkpoint blockade. Cell Rep. 37, 110021–110021 (2021).
Nguyen, L. T. et al. Phase II clinical trial of adoptive cell therapy for patients with metastatic melanoma with autologous tumor-infiltrating lymphocytes and low-dose interleukin-2. Cancer Immunol. Immunother. 68, 773–785 (2019).
Han, X., Wilbanks, G. D., Devaja, O., Ruperelia, V. & Raju, K. S. IL-2 enhances standard IFNγ/LPS activation of macrophage cytotoxicity to human ovarian carcinoma in vitro: a potential for adoptive cellular immunotherapy. Gynecol. Oncol. 75, 198–210 (1999).
Bosco, M. C. et al. IL-2 signaling in human monocytes involves the phosphorylation and activation of p59hck 1. J. Immunol. 164, 4575–4585 (2000).
Cassetta, L. et al. Human tumor-associated macrophage and monocyte transcriptional landscapes reveal cancer-specific reprogramming, biomarkers, and therapeutic targets. Cancer Cell 35, 588–602.e10 (2019).
Cheng, S. et al. A pan-cancer single-cell transcriptional atlas of tumor infiltrating myeloid cells. Cell 184, 792–809.e23 (2021).
Martinez, F. O., Gordon, S., Locati, M. & Mantovani, A. Transcriptional profiling of the human monocyte-to-macrophage differentiation and polarization: new molecules and patterns of gene expression. J. Immunol. 177, 7303–7311 (2006).
Ivashkiv, L. B. IFNγ: signalling, epigenetics and roles in immunity, metabolism, disease and cancer immunotherapy. Nat. Rev. Immunol. 18, 545–558 (2018).
Hu, X. & Ivashkiv, L. B. Cross-regulation of signaling pathways by interferon-γ: implications for immune responses and autoimmune diseases. Immunity 31, 539–550 (2009).
Ning, J. et al. Macrophage-coated tumor cluster aggravates hepatoma invasion and immunotherapy resistance via generating local immune deprivation. Cell Rep. Med. 5, 101505 (2024).
Halse, H. et al. Multiplex immunohistochemistry accurately defines the immune context of metastatic melanoma. Sci. Rep. 8, 11158 (2018).
Murray, P. J. et al. Macrophage activation and polarization: nomenclature and experimental guidelines. Immunity 41, 14–20 (2014).
Grzywa, T. M. et al. Myeloid cell-derived arginase in cancer immune response. Front. Immunol. 11, 938 (2020).
Yoshiura, K. et al. Carbonic anhydrase II is a tumor vessel endothelium–associated antigen targeted by dendritic cell therapy. Clin. Cancer Res. 11, 8201–8207 (2005).
Guilliams, M. et al. Dendritic cells, monocytes and macrophages: a unified nomenclature based on ontogeny. Nat. Rev. Immunol. 14, 571–578 (2014).
Cybulsky, M. I., Cheong, C. & Robbins, C. S. Macrophages and dendritic cells. Circ. Res. 118, 637–652 (2016).
Kim, Y. J. et al. Correlation between tumor-associated macrophage and immune checkpoint molecule expression and its prognostic significance in cutaneous melanoma. J. Clin. Med. 9, 2500 (2020).
Logu, F. D. et al. Spatial proximity and relative distribution of tumor-infiltrating lymphocytes and macrophages predict survival in melanoma. Lab. Investig. 103, 100259 (2023).
Vasilevska, J. et al. Monitoring melanoma patients on treatment reveals a distinct macrophage population driving targeted therapy resistance. Cell Rep. Med. 5, 101611 (2024).
Chin, S. S. et al. T cell receptor and IL-2 signaling strength control memory CD8+ T cell functional fitness via chromatin remodeling. Nat. Commun. 13, 2240 (2022).
Rosenberg, S. A. et al. Prospective randomized trial of high-dose interleukin-2 alone or in conjunction with lymphokine-activated killer cells for the treatment of patients with advanced cancer. JNCI J. Natl Cancer Inst. 85, 622–632 (1993).
Hernandez, R., Põder, J., LaPorte, K. M. & Malek, T. R. Engineering IL-2 for immunotherapy of autoimmunity and cancer. Nat. Rev. Immunol. 1–15 (2022) https://doi.org/10.1038/s41577-022-00680-w.
Durante, M. A. et al. Single-cell analysis reveals new evolutionary complexity in uveal melanoma. Nat. Commun. 11, 496 (2020).
Qin, Y. et al. Immune profiling of uveal melanoma identifies a potential signature associated with response to immunotherapy. J. Immunother. Cancer 8, e000960 (2020).
Anfray, C., Ummarino, A., Andón, F. T. & Allavena, P. Current strategies to target tumor-associated-macrophages to improve anti-tumor immune responses. Cells 9, 46 (2019).
Martin, M. Cutadapt removes adapter sequences from high-throughput sequencing reads. EMBnetJ 17, 10–12 (2011).
Ewels, P., Magnusson, M., Lundin, S. & Käller, M. MultiQC: summarize analysis results for multiple tools and samples in a single report. Bioinformatics 32, 3047–3048 (2016).
Dobin, A. et al. STAR: ultrafast universal RNA-seq aligner. Bioinformatics 29, 15–21 (2012).
Li, B. & Dewey, C. N. RSEM: accurate transcript quantification from RNA-Seq data with or without a reference genome. BMC Bioinform. 12, 323 (2011).
Ritchie, M. E. et al. limma powers differential expression analyses for RNA-sequencing and microarray studies. Nucleic Acids Res. 43, e47–e47 (2015).
Love, M. I., Huber, W. & Anders, S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 15, 550 (2014).
Durinck, S., Spellman, P. T., Birney, E. & Huber, W. Mapping identifiers for the integration of genomic datasets with the R/Bioconductor package biomaRt. Nat. Protoc. 4, 1184–1191 (2009).
Yu, G. & He, Q.-Y. ReactomePA: an R/Bioconductor package for reactome pathway analysis and visualization. Mol. Biosyst. 12, 477–479 (2015).
Acknowledgements
The authors thank the patients, their family members, and the study teams for participating in the study, as well as the following Immunocore employees: D. Berman, M. Dar for critical review of the manuscript, A. Greenshields-Watson for bioinformatic analysis support, J. Houghton and C. Britton-Rivet for support with the preparation of samples for sequencing, C. Perot for designing the graphical summary and illustrations, and F. Amicarella, D. Gascoyne, and D. Depoil for their scientific input. Editorial assistance was provided by Dr Georgia Greaves of Cancer Communications and Consultancy Ltd (part of Bioscript Group). This study was funded by Immunocore Ltd.
Author information
Authors and Affiliations
Contributions
E.G., K.R., and A. Benlahrech. contributed to the conception, design, and planning of the study and drafted the manuscript. E.G., A.T., E.L., A. Broomfield, A.C., J.C., P.N.G., A.K., R.K., L.D.C., H.H., J.C.H., J.J.S., S.S., L.C., J.M.P., K.R., and A. Benlahrech contributed to the conduct of the study, the analysis, interpretation of the data, critically reviewed the manuscript, and approved the final draft for submission.
Corresponding author
Ethics declarations
Competing interests
E.G., A.T., E.L., A. Broomfield, A.C., J.C., A.K., R.K., S.S., L.C., K.R., A. Benlahrech, are/were employees of Immunocore Ltd. H.H. is co-founder and shareholder of Omniscope, scientific advisory board member of Nanostring and MiRXES, a consultant for Moderna, and has received honoraria from Genentech. J.C.H. discloses Advisory Boards (self): GSK, MSD, Pierre Fabre, Sunpharma; Advisory Boards (institution): BMS, Immunocore, Novartis, Nektar, Philogen; Contracted Research: 4SC, BioNTech, BMS, Genentech/Roche, Idera, Immunocore, Iovance, Nektar, Novartis, Philogen, Pierre Fabre, Regeneron, Sanofi; Honoraria: BMS, MSD, Novartis, Pierre Fabre, Roche, Sanofi, Sunpharma; Research Funding to Institution: BMS, Sunpharma. J.J.S. discloses PI on clinical trial: Amgen, AstraZeneca, Bristol-Myers Squibb, Delcath Systems, Merck, Replimune, Transgene; Research Grant/Contract: AstraZeneca, Bristol-Myers Squibb, Immunocore; Consultant/Advisory Board: Bristol-Myers Squibb, Delcath Systems, Immunocore, Merck; Congress attendance: Bristol-Myers Squibb, Merck. J. M. P. Discloses Advisory Boards (self): Astellas, Astra Zeneca, BeiGene, BMS, Immunocore, Janssen, MSD, Novartis, Roche, VCN; Research grants (personal and institutional): BeiGene, BMS, Immunocore, Janssen, Mirati, Pfizer, Regeneron. P.N.G. and L.D.C. report no conflicts of interest.
Peer review
Peer review information
Nature Communications thanks the anonymous reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Güç, E., Treveil, A., Leach, E. et al. Tebentafusp, a T cell engager, promotes macrophage reprogramming and in combination with IL-2 overcomes macrophage immunosuppression in cancer. Nat Commun 16, 2374 (2025). https://doi.org/10.1038/s41467-025-57470-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41467-025-57470-w