Abstract
Fibrous dysplasia is a skeletal disorder caused by activating mutations in Gαs, leading to bone fractures, deformities, and pain. Protein kinase A (PKA), the principal effector of Gαs, plays critical roles in various biological processes. However, its role in fibrous dysplasia is unknown. Here we demonstrate that PKA activation replicates fibrous dysplasia-like lesions in a transgenic mouse model expressing an activating mutation of PKA in the skeletal stem cell lineage. Mechanistically, PKA promotes osteoclastogenesis and aberrant osteogenic differentiation and proliferation of skeletal stem cells, while impairing mineralization. Downregulating PKA activity, using either a genetically engineered PKA inhibitor peptide or small-molecule inhibitors, effectively alleviates fibrous dysplasia lesions in a fibrous dysplasia mouse model and safeguards bone structure by increasing trabecular bone volume in a PKA-inhibition mouse model. Although long-term pharmacological PKA inhibition remains untested, these findings demonstrate that PKA is a dependent factor in fibrous dysplasia initiation and progression, underscoring its potential as a therapeutic target.
Similar content being viewed by others
Introduction
Fibrous dysplasia (FD) is a skeletal disease characterized by the replacement of normal bone with fibrous tissue and irregularly mineralized woven bone, leading to bone fractures, deformities, and pain1. FD is a disease of skeletal stem cells (SSCs) harboring activating mutations in GNAS, which encodes the α-subunit of the Gs stimulatory protein (Gαs)2,3. Currently, there is no cure for FD. Antiresorptive agents such as bisphosphonates (BPs) and Denosumab are used off-label to alleviate FD-related bone pain and reduce fracture risk1,4. However, BPs cannot prevent disease progression and may not alleviate pain effectively for some patients5,6. Although Denosumab has been shown to effectively reduce the progression of FD lesions and control bone pain7,8,9, the possibility of life-threatening bone-turnover rebound with hypercalcemia after discontinuation raises concerns about its safety when used to treat FD10. This issue highlights the urgency of understanding the pathophysiological mechanisms of FD and identifying new therapeutic targets.
Gαs modulates signaling by binding GTP to activate adenylyl cyclase and generate cyclic AMP (cAMP), a key second messenger, and then returns to an inactive state through intrinsic GTPase-mediated hydrolysis of GTP to GDP. GαsR201C, one of the major FD-causing mutations, encodes a Gαs with defective GTPase activity, thereby locking it in a constitutively active state and resulting in sustained accumulation of cAMP2,3. We previously proposed that a cure for FD could be achieved by reducing the expression of the disease-causing mutation and/or its associated downstream molecular events3. Protein kinase A (PKA), the principal intracellular effector of cAMP, is ubiquitously expressed in eukaryotic cells and is involved in numerous biological processes and disease conditions11. Under normal physiological conditions, PKA is tightly regulated by the stability of the holoenzyme12. The inactive tetrameric PKA dissociates after the cooperative binding of cAMP to the regulatory subunits (R), releasing two catalytic subunits (C) to phosphorylate PKA substrates. PRKACA encodes the catalytic α subunit of PKA (PKAcα). The W197R mutant of PRKACA remains active after the binding of R subunits13,14, which has been associated with cortisol-secreting adrenal adenomas and Cushing syndrome15. The R subunit and protein kinase inhibitor peptide (PKI) are two known physiological inhibitors of PKA that competitively bind to the C subunits via their inhibitory consensus sequence16. Our previous study revealed markedly elevated phosphorylation levels of PKA in FD lesions, corresponding to hyperactivated Gαs/cAMP signaling3. We hypothesized that PKA plays an important role in the initiation and progression of FD and thus could be a potential therapeutic target.
The PKA signaling pathway plays a crucial yet ambiguous role in controlling skeletal homeostasis. Studies have reported opposite effects of PKA signaling on osteogenic differentiation and bone formation. Some studies indicate that PKA activation promotes the osteogenic differentiation of osteoprogenitor cells and bone formation17,18,19,20, whereas others show that it inhibits these processes21,22,23. Moreover, several studies have revealed differential roles of cAMP/PKA signaling in the regulation of bone remodeling, with varying effects at different stages of differentiation24,25. In addition to osteogenic differentiation and bone formation, Gαs/cAMP/PKA signaling is also involved in regulating osteoclastogenesis and bone resorption through receptor activator of nuclear factor kappa-B ligand (RANKL)26,27 or nuclear factor of activated T cells c1 (NFATc1)28,29, although the results are conflicting. Global or macrophage/osteoclast-specific deletion of Gαs led to reduced trabecular bone quality and increased trabecular osteoclasts30. However, activation of PKA in osteocytes and late osteoblasts has been reported to cause no significant bone resorption19. Inconsistencies in existing studies largely stem from variations in the experimental materials and methods used across studies and data interpretation. These inconsistencies emphasize the need for further research to better understand PKA’s function and therapeutic potential in bone development, remodeling, and related diseases, including FD.
This study demonstrated that PKA activation in SSCs is sufficient to induce FD-like lesions in a conditional, tetracycline-inducible transgenic mouse model expressing PKAcαW197R. PKA inhibition in our previously established FD mouse model3, either by PKI or by small molecular inhibitors of PKA (H89 and Rp-8-Br-cAMPs)31,32, largely rescued FD lesions. Together, our findings demonstrated that FD initiation and progression are strictly PKA-dependent. PKA promotes osteoclastogenesis, induces aberrant osteogenic differentiation and proliferation of SSCs, but suppresses bone formation, leading to imbalanced osteolytic lesions in FD. Downregulating the PKA signaling pathway effectively alleviates FD lesions in mice and safeguards bone structure, suggesting that PKA is a potential therapeutic target in FD.
Results
PKA activation in skeletal stem cells results in FD-like lesions
PKAcαW197R, the constitutively active mutant of PKAcα, was generated via a site-directed mutagenesis approach to introduce the W197R amino acid substitution in recombinant human PKAcα13. Compared with wild-type PKAcα, PKAcαW197R resulted in more robust transcriptional activation of the cAMP-responsive element (CRE) luciferase reporter in 293T cells (Fig. 1a)3. Immunoblotting for the HA tag, which was added to the PKAcαW197R construct, confirmed the successful expression of the PKAcαW197R transgene in 293 T cells following transfection (Fig. 1b). Furthermore, increased phosphorylation levels of both PKA and CREB, downstream effectors of the Gαs/PKA pathway, were observed, as shown by immunoblotting and ELISA analyses (Fig. 1b, c). These data support the efficient activation of the PKA signaling pathway by PKAcαW197R. Next, we developed conditional transgenic mice expressing PKAcαW197R and reverse tetracycline-regulated transactivator (rtTA) under the control of Tet-responsive element (TRE) and Loxp-STOP-Loxp (LSL) cassettes, respectively (Tet-PKAcαW197R-rtTA). rtTA is transcribed and translated after the LSL cassette is eliminated by Cre recombinase and binds to the TRE. However, it only activates transcription of the target gene PKAcαW197R in the presence of doxycycline (Dox). By crossing the Tet-PKAcαW197R-rtTA mouse with the Prrx1-Cre mouse, we created an SSC-specific, tetracycline-inducible transgenic mouse model, Tet-PKAcαW197R-rtTA/Prrx1-Cre (referred to as PKA mice) (Fig. 1d and Supplementary Fig. 1a, d, f). In PKA mice, the expression of PKAcαW197R is restricted to Prrx1-expressing SSCs in limb and craniofacial bones. All pups were born healthy following a Mendelian distribution with no obvious differences in either size or behavior. The expression of the PKAcαW197R transgene in limb bone was confirmed via quantitative PCR (qPCR) analysis and HA tag immunoblotting and was associated with increased PKA phosphorylation levels (Fig. 1e, f) in PKA mice treated with Dox. These data support the efficient and tissue-specific activation of the PKA signaling pathway in PKA mice.
a Luciferase assay showing transcriptional activation of cAMP-responsive element (CRE) was elevated by both PKAcα and its constitutively active mutant PKAcαW197R in 293T cells (n = 9 independent experiments, one-way ANOVA with Tukey’s multiple comparisons test). PKAcαW197R induced more robust activation of CRE luciferase activity than wild-type PKAcα. b Immunoblot showing the phosphorylation of PKA and CREB in PKAcαW197R-transfected cells, with HA-tag detection confirming transfection. Three independent experiments were performed. c ELISA results showing the level of phosphorylated CREB in PKAcαW197R-transfected cells (n = 6 independent experiments, two-way ANOVA with Sidak’s multiple comparisons test). d Schematic of the Tet-PKAcαW197R/Prrx1-Cre transgenic mouse model (PKA mice) for tissue-specific expression of PKAcαW197R upon Dox administration. e qPCR analysis of PRKACA expression in limb bones of PKA mice (Control n = 5 and PKA n = 8, biologically independent samples, unpaired two-tailed t-test). f Immunoblotting confirming phosphorylated PKA levels in limb bones. Three independent experiments were performed. The data are presented as box-and-whisker plots, with boxes representing the interquartile range (25th–75th percentiles), the minimum and maximum values reached by bars, the median plotted as a line in the middle, and the mean marked as “+”. Source data are provided as a Source Data file.
To investigate whether the expression of PKAcαW197R in SSCs is sufficient to initiate FD, PKA mice were treated with Dox (0.1 g/L in drinking water) at the age of 6 weeks and evaluated visually for signs of bone lesions daily (Fig. 2a and Supplementary Fig. 2a). While littermates appeared normal, all PKA mutant mice developed typical FD-like lesions, as judged by limb swelling (Fig. 2b) and reduced locomotor activity (Supplementary Fig. 2b) rapidly following Dox induction (Fig. 2c). Radiological analyses revealed FD with a “ground-glass” appearance (Fig. 2d, red arrows) and severe osteolytic changes in hindlimb bones and skulls (Fig. 2e, f). Notably, PKA mice presented significant but fewer expansile bone lesions than did those with the disease-causing mutant GαsR201C (Fig. 2e)3. The tibia was used for quantitative μCT analysis. As tibial length did not differ significantly across the different mouse groups (Supplementary Fig. 2c), a standardized region of interest (ROI) was defined 2 mm distal to the growth plate and 1 mm in thickness (Supplementary Fig. 2d). The osteolytic changes in PKA mice were further confirmed by reduced bone volume fraction (BV/TV), bone mineral density (BMD), as shown by μCT analysis (Fig. 2g).To further study the morphological characteristics of these lesions, a cross-sectional ROI located 2.5 mm from the growth plate (Supplementary Fig. 2e) revealed a significant reduction in marrow area (Ma.Ar) and endocortical/periosteal perimeter (Ec.Pm/Ps.Pm) (Supplementary Fig. 2f), suggesting that expansile lesions invade and compress the marrow cavity. Histopathological examinations of tibias and skulls revealed classical histological features of human FD lesions in PKA mice (Fig. 2h and Supplementary Fig. 3a)1. H&E staining revealed that normal lamellar bone was replaced by a fibrous matrix (white stars) and irregularly shaped, immature woven bone (black stars), which lacked osteoblasts rimming its surface. Abundant osteoclasts (black arrows) were observed within the lesional area, suggesting osteoclastic bone resorption and increased bone remodeling. Von Kossa staining of undecalcified tibias revealed severe mineralization defects and prominent osteoid (white arrows). The cortical bone was compromised by widespread undermineralized tissue (white stars). Sirius Red staining revealed widespread green birefringent type III collagen under polarized light, indicating bone tissue damage. In conclusion, the expression of the activating mutant PKAcαW197R in SSCs induces FD-like lesions.
a A summary table listing the genotypes, targeted molecules, and Dox dosage regimens for each transgenic mouse line used in this study. PKI4A is a nonsense mutant of PKI. b Representative hindlimb images of Tet-PKAcαW197R/Prrx1-Cre (PKA mice), Tet-GαsR201C/Tet-PKI4A/Prrx1-Cre (FD-PKI4A mice), Tet-GαsR201C/Tet-PKI/Prrx1-Cre (FD-PKI mice), and littermate controls. c Kaplan‒Meier curve of mice free from visible FD-like symptoms (limb swelling and reduced mobility, biologically independent samples, two-tailed log-rank test). d μCT images of hindlimb bones showing ground-glass deformities (red arrows) in PKA and FD-PKI4A mice, which were not observed in FD-PKI mice. e Representative images of three-dimensional (3D) reconstructions of tibias showing expansile lesions in PKA and FD-PKI4A mice. f Representative 3D reconstructions of skulls revealing bone defects in PKA and FD-PKI4A mice. g Quantitative μCT analyses of the bone volume fraction (BV/TV) and bone mineral density (BMD) in defined ROIs of PKA, FD-PKI4A, FD-PKI, and littermate controls (Control n = 17, PKA n = 5, FD-PKI4A n = 6 and FD-PKI n = 6, biologically independent samples, one-way ANOVA with Tukey’s multiple comparisons test). h Histopathological examination (H&E, von Kossa, and Sirius red staining) of tibias showing FD-like lesions in PKA and FD-PKI4A mice. Lesions include multinucleated osteoclasts (black arrows) located on the surface of irregular woven bone (black stars), osteoid deposition lining the woven bone surfaces (white arrows), and disorganized woven bone lacking osteoblast rimming and embedded within a collagen-rich fibrocellular matrix (white stars). In contrast, FD-PKI and control mice exhibit dense cortical bone with defined boundaries (dashed lines). Sirius red staining reveals disorganized woven bone and type III collagen fibrosis in PKA and FD-PKI4A mice. Three independent experiments were performed. The data are presented as box-and-whisker plots, with boxes representing the interquartile range (25th–75th percentiles), the minimum and maximum values reached by bars, the median plotted as a line in the middle, and the mean marked as “+”. Source data are provided as a Source Data file.
PKA inhibition halts FD-like bone lesions induced by Gαs R201C
The endogenous protein kinase inhibitor peptide (PKI) is a potent PKA-specific inhibitor that has been widely used in PKA-related research16. The synthetic peptide of the PKA-inhibiting domain of PKI (amino acids 1–24) and its nonsense mutant, PKI4A, were employed in our study to modulate PKA activity33,34. In vitro analyses demonstrated the robust inhibitory effect of PKI on the PKA signaling pathway. The phosphorylation of both PKA and CREB induced by a mixture of forskolin and 3-isobutyl-1-methylxanthine (FI) was suppressed after PKI plasmid transfection but not after PKI4A transfection (Fig. 3a, b). A similar strategy as that used for the PKA mice was employed to develop conditional transgenic mice expressing PKI or PKI4A under the control of TRE, along with LSL-rtTA and EGFP elements (Tet-PKI-rtTA and Tet-PKI4A-rtTA, respectively). Unless otherwise indicated, tet-PKI-rtTA and tet-PKI4A-rtTA in this manuscript refer to heterozygous genotypes. PKA activity modulation in our previously established FD mouse model (Tet-GαsR201C/LSL-rtTA/Prrx1-Cre)3 was achieved by replacing LSL-rtTA with Tet-PKI-rtTA or Tet-PKI4A-rtTA mice, creating Tet-GαsR201C/Tet-PKI-rtTA/Prrx1-Cre (referred to as FD-PKI mice) and Tet-GαsR201C/Tet-PKI4A-rtTA/Prrx1-Cre (referred to as FD-PKI4A mice), respectively (Fig. 3c and Supplementary Fig. 1b–f). Only heterozygous FD-PKI and FD-PKI4A mice were utilized in the study. Homozygous FD-PKI mice were excluded due to their ineffectiveness in lowering the PKA signaling pathway for unknown reasons (Supplementary Fig. 4a). Additionally, homozygous FD-PKI4A mice presented a low survival rate (Supplementary Fig. 4b), possibly because of excessive rtTA expression in Tet-PKI4A-rtTA mice. The specific expression of the PKI transgene in limb bones of FD-PKI mice was confirmed by qPCR analysis (Fig. 3d). The GαsR201C mutation upregulated the Gαs/cAMP signaling pathway in both FD-PKI and FD-PKI4A mice, as evidenced by increased GNAS expression in their limb bones (Fig. 3d) and elevated cAMP levels in the serum (Fig. 3e). However, the phosphorylation of PKA was significantly suppressed in FD-PKI mice but not in FD-PKI4A mice (Fig. 3f). These data demonstrated that PKA activity was effectively suppressed in FD-PKI mice without affecting the activation of the upstream Gαs/cAMP signaling pathway.
a Immunoblotting and b ELISA showing the phosphorylation levels of PKA and CREB in 293T cells stimulated with forskolin and 3-isobutyl-1-methylxanthine (FI) with or without PKI plasmid transfection (n = 6 independent experiments, two-way ANOVA with Tukey’s multiple comparisons test). Three independent immunoblotting were performed. c Schematic representation of the Tet-GαsR201C/Tet-PKI/Prrx1-Cre (FD-PKI mice) transgenic mouse model, which is engineered to express the GαsR201C mutation, thereby upregulating the Gαs/cAMP signaling pathway while concurrently expressing PKI to inhibit PKA signaling in a tissue-specific manner upon Dox administration. The Tet-GαsR201C/Tet-PKI4A/Prrx1-Cre (FD-PKI4A mice) model was generated via the same strategy. d qPCR analysis confirming PKI mRNA transcription in FD-PKI mice (Control n = 7 and FD-PKI n = 8, biologically independent samples, unpaired two-tailed t-test) and showing increased GNAS mRNA expression in limb bones of both FD-PKI and FD-PKI4A mice (Control n = 27, FD-PKI4A n = 7 and FD-PKI n = 12, biologically independent samples, one-way ANOVA with Tukey’s multiple comparisons test). e ELISA results showing cAMP levels in the serum of FD-PKI and FD-PKI4A mice (Control n = 6, FD-PKI4A n = 5 and FD-PKI n = 7, biologically independent samples, one-way ANOVA with Tukey’s multiple comparisons test). f Immunoblotting showing the phosphorylation of PKA in PKA, FD-PKI4A, and FD-PKI mice. Three independent experiments were performed. The data are presented as box-and-whisker plots, with boxes representing the interquartile range (25th–75th percentiles), the minimum and maximum values reached by bars, the median plotted as a line in the middle, and the mean marked as “+”. Source data are provided as a Source Data file.
To test whether the progression of FD is PKA-dependent, both FD-PKI4A and FD-PKI mice were treated with same doses of Dox (0.005–0.1 g/L in drinking water) at the age of 6 weeks. The disease burden worsened and caused death in both FD-PKI4A and FD-PKI mice as the dose of Dox increased, although FD-PKI mice presented a milder disease burden than FD-PKI4A mice did (Supplementary Fig. 5a). All FD-PKI4A mice developed severe FD-like bone lesions within 1 week of Dox induction at a dose as low as 0.006 g/L (Fig. 2b–g, Supplementary Fig. 2b–f, Supplementary Fig. 3a, and Supplementary Fig. 4c). The histopathological changes in FD-PKI4A mice (Fig. 2h) mirrored those observed in our previously established FD mice (Supplementary Fig. 6a–c). Interestingly, most FD-PKI mice failed to develop severe limb swelling or reduced mobility after 2 weeks of Dox induction at the same dose despite the mild swelling observed in the limbs and paws (Fig. 2b, c and Supplementary Fig. 2b). The cortical bone and skull of FD-PKI mice appeared continuous and intact, with no evidence of deformities or osteolytic changes (Fig. 2d–f). The anatomical structure of limb bones in FD-PKI mice did not differ from those in control mice (Fig. 2g and Supplementary Fig. 2d–f). Histopathologically, typical FD-like changes were absent in both tibias and skull bones of FD-PKI mice (Fig. 2h and Supplementary Fig. 3a). The cortical bone was well mineralized without the presence of woven bone. Upon close examination of hindlimb samples, only 3 out of 32 FD-PKI mice developed minor FD-like lesions under this dose of Dox, which were confined to the metaphysis with no invasion into the bone marrow cavity (Fig. 2c and Supplementary Fig. 5a). Collectively, these findings suggest that PKA inhibition halts FD-like bone lesions induced by GαsR201C.
PKA inhibition in FD-SSCs suppresses osteoclastogenesis and promotes bone formation
Next, we investigated the bone remodeling events regulated by PKA. The increase in osteoclastogenesis caused by GαsR201C was suppressed to normal levels in FD-PKI mice, as evidenced by the absence of tartrate-resistant acid phosphatase (TRAP)-positive osteoclasts in the cortical bone (Fig. 4a and Supplementary Fig. 7a). In contrast, the differentiation of osteoclasts was significantly increased in PKA and FD-PKI4A mice, which led to severe bone resorption (Fig. 4a and Supplementary Fig. 7a). Consistently, the serum level of tartrate-resistant acid phosphatase 5b (TRACP-5b) (Fig. 4b) and the transcriptional level of osteoclast-specific markers (Csf1r, Rank, Nfatc1, and Acp5) were increased in the bone lesions of PKA and FD-PKI4A mice, similar to those of FD mice (Supplementary Fig. 7b). However, these osteoclast markers demonstrated downregulated expression in FD-PKI mice. Rankl was suppressed to normal levels in FD-PKI mice in both gene and circulating protein forms (Supplementary Fig. 7c and Fig. 4c). Besides the unchanged expression levels of Osteoprotegerin (Opg), the decoy receptor for Rankl, upon PKA signaling modulation, the Rankl/Opg ratio was significantly reduced in FD-PKI mice (Supplementary Fig. 7c, d). However, Rankl level and Rankl/Opg ratio were significantly elevated upon PKA activation in PKA and FD-PKI4A mice, stimulating osteoclast differentiation (Fig. 4c and Supplementary Fig. 7c, d). These data suggest that osteoclastic bone resorption in FD lesions is driven by Rankl-dependent osteoclastogenesis, which is promoted by PKA activation.
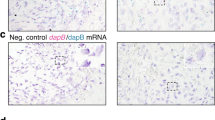
a TRAP staining of tibias showing TRAP-positive cells in PKA, FD-PKI4A and FD-PKI mice. b ELISA results showing the serum TRACP-5b levels in PKA, FD-PKI4A and FD-PKI mice (Control n = 17, PKA n = 6, FD-PKI4A n = 5 and FD-PKI n = 13, biologically independent samples, one-way ANOVA with Tukey’s multiple comparisons test). c ELISA results of serum Rankl levels (Control n = 23, PKA n = 5, FD-PKI4A n = 5 and FD-PKI n = 14, biologically independent samples, one-way ANOVA with Tukey’s multiple comparisons test). d qPCR analyses of osteogenic markers in limb bones (Control n = 34, PKA n = 9, FD-PKI4A n = 7 and FD-PKI n = 31, biologically independent samples, two-way ANOVA with Sidak’s multiple comparisons test). e Immunohistochemical staining and f quantitative analyses showing increased Osx-positive cells in PKA and FD-PKI4A mice, which returned to baseline levels in FD-PKI mice (Control n = 11, PKA n = 9, FD-PKI4A n = 11 and FD-PKI n = 6, biologically independent samples, one-way ANOVA with Tukey’s multiple comparisons test). In contrast, Ocn-positive cells are decreased in PKA and FD-PKI4A mice but elevated in the FD-PKI mice (Control n = 15, PKA n = 15, FD-PKI4A n = 11 and FD-PKI n = 12, biologically independent samples, one-way ANOVA with Tukey’s multiple comparisons test). g EdU staining and h quantitative analysis demonstrating increased proliferation in PKA and FD-PKI4A mice, with no significant difference in proliferation between PKA mice and FD-PKI4A mice (Control n = 9, PKA n = 11, FD-PKI4A n = 8 and FD-PKI n = 13, biologically independent samples, one-way ANOVA with Tukey’s multiple comparisons test). The data are presented as box-and-whisker plots, with boxes representing the interquartile range (25th–75th percentiles), the minimum and maximum values reached by bars, the median plotted as a line in the middle, and the mean marked as “+”. Source data are provided as a Source Data file.
Conversely, PKA activation enhanced the osteogenic lineage commitment of SSCs but inhibited osteoblast maturation. Significantly elevated expression of osteoblast transcription factors, runt-related transcription factor 2 (Runx2) and Osterix (Osx), and other osteogenic genes, such as alkaline phosphatase (Alp) and collagen type 1 (Col1a1), and marginally decreased expression of the mature osteoblast marker osteocalcin (Ocn) were detected in the bones of PKA mice (Fig. 4d). The aberrant osteogenic differentiation of SSCs disrupted by Gαs signaling activation was restored in FD-PKI mice following PKA inhibition. Ocn-expressing matured osteoblasts (lining cells) were observed on the surface of the trabecular bone in FD-PKI mice (Fig. 4e, f). Notably, early osteogenic differentiation was not completely blocked in FD-PKI mice, as demonstrated by the expression of Osx on the surface of trabecular bone (Fig. 4e, f). Furthermore, the highly proliferative activities of the fibroblast-like cells were revealed by a 5-ethynyl-2’-deoxyuridine (EdU) proliferation assay in PKA and FD-PKI4A mice (Fig. 4g, h)3,35. Collectively, our data demonstrated that the PKA signaling pathway promotes Rankl-dependent osteoclastogenesis and induces early osteogenic differentiation and proliferation of SSCs but impairs their maturation and mineralization. Downregulating ectopically activated PKA signaling could reduce osteoclastogenesis and restore the balance between osteogenic differentiation and osteoclastogenesis, resulting in bone formation.
Downregulated PKA signaling safeguards bone structure
To further study the effects of PKA on bone remodeling without hyperactivation of Gαs/cAMP signaling, we created a Tet-PKI-rtTA/Prrx1-Cre mouse model (referred to as PKI mice) (Fig. 5a and Supplementary Fig. 1b, d, f). We hypothesized that the bone volume and density would increase in PKI mice upon PKA inhibition on the basis of accumulated data from PKA and FD-PKI mice. To downregulate PKA signaling in the SSCs of limb bone and observe phenotypic changes, various doses of Dox were administered to PKI mice for up to 6 months (Fig. 5b). The expression of the PKI transgene in limb bone was confirmed by qPCR analysis and EGFP tag immunofluorescence staining in mutant mice (Fig. 5c, d). The phosphorylation of PKA was decreased in limb bones of PKI mice following Dox administration (Fig. 5e). Surprisingly, there were no significant phenotypic differences between PKI and littermate control mice after 6 months of high-dose Dox induction (6 g/kg in the diet) (Fig. 5f). The cortical bone of the tibias was continuous and well mineralized without significant pathological changes in the PKI mice (Fig. 5g, h). Osteoclastogenesis and Rankl signaling remained at a normal level compared with that in control mice (Fig. 5i and Supplementary Fig. 8a–c). Interestingly, abundant adipocytes were observed in the bone marrow of PKI mice, along with subtle but significant changes in a few early osteogenic markers (Fig. 5h, j and Supplementary Fig. 8d)25,36. Contrary to our hypothesis, μCT analysis revealed a trend toward reduced cortical bone thickness in PKI mice compared to littermate controls, although the differences were not statistically significant (Fig. 5k, l). This trend was further confirmed by cross-sectional morphological analysis (Supplementary Fig. 8e). Cortical bone mass was unaffected by PKA inhibition, as shown by the unchanged BV/TV and tissue mineral density (TMD) (Fig. 5l). However, significant increases in both the number and thickness of trabecular bone were observed in PKI mice, resulting in a subtle increase in trabecular bone mass (Fig. 5m, n and Supplementary Fig. 8f, g). Mirroring the findings in PKI and PKA mice, MC3T3-E1-14 osteoblastic cells exhibited markedly increased ALP activity but reduced mineralized nodule formation upon PKA activation, whereas PKA inhibition exerted the opposite effects (Supplementary Fig. 9a–e).
a Schematic representation of the Tet-PKI/Prrx1-Cre (PKI mice) transgenic mouse model, which is designed to express PKA inhibitor peptide (PKI) in a tissue-specific manner upon Dox administration. b Study regimen outlining the Dox treatment schedule for PKI and control mice, along with the timing of sample collection (V video, H histology, TC tissue collection, SC serum collection). c qPCR analysis of limb bones confirming the transcription of PKI mRNA in PKI mice (Control n = 4 and PKI n = 8, biologically independent samples, unpaired two-tailed t-test). d Immunofluorescence staining of tibias showing EGFP-tag expression, verifying successful PKI expression in PKI mice. Three independent experiments were performed. e Immunoblotting demonstrating the suppression of PKA phosphorylation in limb bone. Three independent experiments were performed. f Representative images of limb morphology and g μCT images of hindlimb showing no significant differences in limb swelling or bone deformity between PKI mice and littermate controls. h H&E staining and i TRAP staining of tibias revealing no significant differences in bone histomorphology or osteoclast activity between PKI mice and littermate controls. j Quantitative analysis of the number of adipocytes in tibias of PKI mice (Control n = 4 and PKI n = 5, biologically independent samples, unpaired two-tailed t-test). k, l Representative three-dimensional reconstructions and quantitative analyses of cortical bone and skull (Control n = 5 and PKI n = 9, biologically independent samples, unpaired two-tailed t-test). m, n Representative three-dimensional reconstructions and quantitative analyses of trabecular bone (Control n = 5 and PKI n = 9, biologically independent samples, unpaired two-tailed t-test). The data are presented as box-and-whisker plots, with boxes representing the interquartile range (25th–75th percentiles), the minimum and maximum values reached by bars, the median plotted as a line in the middle, and the mean marked as “+”. Source data are provided as a Source Data file.
PKA is a potential therapeutic target for FD
Inspired by the above data, we explored therapeutic options for FD by targeting PKA. Two small-molecule inhibitors of PKA, H89 and Rp-8-Br-cAMPS, both of which are potent and selective with distinct mechanisms, were utilized to decrease PKA activity in our FD mouse model (Supplementary Fig. 1e–h). The therapeutic regimen is shown in Fig. 6a. First, the FD phenotype was established in all FD mice after 3 days of Dox induction (0.2 g/L in the drinking water) (T1; Supplementary Fig. 10a–c). FD mice were then randomly divided into the FD, FD + H89, and FD + Rp-8-Br-cAMPs groups. While all the mice were subjected to the same dose of Dox throughout the study, the FD mice in the two PKA inhibitor groups received either H89 or Rp-8-Br-cAMPs via intraperitoneal injection every other day for 11 days (T2). At T2, all FD mice presented significantly upregulated GNAS expression in limb bones (Fig. 6b). PKA signaling was effectively suppressed in FD mice from both the FD + H89 and FD + Rp-8-Br-cAMPs groups, as evidenced by the decreased phosphorylation level of PKA in limb bones (Fig. 6c). Limb swelling and reduced mobility observed in FD mice at T1 had significantly improved in both inhibitor-treated groups by T2 (Fig. 6d, e, Supplementary Fig. 10a, and Supplementary Fig. 11a). By T2, FD mice in the PKA inhibitor groups exhibited less limb swelling and significantly improved mobility compared with FD group, although their mobility remained below normal levels (Fig. 6d, e and Supplementary Fig. 11a). Similarly, FD mice treated with PKA inhibitors presented reduced ground-glass opacities in hindlimb bones (Fig. 6f, red arrows) and fewer expansile osteolytic changes in tibias and skulls (Fig. 6g, h). Given the comparable tibial lengths across groups, quantitative μCT analysis was performed within standardized ROIs in the metaphysis and diaphysis (Supplementary Fig. 11b, c, e). PKA inhibition mitigated FD lesions, as evidenced by increased BV/TV and BMD in both regions (Fig. 6i). Accordingly, the marrow space (Ma.Sp) in the diaphyseal region was restored in PKA inhibitor-treated mice (Supplementary Fig. 11d, f). Further analysis revealed that PKA inhibition improved tibial mechanical performance, as indicated by significant increase maximum load capacity, and a trend toward increased elastic modulus (Fig. 6j, k).
a Therapeutic regimen outlining Dox and PKA inhibitor administration in GαsR201C/LSL-rtTA/Prrx1-Cre (FD mice), along with the timing of sample collection (V video, H histology, TC tissue collection, SC serum collection). b qPCR analysis at T2 showing GNAS mRNA expression in limb bones (Control n = 7, FD n = 11, FD + H89 n = 4 and FD + Rp-8-Br-cAMPs n = 4, biologically independent samples, one-way ANOVA with Tukey’s multiple comparisons test). c Immunoblotting at T2 demonstrating PKA phosphorylation in limb bones. Three independent experiments were performed. d Representative limb images at T2 of FD mice, FD + H89 mice, FD + Rp-8-Br-cAMPs mice and littermate controls. e Kaplan‒Meier curve showing the persistence of FD-like symptoms (limb swelling and limping behavior) in the FD group (n = 11), whereas the FD + H89 (n = 11) and FD + Rp-8-Br-cAMPs (n = 7) groups presented a reversal of symptoms within 1 week of PKA inhibitor treatment (biologically independent samples, two-tailed log-rank test). f μCT images of hindlimb at T2 showing more pronounced ground-glass deformities (red arrows) in FD mice compared to FD + H89 mice and FD + Rp-8-Br-cAMPs mice. g Representative three-dimensional (3D) reconstructions of limb bone at T2 showing reduced expansile lesions in FD + H89 mice and FD + Rp-8-Br-cAMPs mice relative to FD mice. h Representative 3D reconstructions of skulls at T2. i Quantitative μCT analyses of the bone volume fraction (BV/TV) and bone mineral density (BMD) in FD mice, FD + H89 mice, FD + Rp-8-Br-cAMPs mice, and littermate controls (Control n = 9, FD n = 6, FD + H89 n = 4 and FD + Rp-8-Br-cAMPs n = 5, biologically independent samples, two-way ANOVA with Sidak’s multiple comparisons test). j Representative of load-displacement curves of tibias at T2 obtained from compression testing, with arrowhead marking the fracture point. k Biomechanical analyses of tibias at T2 showing maximum load and elastic modulus in FD mice, FD + H89 mice, FD + Rp-8-Br-cAMPs mice and controls (Control n = 4, FD n = 6, FD + H89 n = 5 and FD + Rp-8-Br-cAMPs n = 4, biologically independent samples, one-way ANOVA with Tukey’s multiple comparisons test). The data are presented as box-and-whisker plots, with boxes representing the interquartile range (25th–75th percentiles), the minimum and maximum values reached by bars, the median plotted as a line in the middle, and the mean marked as “+”. Source data are provided as a Source Data file.
H&E staining demonstrated that FD lesions were restricted to the metaphysis area in the mice treated with the PKA inhibitors and did not affect the diaphysis. In contrast, mice in the FD group exhibited fully developed FD lesions expanding throughout the whole tibias, accompanied by abundant osteoclasts and severe osteolytic bone damage (Fig. 7a–c). Similarly, FD lesions were significantly reduced in the skulls of inhibitor-treated FD mice (Supplementary Fig. 12a). PKA inhibition restored bone remodeling balance, as evidenced by reduced osteoclastogenesis (Fig. 7c, d and Supplementary Fig. 12b, c) and increased numbers of matured osteoblasts (Fig. 7e, f and Supplementary Fig. 12d). In addition, histological analyses of major non-skeletal organs at T2 revealed no significant pathological abnormalities following PKA inhibitor treatment (Supplementary Fig. 13a–h). However, the short observation period limits conclusions on long-term safety of systemic PKA inhibition, warranting further investigation. In conclusion, our findings demonstrate that PKA inhibition effectively alleviates FD lesions in mice, confirming that PKA is a potential therapeutic target in FD.
a H&E staining of tibias at T2 showing the restricted bone lesions in the inhibitor-treated groups. Lesions in FD group are characterized by multinucleated osteoclasts (black arrows) on the surface of irregular woven bone (black stars), and irregularly shaped woven bone lacking osteoblast rimming and embedded within a fibrocellular matrix (white star). In contrast, diaphysis ROIs of FD + H89 mice and FD + Rp-8-Br-cAMPs mice exhibit dense cortical bone with defined boundaries (dashed lines). b Quantitative analyses of FD lesion areas in the metaphysis and diaphysis ROIs showing reduction in FD-like bone lesions in FD + H89 and FD + Rp-8-Br-cAMPs mice compared to FD mice (Control n = 12, FD n = 8, FD + H89 n = 10 and FD + Rp-8-Br-cAMPs n = 5, biologically independent samples, one-way ANOVA with Tukey’s multiple comparisons test). c TRAP staining of tibias at T2 showing TRAP-positive cells in FD mice, FD + H89 mice, FD + Rp-8-Br-cAMPs mice, and littermate controls. d qPCR analysis of the Rankl/Opg ratio in limb bone tissue (Control n = 14, FD n = 10, FD + H89 n = 5 and FD + Rp-8-Br-cAMPs n = 7, biologically independent samples, one-way ANOVA with Tukey’s multiple comparisons test). e Immunohistochemistry and f quantitative analyses showing a reduction in Osx-positive cells and an increase in Ocn-positive cells Osx-positive cells in FD + H89 mice and FD + Rp-8-Br-cAMPs mice compared to FD mice (Osx Control n = 4, FD n = 10, FD + H89 n = 4 and FD + Rp-8-Br-cAMPs n = 5, Ocn Control n = 10, FD n = 17, FD + H89 n = 5 and FD + Rp-8-Br-cAMPs n = 12, biologically independent samples, one-way ANOVA with Tukey’s multiple comparisons test). The data are presented as box-and-whisker plots, with boxes representing the interquartile range (25th–75th percentiles), the minimum and maximum values reached by bars, the median plotted as a line in the middle, and the mean marked as “+”. Source data are provided as a Source Data file.
Discussion
In this study, we investigated the role of PKA in the pathophysiological mechanisms of FD via a combination of molecular and genetic approaches. Our findings demonstrate that FD initiation and progression are strictly PKA-dependent. PKA promotes osteoclastogenesis, induces aberrant osteogenic differentiation and proliferation of SSCs, but suppresses bone formation, leading to imbalanced osteolytic lesions in FD. Downregulating the PKA signaling pathway effectively alleviates FD lesions in mice and safeguards bone structure, suggesting that PKA is a potential therapeutic target in FD.
FD is caused by activating mutations of Gαs in SSCs, which lead to elevated cAMP concentrations and phosphorylation levels of PKA. Dysregulation of PKA signaling is associated with a wide range of diseases. PKAcαW197R, the mutant used in our study, is a constitutively active variant of the catalytic subunit of PKA13,14. Unlike some other PKAcα mutants, in silico analysis revealed no changes in the PKA substrate specificity of PKAcαW197R37, making it an ideal candidate for studying the mechanisms of PKA in FD pathogenesis.
To examine whether PKA activation is sufficient to initiate FD, we developed a transgenic mouse model expressing PKAcαW197R in SSCs under the control of Dox (Tet-PKAcαW197R-rtTA/Prrx1-Cre). Typical FD-like bone lesions rapidly develop in the limb and skull areas following the upregulation of PKA signaling through the expression of PKAcαW197R. This finding parallels others’ study in which the upregulation of PKA activity through R type I α subunit (R1α) haploinsufficiency led to FD-like bone lesions38. These findings demonstrate that the activation of PKA is sufficient to initiate FD and reinforces the pivotal role of PKA in FD. Notably, the FD-like lesions in the abovementioned mouse model exhibit more severe osteoclastic resorption and less expansion than those initiated by disease-causing GαsR201C mutants (Tet-GαsR201C/LSL-rtTA/Prrx1-Cre and Tet-GαsR201C/Tet-PKI4A-rtTA/Prrx1-Cre), suggesting that PKA plays a dominant role in osteoclastogenesis.
PKA inhibition in our previously established FD mouse model was achieved by introducing PKI into a transgenic system (Tet-GαsR201C/Tet-PKI-rtTA/Prrx1-Cre). Both GαsR201C and PKI were expressed in SSCs in mice upon induction with Dox. PKA activity was effectively suppressed in these mice without affecting the activation of the upstream Gαs/cAMP signaling pathway. As a result, the progression of FD was effectively halted by PKI but not its nonsense mutant PKI4A. Notably, different doses of Dox were used in our transgenic mouse models, including PKA, FD-PKI (4A), and FD mice. This variation may be attributed to the newer third generations of TRE and rtTA and the high-efficiency promoters used in the PKA and FD-PKI (4A) mice. In PKA and PKI (4A) mice, rtTA transgene expression driven by the CAG promoter might be greater than that driven by the PKG promoter in previous LSL-rtTA mice3,39,40, leading to increased sensitivity to Dox. This could explain the low survival rate of homozygous FD-PKI4A mice treated with Dox. As a result, only heterozygous FD-PKI (4A) mice were utilized in the study. For better comparison, the Dox dose for FD-PKI mice was adjusted to match that of FD-PKI4A mice, resulting in comparable lesions to those observed in FD mice. Together, our data demonstrate that FD initiation and progression are strictly PKA-dependent.
Next, we assessed PKA as a therapeutic target for FD. Our data demonstrate that FD lesions in mice were effectively alleviated through the use of the pharmacological PKA inhibitors H89 and Rp-8-Br-cAMPs, highlighting the potential of targeting PKA as a novel therapeutic approach for FD. Notably, many studies have identified the non-PKA-specific actions of H8941. Although Rp-8-Br-cAMPs is considered selective inhibitor of type I PKA due to its cAMP analog structure and mechanisms of action32, their inhibitory efficacy may be compromised when the cAMP level is extremely high, as in our FD mouse model. Additionally, Rp-8-Br-cAMPs may bind to exchange protein activated by cAMP (Epac), another direct target of cAMP that shares similar cyclic nucleotide–binding sites with PKA42. Epac is a guanine nucleotide exchange factor for the small GTPases Rap1/2, and it has been implicated in various cellular processes, such as cell adhesion, cell–cell junction formation, insulin secretion, and neurotransmitter release43,44. There is a complex interconnection between the Epac- and PKA-mediated signaling pathways. For example, a recent study showed that inhibiting PKA via PKI diverts GPCR/Gαs/cAMP signaling toward EPAC and ERK activation and is involved in tumor growth45. More studies are needed to elucidate the role of Epac in FD pathogenesis.
From a disease perspective, Gαs functions as a negative phenotypic regulator of bone mass, as evidenced by the opposing bone manifestations observed in Albright’s hereditary osteodystrophy (AHO), progressive osseous heteroplasia (POH), and FD46,47. AHO and POH are associated with inactivating Gαs mutations, which are clinically characterized by heterotopic ossification48, whereas FD is linked to activating Gαs mutations, leading to bone destruction2. However, the role of Gαs/cAMP/PKA signaling in regulating bone remodeling is controversial and context-dependent, largely due to variations in the experimental materials and methods used across studies and data interpretation. For example, Gαs or PKA dysregulation in different cell populations often leads to complicated or opposing results19,20,30,49,50,51. PKA signaling appears to regulate stem cells and progenitor cells differently from bone cells, such as osteoblasts and osteocytes, although the underlying mechanisms remain unclear. Importantly, the expression levels of osteogenic transcription factors, such as Runx2 and Osterix, do not necessarily correlate with the quantity or quality of bone formation in vivo, as observed phenotypically. Conclusions concerning how PKA regulates osteogenic differentiation should not rely solely on changes in the expression levels of osteogenic markers, which may help explain discrepancies between in vitro and in vivo studies18,20,22,49. Accumulating evidence supports a stage-dependent regulatory model in which Gαs/cAMP/PKA promotes early osteogenic differentiation but impairs maturation3,25,52,53. Additionally, Gαs has been shown to exert differential effects on trabecular and cortical bone29,30,49 and age-dependent54 and sex-dependent19,20,55 influences on osteogenic differentiation or bone formation, suggesting the involvement of complex regulatory mechanisms in bone remodeling.
Our findings suggest a dual regulatory model of bone remodeling in which PKA induces early osteogenic differentiation and proliferation of SSCs but impairs their maturation and mineralization while significantly enhancing RANKL-dependent osteoclastogenesis. However, unlike Gαs, the downstream effector PKA does not appear to function as a straightforward negative regulator of bone mass. Compared with the dramatic bone loss caused by PKA hyperactivation in this study, PKA inhibition in PKI mice had only a subtle effect on trabecular bone anabolism, suggesting the presence of compensatory feedback mechanisms that counterbalance the downregulation of PKA signaling. This bone safeguard effect makes PKA inhibition a promising anabolic therapy for bone destruction diseases, including FD and osteoporosis56. In addition, our findings provide preliminary insights into the altered adipogenic differentiation of stromal cells resulting from PKA inhibition.
FD typically manifests in adolescence and progresses into adulthood57, necessitating early intervention and ongoing treatment. Our study highlights, for the first time, the dependency of PKA on the initiation and progression of FD and suggests the promising therapeutic potential of PKA inhibition in treating FD and other similar bone destruction diseases. The safety of the antiresorptive medications currently used in FD management is an increasing concern. We demonstrated that long-term PKA inhibition in mice, restricted to SSCs in the limb and craniofacial areas, caused no significant side effects on bone or soft tissue. Instead, it slightly increased the trabecular bone volume. However, systemic and long-term effects of pharmacological PKA inhibition could not be assessed in this study. Targeting PKA, rather than the upstream disease-causing Gαs mutations, may offer a more focused therapeutic approach with potentially fewer off-target effects. Encouragingly, the pathophysiological role of the Gαs/PKA pathway has recently gained increased attention from researchers11. Various promising approaches and delivery systems targeting different components of the Gαs/PKA pathway have been developed and continue to evolve58,59,60,61, paving the way for molecular therapies for FD and other Gαs/PKA-related diseases.
This study has several limitations. The regulatory mechanisms of PKA in bone remodeling remain elusive. More in-depth studies are needed to reveal the underlying mechanisms, particularly the possible compensatory crosstalk mechanisms that counterbalance the downregulation of PKA signaling in bone remodeling, as observed in this study. This approach could lead to the identification of additional therapeutic targets for bone metabolism diseases. Moreover, given the broad involvement of PKA in physiological processes, the safety of the general and long-term use of PKA inhibition requires further evaluation.
Methods
Study design
This study aimed to evaluate the influence of PKA on FD development, its regulatory impact on differentiation, and its potential as a therapeutic target. These objectives were addressed by (i) creating a series of tetracycline-inducible, tissue-specific transgenic models (PKA mice, PKI mice, FD-PKI mice, and FD-PKI4A mice) to achieve in vivo regulation of the Gαs/cAMP/PKA signaling axis, (ii) examining the bone tissue phenotype in these mice, (iii) investigating the cellular and molecular changes induced by PKA regulation both in vivo and in vitro, and (iv) studying the effects of the intraperitoneal injection of two small-molecule PKA inhibitors on attenuating FD progression. Sample sizes were determined by the investigators on the basis of previous experimental experience, with exact numbers provided in the respective figure captions. In vivo experiments included all genetically screened animals in which the dosing strategy was adhered to. For experiments involving exogenous drug administration, animals and samples were randomly assigned to experimental and control groups. Endpoints were set at 2 weeks for all models except for PKI mice, with an endpoint of 6 months. The investigators were not blinded during the data analysis. All in vivo and in vitro experiments were replicated three or more times.
DNA constructs
Recombinant human PKAcα was amplified via PCR from pRSET PKAcα, a gift from Dr. Susan Taylor, with a C-terminal HA tag inserted into pCEFL (pCEFL PKAcα-HA). The sequence was verified by Sanger sequencing. The W197R amino acid substitution was carried out using the QuikChange II site-directed mutagenesis kit (Agilent, Santa Clara, CA, 200523)13. The primers used for mutagenesis are as follows: PKAcαW197R forward: 5’-cgtgtgaaaggccgtactAggaccttgtgtg-3’, PKAcαW197R reverse: 5’-cacacaaggtccTagtacggcctttcacacg-3’. The synthetic peptide of the PKA-inhibiting domain of PKI (amino acids 1–24) and its nonsense mutant, PKI4A, were employed in our study to modulate PKA activity34. Briefly, EGFP-PKI was cloned by inserting the 24 coding amino acids of human PKI-alpha (PKIA) into the C-terminus of EGFP. For use as a control, the phenylalanine and arginine residues of the PKI peptide were replaced with alanine to disrupt binding to protein kinase A (PKA), and the resulting protein was named EGFP-PKI4A.
DNA isolation and genotyping
DNA was extracted from the tail tissue. Each sample is incubated with 500 µl of RIPA lysis buffer (Beyotime, Shanghai, China, P0013C) and 10 µl of proteinase K (New England Biolabs, Ipswich, MA, USA, P8107S) at 55 °C overnight to ensure complete digestion. Following digestion, 500 µl of isopropanol is added to precipitate the DNA, which is then centrifuged at 7200 × g for 20 min. The DNA pellet is air-dried and resuspended in 500 µl of TE buffer (Biosharp, Anhui, China, BL531A). For PCR amplification, 2 µl of the gDNA template is used in a 25 µl reaction mixture. The primer used for amplification were as follows: (genotype, positive band position, forward sequence 5’ → 3’, reverse sequence 5’ → 3’): PKAcα-mutant, 601 bp, 5’-AAGCGTGTGAAAGGCCGTACTA-3’, 5’-GATCTCAGTGGTATTTGTGAGCCAG-3’; PKI-mutant, 349 bp, 5’-TGCTTCAGGAAGAACAGGTAGAAG-3’, 5’-CCAACCTTTGTTCATGGCAG-3’; PKI4A-mutant, 356 bp, 5’- ATGCCATTGCTTCAGGAGCC-3’, 5’- CCAACCTTTGTTCATGGCAG-3’; PKAcα/PKI(4 A)-wild type, 825 bp, 5’- AGTCTTTCCCTTGCCTCTGCT-3’, 5’- GGGTCTTCCACCTTTCTTCAG-3’; GαsR201C, 620 bp, 5’- CTAGAATTCGCTGTCTGCGA-3’, 5’- GCACTTTGGTTGCCTTCTC-3’; Prrx1-cre, 280 bp, 5’-GGACATGTTCAGGGATCGCCAGGCG-3’, 5’- GCATAACCAGTGAAACAGCATTGCTG-3’; rtTA-mutant, 215 bp, 5’- GAGTTCTCTGCTGCCTCCTG-3’, 5’- AAGACCGCGAAGAGTTTGTC-3’; rtTA-wild type, 322 bp, 5’- GAGTTCTCTGCTGCCTCCTG-3’, 5’- CGAGGCGGATACAAGCAATA-3’. Subsequent polymerase chain reaction (PCR) was performed using a C1000 Touch Thermal Cycler (Bio-Rad, Hercules, CA, USA) under the following conditions. An initial denaturation step was conducted at 94 °C for 5 minutes. This was followed by 30–35 cycles of denaturation at 94 °C for 30 seconds, primer annealing at Tm - 5 °C for 45 seconds, and extension at 72 °C for 1 min per kilobase of target DNA. After cycling, a final extension step was carried out at 72 °C for 5 minutes. The reaction was then held at 4 °C until agarose gel electrophoresis. After 20–30 min at 120 V, the gel is visualized under a gel imaging system (Clinx, Shanghai, China, GenoSens 2000) to determine the genotypes based on the specific band patterns observed.
Mice
To generate Tet-PKAcαW197R-rtTA, Tet-PKI-rtTA, and Tet-PKI4A-rtTA transgenic mice, the coding sequences were cloned downstream of the tet-responsive elements (TREs) within an improved Tet-On (3G) vector (Clontech® Laboratories, Inc., Mountain View, CA, USA, PT5148-1)62. Mice carrying the mutated human GαsR201C gene were previously described34, and they are referred to as “Tet-GαsR201C” mice. Mice expressing Cre recombinase in mouse limb buds driven by a Prrx1-derived enhancer (B6. Cg-Tg(Prrx1-cre)1Cjt/J), referred to as “Prrx1-Cre mice”, were obtained from The Jackson Laboratory (Bar Harbor, ME, USA)63. We confirmed the presence of transgenes through PCR analysis of tail DNA. Specific primers were used to verify the presence of the Tet-GαsR201C, Tet-PKAcαW197R, Tet-PKI, and Tet-PKI4A transgenes, each producing bands of the expected sizes (620, 601, 349, and 356 bp, respectively). The generation and characterization of the Tet-GαsR201C/LSL-rtTA/Prrx1-Cre mouse model (referred to as “FD mice”) have been previously described3. To create other models, Tet-PKAcαW197R-rtTA mice were crossed with Prrx1-Cre mice to generate Tet-PKAcαW197R-rtTA/Prrx1-Cre mice (referred to as “PKA mice”). Similarly, Tet-PKI-rtTA mice were crossed with Prrx1-Cre mice to produce PKI-rtTA/Prrx1-Cre mice (referred to as “PKI mice”). By crossing Tet-PKI-rtTA mice with Tet-GαsR201C and Prrx1-Cre mice, we generated Tet-GαsR201C/Tet-PKI-rtTA/Prrx1-Cre (referred to as “FD-PKI mice”). Finally, by replacing Tet-PKI-rtTA with Tet-PKI4A-rtTA, we generated Tet-GαsR201C/Tet-PKI4A-rtTA/Prrx1-Cre (referred to as “FD-PKI4A mice”).
Both male and female mice were used in all experimental and control groups. Non-mutant littermates served as controls. Dox (MedChemExpress, Monmouth Junction, NJ, USA, HY-N0565B) induction was initialed at 6 weeks of age for all experimental and control mice. Given the differences in genetic constructs, the Dox dosage was not standardized across models. For FD mice, the dosage was adopted based on prior experience. For PKA and FD-PKI4A mice, Dox dose optimization studies were performed to determine the lowest effective dose that produced stable and reproducible FD-like lesions. FD-PKI mice followed the same dosing strategy as FD-PKI4A mice. Dox was provided in the drinking water at concentrations of 0.1 g/L for PKA mice, 0.006 g/L for FD-PKI4A and FD-PKI mice, and 0.2 g/L for FD mice, and was maintained for up to 2 weeks. As PKI mice did not develop pronounced bone lesions under the above induction conditions, a Dox dose optimization study was conducted to evaluate whether prolonged and high-dose PKA inhibition would lead to additional skeletal effects. The final analysis reported in this study was based on the highest dosage and longest duration: 6 g/kg in diet for up to 6 months.
Two small-molecule PKA inhibitors were used in the FD mice rescue study and were administered via intraperitoneal injection every 2 days: H89 (MedChemExpress, Monmouth Junction, NJ, HY-15979A) at a dose of 50 mg/kg and Rp-8-Br-cAMPs (MedChemExpress, Monmouth Junction, NJ, HY-100530D) at a dose of 100 mg/kg. The animal experiments were conducted in accordance with protocols approved by the Sichuan University Institutional Animal Care and Use Committee (IACUC) and complied with the Guide for the Care and Use of Laboratory Animals and the Animal Research: Reporting of In Vivo Experiments (ARRIVE) guidelines. The mice were housed in specific pathogen-free (SPF) barrier facilities at the Laboratory Animal Center of West China Second University Hospital, Sichuan University. Mice were housed under controlled temperature and humidity conditions, maintained on a 12-hour light/dark cycle, with free access to water and standard laboratory chow (XiaoHe Tech, Jiangsu, China, 1002). Mice were euthanized by inhalation of an overdose of isoflurane, followed by cervical dislocation to ensure death, in accordance with Sichuan University IACUC guidelines. The use of live animals was approved by the Ethics Committee of West China Hospital of Stomatology (WCHSIRB-D-2019-197).
MC3T3-E1 subclone 14 cell lines and osteogenic induction
The MC3T3-E1 subclone 14 cell line was obtained from SAIOS Biotechnology Co., Ltd. (Wuhan, China, CL-077 m). The cells were cultured in complete alpha-MEM supplemented with 90% alpha-MEM (Gibco, Waltham, MA, USA, #12571063) and 10% FBS (Gibco, Waltham, MA, USA, #10099141C) at 5% CO2 and 37 °C. For osteogenic differentiation, the cells were seeded into 24-well plates at a density of 3 × 104 cells/well and cultured in osteogenic (OS) induction medium. The OS medium comprised complete alpha-MEM supplemented with 150 μM ascorbic acid (MilliporeSigma, Burlington, MA, USA, A4403), 10 mM β-glycerophosphate (MilliporeSigma, Burlington, MA, USA, G9422), and 10 nM dexamethasone (MilliporeSigma, Burlington, MA, USA, D4902). Forskolin (MilliporeSigma, Burlington, MA, USA, F6886) was used at a concentration of 10 μM in combination with IBMX (MilliporeSigma, Burlington, MA, USA, I7018) at 100 μM in OS medium (FI medium). H89 (MedChemExpress, Monmouth Junction, NJ, USA, HY-15979A) was used at a concentration of 10 μM in OS medium (H89 medium).
Alkaline phosphatase (ALP) staining and quantitative analysis
ALP staining was conducted after 5 days of osteogenic induction. The MC3T3-E1 cells were rinsed with PBS and fixed with 4% formaldehyde (Biosharp, Anhui, China, BL539A) for 30 min at room temperature, washed with PBS, and subjected to alkaline phosphatase (ALP) staining using the NBT/BCIP substrate solution (Beyotime, Shanghai, China, C3250S) according to the manufacturer’s instructions. Following staining, cells were rinsed with PBS and air-dried. Images were captured via a stereomicroscope (Leica, Wetzlar, Germany, EZ4 HD). For quantitative analysis, images were converted to 8-bit grayscale in ImageJ software (NIH, USA, v1.54 g), and background correction was uniformly applied to all images using a rolling ball radius of 50. The integrated density of the stained area was then measured for quantification.
Alizarin red staining (ARS) and quantitative analysis
ARS was conducted after 14 days of osteogenic induction. The MC3T3-E1 cells were rinsed with PBS and fixed in 4% formaldehyde for 30 min at room temperature. After being washed with PBS three times, the cells were stained with freshly prepared ARS solution (Beyotime, Shanghai, China, C0148S) for 15 min and then washed at least five times with distilled water until the rinsing fluid was clear. Images were captured via a stereomicroscope (Leica, Wetzlar, Germany, EZ4 HD), and quantitative analysis was performed with ImageJ software (NIH, USA, v1.54 g)64, with a consistent HSB threshold (hue: 0–30, saturation: 160–222, brightness: 174–255).
293T cell lines and transfection
The 293T cell line was obtained from ATCC and cultured in complete DMEM supplemented with 90% DMEM (Gibco, Waltham, MA, USA, #C11995500BT) and 10% FBS. The cells were seeded into 24-well plates at a density of 2.5 × 104 cells per well and transfected with Lipofectamine 3000 (Invitrogen, Waltham, MA, USA, L3000001) following the manufacturer’s instructions. At 48 h posttransfection, the cells were harvested. Intracellular total-CREB and phospho-CREB levels were measured via the Total CREB ELISA Kit (Cell Signaling Technology, Danvers, MA, USA, #36001C) and Phospho-CREB (Ser133) Sandwich ELISA Kit (Cell Signaling Technology, Danvers, MA, USA, #7385), respectively, according to the manufacturers’ instructions.
Luciferase assay
A cAMP-responsive-element–driven reporter luciferase (CRE-luc) assay was employed to measure PKA activity65. 293T cells in 24-well plates were co-transfected with CRE (0.05 μg cm−2) plus the DNA constructs indicated in the Fig. 1A: PKAcα (0.1 μg cm−2), and PKAcαW197R (0.1 μg cm−2). The cells were harvested 24 h after transfection, and the luciferase activity was subsequently measured via a Dual-Glo Luciferase Assay Kit (Promega, Madison, WI, USA, E2920) and a microtiter plate luminometer (Thermo Fisher Scientific, Waltham, MA, US). Luciferase normalization was performed in every case by co-transfecting a Renilla luciferase vector (0.005 μg cm−2; Promega).
Tissue collection and processing
Fresh whole limb bones ground into shatters via a tissue homogenizer (Servicebio, Wuhan, China, #KZ-5F-3D) in TRIzol reagent (Invitrogen, Carlsbad, CA, USA, #15596–026) or in freshly prepared RIPA lysis buffer immediately after collection. The RIPA lysis buffer was supplemented with 100X protease inhibitor cocktail (Bimake, Texas, USA, #b14001) and 100X phosphatase inhibitor cocktail (KeyGEN BioTECH, Jiangsu, China, KGB5101-2). The resulting mixture was frozen at –80 °C for subsequent RNA isolation or protein extraction.
Limb bone and skull samples intended for histological analysis and biomechanical testing were collected and fixed in zinc 10% formalin fixative (MilliporeSigma, Burlington, MA, USA, #Z2902) at room temperature overnight and then stored in 70% ethanol for further processing. Fixed limb bone samples were either decalcified in 4% buffered EDTA for subsequent paraffin and optimal cutting temperature (OCT) frozen embedding or directly embedded in polymethyl methacrylate (PMMA) without decalcification. Fixed skull samples were decalcified in 4% buffered EDTA for subsequent paraffin.
Heart, liver, spleen, lung, kidney, and stomach samples intended for histopathological analysis were collected and fixed in 4% formaldehyde at room temperature overnight. Duodenum and colon samples were collected and fixed in Carnoy’s fixative (Servicebio, Wuhan, China, G1120) under the same conditions. All tissues were then processed for paraffin embedding.
RNA isolation and quantitative real-time polymerase chain reaction (qPCR)
RNA was isolated from whole limb bone tissue using TRIzol reagent (Invitrogen, Carlsbad, CA, USA, #15596–026) and from cell lines using the Cell Total RNA Isolation Kit (Foregene, Chengdu, China, RE-03111) following the manufacturer’s instructions. Reverse transcription was conducted with the PrimeScript RT Reagent Kit (Takara Bio, Kusatsu, Japan, #RR037A) on an S1000 Thermal Cycler Platform (BIO–RAD, Irvine, CA, USA). Subsequent quantitative PCR (qPCR) was performed using SYBR Select Master Mix (Applied Biosystems, Waltham, MA, USA, #44729080) on a QuanStudio 3 Real-time PCR system (Thermo Fisher Scientific, Waltham, MA, USA). The target gene expression levels were normalized to Gapdh. The oligonucleotides used for amplification were as follows: (gene, forward sequence 5’ → 3’, reverse sequence 5’ → 3’): Gapdh 5’-TCATTGACCTCAACTACATG-3’, 5’-TCGCTCCTGGAAGATGGTGAT-3’; Gnas 5’-GCAGAAGGACAAGCAGGTCT-3’, 5’-CCCTCTCCGTTAAACCCATT-3’; PRKACA 5’-GCGTGTGAAAGGCCGTACT-3’, 5’-GGATAGGCTGGTCAGCGAAG-3’, PKI 5’-AACGAGAAGCGCGATCACATG-3’, 5’-TGCATTTCTTCTACCTGTTCTTCCTG-3’, Csflr 5’-TGGATGCCTGTGAATGGCTCTG-3’, 5’-GTGGGTGTCATTCCAAACCTGC-3’; Rank 5’-GGACAACGGAATCAGATGTGGTC-3’, 5’-CCACAGAGATGAAGAGGAGCAG-3’; Nfatc1 5’-GGTGCCTTTTGCGAGCAGTATC-3’, 5’-CGTATGGACCAGAATGTGACGG-3’; Acp5 5’-GCGACCATTGTTAGCCACATACG-3’, 5’-CGTTGATGTCGCACAGAGGGAT-3’; Rankl 5’-CACAGCGCTTCTCAGGAGCTC-3’, 5’-GAGATCTTGGCCCAGCCTCGA-3’; Opg 5’-AGTCCGTGAAGCAGGAGTGCA-3’, 5’-AAGTCTCACCTGAGAAGAACC-3’; Runx2 5’-GACTGTGGTTACCGTCATGGC-3’, 5’-ACTTGGTTTTTCATAACAGCGGA-3’; Osx 5’-ATGGCGTCCTCTCTGCTTG-3’, 5’-TGAAAGGTCAGCGTATGGCTT-3’; Alpl 5’-CACGGCCATCCTATATGGTAA-3’, 5’-GGGCCTGGTAGTTGTTGTGA-3’; Col1a1 5’-CACCCTCAAGAGCCTGAGTC-3’, 5’-GTT CGGGCTGATGTACCAGT-3’; Ocn 5’-ACCCTGGCTGCGCTCTGTCTCT-3’, 5’-GATGCGTTTGTAGGCGGTCTTCA-3’.
Protein extraction and immunoblot analysis
Total protein was extracted from whole limb bone tissue and cell lines using the freshly prepared RIPA lysis buffer (Beyotime, Shanghai, China, P0013B) according to the manufacturer’s instructions. Protein concentrations were measured using a BCA Protein Assay Kit (CWBio, Jiangsu, China, CW0014S). Western blot assays were performed and repeated at least three times. Chemiluminescent signals were captured using an Amersham Imager 600 system (GE Healthcare, Chicago, USA). The antibodies used were as follows: GAPDH (1:4000, Cell Signaling Technology, Danvers, MA, USA, #2118; exposure time: 2.6 s), CREB (1:1000, Cell Signaling Technology, Danvers, MA, USA, #9197; 70.5 s), phospho-CREB Ser133 (1:1000, Cell Signaling Technology, Danvers, MA, USA, #9198; 54.2 s), HA-tag (1:100, Santa Cruz Biotechnology, Dallas, TX, USA, #sc-805; 139.2 s), and phospho-PKA substrate (RRXS*/T*) (1:1000, Cell Signaling Technology, Danvers, MA, USA, #9624; 42.5 s). PKA-phosphorylated substrates ranging from ~20 kDa to 200 kDa according to the manufacturer’s reference data. The uncropped and unprocessed scans of the most important blots in the Source Data file.
Serum collection and measurements
Mouse blood (>1 ml) was collected via retro-orbital eye collection prior to euthanasia. The blood was stored at room temperature for 30 min. Subsequently, the serum was separated via centrifugation (30 min, 5000 × g, 4 °C) and frozen at –80 °C for future analysis. Serum levels of cAMP, TRACP-5b, and Rankl were quantified via enzyme-linked immunosorbent assay (ELISA). The ELISA kits used were the Mouse Cyclic Adenosine Monophosphate (cAMP) ELISA Kit (Jianglai Industry Co., Shanghai, China, JL13362), the Mouse Tartrate-Resistant Acid Phosphatase 5b (TRACP-5b) ELISA Kit (US Biological, Salem, MA, USA, 359452), and the Mouse TRANCE (TNFSF11) ELISA Kit (RayBiotech, Norcross, GA, USA, O35235).
Assessment of FD-like limb symptoms
Limb swelling and reduced locomotor activity were assessed as indicators of “FD-like symptoms” in Dox-induced mice. Mice were monitored daily throughout the induction period. Limb swelling was evaluated by visual inspection of the hind limbs and compared to littermate controls. Locomotor activity was quantified using the Animal behavior analyses system (XinRuan Technology, Shanghai, China). Mice exhibiting both swelling and reduced mobility were classified as symptomatic. Animals that showed neither symptom were recorded as “limb-symptoms-free.”
Animal behavior analyses
Animal behavior analyses were conducted using an apparatus (XinRuan Technology, Shanghai, China) consisting of an acrylic test box (internal measurements: 50 cm × 50 cm × 45 cm) equipped with a top-mounted camera (Canon, Tokyo, Japan, S95). Each 300-second test was started immediately after the animals were transported to the test box, given that the novelty aspect of the environment is a crucial component of the test. Video was recorded at 23.98 frames per second, and behavioral parameters— including total distance traveled, average speed, walking periods, and number of standing times—were quantified using VisuTrack software (XinRuan Technology, Shanghai, China, XR-VT, v3.0). Standing behavior was defined as either supported or unsupported rearing, where the animal stands on its hind limbs with or without forelimb contact with the walls of the test box.
Microcomputed tomography (μCT)
The hindlimb specimens were scanned using a SCANCO Medical AG VivaCT 80 scanner (SCANCO Medical, Brüttisellen, Switzerland) with an isotropic voxel size of 10 μm, while skull specimens were scanned using a SCANCO Medical μCT 100 scanner (SCANCO Medical, Brüttisellen, Switzerland) with an isotropic voxel size of 7.5 μm. The acquired tomographic images were reconstructed and analyzed using the SCANCO Medical μCT Evaluation Program (SCANCO Medical, Brüttisellen, Switzerland, v6.1). A global lower threshold of 220 was applied for 3D image reconstruction. Histomorphometric analyses were performed on regions of interest (ROIs) within the tibia, as illustrated in Supplementary Fig. 2d (applied to PKA, FD-PKI4A, FD-PKI and PKI mice), Supplementary Fig. 8f (applied to PKI mice), and Supplementary Fig. 11c (applied to FD mice), to quantify parameters including bone volume fraction (BV/TV), bone mineral density (BMD), tissue mineral density (TMD), trabecular number (Tb.N), trabecular thickness (Tb.Th) and trabecular separation (Tb.Sp), following standard guidelines66.
To further analyze bone length, marrow space (Ma.Sp), cross-sectional marrow area (Ma.Ar), and endocortical and periosteal perimeter (Ec.Pm/Ps.Pm), cross-sectional ROIs were defined as illustrated in Supplementary Fig. 2e and Supplementary Fig. 11e. Image segmentation and quantitative assessments were conducted using Materialise Mimics software (Materialise NV, Leuven, Belgium, V21.0.0.406). Threshold values were set from –1024 to 800 Hounsfield units (HU) for the segmentation of the marrow cavity, and from 1000 to 8000 HU for bone tissue.
Hematoxylin and eosin (H&E) staining and quantification
Following deparaffinization and rehydration, the paraffin sections were stained with hematoxylin (Biosharp, Anhui, China, BL702B), rinsed in running tap water, differentiated in acid alcohol, and counterstained with eosin (Biosharp, Anhui, China, BL700B). After dehydration and clearing, the sections were mounted with neutral resin and scanned using a brightfield slide scanner (Leica, Wetzlar, Germany; Aperio VERSA). Representative images of tibias were taken from defined ROIs shown in Supplementary Fig. 2d (applied to PKA, FD-PKI4A and FD-PKI mice), Supplementary Fig. 11c (applied to FD mice). For PKI mice, representative images of tibias were acquired from regions approximately 1 mm distal to the tibial growth plate. Representative images of skulls were taken from a region approximately 2 mm posterior to the midline cranial suture.
For quantification of fat cells, images were acquired at 400× magnification from regions approximately 1 mm distal to the tibial growth plate. Quantitative analysis was performed using ImageJ software (NIH, USA, v1.54 g) with standardized settings for brightness (215–250), threshold (215–255), and particle size (200–3000 μm²). For quantification of multinucleated giant cells, images were captured at 200× magnification within the defined ROI as illustrated in Supplementary Fig. 2d. Quantification was performed using Aipathwell software (Servicebio, Wuhan, China, v2.0). For quantification of the area of FD lesions, images were captured at 100× magnification within the defined ROI as illustrated in Supplementary Fig. 11c. Lesion boundaries were visually determined based on cortical integrity and the disruption by fibrous tissue, which are readily distinguishable under H&E staining. Quantification was performed using ImageJ software (NIH, USA, v1.54 g), and the lesion area was expressed as a percentage of the total bone area.
Tartrate-resistant acid phosphatase (TRAP) staining
The paraffin sections were incubated at 37 °C in freshly prepared TRAP staining solution for 15 min, with periodic monitoring. Following staining, the sections were washed in distilled water, counterstained with methyl green (Wako, Richmond, VA, USA, #184-67001), dehydrated in graded alcohol, and mounted with Permount mounting medium (Biosharp, Anhui, China, BL704A). The TRAP staining solution was composed of 0.02% naphthol AS-TR phosphate (MilliporeSigma, Burlington, MA, USA, #N6125-1G) and 0.03% Fast Red violet LB salt (MilliporeSigma, Burlington, MA, USA, #F3381-5G) dissolved in 0.1 M sodium acetate buffer (pH 5), containing 50 mM sodium tartrate (MilliporeSigma, Burlington, MA, USA, #S4797-100G) and 0.1 M sodium acetate (MilliporeSigma, Burlington, MA, USA, #S1111500GM). Representative images were taken from defined ROIs shown in Supplementary Fig. 2d (applied to PKA, FD-PKI4A and FD-PKI mice), Supplementary Fig. 11c (applied to FD mice). For PKI mice, representative images were acquired at the level of the tibial growth plate.
Sirius red staining
Following deparaffinization and rehydration, the paraffin sections were stained with Picro-Sirius Red solution for 1 h. The Picrosirius Red solution consisted of 0.1% (wt/vol) Direct Red 80 (MilliporeSigma, Burlington, MA, USA, #2610-10-8) in a saturated aqueous picric acid solution. After two washes in 0.5% acetic acid water, the sections were dehydrated in graded alcohol and mounted with Permount mounting medium (Biosharp, Anhui, China, BL704A). The evaluation was conducted under transmitted and polarized light microscopy (Nikon, Tokyo, Japan, Eclipse Ci-Pol). Images were taken from defined ROIs shown in Supplementary Fig. 2d.
Immunohistochemistry
Paraffin sections were deparaffinized and rehydrated through xylene and a graded alcohol series, followed by microwave antigen retrieval. Endogenous peroxidase activity was blocked with 3% hydrogen peroxide. The sections were then blocked with 10% goat serum (Boster Biological Technology, Wuhan, China, AR1009) for 1 h and incubated with primary antibodies overnight at 4 °C. Detection was performed with the avidin-biotin complex (ABC) and DAB systems using the VECTASTAIN ABC-HRP Kit (Vector Laboratories, Newark, CA, USA, PK-6101) and the DAB Detection Kit (GeneTech, Shanghai, China, GK600510). The sections were subsequently counterstained with hematoxylin. The slides were scanned using a brightfield slide scanner (Leica, Wetzlar, Germany; Aperio VERSA). Each immunostaining was performed in at least three mice, with multiple fields reviewed. The antibodies used in this study included anti-Sp7/osterix (Osx) (1:500, Abcam, Cambridge, MA, USA, ab22552) and anti-osteocalcin (Ocn) (1:200, Abcam, Cambridge, MA, USA, ab93876). Representative images were acquired from regions approximately 0.5 mm distal to the tibial growth plate. For further quantification of positively stained cells, images were captured at 400× magnification within the defined ROI. Three fields were selected per sample, and the mean value was used for analysis. Quantification was performed using Aipathwell software (Servicebio, Wuhan, China, v2.0).
Immunofluorescence
OCT-embedded frozen sections were blocked and incubated with primary EGFP-tag antibody (1:200, Proteintech, Rosemont, IL, USA, 50430-2-AP) overnight at 4 °C. The sections were subsequently incubated with anti-rabbit IgG (H + L) cross-adsorbed secondary antibody (Thermo Fisher Scientific, Waltham, MA, USA, Alexa Fluor 546), followed by nuclear counterstaining and mounting with mounting medium containing DAPI (Vector Laboratories, Newark, CA, USA, H-1200-10). Each immunostaining was performed in at least three mice, with multiple fields reviewed. Representative images were acquired from regions approximately 0.5 mm distal to the tibial growth plate. Images were captured using an A1 HD25 confocal microscope (Nikon, Tokyo, Japan).
Von Kossa (VK) staining
Following embedding in PMMA without decalcification, the hindlimb bone tissues were sectioning, deplasticized, and rehydrated. The VK staining was performed according to the manufacturer’s instructions for the Von Kossa (Calcium Stain) Kit (Solarbio, Beijing, China, G3282). Briefly, sections were incubated in 5% silver nitrate solution under ultraviolet light for 30 minutes, rinsed with distilled water, and treated with 5% sodium thiosulfate for 5 minutes to remove unreacted silver. After counterstaining with nuclear fast red, sections were dehydrated, cleared, and mounted for imaging. Representative images were taken from defined ROIs shown in Supplementary Fig. 2d.
EdU proliferation assay
Briefly, 100 μL of 10 mM EdU (Thermo Fisher Scientific, Waltham, MA, USA, A10044) per 10 g of mouse body weight was administered 3 h prior to euthanasia. The hindlimb bone tissues were then collected, decalcified, and processed for paraffin embedding and sectioning. Click staining and subsequent immunofluorescence staining were performed according to the manufacturer’s instructions for the Click-it EdU Alexa Fluor 555 Imaging Kit (Thermo Fisher Scientific, Waltham, MA, USA, C10338). Images were captured using a confocal microscope (Nikon, Tokyo, Japan, A1 HD25), and representative images were acquired from regions approximately 0.5 mm distal to the tibial growth plate. For quantitative analysis, images were captured at 400× magnification within the defined ROI, and analyzed using ImageJ software (NIH, USA, v1.54 g)64, with a consistent threshold (65–225).
Biomechanical testing
Considering the physiological loading direction of the hindlimb, compression testing was employed67. The mechanical testing was conducted using an Instron 5565 system (Norwood, MA, USA). Prior to testing, all soft tissues were carefully removed from the tibias, which were then fixed onto the adapter to receive axial compression at a rate of 1 mm/min until the specimens fractured. Parameters recorded included the load–displacement curve, maximum load, and elastic modulus.
Statistical analysis
All the data were analyzed using GraphPad Prism software (San Diego, CA, USA, v9.5.1). Significance was determined by the P value. One-way ANOVA, two-way ANOVA, and t tests were performed as appropriate to analyze significant differences among groups. A P value less than 0.05 was considered statistically significant. All the statistical tests were two-tailed. The data are presented as box-and-whisker plots, with boxes representing the interquartile range (25th–75th percentiles), the minimum and maximum values reached by bars, the median plotted as a line in the middle, and the mean marked as “+”.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
All the data supporting the findings of this study are available within the article, supplementary information files, and source data file. Source data is available for Figs. 1a–c, e, f, 2c, g, 3a, b, d–f, 4b–d, f, h, 5c, e, j, i, n, 6b, c, e, i–k, 7b, d and f, and Supplementary Figs. 1a–h, 2b, c, 2f, 4a, b, 7a–d, 8a–e, 8g, 9a, 9d, e, 11a, b, 11d, 11f and 12b–d. Source data are provided with this paper.
References
Boyce, A. M. & Collins, M. T. Fibrous dysplasia/McCune-Albright syndrome: a rare, mosaic disease of Galphas activation. Endocrine Rev. 41, 345–370 (2020).
Weinstein, L. S. et al. Activating mutations of the stimulatory G protein in the McCune-Albright syndrome. N. Engl. J. Med. 325, 1688–1695 (1991).
Zhao, X. et al. Expression of an active Galphas mutant in skeletal stem cells is sufficient and necessary for fibrous dysplasia initiation and maintenance. Proc. Natl Acad. Sci. USA 115, E428–E437 (2018).
Javaid, M. K. et al. Best practice management guidelines for fibrous dysplasia/McCune-Albright syndrome: a consensus statement from the FD/MAS international consortium. Orphanet J. Rare Dis. 14, 139 (2019).
Boyce, A. M. et al. A randomized, double blind, placebo-controlled trial of alendronate treatment for fibrous dysplasia of bone. J. Clin. Endocrinol. Metab. 99, 4133–4140 (2014).
Corsi, A. et al. Zoledronic acid in a mouse model of human fibrous dysplasia: ineffectiveness on tissue pathology, formation of “giant osteoclasts” and pathogenetic implications. Calcif Tissue Int. 107, 603–610 (2020).
Trojani, M. C. et al. Denosumab use in bone fibrous dysplasia refractory to bisphosphonate: a retrospective multicentric study. Bone 174, 116819 (2023).
de Castro, L. F. et al. Safety and efficacy of denosumab for fibrous dysplasia of bone. N. Engl. J. Med. 388, 766–768 (2023).
Liu, Z. et al. RANKL inhibition halts lesion progression and promotes bone remineralization in mice with fibrous dysplasia. Bone, 156, 116301 (2021).
Meier, M. E. et al. Safety of therapy with and withdrawal from denosumab in fibrous dysplasia and McCune-Albright syndrome: an observational study. J. Bone Min. Res. 36, 1729–1738 (2021).
Ramms, D. J. et al. Galphas-protein kinase A (PKA) pathway signalopathies: the emerging genetic landscape and therapeutic potential of human diseases driven by aberrant Galphas-PKA signaling. Pharm. Rev. 73, 155–197 (2021).
Taylor, S. S., Ilouz, R., Zhang, P. & Kornev, A. P. Assembly of allosteric macromolecular switches: lessons from PKA. Nat. Rev. Mol. Cell Biol. 13, 646–658 (2012).
Orellana, S. A. & McKnight, G. S. Mutations in the catalytic subunit of cAMP-dependent protein kinase result in unregulated biological activity. Proc. Natl Acad. Sci. USA 89, 4726–4730 (1992).
Gibson, R. M. & Taylor, S. S. Dissecting the cooperative reassociation of the regulatory and catalytic subunits of cAMP-dependent protein kinase. Role of Trp-196 in the catalytic subunit. J. Biol. Chem. 272, 31998–32005 (1997).
Ronchi, C. L. et al. Genetic landscape of sporadic unilateral adrenocortical adenomas without PRKACA p.Leu206Arg mutation. J. Clin. Endocrinol. Metab. 101, 3526–3538 (2016).
Liu, C., Ke, P., Zhang, J., Zhang, X. & Chen, X. Protein kinase inhibitor peptide as a tool to specifically inhibit protein kinase A. Front Physiol. 11, 574030 (2020).
Siddappa, R. et al. cAMP/PKA pathway activation in human mesenchymal stem cells in vitro results in robust bone formation in vivo. Proc. Natl Acad. Sci. USA 105, 7281–7286 (2008).
Lo, K. W., Kan, H. M., Ashe, K. M. & Laurencin, C. T. The small molecule PKA-specific cyclic AMP analogue as an inducer of osteoblast-like cells differentiation and mineralization. J. Tissue Eng. Regen. Med. 6, 40–48 (2012).
Kao, R. S. et al. Constitutive protein kinase A activity in osteocytes and late osteoblasts produces an anabolic effect on bone. Bone 55, 277–287 (2013).
Tascau, L. et al. Activation of protein kinase A in mature osteoblasts promotes a major bone anabolic response. Endocrinology 157, 112–126 (2016).
Zhao, Y. & Ding, S. A high-throughput siRNA library screen identifies osteogenic suppressors in human mesenchymal stem cells. Proc. Natl Acad. Sci. USA 104, 9673–9678 (2007).
Yang, D. C. et al. cAMP/PKA regulates osteogenesis, adipogenesis and ratio of RANKL/OPG mRNA expression in mesenchymal stem cells by suppressing leptin. PloS one 3, e1540 (2008).
Siddappa, R. et al. cAMP/PKA signaling inhibits osteogenic differentiation and bone formation in rodent models. Tissue Eng. Part A 15, 2135–2143 (2009).
Zhang, S., Kaplan, F. S. & Shore, E. M. Different roles of GNAS and cAMP signaling during early and late stages of osteogenic differentiation. Horm. Metab. Res.44, 724–731 (2012).
Kao, R., Lu, W., Louie, A. & Nissenson, R. Cyclic AMP signaling in bone marrow stromal cells has reciprocal effects on the ability of mesenchymal stem cells to differentiate into mature osteoblasts versus mature adipocytes. Endocrine 42, 622–636 (2012).
Kondo, H., Guo, J. & Bringhurst, F. R. Cyclic adenosine monophosphate/protein kinase A mediates parathyroid hormone/parathyroid hormone-related protein receptor regulation of osteoclastogenesis and expression of RANKL and osteoprotegerin mRNAs by marrow stromal cells. J. Bone Miner. Res. 17, 1667–1679 (2002).
Tseng, W. et al. PKA-induced receptor activator of NF-kappaB ligand (RANKL) expression in vascular cells mediates osteoclastogenesis but not matrix calcification. J. Biol. Chem. 285, 29925–29931 (2010).
Yoon, S. H., Ryu, J., Lee, Y., Lee, Z. H. & Kim, H. H. Adenylate cyclase and calmodulin-dependent kinase have opposite effects on osteoclastogenesis by regulating the PKA-NFATc1 pathway. J. Bone Miner. Res. 26, 1217–1229 (2011).
Ramaswamy, G. et al. Gsalpha controls cortical bone quality by regulating osteoclast differentiation via cAMP/PKA and beta-catenin pathways. Sci. Rep. 7, 45140 (2017).
Ramaswamy, G. et al. Ablation of Gsalpha signaling in osteoclast progenitor cells adversely affects skeletal bone maintenance. Bone 109, 86–90 (2018).
Chijiwa, T. et al. Inhibition of forskolin-induced neurite outgrowth and protein phosphorylation by a newly synthesized selective inhibitor of cyclic AMP-dependent protein kinase, N-[2-(p-bromocinnamylamino)ethyl]-5-isoquinolinesulfonamide (H-89), of PC12D pheochromocytoma cells. J. Biol. Chem. 265, 5267–5272 (1990).
Gjertsen, B. T. et al. Novel (Rp)-cAMPS analogs as tools for inhibition of cAMP-kinase in cell culture. Basal cAMP-kinase activity modulates interleukin-1 beta action. J. Biol. Chem. 270, 20599–20607 (1995).
Knighton, D. R. et al. Structure of a peptide inhibitor bound to the catalytic subunit of cyclic adenosine monophosphate-dependent protein kinase. Science 253, 414–420 (1991).
Iglesias-Bartolome, R. et al. Inactivation of a Galpha(s)-PKA tumour suppressor pathway in skin stem cells initiates basal-cell carcinogenesis. Nat. Cell Biol. 17, 793–803 (2015).
Yu, F. X. et al. Protein kinase A activates the Hippo pathway to modulate cell proliferation and differentiation. Genes Dev. 27, 1223–1232 (2013).
Sinha, P. et al. Loss of Gsalpha early in the osteoblast lineage favors adipogenic differentiation of mesenchymal progenitors and committed osteoblast precursors. J. Bone Miner. Res. 29, 2414–2426 (2014).
Bathon, K. et al. Alterations in protein kinase A substrate specificity as a potential cause of cushing syndrome. Endocrinology 160, 447–459 (2019).
Tsang, K. M. et al. Alternate protein kinase A activity identifies a unique population of stromal cells in adult bone. Proc. Natl Acad. Sci. USA 107, 8683–8688 (2010).
Belteki, G. et al. Conditional and inducible transgene expression in mice through the combinatorial use of Cre-mediated recombination and tetracycline induction. Nucleic Acids Res. 33, e51 (2005).
Dou, Y. et al. The CAG promoter maintains high-level transgene expression in HEK293 cells. FEBS Open Bio 11, 95–104 (2021).
Murray, A. J. Pharmacological PKA inhibition: all may not be what it seems. Sci. Signal 1, re4 (2008).
Christensen, A. E. et al. cAMP analog mapping of Epac1 and cAMP kinase. Discriminating analogs demonstrate that Epac and cAMP kinase act synergistically to promote PC-12 cell neurite extension. J. Biol. Chem. 278, 35394–35402 (2003).
Parnell, E., Palmer, T. M. & Yarwood, S. J. The future of EPAC-targeted therapies: agonism versus antagonism. Trends Pharm. Sci. 36, 203–214 (2015).
Bos, J. L. Epac proteins: multi-purpose cAMP targets. Trends Biochem Sci. 31, 680–686 (2006).
Hoy, J. J., Salinas Parra, N., Park, J., Kuhn, S. & Iglesias-Bartolome, R. Protein kinase A inhibitor proteins (PKIs) divert GPCR-Galphas-cAMP signaling toward EPAC and ERK activation and are involved in tumor growth. FASEB J. 34, 13900–13917 (2020).
Regard, J. B. et al. Activation of Hedgehog signaling by loss of GNAS causes heterotopic ossification. Nat. Med. 19, 1505–1512 (2013).
Yang, W. et al. GNAS locus: bone related diseases and mouse models. Front. Endocrinol. 14, 1255864 (2023).
Shore, E. M. et al. Paternally inherited inactivating mutations of the GNAS1 gene in progressive osseous heteroplasia. N. Engl. J. Med. 346, 99–106 (2002).
Sakamoto, A. et al. Deficiency of the G-protein alpha-subunit G(s)alpha in osteoblasts leads to differential effects on trabecular and cortical bone. J. Biol. Chem. 280, 21369–21375 (2005).
Fulzele, K. et al. Loss of Gsalpha in osteocytes leads to osteopenia due to sclerostin induced suppression of osteoblast activity. Bone 117, 138–148 (2018).
Zhang, L. et al. Overexpression of Galpha(S) in Murine Osteoblasts In Vivo Leads to Increased Bone Mass and Decreased Bone Quality. J. Bone Miner. Res.32, 2171–2181 (2017).
Piersanti, S. et al. Transfer, analysis, and reversion of the fibrous dysplasia cellular phenotype in human skeletal progenitors. J. Bone Miner. Res.25, 1103–1116 (2010).
Wu, J. Y. et al. Gsalpha enhances commitment of mesenchymal progenitors to the osteoblast lineage but restrains osteoblast differentiation in mice. J. Clin. Investig. 121, 3492–3504 (2011).
Hsiao, E. C., Boudignon, B. M., Halloran, B. P., Nissenson, R. A. & Conklin, B. R. Gs G protein-coupled receptor signaling in osteoblasts elicits age-dependent effects on bone formation. J. Bone Miner. Res.25, 584–593 (2010).
McMullan, P., Maye, P., Yang, Q., Rowe, D. W. & Germain-Lee, E. L. Parental origin of Gsalpha inactivation differentially affects bone remodeling in a mouse model of albright hereditary osteodystrophy. JBMR6, e10570 (2022).
Basha, G. et al. Lipid nanoparticle-mediated silencing of osteogenic suppressor GNAS leads to osteogenic differentiation of mesenchymal stem cells in vivo. Mol. Ther. 30, 3034–3051 (2022).
Florenzano, P. et al. Age-related changes and effects of bisphosphonates on bone turnover and disease progression in fibrous dysplasia of bone. J. Bone Miner. Res.34, 653–660 (2019).
Manschwetus, J. T. et al. A stapled peptide mimic of the pseudosubstrate inhibitor PKI inhibits protein kinase A. Molecules 24, 1567 (2019).
Rinaldi, L. et al. Feedback inhibition of cAMP effector signaling by a chaperone-assisted ubiquitin system. Nat. Commun. 10, 2572 (2019).
Coles, G. L. et al. Unbiased proteomic profiling uncovers a targetable GNAS/PKA/PP2A axis in small cell lung cancer stem cells. Cancer Cell 38, 129–143 e127 (2020).
Visscher, M., Arkin, M. R. & Dansen, T. B. Covalent targeting of acquired cysteines in cancer. Curr. Opin. Chem. Biol. 30, 61–67 (2016).
Das, A. T., Tenenbaum, L. & Berkhout, B. Tet-on systems for doxycycline-inducible gene expression. Curr. Gene Ther. 16, 156–167 (2016).
Logan, M. et al. Expression of Cre Recombinase in the developing mouse limb bud driven by a Prxl enhancer. Genesis 33, 77–80 (2002).
Schneider, C. A., Rasband, W. S. & Eliceiri, K. W. NIH Image to ImageJ: 25 years of image analysis. Nat. Methods 9, 671–675 (2012).
Castellone, M. D., Teramoto, H., Williams, B. O., Druey, K. M. & Gutkind, J. S. Prostaglandin E2 promotes colon cancer cell growth through a Gs-axin-beta-catenin signaling axis. Science 310, 1504–1510 (2005).
Bouxsein, M. L. et al. Guidelines for assessment of bone microstructure in rodents using micro-computed tomography. J. Bone Miner. Res. 25, 1468–1486 (2010).
Tiefenboeck, T. M. et al. Effect of two (short-term) storage methods on load to failure testing of murine bone tissue. Sci. Rep. 9, 5961 (2019).
Acknowledgements
We thank Dr. J. Silvio Gutkind and Dr. Susan S. Taylor for generously sharing pRSET PKAcα plasmid with us. We thank Dr. Ramiro Iglesias-Bartolome and Dr. Xiaodong Feng for meaningful discussion. We thank Dr. Li Chen from Analytical & Testing Center Sichuan University for her help with micro-CT scanning and analysis. This project was supported by National Natural Science Foundation of China Grants (82170995, 82470940 to X.Z., 82371002 to D.B., 81991502 to Q.C.); National Regional Joint Key Fund project of China (U24A20712 to X.H.); National Key R&D Program of China (2022YFC2402900 to Q.C.); Sichuan Science and Technology Program, China (2024NSFSC0540 to D.B.); charitable funds from Mr. Mingxu Zhou family for fibrous dysplasia related research (Sichuan University internal grants 18H1134, 19H1134 and 23H0924 to X.Z.).
Author information
Authors and Affiliations
Contributions
X.Z. conceptualized and designed research; X.Z. and Z.L. performed research; L.X., W.H., N.J. and H.Z. provided technical support; X.Z., Z.L, Q.C., X.H. and D.B. analyzed data; X.Z. and Z.L. wrote the paper.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks Christopher Langendorf and the other anonymous reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liu, Z., Xing, L., Huang, W. et al. Protein kinase A is a dependent factor and therapeutic target in mouse models of fibrous dysplasia. Nat Commun 16, 5425 (2025). https://doi.org/10.1038/s41467-025-61402-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41467-025-61402-z