Abstract
H5N1, a highly pathogenic avian influenza virus, presents pandemic risks due to its ability to adapt and spread among mammalian species. Vaccination may control its spread, but the effectiveness of existing H5N1 vaccines against circulating strains, especially clade 2.3.4.4b, remains uncertain. In this study, we assess neutralizing antibody responses to global circulating H5N1 strains, using sera from individuals vaccinated with an inactivated H5N1 vaccine (NCT00535665). Neutralization is measured against 17 pseudoviruses, representing circulating and vaccine H5 strains. Our results indicate that broad protective effects are observed only when high antibody titers are achieved by vaccination. Correlation analysis estimates that a pseudovirus-based neutralization titer of at least 1:980 is required to achieve a cross-protection rate above 60%. The findings suggest that the current H5N1 vaccine can elicit cross-neutralization of circulating H5N1 strains, if high antibody titers are achieved. Until updated H5N1 vaccines are developed, this vaccine may serve as a bridging measure.
Similar content being viewed by others
Introduction
Since 2020, the H5 subtype highly pathogenic avian influenza (HPAI) virus has spread globally, inflicting significant economic losses on the poultry industry1,2. This virus not only triggers outbreaks in poultry and wild birds but also breaches species barriers, infecting carnivorous mammals, aquatic mammals, domestic cats, dogs, and even dairy cows, thereby leading to interspecies transmission and severe diseases in these animals3,4. Such cross-species transmission not only imperils biodiversity but also raises concerns regarding the virus’s potential to adapt to human hosts and precipitate a global pandemic. On March 25, 2024, the United States Department of Agriculture (USDA) initially detected the H5N1 subtype virus from clade 2.3.3.4b in milk and nasal wash samples from an infected dairy cow in Kansas1. This marked the first outbreak of the virus in cattle, and by May 30, 2024, infections had been confirmed in 69 cattle herds across nine states. Additionally, three farm workers presenting with conjunctivitis or respiratory symptoms were also confirmed to have been infected with the H5N1 virus. At a poultry farm in Colorado, six workers tested positive, representing the largest human outbreak of HPAI in the U.S. to date5. According to the Centers for Disease Control and Prevention (as of November 3, 2024), there have been 41 confirmed human cases of avian influenza in the U.S. in 2024, including 21 from cattle, 19 from poultry, and 1 from an unknown source. However, due to the lack of routine testing, this figure likely underestimates the actual number of cases. Even more concerning, the USDA’s National Veterinary Services Laboratory recently reported the first case of H5N1 infection in swine on a farm in Oregon. Swine are regarded as mixing vessels for influenza viruses due to their susceptibility to both avian and human strains, which enables genetic reassortment that can give rise to potentially more transmissible viruses. A similar situation occurred during the 2009 H1N1 pandemic when swine served as intermediaries for both avian and human flu viruses6. The recent detection in Oregon underscores the need for enhanced vigilance, as it may suggest that the H5N1 virus is adapting to human hosts and could potentially spread within human populations. In China, no human H5N1 infections were reported between 2015 and 2021. However, in October 2022, a human case was reported in Jiangsu province, and hemagglutinin (HA) gene sequence analysis indicated that the virus belonged to clade 2.3.3.4b7. This clade has emerged as the dominant strain responsible for avian influenza outbreaks in poultry and wild birds worldwide8,9,10. It has also been detected in wild birds and poultry in southern China since 2021. Additionally, studies have shown that the H5N6 clade 2.3.3.4b virus has been the predominant H5 virus circulating in Chinese poultry since 2014 and has been associated with multiple human infections11. In brief, the ongoing spread of the H5 subtype avian influenza among mammals poses unprecedented challenges to both public health and global biodiversity.
Vaccination is a crucial strategy for preventing and controlling influenza outbreaks12. China’s first pandemic H5N1 vaccine, Panflu, was developed by Sinovac Biotech Ltd. in 200413. This vaccine was produced using the WHO-recommended A/Vietnam/1194/2004 vaccine strain, cultivated in chicken embryos, inactivated, and adjuvanted with aluminum hydroxide. Previous studies have demonstrated that the H5N1 vaccine not only exhibits robust immunogenicity and safety but also induces notable cross-reactivity against heterologous H5N1 strains13. It is intended for preventive vaccination during influenza pandemics or emergencies. Given the current H5 influenza outbreak, it remains uncertain whether this vaccine still provides cross-protection against the circulating strains. Additionally, in the United States, studies have also evaluated whether three approved H5N1 vaccines (derived from clades 1 and 2.1 strains) can generate cross-reactive binding and neutralizing antibodies against the H5N1 2.3.4.4b subtype virus14. Their results indicated that the adjuvanted H5N1 vaccines (clades 1 and 2.1) stored by the U.S. could induce cross-neutralizing antibodies against the circulating H5N1 2.3.4.4b virus. However, the study sample size was small, and the candidate virus used was heterogenous A/Astrakhan/3212/2020(H5N8), rather than the circulating H5N1 A/Texas/37/2024 strain, which differs from the U.S. circulating strain at four amino acid positions.
In the present study, a pseudovirus platform and clinical human immune sera from H5N1 vaccine recipients were utilized to assess the neutralizing antibody responses to globally circulating H5N1 strains. The results indicate that sera from participants who received two doses of the H5N1 vaccine with aluminum hydroxide adjuvant manifested broad-spectrum protective effects against circulating H5N1 strains only when high antibody titers were attained. By analyzing the correlation between pseudovirus-based neutralizing assay (PBNA) titers and overall neutralizing antibody seroconversion rates (SCR) against H5 strains, it was estimated that a PBNA titer of at least 1:980 is required to achieve a cross-protection rate above 60%. Until updated H5N1 vaccines are developed, measures such as using a more efficacious adjuvant, increasing the number of doses, or adjusting the dosage could enhance antibody titers, enabling this vaccine to function as a bridging measure to prevent further outbreaks of HPAI.
Results
The selection and analysis of representative circulating H5 strains
To select representative H5N1 strains, we downloaded all human-infected H5N1 sequences (46 sequences) from the Global Initiative on Sharing All Influenza Data (GISAID) EpiFlu database as of August 2024. After excluding sequences containing non-amino-acid residues or incomplete regions, 33 sequences were retained. We calculated the frequency of occurrence for each sequence and constructed a phylogenetic tree to classify strains into distinct clades (Fig. 1, Supplementary Table 1). Representative strains were selected from each clade based on their high circulation frequency and geographic distribution. As a result, we selected eight dominant representative H5N1 strains (Supplementary Table 1). Using the same approach, we selected four representative H5N6 strains from China, one belonging to the 2.3.4.4b clade and three belonging to the 2.3.4.4h clade (Fig. 1). Amino acid sequence alignment between the selected H5 representative strains and the vaccine strain A/Vietnam/1194/2004 revealed varying degrees of HA protein mutations (Supplementary Fig. 1). More importantly, a significant proportion of these mutations are concentrated in the globular HA1 head domain, particularly within antigenic sites A–D (Supplementary Fig. 1, 2a). This highlights potential concerns regarding the effectiveness of the pandemic influenza vaccine.
Phylogenetic inference was conducted using a maximum likelihood approach based on amino acid sequences of the hemagglutinin (HA) protein. These strains were categorized into various clades, with approved vaccine strains or candidate vaccine viruses marked with red triangles, and selected epidemic representative strains highlighted in bold. A/Darwin/9/2021(H3N2) served as the out-group. Source data are provided as a source data file.
Neutralization potency of the H5N1 vaccine against circulating H5 strains
Pseudotyped viruses, owing to their safety and flexibility, are valuable tools for virological assays15. By employing a vesicular stomatitis virus (VSV)-based pseudovirus production system, we developed a neutralization assay to evaluate the efficacy of immune responses against influenza viruses. After selecting the representative strains, we synthesized the HA amino acid sequences of these strains and cloned them into pcDNA3.1-HA expression plasmids. Using the VSV-based pseudovirus packaging system, we successfully generated pseudoviruses expressing the HA proteins of the selected representative H5N1 and H5N6 strains. In addition to the representative circulating strains, we included three H5N1 vaccine strains (A/Vietnam/1194/2004 [clade 1], A/Vietnam/1203/2004 [clade 1], and A/Indonesia/5/2005 [clade 2.1]) and two candidate vaccine viruses (CVV) (A/Astrakhan/3212/2020/H5N8 [clade 2.3.4.4b] and A/chicken/Ghana/AVL-763_21VIR7050-39/2021/H5N1 [clade 2.3.4.4b]) in the pseudovirus panel. These controls were essential for benchmarking cross-neutralization against both historical and emerging clades.
To assess whether China’s H5N1 vaccines, derived from the clade 1 strain, generate cross-neutralizing antibodies against currently circulating H5 strains, we analyzed serum samples collected before and after vaccination from 129 adults who participated in clinical vaccine trials. As shown in Supplementary Fig. 2b, all 129 participants received two doses of the A/Vietnam/1194/2004 vaccine, adjuvanted with aluminum hydroxide, and among them, 103 participants received doses ranging from 5 to 15 μg with a 28-day interval, while 26 participants received 10 μg doses with a 14-day interval. To confirm minimal background neutralization against pseudoviruses, we examined 50 serum samples from unvaccinated individuals. No significant cross-neutralization activity was observed in these controls, confirming the specificity of the vaccine-induced immune responses (Supplementary Fig. 3).
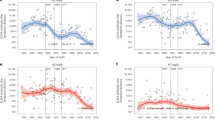
Initially, we grouped the neutralization results based on the clinical vaccination regimens, comparing neutralizing antibody data according to the vaccine dosages. Although there was variability in the data, a general trend emerged showing that higher vaccine dosages correlated with higher neutralizing antibody titers. To further refine the analysis, we categorized the sera based on their neutralizing antibody titers against the vaccine strain A/Vietnam/1194/2004, dividing them into three groups: high responders (titer ≥1:1800), medium responders (1:800 ≤ titer < 1:1800), and low responders (titer <1:800). This classification allowed us to assess whether increasing neutralizing antibody levels against the vaccine strain also led to enhanced cross-neutralizing against circulating strains. For the vaccine strain A/Vietnam/1194/2004 (clade 1), the geometric mean increase (GMI) in neutralizing antibodies ranged from 4.8 (low responders) to 26.3 (high responders), with the SCR—defined as the proportion of individuals with postimmunization neutralizing antibody geometric mean titers greater than the upper limit of the 95% confidence interval of pre-immunization titers—rising from 79.6 to 100%. A similar trend was observed for another vaccine strain in the same clade, A/Vietnam/1203/2004. However, for the clade 2.1 vaccine strain A/Indonesia/5/2005, the GMI increased from 6.1 to 11.4 (less than a twofold increase), and the SCR increased marginally from 51.9 to 66%. This suggests notable differences between the clade 1 and clade 2.1 vaccine strains (Fig. 2a–c). For circulating strains from the currently predominant clade 2.3.4.4b, such as A/Colorado/134/2024, A/England/231990002/2023, and A/Antofagasta/25945/2023, the GMI increased from around 7 (low) to around 12 (high), with the SCR rising from about 60 to 95% (Fig. 2a–c). The circulating strain A/Texas/37/2024 in the U.S. shares the same HA sequence as A/Colorado/134/2024, differing by only four amino acids from the heterologous A/Astrakhan/3212/2020 (H5N8) strain, which was isolated from nasopharyngeal swabs of poultry workers during an outbreak in southern Russia in December 202016. Therefore, the A/Astrakhan/3212/2020 strain is being evaluated as a CVV for the currently circulating highly pathogenic H5N1 clade 2.3.4.4b strain. In our neutralization assay, this heterologous strain showed a GMI increase from 4.8 to 5.9, with a SCR increase from 51.9 to 68.5%. In contrast, for the circulating A/Jiangsu/NJ210/2023 strain in China, the GMI remained unchanged, but the SCR increased from 49 to 65.4%. The circulating heterologous A/HeFei04171/2024 (H5N6), despite belonging to the 2.3.4.4b clade, had a GMI of 4.1 in the high group, with a SCR of 58.3%. For other circulating strains from different clade branches, such as the 2.3.2.1c clade strains, the GMI increased from around 5 (low responders) 0to around 7 (high responders), with SCR rising from 70 to 80%. For the 2.3.2.1a clade strain A/Victoria/149/2024, the GMI increased from 5.8 (low) to 8.0 (high), and the SCR improved marginally from 61.1(low) to 64.8% (high). Additionally, for the H5N6 strain circulating in China from the 2.3.4.4 h clade, the GMI rose from approximately 6 (low) to 9 (high), and the SCR increased from about 60 to 90% (Fig. 2a–c). These results clearly indicate that as the neutralizing antibody titers against the vaccine strain increase, there is a corresponding improvement in cross-neutralizing against other H5 subtypes, highlighting the effectiveness of higher antibody titers in providing broader protection.
Shown are the ID50 values representing neutralizing antibody levels in human sera before and after vaccination against HA of various H5 strains, as measured by PBNA. Based on post-vaccination neutralizing antibody levels against the vaccine strain, subjects were classified into high, medium, and low response groups, as represented in (a, b, c). Orange dots represent pre-vaccination, while light blue dots represent post-vaccination. The thick black line indicates the pre-vaccination geometric mean titer adding a 95% confidence interval. Geometric mean increase (GMI) and seroconversion rates (SCR) between pre- and post-vaccination are shown above each group. The strains were classified into clades in (c). d, e Pearson correlation analysis (two-tailed) was used to evaluate the association between PBNA and HI or MN. f shows the relationship between PBNA and overall neutralizing antibody SCR, with simple linear regression equation. Statistical significance was assessed using multiple unpaired two-sided t tests, assuming individual variances for each row. The False Discovery Rate was controlled at 1% using the two-stage step-up method of Benjamini, Krieger, and Yekutieli. Source data are provided as a source data file.
In the clinical assessment of influenza vaccines, in vitro assays such as hemagglutination inhibition (HI) and microneutralization (MN) assays are commonly used to measure antibody titers in vaccinated individuals. The HI or MN-based SCR is a well-established surrogate marker of clinical efficacy in influenza vaccine trials. This metric is strongly correlated with protection against infection in clinical studies. Our laboratory has previously developed various influenza pseudoviruses and explored the relationship between PBNA and the traditional HI and MN assay17,18. The results indicated a strong correlation between PBNA and both HI and MN assays. In this study, all serum samples were further tested for neutralizing antibody levels using both HI and MN assays against the H5N1 vaccine strain A/Vietnam/1194/2004. The findings demonstrate a good agreement between PBNA titers and the HI, MN assay results, with correlation coefficients of 0.72 and 0.81, respectively (Fig. 2d, e). The correlations validate PBNA as a reliable surrogate for predicting functional antibody responses, akin to HI or MN-based SCR. Then, what antibody level is required for effective protection in clinical practice? In seasonal influenza viruses, serum HI antibody titers of 40 are associated with 50% protection against clinical disease19. However, the correlates of protection against HAPI H5N1 virus have not yet been established. Our analysis further revealed that a PBNA titer threshold of at least 1:980 corresponds to a cross-protection rate exceeding 60% against diverse H5 strains (Fig. 2f). This aligns with clinical benchmarks where HI-based SCR is used to infer vaccine efficacy. By bridging PBNA titers to cross-neutralization outcomes, we establish that PBNA not only mirrors HI-based SCR but also provides a practical tool for evaluating cross-protection against antigenically divergent strains (e.g., clade 2.3.4.4b), which are not fully addressed by traditional assays. This approach is particularly valuable for assessing vaccines against emerging H5N1 variants, where rapid evaluation of cross-reactive immunity is critical for pandemic preparedness.
PBNA offers advantages in safety and scalability for high-throughput screening, but pseudoviruses lack the biological complexity of live viruses, such as replication dynamics and host immunity interactions, which may affect clinical outcomes. Previous international multi-laboratory studies have established that vaccine strains exhibit comparable antigenic behavior to wild-type viruses in HI and MN assays20,21. To strengthen the validity and robustness of our study, we therefore extended our analysis to evaluate neutralizing antibody responses against the vaccine strain A/Vietnam/1194/2004 (clade 1) and the only currently circulating human-infecting strain A/Jiangsu/NJ210/2023 (clade 2.3.4.4b) in China using HI and MN assays. Pre-vaccination sera displayed no detectable neutralizing activity against either live strain (HI titer <1:5, MN titer <1:5). Serum samples were similarly categorized into three groups based on their neutralizing antibody titers against the vaccine strain: high responders (HI titer ≥1:320, MN titer ≥1:640), medium responders (1:80 ≤ HI titer <1:320, 1:160 ≤ MN titer <1:640), and low responders (HI titer <1:80, MN titer <1:160). For the vaccine strain, HI titers exhibited a marked increase in geometric mean titer (GMT) from 25.9 (low) to 426.8 (high), accompanied by a SCR rising from 29.8 to 100%. Similarly, against the circulating A/Jiangsu/NJ210/2023 (clade 2.3.4.4b) strain, HI titers demonstrated a progressive elevation (GMT: 11.1–76.7), with SCR improving from 0 to 64.6% (Supplementary Fig. 4a). In parallel MN assays, GMT for the vaccine strain increased from 60.3 (low) to 775.4 (high), while SCR surged from 51 to 100%. For the circulating strain, MN titers rose from a GMT of 26.5 (low) to 176.1 (high), with SCR advancing from 0 to 76.9% (Supplementary Fig. 4b). These live virus-based results demonstrate that increased neutralizing antibody titers against the vaccine strain are associated with improved cross-neutralization efficacy against the heterologous clade 2.3.4.4b strain, further underscoring the importance of high antibody titers for effective cross-neutralization. These findings are consistent with the PBNA results.
Discussion
In future studies, the correlation between PBNA titers and cross-protection rates should be further validated using in vivo animal models or ex vivo assays with primary human respiratory cells. Moreover, our study only focused on humoral immunity and did not assess other immune mechanisms like T-cell responses or mucosal immunity, which may play a role in scenarios with suboptimal antibody titers. Furthermore, host-specific factors, such as pre-existing immunity and genetic differences, were not explored here. These limitations underscore that neutralizing antibodies, while important, are not the sole factor in cross-protection, and a broader understanding of immune interactions will be critical for improving H5N1 vaccines.
In conclusion, the global H5N1 influenza pandemic in mammals presents multiple challenges. This study, which utilized a pseudovirus platform to evaluate the match between H5N1 vaccine strains and circulating strains, indicates that the inactivated H5N1 vaccine produced by Sinovac in 2005 may provide partial cross-protection against H5 strains, provided that antibody titers are sufficiently elevated. However, the degree of cross-protection varies substantially depending on the antigenic similarity of the circulating strain to the vaccine strain. For example, while high antibody titers achieved over 90% SCR against clade 2.3.4.4b strains (e.g., A/Colorado/134/2024), the SCR remained suboptimal for more divergent clades, such as 2.1 (66%), and certain H5N6 strains (e.g., A/HeFei04171/2024: 58.3%). These differences underscore the importance of considering antigenic drift and strain-specific variability when evaluating vaccine efficacy. Furthermore, we propose a clinical evaluation standard: when the PBNA neutralizing antibody titer reaches 1:980, ~60% cross-protection can be achieved. One potential strategy to enhance antibody titers is the use of more effective adjuvants, such as MF59 or AS03, or by increasing the vaccine dose and the number of immunizations. However, the effectiveness of these approaches still requires experimental validation. Until updated vaccines are developed, this vaccine can serve as a bridging solution to address H5N1.
Methods
Clinical trial serum samples and ethics
Serum samples were obtained from two immunization regimens. In the first regimen, 103 participants received two intramuscular doses of inactivated H5N1 A/Vietnam/1194/04 (clade 1) vaccine with aluminum hydroxide adjuvant, containing 5–15 μg of HA, administered at an interval of 28 days. Serum samples were collected at baseline (day 0), immediately prior to the second dose (day 28), and subsequently on days 42 and 56, representing 14 and 28 days after the second dose, respectively. In the second regimen, 26 participants were administered two doses of 10 μg HA on days 0 and 14. Blood samples were taken on day 0, before the second dose on day 14, and on days 28 and 42, corresponding to 14 and 28 days after the second dose, respectively. The serum samples were blinded for antibody testing, and unblinding was carried out after data lock for subsequent analysis.
This study complies with the ethical principles outlined in the Declaration of Helsinki and has been reviewed and approved by the Medical Ethics Committee of the Beijing Center for Disease Prevention and Control (Ethics Approval Number: 2007 No. (1) Total (1)). The committee’s composition and operational procedures adhere to the Good Clinical Practice guidelines and relevant legal regulations. Written informed consent was obtained from all participants, and the study was conducted strictly in accordance with the approved protocol to ensure the privacy and rights of participants were fully protected. The trial was approved by the Chinese State Food and Drug Administration and was registered with ClinicalTrials.gov (identifier NCT00535665). The primary outcomes of the trial were previously published13.
Generation and production of H5-fluc pseudovirus
The pseudovirus generation procedure was performed as previously described22. Briefly, HA expression plasmids for the H5 influenza virus were constructed by inserting HA genes into the pcDNA3.1 vector. The HA genes utilized in this study were obtained from the GISAID. These encompassed twelve representative circulating H5 strains and three H5N1 vaccine strains, as well as two CVV (Fig. 1). To generate the pseudoviruses, HEK293T cells were transfected with the HA plasmids, facilitating the expression of the HA proteins on the cell membrane. Subsequently, G*ΔG-VSV was employed to provide the viral genome. The first pseudovirus collection was harvested 24 h post-infection and transfection, and stored at 2–8 °C for up to 24 h. After an additional 24 h incubation with complete culture medium, a second pseudovirus collection was obtained. The collected pseudovirus was treated with TPCK-trypsin (Sigma-Aldrich) at a final concentration of 40 μg/ml for enzymatic activation and incubated at 37 °C in a 5% CO2 atmosphere for 30 min. The sample was then centrifuged at 4000 g for 10 min, filtered through a 0.45 μm filter, aliquoted, and stored at −80 °C for future use.
Titration of the pseudotyped virus
The titer of the pseudovirus was determined by infecting Huh7 cells with serial three-fold dilutions of the pseudovirus. Trypsin-treated Huh7 cells were seeded into 96-well culture plates (100 μl per well). After a 24 h incubation at 37 °C with 5% CO2, chemiluminescence was measured using the Britelite Plus reporter gene assay system (PerkinElmer). The 50% tissue culture infectious dose (TCID50) was calculated according to the Reed-Muench method, as described in previous studies23,24.
Pseudovirus-based neutralizing assay
Neutralization was evaluated by quantifying the reduction in luciferase expression. Serum samples were initially diluted 1:120, followed by three-fold serial dilutions. These were incubated with 1.3 × 10^4 TCID50 of influenza H5 pseudoviruses in duplicate wells of a 96-well flat-bottom plate for 1 h at 37 °C. Control wells for virus and cells were included, each with six replicates. After incubation, freshly trypsinized Huh7 cells were added to the wells and cultured for 24 h. Infectivity was assessed by measuring bioluminescence, as previously described25. The 50% infectious dose (ID50) was determined using the Reed-Muench method, and the results were expressed as the mean of three replicates.
HI assay
The HI assay was performed using a 1% chicken red blood cell (RBC) suspension and the HA antigen of the H5N1 vaccine strain A/Vietnam/1194/2004 (NIBRG-14), provided by the National Institute for Biological Standards and Control (NIBSC), and the currently circulating A/Jiangsu/NJ210/2023 strain, provided by the Chinese Center for Disease Control and Prevention (China CDC), in a BSL-2 laboratory facility. Serum samples to be tested were initially treated with receptor-destroying enzyme (RDE) at a 1:5 dilution, incubated overnight at 37 °C, and then inactivated at 56 °C to eliminate the activity of the RDE. Subsequently, chicken RBCs were added to adsorb non-specific agglutination factors in the serum samples. The highest dilution at which complete inhibition of agglutination occurred was defined as the HI antibody titer of the serum sample. Testing was initially performed at a dilution of 1:5, and serum samples with an HI titer less than 1:5 were assigned a titer of 1:2.5. Each serum sample was tested in at least two independent HI assays, with variations between duplicate runs remaining within a twofold difference. The SCR for each group was calculated by dividing the number of seropositive samples (defined as HI titers ≥1:40) by the total number of samples in the group, and then multiplying by 100.
MN assay
The MN assay was conducted using Madin-Darby Canine Kidney (MDCK) cells, with the H5N1 vaccine strain A/Vietnam/1194/2004, and the currently circulating strain A/Jiangsu/NJ210/2023 in a BSL-2 laboratory facility. Serum samples were heat-inactivated at 56 °C, followed by serial dilution. The diluted sera were incubated with the H5N1 virus for neutralization. The neutralized serum-virus mixture was then added to a monolayer of MDCK cells for culture. The MN antibody titer was defined as the highest serum dilution that completely inhibited viral replication. Serum samples were initially diluted at 1:5, with two parallel wells tested for each sample. The GMT of neutralizing antibodies was calculated for each time point in each group.
Statistical information
Statistical analysis was performed using Prism 8 software (GraphPad, San Diego, CA). Results are presented in the form of geometric mean titers. Statistical analyses were performed using multiple unpaired t-tests with individual variances assumed for each row. To correct for multiple comparisons, the False Discovery Rate was controlled at 1.00% using the two-stage step-up procedure of Benjamini, Krieger, and Yekutieli. All tests were two-sided. Pearson correlation analysis was performed (two-tailed).
In this study, we utilized the large language model ChatGPT to assist in refining the manuscript’s language and improving its readability.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
All data generated or analyzed during this study are included in the manuscript figures, Supplementary Information, or Source Data file. The structural information for the HA protein of H5N1-A/Vietnam/1194/2004 (PDB ID: 2IBX) was retrieved from the Research Collaboratory for Structural Bioinformatics Protein Data Bank (https://www.rcsb.org/structure/2IBX). Source data are provided with this paper.
References
Neumann, G. & Kawaoka, Y. Highly pathogenic H5N1 avian influenza virus outbreak in cattle: the knowns and unknowns. Nat. Rev. Microbiol. 22, 525–526 (2024).
Sevilla, N. et al. Highly pathogenic avian influenza A (H5N1) virus outbreak in Peru in 2022–2023. Infect. Med. 3, 100108 (2024).
Burrough, E. et al. Highly pathogenic Avian Influenza A(H5N1) Clade 2.3.4.4b virus infection in domestic dairy cattle and cats, United States, 2024. Emerg. Infect. Dis. J. 30, 1335 (2024).
Plaza, P., Gamarra-Toledo, V., Euguí, J. R. & Lambertucci, S. Recent changes in patterns of mammal infection with highly pathogenic Avian Influenza A(H5N1) virus worldwide. Emerg. Infect. Dis. J. 30, 444 (2024).
Eisfeld, A. J. et al. Pathogenicity and transmissibility of bovine H5N1 influenza virus. Nature 633, 426–432 (2024).
Wille, M. & Holmes, E. C. The ecology and evolution of Influenza viruses. Cold Spring Harb. Perspect. Med 10, a038489 (2020).
Deng, F. et al. Molecular characteristics of the first human case infected with the avian influenza virus H5N1 clade 2.3.3.4b in eastern China. Jiangsu J. Prev. Med. 35, 408–411 (2024).
Ke, X. et al. Highly pathogenic Avian Influenza A (H5N1) virus in Swans, Central China, 2021. Microbiol. Spectr. 10, e02315–e02322 (2022).
Lewis, N. S. et al. Emergence and spread of novel H5N8, H5N5 and H5N1 clade 2.3.4.4 highly pathogenic avian influenza in 2020. Emerg. Microbes Infect. 10, 148–151 (2021).
Cui, P. et al. Global dissemination of H5N1 influenza viruses bearing the clade 2.3.4.4b HA gene and biological analysis of the ones detected in China. Emerg. Microbes Infect. 11, 1693–1704 (2022).
Zhu, W. et al. Epidemiologic, clinical, and genetic characteristics of human infections with Influenza A(H5N6) viruses, China. Emerg. Infect. Dis. J. 28, 1332 (2022).
Oladunni, F. S., Oseni, S. O., Martinez-Sobrido, L. & Chambers, T. M. Equine Influenza virus and vaccines. Viruses 13, 1657 (2021).
Wu, J. et al. Immunogenicity, safety, and cross-reactivity of an inactivated, adjuvanted, prototype pandemic influenza (H5N1) vaccine: a phase II, double-blind, randomized trial. Clin. Infect. Dis. 48, 1087–1095 (2009).
Khurana, S. et al. Licensed H5N1 vaccines generate cross-neutralizing antibodies against highly pathogenic H5N1 clade 2.3.4.4b influenza virus. Nat. Med. 30, 2771–2776 (2024).
Wang, Y. Pseudotyped Viruses (Springer Press, 2023).
Pyankova, O. G. et al. Isolation of clade 2.3.4.4b A(H5N8), a highly pathogenic avian influenza virus, from a worker during an outbreak on a poultry farm, Russia, December 2020. Eurosurveillance 26, 2100439 (2021).
Tian, Y. et al. Development of in vitro and in vivo neutralization assays based on the pseudotyped H7N9 virus. Sci. Rep. 8, 8484 (2018).
Huang, X. et al. Neutralization potency of the 2023-24 seasonal influenza vaccine against circulating influenza H3N2 strains. Hum. Vaccines Immunother. 20, 2380111 (2024).
Potter, C. W. & Oxford, J. S. Determinants of immunity to influenza infection in man. Br. Med. Bull. 35, 69–75 (1979).
Laurie, K. L. et al. International laboratory comparison of influenza microneutralization assays for A (H1N1) pdm09, A (H3N2), and A (H5N1) influenza viruses by CONSISE. Clin. Vaccin. Immunol. 22, 957–964 (2015).
Waldock, J. et al. Haemagglutination inhibition and virus microneutralisation serology assays: Use of harmonised protocols and biological standards in seasonal influenza serology testing and their impact on inter-laboratory variation and assay correlation: a FLUCOP collaborative study. Front. Immunol. 14, 1155552 (2023).
Nie, J. et al. Quantification of SARS-CoV-2 neutralizing antibody by a pseudotyped virus-based assay. Nat. Protoc. 15, 3699–3715 (2020).
Nie, J. et al. Development of in vitro and in vivo rabies virus neutralization assays based on a high-titer pseudovirus system. Sci. Rep. 7, 42769 (2017).
Li, M. et al. Human immunodeficiency virus type 1 env clones from acute and early subtype B infections for standardized assessments of vaccine-elicited neutralizing antibodies. J. Virol. 79, 10108–10125 (2005).
Li, Q. et al. The impact of mutations in SARS-CoV-2 spike on viral infectivity and antigenicity. Cell 182, 1284–1294 (2020).
Acknowledgments
We would like to express our gratitude to GISAID for providing access to the viral sequence data. We also highly appreciate BioRender (https://biorender.com) for offering the tools necessary to create the figures presented in this study. This research was generously supported by the National Key Research and Development Program of China: Development and safety and efficacy evaluation of oral formulation vaccines for respiratory diseases (No. 2022YFC2304302 to C.Y.Z.), the State Key Laboratory of Drug Regulatory Science: Establishment of mouse infection model by influenza and SARS-CoV-2 pseudovirus (No. 2023SKDLS0112 to W.J.H.) and Beijing Natural Science Foundation: Research on Chinese influenza standard (No. L242148 to C.Y.Z.).
Author information
Authors and Affiliations
Contributions
Research design: W.H., C.Z., and X.H. Research performance: X.H., D.Y., X.W., L.P., D.W., L.L., and J.L. Provision of Human clinical samples: D.Y. and J.L. Contribution to writing: X.H. and D.Y.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks the anonymous reviewers for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Huang, X., Yu, D., Pan, L. et al. Increase in H5N1 vaccine antibodies confers cross-neutralization of highly pathogenic avian influenza H5N1. Nat Commun 16, 5517 (2025). https://doi.org/10.1038/s41467-025-60714-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-025-60714-4