Abstract
Osteosarcoma (OS), with a high tendency for recurrence and metastasis, is associated with severe impairment of bone regeneration. The inherent temperature-sensitive property of tumors positions magnetic hyperthermia (MH) as an increasingly significant area in non-pharmacological cancer treatments. However, the temperature threshold for tumor ablation often causes tissue damage and bone homeostasis imbalance. Therefore, development of moderate MH for OS, capable of achieving tumor ablation while concurrently restoring bone homeostasis, offers significant potential for addressing this challenge. This study integrates magnetothermal nanoparticles with defined temperature thresholds and borosilicate bioactive glass (BSG) to create an injectable magnetothermal bioactive system that allows for regulation of MH temperature. The ionic and alkaline microenvironment from BSG degradation primarily impairs the malignant behavior of OS cells by activating the TNF signaling pathway. This sickening effect diminishes the hyperthermia tolerance of OS cells, thereby boosting apoptosis of OS cells, even in the presence of the limited anti-tumor effects of moderate MH. Furthermore, the combination of moderate MH and BSG also promotes optimal bone formation by stimulating human bone marrow mesenchymal stem cells (hBMSCs) via calcium and JAK-STAT3 signaling pathways. Collectively, this flourishes the therapeutic approaches and theories for the prevention and management of clinically refractory bone tumors.
Similar content being viewed by others
Introduction
Primary bone neoplasms, originating from tissues or cells within bones, represent around 0.2% of all malignancies globally1. Osteosarcoma (OS) is the most common primary bone malignancy, predominantly affecting teenagers and young adults, and constitutes roughly 56% of bone sarcomas2. The conventional management of OS consists of three standard procedures applicable to all patients: surgical excision of the tumor, subsequent bone graft implantation to preserve limb structural integrity, and neoadjuvant chemotherapy to prevent metastasis and tumor recurrence. Nevertheless, no specific technologies are available to biologically modify the microenvironment resulting from the interaction between tumor and host cells to achieve customized and exact healing for OS3,4. Despite the positive outcomes of emerging medicines for OS treatment, including targeted medication, monoclonal immunotherapy, and cell therapy, their efficacy is constrained by diminished anti-tumor activity and acute organ toxicity. In this scenario, 20−30% of OS patients still persist in experiencing recurrence and early metastases, with a survival rate of less than 5 years5,6,7. Moreover, those who survive beyond 5 years may experience altered bone homeostasis, characterized by diminished bone regeneration inhibition, leading to limb dysfunction and a deterioration in quality of life6,7. Consequently, it is essential to devise innovative and convenient strategies that can proactively prevent the recurrence and metastasis of OS, restore the osteogenic microenvironment, and reestablish the structural integrity and physiological function of bone tissue, thereby enhancing the prognosis of OS patients.
Due to concerns that systemic administration or local application of antineoplastic agents and interfering with periodic radiotherapy to prevent tumor recurrence and metastasis, potentially leading to drug resistance or systemic intolerance to radiation, researchers have increasingly concentrated on innovative cancer therapies that target the distinct physiology and microenvironment of tumors, to achieve more effective anti-tumor outcomes8. The vascular structure of solid tumors is recognized as intricate, featuring areas of hypoxia and acidic pH that render tumor cells susceptible to thermal fluctuations8. Consequently, the attainment of cancer eradication via the localized thermal effects of implanted materials, referred to as thermotherapy, has exhibited advantageous clinical operability, extensive tumor adaptability to cancerous conditions, and consistent inhibitory efficacy, thereby emerging as a prominent research focus in the domain of non-pharmacological cancer treatment9. In comparison to alternative thermotherapies, magnetic hyperthermia (MH) demonstrates varied adaptability in distinct diseased tissues and can swiftly produce localized hyperthermic effects with superior tissue penetration depth and coverage, thereby garnering increasing clinical interest10. Presently, the predominant device employed in clinical practice to induce hyperthermia through the application of an alternating magnetic field (AMF) is mostly ferrite nanoparticles, such as Fe3O411. Fe3O4 nanoparticles (Feraheme) have received FDA approval for the thermal ablation of malignancies in clinical settings, owing to their considerable saturation magnetization, anisotropic energy, and verified biosafety. Fe3O4 can experience substantial temperature increases when subjected to AMF, creating various temperature gradients that exceed the threshold necessary to eliminate the majority of tumor cells11. Nevertheless, the Curie point of Fe3O4 is considerably elevated, and the temperature threshold is challenging to regulate, frequently above 70 °C, which significantly exceeds the acceptable temperature for human tissues and is likely to induce irreversible heat damage to normal tissues12. Furthermore, the regulation of the temperature threshold for magnetothermal materials primarily depends on techniques such as temperature monitoring, circulating water cooling, and modulating the intensity of the AMF, thereby complicating clinical procedures13. Consequently, the creation of medical devices featuring effective MH and adjustable temperature thresholds can enhance tumor ablation while reducing harm to healthy tissues14. Spinel ferrite, as a self-regulating temperature material, is distinguished by its uncomplicated crystal structure, steady chemical properties, and adjustable magnetic characteristics15. The formula AB2O4 represents the composition of spinel ferrite, with metal ions occupying the A and B positions. The intensity of the superexchange interaction among these ions is crucial in establishing the Curie temperature of spinel ferrite15. The incorporation of non-magnetic elements into the lattice can effectively modulate the Curie temperature and magnetocaloric transformation temperature of spinel ferrite, thereby regulating its temperature threshold16. Thus, employing spinel ferrite offers a potential strategy for attaining temperature self-regulation in MH.
As postulated by Gregory Mundy, the bone microenvironment will create a conducive habitat for tumor cells by supplying ample growth regulatory substances during bone resorption17. Tumor cells in the local bone microenvironment tend to secrete substances, such as parathyroid hormone-related proteins, which stimulate osteoblasts to produce receptor activator of NF-κB ligand (RANKL), thereby inducing osteoclasts and commencing osteolysis. Thereby, a “vicious cycle” was formed in the bone tumor environment to induce ongoing osteolysis and bone structural destruction, which heightens the likelihood of pathological fractures17,18. Furthermore, the osteolysis process initiated by osteoclasts results in an increased release of bone matrix growth factors, which can subsequently stimulate tumor growth and further compromise bone integrity19. Consequently, optimal OS therapy necessitates not only the effective eradication of tumors and robust prevention of metastasis and recurrence but also the restoration of the structural integrity and mechanical stability of bone tissue. This underscores the critical need for the advancement of next-generation implants for bone regeneration within the tumor microenvironment. Currently, multiple techniques for defect regeneration have been established, including inactivated autologous bone reimplantation, allograft implantation20, and artificial bone graft fixation21,22, all of which have exhibited remarkable therapeutic success. Nonetheless, none of the bone defect filling technologies can adjust the disrupted osteogenic/osteoclastic equilibrium under the tumor microenvironment, much less prevent the metastasis and recurrence of OS.
Prior studies demonstrated that bioactive glasses (BGs) exhibit superior tissue regeneration capabilities and can generate an ionic and alkaline microenvironment (IAM) through the release of matrix ions upon implantation in the body23. This IAM of BGs inhibits hyperactive osteoclasts while promoting the migration, proliferation, M1/M2 polarization, and expression of osteogenesis and angiogenesis-related factors in macrophages, thereby mediating local inflammation to effectively activate mesenchymal stem cells for directed osteogenesis and angiogenesis24. Furthermore, the IAM of BGs is anticipated to significantly impede the activity and spread of tumor cells25. Prior research demonstrated that elevating the pH of the extracellular microenvironment might suppress the activation of tumor transferase and hinder the breakdown and remodeling of the extracellular matrix, hence obstructing the invasion and metastasis of tumor cells. Moreover, the in vivo application of a pure alkaline microenvironment, as created by NaHCO3, could neutralize the acidification of the tumor microenvironment and diminish the development of lymph node and liver metastases in mice with breast cancer metastasis, leading to an increased overall survival of the mice. However, the long-term pH regulation with the donor seems uncontrolled by the buffering with human body fluid, that is, the supposed high pH to kill the tumor may be balanced. Thus, the constant high pH is particularly anticipated. Here, the controlled release of alkaline ions may render a controlled alkaline condition by BGs, which seems to provide an approach to monitor the tumor microenvironment. Additionally, prior studies have indicated the considerable anti-tumor effects linked to the implantation of BGs for addressing postoperative bone deficiencies resulting from bone tumors26,27. Consequently, local administration of BGs to unitize its IAM to interfere with tumor deterioration and subsequently inducing osteogenesis presents as a feasible solution to effectively address unbalanced bone homeostasis under the OS microenvironment.
It is commonly recognized that the temperature for effective MH in tumor ablation must surpass 45 °C, while temperatures below this essential threshold will not result in observable necrosis in tumor tissue28. This temperature barrier for tumor ablation creates a conundrum of thermal harm to host tissue, hence impairing the already limited capacity for bone repair29. In this study, inspired by the military strategy of initially depleting the adversary’s power to attain superior annihilation of enemies, we hypothesize that the IAM of borosilicate bioactive glass (BSG) may initially sick the tumor cells by disrupting their normal physiological functions and metabolism in the battlefield of OS. This sickness could diminish the hyperthermia tolerance of tumors, rendering them susceptible even to the inherently minimal or weak anti-tumor effects of moderate MH. Therefore, by integrating BSG with moderate MH, the objective of reducing heat injury to host tissue while achieving effective tumor ablation and the sequential osteogenic activity under moderate MH can be highly accomplished, presenting significant potential for transforming bone tumor treatment without pharmacological intervention.
In this study, we combine BSG with magnetothermal nanoparticles (MNPs) to create injectable magnetothermal bioactive systems (IMBSs) (as depicted in Fig. 1). The MNPs are produced by incorporating non-magnetic chromium (Cr3+) and zinc (Zn2+) ions into the crystal lattice of CoFe2O4 a typical, which allowed the temperature threshold to be adjusted. CoFe2O4 is regarded as a superior magnetic ferrite material, with high magnetic anisotropy, significant coercivity, and moderate saturation magnetization30. Results show that the IMBSs include 5-MNP-BSG (5% MNP in BSG) and 10-MNP-BSG (10% MNP in BSG), which exhibit good injectability, mechanical strength, high degradability, and a stable temperature threshold. Our tests in an AMF with a current of 20 A and a constant frequency of 550 kHz reveal that the temperature threshold for the 5-MNP-BSG is 42.3 °C ± 0.2 °C, while the 10-MNP-BSG is 45.8 °C ± 0.5 °C. In vitro experiments show that 5-MNP-BSG (+) significantly suppressed the proliferation, migration, and invasion of OS cells, just like 10-MNP-BSG. RNA sequencing (RNA-seq) indicates that BSG degradation upregulates the TNF signaling pathway in OS cells, leading to TNF-induced apoptosis of OS cells after moderate MH (42.3 °C ± 0.2 °C). Furthermore, the moderate MH caused by 5-MNP-BSG has no negative effect on hBMSC viability, but instead synergistically improves osteogenic differentiation of hBMSCs by activating calcium and JAK-STAT3 signaling pathways. In vivo studies include inhibition of xenograft OS in BALB/c nude mice, tumor ablation of IMBSs in rat tibia in situ OS model, as well as femoral condyle bone defects in rats. After implanting 5-MNP-BSG and administering intermittent AMF, significant anti-OS effects and bone regeneration are seen in the aforementioned animal models. As a result, IMBSs emerge as a viable method for moderate OS hyperthermia in the context of BSG degradation, promoting the removal of remaining OS cells while also addressing bone regeneration at the tumorous bone defect. This technique provides useful insights into addressing current therapeutic difficulties related to OS recurrence, metastatic disease, and bone defect healing.
a An in situ OS model in the tibia of SD rat, subjected to moderate MH utilizing IMBSs in an AMF. b Anti-OS mechanisms through the combination of moderate MH and BSG therapy: b1 The ionic and alkaline microenvironment induced by the degradation of BSG triggers TNF signaling pathway in OS cells; b2 Moderate MH facilitates apoptosis of OS cells; and b3 the synergistic effect of moderate MH and BSG enhances tumorous bone defect repair.
Results
Fabrication and characterization of IMBSs
IMBSs (Supplementary Table 1) were constructed by bonding BSG and MNPs using an adhesive, with the preparation process of IMBSs illustrated schematically in Fig. 2a. In IMBSs, MNPs fulfill the requirement for MH, whereas BSG provides the IAM. The melted-derived BSG exhibited a characteristic irregular morphology, with particle sizes measuring less than 20 μm (Fig. 2b). Additionally, the composition of BSG was analyzed and quantified using inductively coupled plasma mass (ICP-MS) spectrometry, revealing no significant discrepancies between the actual oxide compositions (Supplementary Table 2) of BSG and the intended formulations. X-ray diffraction (XRD) patterns of BSG demonstrated its amorphous state, as evidenced by the broad diffuse peak around 30o (Supplementary Fig. 1a). Fourier transform infrared (FT-IR) spectroscopy results confirmed that boron-oxygen and silicon-oxygen serve as the primary network structure formers in BSG. This was indicated by the bending and asymmetric stretching vibrations of Si-O-Si, which correspond to broad bands in the ranges of 440-540 cm-1 and 994-1075 cm-1, respectively, as well as the stretching vibration of B-O-B in boron-oxygen tetrahedra [BO4], corresponding to approximately 1400 cm-1 (Supplementary Fig. 1b).
a Schematic diagram illustrating the preparation of producers for IMBSs, with a solid to liquid ratio of 2. b Morphology of the Borosilicate bioactive glass (BSG) particles derived from high-temperature melting (white bar = 20 μm; black bar = 5 μm). c Morphology of the magnetothermal nanoparticles (MNPs) synthesized via the hydrothermal method (blue bar = 1 μm; black bar = 200 nm). d Surface morphology of the pre-cured 5-MNP-BSG sample (white bar = 100 nm; yellow bar = 50 nm). e pH value and temperature variation of IMBS pastes during the curing process (n = 3 independent experiments). f Temperature variation of IMBS pastes during the curing process (n = 3 independent experiments). g XRD pattern of pre-cured IMBSs following 24 h of curing time. h–j FT-IR spectra of setting liquid, BSG, and IMBSs after 24 h of curing time.
The results of magnetothermal conversion and temperature thresholds of MNPs (Supplementary Fig. 2) demonstrated that, just 1 min after exposure to an AMF (20 A, 550 kHz), the MNPs with the formula of Zn0.4Co0.6Cr0.6Fe1.4O4 reached a temperature of 119.4 °C ± 0.2 °C. This temperature significantly exceeds the physiological temperature tolerance of humans, potentially causing severe thermal damage to normal tissues29. In contrast, MNPs with the composition of Zn0.54Co0.46Cr0.6Fe1.4O4 demonstrated a more gradual increase in temperature, achieving a threshold of 58.7 °C ± 0.1 °C after 5 min of exposure to AMF under identical parameters. The MNPs with the formula of Zn0.7Co0.3Cr0.6Fe1.4O4, when subjected to the same AMF, exhibited a maximum temperature of 38.5 °C ± 0.2 °C after a 7-min observation period, which is inadequate for effective tumor magnetothermal therapy (Supplementary Fig. 2). Consequently, the MNP characterized by the formula of Zn0.54Co0.46Cr0.6Fe1.4O4 was chosen to investigate the moderate MH, aiming to minimize or eliminate damage to surrounding tissue31. Electron probe X-ray microanalysis (EPMA) validated that the composition of the synthetic MNP (Zn0.54Co0.46Cr0.6Fe1.4O4) was consistent with the intended design (Supplementary Fig. 3). Transmission electron microscopy (TEM) images indicated that MNPs displayed an irregular polyhedral morphology, with particle sizes under 200 nm, and exhibited characteristics of the cubic crystal system and spinel type (Fig. 2c). The XRD results also confirmed the presence of the spinel cubic structure phase of the MNPs, with no impurities detected (Supplementary Fig. 4a). The hysteresis loop illustrates the relationship between magnetization and magnetic field strength of MNP32, and the relevant results indicated that the M/H values of the MNPs were approximately 1/3, suggesting that these MNPs possess similar magnitudes, thereby confirming their ferrimagnetic nature (Supplementary Fig. 4b). The aforementioned characterizations confirm the successful synthesis of MNPs with defined temperature thresholds for magnetothermal conversion capabilities.
The bonding glue for IMBSs utilized in this study was identical to that employed in our prior research33. The initial pH of this bonding glue was 2.1 ± 0.3 (n = 3 independent experiments), and it will undergo a sol-gel transformation when the pH value exceeds 6.5. BSG, as a biodegradable material, can simultaneously release ions such as Ca2+, Na+, K+, Mg2+, and BO33- during degradation, thus creating a localized alkaline environment33,34. When mixing the glue with BSG and MNPs, the alkaline environment generated from BSG, thus rapidly increased the local pH value (Fig. 2e) and initiated the sol-gel transformation of the bonding glue within a brief period. This process resulted in the formation of IMBSs with self-curing capabilities, occurring within 10 min (Fig. 2e). These systems are designed to fill bone cavities minimally invasively, facilitating the combination therapy of MH and BSG in the OS microenvironment. Consequently, to methodically ascertain the MH of IMBSs, IMBSs with varying ratios of MNP incorporation were synthesized, specifically 0 wt.%, 2.5 wt.%, 5 wt.%, 7.5 wt.%, 10 wt.%, 12.5 wt.%, and 15 wt.%. The exposure of IMBSs to an AMF with defined settings (15 A, 550 kHz) yielded the subsequent temperature thresholds: The 2.5 wt.% group attained 35.4 °C ± 0.7 °C, inadequate for tumor ablation28; the 5 wt.% group reached 42.3 °C ± 0.2 °C; the 7.5 wt.% group achieved 44.0 °C ± 0.4 °C; and the 10 wt.% group attained 45.8 °C ± 0.5 °C, which presents a danger of harm to both normal and aberrant tissues29. The 15 wt.% group demonstrated a temperature of around 49.2 °C ± 0.7 °C (Supplementary Fig. 5). Consequently, after a thorough evaluation of IMBSs employing tumor ablation and regeneration of tumorous bone defects, the 0 wt.% group (designated as the BSG group) was established as the negative control, the 5 wt.% group (designated as 5-MNP-BSG) was identified as the experimental group, and the 10 wt.% group (designated as 10-MNP-BSG) functioned as the positive control group to highlight the anti-tumor effects of moderate MH (42.3 °C ± 0.2 °C) in combination with BSG, thereby ensuring tumor eradication while optimizing the preservation of healthy tissue. The maximum temperature observed during the curing of the established 3 formulations of IMBSs without AMF was 31.6 °C, which is considerably lower than normal physiological temperature, indicating no detrimental effects on surrounding tissues (Fig. 2f). Post-curing, IMBSs exhibited a uniform surface morphology characterized by fine granules arranged in a three-dimensional (3D) network, as illustrated in Fig. 2d and Supplementary Fig. 6a, b. The XRD results of the pre-cured IMBSs exhibited characteristic diffraction peaks at 35°, 43°, and 63°, which correspond to the spinel phase of MNPs. Additionally, a broad diffuse peak around 30° was observed, indicating the formation of the hydroxyapatite (HA) phase during the curing of IMBSs (Fig. 2g). FT-IR spectra of the pre-cured IMBSs indicated a broad peak at 1649 cm-1, which corresponds to the vibrational peak of the primary amide group in the acetylated chitosan units, and a broad peak at 1097 cm-1, associated with the asymmetric stretching vibration of the C-O group in chitosan. The vibration peak at 700 cm-1 corresponds to the B-O stretching resonance of [BO4]. The ranges of 800-1200 cm-1 and 1200-1600 cm-1 are attributed to the B-O stretching vibration of [BO4] and the asymmetric vibration of [BO3], respectively. Additionally, an infrared vibrational peak identified within the 500-700 cm-1 range is associated with the P-O functional group in HA, indicating that the biomineralization of released Ca2+ from BSG occurs with PO43− in bonding glue during the curing process of IMBSs. What was also noteworthy that, the shifts of the amine group (approximately 1649 cm-1) and C-O asymmetric stretching (approximately 1097 cm-1) of chitosan toward lower wavenumbers, resulting from the chemical chelation between BSG and chitosan, confirm the successful synthesis of IMBSs (Fig. 2h–j).
Rheology, handling and magnetothermal properties of IMBSs
The proper rheological and handling properties are essential for the effective application of IMBSs in vivo35. In this study, the storage modulus (G’), loss modulus (G”), and tan δ (G”/G’) were measured and documented over time. The gel point time was investigated by monitoring G’, G”, and tan δ, as illustrated in Fig. 3a–c. The findings indicated that all IMBSs achieved their gel points before the commencement of the test, as evidenced by G’ consistently exceeding G” during the entire testing period. The increase in MNPs within IMBSs results in a later occurrence of the point where G’ exceeds G” for the 5-MNP-BSG and 10-MNP-BSG groups, suggesting that MNPs have extended the curing process of IMBSs. Subsequently, dynamic strain scanning tests were performed to identify the linear viscoelastic region of the IMBS samples. The results (Supplementary Fig. 7a–c) indicated that all tested samples exhibited an initial plateau where the elastic modulus exceeded the loss modulus, confirming the linear viscoelastic characteristics of IMBSs. The strain curves indicate that the linear viscoelastic regions of all tested samples are approximately 1 − 10%. The internal structures of the IMBSs paste were examined by evaluating the relationships between G’, G”, and frequency. Supplementary Fig. 7d–f demonstrates that the elastic modulus consistently exceeds the loss modulus across all frequencies, indicating that the elastic properties of IMBSs paste are always superior to the viscous properties36,37. The narrower gap between G’ and G” in the 5-MNP-BSG and 10-MNP-BSG groups compared to the BSG group suggests that the viscosity of the IMBSs paste in the former groups is lower. This phenomenon may be attributed to the MNPs impeding interactions between BSG and the chitosan liquid phase, as MNPs function solely as inert fillers in IMBSs. Subsequently, the handling properties of IMBSs, including injectability, curing time, and compressive strength, were characterized to assess their suitability for implementation in minimally invasive treatments38. Assessments of the injectability of IMBSs indicated a slight increase with the incorporation of MNPs, as evidenced by injectability values of 96.7% ± 0.2% for the BSG group, 97.8% ± 0.4% for the 5-MNP-BSG group, and 98.5% ± 0.1% for the 10-MNP-BSG group (Fig. 3d). The curing times of IMBSs were 8.3 min ± 0.5 min for the BSG group, 9.9 min ± 0.3 min for the 5-MNP-BSG group, and 10.3 min ± 0.3 min for the 10-MNP-BSG group (Fig. 3e). This data indicates that the incorporation of MNPs is associated with an increase in the curing time of the IMBSs. The compressive strength of the pre-cured IMBSs was measured at 30.9 MPa ± 0.5 MPa for the BSG group, 28.6 MPa ± 0.3 MPa for the 5-MNP-BSG group, and 26.1 MPa ± 0.5 MPa for the 10-MNP-BSG group, respectively (Fig. 3f). The tests conducted on the compressive strength of IMBSs demonstrated that all formulations are comparable to the compressive strength of human trabecular bone, underscoring their potential application in the repair of long bone diaphyseal defects39.
a–c. The storage modulus (G’), loss modulus (G”), and tan δ (G”/G’) for IMBSs pastes. d Injectability of IMBSs pastes. e Curing time of IMBSs pastes. f Compressive strength of pre-cured IMBSs as analyzed using a tensile testing machine. g Hysteresis loops of pre-cured IMBSs subjected to AMF (20 A, 550 kHz). h Thermal images of IMBSs in a 24-well plate subjected to AMF (20 A, 550 kHz). i, j Heating curves of the pre-cured 5-MNP-BSG and 10-MNP-BSG samples under varying AFM, utilizing different currents of 10 A, 15 A, 20 A, and 25 A, while maintaining a constant magnetic field frequency of 550 kHz. k Schematic diagram and temperature threshold images of IMBSs in PBS (600 μL) utilizing a co-culture approach under an AMF (20 A, 550 kHz). l Cyclic heating profiles of pre-cured IMBSs for three on/off cycles under AMF, with an output current of 20 A and a constant frequency of 550 kH. Statistical data are presented as means ± SD, n = 3 independent experiments; statistical significance was determined using the one-way ANOVA method with Tukey’s multiple comparisons tests. Statistical significance was defined as *P < 0.05, **P < 0.01, and ***P < 0.001, whereas nsP > 0.05 was deemed not statistically significant.
The primary objective of this research is to simultaneously achieve efficient inhibition of OS and promote bone regeneration. The temperature change and the corresponding threshold of IMBSs under AMF are crucial for attaining optimal MH. Despite the adequate anti-tumor efficacy of MH at elevated temperatures, the risk of irreversible damage to normal tissue when local temperatures exceed 45 °C raises significant global concerns28,29. Thereby the significance of suitable magnetic properties and thermal conversion efficiency is paramount for tumor treatment. The hysteresis loop is a closed magnetization curve that illustrates the hysteresis phenomenon in strong magnetic materials subjected to periodic variations in magnetic field strength. The standard hysteresis loop exhibits symmetry about the origin, characterized as an S-shaped loop. This loop effectively represents the relationship between magnetization intensity (M) or magnetic induction intensity (B) and magnetic field intensity (H) in magnetic materials throughout repeated magnetization processes32. Figure 3g illustrated that the hysteresis loops for the 5-MNP-BSG and 10-MNP-BSG groups exhibit a “S” shape, thereby confirming the typical ferrimagnetic characteristics of IMBSs. The increase of MNPs in IMBSs has resulted in an enhancement of their magnetic properties. Furthermore, the pre-cured IMBSs measuring 3.5 mm in diameter and 5 mm in height were placed in a 24-well plate and subjected to AMF with output currents of 10 A, 15 A, 20 A, and 25 A at a constant frequency of 550 kHz, as depicted in the experimental schematic (Fig. 3h), to examine their magnetothermal conversion and temperature thresholds. The absence of MNPs resulted in the BSG group exhibiting no significant temperature increase under AMF across all output currents (Supplementary Fig. 8). The incorporation of MNPs resulted in immediate temperature increases for the 5-MNP-BSG and 10-MNP-BSG groups upon exposure to AMF, with all output currents, and rapidly reached stable temperature thresholds (Fig. 3i, j). The 5-MNP-BSG group exhibited stable temperature thresholds under AMF at output currents of 10 A, 15 A, 20 A, and 25 A, recorded as 37.1 °C ± 0.5 °C after 4.5 min, 41.6 °C ± 0.6 °C after 3 min, 47.6 °C ± 0.2 °C after 3 min, and 54.6 °C ± 0.3 °C after 3 min, respectively (Fig. 3i). For the 10-MNP-BSG group, the stable temperature thresholds under AMF with output currents of 10 A, 15 A, 20 A, and 25 A were recorded as 43.1 °C ± 0.1 °C after 4 min, 48.6 °C ± 0.6 °C after 2.5 min, 54.6 °C ± 0.3 °C after 3 min, and 58.5 °C ± 0.2 °C after 3.5 min, respectively (Fig. 3j). Analyzing the magnetothermal conversion outcomes of IMBSs under varying AMFs reveals that by simultaneously manipulating the MNPs in IMBSs and the strength of the applied AMF, diverse MH applications could be effectively utilized in various diseases. Following an investigation into the magnetothermal properties of IMBSs under varying AMFs, pre-cured IMBSs were subsequently positioned in Transwell chambers of a 24-well plate, with 600 μL of phosphate-buffered saline (PBS) added to each well (Fig. 3k). This setup was utilized to evaluate their temperature thresholds and the stability of magnetothermal conversion during multiple on/off cycles of AMF, with an output current of 20 A at a constant frequency of 550 kHz, simulating clinical conditions40. Following three cycles of activation and deactivation of AMF, the temperature variations and corresponding thresholds for the 5-MNP-BSG and 10-MNP-BSG groups exhibited no significant differences, with temperature thresholds recorded at 41.5 °C ± 0.2 °C and 44.6 °C ± 0.4 °C, respectively (Fig. 3l). This indicates the consistent stability of the magnetothermal performance of IMBSs and their potential for clinical applications in disease treatment utilizing MH.
The results of rheology, handling, and magnetothermal properties indicate that IMBSs exhibit significant minimally invasive potential and adjustable magnetic heating, suggesting promising applications in effective tumor therapy without causing harm to surrounding tissue during implantation31.
In vitro ionic release and biomineralization of IMBSs
BSG-based biomaterials exhibit degradation in both in vivo and in vitro settings, facilitating the release of matrix ions and subsequently creating an IAM. This IAM is essential in mediating macrophage polarization and functional expression, while also directing the osteogenic and angiogenic differentiation of stem cells, thus exhibiting notable tissue regeneration and repair capabilities. Hence, we systematically examined the effects of MH on weight loss, biomineralization, ionic release, and the formation of an alkaline environment in IMBSs upon exposure to AMF. As depicted in Supplementary Fig. 9, no significant differences in weight loss were observed among all groups of IMBSs during the initial 7-day and 14-day immersed intervals in PBS without AMF. However, application of AMF for 30 min daily resulted in greater weight losses in the 5-MNP-BSG and 10-MNP-BSG groups compared to the BSG group after 7 and 14 days of immersion. This observation indicates that MH has enhanced the biodegradation of BSG in IMBSs, and that the promotion of BSG biodegradation can be further improved with increased incorporation of MNPs. After 7 days of soaking in PBS, a layer of spherical fine particles was observed on the surfaces of IMBSs across all groups. The 5-MNP-BSG and 10-MNP-BSG groups demonstrated a significantly higher density of biomineralized particles compared to the BSG group, indicating that an increased quantity of MNPs in IMBSs leads to enhanced surface mineralization. With a soaking duration of 14 days, the biomineralized particles on the surfaces of IMBSs exhibited a greater presence in the 5-MNP-BSG and 10-MNP-BSG groups compared to the BSG group (Fig. 4a). EDS mapping of IMBSs after a 14-day immersion in PBS revealed that the elemental composition of the biomineralized particles on the surfaces of 5-MNP-BSG (+) and 10-MNP-BSG (+) consisted of carbon (C), oxygen (O), phosphorus (P) and calcium (Ca), exhibiting a stoichiometric ratio greater than that observed in BSG (Supplementary Fig. 10). XRD analysis of IMBSs with identical soaking durations indicated that the biomineralized particles corresponded to HA, as evidenced by broad diffraction peaks at 2θ of 32° in the XRD patterns. The 5-MNP-BSG and 10-MNP-BSG groups exhibited higher and more distinct diffraction peaks at 2θ = 32° (Fig. 4b). The results of ionic release indicated that, at the initial immersion period of 7 days without AMF application, there were no significant differences in the cumulative concentrations of BO33- and Ca2+ in PBS across the various groups of IMBSs (Fig. 4c, d). Under an immersion period of 7 days in PBS under AMF with an output current of 20 A at a magnetic frequency of 550 kHz, the cumulative releases of BO33- and Ca2+ in the 5-MNP-BSG and 10-MNP-BSG groups were significantly higher than in the BSG group. Furthermore, the increase in cumulative ion release was enhanced with a greater quantity of MNPs in IMBSs. The extension of soaking duration to 14 and 28 days resulted in a gradual reduction in the promotion of the ionic release of IMBSs by MH. Additionally, the cumulative ionic release of BO33- and Ca2+ exhibited no significant differences across all IMBSs groups, including those with AMF groups. This indicates that although the mineralization and ion release of BSG during the initial soaking phase were enhanced by the MH of IMBSs under AMF, these effects were not significant in the middle and later soaking periods. Additionally, no detection of ionic release of Fe3+, Zn2+, and Co2+ in PBS (Fig. 4e and Supplementary Fig. 11a, b) indicated that MNPs in IMBSs exhibited no degradation. This stability of MNPs ensures the longevity of MH throughout the entire service period of IMBSs in vivo. After immersing IMBSs for varying durations, the pH value of PBS initially increased and subsequently stabilized during the later immersion stage across all groups, indicating the capacity to create an alkaline microenvironment due to the degradation of BSG. Notably, the MH of MNPs under AMF increased the pH value of PBS during the initial immersion period, while no significant differences in pH values were observed between the 5-MNP-BSG and 10-MNP-BSG groups (Fig. 4f). Subsequently, the cumulative release of BO33- and Ca2+ along with the solution pH from IMBSs after soaking in PBS for 30 min under AMF with variation output currents (10 A, 15 A, 20 A, and 25 A) and a constant frequency (550 kHz) were analyzed. The results indicated that an increase in the output current, corresponding with rising temperature, led to a gradual increase in ion release from IMBSs and the pH value of PBS (Supplementary Fig. 12a–c).
a Surface biomineralization (as indicated by the yellow circles) of IMBSs after immersion periods of 7 and 14 days as detection by SEM (scale bar = 10 μm). b XRD patterns of IMBSs following immersion in PBS of 14 days. c–e Cumulative concentration of BO33-, Ca2+ and Zn2+ in PBS. f pH curves of PBS following IMBSs immersed until 28 days. g, h Dynamic release profiles of BO33- and Ca2+ after IMBSs immersed in PBS for 28 days, with PBS being changed daily. Data in c-h are presented as means ± SD, n = 3 independent experiments.
In addition to testing cumulative ion release, dynamic ion release of IMBSs was also conducted to simulate in vivo dynamic circulation by replacing the PBS daily for a duration of 28 days. The results indicated that the MH of MNPs under an AMF enhanced the dynamic release of ions in the 5-MNP-BSG and 10-MNP-BSG groups compared to the BSG group during the initial 5 days of soaking. This was evidenced by the higher concentrations of BO33- in PBS, with 5-MNP-BSG at 51.4 μg/mL ± 0.2 μg/mL and 10-MNP-BSG at 50.9 μg/mL ± 0.7 μg/mL, as shown in Fig. 4g, h. However, no significant differences were observed in the dynamic release of BO33- between the 5-MNP-BSG (43.4 μg/mL ± 0.3 μg/mL) and 10-MNP-BSG (42.6 μg/mL ± 0.2 μg/mL) groups (Fig. 4g, h).
Combining the results of weight loss, SEM, XRD, EDS, ionic release, and pH value of PBS, it can be concluded that MH unfolding from MNPs under AMF accelerated the biodegradation and biomineralization of BSG, subsequently forming a reinforced IAM41. Upon interaction with tumor cells both in vivo and in vitro, the MH of IMBSs initially facilitates tumor suppression, while the enhanced IAM is anticipated to more effectively disrupt the acidic microenvironment within tumor tissue, potentially inhibiting the onset and metastasis of OS41. This reinforced IAM promotes the biomineralization of HA, which supports osteogenesis after OS resection42. This synchronous modulation of tumor suppression and osteogenic promotion signifies a progressive trend in the treatment of bone tumors.
Inhibition of MH, BSG, and their combination on the viability of OS cells
The effects of MH, BSG and IMBSs on the viability of OS cells were initially evaluated through CCK-8 assays. To evaluate the anti-tumor ability of MH solely, culture media for 143B and UMR106 cells were maintained in a cell incubator at temperature gradients of 37 °C, 42 °C, and 45 °C to stimulate regular culture temperature. The temperature thresholds for 5-MNP-BSG (41.5 °C ± 0.2 °C) and 10-MNP-BSG (44.6 °C ± 0.4 °C) were determined under AMF (20 A, 550 kHz), as illustrated in Fig. 3l. However, whether AMF will affect the temperature of culture medium should be preliminarily concerned. By exposing the standard cell culture media for 143B and UMR106 cells to AMF (20 A, 550 kHz), we verified that AMF imparted no effects on the temperature of culture media without IMBSs, because no significant temperature variations were detected under AMF with the duration time of 6 min (Supplementary Fig. 13). When incubated in temperature gradients for 5 h, only culture temperature of 45 °C exhibited a significant reduction in viability of 143B cells (77.1% ± 3.5%) and UMR106 cells (70.3% ± 4.2%), while for culture temperatures of 37 °C and 42 °C, no significant inhibitions on viability of 143B and UMR106 cells were detected (Supplementary Fig. 14), suggesting that elevated temperatures are responsible for the inhibition of tumor cells.
Subsequently, the cytotoxicity of MNPs (Zn0.54Co0.46Cr0.6Fe1.4O4) to143B cells, UMR106 cells, hBMSCs, and RAW 264.7 cells were systematically examined. Following UV sterilization, MNPs were diluted in the corresponding regular culture medium, resulting in concentration gradients of 0 μg/mL, 15 μg/mL, 30 μg/mL, 60 μg/mL, 120 μg/mL, 240 μg/mL, 480 μg/mL, and 1000 μg/mL. After 24 h, MNPs at a concentration of 240 μg/mL began to demonstrate mild toxicity across all cell types, whereas only MNPs at concentrations exceeding 480 μg/mL exhibited significant toxicity to those cells, as determined by the CCK-8 assay (Supplementary Fig. 15a–d).
Furthermore, extracts of IMBSs were produced to assess the impact of IAM derived from the degradation of BSG on the cell viability of 143B cells over a culture period of 1 to 10 days. Supplementary Fig. 16 illustrated that in the absence of AFM, no significant temperature increase in the culture media was observed. The inhibition of OS cells under these conditions may primarily result from the IAM formed from BSG degradation in IMBSs37,38. The in vitro anti-tumor activity of extracts from IMBSs (Supplementary Fig. 16) demonstrated the highest inhibition of OS cells on the first day of culture, which subsequently declined and stabilized at 48.0% ± 4.6% for the BSG group, 47.6% ± 4.3% for the 5-MNP-BSG group, and 48.5% ± 4.1% for the 10-MNP-BSG group on the 7th day and thereafter. No significant difference in the in vitro anti-tumor activity of extracts across all IMBSs was observed, indicating that the incorporation of MNPs without AMF application does not significantly affect the degradation of BSG in IMBSs. In conclusion, the initial degradation of BSG has a measurable inhibitory effect on OS cells; however, as degradation decreases, the ions released from BSG in IMBSs become inadequate to sustain a significant inhibitory effect on OS cell activity. Therefore, incorporating MH is essential to enhance the long-term inhibitory effects of bioactive glass on OS cells.
Following the exclusive assessment of the anti-tumor effects of MH and BSG, a culture model (Fig. 3h) was utilized to investigate the inhibitory effects of the IMBSs on OS cells. In this setup, IMBSs samples (φ = 3.5 mm, h = 5.0 mm) were positioned in the upper chamber of a Transwell apparatus, while tumor cells were cultured in the lower chamber. Following exposure in AMF with an output current of 20 A and a frequency of 550 kHz, the temperatures of the culture medium increased immediately for the 5-MNP-BSG and 10-MNP-BSG groups, whereas the BSG group exhibited no significant temperature change. For duration times of 0, 1, 3, 5, 8, and 12 min, the temperatures of the culture medium were recorded as follows: 24.0 °C ± 0.4 °C, 28.5 °C ± 0.2 °C, 36.5 °C ± 0.2 °C, 39.2 °C ± 0.4 °C, 41.9 °C ± 0.4 °C, and 42.0 °C ± 0.3 °C for the 5-MNP-BSG (+) groups; and 23.9 °C ± 0.3 °C, 30.2 °C ± 0.3 °C, 39.6 °C ± 0.2 °C, 43.4 °C ± 0.3 °C, 45.3 °C ± 0.2 °C, and 45.5 °C ± 0.2 °C for the 10-MNP-BSG (+) groups (Supplementary Fig. 17). Nonetheless, in the absence of AMF, none of the IMBSs groups exhibited significant temperature variations in the culture medium (Supplementary Fig. 17). After exposure in AMF for varying durations, the cells were incubated for 2 h and then subjected to the CCK-8 assay. Supplementary Fig. 18 illustrated that the viability of OS cells in the BSG group was approximately 80%, with no significant differences observed across various durations. In the 5-MNP-BSG (+) and 10-MNP-BSG (+) groups, the viability of OS cells decreased over time, with the 10-MNP-BSG (+) group consistently exhibiting greater inhibition of OS cells compared to the 5-MNP-BSG (+) group during the initial treatment period. At the 8-min interval of IMBSs, both the 5-MNP-BSG (+) and 10-MNP-BSG (+) groups exhibited maximal inhibition of OS cells. The cell viability of 143B in the 5-MNP-BSG (+) and 10-MNP-BSG (+) groups was recorded at 28.1% ± 0.7% and 25.9% ± 3.0%, respectively. For UMR106, the cell viability in the 5-MNP-BSG (+) and 10-MNP-BSG (+) groups was 27.3% ± 1.3% and 27.0% ± 2.7%, respectively. The findings indicate that a duration of 8 min for IMBSs is sufficient to reach the temperature thresholds of IMBSs and effectively kill tumors, whereas longer durations do not significantly enhance temperature thresholds or anti-tumor activity. The 8-min duration of IMBSs was then established as the standard for subsequent treatments involving migration and invasion tests of these tumor cells, as well as for subsequent animal studies.
Subsequently, OS cells were cultured with IMBSs and subjected to AMF (20 A, 550 kHz) for a duration of 8 min to investigate the specific inhibition of OS cells. Inhibition rates for 143B cells were recorded as follows: 52.6% ± 3.7% for the BSG group, 53.7% ± 1.8% for the 5-MNP-BSG group, 53.1% ± 3.7% for the 10-MNP-BSG group, 85.2% ± 1.4% for the 5-MNP-BSG (+) group, and 87.3% ± 1.7% for the 10-MNP-BSG (+) group. the blank control group exhibited no significant inhibition of 143B cells. The inhibition rates for UMR106 cells were as follows: 39.0% ± 1.3% for the BSG group, 39.3% ± 2.7% for the 5-MNP-BSG group, 37.9% ± 0.4% for the 10-MNP-BSG group, 80.8% ± 1.9% for the 5-MNP-BSG (+) group, and 88.0% ± 1.2% for the 10-MNP-BSG (+) group. No significant inhibition was observed in the blank control group. The results indicated that the inhibition of IMBSs in the 5-MNP-BSG (+) and 10-MNP-BSG (+) groups on OS cells was significantly greater than that of IAM in the BSG, 5-MNP-BSG, and 10-MNP-BSG groups. Furthermore, the inhibition of IAM of BSG (IMBSs without AMF) on OS cells exhibited minimal differences across the groups of BSG, 5-MNP-BSG, and 10-MNP-BSG (Fig. 5a).
a Suppression of cell viability in 143B and UMR106 when cultured with IMBSs under AMF (20 A, 550 kHz). b Alamar blue staining of 143B and UMR106 cells when cultured with IMBSs under AMF (20 A, 550 kHz) for 8 min. c, d Colony capacity of 143B and UMR106 cells when cultured with IMBSs under AMF (20 A, 550 kHz), along with the corresponding quantitative analysis. e, f Migration capacity of 143B and UMR106 cells when cultured with IMBSs under AMF (20 A, 550 kHz), along with the corresponding quantitative analysis (scale bar = 50 μm). g, h The invasive behavior of 143B and UMR106 cells when cultured with IMBSs under AMF (20 A, 550 kHz) for 8 min by a Transwell method, along with the corresponding quantitative analysis (scale bar = 100 μm). i, j Analysis of the proteins associated with the EMT process in 143B and UMR106 cells when cultured with IMBSs and subjected to AMF (20 A, 550 kHz) for 8 min, as assessed by Western blot and corresponding semi-quantitative analysis. k, l Analysis of the proteins associated with the EMT process in 143B and UMR106 cells when cultured with IMBSs and subjected to AMF (20 A, 550 kHz) for 8 min, as assessed by Western blot and corresponding semi-quantitative analysis. Statistical data in a, d, f, h, j, l are presented as means ± SD (n = 3 independent experiments), statistical significance was calculated using two-way ANOVA method with Tukey’s multiple comparisons tests. *P < 0.05, **P < 0.01, ***P < 0.001, and ****P < 0.0001 were considered statistically significant, while nsP > 0.05 were considered not statistically significant.
In vitro systematic evaluation of the anti-tumor properties of IMBSs
Following the investigation into the inhibition of IMBSs on the viability of OS cells, the candidates selected for further systematic evaluation of the anti-tumor efficacy of IMBSs in vitro included the blank control group, BSG group, 5-MNP-BSG (+) group, and 10-MNP-BSG (+) group. Cell morphology analysis, as shown in Supplementary Fig. 19, revealed no significant changes in OS cells from the blank control group, indicating their healthy status. In the BSG group, both 143B and UMR106 cells exhibited slight cellular shrinkage and increased refractility, accompanied by larger intercellular spaces, indicating moderate damage to OS cells by BSG. In the groups treated with 5-MNP-BSG (+) and 10-MNP-BSG, a greater proportion of dead OS cells was observed floating in the medium. Additionally, the surviving adherent cells exhibited signs of distress, characterized by rounding and shrinkage, following 8 min of IMBSs treatment. Further investigation revealed that numerous highly refractive circular structures were present on the surfaces of OS cells, alongside the simultaneous formation of tentacle-like circular bodies with multiple surface protrusions. These phenomena were particularly noted in UMR106 cells within the 5-MNP-BSG (+) and 10-MNP-BSG (+) groups, indicating the optimal lethality of IMBSs therapy.
Meanwhile, Alamar blue staining was performed to assess the cell viability of OS cells under IMBSs therapy. The pink staining indicates high cell viability, while blue staining signifies a substantial reduction in cell viability43. Fig. 5b demonstrated that the culture medium in the blank control exhibited a pink appearance, whereas the culture medium in the BSG group showed a red color. In contrast, the culture media in the 5-MNP-BSG (+) and 10-MNP-BSG (+) groups presented a blue color. The Alamar blue staining images demonstrated that OS cells in the blank control experienced minimal damage. IAM resulting from BSG degradation in IMBSs exhibited moderate inhibition of OS cells. In contrast, hyperthermia derived from the 5-MNP-BSG (+) and 10-MNP-BSG (+) groups caused significant harm to 143B and UMR106 cells.
The formation of colonies by tumor cells indicates their capacity for proliferation and aggregation, and tumor cells exhibiting significant in vitro clonogenic ability often demonstrate enhanced tumorigenic potential in vivo44. Following an 8-min treatment with IMBSs, OS cells were harvested, diluted with complete cell medium at a 1:100 ratio, and then cultured in a 6-well plate. Following an additional 7-day incubation period, the colony formation was subjected to staining with 0.1% Crystal Violet, and the corresponding colony counts were determined. Fig. 5c, d illustrated that the positive staining area for colony formation was highest in the blank control group (935.0 ± 30.0 for 143B cells and 1143.0 ± 75.0 for UMR106 cells), moderate in the BSG group (486.0 ± 32.5 for 143B cells and 955.3 ± 22.0 for UMR106 cells), and lowest in the 5-MNP-BSG (+) and 10-MNP-BSG (+) groups. No significant difference in colony formation was observed between the 5-MNP-BSG (+) group (59.3 ± 18.2 for 143B cells and 72.0 ± 20.1 for UMR106 cells) and the 10-MNP-BSG (+) group (53.3 ± 15.5 for 143B cells and 58.7 ± 18.2 for UMR106 cells). The investigation of colony formation reveals that the BSG combination significantly improved the anti-tumor efficacy of moderate MH, achieving OS killing comparable to that of high temperature (48 − 50 °C) while minimizing damage to normal tissue.
Cell migration denotes the movement of cells in response to migration signals or gradients of specific substances. Tumor cells exhibiting robust migratory capabilities frequently demonstrate increased malignancy and a heightened propensity for metastasis within the organism45. A small wound area was created in the 90% confluent monolayer of 143B and UMR106 cells using a 10 μL pipette tip in a lengthwise stripe prior to culturing with IMBSs. Following culture with IMBSs and exposure to the designated AMF for 8 min, OS cells were subsequently cultured for 24 h. Their migrations were then photographed and semi-quantitatively assessed, as illustrated in Fig. 5e, f. The migration rates of 143B cells were 48.9% ± 2.4% for the blank control group, 2.0% ± 0.6% for the BSG group, 1.3% ± 0.1% for the 5-MNP-BSG (+) group, and 0.9% ± 0.2% for the 10-MNP-BSG (+) group. The migration rates of UMR106 cells were 65.6% ± 6.4% for the blank control group, 1.3% ± 0.1% for the BSG group, 1.3% ± 0.1% for the 5-MNP-BSG group, and 0.9% ± 0.2% for the 10-MNP-BSG (+) group. Cell invasion, a specialized type of cell migration, requires tumor cells to penetrate the basement membrane or extracellular matrix and invade surrounding tissues, including blood and lymphatic vessels45. To further assess the impact of IMBSs therapy on the invasive potential of OS cells, a Transwell assay was conducted. Following a 24-hour incubation in the lower chamber with Matrigel (1:8), 143B and UMR106 cells were collected, treated with IMBSs for 8 min, and then transferred to the upper chamber. The cells were subsequently cultured at 37 °C in a 5% CO2 environment for an additional 24 h. Invading OS cells were stained with 0.1% Crystal Violet and subsequently counted in five random fields per filter at 200× magnification across triplicate wells for each group. Fig. 5g, h illustrates that the inhibition rates of OS cells were moderate in the BSG group (21.9% ± 2.0% for 143B cells and 11.5% ± 1.9% for UMR106 cells). The highest rates were observed in the 5-MNP-BSG (+) group (4.4% ± 0.3% for 143B cells and 6.0% ± 0.3% for UMR106 cells) and the 10-MNP-BSG (+) group (4.1% ± 0.9% for 143B cells and 4.1% ± 0.7% for UMR106 cells), in comparison to the blank control group. A comprehensive analysis of the migration and invasion results of OS cells indicates that IAM derived from BSG degradation (BSG group) significantly inhibited these processes compared to the blank control group. Furthermore, the IMBSs (5-MNP-BSG (+) and 10-MNP-BSG (+) groups) showed a more pronounced reduction in the migration and invasion of OS cells after 24-hour of culture period (Fig. 5e–h). Nonetheless, no statistically significant difference was observed between the 5-MNP-BSG (+) and 10-MNP-BSG (+) groups (P > 0.05) (Fig. 5e–h). These results indicate that the application of a moderate MH combination with IAM of BSG demonstrates significant potential in inhibiting malignancy, metastasis, and recurrence of OS cells while minimizing thermal damage to adjacent normal tissues.
Epithelial-mesenchymal transition (EMT) is the process whereby tumor cells, under certain conditions, lose their polarity and adhesion properties, subsequently acquiring characteristics typical of mesenchymal cells. This transformation involves substantial changes in cell morphology, molecular marker expression, and gene expression patterns46. Molecular markers of OS cells associated with the EMT process, including E-cadherin, N-cadherin, Vimentin, and Slug, were analyzed using Western blot. Figure 5i-l illustrated that, in comparison to the blank control, the BSG group exhibited an up-regulation of E-cadherin protein expression in 143B and UMR106 cells, alongside a down-regulation of N-cadherin, Vimentin, and Slug proteins. Additionally, the 5-MNP-BSG (+) and 10-MNP-BSG (+) groups demonstrated an increased expression of E-cadherin, alongside a sustained reduction in the levels of N-cadherin, Vimentin, and Slug. However, the variations in Slug expression between the 5-MNP-BSG (+) and 10-MNP-BSG (+) groups were not statistically significant (P > 0.05).
In summary, IAM derived from the degradation of BSG exhibits moderate inhibition of OS cell migration and invasion of OS cells. Nonetheless, the IMBSs therapy significantly reduced the migratory and invasive capabilities of OS cells, even at a moderate temperature of 42 °C for MH.
Moderate MH and BSG combination mediated TNF signaling pathway to induce apoptosis in OS cells
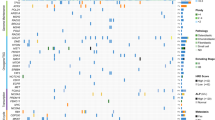
On the basis of systematic research on the anti-tumor properties of moderate MH and BSG combination, the relevant biological mechanism involved in the inhibition of human OS cells (143B) when cultured with IMBSs under AMF was discussed by conducting RNA-seq. Four experimental groups were established: the blank control group (pure cell culture medium), the BSG group (co-cultured with the BSG sample), the 5-MNP-BSG group (co-cultured with the 5-MNP-BSG sample without AMF), and the 5-MNP-BSG (+) group (co-cultured with the 5-MNP-BSG sample under AMF (20A, 550 kHz)). Following a culture period of 2 h, 143B cells were harvested for RNA-seq. The database information and data analysis software were included in Supplementary Tables 3 and 4, respectively. RNA-Seq data identified 371 up-regulated genes and 272 down-regulated genes between the BSG group and the blank control group. Additionally, 2 up-regulated genes and 25 down-regulated genes were found between the BSG and 5-MNP-BSG groups (Supplementary Figs. 20 and 21a, b). This indicates that the simple inclusion of MNPs did not substantially influence the anti-tumor mechanisms of BSG within IMBSs. The application of AMF subjecting in the identification of 90 up-regulated and 267 down-regulated genes when comparing the 5-MNP-BSG (+) group to the blank control group. Additionally, 6 up-regulated and 80 down-regulated genes were observed between the 5-MNP-BSG (+) group and the BSG group. The Venn diagram illustrated the differentially expressed genes (DEGs) across various groups (Supplementary Fig. 22).
Gene Ontology (GO) analysis indicated that the combination of BSG and moderate MH synergistically triggered a pro-inflammatory response in OS cells, which was associated with biological processes referring to pro-inflammatory response, CXCR chemokine receptor binding, and calcium channel regulatory activity (Supplementary Fig. 23). Assessment of KEGG analysis revealed that the significantly upregulated signaling pathways in OS cells included the TNF, NF-κB, and IL-17 signaling pathways, while the downregulated signaling pathways comprised the TGF-β, Sphingolipid, and mTOR pathways, in comparison of the BSG group to the blank control (Supplementary Fig. 24a, b). Regarding the 5-MNP-BSG (+) group in comparison to the blank control, in addition to the TNF, NF-κB, and IL-17 signaling pathways, the apoptotic signaling pathway in OS cells, including apoptosis and necrotic apoptosis, was also noted. Conversely, signaling pathways such as calcium and GnRH were down-regulated in the tumor cells of the 5-MNP-BSG (+) group. Therefore, it is reasonable to conclude that, for the elimination of OS cells, whether through BSG alone or in combination with moderate MH, the up-regulation of TNF and NF-κB signaling pathways in OS cells consistently persists, indicating the sustained inhibition of tumor cells by BSG via the activation of these pathways. Moreover, the apoptosis pathway in OS cells (Supplementary Fig. 25a, b) was exclusively activated in the 5-MNP-BSG (+) group, as opposed to the BSG group, when compared to the blank control. This indicates that moderate MH can subsequently induce cell apoptosis, ultimately leading to the complete demise of OS cells through the inhibition of BSG. Consequently, it can be considered that the IAM resulting from BSG degradation can primarily impair the viability and malignant behavior of OS cells by activating the TNF signaling pathway. This sickening effect diminishes the hyperthermia tolerance of OS, thereby boosting apoptosis of OS cells, even in the presence of the fundamentally limited anti-tumor effects of moderate MH.
Moreover, genes expression in 143B cells linked to the TNF and NF-κB signaling pathways were up-regulated in the BSG group as compared to the blank control group (Fig. 6a), and the expression of stress-related AP1 genes, including FOS and JUNB, was also notably elevated from 143B cells the BSG group according to the Volcano plot (Fig. 6b and Supplementary Fig. 21a). As is well known, the TNF signaling pathway functions as a pro-apoptotic pathway, while the NF-κB signaling pathway operates as an anti-apoptotic pathway47. Previous study also demonstrated that FOS regulates downstream gene expression by binding to JUN family proteins, specifically JUNB, to form AP-1 transcription complexes48. This interaction influences cell cycle, proliferation, and differentiation, while JUNB assists cells in adapting to stressful environments49, and prolonged stress or injury can lead to FOS promoting the expression of apoptosis-related genes, which ultimately induces cell apoptosis50. Those findings indicated that the IAM of BSG markedly activated pro-inflammatory pathways, consistent with GO analysis (Supplementary Fig. 23), thereby increasing the propensity for TNF-induced apoptosis in OS cells. Under this scenario, to counteract TNF-induced apoptosis, tumor cells tend to activate the NF-κB pathway inherently, thereby increasing their survival and aggressiveness50. Therefore, it is reasonable to conclude that, while IAM of BSG induce a certain of apoptosis to the tumor cells, the activation of NF-κB signaling pathway may evoke their natural resistance to apoptosis to adapt and further survival on hazard environment. Noteworthily, log2 transformation and row-wise normalization of the heatmap (Fig. 6c) illustrated that, besides the higher expression of the FOS and TNF genes from 143B cells in the 5-MNP-BSG (+) group, no notable alteration in JUNB gene expression was detected. Those findings revealed that, moderate MH transpired the natural apoptotic resistance of the tumor cell via the activation of the NF-κB signaling pathway. Therefore, the TNF, NF-κB, and cell apoptosis signaling pathways were chosen for subsequent verification.
a, b Analysis of DEGs in the TNF, NF-κB, and apoptosis signaling pathways of 143B cells following treatment with BSG as determined by RNA-seq. c Heatmap of DEGs to analyze the TNF, NF-κB, and apoptosis signaling pathways in 143B cells following IMBSs therapy. d, e Expression of TNF and NF-κB signaling pathway-related proteins in 143B cells following treatment with BSG and IMBSs as analyzed by Western Blot, alongside with relevant semi-quantitative analysis. f Expression of apoptosis signaling pathway-related proteins in 143B cells following treatment with BSG and IMBSs as analyzed by Western Blot. g TEM detection of the morphology of 143B cells following treatment with BSG and IMBSs (black bar = 2 μm, white bar = 1 μm). h Hoechst 33258 staining of the apoptosis status in 143B cells following treatment with IMBSs after the TNFR1 silence by siRNA (scale bar = 100 μm). i Flow cytometry analysis in early and late apoptotic OS cells following treatment with BSG and IMBSs therapy after the TNFR1 silence by siRNA. j Schematic diagram illustrating the biological mechanism involved in BSG and IMBSs therapy inhibition of OS cells. All experiments were conducted under AMF (20 A, 550 kHz) for a duration of 8 min. Statistical data in a–e are presented as means ± SD, n = 3 independent experiments. Statistical significance in b, e was calculated using two-way ANOVA method with Tukey’s multiple comparisons tests. **P < 0.01 and ****P < 0.0001 were considered statistically significant, while nsP > 0.05 were considered not statistically significant.
The protein expression levels in 143B cells associated with TNF and NF-κB signaling pathways including TNF-α, TNFR1, NF-κB p65, Phospho-NF-κB p65 (Ser536), IκB-α, and Phospho-IκB-α (Ser32/Ser36) were assessed through Western Blot analysis. The results indicated (Fig. 6d, e) that, compared to the blank control group, the expression levels of TNF-α, TNFR1, NF-κB p65, Phospho-NF-κB p65 (Ser536), IκB-α, and Phospho-IκB-α (Ser32/Ser36) were significantly elevated in the BSG group, whereas the 5-MNP-BSG (+) group demonstrated the most significant increase in protein expression associated with the TNF signaling pathway in 143B cells (Fig. 6d, e). This finding indicates that the combination of moderate MH and IAM of BSG activates the TNF signaling pathway, promoting apoptosis in OS cells while inhibiting their proliferation, migration, and invasion capabilities. The effect of IMBSs therapy on the expression of apoptosis-related proteins in 143B cells was also evaluated using Western Blot. The results indicated that, compared to the blank control group, the expression of Cleaved PARP and Cleaved caspase-3 in 143B cells within the BSG group was elevated, whereas the expression of Bcl-2 was reduced. The 5-MNP-BSG (+) group exhibited the most significant increase in the expression of Cleaved PARP and Cleaved caspase-3 in 143B cells, while also showing the lowest expression of Bcl-2 (Fig. 6f and Supplementary Fig. 26).
Prior studies indicate that TEM effectively reveals the nuanced structural alterations in cells undergoing apoptosis, including cell shrinkage, mitochondrial swelling, and endoplasmic reticulum expansion51. The nucleus experiences several alterations, such as condensation, increased density, chromatin condensation, and edge aggregation, resulting in nuclear fragmentation and the eventual formation of apoptotic bodies51. Figure 6g demonstrated that 143B cells in the blank control group exhibited healthy morphologies, whereas those in the BSG group displayed signs of damage, characterized by a loosened morphology and the presence of small vesicles of varying sizes within the cytoplasm. The 5-MNP-BSG (+) group exhibited contraction and compromised membrane integrity in 143B cells. Substantial vacuolar material surrounding the nucleus, along with chromatin condensation and nuclear fragmentation, was observed, indicating apoptosis in 143B cells (Fig. 6g).
To clarify the important function of the TNF signaling pathway in the induction of apoptosis in OS cells, the expression of the TNFR1 gene in 143B cells was silenced using siRNA prior to the application of moderate MH and BSG (Supplementary Figs. 27 and 28). After 24 h of incubation period, Hoechst 33258 staining and flow cytometry were employed to qualitatively and quantitatively analyze the apoptosis of OS cells. The Hoechst 33258 staining allowed for a clearer distinction of apoptotic 143B cells with fragmented nuclei from normal karyomorphism52. The results showed that no fragmented nuclei in 143B cells was detected in the blank control group, while the highest incidence of fragmented nuclei in 143B cells occurred in the 5-MNP-BSG (+) group, whereas a limited number of fragmented nuclei was noted in the BSG and siTNFR1/5-MNP-BSG (+) groups (Fig. 6h). Flow cytometry results indicated that, in comparison to the blank control group, the BSG group exhibited a modest increase in early and late apoptotic cells (7.2%; 6.7%, respectively), whereas the 5-MNP-BSG (+) group exhibited a significant increase in early and late apoptotic cells (25.1%; 18.5%, respectively). After the knockdown of TNFR1 expression, the siTNFR1/5-MNP-BSG (+) group demonstrated a decrease in apoptotic cells with rates of 5.4% for early-stage and 12.7% for late-stage apoptosis (Fig. 6i). Collectively, the findings validate that IAM produced from BSG degradation can activate the TNF signaling pathway, resulting in a moderate inhibitory effect on OS cells. This weakness effect thus diminishes the hyperthermia tolerance of OS, thereby boosting apoptosis of OS cells, even in the presence of the fundamentally limited anti-tumor effects of moderate MH (Fig. 6j).
Moderate MH and BSG combination mediated the osteogenic differentiation of human bone marrow stromal cells (hBMSCs)
Clinicians aim to utilize advanced therapeutic technologies for the optimal management of bone tumors, effectively eliminating tumors while preventing metastasis and recurrence, and restoring the disrupted balance between osteogenic regeneration and osteoclast resorption, thus achieving an ideal sequence of tumor suppression and subsequent bone defect regeneration53. Therefore, we investigated the impact of moderate MH, the IAM of BSG, and their combination on the osteogenesis of hBMSCs and the related biomolecular mechanism. To replicate the dynamic degradation microenvironment of implants implemented in vivo, dynamic extracts of IMBSs were produced by submerging IMBSs samples in DMEM culture medium supplemented with 1% penicillin/streptomycin (P/S) following standard procedures outlined in ISO 10993, with the culture medium being refreshed every 24 h for a duration of 18 days. Dynamic extracts were collected at various time intervals, and hBMSCs were then grown in these extracts for 24 h to comprehensively evaluate the impact of dynamic extracts on the activity and osteogenic differentiation of hBMSCs. For immersion times shorter than 10 days, nearly no viable cells were observed when cultured with dynamic extracts. After a period beyond 10 days of immersion, the inhibitory effects of dynamic extracts on hBMSCs diminished, resulting in relative growth rates (RGRs) of 45.4% ± 4.5%, 45.3% ± 1.1%, and 46.2% ± 2.6% for the BSG, 5-MNP-BSG, and 10-MNP-BSG groups, respectively. During an immersion period of 18 days, dynamic extracts of IMBSs exhibited significant cytotoxicity on hBMSCs (> 70%). The RGRs of hBMSCs were 85.3% ± 1.4%, 85.2% ± 2.2%, and 84.8% ± 2.3% for the BSG, 5-MNP-BSG, and 10-MNP-BSG groups, respectively (Supplementary Fig. 29). The findings indicate that, in conjunction with a reduced ionic release, particularly the significantly lower release of BO33- from IMBSs (375.2 μg/mL ± 36.5 μg/mL on the first day of immersion in PBS, compared to 52.16 μg/mL ± 6.7 μg/mL after 18 days of immersion), and enhanced HA biomineralization on the IMBSs surface, the cytotoxicity of IAM formation resulting from BSG degradation towards hBMSCs progressively diminishes. No significant changes in RGRs were seen among the BSG, 5-MNP-BSG, and 10-MNP-BSG groups when hBMSCs were grown in dynamic extracts at all designated time periods (Supplementary Fig. 30).
As a result, based on the findings regarding the dynamic extracts of IMBSs on the cytotoxicity of hBMSCs, the culture medium devoid of extract (blank control group) and the dynamic extract with a settled immersion duration of 18 days from the BSG group were chosen to examine the effects of MH or BSG individually, as well as the combined influence of MH and BSG on the osteogenic differentiation of hBMSCs. The schematic diagram was presented in Fig. 7a. As stated above, only IMBSs themselves, not the extracts under AMF, can exhibit MH, and the cellular modulation of MH essentially depends on the temperature response. Consequently, it is prudent and highly effective to investigate MH and BSG, either separately or in combination, regarding their influence on the osteogenic differentiation of hBMSCs by concurrently incubating hBMSCs with the prepared dynamic extracts in an oven set at precise temperatures of 37 °C, 42 °C, and 45 °C, respectively. For clear identification, the culture medium incubated at 37 °C without dynamic extract served as the blank control, while the culture medium incubated at 42 °C without dynamic extract was designated as the low temperature (LT) group, and the culture medium incubated at 45 °C without dynamic extract was designated as the high temperature (HT) group. The dynamic extract of the BSG group at an incubation temperature of 37 °C was designated as the BSG group, the extract at 42 °C was designated as the LT/BSG group, and the extract at 45 °C was designated as the HT/BSG group.
a Schematic diagram of osteogenic inductive experiments conducted under hyperthermia in vitro. b Cytotoxicity of hBMSCs after culture with groups of BSG (37 °C), low temperature (LT)/BSG (42 °C), and high temperature (HT)/BSG (45 °C) for 24 h and 72 h, respectively; and hBMSCs cultured with regulated media at temperatures of 37 °C (control), 42 °C (LT), and 45 °C (HT) serving as the control groups. c Live/dead and cytoskeleton staining of hBMSCs after culturing for 24 h (scale bar = 500 μm). d ALP staining of hBMSCs (upper row) after culturing for 7 days, and ARS of hBMSCs (bottom row) after culturing for 14 days (black bar = 5 mm; red bar = 500 μm). e–g Expression of early osteogenic-related genes (ALP, RUNX2, and COL-1) in hBMSCs after culturing for 7 days. h, i Expression of middle to late osteogenic-related genes (OCN and OPN) in hBMSCs after culturing for 14 days. j Volcano plot showing DEGs of hBMSCs with a culture time of 7 days between the BSG group and the blank control group. k Volcano plot showing DEGs of hBMSCs between the LT/BSG group and the blank control group. l Alterations in upregulated signaling pathways for hBMSCs between the BSG group and the blank control group, as assayed by KEGG analysis. m Changes in upregulated signaling pathways for hBMSCs between the LT/BSG group and the blank control group, as assayed by KEGG analysis. n Heatmap of DEGs of hBMSCs in the calcium and JAK-STAT3 signaling pathways between the LT/BSG and the blank control groups. o Protein expression of hBMSCs in the calcium and JAK-STAT3 signaling pathways after culturing for 7 days analyzed by Western Blot. p Mechanism diagram illustrating the effect of the IMBSs therapy on hBMSCs. Statistical data in b, e–i, n are presented as means ± SD, n = 3 independent experiments; Statistical significance in b, e–i was calculated using two-way ANOVA method with Tukey’s multiple comparisons tests. *P < 0.05, **P < 0.01 and ***P < 0.001 were considered statistically significant, while nsP > 0.05 were considered not statistically significant.
After a 24-hour culture period, CCK-8 results illustrated a significant decrease in the survival of hBMSCs in both the HT group and the HT/BSG group, with relative RGRs of hBMSCs at about 50%. In the blank control, BSG, LT, and LT/BSG groups, hBMSCs exhibited significantly higher RGRs compared to the HT and HT/BSG groups (Fig. 7b). These data reveal that elevated culture temperatures, such as 45 °C in our study, demonstrated confirmed anti-tumor efficacy in vitro, while concurrently diminishing the survival of hBMSCs, suggesting that excessive MH may negatively impact bone healing in vivo. What noteworthy was that moderate culture temperatures progressively facilitated the proliferation of hBMSCs over an extended duration of 72 h, whereas the detrimental effect of elevated culture temperatures on the survival of hBMSCs intensified, as illustrated in Fig. 7b. The Live/Dead staining of hBMSCs demonstrated no significant presence of dead cells in the blank control, BSG, LT, and LT/BSG groups, as seen by the seldom occurrence of red staining. Conversely, significant red staining regions were observed in the HT and HT/BSG groups, indicating the detrimental effects of increased culture temperatures on hBMSCs (Fig. 7c). Cytoskeletal staining revealed that hBMSCs in the HT and H/BSG groups had infrequent, distorted, shriveled, or fragmented morphologies, whereas no such morphological damage was observed in the blank control, BSG, LT, and LT/BSG groups (Fig. 7c). The results preliminarily indicated that only moderate hyperthermia promoted the proliferation of hBMSCs, whereas excessive hyperthermia inevitably inflicted damage on cells and surrounding tissue, thereby emphasizing the necessity of enhancing osteogenesis in hBMSCs and highlighting the detrimental effects of hyperthermia on cells and local tissue.
Based on the investigation of proliferation, Live/Dead staining, and cytoskeletal labeling of hBMSCs, Alkaline phosphatase (ALP) staining and Alizarin red S (ARS) staining were subsequently performed to assess the effects of moderate MH and IAM combination, concentrating on the blank control, BSG, LT, and LT/BSG groups. Following a 7-day incubation period, the positive ALP staining regions in the blank control were comparatively weak, while the positive ALP staining regions in the BSG, LT, and LT/BSG groups were markedly more pronounced than in the blank control, with the LT/BSG group demonstrating the highest intensity of ALP staining. The in vitro mineralization assay performed after 14 days of incubation indicated that the positive ARS areas in the blank control group were relatively faint. In contrast, the positive ARS areas in the BSG, LT, and LT/BSG groups were significantly greater than those in the blank control group, with the LT/BSG group exhibiting the highest ARS intensity (Fig. 7d). The results of ALP staining and ARS demonstrate that both moderate MH and IAM of BSG alone boost the differentiation and in vitro mineralization of hBMSCs, whereas their combination optimally promotes osteogenesis in vitro.
A comprehensive examination was conducted to evaluate the impact of moderate MH, IAM of BSG, and their combination on the expression of osteogenic-related genes in hBMSCs. After 7 days of culture, a notable up-regulation of osteogenic-related genes, such as ALP, RUNX2, COL-1, OCN, and OPN, was observed in the BSG, LT, and LT/BSG groups compared to the blank control. The hBMSCs in the LT/BSG group exhibited the greatest expression levels of osteogenic-related genes (Fig. 7e–i). The findings indicate that both moderate MH and IAM of BSG can augment the expression of osteogenic-related genes in human bone marrow stem cells, with their combination producing the most significant effects on these gene expressions.
The integration of moderate MH with IAM of BSG presents a therapeutic strategy for successful tumor ablation and subsequent osteogenic induction, facilitating optimal bone defect regeneration following tumor removal in clinical practice. Therefore, it is essential to clarify the biomolecular mechanisms by which moderate MH and BSG individually promote osteogenesis, as well as how their combination amplifies this process. Consequently, hBMSCs cultured for 7 days in the blank control, BSG, LT, and LT/BSG groups underwent RNA-seq. The database information and data analysis software were the same as those used in the RNA-seq analysis of OS cells (Supplementary Tables 3 and 4). Volcano plots of RNA-seq data from hBMSCs (Fig. 7j, k) revealed DEGs comprising 87 up-regulated and 123 down-regulated genes between the Control and BSG group, 143 up-regulated and 507 down-regulated genes between the Control and LT group, and 261 up-regulated and 563 down-regulated genes between the blank control and LT/BSG group. Moreover, the Venn diagram depicted the DEGs interactions among the groups (Supplementary Fig. 31), indicating that the relatively low temperature (42 °C) combined with the late-stage degradation microenvironment of BSG significantly promotes the osteogenic development and differentiation of hBMSCs.
KEGG analysis revealed that, the Hippo, Notch, calcium, and IL-17 signaling pathways in hBMSCs were up-regulated, whereas the TNF and NF-κB signaling pathways in hBMSCs were downregulated in BSG group, as compared to blank control (Fig. 7l). As well known, the upregulation of TNF signaling pathways trends to induce cell apoptosis. Thereby, it can be concluded that BSG offers dual roles in regulating the functions of hBMSCs by modulating their osteogenesis and simultaneously inhibiting cell apoptosis. Additionally, the KEGG analysis from the comparing between groups of LT/BSG and blank control (Fig. 7m) revealed that, the HIF-1, JAK-STAT, and calcium signaling pathways were significantly up-regulated, while the TNF, FoxO, and Rap 1 signaling pathways were downregulated in the LT/BSG group, as compared to the blank control. Therefore, as concluded from KEGG analysis between groups of BSG and blank control, and groups of LT/BSG and blank control, it was found that a consistent up-regulation of the calcium signaling pathways was observed across the BSG and LT/BSG groups (Fig. 7l, m and Supplementary Fig. 32a, b), and LT significantly upregulated the JAK-STAT signaling pathways in hBMSCs (Supplementary Fig. 33), whereas signal pathways such as Hippo, Notch, HIF-1, FoxO, and Rap 1 in groups of BSG, and LT/BSG only exhibited a slight fluctuation to some extent as compared to blank control (Fig. 7l, m; Supplementary Figs. 32a, b, and 33). Based on the aforementioned information, the calcium and JAK-STAT signaling pathways are selected as key points as the underlying mechanism of osteogenesis promotion of BSG and moderate MH combination.
Furthermore, the heatmap (Fig. 7n) illustrated the up-regulated genes of hBMSCs related to the calcium and JAK-STAT signaling pathways in the LT/BSG group compared to the blank control group. The JAK-STAT3 signaling pathway is crucial for the proliferation and differentiation of cells across various JAK-STAT pathways. Consequently, its role in the osteogenesis of hBMSCs influenced by moderate hyperthermia is of significant concern. Thus Western Blot analysis was conducted to assess the protein secretion of hBMSCs associated with calcium and JAK-STAT3 signaling pathways. The proteins linked to the calcium signaling pathway in hBMSCs within the BSG group, such as CACNA1G and PKC-β, exhibited significant elevation relative to the blank control group (Fig. 7o), suggesting IAM of BSG activates the Cav3.1 channel in hBMSCs to enhance their osteogenic expression. Whereas the combination of moderate hyperthermia and BSG resulted in the upregulation of proteins linked to the JAK-STAT3 signaling pathway (such as Bcl-2, STAT3, and p-STAT3) and the calcium signaling pathway (including CACNA1G and PKC-β) in hBMSCs, in comparison to the blank control and BSG groups (Fig. 7o). In conclusion, IAM production from BSG degradation leads to the up-regulation of the Cav3.1 calcium channel in the cell membrane of hBMSCs, which results in increased Ca2+ influx. Additionally, moderate MH initially activates the JAK-STAT3 signaling pathway, further promoting the osteogenic differentiation of hBMSCs (Fig. 7p). The combination of moderate MH and BSG synergistically enhances the efficient osteogenesis of hBMSCs through both the calcium and JAK-STAT3 signaling pathways.
Inhibition of IMBSs on xenograft OS in nude mice
To evaluate the in vivo inhibition of IMBSs on OS, IMBSs samples were implanted at the center of subcutaneous xenografts in nude mice. Four animal groups were designated (n = 4 mice): a blank control group (without any subcutaneous implantation), a BSG group (with BSG samples implanted subcutaneously under an AMF), a 5-MNP-BSG (+) group (with 5-MNP-BSG samples implanted subcutaneously under an AMF), and a 10-MNP-BSG (+) group (with 10-MNP-BSG samples implanted subcutaneously under an AMF). The schematic diagram for constructing the subcutaneous xenograft model using nude mice and the sample implantation was illustrated in Supplementary Fig. 34a. Fig. 8a displayed the timing of subcutaneous OS treatment. Consistent with the in vitro temperature elevation profiles and temperature threshold results of IMBSs (Fig. 3i, j), the nude mice were exposed to an AMF (15 A, 550 kHz) to observe the heating curve of MH. As demonstrated in Fig. 8b–d, both the 5-MNP-BSG (+) and 10-MNP-BSG (+) groups reached temperature thresholds within 2 min of AMF application, while the BSG group showed no temperature variation during the AMF exposure. Additionally, the heating profiles of 5-MNP-BSG and 10-MNP-BSG under AMF corresponded with the in vitro results (Fig. 3i, j).
a Timeline of xenograft OS implantation into tumors bearing nude mice and the subsequent management with MH therapy. b Schematic diagram of MH therapy. c, d Magnetic thermal imaging of IMBSs implanted in subcutaneous xenograft OS under AMF (15 A, 550 kHz), together with the corresponding temperature variation over time. e Weight variation of nude mice throughout the observation period (n = 4 mice). f Alterations in tumor volume in nude mice throughout the observation period. g Tumor weight and photos of nude mice at the conclusion of the experiment. h IHC on the expression of EMT, TNF singling pathway, NF-κB singling pathway, and apoptosis singling pathway related biomarkers after IMBSs implanted in nude mice subcutaneous xenograft OS model for 2 weeks under AMF (15 A, 550 kHz) (scale bar = 100 μm). Statistical data in d–g are presented as means ± SD with 4 replicates; Statistical significance in f, g was determined using the one-way ANOVA method with Tukey’s multiple comparisons tests. Statistical significance was defined as *P < 0.05, **P < 0.01 and ****P < 0.0001, whereas nsP > 0.05 was deemed not statistically significant.
Two days post-implantation, the identified AMF were delivered to all the subcutaneous OS-bearing nude mice for a duration of 8 min, corresponding to the time required for the implanted magnetic beads to reach the prescribed threshold temperature. AMF was provided bi-daily during a 2-week period following surgery. After each timepoint of IMBSs therapy, the body weights, together with the appearances, weights, and volumes of tumors in nude mice, were documented (Fig. 8e and Supplementary Fig. 34b). Over the course of IMBSs therapy, no significant variations in body weight were noted among the different groups of naked mice; nevertheless, substantial alterations in tumor volumes and weights were found. The tumor volumes and weights in the BSG group were smaller than those in the blank control, whereas the 5-MNP-BSG (+) and 10-MNP-BSG (+) groups demonstrated significantly reduced tumor volumes and weights compared to the BSG group (Fig. 8f, g), indicating a more potent inhibition of IMBSs therapy on tumor progression.
Figure 8h depicted graphs of immunohistochemistry staining (IHC) concerning the secretion of biomarkers associated with EMT, TNF signaling pathway, NF-κB signaling pathway, and apoptosis signaling pathway following treatments after 2 weeks. Relative to the blank control group, the positive staining regions for E-cadherin and Vimentin were more pronounced, as well as N-cadherin was weaker in the BSG group, particularly in the 5-MNP-BSG (+) and 10-MNP-BSG (+) groups. The biomarkers of TNF signaling pathway, NF-κB signaling pathway, and apoptosis pathway showed a gradient decrease in positive staining regions for Bcl-2 from the blank control group to the 10-MNP-BSG (+) group, but positive staining areas for TNF-α, and Cleaved caspase-3 exhibited a gradient rise. Moreover, Bcl-2 and NF-κB positive staining regions in the 5-MNP-BSG (+) and 10-MNP-BSG (+) groups were markedly reduced compared to the BSG group, although the positive staining regions for TNF-α and Cleaved caspase-3 were dramatically increased in relation to the BSG group. The IHC data indicated that IMBSs therapy demonstrated more OS inhibition in a nude mice subcutaneous xenograft model, with these amplified effects achieved through the activation of TNF-mediated apoptotic pathways in OS cells (Fig. 8h and Supplementary Fig. 35).
Tumor ablation of IMBSs in rat tibia in situ OS models
To systematically assessments of the tumor ablation, inhibitory effect on OS recurrence and metastasis, and modulation the afterward tumor immune microenvironment, two animal models were employed, namely the rat tibial OS backfill defect model, which assesses the inhibitory effect of IMBSs on OS recurrence and metastasis, and the tumor ablation of IMBSs in rat tibial in situ OS model, which evaluates the capacity of IMBSs to eliminate tumor and modulate the tumor immune microenvironment. The IMBSs were first implanted concurrently with OS tissue into rat tibial defects to evaluate the in situ anti-OS efficacy and bone regeneration of MH or BSG individually, as well as IMBSs therapy, with the surgical procedures depicted in Supplementary Fig. 36a. Two days after implantation, anesthetized rats were treated to an AMF (15 A, 550 kHz) to induce MH. The AMF was provided every two days for a duration of 8 min each time, as illustrated in Fig. 9a. After a treatment duration of 6 weeks, OS invasion in rat tibial defects was initially assessed using MRI. Results (Fig. 9b) indicated that, in the blank control group, OS tissue invaded the neighboring bone and knee joint, resulting in significant bone resorption in the tibia and structural damage to the knee joints. Nonetheless, tumor invasion, along with associated bone resorption and knee joint damage, was moderate in the BSG group, and significantly less pronounced in the 5-MNP-BSG (+) and 10-MNP-BSG (+) groups. Optical images of rat ex vivo tibial tissue revealed that, in the blank control group, extensive OS tissue surrounding the proximal tibia and knee joint exhibited characteristics of central necrosis. In contrast, the OS volume in tibial defects was moderate in the BSG group, while minimal or absent OS growth was observed in the 5-MNP-BSG (+) and 10-MNP-BSG (+) groups (Supplementary Fig. 36b, c). Moreover, in situ OS is particularly prone to lung metastasis, significantly reducing patient life after bone tumor removal5,6,7. Lung tissue was subsequently collected to identify the OS metastases. Supplementary Fig. 37 and Fig. 9c demonstrated that substantial metastatic lesions were present in the lung tissue of the blank control group, while the 5-MNP-BSG (+) and 10-MNP-BSG (+) groups displayed no noticeable lung metastatic lesions. Moreover, hematoxylin and eosin (H&E) staining of the lung tissue (Fig. 9c) demonstrated the presence of several regions of cancer cells, distinguished by dark-stained nuclei and elevated cell density in the blank control group, indicating a high incidence of OS metastasis to the lungs. Cancer cells with dark-stained nuclei were only identified in the pulmonary artery region of the BSG group. Conversely, no indications of cancer cells with dark-stained nuclei were observed in the H&E staining of the 5-MNP-BSG (+) and 10-MNP-BSG (+) groups. These results indicate that the creation of the IAM allows BSG to moderately reduce OS, whereas the combination of MH and IAM demonstrates the most potent tumoricidal effect and further inhibits lung metastasis and recurrence of OS.
a Timeline for the implantation of OS and IMBSs into rat tibia defects and the subsequent management with MH treatment. b MRI images of tumor progression in rat tibia defects at the conclusion of IMBSs. c H&E staining of SD rat lung metastasis of OS (black bar = 500 μm; red bar = 100 μm). d MTS of tumor progression in rat tibia defects at the conclusion of IMBSs (black bar = 500 μm; red bar = 100 μm). e, f 3D and 2D reconstructions of Micro-CT scans illustrating bone formation in SD rat femoral condyle defects following 8 weeks of IMBSs therapy. g MBAFS of bone formation in rat femoral condyle defects following 4 weeks of IMBSs therapy (black bar = 500 μm; red bar = 100 μm). h GTS of bone formation in rat femoral condyle defects following 8 weeks of IMBSs therapy (black bar = 500 μm; red bar = 100 μm).
IHC staining of the tibia with simultaneous implantation of IMBSs and OS tissue blocks revealed that E-cadherin positive staining areas exhibited an increasing trend from the blank control to the BSG group, and further to the 5-MNP-BSG (+) and 10-MNP-BSG (+) groups; conversely, Vimentin positive staining areas demonstrated a decreasing trend from the blank control to the BSG group, with Vimentin positive staining areas diminishing in the 5-MNP-BSG (+) and 10-MNP-BSG (+) groups. The TNF-α and Cleaved caspase-3 exhibited a gradient rise, whereas the positive expression of Bcl-2 was a gradient decrease. The positive expression of NF-κB exhibited an initial increase followed by a decrease. Furthermore, the positive staining regions of Bcl-2 and NF-κB in the 5-MNP-BSG (+) and 10-MNP-BSG (+) groups were significantly reduced compared to the BSG group, whereas the positive staining regions for TNF-α and Cleaved caspase-3 were substantially elevated in the 5-MNP-BSG (+) and 10-MNP-BSG (+) groups relative to the BSG group (Supplementary Figs. 38 and 39). These data indicate that IMBSs therapy provides optimal OS cytotoxicity via activating the TNF signaling pathway, thereby triggering the death of OS cells in vivo.
To evaluate the subsequent promotion of IMBSs therapy on bone regeneration following tumor eradication under simultaneous implantation of IMBSs and OS tissue blocks in tibial defects, Masson trichrome staining (MTS) was utilized. MST images (Fig. 9d) revealed that, in the blank control, significant resorption of the bone matrix was observed, accompanied by tumor tissue infiltrating and extending beyond the boundaries of the tibial defect. The BSG group exhibited limited collagen fiber encapsulation around the IMBSs implants in the tibial defect, with infrequent indications of OS diffusion observed. Significant collagen fiber encapsulation was observed surrounding the implants in the tibial defects of the 5-MNP-BSG (+) groups, along with considerable new bone growth at the center of the defect. Conversely, the 10-MNP-BSG (+) group had only minimal collagen fiber deposition, with infrequent development of new bone tissue observed. These indicated that BSG exhibits specific tumor-suppressive properties while concurrently facilitating moderate bone regeneration in the OS microenvironment. However, excessive MH may hinder local bone regeneration due to unavoidable thermal damage to normal bone tissue, despite its recognized anti-tumor efficacy. Consequently, only a moderate IMBSs can simultaneously provide enhanced overall survival inhibition and promote osteogenesis to attain optimal sequential anti-tumor effects and bone regeneration within the OS milieu.
Prior to the construction of rat in situ proximal tibia OS model, the lentivirus-loaded mCherry fluorescent protein was transduced into rat OS cells (UMR106 cells) (Supplementary Fig. 40). At the concluding of treatment, with stable mCherry expression using puromycin, an augment bioluminescence emitting from OS tissue can be detected to enable the observation of the lung metastasis of OS. Stable fluorescence expression of the UMR106 cells with the transfection of mCherry solidly verified the successful transfection of lentivirus-loaded mCherry fluorescent protein into UMR106 cells, as illustrated in Supplementary Fig. 40. Two weeks after the construction of rat in situ proximal tibia OS model, IMBSs was implanted into the core position of the in situ OS tissue, and PBS was injected into the core position of the in situ OS tissue to serve as the blank control. Thereby, four categorizations, including blank control, BSG group, 5-MNP-BSG (+) group, and 10-MNP-BSG (+) group, were built up, subjecting to an AMF two days after implantation, delivering an output current of 15 A and a frequency of 550 kHz for 8 min once daily until the therapeutic conclusion. After 4 weeks of treatment, Optical and bioluminescence images of the lung tissue (Supplementary Fig. 41a, b) illustrated that, significant fluorescence was visualized in blank control, while the weaker fluorescence was revealed from the BSG group, and almost no detectable fluorescence can be recognized in groups of 5-MNP-BSG (+) and 10-MNP-BSG (+) groups. H&E staining further revealed that OS cells predominantly localized in the pulmonary hilum vascular region of rats in the blank control, suggesting early OS metastasis. In contrast, no evidence of OS cells was observed in groups of 5-MNP-BSG (+) and 10-MNP-BSG (+) groups (Supplementary Fig. 41c), consistent with the findings from the rat tibial OS backfill defect model. These findings further indicate that BSG already exhibited certain ablation of cancer, thereby impeding the progress and lung metastasis of OS, whereas with the combination of moderate MH, more profound tumor anti-activity can be realized, enabling the complete elimination of OS, as consistent with in vitro results (Fig. 5).
Simultaneously, the quantities of tumor-associated macrophages (TAMs)54, dendritic cells (DCs), and CD8+ T cells within the cancer tissue were evaluated using flow cytometry and IHC to determine the immunomodulation of IMBSs in the tumor microenvironment following an implantation period of 4 weeks. As illustrated in the Supplementary Fig. 42, the proximal tibia is expanded due to tumor growth on its surface; upon dissection, the tumor reveals fleshy tissue accompanied by substantial hemorrhage, indicating extensive angiogenesis. The quantities of TAMs, DCs, and CD8+ T cells within the tumor microenvironment were assessed via flow cytometry, as illustrated in Supplementary Fig. 43. In comparison to the blank control group, BSG and moderate MH facilitated the transformation of M2 macrophages (F4/80+CD163+) into M1 macrophages (F4/80+CD86+), augmented the population of CD8+ T cells (CD3+CD8+), and enhanced the maturation of DCs (CD86+CD80+) within in situ OS. IHC labeling revealed a significant presence of CD86+, CD206+, and CD8+ T cells in the OS tissue of the 5-MNP-BSG group (+), in comparison to other groups (Supplementary Fig. 44).
Subsequently, the in vitro assays about the immune regulation of IMBSs on M2 macrophage reversal and DCs maturation were also conducted. RAW 264.7 cells were polarized from M0 to the M2 phenotype to emulate TAMs. After 24 h, the cell media was substituted with fresh medium with BSG extract. The medium at 37 °C devoid of BSG extract served as the blank control group, whereas the medium at 42 °C containing BSG extract constituted the LT/BSG group. The BSG extract at 37°C constituted the BSG group. Flow cytometry analysis indicated that the BSG extract facilitated the polarization of M2 macrophages towards the M1 phenotype (22.9%), with the LT/BSG group demonstrating a notably elevated percentage of CD86+ cells (25.9%) (Supplementary Fig. 45a). Simultaneously, the DC2.4 cells were grown with the BSG extract augmented with lipopolysaccharide (LPS) for 24 h. The results indicated that, compared to the blank control group, the BSG extract enhanced CD86 expression by 23.7% in DC2.4 cells. The combination of BSG and mild MH considerably improved the maturation of DCs, evidenced by a high CD86 expression of 26.4% (Supplementary Fig. 45b). Furthermore, TRAP staining of the OS tissues at the treatment endpoint revealed that, the staining intensity in the OS tissue was significantly lower in the BSG group compared to the blank control group, whereas the combination of moderate MH with BSG resulted in more profound reduction on the positive area of TRAP staining in groups of 5-MNP-BSG (+) and 10-MNP-BSG (+) groups (Supplementary Fig. 46). These findings suggest that IAM of BSG is essential for reversing abnormal tumor microenvironments, and either BSG alone or BSG combination with moderate MH can considerably inhibit both the formation and activity of tumor associated osteoclasts, consequently reducing the bone resorption and metastasis due to the progression of OS.
Bone regeneration of IMBSs in rat femoral condylar defects
Additionally, pre-cured IMBSs were implanted in rat femoral condyle defect models to further validate the osteogenic enhancement of the IMBSs therapy. This research model involved the selection of four groups: a negative control group (implanted with pre-cured commercial CaSO4), a BSG group (implanted with BSG samples), a 5-MNP-BSG (+) group (implanted with 5-MNP-BSG samples), and a 10-MNP-BSG (+) group (implanted with 10-MNP-BSG samples). Following the in vitro temperature elevation curves and temperature threshold results of IMBSs (Fig. 3i, j), two days post-implantation, animals in the four groups underwent an AMF (15 A, 550 kHz) for 8 min, administered bi-daily for 8 weeks post-surgery. Micro-CT analysis and histopathological examination of the rat femoral condyle were performed at 4- and 8-weeks of post-implantation, respectively. Micro-CT images of 2D and 3D reconstructions (Supplementary Fig. 47a and Fig. 9e, f) demonstrated that, at both 4- and 8-weeks of post-implantation, the negative control displayed significant degradation and absorption of the implants; however, this accelerated degradation did not promote new bone ingrowth, leading to a pronounced cavity devoid of bone infiltration around the implantation site. In the BSG group, BSG dramatically enhanced bone regeneration at the implantation site, resulting in the formation of ring-like new bone around the implants, with the thickness of this new bone markedly exceeding that of the negative control. The 5-MNP-BSG (+) group had the most significant new bone growth compared to all other animal groups, but new bone formation around the implant in the 10-MNP-BSG (+) group was infrequent and minimal. Bone characteristics obtained from the micro-CT analysis, such as bone volume/total volume (BV/TV) and trabecular thickness (Tb.Th), revealed that the 5-MNP-BSG (+) group exhibited the highest BV/TV and Tb.Th values compared to the other animal groups (Supplementary Figs. 47b, c and 48a, b).
Methylene blue acid fuchsin staining (MBAFS) and Goldner’s trichrome staining (GTS) were further conducted to evaluate the osteoinductivity of IMBSs therapy. At 4 weeks of post-implantation time, MBAFS results showed that rapid degradation of CaSO4 in the negative control resulted in a substantial loss in the integrity of the implant, with only minimal new bone formation presented around the implant. As for the BSG group, more profound new bone formation was demonstrated around the implants as compared with the negative control at 4 weeks of implantation time. Whereas the 5-MNP-BSG (+) group illustrated coherent and complete ring-like new bone formation surrounding the implants. However, histopathology results of 10-MNP-BSG (+) group at implantation time of 4 weeks still release signs of local thermal damage due to excessive MH, thereby presenting the relatively less new bone formation around implants (Fig. 9g). With implantation time lengthening to 8 weeks, GTS results (Fig. 9h) showed that, for CaSO4 cement group, implants had nearly completely degraded and left vast cavities with no significant continuous new bone formation. For the BSG and 5-MNP-BSG group, ring-like, coherent, and connected new bone was formed around the implants, showing osteoinduction because of the degradation of BSG in IMBSs. For the 10-MNP-BSG (+) group, much less new bone formation around implants can be detected due to thermal injury of the overwhelmed MH. Summarizing those micro-CT and histopathology results indicated that, as corresponding to our previous research33, BSG already offers efficient osteogenesis in vivo, and IMBSs therapy blooms the strongest osteogenic capacity, while thermal damages to surrounding tissue that were caused by excessive MH can even deplete bone regeneration capacity of the BSG.
Biocompatibility evaluation of IMBSs under different animal models
Biosafety is as crucial as therapeutic efficacy in assessing the clinical viability of implants used for disease treatment and remediation34. Consequently, after systematically investigating the anti-tumor efficacy and osteoinduction of IMBSs therapy in several animal models, visceral organs such as the heart, liver, spleen, lungs, and kidneys were excised and subjected to H&E staining. The results demonstrated that the tissue morphology of visceral organs (heart, liver, spleen, lungs, and kidneys), regardless of whether sourced from nude mice or SD rats, displayed a relatively uniform texture with no significant inflammation, damage, or necrosis detected (Supplementary Figs. 49,50). This provides substantial evidence that MNPs and degradation products of BSG do not adversely affect the normal physiological functions of tissues or organs.
Discussion
As a highly malignant neoplasm characterized by rapid growth and metastasis, the OS results in significant damage to bone integrity and function, as well as that of the surrounding tissue. Despite breakthroughs in treatment of OS, the 5-year overall survival rate for malignancies remains below 70%, drastically decreasing to 20 - 30% for people who are poor responders to therapies or those with metastatic tumors55. Consequently, there is an urgent need to identify innovative therapeutic approaches for enhanced management of OS. MH, regarded as a formular of green therapy, utilizes an external AMF to address its function, which positions advancements of rapid induction of substantial thermal effects, deep tissue penetration, and the treatment of larger areas, thus attracting heightened clinical interest6,7,8,9.
However, the uncontrolled warming nature often hinders the utilization of magnetothermal materials, and there is particular concern that this can lead to irreversible thermal damage to healthy tissues. Moreover, the distinct characteristics of solid tumors, including chronic hypoxia, an acidic microenvironment, and a deficient vascular system, impair the development of sensory receptors for temperature fluctuations, potentially mitigating the detrimental effects of hyperthermia on tumor tissue56,57. Thus, these inspire us to develop an innovative strategy for microenvironmental therapy for OS, incorporating adjustable temperature thresholds of implants for tumor-targeted hyperthermia and altering the tumor environment from acidic to alkaline through the degradation products of implants.
Temperature thresholds of hydrothermally derived CoFe2O4 MNPs can be adjusted by manipulating the Cr3+/Zn2+ ratio within the crystal lattice, with the underlying mechanism involving a reduction of the magnetic moment at octahedral B sites caused by the presence of Cr3+ and Zn2+. Consequently, an effective strategy to manipulate hyperthermia for tailored cancer therapy scenarios is presented. Nevertheless, the temperature threshold necessary for effective tumor eradication (>45 °C) frequently surpasses the tolerance of adjacent normal tissues and hinders bone tissue regeneration, despite the fact that tumor cells can only promptly be obliterated via coagulative necrosis or apoptosis induced by increased heat shock protein production at temperatures exceeding 45 °C58,59. Consequently, equipping moderate MH with effective tumor targeting is essential in the non-pharmacological treatment of OS and the restoration of impaired bone homeostasis caused by tumor development.
This study demonstrates that the amalgamation of MNPs (Zn0.54Co0.46Cr0.6Fe1.4O4) with specific temperature thresholds and BSG utilizing a chitosan-based glue led to the effective construction of IMBSs. These IMBSs demonstrated adequate mechanical strength and substantial operational capacity, effectively addressing the combined therapy of MH and BSG to eradicate postoperative residual tumor cells and avert potential tumor metastasis, while also promoting highly efficient in situ bone healing within an OS microenvironment. Furthermore, by manipulating the concentration of MNPs in IMBSs, elevated (45 °C) and moderate (42 °C) MH can be achieved upon exposure to AMF. This MH promotes the degradation of BSG within IMBSs, suggesting that MH contributes to the establishment of an enhanced IAM for BSG.
As previously stated60, the extracellular acidic environment is acknowledged as one of the hallmarks for advanced cancer, and this excess extracellular H+ induces adaptive selection in tumor cells, facilitates survival via metabolic plasticity, and ultimately enhances the resistance of tumor cells to harsh extracellular environments60,61. Research indicated that elevating the extracellular pH of tumor cells can suppress the activation of enzymes associated with tumor metastasis, hindering the breakdown and remodeling of the extracellular matrix, therefore obstructing tumor invasion and metastatic activity62. Furthermore, biomolecular mechanism research stated that modifying the acidity and alkalinity of the tumor microenvironment might impede the function of acidic receptors (GPCRs) on macrophage surfaces, hence obstructing the inhibitory influence of the downstream cAMP-ICER signaling cascade on pro-inflammatory genes such as TNF-α63. This impedes macrophage chemotaxis towards pro-cancer non-inflammatory states (downregulating the expression of pro-cancer factors such as TGF-β and IL-10), prompts macrophages to differentiate into anti-cancer pro-inflammatory cells, and inhibits tumor cell biological activity via the secretion of inflammatory factors including TNF-α, IL-1β, and iNOS, ultimately suppressing tumor growth and metastasis while inducing tumor regression64. Thus, establishing a localized alkaline microenvironment by implanted materials to suppress tumor activity and metastasis presents opportunities for non-pharmacological therapy of solid tumors. Therefore, following the implantation of IMBSs, the enhanced IAM of BSG, as a result of hyperthermia, is highly expected to be employed for the eradication and suppression of localized malignancies during the initial contact phase of the moderate IMBS therapy. As reported by Wang and her coworkers, an integrative anti-tumor and bone-repairing scaffold was developed by applying a photothermal treatment (PTT) composite MoS2-PLGA film onto the surface of BSG. The scaffolds significantly diminish the viability of OS cells in vitro and impede tumor formation in subcutaneous tumors in nude mice. Moreover, scaffolds can induce the osteogenic development of rat bone mesenchymal stem cells (rBMSCs) and facilitate bone regeneration in critical-sized calvarial defects65. Nonetheless, the role of BSG in OS metastasis inhibition and the repair of tumorous bone defects has not been comprehensively validated. Furthermore, the involved biological mechanisms through which IAM of BSG influences the proliferation and metastasis of OS also remain unexamined. What is noteworthy is that this article focuses on addressing the treatment of bone abnormalities following the excision of OS. After engagement with the OS, the tumor’s acidic microenvironment was alleviated by IAM of BSG in IMBSs, hence reducing the malignancy and metastasis of OS. Following the impairment of BSG, the ill OS cells demonstrated less tolerance to hyperthermia. Consequently, the combination of long-term IAM with BSG demonstrated remarkable thermal apoptotic effects on OS, both in vitro and in vivo, whereas moderate MH alone exhibited negligible or highly ineffective anti-tumor efficacy. Moreover, the anti-tumor effects of the 5-MNP-BSG (+) group are analogous to those of the 10-MNP-BSG (+) group, indicating that, in addition to the degradation of BSG, the ionic permeability and alkaline microenvironment confer comparable OS suppression in moderate MH to that observed in elevated MH. A further advantage of the moderate MH of IMBSs is the possible mitigation of harm to adjacent healthy tissues. Furthermore, the synergistic anti-OS and osteogenic effects of BSG and moderate MH were further corroborated using subcutaneous OS models in nude mice, an in situ OS model in rats, and an in situ bone defect model. In contrast to Wang et al., our study prioritizes the utilization of IAM produced by degradation of BSG to sequentially modulate the initial anti-tumor effects and subsequent osteogenic stimulation of the implant. Concurrently, the IMBSs with a magnetothermal threshold markedly diminish the danger of harm to adjacent healthy tissues. Consequently, the IMBSs present a viable avenue for the therapy of OS-related bone abnormalities, with potential for swift clinical translation.
Furthermore, to clearly elucidate the biological mechanism of BSG degradation in combination with moderate MH against OS, RNA-seq analysis of the 143B cells following BSG and IMBSs therapy was conducted. The activation of TNF and NF-κB signaling pathways were notably significant and consistently persisted during the treatment of OS cells with BSG solely or BSG combination with moderate MH, indicating the IAM of BSG fundamentally activated the TNF signaling pathways in OS cells. As well known, TNF and the NF-κB signaling pathways exhibit a crucial relationship in the progression of tumors47. Deeper detection reveals that the TNF pathway exerts its effects, such as pro-apoptosis and inflammatory response, mainly through two receptors, TNFR1 and TNFR2, which were activated by both soluble and transmembrane-bound TNF-α. Therefore, TNF signaling pathway possesses the capability to activate the caspase family cascade reaction, thereby facilitating the apoptosis of tumor cells47. With the activity of TNF, the NF-κB becomes active in parallel through the IKK complex, which Phospho-IκB (the inhibitory protein of NF-κB), thereby releasing NF-κB to enter the nucleus and activate transcription to inhibit apoptotic processes66. The released NF-κB thus contributes to the proliferation, migration, and metastasis of tumor cells67. This study demonstrated that, following the engagement of tumor microenvironment both in vitro and in vivo, the IAM of BSG initially induced the pathological status of OS cells through activation the TNF signaling pathway. Nonetheless, its comparatively weak effect is insufficient to induce cell apoptosis, as the feedback activation of the NF-κB signaling pathway promotes the survival of OS cells in the BSG degradation microenvironment. With the combination of moderate MH, expression of the TNF signaling pathway in OS cells can be enhanced, enabling the irreversible apoptosis to OS cells. Therefore, it is proposed that the IAM of BSG functions as a trigger for apoptosis in OS cells, whereas moderate MH therapy functions as a promoter of apoptosis in OS cells.
Research on primary and metastatic bone cancers reveals a relationship akin to seed and soil interaction involving tumor cells, osteoblasts, and osteoclasts. Tumor cells specifically release proteins such as osteopontin and osteonectin, adopting features akin to bone cells, a process termed bone matrix production, which improves the adherence, proliferation, and survival of tumor cells at bone locations68. Simultaneously, colonized tumor cells release parathyroid hormone-related peptide, which activates osteoblasts to generate NF-κB ligand, thereby enhancing osteoclast-mediated bone resorption68. The secretion of bone matrix growth factors, triggered by bone resorption in the tumor microenvironment, can promote tumor proliferation, hence intensifying bone resorption and degradation. Thus, the bone resorption microenvironment creates a soil environment favorable for the adherence and proliferation of tumor cells, whereas the tumor microenvironment supplies several stimulatory elements for bone resorption68. The interaction and reciprocal enhancement of these two environments facilitate tumor growth and migration within and adjacent to bone tissue, leading to a high recurrence and lung metastasis rate post-OS surgery and presenting considerable challenges for the regeneration and repair of tumor-associated bone defects68,69. Consequently, the investigation into whether tumor progression induced osteoblast activation and resulted in significant secondary bone resorption was carried out using TRAP staining of the tumor tissue. At the treatment endpoint, TRAP staining-positive area in the OS tissue was significantly lower in the BSG group compared to the blank control group, whereas the combination of moderate MH with BSG resulted in more profound reduction on the positive area of TRAP staining in groups of 5-MNP-BSG (+) and 10-MNP-BSG (+) groups. These findings suggest that the IAM of BSG, and moderate MH can rectify the distorted seed and soil relationship within the OS, thereby promoting the reconstruction of an alkaline microenvironment that inhibits OS metastasis induced by tumorous osteoclasts17,18. In addition, the inhibition of tumor cell activity and malignance, along with the effective promotion of directed osteogenic differentiation of stem cells, is crucial for mitigating tumor metastasis and restoring bone homeostasis within the tumor microenvironment.
By designing the network formed by BSG and inducing elements with the function of regulating body metabolism into BSG’s network, the chemical reactivity and degradation rate of the BSG can be customized to accommodate the diverse microenvironmental requirements for tissue regeneration33. Studies indicate that this IAM can facilitate the biomineralization of BSG through the reaction of Ca2+ and PO43- to form HA, while simultaneously activating bone metabolism pathways, including BMP-smad, MAPK, and Wnt/β-catenin, thereby regulating the osteogenic and angiogenic differentiation of mesenchymal stem cells70. Our previous research have shown that integrating BSG into commercial PMMA cement markedly improves osteointegration and promotes new bone development around implants in traumatic, osteoporotic, or even infectious milieu34,71. In this work, the preliminary test on cytotoxicity of IMBSs to hBMSCs showed that, only after 2 weeks of degradation period in vitro that simulate the dynamic circulation in vivo, the extracts of IMBSs can conform to the requirement of cytotoxicity to hBMSCs under international standard biological evaluation (ISO 10993). Thus, accordingly, we diluted the extraction solution of IMBSs with a specific ratio to meet the subsequent evaluation of the activity and osteogenic potential of hBMSCs. Subsequently, a controlled environment was established to replicate standard culture conditions and moderate to elevated MH culture conditions, with precise temperature gradients of 37 °C, 42 °C, and 45 °C, to assess the impact of hyperthermia induced by AMF on the osteogenesis of hBMSCs. Additionally, the aforementioned temperature gradient cultivation environment was synchronously assembled using the specific diluted extracts of IMBSs to replicate the IMBSs therapy in vitro. Results depicted that moderate MH has increased the osteogenic activity of hBMSCs as evidenced by the upregulation of ALP, RUNX2, OCN, and others, whereas the elevated MH (45°C) inhibited the viability of hBMSCs. Moreover, even though the IAM of BSG alone had already significantly promoted proliferation, osteogenic differentiation, and biomineralization of hBMSCs, the IMBSs therapy still illustrated the optimal promotion of the viability and osteogenesis of hBMSCs.
On the basis of the modulation of osteogenesis of hBMSCs, it is then of great necessity to conduct the RNA-seq to deeply elucidate the biological mechanism involved in the processes of osteogenic expression of hBMSCs when cultured with moderate MH, BSG, and their combination. Analysis of RNA-seq data revealed that the IAM of BSG can notably enhance the calcium signaling pathway in hBMSCs, especially the upregulated activity of Cav3.1 calcium channel. The Cav3.1 calcium channel is categorized in T-type Cav3 calcium channels family recognizing for their transient activation, which comprise a family of voltage-gated calcium ion channel proteins72,73. Therefore, augmented influx of Ca2+ into cells is crucial for the osteogenic differentiation and mineralization of hBMSCs. Research further elucidates that, the JAK-STAT signaling pathway significantly contributes to biological processes like cell proliferation, differentiation, death, and immunological control. The STAT family comprises transcription factors that govern gene expression in the cell nucleus, including STAT1, STAT2, STAT3, STAT4, STAT5, and STAT6, and within JAK-STAT signaling pathways, the JAK-STAT3 pathway serves as a primary mechanism for cell proliferation, differentiation, and migration74. In this work, it was revealed that the IAM of BSG promotes the osteogenic development and mineralization of hBMSCs by facilitating cellular Ca2+ consumption, while moderate MH further increases this process by activating the JAK-STAT3 signaling pathway, demonstrating their synergistic effect on osteogenic promotion of the BSG and moderate MH combination. This study revealed that moderate administration of MH and BSG combination therapy yielded significant anti-OS effects in both xenograft and in situ tibia OS models, while also mitigating severe thermal damage linked to elevated MH levels, thus facilitating bone regeneration in both in situ OS and standard femoral condyle defect models.
Beyond the osteogenic promotion, the IAM established by degradation of BSG can synchronously influence the tumor immune microenvironment, such as through macrophage polarization, thereby facilitating the recruitment and differentiation of tissue repair-related cells by creating a conducive immune environment. Pan et al. demonstrated that Sr/Cu-BSG bone cement facilitates the spontaneous regulation of macrophage polarization, angiogenesis, and osteogenesis in the repair of critical bone defects33. Meanwhile, the research conducted by Ding et al. also demonstrates that the optimal synergistic effects of B and Sr elements in BSG modulate M2 macrophage polarization from the spleen and enhance bone formation in defects, indicating that BSG can influence systemic immune responses to facilitate local bone regeneration75. In alignment with prior studies, the effects of BSG and moderate MH on immune regulation were also assessed both in vitro and in vivo. The combination of BSG and moderate MH can synergistically enhance the polarization of M2 macrophages towards the M1 phenotype, thereby reversing IMBSs over TAMs. In vivo studies in this work further revealed that the combination of BSG and moderate MH resulted in an increased population of cytotoxic T cells (CD8+ T cells) within OS. Previous report illustrates that exertion of tumor elimination for CD8+ T cells primarily relies on DCs, while various immunosuppressive cytokines present in tumors, such as TGF-β and IL-6, can reduce the efficacy of DCs76. Therefore, an increased population of CD8+ T cells within OS positively indicates the mature of DCs without suppressing by tumorous immunosuppressive cytokines, as consistent with the enhanced maturation of DCs liberating from the combination of BSG and moderate MH also enhanced the maturation of DCs both in vitro and in vivo.
In general, utilizing IAM of BSG to prioritize disrupting the normal metabolism of tumor cells, and up regulating their inflammatory response to initiate the intercellular self-apoptosis procedures of tumor cells, illustrates a feasible strategy to boost the original negligible or highly ineffective anti-tumor efficacy of moderate MH, and ultimately accomplish successfully preventing the recurrence and metastasis of OS while efficiently restoring osteogenic and osteoclastic equilibrium at the site of the tumor-induced bone defect, maintaining acceptable biological safety. Furthermore, this dysfunction addressed by IAM of BSG shows the high potential in indiscriminately torturing different kinds of tumor cells, thereby augmenting killing functions for lots of advanced tumor treatment technologies such as piezoelectric therapy, sonodynamic therapy, photothermal therapy, and photodynamic therapy, illustrating the synergetic effects on a broad-spectrum anti-tumor scenario.
Nevertheless, this study also possesses shortcomings that require attention in future systematic investigations. First, the one-step treatment for bone tumor ablation and related defect regeneration seeks to avoid side effects of chemotherapy by utilizing macroscopic implant materials as devices for moderate MH and BSG combination therapy. However, that suppression on OS activities of IMBSs is limited to the vicinity of the implant and is not possible to precisely track and kill tumor tissues or cells that are farther away from the implant material, or those that have metastasized to other organs. So, future research should focus on creating a nano-delivery system using BSGs that can precisely target tumor locations, effectively kill tumors, and simultaneously enhance bone regeneration, making OS easier to diagnose and treat tumors. Secondly, this study found that the magnetic heat conversion effect promotes the degradation, ion release, and biomineralization of BSGs within the IMBSs matrix, while also increasing the pH of the soaking solution. The exact mechanism by which the magnetic heat conversion effect facilitates these activities is still ambiguous and requires additional rigorous exploration. Thirdly, the IAM from BSG and moderate MH can influence M2 macrophage polarization, DC maturation, and T cell activity. Therefore, future research must focus on elucidating the molecular mechanisms that govern this regulation to enhance the development of tumor-immune-targeted therapies. It is also crucial to understand the regulatory role of BSG in OS lung metastasis mediated by tumor-osteoclasts. The fourth, despite using diverse models such as subcutaneous tumors in nude mice, rat tibial in situ bone tumors, and rat femoral in situ bone defects to assess the biological safety and efficacy of the previously mentioned treatment strategy that combines moderate MH and BSG, these models fail to accurately replicate human OS surgical resection and the subsequent processes of bone defect regeneration and repair.
Consequently, interdisciplinary collaboration is essential to authentically replicate the clinical treatment process and cycle of OS, as well as to precisely assess the therapeutic effects of moderate MH and BSG combination on tumor ablation and bone regeneration. We expect a comprehensive examination and resolution of these difficulties to enhance treatment methods for bone cancers and reinforce the pertinent theoretical foundations of the bone tumor microenvironment. In the future, this will be very helpful for making non-invasive or minimally invasive tumor treatment methods that are based on the functional design of bioactive materials.
In conclusion, IMBSs is considered an innovative and efficient approach for preventing and treating tumor recurrence and metastasis in postoperative bone deficiencies caused by OS. By establishing enhanced biosafety, BSG combination can considerably lower the temperature threshold required for MH therapy, while also facilitating osteogenic regeneration and immune modulation of tumorous bone defects through moderate MH stimulation, hence augmenting osteogenesis. Additionally, validating that BSG can effectively treat OS and figuring out how IMBSs work to fight OS and help bones heal will have a big effect on how IMBSs can be used to mitigate tumor recurrence and metastasis in bone abnormalities caused by OS after surgery. Primarily, due to its unique biological characteristics, the non-pharmacological anti-OS approach of BSG serves as a superior clinical alternative to PMMA-based implants for the reconstruction of tumor-associated bone abnormalities. Overall, the IMBSs, which are made by mixing a specific amount of MNPs with BSG, offer a promising and useful way to reduce the recurrence and metastasis of OS after surgery and speed up the healing of bone defects. This study focuses on using the important anticancer microenvironment created by BSG’s degradation as an effective way to lower the temperature needed for MH therapy while increasing osteogenic activity. These results are meant to help with the main problems of tumor recurrence and metastasis after OS surgery, as well as the healing of bone defects caused by tumors in real life.
Methods
Ethics statement
All experimental techniques involving mice and rats were received the approval from the Animal Ethics Committee of Shenzhen Institutes of Advanced Technology, Chinese Academy of Sciences (approval number: SITA-IACUC-200401-YYS-CX-A1220-01). The tumor burden in this study was controlled within the following ranges: mouse tumor diameter ≤ 20 mm with a volume ≤ 2000 mm3; rat tumor diameter ≤ 40 mm with a volume ≤ 4000 mm3. During the study, the body weight and tumor growth of the animals were monitored daily. Once the humane endpoint was reached (e.g., mouse tumor diameter ≥ 15 mm or body weight loss ≥ 20%), euthanasia was immediately performed. This procedure ensured compliance with the standards specified in the NIH Guide for the Care and Use of Laboratory Animals. Animals, including mice and rats, were randomly allocated to several experimental groups. The investigators examining the histology were unaware of the treatment assignments for the mice and rats. All in vitro and in vivo analysis were predicated on objectively quantifiable data, with the precise number of animals and experimental repetitions delineated in the figure legends.
Fabrication of BSG
BSG with a composition of 6 mol.% Na2O, 8 mol.% K2O, 8 mol.% MgO, 22 mol.% CaO, 54 mol.% B2O3, 2 mol.% P2O5 was fabricated by the regular high-temperature melting method, which is described briefly as follows. The above components were weighed corresponding to carbonate, boric acid, silica, and phosphate (Analytical grade; China National Pharmaceutical Chemical Reagent Co., Ltd., Shanghai, China), and then homogeneously mixed in a 3D mixer (GH-5 L, Range Machinery Co., Ltd., Jiangyin, China) at 300 rotations/min for 30 min. The mixture was then transferred into a platinum crucible and melted in a muffle furnace at 1200°C for 1 h. Subsequently, the resulting molten glass was poured into an ice/water mixture and quenched to form BSG coarse particles. With further processing involving crushing, ball milling, and sieving, BSG particles with a size of less than 20 μm were acquired. The actual composition, morphology, and phase of BSG (n = 3 independent experiments) were characterized using ICP-MS spectroscopy (Optima 7000DV, PerkinElmer, Waltham, USA), SEM (Hitachi, Japan), FT-IR spectroscopy (Thermo Fisher Scientific, USA), and XRD (D8A25; Bruker, Germany), respectively.
Synthesis and characterization of MNPs
It was previously reported that, as featured in inverse spinel structure, CoFe2O4 exhibits a diverse range of applications across fields including magnetism and electricity. By attenuating the superexchange interaction between the A and B sites of CoFe2O4, its Curie temperature and magnetocaloric transition temperature can be conveniently modulated16,30. Thereby, it makes the reality for endowment and adjustment on temperature threshold of CoFe2O4 through the manipulation of the proportions between non-magnetic chromium (Cr3+) and zinc (Zn2+) ions in the crystal lattice to adapt to the individualized needs in different pathological microenvironments30. Thereby, serial MNPs with the composition of ZnxCo1-xCr0.6Fe1.4O4 (Supplementary Table 5) were synthesized by hydrothermal reaction in this work. In brief, the precursor salts employed in the hydrothermal synthesis of cobalt ferrite nanocrystals were CoCl2·6H2O, ZnCl2, CrCl3·6H2O, and FeCl3·6H2O, as well as a ≥ 98 wt.% NaOH (Aladdin, China) solution, which acted as the precipitant agent. All those reagents were analytical grade and purchased from China National Pharmaceutical Chemical Reagent Co., Ltd. Stoichiometric amounts of CoCl2·6H2O, ZnCl2, CrCl3·6H2O, and FeCl3·6H2O, were added to an excess of the above NaOH solution and simultaneously mechanically stirred under room temperature for 30 min to achieve complete reaction. Then, the above mixture was placed in a hydrothermal reactor and reacted at 250 oC for 4 h. After the furnace cooled to room temperature, the reaction mixture was centrifuged at 1500 x g for 10 min. Then, the precipitated products were rinsed with anhydrous ethanol 3 times, dried in an oven, and ultimately stored in a vacuum moisture-proof box. The actual element composition, morphology, and phase of MNPs (n = 3 independent experiments) were determined by TEM, EPMA, and XRD, respectively, with test details presented in Fig. 2c and Supplementary Fig. 3.
TEM testing
In brief, a 5 mg sample was added to 1.5 mL of chromatography-grade ethanol and dispersed uniformly using an ultrasonic device for 5 min. A 20-microliter aliquot of the well-dispersed suspension was pipetted and dropped onto a TEM copper grid coated with a support film. The grid was then placed under an infrared drying lamp for 10 min and allowed to cool to room temperature. Under a microscope, the dispersion uniformity of the sample on the grid was checked. Once confirmed, the prepared copper grid with the sample was loaded onto the TEM sample holder for testing.
EPMA testing
Samples were coated with a thin nanolayer of Pt to enhance conductivity. A flat area of the sample was then selected for testing with the following parameters: a voltage of 20 kV, a current of 20 nA, a beam spot diameter of 1 μm, and a collection time of 10 s. Secondary electron imaging was employed to obtain low- and high-magnification morphological images. Additionally, the excited characteristic X-rays were collected by an X-ray spectrometer to obtain high-resolution and high-precision elemental content and distribution maps.
XRD testing
According to the industrial standard of China “JY/T 0587-2020 General Rules for Polycrystalline XRD Methods”, the well-ground and dried powder sample was evenly spread on the sample stage. Bragg diffraction of the powder was conducted using Cu Kα X-rays with a wavelength of 0.154 nm, excited by the X-ray tube. Parameter settings included a Cu target tube voltage of 40 kV, tube current of 40 mA, and an X-ray wavelength of 0.154 nm. The scan was performed over a range of 5° - 95° with a scanning speed of 5°/min and a step size of 0.02°, resulting in an XRD spectrum that shows the diffraction intensity distribution as a function of angle.
The magnetothermal conversion and temperature thresholds of MNPs
100 mg of MNPs were placed into an AMF with an output current of 20 A and a frequency of 550 kHz, and the real-time temperature changes of those MNPs were monitored using an infrared thermometer (FLIR, Forward-looking Infrared Technology, China). The actual compositions of MNPs were listed in Supplementary Table 5.
Preparation and characterization of IMBSs
Preparation of IMBSs
IMBSs, with detailed compositions listed in Supplementary Table 1, were constructed by bonding BSG and specific MNPs with a glue. The glue was prepared according to our previous research33, with its composition details listed in Supplementary Table 1. The surface morphology, phase, and composition of the IMBSs (n = 3 independent experiments) were analyzed by SEM, XRD, and FT-IR, respectively. The test details were presented in Fig. 2d, g, and Supplementary Fig. 6.
FT-IR spectroscopy testing
The chemical characterization of the surface of the aforementioned samples was characterized using an FT-IR spectrometer. The samples were prepared using the KBr pellet method. Initially, 5 mg of the sample was finely mixed with 250 mg of pure KBr and placed uniformly in a model. The die was then gradually pressurized up to 20 MPa using a hydraulic press to compress the mixture into a transparent thin pellet. Subsequently, the FT-IR transmission mode was utilized to measure the infrared absorption spectrum of the pellet.
SEM testing
Prior to testing, the sample was desiccated at a temperature of 60°C for about 30 min. Subsequently, the sample was applied to a carbon coating to mitigate charge accumulation. The prepared sample was placed on the sample stage, and the vacuum pump was activated to evacuate the chamber. The secondary electron imaging analysis encompassed: resolution (0.8 nm at 15 kV, 1.6 nm at 1 kV); magnification range (10x to 106); accelerating voltage (0.02 kV to 30 kV); probe current (4 pA to 20 nA); sample chamber dimensions (358 mm in diameter and 270.5 mm in height); an automated 5-axis optimized centering specimen stage (tilting from 5° to 60°); working distance (2 mm to 24 mm); and accelerating voltage (10 - 15 kV).
Rheology properties
The rheological alterations throughout the curing process of IMBSs were examined to elucidate the influence of MNPs on the setting properties of the IMBSs. The paste of IMBSs was examined over time at a constant angular frequency of 10 rad/s using a rheometer (MCR 302, Anton Paar, Austria) with the same loading method settings. The IMBSs paste was extruded from the cartridge via an affixed static mixing nozzle, which effectively combined the two components. Upon ejection from the mixing nozzle, the contents of the two cartridges were completely blended, initiating the polymerization reaction. The G’, G”, and tan δ (G”/G’) were measured over time. The gel point of IMBSs, defined as the intersection of the storage modulus and loss modulus, was also recorded. Furthermore, dynamic strain scanning tests and dynamic angular frequency scanning tests were conducted35.
Curing time
The curing time of pre-cured were evaluated utilizing a Vicat apparatus (Wuxi Construction Co., Ltd., China) in accordance with previously documented methodologies33, with a concise summary provided below: Subsequent to comprehensive mixing, the IMBSs were promptly put into a bespoke stainless steel mold with a diameter of 30 mm and a height of 10 mm. Subsequently, the needle of the Vicat device was permitted to descend vertically and unobstructively into the IMBS, with the curing period of the IMBS defined as the duration during which the needle’s penetration into the IMBS is less than 1 mm (n = 3 independent experiments).
Injectability
After thorough mixing, the IMBSs were quickly placed into a 5 mL medical syringe (Kindly Medical Devices Co., Ltd, China). Subsequently, the IMBSs slurries were extruded from the syringe smoothly and gently using bare hands, ensuring full expulsion. The injectability of the IMBSs is calculated using the formula: I = [(M0 - M1) / (M0 - M)] × 100%, where M denotes the weight of the empty syringe, M0 signifies the weight of the syringe filled with IMBSs, and M1 represents the weight of the syringe after extruding the IMBSs (n = 3 independent experiments).
Compressive strength
Following a comprehensive mixing process, the pre-cured IMBSs were promptly placed into a stainless mold and allowed to cure for a duration of 24 h. Subsequently, pre-cured IMBSs measuring 6 mm in diameter and 12 mm in height underwent compressive strength testing utilizing a universal testing machine (ZQ-990LA, Instrument Technology Co., Ltd., China) at a descending velocity of 1.0 mm/min (n = 3 independent experiments).
Magnetothermal conversion of IMBSs
Real-time temperature profile of IMBSs with duration time
Pre-cured IMBSs with diameters of 5 mm and heights of 3.5 mm were placed in 24-well plates, each containing 0.6 mL of PBS (Haiclone, China) to ensure slight coverage of the upper surface of the IMBSs sample. Before conducting the tests, the surfaces of the pre-cured IMBSs were meticulously polished using sandpaper. Upon activation of the AMF, an infrared thermometer (FLIR, Portland, USA) was promptly utilized to observe the real-time temperature rise of the pre-cured IMBSs at output currents of 10 A, 15 A, 20 A, and 25 A, maintaining a frequency of 550 kHz across varying duration times. The temperature thresholds for the pre-cured IMBSs were documented as well (n = 3 independent experiments).
Hysteresis loop
The vibrating sample magnetometer (VSM) (Quantum Design MPMS SQUID, USA) was employed to perform M-H curve measurements at a constant room temperature of 25 °C. A 5 mg sample of dried powder or a thin film of appropriate dimensions (not exceeding 3 mm) was directly placed onto the VSM to examine the changes in magnetization intensity of the sample.
The magnetothermal stability of during alternating cycles of AMF activation and deactivation
Pre-cured IMBSs measuring 5 mm in diameter and 3.5 mm in height were positioned in 24-well plates, with 0.6 mL of PBS added to each well to provide a slight coverage over the upper surface of the IMBSs sample. Before conducting the tests, the surfaces of the pre-cured IMBSs were meticulously smoothed with sandpaper. During three cycles of AMF (20 A, 550 kHz), the real-time temperature variations of the pre-cured IMBSs were documented using an infrared thermometer (n = 3 independent experiments).
Biomineralization and ions release of IMBSs
Weight loss and biomineralization
IMBSs that were pre-cured and weighted, featuring diameters of 10 mm and heights of 3.0 mm, were immersed in 25.1 mL of PBS (the PBS volume was determined based on reference77) within sterile polyethylene bottles at an incubation temperature of 37 oC for a duration of 28 days (n = 3 independent experiments). The 5-MNP-BSG (+) and 10-MNP-BSG (+) groups were subjected to magnetothermal treatment for 30 min daily in an AMF (20 A, 550 kHz). At the designated time intervals, IMBSs were retrieved and carefully rinsed with deionized water before being dried at 90 °C. The weight loss of IMBSs was calculated by dividing the weight difference before and after soaking by the weight before soaking. The surface morphology, phase, and composition of the IMBSs were examined using SEM equipped with EDS mapping, XRD, and FT-IR spectroscopy.
pH measurement of PBS and the associated cumulative ion release
Following the procurement of IMBSs with diameters of 10 mm and heights of 3.0 mm, these samples were immersed in 25.1 mL of PBS for durations of 1, 3, 7, 10, 14, 21, and 28 days. Subsequently, the PBS was collected and centrifuged to isolate the supernatant. The pH value of PBS was assessed using a pH meter (FiveEasyPlus™, METTLER TOLEDO, Shanghai, China), while the cumulative release of ions (BO33-, Ca2+, Fe3+, Co2+, and Zn2+) was quantified through ICP-MS analysis. The 5-MNP-BSG (+) and 10-MNP-BSG (+) groups received magnetothermal treatment for 30 min daily in an AMF (20 A, 550 kHz) (n = 3 independent experiments).
Dynamic ion release in PBS
To replicate the dynamic circulatory environment in vivo, pre-cured IMBSs with diameters of 10 mm and heights of 3.0 mm were immersed in 25.1 mL of PBS for a duration of 28 days, with the PBS being refreshed every 2 days. The 5-MNP-BSG (+) and 10-MNP-BSG (+) groups received magnetothermal treatment for 30 min daily in an AMF (20 A, 550 kHz). At designated intervals, the soaking medium was collected and subjected to centrifugation to isolate the supernatant. The dynamic release of ions (BO33-, Ca2+) was subsequently analyzed utilizing ICP-MS (n = 3 independent experiments).
In vitro the effects of IMBSs on the viability of OS cells
OS cell culture
The human OS cell line (143B) and the rat OS cell line (UMR106), have been authenticated and tested for mycoplasma, were obtained from CellCook (Guangzhou, China). All cells were cultured in DMEM media supplemented with 10% fetal bovine serum (FBS) (Thermo Fisher Scientific, USA) and 1% P/S, at 37 °C in a humidified atmosphere containing 5% CO2.
The viability of OS cells
The viability of OS cells was initially assessed through CCK-8 assays. It was understood that only IMBSs under AMF could exhibit MH and that the tumor suppression associated with MH fundamentally depends on the thermal response induced by IMBSs in the presence of AMF. To achieve this, a cell incubator was employed to systematically create culture temperature gradients (37, 42, and 45 °C) to simulate MH, and conducted experiments to assess how these temperature gradients influence the viability of 143B and UMR106 cells. Cells at a density of 2.0 × 105 were cultured in 500 μL of DMEM with 10% FBS in a 24-well plate, followed by incubation under temperature gradients (37, 42, and 45 °C) for 6 h (n = 3 independent experiments).
To evaluate the effects of IAM of BSG in IMBSs on the viability of OS cells, extracts from the BSG, 5-MNP-BSG, and 10-MNP-BSG groups were prepared following the protocols outlined in ISO 10993, which are briefly described as follows: The IMBSs, measuring 10 mm in diameter and 3.0 mm in height, were immersed in DMEM medium enriched with 1% P/S at a concentration of 0.2 g/mL. The samples were subsequently incubated in a shaker at 37 °C for a duration of 24 h. Following the filtration process, the extract was gathered and preserved for subsequent applications. Following this, an equal volume of DMEM medium enriched with 1% P/S was introduced, which were then incubated in a shaker at 37 °C for another 24 h. The procedure was carried out repeatedly, with extracts gathered from the identical IMBSs on a daily basis until the 28th day. Subsequently, cells at a density of 2.0 × 105 were cultured using extracts from IMBSs over a period spanning from the 1st to the 10th day. Following a 24-hour culture period in a 37 °C incubator with 5% CO2, CCK-8 reagent was introduced at a dilution of 1:10. After an additional 1.5 h, the absorbance was then measured at 450 nm using a Microplate reader (ThermoFisher Scientific, USA).
To assess the impacts of IMBSs therapy on the viability of OS cells, a cell density of 2.0 × 105 was established, with pre-cured IMBSs (3.5 mm in diameter and 5 mm in height) cultured in a 24-well plate (n = 3 independent experiments). Following an incubation period of 2 h, the AMF was activated with output currents of 20 A and a frequency of 550 kHz, maintained for durations of 1, 3, 5, 8, and 12 min to deliver IMBSs therapy to OS cells. At the endpoint of treatment, 50 μL of CCK-8 reagent were added to the medium respectively, and were further incubated for 1.5 h. For CCK-8 assay, the absorbance of the culture medium in each well was measured at a wavelength of 450 nm, and viability of OS cells was calculated using the formula: (Fluorescence intensity in the experimental group - fluorescence intensity in the blank group) / (Fluorescence intensity in the blank control group - fluorescence intensity in the blank group) × 100%. Through a thorough examination of the impacts of MH, IAM of BSG, and IMBSs therapy on the viability of OS cells, the aim was to refine the group settings and identify the optimal AMF application parameters for subsequent systematic studies regarding the anti-tumor properties of IMBSs.
In vitro comprehensive investigation of the anti-OS effects of IMBSs
Cell culture
To systematically evaluate the anti-tumor activity of IMBSs in vitro, 143B cells were cultured with pre-cured IMBSs in DMEM medium supplemented with 10% FBS and 1% P/S under AMF with output currents of 20 A and frequency of 550 kHz for 8 min, a settled AMF application parameter that constructed on the basis of the section of “In vitro the effects of IMBSs on the viability of OS cells” The entire culture environment was maintained at 37°C within a humidified atmosphere containing 5% CO2.
Cell morphology
Following culture with IMBSs and exposure to AMF for 8 min, the OS cells were incubated for 2 h. The cell culture plates were positioned beneath an inverted optical microscope (Olympus Optical Technology, Japan) for detailed observation and photography (n = 3 independent experiments).
Alma blue staining
Following culture with IMBSs and exposure to AMF (20 A, 550 kHz) for 8 min, the harvested OS cells were then incubated for 2 h. Subsequently, Alma blue reagent (1:10) was introduced to the medium, and the aforementioned culture systems were incubated for an additional 2 h. Optical images of alma blue staining in each well were captured (n = 3 independent experiments).
Colony formation assay
Following culture with IMBSs and exposure to AMF for 8 min, the harvested OS cells were further incubated in a 6-well plate for 14 days with continuous shaking to ensure even cell dispersion throughout the incubation period (n = 3 independent experiments). Following a 14-day period, the culture medium was discarded, and the cells in each well underwent two rinses with PBS. After fixation using 4% paraformaldehyde (PFA) for 15 min and dehydration through a gradient ethanol series, the collected OS cells were stained with a 0.1% Crystal Violet solution for 10 min, followed by three washes with deionized water. Areas with over 50 positively stained cells were designated as colonies, and optical images of the colony formation were captured.
Wound healing assay
Initially, a small wound area was established in the 90% confluent monolayer of cells by employing a 10 μL pipette tip to create a lengthwise stripe. Photomicrographs of the cells at this stage were taken using an inverted fluorescence microscope (Olympus Optical Technology, Japan). Following cultivation with IMBSs and exposure to AMF for 8 min, the collected OS cells underwent an additional incubation period in a 24-well plate for 24 h (n = 3 independent experiments). Photomicrographs of the cells’ wound healing were captured using a phase-contrast microscope at the same magnification as previously utilized for IMBSs. The remaining wound area as a percentage of the initial wound area was quantified using the Image J program to assess the percentage of wound closure.
Transwell assay
The filters measuring 6.5 mm in diameter with pore sizes of 8 μm were placed in the center of the chamber, followed by the addition of 800 μL of DMEM medium containing 10% FBS to the bottom of the chamber. Prior to the cultivation of OS cells, 20 μl of Matrigel, diluted with serum-free DMEM at a ratio of 1:8, was initially applied to the surface of the filters. Following cultivation with IMBSs and an 8-min exposure to AMF, OS cells were collected and subsequently seeded onto the Matrigel-coated filters. Following an additional incubation period of 24 h, the non-invading cells within the Matrigel were extracted from the upper chamber (n = 3 independent experiments). The cells that invaded the filters were initially rinsed with PBS, followed by fixation with methanol for 20 min, and finally stained using a Crystal Violet solution. Cells that invaded the filters were quantified in five random fields for each filter.
Western Blot assays examining the EMT process
Following cultivation with IMBSs and exposure to AMF for 8 min, the collected OS cells were then incubated for 2 h. The harvested OS cells underwent lysis with RIPA lysis solution (Beyotime, China), which included the protease inhibitor PMSF (Beyotime, China). The BCA protein quantification kit from Thermo Fisher Scientific (USA) was utilized to assess the concentration of total protein. In accordance with the guidelines provided by the SDS-PAGE gel kit (Vazyme, China), the proteins were separated at the optimal voltage. Following this, the proteins contained in the gel were transferred onto a polyvinylidene fluoride (PVDF) membrane (Sigma-Aldrich, USA). The PVDF membrane underwent blocking with 5% milk (Beyotime, China) at room temperature for a duration of 1.5 h. The primary antibodies, including anti-E-cadherin (HUABIO, #EM0502, China), anti-N-cadherin (HUABIO, #ET1607-37, China), anti-Vimentin (HUABIO, #ET1610-39, China), anti-Slug (Abmart, #TA6032, China), and anti-GAPDH (Abmart, #P60037, China) were incubated with the membrane at 4 °C overnight. On the subsequent day, the membrane underwent a washing process with TBST and was subsequently incubated with the Goat Anti-Rabbit IgG-HRP (Abmart, #M21002, China) at room temperature for a duration of 1.5 h. The blots were visualized with a chemiluminescence kit from Sigma-Aldrich, USA. In conclusion, a semi-quantitative analysis was performed utilizing Image J software (National Institutes of Health, version 1.8.0_172, USA) (n = 3 independent experiments).
In vitro the anti-tumor mechanism of IMBSs
Cell culture
To assess the anti-tumor mechanism of moderate MH and BSG combination therapy in vitro, 143B cells were cultured with pre-cured IMBSs in DMEM medium supplemented with 10% FBS and 1% P/S, both in the presence and absence of AMF, utilizing output currents of 20 A and a frequency of 550 kHz. The culture environment was sustained at 37 °C in a humidified atmosphere with 5% CO2.
RNA-seq for 143B cells
Following a 2-hour incubation, 143B cells were harvested for the extraction of total RNA utilizing TRIzol reagent (Invitrogen, USA) (n = 3 independent experiments). The sequencing of the RNA libraries was conducted using the Illumina NovaseqTM 6000 platform at OE Biotech, Inc., located in Shanghai, China. We acknowledged the support provided by OE Biotech, Inc., (Shanghai, China) in the areas of sequencing and bioinformatics analysis. The bioinformatic analysis was performed utilizing the OECloud tools accessible at https://cloud.oebiotech.com/task/. The database information and data analysis software were provided in Supplementary Tables 3 and 4. The volcano map was created utilizing R on the OECloud platform (https://cloud.oebiotech.com/task/). Genes exhibiting |log2 FC | > 1 and a P-value below 0.05 were identified as differentially expressed. The differentially expressed genes (DEGs) were analyzed by the quantification method (FPKM). The differential pathways were conducted using GO analysis and KEGG analysis.
Western Blot assays on the mechanism-related protein expression in 143B cells
Following a 2-hour incubation, 143B cells were harvested. The primary antibodies including anti-TNF-α (Abmart, #PY19810, China), anti-TNFR1 (Abmart, #T56804, China), anti-NF-κB p65 (Abmart, #T55034, China), anti-Phospho-NF-κB p65 (Ser536) (HUABIO, #HA723223, China), anti-IκB-α (HUABIO, #ET1603-6, China), anti-Phospho-IκB-α (Ser32/Ser36) (HUABIO, #HA722770, China), anti-cleaved PARP (Abmart, #T611503, China), anti-Bcl-2 (HUABIO, #ET1702-53, China), anti-cleaved caspase-3 (Abmart, #T61532, China), and anti-GAPDH were incubation with 143B cells at 4 °C overnight. After that the Goat Anti-Rabbit IgG-HRP was incubated at room temperature for a duration of 1.5 h. The Western Blots bands were then visualized with a chemiluminescence kit (n = 3 independent experiments).
TEM testing
Following a 2-hour incubation, the harvested 143B cells underwent three washes with PBS, after which they were fixed in a 2.5% (v/v) glutaraldehyde solution (Aladdin, China) overnight. Following the elimination of residual fixative using PBS, the fixed 143B cells underwent uranyl acetate staining and a series of gradient ethanol dehydration steps (30%, 50%, 75%, 90%, 95%, and 100% v/v). Subsequently, the cells underwent immersion in acetone for a duration of 10 min, followed by a 10-min exposure to a 1:1 mixture of acetone and epoxy resin, and finally, a 10-min immersion in epoxy resin. This sequence was essential to ensure proper polymerization of the epoxy resin and optimal embedding of the cells. Following this, the embedded samples were shaped into a trapezoidal form and sliced into sections with a thickness ranging from 50 to 70 nm utilizing a microtome. Following double staining with 3% uranyl acetate and lead citrate, the resulting slices were analyzed using a TEM to investigate the morphology of 143B cells subjected to IMBSs.
Hochst 33258 staining
Apoptotic cells were characterized by a rounded shape, deeply stained nuclei, condensed cytoplasm, and clumped chromatin, leading to the “budding” profile of cell morphology47. Hoechst 33258 is widely utilized for detecting apoptosis, analyzing the cell cycle, and differentiating apoptotic cells48. The details of the experiment were outlined as follows: Prior to the implementation of MH, 143B cells were underwent transfection with siTNFR1 (siG09921145457-1-5, Ruibo, China) utilizing Lipofectamine 2000 (Thermo Fisher Scientific, USA) in accordance with the manufacturer’s instructions. Following a 2-hour incubation after the implementation of MH, the culture medium was substituted with 100 μL of Hoechst 33258 staining solution, and the 143B cells were incubated for an additional 20 – 30 min. Following the removal of the Hoechst 33258 solution, fresh PBS was introduced, and fluorescence detection was conducted on the 143B cells to examine and quantify the proportion of apoptotic cells.
Flow cytometry analysis
Prior to the implementation of MH, 143B cells were underwent transfection with siTNFR1 utilizing Lipofectamine 2000 in accordance with the manufacturer’s instructions. Following a 2-hour incubation after the implementation of MH, the adherent cells underwent a single wash with PBS prior to the application of EDTA-free trypsin solution to promote cell detachment. The cells were maintained at room temperature until they could be carefully dislodged through pipetting, ensuring that excessive digestion by the trypsin was avoided. The previously collected medium was reintroduced, and the cells were carefully resuspended prior to being transferred to a centrifuge tube. The cell suspension underwent centrifugation at 1000 x g for 5 min. Following this, the supernatant was removed. A sample of 50,000 to 100,000 resuspended cells was subjected to a second centrifugation, after which the supernatant was removed. Following this, 195 μL of Annexin V-FITC binding solution was added to resuspend the cells. Subsequently, 5 μL of Annexin V-FITC and 10 μL of propidium iodide (PI) staining solution were introduced and mixed gently. The cells were incubated in the dark at room temperature (20 - 25 °C) for 20 min prior to being transferred to an ice bath. A prompt analysis was conducted utilizing a flow cytometer (Beckman, USA), with Annexin V-FITC showing green fluorescence and PI revealing red fluorescence.
In vitro osteogenic promotion of IMBSs on hBMSCs
Cell culture
hBMSCs (Cyagen, China), have been authenticated and tested for mycoplasma, were cultured in α-MEM (Thermo Fisher Scientific, USA) with 10% FBS and 1% P/S in a 5% CO2 incubator.
Construction of temperature gradients
It is understood that only IMBSs exposed to AMF can exhibit MH, and that the tumor suppression associated with MH fundamentally depends on the thermal response generated by IMBSs exposed to AMF. Aiming to simulate the effects of MH specifically on the viability of hBMSCs, a cell incubator that systematically creates culture temperature gradients (37, 42, and 45 °C) to mimic MH and conducted experiments was employed to assess how these temperature gradients influence the viability of hBMSCs.
Preparation of dynamic extracts of IMBSs
To simulate the dynamic IAM forming from implants degradation in vivo, dynamic extracts of pre-cured IMBSs were used to incubate with hBMSCs, and the preparation details are stated as follows: The IMBSs, measuring 10 mm in diameter and 3.0 mm in height, were immersed in DMEM medium enriched with P/S at a concentration of 0.2 g/mL. The samples were subsequently incubated in a shaker at 37 °C for a duration of 24 h. Following the filtration process, the extract was gathered and preserved for subsequent applications. Following this, an equal volume of DMEM medium enriched with P/S was introduced, which were then incubated in a shaker at 37 °C for another 24 h. The procedure was carried out repeatedly, with extracts gathered from the identical IMBSs on a daily basis until the 28th day.
Cytotoxicity and proliferation
With a density of 3.5 × 104 cells per well, hBMSCs were cultured in a 48-well plate containing a complete medium under temperature gradients (37, 42, and 45 °C), or cultured in complete medium supplemented with dynamic extracts of IMBSs, or complete medium supplemented with specific dynamic extracts of IMBSs under temperature gradients (37, 42, and 45 °C) (n = 3 independent experiments). At 24- and 72-hour post-incubation, the CCK-8 reagent (1:9) was administered. Following a 1.5-hour incubation period, the absorbance was quantified at 450 nm.
Live/Dead staining and cytoskeleton staining
With a density of 3.5 × 105 cells per well, hBMSCs were cultured in a 12-well plate containing a complete medium under temperature gradients (37, 42, and 45 °C), or cultured in complete medium supplemented with a specific dynamic extract of IMBSs under temperature gradients (37, 42, and 45 °C) (n = 3 independent experiments). After incubation time of 24 h, 300 μL of a pre-mixed reagent solution, comprising calcein and PI, was added to each well in accordance with the Live/Dead staining protocol (Beyotime, China). After another 15-min incubation, Live/Dead staining images of hBMSCs were then captured using an inverted fluorescence microscope. For the cytoskeleton staining assay, after an incubation time of 24 h, 500 μL of 4% PFA was first added to fix the cells for 30 min, followed by the addition of 300 μL of 0.1% Triton X-100 (Sigma-Aldrich, USA) to enhance cell membrane permeability. Following the above procedures, 300 μL of Actin Tracker Red-594 (diluted 1:500, Beyotime, China) was used to stain the cytoskeletal actin for 15 min, while the cell nuclei were stained with 4’,6-diamidino-2-phenylindole dihydrochloride (DAPI) for 10 min. The cytoskeleton images of hBMSCs were captured using an inverted fluorescence microscope.
Osteogenic differentiation
The hBMSCs, at a density of 3.5 × 105 cells per well, were firstly cultured in 12-well plates under controlled conditions of 37 °C and 5% CO2 (n = 3 independent experiments). Upon reaching 85% confluence, 2 mL of osteogenic induction medium was introduced, which comprised 10 mM β-glycerophosphate (Sigma-Aldrich, USA), 50 μM L-ascorbic acid (Solarbio, China), 0.1 μM dexamethasone (Sigma-Aldrich, USA), and a specific dynamic extract of IMBSs. With 7 days of incubation time in a complete medium under temperature gradients (37, 42, and 45°C), or in complete medium supplemented with a specific dynamic extract of IMBSs under temperature gradients (37, 42, and 45 °C), 500 μL of 4% PFA (Beyotime, China) was applied to fix the cells for a duration of 20 min. Following fixation, 300 μL of the ALP assay premix (Beyotime, China) was added to each well and incubated at room temperature for 12 h. With 14 days of incubation time in a complete medium under temperature gradients (37, 42, and 45 °C), or in complete medium supplemented with a specific dynamic extract of IMBSs under temperature gradients (37, 42, and 45 °C), 300 μL of a 2% ARS working solution (Beyotime, China) was added for 15 min post-fixation. All samples were examined, and images were captured using an inverted microscope.
RNA-seq for hBMSCs
Following the same culture procedures in “Osteogenic differentiation of hBMSCs”, hBMSCs were harvested for the extraction of total RNA utilizing TRIzol reagent (Invitrogen, USA) (n = 3 independent experiments). The RNA-seq and analysis steps are described in the “RNA-seq for 143B cells” section.
qRT-PCR analysis on the osteogenic related genes expression
Following the same culture procedures in “Osteogenic differentiation of hBMSCs”, but with different culture time. After incubation, total RNA was extracted from the harvested hBMSCs using the mRNA extraction kit (Magen, China) (n = 3 independent experiments) and subsequently reverse transcribed into complementary DNA (cDNA) with the PrimeScript RT reagent kit (20 μL) (Vazyme, China). qRT-PCR was conducted to assess the expression levels of osteogenic-related genes in hBMSCs, specifically ALP (7 days), RUNX2 (7 days), COL-1 (7 days), OCN (14 days), and OPN (14 days). GAPDH served as the reference gene. The primer sequences for the genes analyzed are provided in Supplementary Table 6.
Western Blot assays on the mechanism-related protein expression in hBMSCs
Following the same culture procedures in “Osteogenic differentiation of hBMSCs”, hBMSCs were harvested with an incubation time of 7 days. The primary antibodies including anti-CACNA1G (Abmart, #TD10014, China), anti-PKC-β (HUABIO, #ER1802-14, China), anti-Bcl-2, anti-STAT3 (HUABIO, #ET1607-38, China), anti-p-STAT3 (Y705) (HUABIO, #ET1603-40, China), and anti-GAPDH (Abmart, #P60037, China) were incubated with hBMSCs at 4 °C overnight. After that, the Goat Anti-Rabbit IgG-HRP was incubated at room temperature for a duration of 1.5 h. The Western Blots bands were then visualized with a chemiluminescence kit (n = 3 independent experiments).
In vitro evaluation on the reprogramming of tumorous microenvironments by IMBSs
Cell culture
RAW 264.7 and DC2.4 cells (Procell, China), have been authenticated and tested for mycoplasma, were cultured in DMEM with 10% FBS and 1% P/S in an incubator of 37 °C with 5% CO2. To simulate the dynamic IAM formation from implant degradation in vivo, dynamic extracts of pre-cured IMBSs were incubated with RAW 264.7 and DC2.4 cells with their inducer, and the preparation are stated as follows: The IMBSs (φ = 10 mm, h = 3.0 mm) were immersed in DMEM medium with P/S, were incubated in a shaker at 37 °C for a duration of 24 h. Following the filtration process, the extract was gathered.
Re-programming assays of TAMs
RAW 264.7 cells were seeded into a 12-well plate at a density of 2.0 × 105 cells per well for 24 h. After being induced with IL-4 (20 ng/mL) and IL-13 (20 ng/mL) with dynamic extract of IMBSs for 24 h. the cells were harvested and washed with PBS. Then cells were blocked by 1% BSA solution for 1 h at 4 °C. After washed with PBS, and anti-CD86 (PE, Thermo Fisher Scientific, #12-0862-82, USA) and anti-CD206 (FITC, Thermo Fisher Scientific, #MA-5168-70, USA) were added and incubated for 1 h in the dark at 4 °C. The cells were analyzed by flow cytometry.
Maturation assays of DCs
DC2.4 cells were seeded in a 12-well plate at a density of 3.5 × 105 cells per well for 24 h. After being induced with LPS (100 μg/mL) with dynamic extract of IMBSs for 24 h. The cells were harvested. Then, cells were blocked by 1% BSA solution for 1 h at 4 °C. After washing, anti-CD86 and anti-CD80 (FITC, Thermo Fisher Scientific, #11-0801-82, USA) were added and incubated for 1 h in the dark at 4 °C. The cells were analyzed by flow cytometry.
The inhibition of IMBSs on nude mice subcutaneous xenograft OS
All animal experiments were conducted in compliance with the guidelines established by the Animal Ethics Committee of Shenzhen Institutes of Advanced Technology, Chinese Academy of Sciences (approval number: SITA-IACUC-200401-YYS-CX-A1220-01), and adhered to the National Laboratory Animal Care and Use Guide. A total of 16 female BALB/c nude mice, aged 6 to 8 weeks, were purchased from Weitong Lihua Biotechnology Co., Ltd., China. The mice were divided into four groups: the blank control group, BSG group, 5-MNP-BSG (+) group, and 10-MNP-BSG (+) group (n = 4 mice), and were kept under uniform feeding conditions. Prior to implantation, pre-cured IMBSs measuring 3.5 mm in diameter and 5.0 mm in height underwent sterilization through ultraviolet light (UV) exposure for a duration of 2 h. Xenograft OS models were established through the subcutaneous injection of 100 μL of 143B cells (1.5 × 107 cells) into the right axillary region of mice. Upon reaching a tumor volume of 100 mm3, pre-cured IMBSs were strategically implanted into the tumor tissue’s center. The duration of IMBSs therapy was 14 days, involving 8 min of treatment daily. At the end of IMBSs therapy, all mice were euthanized, weighed, and the tumors were excised, weighed, and subjected to IHC staining to assess the relevant cytokine expression of TNF, NF-κB, and apoptotic signaling pathways in OS tissues. Two pathologists conducted an independent analysis of the results. Using Image J software, the percentage of positively stained cells was scored as follows: Assign a score of 1 for values less than or equal to 33%, 2 for values between 33% and 66%, and 3 for values greater than or equal to 66%. Furthermore, the intensity of cell staining was categorized as 1 for absent/weak, 2 for moderate, and 3 for strong. The two scores were multiplied to produce a total immune score, categorized as either low (0 - 3) or high (4 - 9) for each pathological section.
Tumor ablation and osteogenic efficacy of IMBSs in rat tibial OS backfill defect model
Firstly, BALB/c nude mice (female, 6 - 8 weeks old) were subcutaneously injected with 100 μL of UMR106 cells (1.5 × 107 cells) at the right axilla to construct the subcutaneous tumor model. When the tumor volume reached approximately 200 mm3, the tumors were excised under sterile conditions and further sectioned into approximately 1 mm3 tissue blocks. Meanwhile, 16 SD rats (female, 300 - 350 g), purchased from Weitong Lihua Biotechnology Co., Ltd., China, were randomly divided into four groups (n = 4 rats), namely the blank control, BSG group, 5-MNP-BSG (+) group, and 10-MNP-BSG (+) group. All animal groups received identical feeding protocols. With continuous inhalation anesthesia using a small animal anesthesia machine (RWD, China) in conjunction with isoflurane (RWD, China), a transverse bone defect with a diameter of 2.0 mm and a length of 3.5 mm was created directly beneath the tibial plateau. After that, IMBS samples, sterilized using UV for 2 h, alongside approximately 10 mg of tumor tissue blocks, were implanted synchronously into the tibia defects. On the third day after implantation, AMF (15 A, 550 kHz) was delivered to commence IMBSs therapy. The period of IMBSs therapy lasted for 6 weeks, with 8 min of treatment each day. At the end of treatment, MRI was first conducted to monitor the expansion of UMR106 cells around the rat knees. After photographing the general state, the rats’ lower limbs and lung tissues were collected and photographed. The ex vivo lungs were subsequently subjected to H&E staining to detect the metastasis of OS. Meanwhile, IHC staining of the tumor tissues was employed to assess the protein expression, relating to the TNF, NF-κB, and apoptotic signaling pathways. Furthermore, the ex vivo lower limbs of rats were further processed with decalcification in a 12% EDTA solution and embedding in paraffin to fabricate histological sections with a thickness of 5 µm. Subsequently, H&E staining and MTS were performed to analyze the in situ osteogenic capacity of IMBSs therapy under an inverted fluorescence microscope.
Tumor ablation and immunoregulation of IMBSs in rat tibial OS model
Animal model construction and experimental grouping
To confer fluorescence imaging capability to lung metastatic OS, the empty lentiviral vector (U6-MCS-Ubc-Cherry-IRES-Puromycin), designed and supplied by GeneChem (Shanghai, China), was transfected into UMR106 cells to establish stable Cherry expression in the UMR106 cell line. UMR106 cells were plated in a 12-well format at a density of 3 × 105 cells per well. After 24 h, the infectious fluid containing lentivirus (1 × 107 TU/mL) was added to the wells. Following a 72-hour incubation, puromycin (1 µg/mL) was employed to select for stable mCherry expression in the cells. Similar to the tumor ablation and osteogenic efficacy of IMBSs in the rat tibial OS backfill defect model, tumors were excised and sectioned into approximately 1 mm3 blocks from nude mice. Sixteen female SD rats, weighing between 200 and 250 g, were allocated into four groups (n = 4 rats): the blank control group, the BSG group, the 5-MNP-BSG (+) group, and the 10-MNP-BSG (+) group. A bone defect measuring 3.0 mm in diameter and 5.0 mm in length was created beneath the tibial plateau under continuous inhalation anesthesia. Subsequently, tumor blocks (10 mg) were implanted into all defects. After a duration of two weeks, tumor proliferation was observed around the proximal tibia. The IMBS samples, sterilized with UV for 2 h, were then implanted into the tumor core. On the third postoperative day, AMF (15 A, 550 kHz) was administered to initiate IMBS therapy. The treatment duration was 4 weeks, with a daily application of 8 min. At the conclusion of treatment, the proximal tibia containing OS tissues and the lungs of rats were collected.
In vivo evaluation of immunoregulation and inhibition of OS lung metastasis by IMBSs within the tumorous microenvironment
A portion of the OS tissues was minced in a EP tube and then transferred to a 50 mL centrifuge tube with 45 mL of HBSS. Subsequently, 5 mL of 10×Triple Enzyme Mix (containing collagenase IV (Sigma-Aldrich, USA), hyaluronidase (Solarbio, China), and DNase IV (Sigma-Aldrich, USA)) was added. The OS blocks were digested on a shaker at 37 °C for 1.5 h. The mixture was filtered using a 200-mesh filter. The supernatant of OS tissues was centrifuged and collected at 1200 x g for 5 min. The cells were resuspended in 3 mL of 30% Percoll. At the same time, 3 mL of 70% Percoll was added to a 15 mL centrifuge tube. Subsequently, 3 mL of 30% Percoll containing the cells was carefully layered on top of the 70% Percoll. The samples were centrifuged at 1200 x g for 15 min (acceleration = 4, deceleration = 2). The immune cells at the interface between the 30% Percoll and 70% Percoll were collected and blocked with 1% BSA. The immune cells were then incubated with antibodies including anti-CD86 (FITC, Thermo Fisher Scientific, #11-0860-82, USA), anti-CD80 (PE, Thermo Fisher Scientific, #12-0800-82, USA), anti-CD163 (PE, BD Biosciences, #759120, USA), anti-CD3 (FITC, Thermo Fisher Scientific, #11-0030-82, USA), and anti-CD8 (PE, Thermo Fisher Scientific, #48-0084-82, USA) for 1 h in the dark at 4 °C. Subsequently, the cells were analyzed by flow cytometry. Meanwhile, IHC staining was employed to assess the immune markers, including CD86, CD206, and CD8, in the ex vivo proximal tibia with OS tissue in rats. The TRAP staining was also performed to analyze the tumor-osteoclasts. The ex vivo lungs were subjected to bioluminescence by IVIS spectrum and H&E staining to detect the lung metastasis of OS.
Bone repair ability of IMBSs in the rat femoral condyle defect model
A total of 32 SD rats (male, weighing 350 to 400 g), purchased from Weitong Lihua Biotechnology Co., Ltd., China, were randomly divided into four groups (n = 8 rats), namely the CaSO4 group (with CaSO4 implantation), the BSG group, the 5-MNP-BSG (+) group, and the 10-MNP-BSG (+) group, with all animal groups receiving identical feeding protocols. Under continuous inhalation anesthesia using a small animal anesthesia machine, femoral condyle defects (φ = 3.5 mm, h = 5.0 mm) were created and implanted with samples corresponding to each animal group. All implants were sterilized using UV for 2 h before the operation. On the third day after implantation, AMF (15 A, 550 kHz) was delivered to the rats to commence IMBSs therapy for 8 weeks, with 8 min of treatment each day. At 4- and 8-weeks post-implantation, the femur samples were harvested to conduct micro-CT scanning (SCANCO Medice AG, VivaCT40, Switzerland), MBAFS, and GTS to examine the osteogenesis. The region of interest (ROI) for micro-CT analysis was defined as a height of 5.00 mm and a diameter of 4 mm. 3D reconstruction was conducted to quantitatively assess bone parameters of the ROI, including BV/TV and Tb.Th. Images of histopathology were captured using an inverted fluorescence microscope.
In vivo biocompatibility evaluation of IMBSs after implanting in different animal models
At the endpoint of the OS treatment in the nude mice subcutaneous model, the vital organs of the nude mice, specifically the heart, liver, spleen, lungs, and kidneys, were harvested. For the rat femoral condyle defect model, vital organs were also collected at the endpoint of treatment. These vital organs from different animals were subjected to H&E staining to systematically assess the biocompatibility of IMBSs therapy.
Statistics & reproducibility
Statistical significance was assessed using GraphPad Prism 9.0 software. Data are graphed with an error bar showing the standard deviation (SD). All key findings were reproduced in at least three independent experiments. Comparisons between two groups were performed using the two-tailed Student’s t-test. For comparisons among more than two groups, two-way ANOVA was conducted, followed by Tukey’s post hoc test, as described in the figure legends. Additional information on the study design, the number of replicates, and the statistical methods used are showed in the figure legends.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
All data substantiating the conclusions of this study are accessible within the paper, Supplementary Information, or source data file. All RNA sequencing data have been archived publicly at GEO (https://www.ncbi.nlm.nih.gov/gds/) with accession code GSE294322 for OS cells and GSE294487 for hBMSCs. This publication includes the source data. Source data are provided with this paper.
References
Shao, R. et al. Bone tumors effective therapy through functionalized hydrogels: current developments and future expectations. Drug Deliv. 29, 1631–1647 (2022).
Siegel, R. L. et al. Cancer statistics, 2022. CA Cancer J. Clin. 72, 7–33 (2022).
Yu, S. et al. Advances on immunotherapy for osteosarcoma. Mol. Cancer 23, 192 (2024).
Gill, J. et al. Advancing therapy for osteosarcoma. Nat. Rev. Clin. Oncol. 18, 609–624 (2021).
Chen, C. L. et al. miR-134 inhibits osteosarcoma cell invasion and metastasis through targeting MMP1 and MMP3 in vitro and in vivo. FEBS Lett. 593, 1089–1101 (2019).
Wedekind, M. F. et al. Immunotherapy for osteosarcoma: Where do we go from here?. Pediatr. Blood Cancer 65, e27227 (2018).
Xu, J. et al. PDGF/PDGFR effects in osteosarcoma and the “add-on” strategy. Clin. Sarcoma Res 8, 15 (2018).
Fang, J. et al. Exploiting the dynamics of the EPR effect and strategies to improve the therapeutic effects of nanomedicines by using EPR effect enhancers. Adv. Drug Deliv. Rev. 157, 142–160 (2020).
de la Encarnación, C. et al. Multifunctional plasmonic-magnetic nanoparticles for bioimaging and hyperthermia. Adv. Drug Deliv. Rev. 189, 114484 (2022).
Beola, L. et al. Drug-loaded lipid magnetic nanoparticles for combined local hyperthermia and chemotherapy against glioblastoma multiforme. ACS Nano 17, 18441–18455 (2023).
Dadfar, S. M. et al. Iron oxide nanoparticles: Diagnostic, therapeutic and theranostic applications. Adv. Drug Deliv. Rev. 138, 302–325 (2019).
Khan, U. et al. Rahim, transformation mechanism of magnetite nanoparticles. Mater. Sci.-Pol. 33, 278–285 (2015).
Rivera, D. et al. Neurosurgical applications of magnetic hyperthermia therapy. Neurosurg. Clin. N. Am. 34, 269–283 (2023).
Feddersen, T. V. et al. Clinical performance and future potential of magnetic resonance thermometry in hyperthermia. Cancers (Basel) 13, 31 (2020).
Kumar, A. et al. Impact of Gd3+ doping on structural, electronic, magnetic, and photocatalytic properties of MnFe2O4 nanoferrites and application in dye-polluted wastewater remediation. Environ. Sci. Pollut. Res Int 30, 18820–18842 (2023).
Zheng, Y. et al. Effects of rhenium substitution of Co and Fe in spinel cofe2o4 ferrite nanomaterials. Nanomaterials (Basel) 12, 2839 (2022).
Buenrostro, D. et al. The bone microenvironment: A fertile soil for tumor growth. Curr. Osteoporos. Rep. 14, 151–158 (2016).
Sterling, J. A. et al. Advances in the biology of bone metastasis: how the skeleton affects tumor behavior. Bone 48, 6–15 (2011).
Riggi, N. et al. Cancer metastasis: A reappraisal of its underlying mechanisms and their relevance to treatment. Annu Rev. Pathol. 13, 117–140 (2018).
Bryan, J. N. Updates in osteosarcoma. Vet. Clin. North Am. Small Anim. Pr. 54, 523–539 (2024).
Liang, B. et al. Multifunctional bone cement for synergistic magnetic hyperthermia ablation and chemotherapy of osteosarcoma. Mater. Sci. Eng. C. Mater. Biol. Appl 108, 110460 (2020).
Huang, H. et al. 3D-printed tri-element-doped hydroxyapatite/ polycaprolactone composite scaffolds with antibacterial potential for osteosarcoma therapy and bone regeneration. Bioact. Mater. 31, 18–37 (2023).
Gupta, S. et al. Bioactive glass: A multifunctional delivery system. J. Control Release 335, 481–497 (2023).
Zheng, K. et al. Immunomodulatory bioactive glasses for tissue regeneration. Acta Biomater. 133, 168–186 (2021).
Wang, L. et al. Engineering single-atomic iron-catalyst-integrated 3D-printed bioscaffolds for osteosarcoma destruction with antibacterial and bone defect regeneration bioactivity. Adv. Mater. 33, e2100150 (2021).
Silva, A. S. et al. The potential role of systemic buffers in reducing intratumoral extracellular pH and acid-mediated invasion. Cancer Res 69, 2677–2684 (2009).
Robey, I. F. et al. Bicarbonate increases tumor pH and inhibits spontaneous metastases. Cancer Res 69, 2260–2268 (2009).
Harmon, B. V. et al. Cell death induced in a murine mastocytoma by 42-47 degrees C heating in vitro: evidence that the form of death changes from apoptosis to necrosis above a critical heat load. Int J. Radiat. Biol. 58, 845–858 (1990).
Tang, Y. et al. Influence of different heat transfer models on therapeutic temperature prediction and heat-induced damage during magnetic hyperthermia. J. Therm. Biol. 118, 103747 (2023).
Rivas-Murias, B. et al. Interfaceless exchange bias in CoFe2O4 nanocrystals. Nano Lett. 23, 1688–1695 (2023).
Pan, J. et al. Mild magnetic hyperthermia-activated innate immunity for liver cancer therapy. J. Am. Chem. Soc. 143, 8116–8128 (2021).
Ghara, S. et al. Magnetization reversal through an antiferromagnetic state. Nat. Commun. 14, 5174 (2023).
Li, S. et al. Spontaneous immunomodulation and regulation of angiogenesis and osteogenesis by Sr/Cu-borosilicate glass (BSG) bone cement to repair critical bone defects. Bioact. Mater. 23, 101–117 (2022).
Zhang, H. et al. Dual-functional borosilicate glass (BSG) delivery implant for osteomyelitis treatment and bone regeneration. Compos. Part B: Eng. 259, 110749 (2023).
Farrar, D. F. et al. Rheological properties of PMMA bone cements during curing. Biomaterials 22, 3005–3013 (2001).
Trivedi, Z. et al. Rheological analysis and evaluation of measurement techniques for curing poly(methyl methacrylate) bone cement in vertebroplasty. ACS Biomater. Sci. Eng. 10, 4575–4586 (2024).
Şahin, E. et al. The rheological behavior of a fast-setting calcium phosphate bone cement and its dependence on deformation conditions. J. Mech. Behav. Biomed. Mater. 72, 252–260 (2017).
Zhang, J. et al. Calcium phosphate cements for bone substitution: chemistry, handling and mechanical properties. Acta Biomater. 10, 1035–1049 (2014).
Sparks, D. S. et al. A preclinical large-animal model for the assessment of critical-size load-bearing bone defect reconstruction. Nat. Protoc. 15, 877–924 (2020).
Kasparis, G. et al. Zn doped iron oxide nanoparticles with high magnetization and photothermal efficiency for cancer treatment. J. Mater. Chem. B 11, 787–801 (2023).
Abd et al. Incorporation of strontium borosilicate bioactive glass in calcium aluminate biocement: Physicomechanical, bioactivity and antimicrobial properties. J. Mech. Behav. Biomed. Mater. 144, 105976 (2023).
Abodunrin, O. D. et al. A review on borate bioactive glasses (BBG): effect of doping elements, degradation, and applications. J. Mater. Chem. B 11, 955–973 (2023).
Janani, G. et al. Functional hepatocyte clusters on bioactive blend silk matrices towards generating bioartificial liver constructs. Acta Biomater. 67, 167–182 (2018).
Tang, Q. L. et al. Glycogen synthase kinase-3β, NF-κB signaling, and tumorigenesis of human osteosarcoma. J. Natl Cancer Inst. 104, 749–763 (2012).
Jiang, M. et al. Exosome-mediated miR-144-3p promotes ferroptosis to inhibit osteosarcoma proliferation, migration, and invasion through regulating ZEB1. Mol. Cancer 22, 113 (2023).
Hou, C. H. et al. Cyr61 promotes epithelial-mesenchymal transition and tumor metastasis of osteosarcoma by Raf-1/MEK/ERK/Elk-1/TWIST-1 signaling pathway. Mol. Cancer 13, 236 (2014).
Gupta, S. et al. Molecular changes associated with increased TNF-α-induced apoptotis in naïve (TN) and central memory (TCM) CD8+ T cells in aged humans. Immun. Ageing 15, 2 (2018).
Wang, X. et al. MEK inhibition prevents CAR-T cell exhaustion and differentiation via downregulation of c-Fos and JunB. Signal Transduct. Target Ther. 9, 293 (2024).
Liu, L. et al. Gli1 depletion induces oxidative stress and apoptosis of nucleus pulposus cells via Fos in intervertebral disc degeneration. J. Orthop. Transl. 40, 116–131 (2023).
Cong, Y. et al. Tim-3 promotes cell aggressiveness and paclitaxel resistance through NF-κB/STAT3 signalling pathway in breast cancer cells. Chin. J. Cancer Res 32, 564–579 (2020).
Horký, M. et al. Nucleolus and apoptosis. Ann. N. Y Acad. Sci. 973, 258–264 (2002).
Shen, Q. et al. Proliferation inhibition and apoptosis induction of imatinib-resistant chronic myeloid leukemia cells via PPP2R5C down-regulation. J. Hematol. Oncol. 6, 64 (2013).
Sreeja, S. et al. Hierarchically porous osteoinductive poly(hydroxyethyl methacrylate-co-methyl methacrylate) scaffold with sustained doxorubicin delivery for consolidated osteosarcoma treatment and bone defect repair. ACS Biomater. Sci. Eng. 7, 701–717 (2021).
Xiang, X. et a. Targeting tumor-associated macrophages to synergize tumor immunotherapy. Signal Transduct. Target Ther. 6, 75 (2021).
Moukengue, B. et al. Origin and therapies of osteosarcoma. Cancers (Basel) 14, 3503 (2022).
Viallard, C. et al. Tumor angiogenesis and vascular normalization: alternative therapeutic targets. Angiogenesis 20, 409–426 (2017).
Liu, J. et al. Acidic tumor microenvironment-activatable fluorescent diagnostic probe for the rapid identification and resection of human tumors via spraying. Biosens. Bioelectron. 234, 115343 (2023).
Ahmed, K. et al. Hyperthermia: an effective strategy to induce apoptosis in cancer cells. Apoptosis 20, 1411–1419 (2015).
Litman, R. S. et al. Malignant hyperthermia: update on susceptibility testing. JAMA 293, 2918–2924 (2005).
Boedtkjer, E. et al. The acidic tumor microenvironment as a driver of cancer. Annu Rev. Physiol. 82, 103–126 (2020).
Kamphuis, G. M. et al. Method of alkalization and monitoring of urinary pH for prevention of recurrent uric acid urolithiasis: a systematic review. Transl. Androl. Urol. 8, S448–S456 (2019).
Estrella, V. et al. Acidity generated by the tumor microenvironment drives local invasion. Cancer Res 73, 1524–1535 (2013).
Sisignano, M. et al. Proton-Sensing GPCRs in Health and Disease. Cells 10, 2050 (2021).
Haabeth, O. A. et al. A model for cancer-suppressive inflammation. Oncoimmunology 1, 1146–1155 (2012).
Wang, H. Integrative treatment of anti-tumor/bone repairing by combination of MoS2 nanosheets with 3D printed bioactive borosilicate glass scaffolds. Chem. Eng. J. 396, 125081 (2020).
Aggarwal, B. B. signaling pathways of the TNF superfamily: a double-edged sword. Nat. Rev. Immunol. 3, 745–756 (2003).
Iyer, S. V. et al. Genome-wide RNAi screening identifies TMIGD3 isoform1 as a suppressor of NF-κB and osteosarcoma progression. Nat. Commun. 7, 13561 (2016).
Yang, C. et al. Bone microenvironment and osteosarcoma metastasis. Int J. Mol. Sci. 21, 6985 (2020).
Russo, S. et al. The osteoclast traces the route to bone tumors and metastases. Front Cell Dev. Biol. 10, 886305 (2022).
Cui, X. et al. Strontium modulates osteogenic activity of bone cement composed of bioactive borosilicate glass particles by activating Wnt/β-catenin signaling pathway. Bioact. Mater. 5, 334–347 (2020).
Fan, M. et al. Borosilicate bioactive glass synergizing low-dose antibiotic loaded implants to combat bacteria through ATP disruption and oxidative stress to sequentially achieve osseointegration. Bioact. Mater. 44, 184–204 (2024).
Catterall, W. A. Voltage-gated calcium channels. Cold Spring Harb. Perspect. Biol. 3, a003947 (2011).
Manning, D. et al. Regulating voltage-gated ion channels with nanobodies. Nat. Commun. 13, 7557 (2022).
Hu, X. et al. The JAK/STAT signaling pathway: from bench to clinic. Signal Transduct. Target Ther. 6, 402 (2021).
Ding, J. et al. Regulated contribution of local and systemic immunity to new bone regeneration by modulating B/Sr concentration of bioactive borosilicate glass. Mater. Today Bio 19, 100585 (2023).
Sharma, P. et al. Hyperglycosylation of prosaposin in tumor dendritic cells drives immune escape. Science 383, 190–200 (2024).
Kokubo, T. et al. How useful is SBF in predicting in vivo bone bioactivity?. Biomaterials 27, 2907–2915 (2006).
Acknowledgements
This work was supported by the National Key R&D Program of China [Grant No. 2021YFC2400500 and 2023YFC2416900], Guangdong Marine Economic Development Program [GDNRC(2023)35], Shenzhen Science and Technology Program [Grant No. JCYJ20230807140714030, JCYJ20220818101613028, and JSGGKQTD20210831174330015], the National Natural Science Foundation of China [Grant No. U22A20357 and 32161160327], Guangdong Basic and Applied Basic Research Foundation [Grant No. 2022B1515420048], and Shenzhen Medical Research Foundation [B2302031].
Author information
Authors and Affiliations
Contributions
These authors contributed equally: M.F., C.L., and Y.Z. H.P., X.C,. and W.C. were responsible for funding acquisition and designing the research. H.P., X.C., and W.C. supervised the experiments. M.F., C.L. and Y.Z. performed experiments and interpreted the data. M.F., J.Z., and Y.L. contributed to the interpretation and visualization of the sequencing data. C.L., Y.Z., K.S., P.T., Y.Z., L.Z., X.G., H.L., and S.L. contributed to the interpretation of the tissue section in vivo. M.F., H.P., and W.C. reviewed and edited the manuscript. H.P. and X.C. revised the manuscript. All authors read and approved the final manuscript. These authors provided important experimental insights: H.P., X.C., W.C., P.D,. and X.L.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks Hongwei Ouyang, Colin R. Dunstan, and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Fan, M., Liu, C., Zhang, Y. et al. A strategy for challenging tumorous bone regeneration by borosilicate bioactive glass boosting moderate magnetic hyperthermia. Nat Commun 16, 8057 (2025). https://doi.org/10.1038/s41467-025-63270-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-025-63270-z