Abstract
Nivolumab alone and in combination with ipilimumab demonstrated durable clinical benefit in patients with previously treated microsatellite instability-high/mismatch repair-deficient metastatic colorectal cancer in the phase 2 CheckMate 142 study. Here, we report exploratory biomarker analyses from CheckMate 142 evaluating associations between various tissue biomarkers and the efficacy of nivolumab monotherapy and nivolumab plus ipilimumab combination in these patients. Higher expression of inflammation-related gene expression signatures is associated with improved response per investigator assessment and survival benefit with nivolumab monotherapy. In contrast, higher tumor mutational burden, tumor indel burden, and degrees of microsatellite instability are associated with improved response per investigator assessment and survival benefit with nivolumab plus ipilimumab. While interpretation is limited by the exploratory nature of these analyses, they suggest that tumor antigenicity rather than baseline tumor inflammation might be important for the combinatorial efficacy. Validation of these findings in larger, randomized studies is necessary.
Similar content being viewed by others
Introduction
Colorectal cancer (CRC) is the third most common malignancy worldwide and the second leading cause of cancer-related death1. Among patients with CRC, approximately 14% of all cases and 4–7% of metastatic cases have microsatellite instability-high/mismatch repair-deficient (MSI-H/dMMR) status2,3,4. Studies in recent years investigating the use of immune checkpoint inhibitors (ICIs) for the treatment of MSI-H/dMMR metastatic CRC (mCRC) have established the clinical benefit of programmed death-1 (PD-1) inhibitor-based regimens in these patients5,6,7,8,9,10. In the multicohort, non-randomized phase 2 CheckMate 142 study (NCT02060188), nivolumab (a PD-1 inhibitor), both alone and in combination with ipilimumab (a cytotoxic T lymphocyte antigen-4 [CTLA-4] inhibitor), demonstrated durable responses and long-term survival benefit, with manageable safety in previously treated patients with MSI-H/dMMR mCRC5,9,10,11. Based on the results from CheckMate 142, nivolumab received approval as monotherapy and/or in combination with ipilimumab for the treatment of MSI-H/dMMR mCRC that has progressed following chemotherapy in many countries, including the United States and European Union12,13. These findings also led to the inclusion of nivolumab-based regimens in the National Comprehensive Cancer Network and European Society for Medical Oncology guidelines (National Comprehensive Cancer Network. NCCN guidelines: colon cancer version 2.2023, https://www.nccn.org/professionals/physician_gls/pdf/colon.pdf; National Comprehensive Cancer Network. NCCN guidelines: rectal cancer version 2.2023, https://www.nccn.org/professionals/physician_gls/pdf/rectal.pdf)14. Despite the clinical benefit observed with nivolumab-based treatment in previously treated patients with MSI-H/dMMR mCRC, not all patients respond5,8,9,10, underscoring the need to identify additional biomarkers associated with efficacy in these patients. Recently published biomarker analyses showcase the active research interest in exploring potential biomarkers that could be predictive of response to immunotherapy in patients with MSI-H/dMMR mCRC15,16.
MSI-H/dMMR CRC tumors have high levels of immune infiltration and immune checkpoint protein expression17, which are thought to result from the immunogenic characteristics of such tumors, including their elevated levels of mutations and neoantigens17,18. This exploitation of immune checkpoint pathways by the tumors and inflamed tumor microenvironment provides a plausible rationale for the efficacy of ICIs observed in this population17, but does not fully explain why some patients benefit more from ICIs than others. Differences in the level of tumor mutational burden (TMB) might also partially explain the variability in response among patients19 and multiple studies suggest that higher TMB is indeed associated with response to ICIs in MSI-H/dMMR mCRC and other tumor types20,21,22,23,24. Tumor indel burden (TIB) is an indicator of frameshift insertions and deletions that may be more likely to generate neoantigens and can have strong associations with ICI response in some cancer types25. Additionally, the degree of MSI in CRC and other tumors has also been associated with response to PD-1 inhibitors19. Other analyses have noted associations between inflammatory gene expression signatures (GES), which indicate T-cell tumor infiltration, and clinical benefit with ICIs in various malignancies22,23,26. The presence of tertiary lymphoid structures (TLS) in the tumor microenvironment has also been associated with improved survival in several solid tumor types, and a 12-gene–based chemokine GES used to infer the presence and abundance of TLS was also predictive of improved outcomes in patients treated with ICIs27. These various biomarkers, therefore, hold promise as potential predictors for response with ICIs in patients with MSI-H/dMMR mCRC.
Here, we present exploratory analyses from CheckMate 142 that evaluated the associations between these biomarkers and efficacy with nivolumab, either alone or in combination with ipilimumab, in patients with previously treated MSI-H/dMMR mCRC.
Results
Among all treated patients (n = 193), 59 (31%) were evaluable for whole-exome sequencing (WES), 57 (30%) for RNA sequencing (RNA-seq), and 59 (31%) for CD3 immunohistochemistry (IHC). At clinical data cutoff (September 2021), the median duration of follow-up (time from first dose to data cutoff) was 70.0 months (range, 66.2–88.7 months) for the nivolumab monotherapy cohort and 64.0 months (range, 60.0–75.8 months) for the nivolumab plus ipilimumab cohort. Aside from the WES-evaluable and RNA-seq–evaluable subgroups having smaller percentages of patients with a clinical history of Lynch syndrome, baseline characteristics and clinical responses of each biomarker-evaluable subgroup were generally consistent with those of all treated patients (Table 1). Additionally, progression-free survival (PFS) per investigator assessment (INV) and overall survival (OS) were similar between all treated patients and the biomarker-evaluable subgroups (Supplementary Fig. 1).
In both cohorts, patients were clustered into two major subgroups of high and low expression of inflammation-related signatures (Fig. 1). Responders in the nivolumab monotherapy cohort were enriched in the cluster with high expression of inflammation-related signatures. In the nivolumab plus ipilimumab cohort, patients were further clustered into subgroups with different levels of TMB, TIB and degree of MSI. Responders in this cohort were enriched in the clusters with high TMB, TIB and degrees of MSI (Fig. 1). On an individual patient level, patients with high four-gene inflammatory and TLS GES scores also tended to have high expression of other inflammatory biomarkers; those with high TMB generally had high TIB and degrees of MSI (Fig. 1). An analysis of correlations between biomarkers revealed that the four-gene inflammatory GES and TLS GES were highly correlated (R = 0.89), and both were also correlated with other inflammatory biomarkers (Supplementary Fig. 2). Additionally, TMB, TIB and degree of MSI were found to be highly correlated with each other (Supplementary Fig. 2). Inflammatory biomarkers demonstrated no strong correlation with TMB, TIB or degree of MSI (Supplementary Fig. 2).
For visualization purpose, continuous biomarkers with missing values were imputed by the median and then z-score transformed. BOR best overall response, CD3 cluster of differentiation 3, CR complete response, DC dendritic cell, GES gene expression signature, IHC immunohistochemistry, IPI ipilimumab, MSI microsatellite instability, NE not evaluable, NIVO nivolumab, NK natural killer cell, PD progressive disease, PR partial response, SD stable disease, TCD8 CD8 + T cell, TIB tumor indel burden, TLS tertiary lymphoid structure, TMB tumor mutational burden, Treg regulatory T cell. Source Data are available.
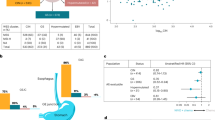
Overall, higher expression of inflammation-related biomarkers was generally associated with improved objective response per INV and survival benefit with nivolumab monotherapy, and higher TMB, TIB and degrees of MSI were associated with improved objective response and survival benefit with nivolumab plus ipilimumab (Fig. 2).
Biomarker associations are shown with A ORR per INV, B PFS per INV, and C OS. Data are presented as odds ratios ± 95% CIs (A) or hazard ratios ± 95% CIs (B, C). Data for GES and CD3 IHC are from all RNA-seq–evaluable patients (n = 57) and all CD3 IHC-evaluable patients (n = 59), respectively; data for TMB, degree of MSI, and TIB, are from all WES-evaluable patients (n = 59). CD3 cluster of differentiation 3, CI confidence interval, DC dendritic cell, GES gene expression signature, IHC immunohistochemistry, IPI ipilimumab, MSI microsatellite instability, NIVO nivolumab, NK natural killer cell, TCD8 CD8+ T cell, TIB tumor indel burden, TLS tertiary lymphoid structure, TMB tumor mutational burden, Treg regulatory T cell. Source Data are available.
Inflammatory biomarker analyses
Of the 57 RNA-seq–evaluable patients, 22 received nivolumab monotherapy and 35 received nivolumab plus ipilimumab. Objective responders in the nivolumab monotherapy cohort were found to have higher four-gene inflammatory GES scores than non-responders, while no obvious difference was observed in the nivolumab plus ipilimumab cohort (Fig. 3A). Using a median cutoff, patients in both cohorts were categorized as tumor inflammation-high or -low to assess the association of the four-gene inflammatory GES with survival. High expression was associated with improved PFS (hazard ratio [HR], 0.23; 95% confidence interval [CI], 0.07–0.75) and OS (HR, 0.13; 95% CI, 0.03–0.65) in the nivolumab monotherapy cohort, but no obvious association was seen in the nivolumab plus ipilimumab cohort (Fig. 3B, C). Higher TLS GES scores were also observed in responders who received nivolumab monotherapy compared with non-responders (Fig. 4A). There was no obvious difference between responders and non-responders in the nivolumab plus ipilimumab cohort (Fig. 4A). A median cutoff was used to distinguish TLS-high and -low subgroups and high TLS GES scores were also associated with improved PFS and OS with nivolumab monotherapy (HR, 0.15; 95% CI, 0.04–0.56; and HR, 0.12, 95% CI, 0.02–0.59, respectively), but not with nivolumab plus ipilimumab (Fig. 4B, C).
Association of four-gene inflammatory GES is shown with A ORR per INV, B PFS per INV and C OS. Data are from all RNA-seq–evaluable patients (n = 57). For the box plots, the box and middle bar within represent the interquartile range and median; the whiskers extend to the most extreme data point which is no more than 1.5 times the interquartile range from the box. P values (two-sided Wilcoxon rank-sum tests) are nominal and descriptive and are not intended to show statistical significance. Responders were defined as patients with the best overall response of complete or partial response, and non-responders were defined as patients with the best overall response of stable disease or progressive disease, and patients not evaluable for response. Source data are provided as a Source Data file. CI confidence interval GES gene expression signature, HR hazard ratio, IPI ipilimumab, NIVO nivolumab, ORR objective response rate.
Association of TLS GES is shown with A ORR per INV, B PFS per INV and C OS. Data are from all RNA-seq–evaluable patients (n = 57). For the box plots, the box and middle bar within represent the interquartile range and median; the whiskers extend to the most extreme data point which is no more than 1.5 times the interquartile range from the box. P values (two-sided Wilcoxon rank-sum tests) are nominal and descriptive and are not intended to show statistical significance. Responders were defined as patients with best overall response of complete or partial response, and non-responders were defined as patients with best overall response of stable disease or progressive disease and patients not evaluable for response. CI confidence interval, GES gene expression signature, HR hazard ratio, IPI ipilimumab, NIVO nivolumab, ORR objective response rate, TLS tertiary lymphoid structure. Source Data are available.
The association between tumor T-cell density (measured by CD3 IHC) and efficacy of nivolumab-based regimens was assessed in 59 CD3 IHC-evaluable patients (nivolumab monotherapy, n = 36; nivolumab plus ipilimumab, n = 23). Patient subgroups were classified using a median cutoff. Tumor T-cell density was higher in responders than non-responders in the nivolumab monotherapy cohort, and no difference was observed in the nivolumab plus ipilimumab cohort (Supplementary Fig. 3A). No association was found between tumor T-cell density and survival in either cohort (Supplementary Fig. 3B, C).
TMB, TIB and MSI analyses
Fifty-nine WES-evaluable patients (nivolumab monotherapy, n = 22; nivolumab plus ipilimumab, n = 37) were included for TMB, TIB and MSI analyses. As patients with MSI-H/dMMR disease in general have high TMB, a 20 mutations per megabase (Mb) cutoff was used to define TMB-high (≥20 mutations/Mb) and TMB-low (<20 mutations/Mb) tumors based on TMB distribution (Supplementary Fig. 4). ORR was higher in the TMB-high subgroup versus the TMB-low subgroup in the nivolumab plus ipilimumab cohort, but no obvious difference in ORR was observed in patients receiving nivolumab monotherapy (Fig. 5A). High TMB was also associated with survival benefit with nivolumab plus ipilimumab (PFS, HR, 0.12; 95% CI, 0.04–0.31; and OS, HR, 0.08; 95% CI, 0.02–0.30; Fig. 5B, C). No difference in survival outcomes was observed between high and low TMB levels in the nivolumab monotherapy cohort (Fig. 5B, C).
Association of TMB is shown with A ORR per INV, B PFS per INV and C OS. Data are from all WES-evaluable patients (n = 59). The bars and error bars in the bar plots represent the objective response rate and two-sided 95% CIs estimated by the Clopper-Pearson exact method. P values (two-sided Fisher’s exact tests) are nominal and descriptive and are not intended to show statistical significance. CI confidence interval, GES gene expression signature, HR hazard ratio, IPI ipilimumab, NIVO nivolumab, ORR objective response rate, TMB tumor mutational burden. Source Data are available.
TIB was higher in responders versus non-responders in the nivolumab plus ipilimumab cohort (Supplementary Fig. 5A). No association was found between TIB and response in the nivolumab monotherapy cohort (Supplementary Fig. 5A). TIB-high and TIB-low were defined using a median cutoff to assess associations between TIB and survival. High TIB was associated with greater PFS (HR, 0.19; 95% CI, 0.07–0.53) and OS (HR, 0.11; 95% CI, 0.02–0.49) benefit in patients receiving nivolumab plus ipilimumab, while no association was found in those receiving nivolumab monotherapy (Supplementary Fig. 5B, C).
Responders in the nivolumab plus ipilimumab cohort were found to have higher degrees of MSI as measured by MSIsensor score compared with non-responders, but no association was observed between the degree of MSI and response with nivolumab monotherapy (Supplementary Fig. 6A). High and low degrees of MSI were defined using a median cutoff. High degrees of MSI were associated with improved PFS (HR, 0.23; 95% CI, 0.09–0.63) and OS (HR, 0.20; 95% CI, 0.05–0.75) with nivolumab plus ipilimumab, but not with nivolumab monotherapy (Supplementary Fig. 6B, C).
TMB and four-gene inflammatory GES composite and multivariate analyses
The association between the four-gene inflammatory GES and efficacy with nivolumab monotherapy and the association between TMB and efficacy with nivolumab plus ipilimumab prompted a composite analysis with both biomarkers. In patients with available four-gene inflammatory GES and TMB results, there was no correlation between four-gene inflammatory GES scores and TMB (R = 0.0052 and R = − 0.16 in the nivolumab monotherapy [n = 21] and nivolumab plus ipilimumab [n = 33] cohorts, respectively; Supplementary Fig. 7A, B). Improved response and survival benefit were still associated with high four-gene inflammatory GES scores in the nivolumab monotherapy cohort, irrespective of TMB levels (Supplementary Fig. 7A). In patients who received nivolumab plus ipilimumab, high TMB was associated with improved response and survival benefit regardless of four-gene inflammatory GES expression scores (Supplementary Fig. 7B). We further evaluated the four-gene inflammatory GES and TMB in a multivariate model, including additional covariates of age, sex, and Eastern Cooperative Oncology Group performance status. After adjustment for TMB and other covariates, there were associations between the four-gene inflammatory GES and ORR, PFS, and OS in the nivolumab monotherapy cohort. Similarly, after adjustment for four-gene inflammatory GES and other covariates, there were associations between TMB and ORR, PFS and OS in the nivolumab plus ipilimumab cohort (Supplementary Fig. 8).
Discussion
Nivolumab, alone and in combination with ipilimumab, demonstrated durable responses and disease control in previously treated patients with MSI-H/dMMR mCRC in the CheckMate 142 trial5,10,11. The exploratory biomarker analyses from CheckMate 142 reported here aimed to identify associations between various biomarkers and efficacy with nivolumab-based regimens. We found associations between inflammation-related GES and efficacy in patients who received nivolumab monotherapy and associations between TMB, TIB, and degree of MSI and efficacy in patients who received nivolumab plus ipilimumab.
Previous studies have identified associations between inflammatory GES and efficacy of PD-1/PD-ligand 1 (PD-L1) blockade across different tumor types22,23,28. The current analysis also supports this conclusion, with higher four-gene inflammatory and TLS GES scores associating with greater response and survival benefit with nivolumab monotherapy. These findings suggest that preexisting tumor immunity, as measured by baseline tumor T-cell inflammation, may be associated with nivolumab benefit because PD-1 blockade facilitates reactivation of dysfunctional T cells in the tumor microenvironment. Interestingly, higher inflammatory signature scores were not associated with improved outcomes with nivolumab plus ipilimumab. This may be due, in part, to ipilimumab enhancing T-cell priming, activation, and infiltration29,30 such that the requirement for preexisting immune-cell infiltration is alleviated. On the other hand, in our analyses, higher TMB, TIB, and degrees of MSI were associated with nivolumab plus ipilimumab efficacy. Successful antitumor immunity requires the presence of effector T cells (as measured by baseline inflammation) and tumor recognition by the immune system through neoantigen burden (as indirectly measured by TMB)29. Given that the addition of ipilimumab to nivolumab appears to reduce the need for preexisting tumor inflammation, tumor antigenicity rather than baseline tumor inflammation might be important for the combinatorial efficacy. Our composite and multivariate analyses indicate that the four-gene inflammatory GES and TMB are independent from each other and further suggest that inflammatory GES and TMB are biomarkers associated with the efficacy of nivolumab monotherapy and nivolumab plus ipilimumab, respectively.
The results of these analyses should be interpreted with caution due to the limitations of this study, including the exploratory nature of the analyses and small sample sizes. Given its non-randomized nature, this study was not designed for a formal comparison of the nivolumab monotherapy and nivolumab plus ipilimumab cohorts. Additionally, due to the high response rate and long-term survival benefit observed in the nivolumab plus ipilimumab cohort, the numbers of non-responders and survival events were small. Any biomarker signal identified in this cohort should be interpreted with caution due to limited statistical power. Therefore, the results presented here should be considered hypothesis-generating only. Another important caveat of these analyses was that the study enrolled patients based on local MMR/MSI testing. A previous study found that higher TMB was no longer associated with nivolumab plus ipilimumab efficacy when excluding false-positive MSI-H/dMMR diagnoses identified via central assessment16, and thus our reliance on local testing might have influenced the biomarker associations observed in our analyses.
In summary, our biomarker analyses indicated that higher scores of inflammation-related GES were associated with improved response and survival benefit with nivolumab monotherapy, and higher TMB, TIB and degrees of MSI were associated with improved response and survival benefit with nivolumab plus ipilimumab in CheckMate 142; however, the small number of patients and exploratory nature of these analyses may limit interpretation of the results. These findings provide insights into the mechanisms of action of nivolumab and ipilimumab and warrant further investigation in larger, carefully controlled studies. The ongoing randomized phase 3 CheckMate 8HW trial (NCT04008030) comparing nivolumab plus ipilimumab with nivolumab monotherapy or chemotherapy in MSI-H/dMMR mCRC met both dual primary endpoints of PFS with nivolumab plus ipilimumab versus chemotherapy in the first-line setting (HR, 0.21; 95% CI, 0.14–0.32; P < 0.0001) and PFS with nivolumab plus ipilimumab versus nivolumab across all treatment lines (HR, 0.62; 95% CI, 0.48–0.81; P < 0.0003) in patients with centrally confirmed MSI-H/dMMR mCRC31,32,33. Considering the improvement in PFS observed with nivolumab plus ipilimumab versus nivolumab, biomarker-driven approaches may help identify patients who are more likely to benefit from single- or dual-agent immunotherapy in this tumor indication, and the CheckMate 8HW trial offers an opportunity to further explore these biomarkers in a larger randomized trial.
Methods
Study design
The study design of CheckMate 142 (NCT02060188) has been reported previously9,10. Briefly, adult patients with histologically confirmed metastatic/recurrent CRC with tumors locally assessed as dMMR and/or MSI-H and who had progressed on/after or been intolerant of at least one prior line of treatment were enrolled and received nivolumab monotherapy or nivolumab plus ipilimumab. Patients in the CheckMate 142 study who provided appropriate consent for the biomarker testing with evaluable baseline tumor tissue and matched whole-blood samples that passed the quality control criteria were eligible for the WES analyses, and those with evaluable baseline tumor samples that passed the quality control criteria were eligible for the RNA-seq analyses. The study was conducted in accordance with the Declaration of Helsinki and Good Clinical Practice guidelines. The study protocol and amendments were approved by the institutional review board or independent ethics committee at each study site (Supplementary Table 1), and all patients provided written informed consent before enrollment.
Efficacy assessments
The primary endpoint of ORR per INV was defined as the number of patients with a best overall response of complete response or partial response divided by the number of treated patients per Response Evaluation Criteria in Solid Tumors version 1.1. Other key efficacy endpoints were PFS per INV, defined as the time from the first dose to the first documented progression or death resulting from any cause, and OS, defined as the time from the first dose to death9,10.
Biomarker sampling
Tumor tissue and whole-blood samples were collected from consenting patients as specified by the protocol. For all biomarker-evaluable patients, baseline samples were assessed for biomarkers in an exploratory and retrospective manner using the following methodologies: WES, RNA-seq and IHC. RNA and DNA from tissue samples were co-exacted for RNA-seq and WES analysis, respectively, using the AllPrep DNA/RNA FFPE Kit (Qiagen, Germantown, MD, USA).
Whole-exome sequencing
Baseline tumor tissue and matched whole-blood samples were processed using the Agilent SureSelect Human All Exon V5 in-solution hybrid capture panel (Agilent, Santa Clara, CA) and underwent subsequent next-generation sequencing (NGS) on the Illumina NovaSeq platform (Illumina, San Diego, CA). Sequence alignment and variant calling were performed using a published WES processing pipeline based on Human Build 37 (GRCh37)34.
TMB is defined as the total number of somatic missense mutations and expressed as mutations/Mb, converted based on a linear regression model established in an assay bridging study34. TIB is defined as the total number of small insertions and deletions (indels) called by Strelka35. The degree of MSI was quantified using MSIsensor score (microsatellite instability level) derived from WES data using MSIsensor36. The MSIsensor score is a well-established tool to quantify tumor MSI on a continuous scale from sequencing data37. Median cutoffs were used for patient subgroup classification (high degree of MSI: ≥23.45%; low degree of MSI: <23.45%; high TIB, ≥804.00 indels; low TIB, <804.00 indels); a 20 mutations/Mb cutoff was used to define TMB-high (≥20 mutations/Mb) and TMB-low (<20 mutations/Mb) tumors given the high TMB in MSI-H patients and the TMB distribution observed in these cohorts (Supplementary Fig. 4).
RNA sequencing
Baseline tumor tissue samples were processed using the Illumina TruSeq RNA Access in-solution hybrid capture panel (Illumina, San Diego, CA) and underwent subsequent NGS on the Illumina NovaSeq platform. All gene expression signatures listed in Supplementary Table 2 were derived from RNA-seq data. Median cutoffs were used for patient subgroup classification (low versus high expression).
Raw RNA-seq reads were aligned and filtered using STAR (v2.6.0c)38. After removal of microbial contaminants, sequences were aligned to the human reference genome GRCh38 using the Ensembl 91 gene model, and read counts were quantified using RNA-seq by expectation-maximization. Sequencing quality was assessed using the Picard QC tool kit (v1.14) and dupRadar39 to ensure adequate transcriptome coverage and quantify polymerase chain reaction artifacts. Samples with Picard MarkDuplicates Estimated Library Size <2 million or DupRadar Deduplicated Dynamic Range <265 were excluded. Quantified raw counts from the remaining samples were normalized using edgeR’s40 trimmed mean of M-values method, and normalized counts per million were log2-transformed for further analysis.
GES scores were calculated from the normalized gene expression data by first z-score (normalized to a mean of 0 and a standard deviation of 1) across all patients in the RNA-seq–evaluable samples. For each patient, the gene signature score was then defined as the median over the selected genes of these z-scored normalized expression values.
Immunohistochemistry
A multiplex IHC assay (CD68, PD-L1, CD3) using an anti-CD3 antibody (mouse clone LN10) was used to interrogate CD3 T-cell infiltration in formalin-fixed, paraffin-embedded tumor tissue samples. Median cutoff was used for patient subgroup classification (CD3-high: ≥7.4%; CD3-low: <7.4%).
Statistical analyses
Baseline patient characteristics were reported using descriptive statistics. Associations between continuous variables and objective response were evaluated using two-sided Wilcoxon rank-sum tests (R function wilcox.test). Associations between categorical variables and ORR were evaluated using two-sided Fisher’s exact tests (R function fisher.test). Odds ratios and corresponding 95% CIs for biomarker associations with ORR were assessed using logistic regression. Kaplan-Meier curves were generated by survminer (v0.4.8). Forest plots of HRs and corresponding 95% CIs for biomarker associations with PFS and OS were assessed using Cox proportional-hazard models from R survival package (v3.2.7). Composite multivariate analysis was conducted by fitting multivariable logistic regression models using the following R formula: ORR ~ TMB + BMS4Gene + sex + age + Eastern Cooperative Oncology Group performance status. A similar formula was used for PFS and OS analysis by fitting multivariable Cox PH models. All P values calculated were nominal (not adjusted for multiple testing) and descriptive and were not intended to show statistical significance. All statistical analyses were performed with R software (v4.0.3). The unsupervised hierarchical baseline biomarker clustering analysis was conducted using Spearman’s correlation coefficient for distance and ward.D2 as the clustering method, and displayed using ComplexHeatmap (v2.6.2)41. The clustering was separately applied to the nivolumab monotherapy and nivolumab plus ipilimumab cohorts. Correlation between biomarkers was calculated using Spearman’s correlation and displayed using corrplot (v0.84). Measurements were taken from distinct samples.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
DNA and RNA sequencing data have been deposited in the European Genome-phenome Archive (EGA) under accession number EGAS50000000416. Sequencing data is stored under restricted access to protect patient privacy. Access to this data may be requested through the EGA website by submitting a form to the Data Access Committee (DAC) EGAC00001003376. Bristol Myers Squibb will honor legitimate requests for our clinical trial data from qualified researchers with a clearly defined scientific objective. Consistent with expectations of good scientific practice, researchers can request access to data from our studies by providing a research proposal with a commitment to publish their findings. The research proposal is reviewed by an independent review panel. We share data from Phase 2-4 interventional clinical trials completed on or after 1 January 2008 and evaluate medicines and indications approved in the US, EU and other designated markets. Data shared may include nonidentifiable patient-level and study-level clinical trial data, full clinical study reports and protocols. Sharing is subject to protection of patient privacy and respect for the patient’s informed consent, and publication of the primary results in peer-reviewed journals. Bristol Myers Squibb reserves the right to update and change criteria at any time. Other criteria may apply, for details please visit Bristol Myers Squibb at www.vivli.org. The remaining data are available within the Article, Supplementary Information, or Source Data file. Source data are provided with this paper.
References
Sung, H. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71, 209–249 (2021).
Gutierrez, C., Ogino, S., Meyerhardt, J. A. & Iorgulescu, J. B. The prevalence and prognosis of microsatellite instability-high/mismatch repair-deficient colorectal adenocarcinomas in the United States. JCO Precis Oncol. 7, e2200179 (2023).
Ali, S. M. et al. MSI-high and MSI-stable colorectal carcinomas (CRC): a comprehensive genomic profiling (CGP) study. J. Clin. Oncol. 36, 3574–3574 (2018).
Venderbosch, S. et al. Mismatch repair status and BRAF mutation status in metastatic colorectal cancer patients: a pooled analysis of the CAIRO, CAIRO2, COIN, and FOCUS studies. Clin. Cancer Res. 20, 5322–5330 (2014).
Andre, T. et al. Nivolumab plus low-dose ipilimumab in previously treated patients with microsatellite instability-high/mismatch repair-deficient metastatic colorectal cancer: 4-year follow-up from CheckMate 142. Ann. Oncol. 33, 1052–1060 (2022).
Andre, T. et al. Pembrolizumab in microsatellite-instability-high advanced colorectal cancer. N. Engl. J. Med. 383, 2207–2218 (2020).
Le, D. T. et al. Phase II open-label study of pembrolizumab in treatment-refractory, microsatellite instability-high/mismatch repair-deficient metastatic colorectal cancer: KEYNOTE-164. J. Clin. Oncol. 38, 11–19 (2020).
Lenz, H. J. et al. First-line nivolumab plus low-dose ipilimumab for microsatellite instability-high/mismatch repair-deficient metastatic colorectal cancer: the phase II CheckMate 142 study. J. Clin. Oncol. 40, 161–170 (2022).
Overman, M. J. et al. Durable clinical benefit with nivolumab plus ipilimumab in DNA mismatch repair-deficient/microsatellite instability-high metastatic colorectal cancer. J. Clin. Oncol. 36, 773–779 (2018).
Overman, M. J. et al. Nivolumab in patients with metastatic DNA mismatch repair-deficient or microsatellite instability-high colorectal cancer (CheckMate 142): an open-label, multicentre, phase 2 study. Lancet Oncol. 18, 1182–1191 (2017).
Overman, M. J. et al. Nivolumab (NIVO) ± ipilimumab (IPI) in patients (pts) with microsatellite instability-high/mismatch repair-deficient (MSI-H/dMMR) metastatic colorectal cancer (mCRC): five-year follow-up from CheckMate 142. J. Clin. Oncol. 40, 3510 (2022).
OPDIVO (nivolumab) [prescribing information]. Princeton, NJ, USA: Bristol Myers Squibb. https://packageinserts.bms.com/pi/pi_opdivo.pdf (2025).
OPDIVO (nivolumab) [summary of product characteristics]. Dublin, Ireland: Bristol Myers Squibb. https://www.ema.europa.eu/en/documents/product-information/opdivo-epar-product-information_en.pdf (2025).
Cervantes, A. et al. Metastatic colorectal cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up. Ann. Oncol. 34, 10–32 (2023).
Gallois, C. et al. Transcriptomic signatures of MSI-high metastatic colorectal cancer predict efficacy of immune checkpoint inhibitors. Clin. Cancer Res. 29, 3771–3778 (2023).
Ratovomanana, T. et al. Prediction of response to immune checkpoint blockade in patients with metastatic colorectal cancer with microsatellite instability. Ann. Oncol. 34, 703–713 (2023).
Llosa, N. J. et al. The vigorous immune microenvironment of microsatellite instable colon cancer is balanced by multiple counter-inhibitory checkpoints. Cancer Discov. 5, 43–51 (2015).
Giannakis, M. et al. Genomic correlates of immune-cell infiltrates in colorectal carcinoma. Cell Rep. 15, 857–865 (2016).
Mandal, R. et al. Genetic diversity of tumors with mismatch repair deficiency influences anti-PD-1 immunotherapy response. Science 364, 485–491 (2019).
Schrock, A. B. et al. Tumor mutational burden is predictive of response to immune checkpoint inhibitors in MSI-high metastatic colorectal cancer. Ann. Oncol. 30, 1096–1103 (2019).
Carbone, D. P. et al. First-line nivolumab in stage IV or recurrent non-small-cell lung cancer. N. Engl. J. Med. 376, 2415–2426 (2017).
Cristescu, R. et al. Pan-tumor genomic biomarkers for PD-1 checkpoint blockade-based immunotherapy. Science 362, (2018).
Ott, P. A. et al. T-cell-inflamed gene-expression profile, programmed death ligand 1 expression, and tumor mutational burden predict efficacy in patients treated with pembrolizumab across 20 cancers: KEYNOTE-028. J. Clin. Oncol. 37, 318–327 (2019).
Wang, F. et al. Safety, efficacy and tumor mutational burden as a biomarker of overall survival benefit in chemo-refractory gastric cancer treated with toripalimab, a PD-1 antibody in phase Ib/II clinical trial NCT02915432. Ann. Oncol. 30, 1479–1486 (2019).
Wu, H. X. et al. Tumor mutational and indel burden: a systematic pan-cancer evaluation as prognostic biomarkers. Ann. Transl. Med. 7, 640 (2019).
Lei, M. et al. Analyses of PD-L1 and inflammatory gene expression association with efficacy of nivolumab +/- ipilimumab in gastric cancer/gastroesophageal junction cancer. Clin. Cancer Res. 27, 3926–3935 (2021).
Vanhersecke, L. et al. Mature tertiary lymphoid structures predict immune checkpoint inhibitor efficacy in solid tumors independently of PD-L1 expression. Nat. Cancer 2, 794–802 (2021).
Havel, J. J., Chowell, D. & Chan, T. A. The evolving landscape of biomarkers for checkpoint inhibitor immunotherapy. Nat. Rev. Cancer 19, 133–150 (2019).
Chen, D. S. & Mellman, I. Oncology meets immunology: the cancer-immunity cycle. Immunity 39, 1–10 (2013).
Tarhini, A. A. et al. Immune monitoring of the circulation and the tumor microenvironment in patients with regionally advanced melanoma receiving neoadjuvant ipilimumab. PLoS One 9, e87705 (2014).
Andre, T. et al. Nivolumab (NIVO) plus ipilimumab (IPI) vs chemotherapy (chemo) as first-line (1L) treatment for microsatellite instability-high/mismatch repair-deficient (MSI-H/dMMR) metastatic colorectal cancer (mCRC): first results of the CheckMate 8HW study. J. Clin. Oncol. 42, LBA768–LBA768 (2024).
André, T. et al. Nivolumab plus Ipilimumab in Microsatellite-Instability–High Metastatic Colorectal Cancer. N. Engl. J. Med. 391, 2014–2026 (2024).
André, T. et al. Nivolumab plus ipilimumab versus nivolumab in microsatellite instability-high metastatic colorectal cancer (CheckMate 8HW): a randomised, open-label, phase 3 trial. Lancet 405, 383–395 (2025).
Chang, H. et al. Bioinformatic methods and bridging of assay results for reliable tumor mutational burden assessment in non-small-cell lung cancer. Mol. Diagn. Ther. 23, 507–520 (2019).
Saunders, C. T. et al. Strelka: accurate somatic small-variant calling from sequenced tumor-normal sample pairs. Bioinformatics 28, 1811–1817 (2012).
Niu, B. et al. MSIsensor: microsatellite instability detection using paired tumor-normal sequence data. Bioinformatics 30, 1015–1016 (2014).
Johansen, A. F. B. et al. Validation of computational determination of microsatellite status using whole-exome sequencing data from colorectal cancer patients. BMC Cancer 19, 971 (2019).
Dobin, A. et al. STAR: ultrafast universal RNA-seq aligner. Bioinformatics 29, 15–21 (2013).
Sayols, S., Scherzinger, D. & Klein, H. dupRadar: a Bioconductor package for the assessment of PCR artifacts in RNA-Seq data. BMC Bioinforma. 17, 428 (2016).
Robinson, M. D., McCarthy, D. J. & Smyth, G. K. edgeR: a Bioconductor package for differential expression analysis of digital gene expression data. Bioinformatics 26, 139–140 (2010).
Gu, Z., Eils, R. & Schlesner, M. Complex heatmaps reveal patterns and correlations in multidimensional genomic data. Bioinformatics 32, 2847–2849 (2016).
Acknowledgements
We thank the patients and their families who made this study possible, the investigators and the clinical study teams (including Karolina Kolodziejska who served as the Global Trial Manager, and Lixian Jin who was the Clinical Trial Physician); Danielle Greenawalt, David Balli, Tracy Tang, Jun Li, Meeta Panda, Carlos Mackintosh and Alex Cao who all supported the execution of these biomarker analyses; and Bristol Myers Squibb (Princeton, NJ, USA) and Ono Pharmaceutical Company, Ltd. (Osaka, Japan). This study was supported by Bristol Myers Squibb. Scott Kopetz discloses support for this work from the National Cancer Institute Cancer Center Support Grant (award number P30CA016672). Medical writing and editorial assistance were provided by Nitesh Sule, PhD, of Parexel, funded by Bristol Myers Squibb.
Author information
Authors and Affiliations
Contributions
M.L., M.O., S.A., R.N., and S. Kopetz were responsible for the conceptualization of the study. M.L., M.O., R.R.J., and S. Kopetz contributed to the methodology. M.O., T.A., S.L., H.-J.L., M.A., F.G., R.M., M.W., M.M., E.V.C., A. Hendlisz, D.C., B.N., A. Hill, A.K., F.C., S. Kochuparambil, and S. Kopetz conducted the investigation. M.L., J.Y., R.R.J., and B.H. undertook data curation. J.Y. and B.H. were responsible for formal analysis. All authors contributed to and approved the manuscript.
Corresponding authors
Ethics declarations
Competing interests
M. Lei reports employment and stocks from Bristol Myers Squibb; and patents, PCT/US2020/025456, PCT/US2020/025441, and Methods of treating tumor application number 63328715. M. Overman reports consulting roles at 3D Medicines, Array BioPharma, Bristol Myers Squibb, Eisai, Gritstone Bio, Janssen, MedImmune, Merck, Novartis, Pfizer, Roche/Genentech, and Simcere; and research funding from Bristol Myers Squibb, MedImmune, Merck, and Roche. J. Yao reports employment and stocks from Bristol Myers Squibb. T. André reports consulting roles at AbbVie, Aptitude Health, Bristol Myers Squibb, Gilead Sciences, GlaxoSmithKline, MSD Oncology, Nimbus Therapeutics, Nordic Bioscience, Pfizer, Seagen, Servier, and Takeda; honoraria from Bristol Myers Squibb, Merck, Merck Serono, Sanofi, Seagen, and Servier; travel support from Bristol Myers Squibb, MSD Oncology, and Takeda; uncompensated relationships with Adjuvant Colon Cancer End Points (ACCENT) Collaborative Group and ARCAD Foundation; and other relationship with Ispima. S. Lonardi reports honoraria from Amgen, Bristol Myers Squibb, GlaxoSmithKline, Incyte, Lilly, Merck Serono, MSD Oncology, Pierre Fabre, Roche, and Servier; consulting roles at Amgen, Astellas Pharma, Bayer, Beigene, Bristol Myers Squibb, Daiichi Sankyo, GlaxoSmithKline, Heylon, Incyte, Lilly, Merck Serono, Merck Sharp & Dohme, Nimbus Therapeutics, Rottapharm Biotech, Servier, and Takeda; and research funding from Amgen, AstraZeneca, Bayer, Bristol Myers Squibb, Lilly, Merck Serono, and Roche. H.-J. Lenz reports honoraria from AbbVie, Adagene, Bayer, Boehringer Ingelheim, Fulgent Genetics, Jansen Oncology, Jazz Pharmaceuticals, Merck Serono, Merus and Roche; consulting roles at 3 T BioSciences, AbbVie, Adagene, Bayer, Bristol Myers Squibb, Fulgent Genetics, GlaxoSmithKline, Merck Serono and Roche; and travel support from Bayer, Bristol Myers Squibb and Merck Serono. M. Aglietta reports consulting roles at Bristol Myers Squibb, Merck, and Roche; travel support from Bristol Myers Squibb, Merck, and Tesaro; and research funding from AstraZeneca. R. McDermott reports honoraria from Astellas, Bristol Myers Squibb, Ipsen, Janssen, and Merck Sharpe & Dohme; and travel support from Bayer, Novartis and Pfizer. M. Wong reports a consulting role at MSD Oncology; and honoraria from MSD Oncology and Sirtex Medical. M. Morse reports honoraria from Pfizer and Taiho Pharmaceutical. E. Van Cutsem reports consulting roles at AbbVie, Agenus, ALX Oncology, Amgen, Arcus Biosciences, Astellas Pharma, AstraZeneca, Bayer, BeiGene, BioNTech, Boehringer Ingelheim, Bristol Myers Squibb, Daiichi Sankyo, Debiopharma Group, Eisai, ElmediX, GlaxoSmithKline, Hookipa Biotech, Incyte, Ipsen, Lilly, Merck KGaA, Merck Sharp & Dohme, Mirati Therapeutics, Nordic Group, Novartis, Pfizer, Pierre Fabre, Roche, Seagen, Servier, Simcere, Taiho Pharmaceutical, Takeda, and TERUMO. D. Cardin reports honoraria from OncLive/MJH Life Sciences; consulting role at Clarivate and The KOL Connection Ltd.; and research funding from Array BioPharma, Corcept Therapeutics, Elicio Therapeutics, Lilly, Novartis, Rafael Pharmaceuticals, and Xbiotech. B. Neyns reports consulting roles at Bristol Myers Squibb, Merck Sharp & Dohme, Novartis, and Pierre Fabre; research funding from Novartis; and travel support from Merck Sharp & Dohme and Pierre Fabre. A. Hill reports employment and stocks from Tasman Oncology. R.R. Jenq reports consulting roles at MaaT Pharma and Prolacta Bioscience; patent royalties from Seres Therapeutics; and stocks from Postbiotics Plus and Seres Therapeutics. S. Abdullaev reports employment and stocks from Bristol Myers Squibb. B. He reports employment and stocks from Bristol Myers Squibb/Celgene. R. Novosiadly reports employment at Bristol Myers Squibb and stocks from Bristol Myers Squibb and Eli Lilly. S. Kopetz reports consulting roles at Agenus, Amgen, AmMax Bio, Arcus Biosciences, AstraZeneca, Aveo, Bayer Health, Beigene, Boehringer Ingelheim, Bridgebio, Bristol Myers Squibb/Medarex, Carina Biotech, Clasp Therapeutics, Cytovation, Dewpoint Therapeutics, EMD Serono, Flame Biosciences, Frontier Medicines, Genentech, Harbinger Oncology Inc, Ikena Oncology, Kestrel Therapeutics, Marengo Therapeutics, Merck, Mirati Therapeutics, Pfizer, Replimune, Revolution Medicines, Roche, SageMedic, Servier, Sibylla, T-Cypher Bio, Tachyon Therapeutics, Xaira Therapeutics and Zentalis; research funding from Amgen, Boehringer Ingelheim, BridgeBio, Daiichi Sankyo, EMD Serono, Genentech/Roche, Guardant Health, Lilly, Pfizer and Zentalis; and stocks from Frontier Medicines, Lutris and Navire. All other authors have nothing to report.
Peer review
Peer review information
Nature Communications thanks the anonymous reviewers for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lei, M., Overman, M.J., Yao, J. et al. Inflammation and mutational burden differentially associated with nivolumab or ipilimumab combination efficacy in colorectal cancer. Nat Commun 16, 8868 (2025). https://doi.org/10.1038/s41467-025-63960-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-025-63960-8